Introduction
Phyllodes tumor (PT) was first described in 1838 by
the German physician Johannes Müller as cystosarcoma
phyllodes (1). The name
‘phyllodes’ derives from the Latin Phyllodium and means
‘leaf-like’ which relates to its morphology under the microscope
(2). Phyllodes tumors of the breast
(PTB) are rare, accounting for less than 1% of breast neoplasms
overall (3) which translates into
about 500 cases diagnosed in the USA annually (4). The mean age of diagnosed patients is 40
years old, which is lower than patients with conventional breast
carcinomas (2). PTBs are classified
into three categories: Benign, borderline and malignant (5). Malignant lesions with the ability to
metastasize distantly can be observed in 30% of cases (6). Recommended treatment includes wide
excision with clear margins and prognosis depends on the
histological analysis of the mesenchymal component (7). Benign histology, negative tumor margins
and an absence of residual disease after initial treatment and
radiation therapy have been determined as favorable prognostic
factors (8). The main problem in the
treatment and management of PTB is its local recurrence in both
benign and malignant cases (2). With
no prospective trials of chemotherapy for malignant phyllodes
tumors (MPT), the utility of drug treatment remains unclear and
requires more detailed case-by-case studies (2,9).
Although routine chemotherapy is not a standard treatment for MPT
it can be considered for large tumors or when secondary structures
such as the chest wall are involved (2). So far neoadjuvant doxorubicin (DOX)
with dacarbazine versus no medical therapy has been studied in a
small observational biased trial where no positive outcome on
relapse-free survival has been observed (10). The other approach was described by
Hashimoto el al (11) where
pre-operative chemoembolization of a large MPT of the breast (MPTB)
led to successful avoidance of skin grafting after excision.
The development of antitumor drugs has depended
largely on cancer cell lines and animal models, and these have
played an important role in rapid screening and identification of
candidates for further evaluation. The NCI 60 cell line panel, for
example, is a popular screening tool (12). Cell lines offer several advantages
including ease of handling and convenient restoration from frozen
storage, and their ability to serve as an essentially unlimited
source of large quantities of relatively homogenous cells (13). However, they also have drawbacks that
limit their usefulness. For example, cell culture models lack the
tumor microenvironment which is known to critically impact
therapeutic response; the engraftment of tumor cells in xenograft
models relies on the host response in a non-native setting; and
transgenic mouse models do not always reproduce aspects of human
disease (14,15). In addition, in the case of a
heterogeneous disease such as breast cancer, single models do not
represent the various subtypes observed clinically. Furthermore,
cell lines are prone to undergo phenotypic and genetic drift, such
that ostensibly identical cell lines may differ substantially from
one laboratory to another (13).
Many of these problems can be circumvented through the use of
explant cultures, where pieces of fresh tumor are incubated ex
vivo on media-soaked sponges. Importantly, explants retain
tissue architecture, degrees of cellularity, and specific tumor
markers found in the originating tumor (16–18).
Such a system has tremendous general promise for breast cancer drug
discovery and biomarker development, with the potential to
accelerate personalized treatment options. However, a drawback of
explants is their limited timespan of utility of 3–4 days from
excision.
The generation of primary cell lines from
epithelial-derived tumors has historically been difficult because
the cells can only be cultured for a few passages before ceasing
proliferation and undergoing senescence (19). Although primary cells can be
immortalized through the introduction of oncogenes or telomerase
(20), such cells do not retain
lineage commitment, and they exhibit aberrant retinoblastoma and
p53 pathways and display abnormal growth or differentiation
potential. Recently it has been shown that human epithelial cells,
from a variety of sources both normal and tumor, can bypass
senescence and be cultured long-term if grown on irradiated
fibroblast feeder cells in the presence of the Rho kinase inhibitor
Y-27632 (21–23). These ‘conditionally reprogrammed’
cells (CRCs) represent a powerful and novel model for breast cancer
drug discovery, and serve as a more durable complement to explant
cultures.
In the present study, we evaluated the effectiveness
of seven drugs namely the Bcl-2/Bcl-xL inhibitor ABT-263,
salinomycin (SAL), DOX, paclitaxel (TAX), vincristine (VCR),
colchicine (COL), and cisplatin (CIS) in an ex vivo model of
PTB (24–26). These drugs were selected because they
represent a cross section of standard drugs used for breast cancer
treatment (DOX, TAX, CIS) (24) or
are related in mechanism (VCR and COL, which are microtubule
inhibitors like TAX) (25). In
addition, we tested ABT-263 since it is being advanced clinically
as a direct inducer of intrinsic apoptosis (26), and we also examined SAL since we have
shown previously that it is effective against ductal breast cancer
in an ex vivo model (27). We
also successfully generated primary PTB cells from the same tumor
specimen and have initiated drug testing in this system. The
results presented demonstrate the feasibility of using explants and
primary cells for drug discovery selectively targeting PTB
cells.
Materials and methods
Materials
TAX (cat. no. T1912), COL (cat. no. C-9754), DOX
(cat. no. PHR1789) and CIS (cat. no. 479306) were purchased from
Sigma-Aldrich (Darmstadt, Germany). VCR sulfate (cat. no.
SC-201434) was obtained from Santa Cruz Biotechnology (Dallas, TX,
USA) and ABT-263 (Navitoclax) (cat. no. A3007) from ApexBio
(Houston, TX, USA). SAL sodium salt was obtained from commercially
available veterinary premix SACOX® following acidic
extraction using the procedure described previously (28).
Preparation and culture of tissue
slices
Breast tumor tissue was provided by the Cooperative
Human Tissue Network (CHTN, http://www.chtn.org/), a National Cancer Institute
supported resource. Other investigators may have received samples
from these same tissue specimens. Fresh breast cancer tissue was
collected from a 33 year old African American female patient
diagnosed with 16.3 cm malignant phyllodes tumor of the breast.
Immediately after surgical resection, a portion of the specimen was
transported and stored in fresh RPMI 1640 medium on ice for 24 h
prior to use. The day after surgical removal, slices were prepared
from the specimen according to our previously established
methodology (27) based on the
studies of Van der Kuip et al (29). Briefly, 200 µm slices were cut in
sterile, cold PBS (cat. no. 21-030-CM, Corning, Manassas, VA, USA)
supplemented with 1% antibiotic/antimycotic solution (cat. no.
A5955, Sigma-Aldrich, Deisenhofen, Germany) using a microtome with
vibrating blade (Leica Biosystems VT1200, Nussloch, Germany).
Blades were steam sterilized before use. Several individual slices
from different parts of the specimen were immediately placed into
embedding cassettes (cat. no. 27158-2B and cat. no. 27154-1, Ted
Pella, Redding, CA, USA) and fixed in 10% neutral-buffered formalin
for 24 h and further stored in 70% ethanol prior to processing. The
remaining slices were distributed in separate wells of a 24 well
plate in 1 ml of Mammary Epithelial Cell Basal Medium (cat. no.
C-21215, Promo Cell, Heidelberg, Germany) supplemented with Mammary
Epithelial Cell Supplement Pack (cat. no. C-39110, Promo Cell,
Heidelberg, Germany), 100 µg/ml gentamicin (cat. no. G1397,
Sigma-Aldrich, Deisenhofen, Germany) and 0.05 µg/ml amphotericin B
(cat. no. A2942, Sigma-Aldrich, Deisenhofen, Germany). The plate
was incubated at 37°C in a constant atmosphere of 5% CO2
on a shaking platform at 150 rpm (Orbi-Shaker Jr, Benchmark
Scientific, Sayreville NJ, USA). After 24 h to allow tissue
equilibration, treatment with 0.2 % DMSO or ABT-263, SAL, DOX, TAX,
VCR, COL and CIS, at concentrations of 2, 8 and 16 µM was initiated
for 72 h. Concentrations were selected based on previous findings
of van der Kuip et al (29).
The medium was changed every 24 h. Tissue slices were then fixed
and stored as described above.
Immunohistochemical staining
Immunohistochemical staining of untreated, vehicle-
and drug-treated samples was performed by UAMS Experimental
Pathology Core. For histopathological examination, paraffin
embedded sections (4 µm) were stained with hematoxylin and eosin
(H&E) (cat. no. 7231, Richard-Allan Scientific, Thermo Fisher
Scientific, Waltham, MA, USA). Dako DAB+ (cat. no. K3468, Dako
Liquid, Carpenteria, CA, USA) was used for 3 min prior to
counterstaining with hematoxylin. Immunohistochemical staining for
Ki-67 (1:100, rabbit monoclonal anti-Ki67, cat. no. ab16667, Abcam,
Cambridge, MA, USA) was performed with biotinylated goat
anti-rabbit second antibody (1:400) (cat. no. BA-1000, Vector,
Burlingame, CA, USA) followed by detection using the Vectastain ABC
Elite detection system for 30 min (cat. no. PK-6100, Vector,
Burlingame, CA, USA). Epitope retrieval (cat. no. S1699, Target
Retrival Solution, Dako, Carpenteria, CA, USA) was achieved prior
to the staining in a decloaking chamber for 20 min (Biocare
medical). Dead or dying tumor cells were quantified manually based
on changes in cell and nuclear morphology. Quantification was
performed employing a Nikon Eclipse E600 microscope at 4×, 10× and
20×. Specifically, tumor cells which were markedly reduced in size
and/or showed nuclear fragmentation were scored. Effects of drugs
on normal ductal epithelial cells were similarly assessed by
evaluating cellular and nuclear morphology of individual cells as
well as the extent to which epithelial organization was disrupted.
