Introduction
Primary hematological malignancy of the uterine
cervix is rare and thus, the literature regarding the disease is
primarily limited to case reports and small case series, to the
best of the authors' knowledge (1–5). The
uterine cervix was previously identified to be involved in one out
of 730 cases of non-Hodgkin's lymphoma (NHL) and 1 out of 175 cases
of extra-nodal lymphoma in the UK in 1974 (1). Furthermore, myeloid sarcoma (MS) was
observed in 3–5% of the patients with acute myeloid leukemia (AML)
(5). There are ~0.7 per 1,000,000
young individuals who are diagnosed with MS and ~2 per 1,000,000
individuals in the adult population who are diagnosed with MS
(5). The most common symptom of MS
is vaginal bleeding, thus, the pathological diagnosis of NHL and MS
is very important. In the present case report, the pathological
reports of three patients with NHL and two patients with MS are
described. Immunohistochemical (IHC) staining demonstrated the
presence of B-lymphoid in the patients with NHL and the presence of
myeloid lineage markers in the patients with MS. The cancer of the
patients was managed with chemotherapy and either
radiotherapy/surgery alone or together. Hematopoietic stem cell
transplantation (HSCT) may improve the prognosis for patients with
MS. For example, Chen et al (6) reported that 4 patients with MS
underwent allogeneic HSCT (allo-HSCT). Among them, 3 patients
remained alive with complete remission (CR) (6).
Case report
Case 1
A 65-year-old female was admitted to The Department
of Obstetrics and Gynecology at The Shanxi Tumor Hospital (Shanxi,
China) in January 2016 after 2 weeks of post-menopausal vaginal
bleeding. A biopsy of the cervical mass identified the presence of
a suspicious uterine cervical cancer. A physical examination
demonstrated no evidence of superficial lymph node enlargement or
hepatosplenomegaly. A gynecological examination demonstrated that
the uterine cervix was 6 cm in size and featured an endogenous
mass; a mass had grown on the inside of the cervical canal, which
could not be seen from the outside of the cervix. Laboratory tests
demonstrated that the hemoglobin (HGB) count was 140 g/l, the white
blood cell (WBC) count was 6.2×109/l and the platelet
(PLT) count was 3.8×1011/l. The lactate dehydrogenase
(LDH), β2-microglobulin (β2MG), liver and renal function,
coagulation test, Epstein Barr virus (EBV), cytomegalovirus (CMV)
and erythrocyte sedimentation rate (ESR) results were all normal.
There was no detectable abnormity in the bone marrow (BM) smear, BM
biopsy (BMB) or flow cytometry (FCM) analysis of the BM cells.
Computerized tomography (CT) demonstrated bilateral inguinal,
para-iliac vessels and retroperitoneal lymph node enlargement
(maximum lymph node size was 0.8×0.9 cm). The patient underwent
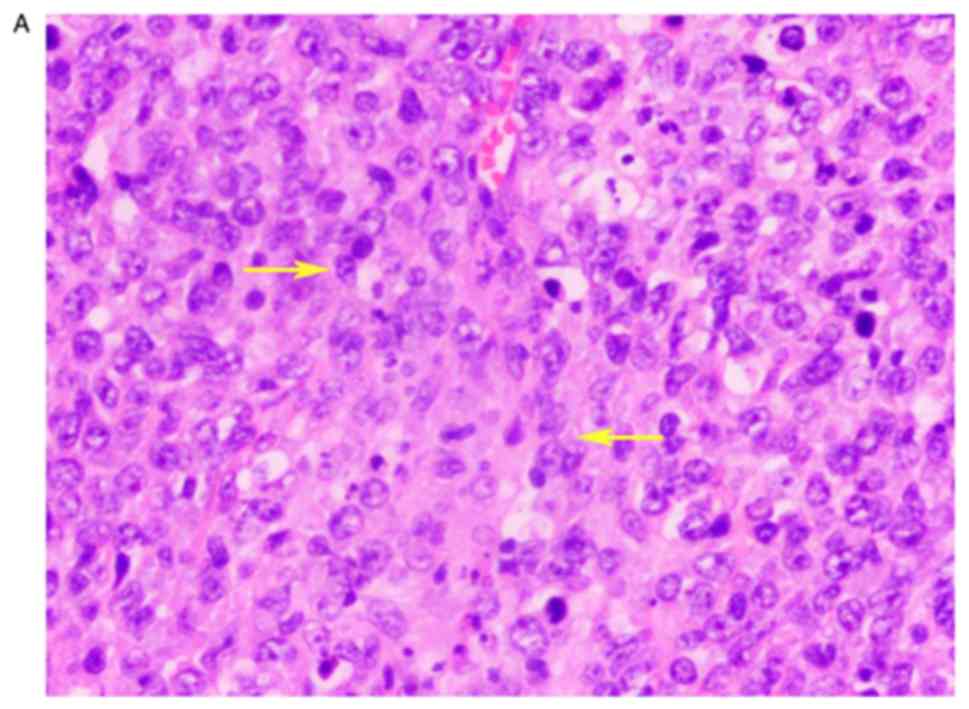
adnexectomy and resection of pelvic lymph nodes. A pathological