A total of at least 50 cells were examined per condition each of
which was conducted in triplicate.
Generation of primary phyllodes
cells
To establish primary PTB cells, a procedure for
conditional reprogramming of cells (CRC) was followed (21). Briefly, the remaining tumor specimen
was cut into 1-mm thick slices which were dissociated by incubating
in a mixture of 0.25× Collagenase/Hyaluronidase and 0.25× Dispase
(cat. no. 7919, cat. no. 7913, Stem Cell Technologies, Vancouver,
Canada) diluted in F-medium 3:1 (v/v) F-12 Nutrient Mixture
(Ham)/Dulbecco's modified Eagle's medium (cat. no. 11765-054,
Gibco, Grand Island, NY, USA), 5% fetal bovine serum (cat. no.
FP-0500-A, Atlas Biologicals, Fort Collins, CO, USA), 24 µg/ml
adenine (cat. no. A2786-5G, Sigma-Aldrich, Deisenhofen, Germany),
8.4 ng/ml cholera toxin (cat. no. C8052-.5MG, Sigma-Aldrich,
Deisenhofen, Germany), 10 ng/ml epidermal growth factor (cat. no.
PHG0311, Life Technologies, Waltham, MA, USA), 1×
antibiotic/antimycotic solution (cat. no. A5955, Sigma-Aldrich,
Deisenhofen, Germany), 0.4 µg/ml hydrocortisone (cat. no. H4001,
Sigma-Aldrich, Deisenhofen, Germany), 5 µg/ml insulin (cat. no.
128-100, Cell Applications, Inc., San Diego, CA, USA) for 2 h.
Mouse fibroblast conditioned medium was prepared from Swiss 3T3-J2
mouse fibroblasts (cat. no. EF3003, Kerafast, Inc., Boston MA, USA)
cultured in DMEM supplemented with 10% bovine calf serum (iron
supplemented without gamma-irradiation or heat-inactivation from GE
Healthcare, Little Chalfont, England) following manufacturer
instructions. Dissociated cells were then seeded in 12-well tissue
culture plates in a mixture of F-medium and mouse fibroblast
culture supernatant at a ratio of 4:1 (v/v) supplemented with 5 µM
Rho kinase inhibitor (cat. no. ALX-270-333-M005, Enzo Life
Sciences, Farmingdale, NY, USA). Cells were maintained at 37°C in a
humidified incubator with 5% CO2. Colonies became
visible after 5 to 7 days and cells were passaged after two weeks
(approximately 105 cells) and expanded after reaching 80
to 90% confluence. An image of cells at passage 6 was recorded
using phase contrast microscopy using an EVOS FL Auto Cell Imaging
System (Thermo Fisher Scientific).
MCF-7, MDA-MB-231 and MCF 10A cell
lines
Human MCF-7 mammary gland adenocarcinoma cells
originally isolated from a 69 year old Caucasian woman with several
characteristics of differentiated mammary epithelium were cultured
in Eagle's Minimum Essential Medium (EMEM) (cat. no. 30-2003, ATCC,
Manassas, VA, USA) supplemented with 10% (v/v) heat-inactivated
fetal bovine serum (FBS) (cat. no. FP-0500-A, Atlas Biologicals,
Fort Collins, CO, USA), and 1% Penicillin/Streptomycin Solution
100× (cat. no. 30-002-Cl, Corning, Manassas, VA, USA). Human
MDA-MB-231 mammary gland adenocarcinoma cells isolated as one of a
series of breast tumor lines from pleural effusions of a 47 year
old Caucasian female were cultured in DMEM/Ham's Nutrient Mixture
F12 1:1 (cat. no. 51445C, Sigma-Aldrich, Deisenhofen, Germany)
supplemented with 5% (v/v) heat-inactivated fetal bovine serum
(FBS) (cat. no. FP-0500-A, Atlas Biologicals, Fort Collins, CO,
USA), 1% Penicillin/Streptomycin Solution 100× (cat. no. 30-002-Cl,
Corning, Manassas, VA, USA) and 1 mM L-Glutamine (cat. no.
25005-Cl, Corning, Manassas, VA, USA). Both cell lines were tested
via short tandem repeat profiling in July 2018 by Genetica DNA
Laboratories (Burlington, NC, USA) and verified as authentic,
giving a 100% match when compared to the known reference profile
(30). Human MCF 10A mammary
epithelial cells originally isolated from 36 year old Caucasian
women were purchased from ATCC, Manassas, VA, USA (cat. no.
CRL-10317) and cultured in Mammary Epithelial Cell Basal Medium
(cat. no. C-21215, Promo Cell, Heidelberg, Germany) supplemented
with Mammary Epithelial Cell Supplement Pack (cat. no. C-39110,
Promo Cell, Heidelberg, Germany), 100 µg/ml gentamicin (cat. no.
G1397, Sigma-Aldrich, Deisenhofen, Germany) and 0.05 µg/ml
amphotericin B (cat. no. A2942, Sigma-Aldrich, Deisenhofen,
Germany).
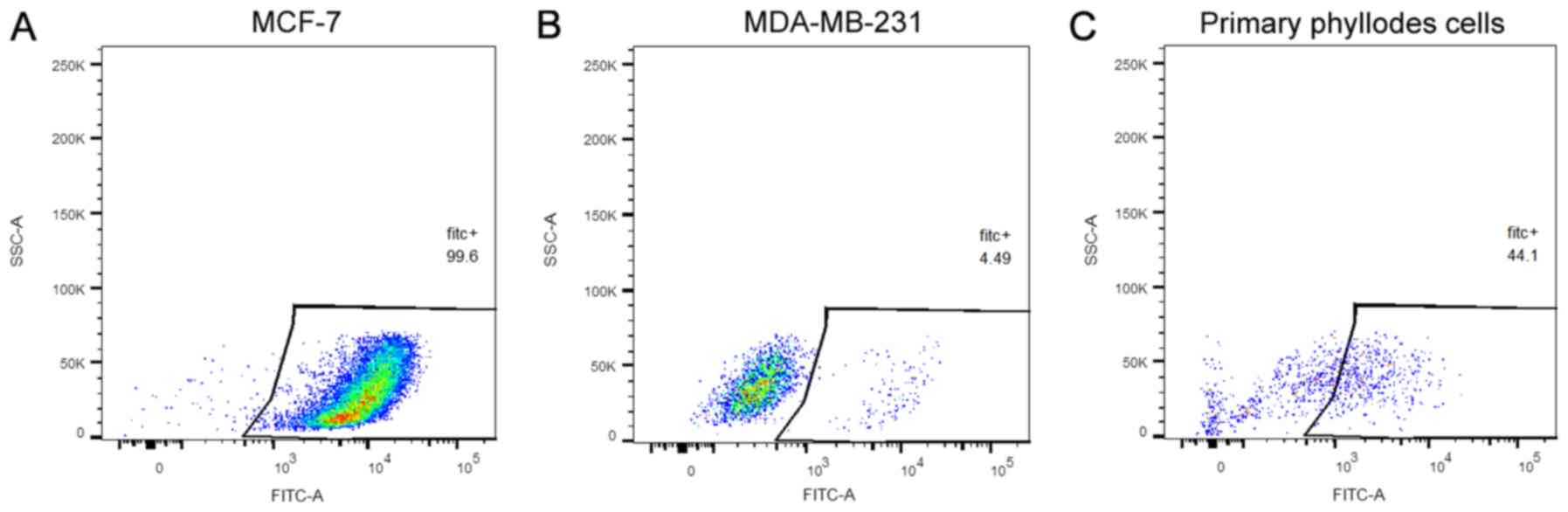
Flow cytometry analysis
EpCAM expression was assessed by binding of
FITC-conjugated anti-EpCAM monoclonal mouse anti-human antibody
(1:10 dilution) (cat. no. 324203, Biolegend, San Diego, CA, USA).
MCF-7, MDA-MB-231 and human primary phyllodes cells (about
5×104 cells) were harvested with GIBCO®
enzyme-free cell-dissociation buffer (cat. no. 13151-014, Life
Technologies, Grand Island, NY, USA), washed with flow-cytometry
buffer (PBS containing 1% BSA) and incubated with FITC-conjugated
anti-EpCAM antibody (1:10 dilution) in the same buffer for 30 min
followed by washing twice with flow-cytometry buffer. Cells were
fixed with 1% (final concentration) PFA. Acquisition and analysis
of data was performed by UAMS Flow Cytometry Core using a
LSRFORTESSA flow cytometer (BD Biosciences, San Jose, CA, USA) and
FlowJo® software (FlowJo LLC, Ashland, OR, USA).