examination identified diffuse large B cell lymphoma (DLBCL) of the
uterine cervix (Fig. 1). The tumor
was 6×5×4 cm and was involved in full-thickness cervical stromal
invasion. Chronic endometritis and reactive hyperplasia of 31
pelvic lymph nodes were confirmed. IHC staining demonstrated the
presence of cells that were positive for B-lymphocyte antigen CD20
(CD20), Myc proto-oncogene protein (c-Myc), B-cell lymphoma
(Bcl)-2, Bcl-6, multiple myeloma oncogene1 (MUM1), tumor protein
p63 (p63) and proliferation marker protein Ki-67 (Ki67)
80%+, and were negative for T-cell surface glycoprotein
CD3 ε chain (CD3), neprilysin (CD10), FcγRIII (CD16), neural cell
adhesion molecule 1 (CD56), cytokeratin (CAM5.2), cytokeratin pan
(AE)1/AE3 and myeloperoxidase (MPO). The patient was diagnosed with
primary DLBCL of the uterine cervix stage IIEA, with an
International Prognosis Index (IPI) score of 1 and an Eastern
Cooperative Oncology Group (ECOG) score of 1 (7). The patient received a regimen of
rituximab (R)-cyclophosphamide, pirarubicin, vincristine and
dexamethasone (R-CHOP) for six cycles. CR was achieved, and R-CHOP
was administered for two additional cycles. A follow-up of the
patient was conducted after 35 months with no evidence of
recurrence.
Case 2
A 43-year-old female was admitted to The Department
of Obstetrics and Gynecology at the Shanxi Tumor Hospital in
January 2005 with a 1-year history of increased leucorrhea and
contact vaginal bleeding. Gynecological and ultrasound examinations
identified the presence of a 4.4×5.1 cm mass of the uterine cervix.
The laboratory tests demonstrated that the routine blood, liver and
renal function, coagulation test, LDH and β2MG results
were all normal. The patient underwent adnexectomy resection of a 4
cm mass between the uterine cervix and the upper section of the
vagina. A pathological examination demonstrated mucosa-associated
lymphoid tissue lymphoma (MALToma) of the uterine cervix,
endometrial proliferation, reactive hyperplasia of 9 pelvic lymph
nodes, and there was no evidence of abnormities in the vaginal
stump and ovary. IHC staining demonstrated that the cells were
positive for CD20, B-cell antigen receptor complex-associated
protein β chain and Ki67 10%+, and were negative for
CD3, AE1/AE3, muscle creatine kinase, p63, synapsin (Syn),
chromogranin A glycoprotein hormones α-chain (CGA) and myogenin.
The patient was transferred to The Department of Hematology at The
Shanxi Tumor Hospital. There was no evidence of superficial lymph
node enlargement or hepatosplenomegaly, and a BM smear/BMB did not
raise any cause for concern. The patient was diagnosed with primary
MALToma of the uterine cervix stage IEA, with an IPI score of 0 and
an ECOG score of 1. The patient received a regimen of CHOP with
etoposide for six cycles and achieved CR. The patient survived 82
months with no evidence of disease (NED) and was lost to follow-up
during 2012.
Case 3
A 36-year-old female was admitted to The Department
of Hematology at The Shanxi Tumor Hospital in January 2011 with a
1-month history of vaginal bleeding. A gynecological examination
identified a mass of 4×3 cm in the uterine cervix. A biopsy
demonstrated DLBCL of the cervical mass and chronic vaginitis of
the upper section of the vagina. According to the consultation with
the resident pathologists, IHC staining demonstrated that the cells
were positive for leukocyte common antigen (LCA), CD20, p63 and
Ki67 80%+ and were negative for CD3, CD56, casein kinase
II subunit α, MPO, epithelial membrane antigen (EMA), CGA, Syn and
human melanoma black 45. The pathologists agreed with the DLBCL
diagnosis. During the physical examination, no superficial lymph
node enlargement or hepatosplenomegaly was observed. The laboratory
tests demonstrated that routine blood LDH, β2MG, liver
and renal function, EBV, CMV and ESR were normal. A BM smear/BMB
did not raise any cause for concern. An ultrasound examination
identified a small myoma of the uterus. The patient was diagnosed
with primary DLBCL of the uterine cervix stage IEA with an IPI
score of 0 and an ECOG score of 1. The patient received a regimen
of CHOP for six cycles and achieved CR. The patient survived for 73
months with NED.
Case 4
A 46-year-old female received a routine health
examination. The gynecological examination identified a mass of 6×5
cm of the uterine cervix. The left upper section of the vaginal
wall was possibly involved. The uterus was 7×5 cm and left
parametric narrow. The patient was admitted to The Department of
Obstetrics and Gynecology at The Shanxi Tumor Hospital in December
2012. A physical examination did not identify any superficial lymph
node enlargement or hepatosplenomegaly. Laboratory tests
demonstrated that HGB 133 g/l, WBC 7.71×109/l, PLT
1.62×1011/l, LDH, β2MG, liver and renal
function, coagulation test, EBV, CMV and ESR were all normal. A BM
smear/BMB did not raise any cause for concern. FCM of BM did not
demonstrate any abnormal expression levels of CD10, CD14 or CD64.
An ultrasound examination identified a mass of 6×5 cm of the
uterine cervix and normal uterus. A biopsy of the mass in the
uterine cervix confirmed the diagnosis of MS. IHC staining
demonstrated that cells were positive for LCA, MPO, CD99
antigen-like protein 2 (CD99), CD117, lysozyme and Ki67
70%+, and were negative for CD3, T-cell surface
glycoprotein CD5, CD10, Sialyl-Lewis X (CD15), CD20, FcεRII, tumor
necrosis factor receptor superfamily member 8, hematopoietic
progenitor cell antigen CD34 (CD34), ADP-ribosyl cyclase/cyclic
ADP-ribose hydrolase 1 (CD38), macrosialin, anaplastic lymphoma
receptor tyrosine kinase receptor (ALK), ALK tyrosine kinase
receptor, Bcl-6, cell cycle protein D1, ubiquitin-conjugating
enzyme E2 D1, MUM1, myogenin, desmin, paired box protein Pax-5 and
terminal deoxynucleotide transferase. DNA
nucleotidylexotransferase. Histological analysis of the cervical
mass at The Beijing Friendship Hospital (Beijing, China)
demonstrated that the neoplastic cells were medium in size with
chromatin, with morphology and IHC features typically associated
with blasts, and the diagnosis confirmed MS. The clinical diagnosis
was primary MS of the uterine cervix stage IIEA, with an IPI score
of 0 and ECOG score of 1. At the request of the patient,
adnexectomy was performed. The uterine cervix was not resected due
to involvement of the left wall of the upper section of the vagina.
A pathological examination identified a myoma in the uterus. After
3 weeks, the patient complained of a yellow fluid coming from the
vagina. Consultation with an urologist confirmed ureteral vaginal
fistulas, whereas, a CT scan demonstrated left pyeloureterectasis.