Cell viability assay
A
3-(4,5-dimethylthiazol-2-yl)-2,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium
bromide (MTT)-based assay (31,32), was
used to evaluate the effect of drugs on the viability of primary
phyllodes cells and MCF 10A cells. Phyllodes cells
(0.35×104/well) in 100 µl of F-medium were seeded in
96-well plates (TPP, Trasadingen, Switzerland). After 24 h cells
were treated with DOX in the following concentrations: 1, 3, 10,
30, 100, 300, 1,000, 3,000 and 10,000 nM, as well as SAL and
ABT-263 at a single concentration of 10 µM for 96 h with control
cells receiving vehicle (0.1% DMSO) alone. The experiment was
performed in triplicate. MCF 10 A cells (1×104/well) in
100 µl of MEGM were seeded in 96-well plates (TPP, Trasadingen,
Switzerland) and after 24 h treated with DOX, SAL and ABT-263 at
the following concentrations: 1, 3, 10, 30, 100, 300, 1,000, 3,000
and 10,000 nM (of DOX and SAL) and 300, 1,000, 1,200, 1,400, 1,600,
1,800, 2,200, 3,000 nM of ABT-263 for 96 h with control cells
receiving vehicle (0.1% DMSO) alone. The experiment was performed
in quadruplicate. After treatment, 10 µl of MTT solution (5 mg/ml,
cat. no. M2128, Sigma-Aldrich, Deisenhofen, Germany) was added to
each well, and the plate was incubated at 37°C for 4 h in a
humidified 5% CO2 incubator. Medium was then aspirated
and 150 µl of DMSO was added to each well and the plate agitated on
a shaking platform (150 rpm) for 10 min. Absorbance was recorded at
540 nm using a BioTek Plate Reader. Inhibition of formation of
colored MTT formazan was taken as an index of cytotoxicity
activity. IC50 values were determined by non-linear
regression analysis using GraphPad Prism 6 for Windows (GraphPad
Software).
Statistical analysis
1-way ANOVA with Tukey's multiple comparisons test
was used to determine statistically significant differences between
means in experimental groups. Data are presented as a mean ± SD.
For ex vivo experiments three biological replicates were
performed for every drug concentration. Cell viability assay
employing primary phyllodes cells was performed in triplicate,
whereas MCF 10 A cells in quadruplicate. EpCAM staining was
performed in duplicate. Statistical analysis was performed using
GraphPad Prism 6 for Windows (GraphPad Software, Inc., San Diego,
CA, USA).
Results
Screening of cancer chemotherapeutics
in an ex vivo model of MPTB
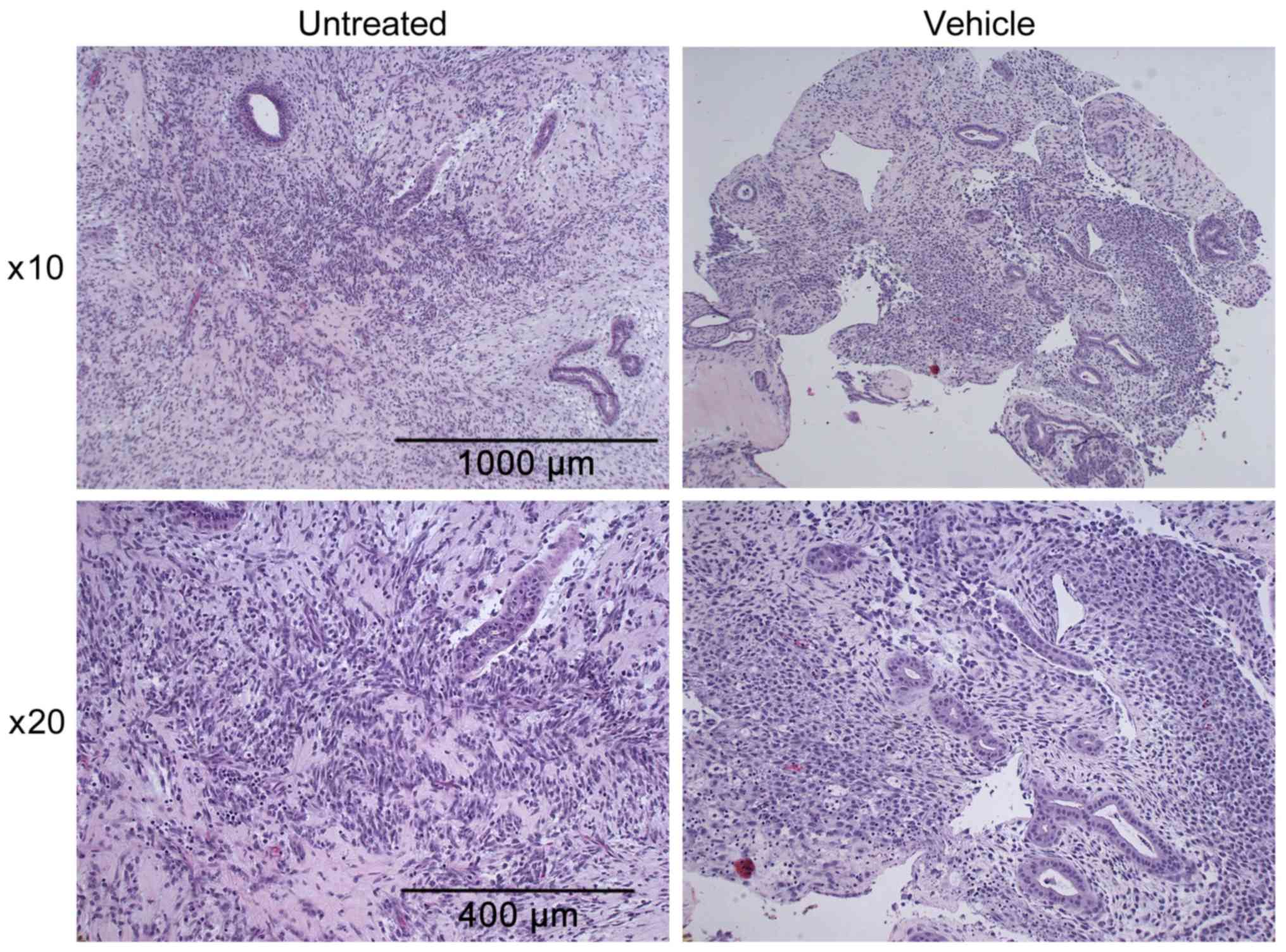
A single specimen of fresh, unfrozen MPTB was
obtained, sliced, incubated with select drugs, and subjected to
H&E staining, as described in Materials and methods. A
representative image of an untreated MPTB section fixed and stained
immediately upon receipt is shown in Fig. 1 (left panel). The presence of a
biphasic neoplasm made of neoplastic epithelial and mesenchymal
(spindle cell) elements is consistent with PT. This was confirmed
by the CHTN pathology report which subsequently became available.
The report indicated that the tumor showed biphasic fibroepithelial
growth with pushy lobulated margins, hypercellular stroma with
leaf-like architecture, stromal outgrowth, moderate to severe
nuclear atypia, high mitotic rate, and focal necrosis. Importantly,
the overall morphological features and tumor cell viability
remained unchanged in vehicle treated samples at 72 h (Fig. 1, right panel) compared to the
untreated original tumor sample (Fig.