Mild left hydronephrosis suggested that the patient required
surgery. The surgeon identified a severe lower ureteral stricture
and adhesion near the bladder. Left ureterocystostomy and
catheterization of the left ureter with a D-J tube were performed.
The patient was transferred to The Department of Hematology at The
Shanxi Tumor Hospital subsequent to pulling out the D-J tube. A BM
smear did not raise any cause for concern. A CT scan identified the
presence of a 4.4×3.2 cm mass in the right renal outer edge; right
iliac region lymph nodes (maximum lymph node size was 1.2 cm) and
left pyeloureterectasis. The patient received a regimen of
idarubicin and arabinoside (Ara-c) (IA) for three cycles, and a
regimen of aclacinomycin and Ara-c for two cycles. An ultrasound
examination identified mild bilateral hydronephrosis and right
upper ureterectasia. The patient achieved partial remission. The
patient was administered IA for three cycles and homoharringtonine
and Ara-c for one cycle, and achieved CR. After 3 months, an
ultrasound examination identified bilateral cervical, inguinal and
para-iliac vessels, lymph node enlargement, bilateral
hydronephrosis and bilateral ureterectasia. A regimen of
mitoxantrone and Ara-c (MA) was administered for two cycles. An
ultrasound examination identified the presence of a 4.2×4.5 cm mass
in the right pelvis with bilateral hydronephrosis. The BM smear was
normal. The patient succumbed to the cancer 21 months after
diagnosis.
Case 5
A 39-year-old female was admitted to The Department
of Obstetrics and Gynecology at The Shanxi Tumor Hospital in
February 2014 with a 5-day history of vaginal bleeding.
Gynecological examination identified a 6.9×5.4 cm mass of the
uterine cervix. An ultrasound examination identified a mass in the
uterine cervix and involvement of the lower section of the uterus.
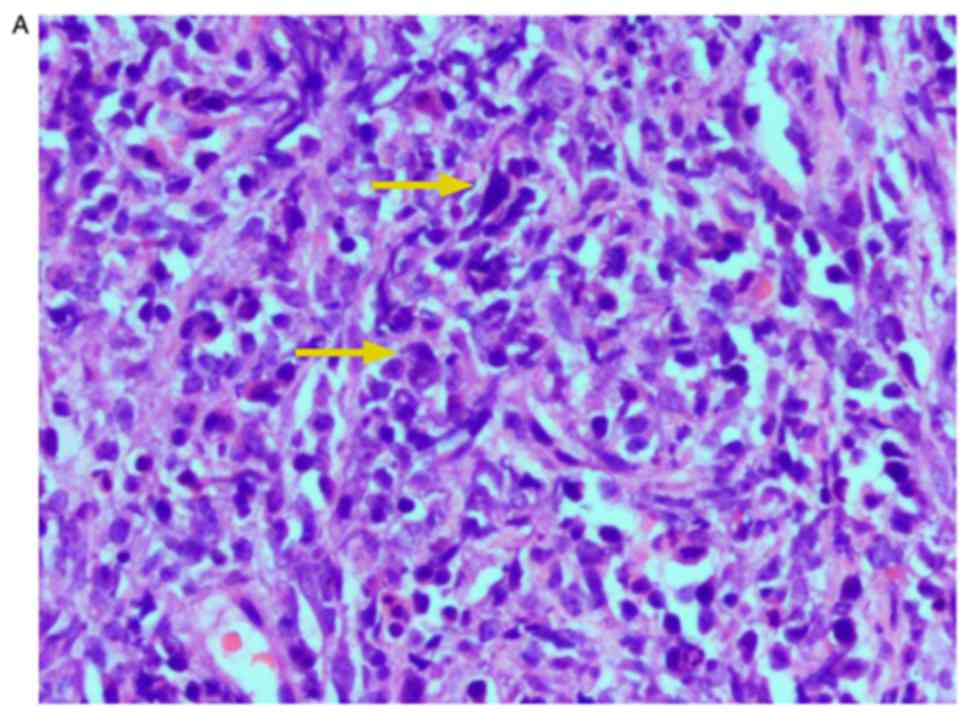
A biopsy identified medium size neoplastic cells. IHC staining
demonstrated that the cells were positive for LCA, MPO, CD34, CD38,
leukosialin (CD43), CD56, CD99, CD117, lysozyme and Ki67
80%+, and were negative for CD3, T cell antigen CD7,
cluster of differentiation 8, neprilysin (CD10), CD15, CD20,
AE1/AE3, CGA, Syn, desmin and vimentin. The pathological diagnosis
confirmed MS of the uterine cervix. Positron emission
tomography-computed tomography (PET-CT) demonstrated bilateral
cervical, near the abdominal aorta, right para-iliac vessel large
lymph nodes, and identified a 6.1×3.7-cm mass in the uterine cervix
in the lower part of the uterus. The standard uptake value maximum
was 6.79 and 4.63 for the uterine cervix and BM, respectively. The
laboratory test demonstrated counts of HGB 67 g/l, WBC
31.3×109/l, PLT 5.9×1010/l and LDH 1,014 U/l.