1, left panel), indicating that incubation had no deleterious
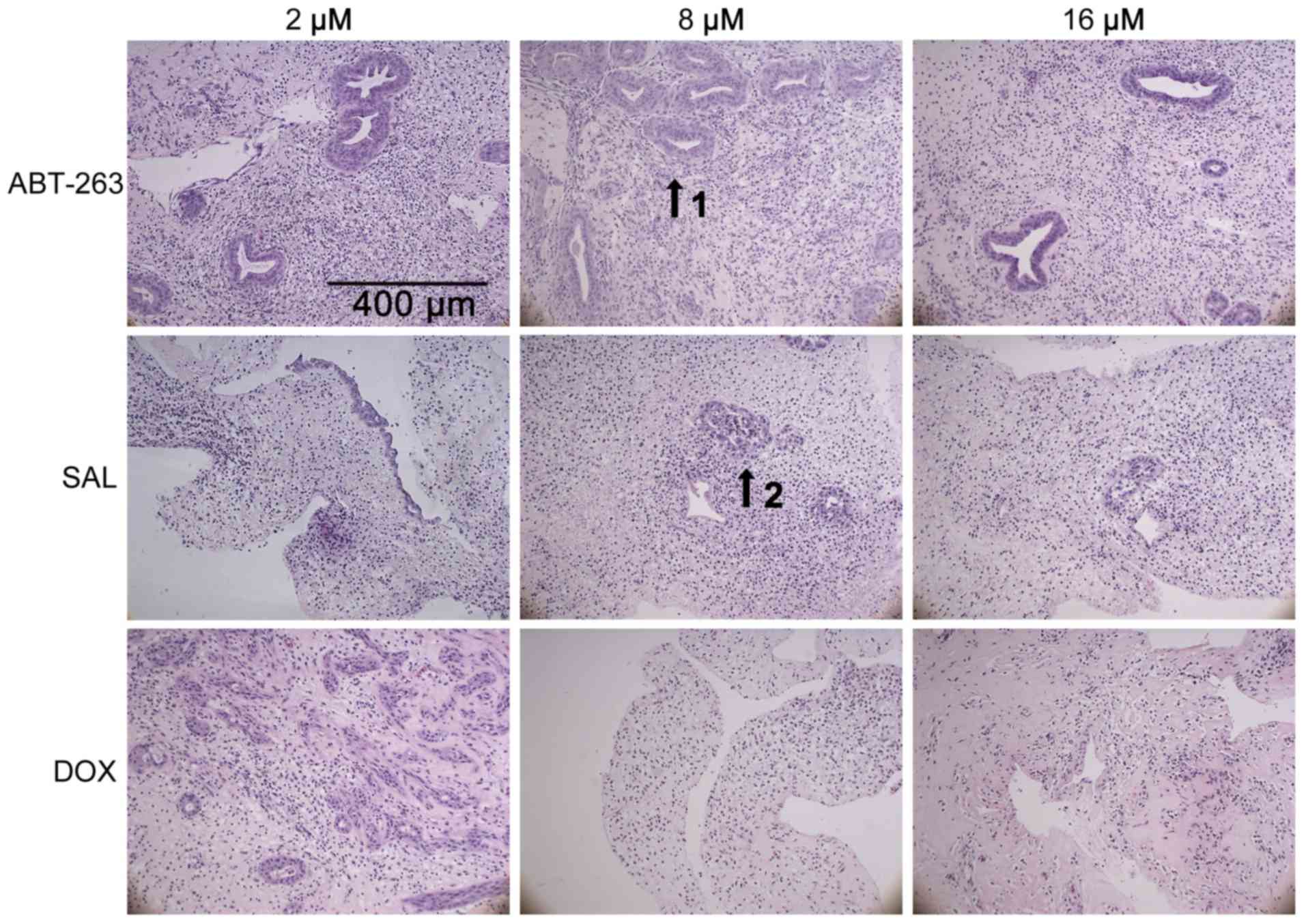
effects. Next, explant cultures were treated with drugs including
ABT-263, SAL, DOX, TAX, VCR, COL, and CIS. Representative images of
H&E stained slices at 20× magnification are presented in
Fig. 2 for the most active compounds
ABT-263, SAL, DOX, and in Fig. S1
for the other compounds. Healthy versus dead or drug-affected tumor
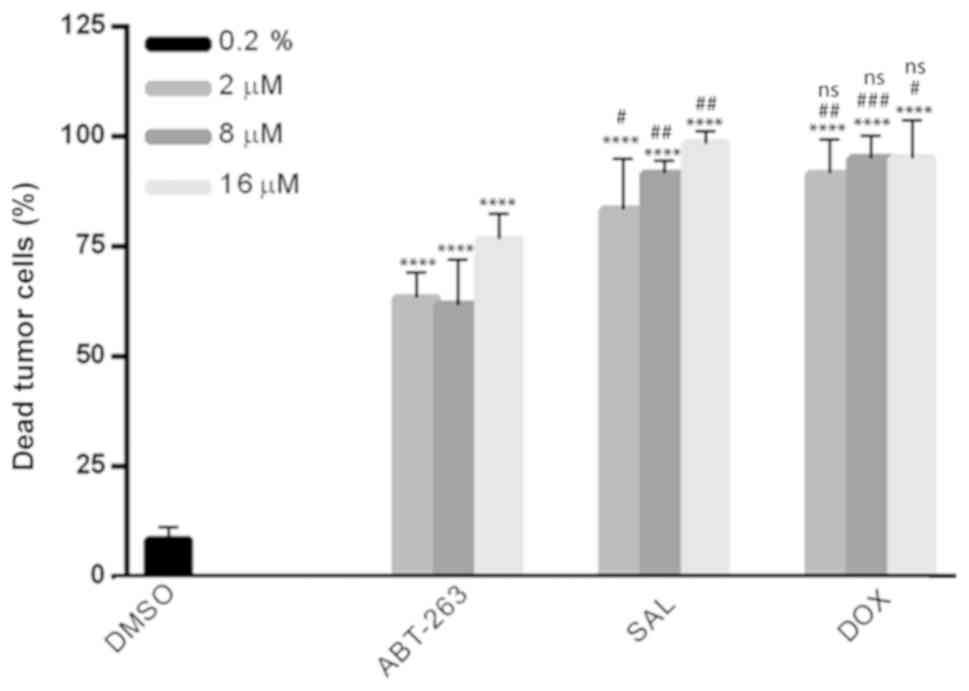
or normal epithelial cells were distinguished and quantified. As
evident from representative images in Fig. 2 and the corresponding quantitation in
Fig. 3, ABT-263, SAL and DOX
treatment caused marked tumor cell death in a dose-dependent manner
compared to vehicle treated slices (Fig.
3). Of additional interest, treatment with ABT-263 had very
little to no toxic effect on normal epithelial cells regardless of
the dose (Fig. 2). This is evident
from examination of the images in Fig.
2, where ducts retained their normal architecture and
cellularity even with the highest tested ABT-263 concentration
(indicated by arrow 1), and from quantitative assessment of
toxicity (Table I). In contrast, the
anti-tumor activities of SAL and DOX were accompanied by
significant toxic effects on normal epithelial cells, particularly
after DOX treatment (arrow 2 in Fig.
2; Table I).
 | Table I.Toxic effect of 2, 8 and 16 µM of
ABT-263, SAL and DOX on normal epithelial cells in the ex
vivo model (n=3). |
Table I.
Toxic effect of 2, 8 and 16 µM of
ABT-263, SAL and DOX on normal epithelial cells in the ex
vivo model (n=3).
|
| Concentration
[µM] |
|---|
|
|
|
|---|
|
| 2 | 8 | 16 |
|---|
|
|
|
|
|
|---|
|
| Sample number |
|---|
| Drug | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 |
|---|
| ABT-263 | 0 | 0 | 0 | 0 | 0 | † | 0 | 0 | 1 |
| SAL | 2 | 2 | 3 | 3 | 2 | † | 3 | 3 | 3 |
| DOX | 3 | 3 | 1 | 3 | 3 | 3 | 3 | 3 | 3 |
Treatment of PTB explant cultures with TAX, VCR,
COL, and CIS was also performed under similar conditions (Fig. S1A). However, none of these drugs
produced significant effects on the tumor cells thus quantification
and statistical analysis of dead tumor cells was not performed.
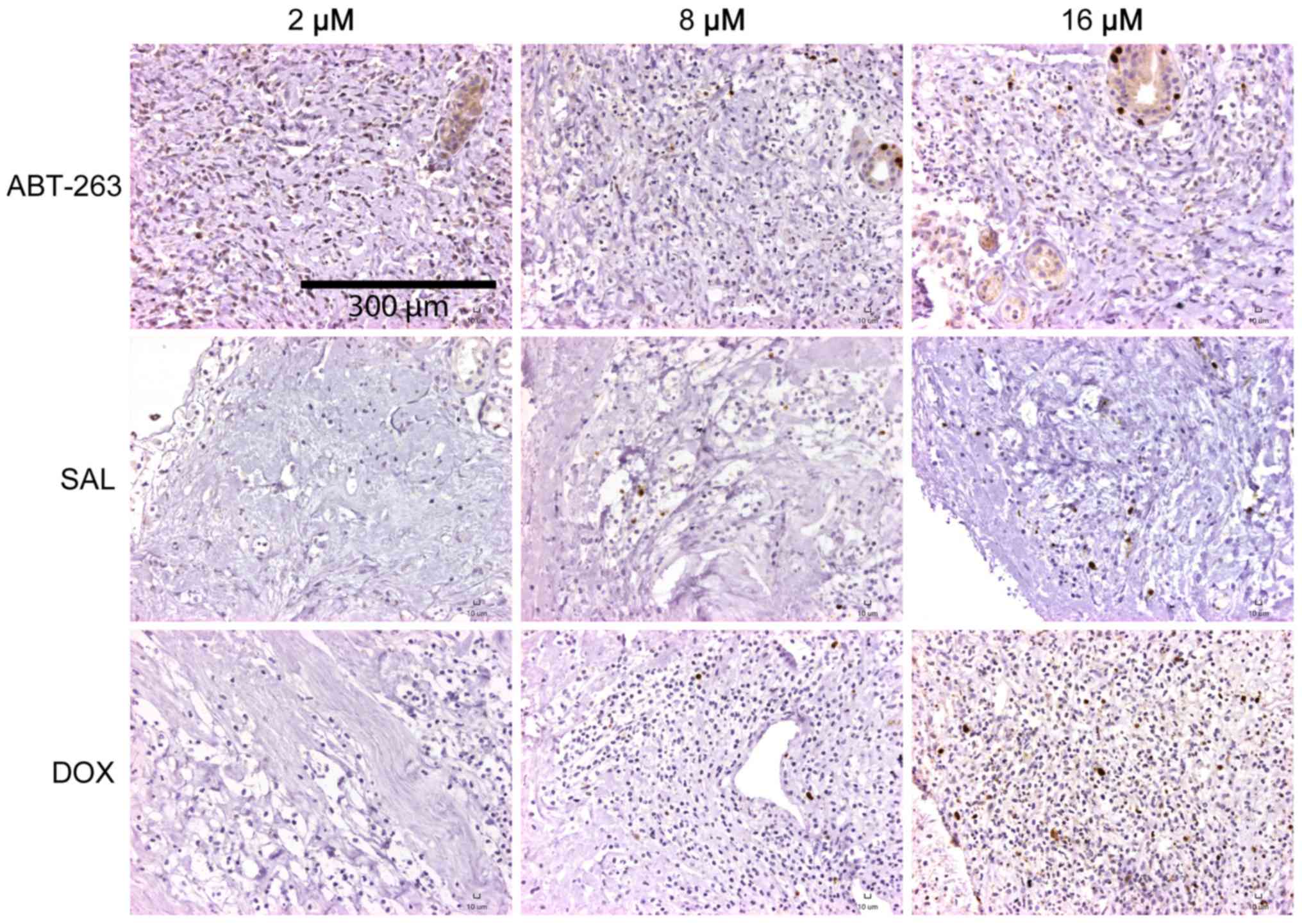
Additionally, sections from paraffin embedded tissue
were analyzed by immunohistochemical staining for Ki-67, which is
an established marker of cell proliferation (33). Representative images at 20×
magnification are presented in Fig.