BM and a peripheral blood smear demonstrated the presence of
myeloblasts at 16 and 11%, respectively (Fig. 2). A BMB presented a cluster
distribution of myeloblasts. FCM of a BM smear demonstrated
positive expression of integrin αM, membrane alanyl aminopeptidase,
CD15, CD16, sialic acid binding Ig-like lectin 3, CD34, CD117 and
human leukocyte antigen-DR isotype, and was negative for CD10. The
patient was diagnosed with MS of the uterine cervix stage IVEA. The
patient received an IA regimen for four cycles and an MA regimen
for two cycles, and achieved CR. After 5 months, the patient
complained of hemorrhagic vaginal secretions. A BM smear
demonstrated blasts at 21.5% and AML was confirmed. The patient
received a regimen of IA and CIG regimen and (Ara-c, idarubicin and
human granulocyte colony stimulating factor) for two cycles each. A
BM smear, performed approximately 2 months later, demonstrated
blasts at 2%, which was a lower percentage than in the first BM
smear. The patient achieved CR. At the request of the patient,
adnexectomy was performed. A pathological diagnosis later
demonstrated chronic cervicitis, cervical erosion and endometrial
proliferation. After 6 months, the patient reported vaginal
hemorrhagic secretions discharges again. An ultrasound examination
demonstrated a mass in the vaginal stump. A BM smear identified
myeloblasts at 63.6%. The patient succumbed to the cancer 26 months
after the initial diagnosis (Table
I).
 | Table I.Clinical data for primary
hematological malignancy of uterine cervix. |
Table I.
Clinical data for primary
hematological malignancy of uterine cervix.
| Case number | Age, years | LDH, U/l | Stage | Mass of uterine
cervix, cm | Biopsy | Pathological
type | Treatment | Treatment
outcome | OS, months |
|---|
| 1 | 65 | 221 | IIEA | 6×2 | Yes | DLBCL | Surgery, CT | Alive with CR | 35 |
| 2 | 43 | 210 | IEA | 4.5 | No | MALToma | Surgery, CT | Alive with CR | 82a |
| 3 | 36 | 169 | IEA | 4×3 | Yes | DLBCL | CT | Alive with CR | 73 |
| 4 | 46 | 133 | IIEA | 6×5 | Yes | MS | Surgery, CT | Succumbed to
progressive disease | 21 |
| 5 | 39 | 1,014 | IVEA | 6.9×5.6 | Yes | MS | Surgery, CT | Succumbed to
leukemia | 26 |
Discussion
NHL affects extra-nodal sites in one-third of
primary hematological malignancies of the uterine cervix, and the
majority of the extra-nodal sites are present in the
gastrointestinal tract. Primary extra-nodal NHL of the uterine
cervix is extremely rare. The uterine cervix was previously
identified to be involved in one out of 730 cases of NHL and one
out of 175 cases of extra-nodal lymphoma (1). Primary MS of the uterine cervix is
additionally uncommon. These diseases were only reported in the
form of case reports and small case series (2–4). MS is
present in 3–5% of patients with AML and represents a disease which
is encountered in ~0.7 young individuals per 1,000,000 and 2 per
1,000,000 in the adult population (5). MS may occur de novo,
concurrently with AML or as blastic transformation of
myelodysplastic syndrome. Antecedent myeloid neoplasms or
concurrent AML is present in approximately two-thirds of the cases.