4 and Fig. S1B. In untreated
tumor sections, the Ki-67 proliferation index was very low
(<5%), in a good agreement with a previous study (34), whereas strong Ki-67 immunolabeling
was observed in some of the ductal epithelial cells (Fig. S1B). Ductal epithelial Ki-67
immunolabeling was largely maintained after ABT-263 treatment but
was not observed after treatment with SAL or DOX (Fig. 4), consistent with the differential
effects of the drugs on normal cells.
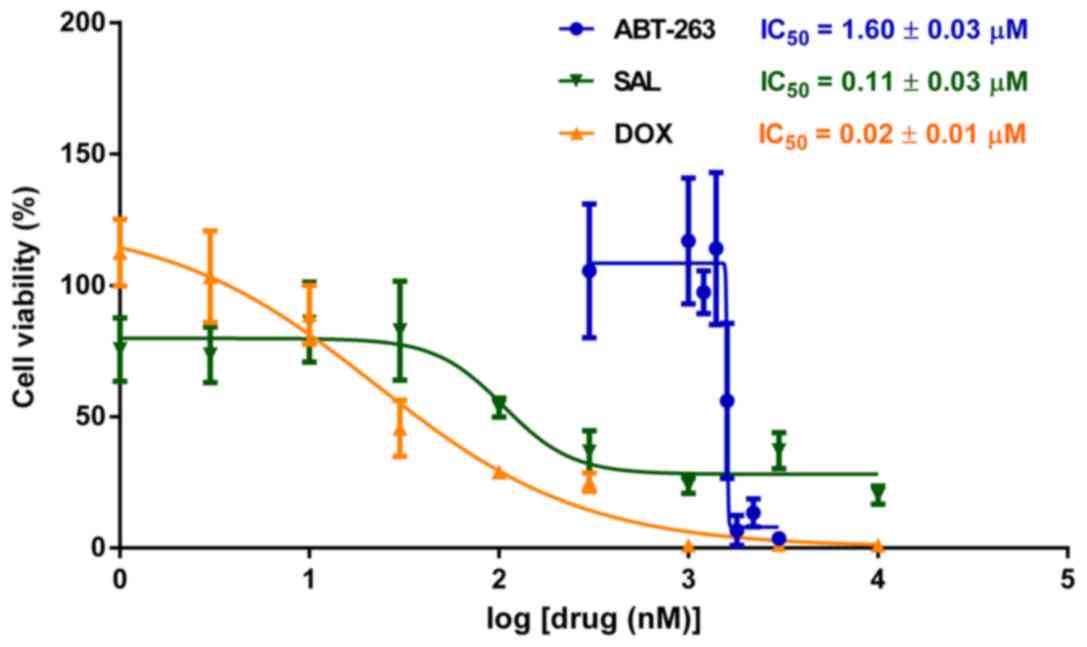
In order to further assess the selectivity of
ABT-263 towards tumor versus normal cells compared to SAL and DOX,
both of which appeared less discriminate in the ex vivo
model, we performed MTT viability assay on the MCF 10A cell line.
These are non-tumorigenic mammary epithelial cells commonly used as
a surrogate for normal mammary cells. As shown in Fig. 5, IC50 values were ABT-263,
1.60±0.03 µM; SAL, 0.11±0.03 µM; and DOX, 0.02±0.01 µM. Thus MCF
10A cells are much more sensitive to SAL (20×) and DOX (120×)
compared to ABT-263, in good agreement with observations made in
the ex vivo model (Fig. 2 and
Table I).
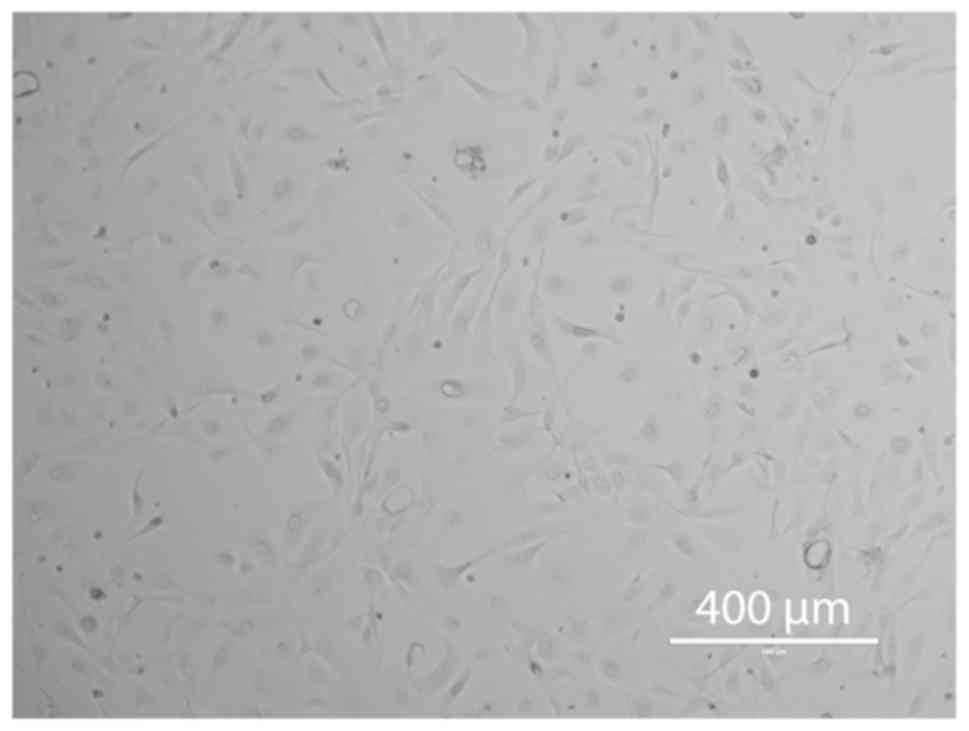
Generation of primary phyllodes
cells
To further investigate the response of PTB cells to
anticancer drugs we sought to generate primary cells from the MPTB
we obtained. This was facilitated by recent advances in the
preparation of primary cells through Rho kinase inhibition and the
use of fibroblast feeder cells or conditioned medium derived
therefrom (21,22). An image from a phase contrast
microscope of the cells derived from the MPTB tissue using this
procedure is shown in Fig. 6. It is
evident that the population of cells was mixed, with the majority
showing an elongated, triangular morphology. In addition, cells
with a more spherical morphology were present, as were infrequent
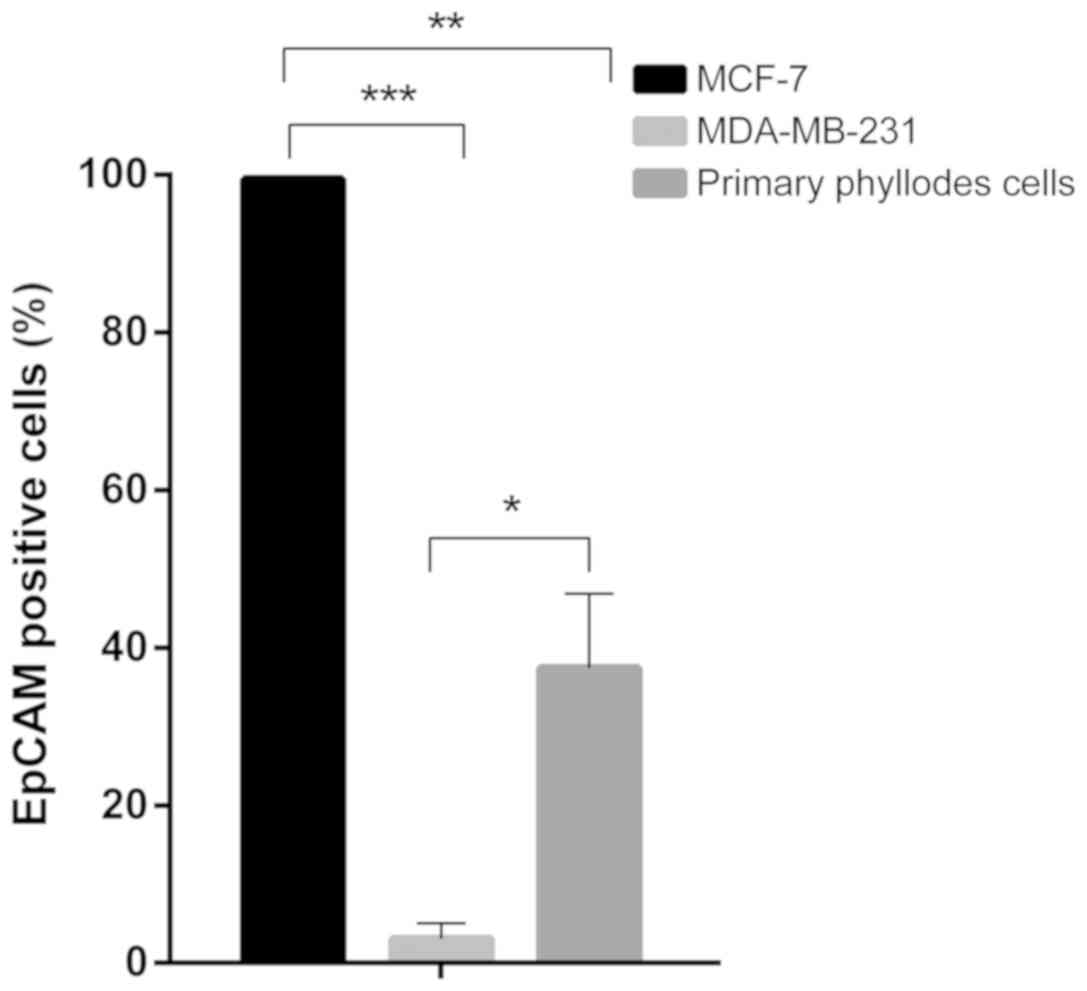
cells with large intracellular vacuoles or vesicles. In order to