It was previously demonstrated that in 21 cases of MS, four cases
involved lesions in the uterine cervix and three of these patients
were diagnosed with antecedent AML (6,8).
Therefore, MS of the uterine cervix was secondary to AML. Frequent
sites of MS include the skin, lymph nodes, mediastinum,
gastrointestinal tract, bones, brain, ovary, uterine cervix and
testis (3,6).
The diagnosis of primary lymphoma of the uterine
cervix was determined by pathological evaluation; the disease was
additionally localized to the uterine cervix without evidence of
involvement of other organs or lymph nodes. Cases 1–4 were
confirmed to possess a primary malignancy. Case 5 was diagnosed
with an advanced stage cancer with BM involvement; BM and a
peripheral blood smear demonstrated the presence of myeloblasts was
<20% and therefore, AML was not diagnosed and primary MS was
considered. The majority of cervical lymphomas, as determined by
histological examination, are DLBCL with diffuse infiltration of
atypically large lymphoid cells (1).
IHC staining demonstrated that cells were positive for LCA, CD20,
Bcl-2, Bcl-6 and MUM1. IHC staining of the patient in case 1
demonstrated that cells were positive for c-Myc and Bcl-2. The
prognosis for cases involving the co-expression of these two
proteins is poor (9). Therefore,
case 1 received R in addition to the CHOP regimen and achieved CR,
although long-term follow-up is necessary. Histology of MS
demonstrated neoplastic cells were medium sized and consistently
had a blast-like morphology. IHC staining demonstrated positive
cells for LCA, CD34, CD38, CD43, CD117, MPO and lysozyme. Positive
expression of MPO, lysozyme and CD117 confirmed the diagnosis of
MS. Imaging modalities, including ultrasound, magnetic resonance
imaging and PET-CT, are useful in the detection of lymphoma in the
uterine cervix. PET-CT may be used for detecting early foci,
analyzing the extent of the disease and assessing the treatment
response (10,11).
The majority of primary cervical NHL cases are
either stage I or II. In such cases, the prognosis is considered to
be good, with an overall 5-year survival rate of 77%. These cases
were managed with pelvic radiotherapy or neoadjuvant chemotherapy,
successfully applied as a first line of treatment (2) Mouhajir et al (2) identified a case of primary NHL of the
uterine cervix treated with CHOP and external radiotherapy. The
patient achieved CR and survived 16 years with NED. According to
the previous study, chemotherapy based on CHOP alongside moderate
doses of radiation was deemed to be the most successful mode of
treatment (2). Similarly, in the
present study, case 3 achieved a favorable outcome from CHOP
chemotherapy alone. The addition of R may improve progression-free
survival (12). Case 1 received
R-CHOP for eight cycles and the effect of this treatment was
satisfactory. The prognosis of patients with cervical MS appears to
be poor, with <20% of cases surviving (4). MS is a highly aggressive type and with
a fulminant course. At present, chemotherapy is the main regimen
for AML and MS. Cases were treated with a standard induction
regimen for AML and achieved CR, although they eventually succumbed
to the progressive disease. However, prognosis may be improved if
such individuals were to undergo allo-HSCT. Recently, a 40-year-old
female patient with MS of the larynx who additionally presented
with AML-M2 was treated at The Shanxi Tumor Hospital. Following CR,
the patient underwent allo-HSCT. At the time of writing, 36 months
had passed since transplantation and the patient continues to
experience CR. In previous unpublished data, Chen et al
(6) identified three cases of
ovarian and vulvae MS with AML. Allo-HSCT improved the prognosis of
these patients. Therefore, allo-HSCT requires consideration for
patients with MS following CR.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the author upon reasonable request.
Authors' contributions
WG collected and analyzed the clinical data,
reviewed the literature, designed the study, drafted the work and
revised it critically for important intellectual content. JL was
responsible for the pathological diagnosis. ZZ analyzed the results
of the bone marrow smear. LW, JZ and LM participated in the
collection of clinical data. LS participated in the design of the
study. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Informed consent was obtained from the patients and
their families for the publication of this data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sharma V, Dora T, Patel M, Sancheti S and
Sridhar E: Case report of diffuse large B cell lymphcma of uterine
cervix treated at a Semiurban Cancer Center in North India. Case
Rep Hematol. 2016:30425312016.PubMed/NCBI
|
|
2
|
Mouhajir N, Diakité A, Toulba A, Hemmich
M, Saadi I, Elkacemi H, Kebdani T and Benjaafar N: Primary
non-hodgkin lymphoma of the uterine cervix: case report of
long-term survival patient. J Obstet Gynaecol India. 64 (Suppl
1):S145–S147. 2014. View Article : Google Scholar
|
|
3
|
Parnis J, Camilleri DJ, Babic D, DeGaetano
J and Savona-Ventura C: Lymphoma of the cervix. Case Rep Hematol.
2012:3261272012.PubMed/NCBI
|
|
4
|
Gill H, Loong F, Mark V, Chan K, Au WY and
Kwong YL: Myeloid sarcoma of the uterine cervix presenting as
missed abontion. Arch Grnecol Obstet. 286:1339–1341. 2012.
View Article : Google Scholar
|
|
5
|
Gunyeli I, Kose SA, Ozkaya O, Kose AG,
Karabulut A and Kapucuoglu N: Granulocytic sarcoma of the cervix:
Is hysterectomy necessary? J Obstet Gynaecol. 35:315–316. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chen DB, Zhang H, Zhang YH, Wang Y, Song
QJ, Yang SM, Cui H, Zhao Y, Fang XZ and Shen DH: Analysis of
proliferative lesions of haematopoietic and lymphoid tissue in the
female productive tract. Zhonghua Fu Chan Ke Za Zhi. 53:263–269.
2018.(In Chinese). PubMed/NCBI
|
|
7
|
Sehn LH, Berry B, Chhanabhai M, Fitzgerald
C, Gill K, Hoskins P, Klasa R, Savage KJ, Shenkier T, Sutherland J,
et al: The revised International Prognostic Index (R-IPI) is a
better predictor of outcome than the standard IPI for patients with
diffuse large B-cell lymphoma treated with R-CHOP. Blood.
109:1857–1861. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jiang YJ, Wang HX, Zhuang WC, Chen H,
Zhang C, Li XM, Zhu GH and He Y: Clinical and pathologic features
of myeloid sarcoma. Zhongguo Shi Yan Xue Ye Xue Za Zhi. 25:926–931.
2017.(In Chinese). PubMed/NCBI
|
|
9
|
Yu WJ, Cao LH, Wang JH, Wang ZM, Qian WB,
Tong HY, Meng HT, Mai WY, Mao LP, Qian JJ and Jin J: Prognostic
significance of proteins expression by immunohistochemical method
in diffuse large B cell lymphoma. Zhonghua Xue Ye Xue Za Zhi.
38:784–788. 2017.(In Chinese). PubMed/NCBI
|
|
10
|
Zheng LC, OuYang XL, Zhang WJ, Liu GC and
Zhang XM: 18F-FDG PET/CT of primary cervical granulocytic sarcoma.
Clin Nucl Med. 40:917–918. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Korivi BR, Jensen CT, Patnana M, Patel KP
and Bathala TK: A rare presentation of lymphoma of the cervix with
cross-sectional imaging correlation. Case Rep Radiol.
2014:1572682014.PubMed/NCBI
|
|
12
|
Baijal G, Vadiraja BM, Fernandles DJ and
Vidyasagar MS: Diffuse large B-cell lymphoma of the uterine cervix:
A rare case managed novelly. J Cancer Res Ther. 5:140–142. 2009.
View Article : Google Scholar : PubMed/NCBI
|