confirm the presence of PT cells in this population, the expression
of EpCAM (CD326), a transmembrane glycoprotein present on the
surface of epithelial cells, was evaluated (35). MCF-7 and MDA-MB-231 cell lines,
characterized by high and low EpCAM expression, respectively
(36), were used as positive and
negative controls. As shown in Fig.
7, the two breast cancer cell lines expressed EpCAM consistent
with expectations, and were used to set a gate denoting high versus
low expression. When the phyllodes primary cells were examined, a
range of EpCAM expression was observed, with about 30% of the
population in the range defined as high, indicating the presence of
epithelial derived cells (Fig. 8).
Once primary cells were established, they proliferated with a
doubling time of 3–5 days initially, and viable cells up to passage
6 were obtained before they showed signs of slowed growth. Thus the
overall number of cells obtained was limited and precluded an
in-depth characterization of their properties and response to the
drugs. Nonetheless, viability assays after select drug treatment
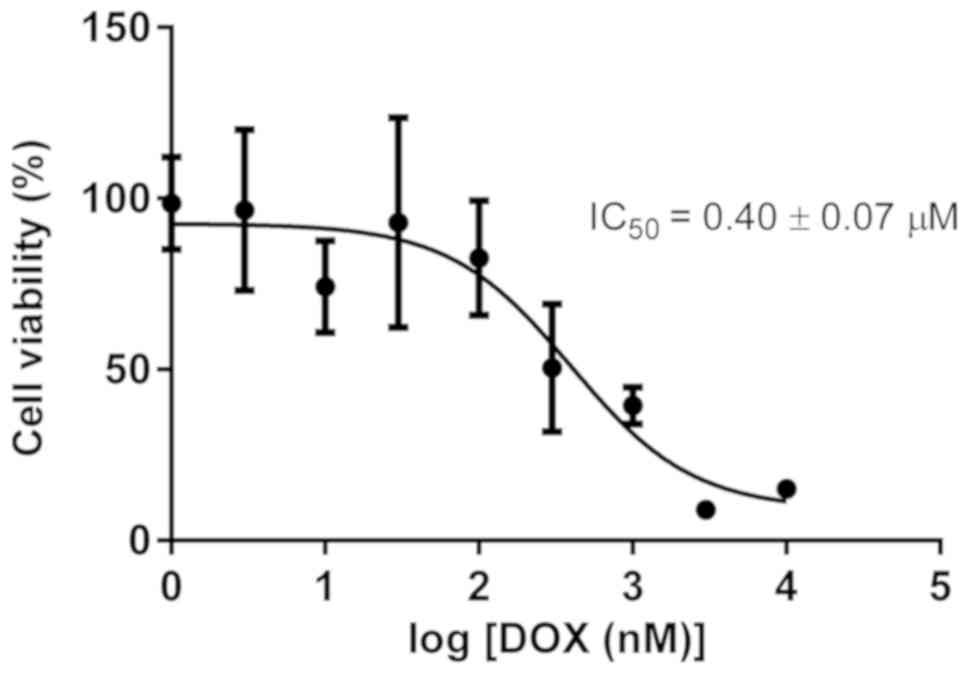
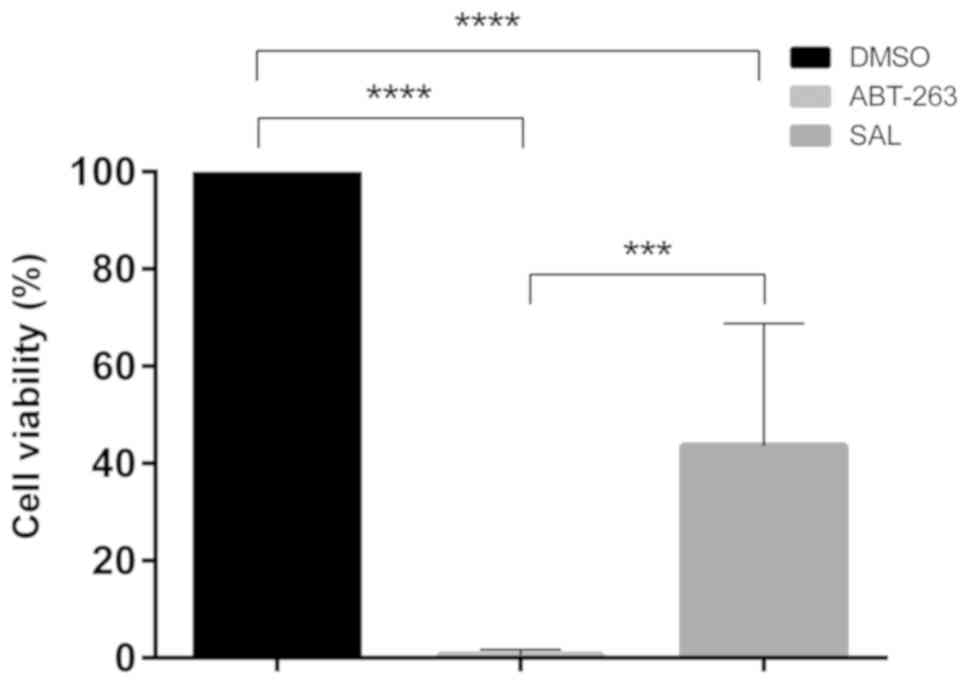
were conducted using the colorimetric MTT assay (Figs. 9 and 10) (31,32).
This method is based on the conversion of MTT to blue MTT-formazan
crystals by mitochondrial enzymes present in viable cells. Data for
DOX using primary phyllodes cells at passage 6 are shown in
Fig. 9. A concentration-dependent
decrease in viability was observed with an IC50 value of
0.40±0.07 µM. Because of limited numbers of cells, other drugs
could not be tested with a full range of concentrations, but
preliminary experiments indicated that the primary PTB cells were
also sensitive to ABT-263 and to SAL used at 10 µM, which was the
highest concentration employed in MTT assay (Fig. 10).
Discussion
Surgical wide excision is the primary treatment for
malignant PTBs but it frequently recurs and rarely responds to
radiation or conventional chemotherapy (1–8).
Although chemotherapy is not a standard PTB treatment, its
application in the treatment of malignant cases would be greatly
facilitated by the availability of appropriate experimental models
to identify effective compounds. Primary cells derived from
malignant phyllodes breast cancer have been described (37), but they are no longer available (R.K.
Oldham, personal communication). In addition, although a cell line
termed RW962 derived from a human phyllodes breast tumor has been
reported, it was propagated as a xenograft in a mouse (38).
The present study describes two complementary
laboratory models of human PTB amenable to novel drug discovery.
The first involves thin tissue sections of freshly excised tumor as
an experimental model to test agents active against this form of
cancer. The preservation of tissue architecture and the
co-existence in the same sample of both cancer and normal cells
creates an extremely powerful tool for therapeutic drug screening
and identification of effective as well as selective agents under
uniform conditions. The activity of seven compounds was initially
tested in this system including ABT-263, SAL, DOX, TAX, VCR, COL,
and CIS. Three of the agents studied, namely ABT-263, SAL and DOX,
were effective in killing PTB cells in the explant cultures
(Figs. 2 and 3). However, the other compounds were not
effective and did not result in significant induction of tumor cell
death. Of possible relevance, the agents inactive in this system
are cell cycle-dependent drugs. Thus TAX, VCR, and COL are all
microtubule targeting agents, and the mechanism of action of CIS
depends on interfering with DNA replication (39,40). PTB
cells are relatively slow growing and have a low proliferation
index based on Ki-67 immunolabeling (Figs. 4 and S1B) (34),
and this may render cell cycle-active drugs ineffective. Of the
three drugs tested in the explant system that were effective, only
ABT-263 was selective for the tumor cells, having only a very mild
effect on normal epithelial cells even at the highest concentration
of 16 µM (Table I). These results
are intriguing since they suggest that PTB cells may be primed for
apoptosis through the intrinsic pathway (41), and indicate that further
investigation of Bcl-2 inhibitors as a chemotherapeutic approach
for PTB is warranted. The higher selectivity of ABT-263 for tumor
versus normal cells relative to DOX and SAL was confirmed by
studies with the non-tumorigenic MCF 10A cell line (Fig. 5).
It is of interest to compare our findings with case
reports in the literature describing treatment of PTB in the
clinic. Of the drugs we tested, three, namely DOX, SAL and ABT-263,
were effective in killing PTB cells. Of these, only DOX has been
used in the clinical setting for PTB. DOX was found to improve
median survival of patients with metastatic PTB, especially when
used in combination with cisplatin, cyclophosphamide, or ifosfamide
(42,43), and in one case complete remission was
achieved with the combination of doxorubicin and cisplatin
(44). Effective therapy of
metastatic PTB with the combination of cisplatin and etoposide was
also reported in three patients (45), measured via a reduction in tumor
burden, but all three eventually died, and a larger study is needed
to define response rate and median survival. These studies
highlight the need for more systematic investigation of
chemotherapy for PTB, and further emphasize the potential impact on
drug discovery of the ex vivo and CRC models we described
here. In particular, there are no reports to our knowledge testing
Bcl-2 inhibition for PTB, and our finding that ABT-263 is highly
effective without affecting neighboring normal cells represents an
important advance. The explant system we employed represents a
powerful screening tool. Importantly, several genome studies have
been conducted that have provided insight into PTB pathogenesis and
defined potential targets and opportunities for personalized
therapeutic intervention (46–47). For
example, the combined expression of CD34 and Bcl-2 have been shown
to occur in 35–57% of malignant PTBs analyzed (48). Data from these types of studies can
suggest molecular targets for inhibition which can be readily
tested in the explant system we have described here to expedite
identification of drugs and drug combinations that have particular
utility for treating PTBs (49).
While explants retain tissue architecture, degrees
of cellularity, and specific tumor markers, the main drawback is
the lack of durability, with a time-span of utility of just a few
days. On the other hand, established cell lines are highly adapted
to culture and there is uncertainty over how well they reflect the
original tumor cells (13). Primary
tumor cells represent a useful intermediate model system that
offers durability without the problem of adaptation. As indicated
above, while there are numerous cell lines derived from
conventional forms of breast cancer, PTB cell lines or primary cell
cultures are not available. In order to obtain primary PTB cells
from the original tumor we followed established protocols for the
generation of CRCs (21–23). Microscopic examination, EpCAM
expression and the proliferative nature of the population of cells
obtained were consistent with the presence of PT cells. While the
number of cells generated was insufficient to fully screen all of
the compounds used in the explant system, the cells were sensitive
to the three agents effective in the explant culture, namely
ABT-263, DOX and SAL, strengthening the conclusion that PTB cells
were present. According to published reports, CRCs typically can be
passaged for extended periods (21–23), yet
the primary PTB cells we generated began to show signs of slowed
growth after passage 6. Therefore further optimization of the
conditions will be required to generate more robust cultures.
Nonetheless, the results presented here demonstrate the feasibility
of PTB drug discovery using explant and primary cultures.
Supplementary Material
Supporting Data
Acknowledgements
The authors would like to thank Mrs. Jennifer James
(UAMS Experimental Pathology Core) for processing samples for
immunochemistry, Ms. Andrea Harris (UAMS Flow Cytometry Core) for
performing flow cytometry experiments and assisting with
interpretation and Dr Mustafa Sarimollaoglu (Department of
Otolaryngology, UAMS), for assistance with the figures.
Funding
The present study was supported by funds from the
Arkansas Breast Cancer Research Program.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request
Authors' contributions
AU performed the ex vivo study and in
vitro MTT assays, cell cultures, data preparation and analysis
and wrote the draft version of manuscript, FJ acquired the primary
phyllodes cells and performed the EpCAM staining experiment, YY
analysed and quantified the H&E stained slides and prepared the
representative images. SPO analyzed the Ki-67 stained slides and
prepared the representative images; AH performed the salinomycin
acquisition and purification. MD performed the cell culture and
performed the data analysis. TKE participated in securing funding
for the project, experimental design, data interpretation and read
and approved all versions of the manuscript. BMK supervised the
acquisition of primary phyllodes cells and the EpCAM staining
experiment, designed the experiments, interpretated results,
supported manuscript writing and read and approved all versions of
the manuscript. TCC supervised the project supervision, performed
the data analysis, wrote the final version of the manuscript and
acquired funding for the project. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
The protocol was determined by UAMS IRB to be ‘not
human subjects research’ and therefore does not require IRB
approval.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Parker SJ and Harries SA: Phyllodes
tumors. Postgrad Med J. 77:428–435. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Strode M, Khoury T, Mangieri C and Takabe
K: Update on the diagnosis and management of malignant phyllodes
tumors of the breast. Breast. 33:91–96. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Roberts N and Runk DM: Aggressive
malignant phyllodes tumor. Int J Surg Case Rep. 8:161–165. 2015.
View Article : Google Scholar
|
|
4
|
Mishra SP, Tiwary SK, Mishra M and Khanna
AK: Phyllodes tumor of breast: A review article. ISRN Surg.
2013:3614692013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Norat F, Dreant N, Riah Y and Lebreton E:
Ann ital chir extraordinary case of malignant phylloid tumor of the
breast: Surgical reconstruction treatment (Italian). 80:475–478.
2009.PubMed/NCBI
|
|
6
|
Chaney AW, Pollack A, McNeese MD, Zagars
GK, Pisters PWT, Pollock RE and Hunt KK: Primary treatment of
cystosarcoma phyllodes of the breast. Cancer. 89:1502–1511. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Matar N, Soumani A, Noun M, Chraibi T,
Himmi A, el Mansouri A, Aderdour M and Bekkay M: Phyllodes tumors
of the breast. Forty one cases. J Gynecol Obstet Biol Reprod
(Paris). 26:32–36. 1997.PubMed/NCBI
|
|
8
|
Belkacémi Y, Bousquet G, Marsiglia H,
Ray-Coquard I, Magné N, Malard Y, Lacroix M, Gutierrez C, Senkus E,
Christie D, et al: Phyllodes tumor of the breast. Int J Radiat
Oncol Biol Phys. 70:492–500. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Guillot E, Couturaud B, Reyal F, Curnier
A, Ravinet J, Laé M, Bollet M, Pierga JY, Salmon R and Fitoussi A:
Breast cancer study group of the institut curie: Management of
phyllodes breast tumors. Breast J. 17:129–137. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Morales-Vasquez F, Gonzalez-Angulo AM,
Broglio K, Lopez-Basave HN, Gallardo D, Hortobagyi GN and De La
Garza JG: Adjuvant chemotherapy with doxorubicin and dacarbazine
has no effect in recurrence-free survival of malignant phyllodes
tumors of the breast. Breast J. 13:551–556. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hashimoto K, Mimura H, Arai Y, Doi M,
Kojima Y, Tsugawa K and Nakajima Y: Successful preoperative
chemoembolization in the treatment of a giant malignant phyllodes
tumor. Cardiovasc Intervent Radiol. 39:1070–1075. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Shoemaker RH: The NCI60 human tumour cell
line anticancer drug screen. Nat Rev Cancer. 6:813–823. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Burdall SE, Hanby AM, Lansdown MR and
Speirs V: Breast cancer cell lines: Friend or foe. Breast Cancer
Res. 5:89–95. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Witkiewicz AK, Rivadeneira DB, Ertel A,
Kline J, Hyslop T, Schwartz GF, Fortina P and Knudsen ES:
Association of RB/p16-pathway perturbations with DCIS recurrence:
Dependence on tumor versus tissue microenvironment. Am J Pathol.
179:1171–1178. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Vargo-Gogola T and Rosen JM: Modelling
breast cancer: One size does not fit all. Nat Rev Cancer.
7:659–672. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
16
|
Dean JL, McClendon AK, Hickey TE, Butler
LM, Tilley WD, Witkiewicz AK and Knudsen ES: Therapeutic response
to CDK4/6 inhibition in breast cancer defined by ex vivo analyses
of human tumors. Cell Cycle. 11:2756–2761. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Majumder B, Baraneedharan U, Thiyagarajan
S, Radhakrishnan P, Narasimhan H, Dhandapani M, Brijwani N, Pinto
DD, Prasath A, Shanthappa BU, et al: Predicting clinical response
to anticancer drugs using an ex vivo platform that captures tumour
heterogeneity. Nature Commun. 6:61692015. View Article : Google Scholar
|
|
18
|
Nagourney RA: Ex vivo programmed cell
death and the prediction of response to chemotherapy. Curr Treat
Options Oncol. 7:103–110. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kuilman T, Michaloglou C, Mooi WJ and
Peeper DS: The essence of senescence. Genes Dev. 24:2463–2479.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Roig AI, Eskiocak U, Hight SK, Kim SB,
Delgado O, Souza RF, Spechler SJ, Wright WE and Shay JW:
Immortalized epithelial cells derived from human colon biopsies
express stem cell markers and differentiate in vitro.
Gastroenterology. 138:1012–1021. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Liu X, Ory V, Chapman S, Yuan H, Albanese
C, Kallakury B, Timofeeva OA, Nealon C, Dakic A, Simic V, et al:
ROCK inhibitor and feeder cells induce the conditional
reprogramming of epithelial cells. Am J Pathol. 180:599–607. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Saenz FR, Ory V, AlOtaiby M, Rosenfield S,
Furlong M, Cavalli LR, Johnson MD, Liu X, Schlegel R, Wellstein A
and Riegel AT: Conditionally reprogrammed normal and transformed
mouse mammary epithelial cells display a progenitor-cell-like
phenotype. PLoS One. 9:976662014. View Article : Google Scholar
|
|
23
|
Brown DD, Dabbs DJ, Lee AV, McGuire KP,
Ahrendt GM, Bhargava R, Davidson NE, Brufsky AM, Johnson RR,
Oesterreich S and McAuliffe PF: Developing in vitro models of human
ductal carcinoma in situ from primary tissue explants. Breast
Cancer Res Treat. 153:311–321. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Moo TA, Sanford R, Dang C and Morrow M:
Overview of breast cancer therapy. PET Clin. 13:339–354. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Steinmetz MO and Prota AE:
Microtubule-targeting agents: Strategies to hijack the
cytoskeleton. Trends Cell Biol. 28:776–792. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Billard C: BH3 mimetics: Status of the
field and new developments. Mol Cancer Ther. 12:1691–700. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Antoszczak M, Urbaniak A, Delgado M, Maj
E, Borgström B, Wietrzyk J, Huczyński A, Yuan Y, Chambers TC and
Strand D: Biological activity of doubly modified salinomycin
analogs - Evaluation in vitro and ex vivo. Eur J Med Chem.
156:510–523. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Antoszczak M, Popiel K, Stefańska J,
Wietrzyk J, Maj E, Janczak J, Michalska G, Brzezinski B and
Huczynski A: Synthesis, cytotoxicity and antibacterial activity of
new esters of polyether antibiotic-alinomycin. Eur J Med Chem.
76:435–444. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Van der Kuip H, Mürdter TE, Sonnenberg M,
McClellan M, Gutzeit S, Gerteis A, Simon W, Fritz P and Aulitzky
WE: Short term culture of breast cancer tissues to study the
activity of the anticancer drug taxol in an intact tumor
environment. BMC Cancer. 6:862006. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Dirks WG, MacLeod RA, Nakamura Y, Kohara
A, Reid Y, Milch H, Drexler HG and Mizusawa H: Cell line
cross-contamination initiative: An interactive reference database
of STR profiles covering common cancer cell lines. Int J Cancer.
126:303–304. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Alley MC, Scudiere DA, Monks A, Czerwinski
M, Shoemaker RH and Boyd MR: Validation of an automated
microculture tetrazolium assay (MTA) to assess growth and drug
sensitivity of human tumor cell lines. Proc Am Assoc Cancer Res.
27:389–391. 1986.
|
|
32
|
Alley MC, Scudiere DA, Monks A, Hursey ML,
Czerwinski MJ, Fine DL, Abbott BJ, Mayo JG, Shoemaker RH and Boyd
MR: Feasibility of drug screening with panels of human tumor cell
lines using a microculture tetrazolium assay. Cancer Res.
48:589–601. 1988.PubMed/NCBI
|
|
33
|
Yerushalmi R, Woods R, Ravdin PM, Hayes MM
and Gelmon KA: Ki67 in breast cancer: Prognostic and predictive
potential. Lancet Oncol. 11:174–183. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Lin CK, Tsai WC, Lin YC and Yu JC:
Biomarkers distinguishing mammary fibroepithelial neoplasms: A
tissue microarray study. Appl Immunohistochem Mol Morphol.
22:433–441. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Went P, Dirnhofer S, Schöpf D, Moch H and
Spizzo G: Expression and prognostic significance of EpCAM. J Cancer
Mol. 3:169–174. 2008.
|
|
36
|
Martowicz A, Spizzo G, Gastl G and
Untergasser G: Phenotype-dependent effects of EpCAM expression on
growth and invasion of human breast cancer cell lines. BMC Cancer.
12:5012012. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Lewko WM, Vaghmar R, Maleckar JR, Husseini
S, Montgomery CA, Thurman GB and Oldham RK: Cultured breast
cystosarcoma phylloides cells and applications to patient therapy.
Breast Cancer Res Treat. 17:131–138. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Tibbetts LM, Poisson MH, Tibbetts LL and
Cummings FJ: A human breast stromal sarcoma cell line with features
of malignant cystosarcoma phyllodes. Cancer. 62:2176–2182. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Jordan MA and Wilson L: Microtubules as a
target for anticancer drugs. Nat Rev Cancer. 4:253–265. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Wheate NJ, Walker S, Craig GE and Oun R:
The status of platinum anticancer drugs in the clinic and in
clinical trials. Dalton Trans. 39:8113–8127. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Tait SW and Green DR: Mitochondrial
regulation of cell death. Cold Spring Harb Perspect Bio. 5(pii):
a0087062013. View Article : Google Scholar
|
|
42
|
Mituś JW, Blecharz P, Walasek T, Reinfuss
M, Jakubowicz J and Kulpa J: Treatment of patients with distant
metastases from phyllodes tumor of the breast. World J Surg.
40:323–328. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Liu M, Yang S, Liu B, Guo L, Bao X, Liu B
and Dong L: Giant malignant phyllodes tumor of the breast: A rare
case report and literature review. Oncol Lett. 12:121–124. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Allen R, Nixon D, York M and Coleman J:
Successful chemotherapy for cystosarcoma phyllodes in a young
woman. Arch Intern Med. 145:1127–1128. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Burton GV, Hart LL, Leight GS, Iglehart
JD, McCarty KS Jr and Cox EB: Cystosarcoma phyllodes effective
therapy with cisplatin and etoposide chemotherapy. Cancer.
63:2088–2092. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Lim SZ, Ng CCY, Rajasegaran V, Guan P,
Selvarajan S, Thike AA, Nasir NDBM, Koh VCY, Tan BKT, Ong KW, et
al: Genomic profile of breast sarcomas: A comparison with malignant
phyllodes tumours. Breast Cancer Res Treat. 174:365–373. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Nozad S, Sheehan CE, Gay LM, Elvin JA,
Vergilio JA, Suh J, Ramkissoon S, Schrock AB, Hirshfield KM, Ali N,
et al: Comprehensive genomic profiling of malignant phyllodes
tumorsof the breast. Breast Cancer Res Treat. 162:597–602. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Moore T and Lee AH: Expression of CD34 and
bcl-2 in phyllodes tumours, fibroadenomas and spindle cell lesions
of the breast. Histopathology. 38:62–67. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Jardim DL, Conley A and Subbiah V:
Comprehensive characterization of malignant phyllodes tumor by
whole genomic and proteomic analysis: Biological implications for
targeted therapy opportunities. Orphanet J Rare Dis. 8:1122013.
View Article : Google Scholar : PubMed/NCBI
|