Introduction
Cervical lesions include inflammatory lesions of the
cervix, cervical intraepithelial neoplasia (CIN) and cervical
cancer. According to the 2014 World Health Organization
Classification of Tumors, Pathology and Genetics of Tumors of the
Breast and Female Genital Organs, which is commonly used
internationally at present (1,2),
cervical lesions are divided into classes: Low-grade squamous
intraepithelial lesions (LSIL), including CINI; and high-grade
squamous intraepithelial lesions (HSIL), including CIN II, CIN III
and invasive cervical cancer. A number of studies have confirmed
that cervical lesions are infectious diseases (3,4).
Persistent infection with human papilloma virus (HPV) is the
primary risk factor for these diseases. The cervix is exposed in
the vagina and is therefore affected by the vaginal
microenvironment, which is composed of the vaginal local immunity,
the vaginal microbial flora and the endocrine regulation of the
body. The vaginal local immunity has a similar composition to
systemic immunity, which primarily includes humoral and cellular
immunities (5). When cervical HPV
infection occurs, the anti-infection mechanism of the immune system
is able to resist the invasion of pathogens (6). However, if systemic or local immune
damage occurs, HPV causes damage to epithelial cells and the immune
escape mechanism evolves. This increases the possibility of
malignancy and triggers a cycle of tumor and immune damage
(6). Therefore, the present study
analyzed the expression levels of secretory immunoglobulin A
(sIgA), IgG, interleukin (IL)-2 and IL-10, as well as the
IL-2/IL-10 ratio, in order to evaluate whether these may reflect
the immune status of patients with vaginal HPV infection.
Furthermore, another principal aim of the present study was to
determine whether cervical HPV seroconversion may promote the
recovery of immune status.
Materials and methods
Subjects
The present study was approved by the Ethics
Committee of the Inner Mongolia Medical University of China (Inner
Mongolia, China). The experimental group comprised 136 patients
with LSIL, 263 patients with HSIL and 33 patients with cervical
squamous cell carcinoma (SCC). These patients were all residents of
Inner Mongolia and were diagnosed in the Department of Pathology of
the Inner Mongolia Medical University Affiliated Hospital (Inner
Mongolia, China) between November 2012 and September 2015. The
control group comprised 100 healthy subjects with a sexual history.
None of these patients were pregnant or lactating, had vaginal
bleeding, had acute inflammation of the reproductive organs, and
none of them had received systemic administration of antibiotics
within 2 weeks or sex hormones within 3 months. None of the
participants had severe heart, lung, liver, kidney or hematopoietic
system diseases, nor any psychiatric illnesses or a
poorly-functioning immune system (such as in cases of other
malignancies, various immune diseases or following the
administration of immunosuppressive agents).
The age ranges of all groups were homogeneous and
could be compared. In the control group, the mean age of the
patients was 39.98±6.00 years (range, 29–56 years). In the LSIL
group, the mean age of the patients was 41.81±7.97 years (range,
24–58 years). In the HSIL group, the mean age of the patients was
44.22±9.13 years (range, 23–57 years). In the cervical SCC group,
the mean age of the patients was 50.70±11.06 years (range, 27–77
years). Within the 1-year follow-up period, the percentage of
patients lost to follow-up at 3, 6 and 12 months after treatment
was 25, 15.4 and 14.0%, respectively, in the LSIL group; 22.8, 16.7
and 16.3%, respectively, in the HSIL group; and 0, 12.1 and 15.1%,
respectively, in the cervical SCC group.
Specimen collection
Sterile syringes were used to rinse the upper 1/3 of
the vaginal wall and the cervix with 5 ml 0.9% sodium chloride.
Next, vaginal lavage fluid was drawn from the posterior fornix and
centrifuged at 1,006.2 × g for 10 min at 37°C. The supernatant was
transferred into small tubes and was stored for ~1 month at −20°C
for subsequent sIgA, IgG, IL-2 and IL-10 analysis. A HPV sampling
brush (Guangdong Hybribio Biotechnology Co., Ltd., Guangzhou,
China) was placed deep into the cervix, rotated clockwise in a full
circle 3–5 times, and placed into a sample tube with
cell-preserving fluid (Guangdong Hybribio Biotechnology Co., Ltd.).
The brush head was left in the sample tube, which was subsequently
placed into a frozen storage box, according to the manufacturer's
protocols, and then sent to the Clinical Laboratory of The
Affiliated Hospital of Inner Mongolia Medical University (Hohhot,
China) due to insufficient experimental funds and sites in the
present institute.
Treatment methods
Low-grade patients were administered vaginal
medication (recombinant human interferon α2a vaginal suppository;
S10980006; Wuhan Vio Pharmaceutical, Co., Ltd., Wuhan, China). CIN
grade II patients were treated with vaginal medication following a
loop electrosurgical excision procedure. All CIN III patients
underwent cervical conization. All patients with cervical SCC at
stage IA1 underwent a total hysterectomy via the vagina.
Experimental methods
The expression levels of immune factors, sIgA, IgG,
IL-2 and IL-10, in the vaginal lavage fluid were determined by
ELISA (R&D systems Quantikine ELISA human sIgA, IgG, IL-2 and
IL-10 kit, 96t; catalog nos.: sIgA, E0364; IgG, F0119; IL-2, D2050;
IL-10, D1000B) prior to and 3, 6 and 12 months after treatment. The
presence of HPV in the cervical secretion was detected using the
Fluorescent PCR for HPV DNA test.
Data analysis
Data were analyzed in the Public Health College of
the Medical University of Tianjin (Tianjin, China) using SAS 9.2
statistical software (SAS Institute, Inc., Cary, NC, USA).
Quantitative data in a single-factor design with multiple levels
were expressed as the mean ± standard deviation, and were evaluated
using multiple-level one-way analysis of variance (ANOVA) followed
by Student-Newman-Keuls post hoc test. Quantitative data in
multi-factor design were evaluated using two-way ANOVA followed by
Fisher's least significant difference post hoc test. P≤0.05 was
considered to indicate a statistically significant difference.
Results
Associations between the expression
levels of IL-2, IL-10, IgG and sIgA and the IL-2/IL-10 ratio prior
to treatment
Two-way ANOVA revealed that differences in IL-2,
IL-10 and sIgA levels and the IL-2/IL-10 ratio between the
experimental groups were statistically significant (P<0.05;
Table I). The difference in IgG
expression between the experimental groups was not statistically
significant (P>0.05; Table I).
Expression levels of immune factors were generally higher in
patients with HPV infection than in those without HPV infection,
but the difference in the same immune index between patients with
or without HPV infection was not statistically significant
(P>0.05; Table I).
 | Table I.Association between the expression
levels of IL-2, IL-10, IgG and sIgA, and the IL-2/IL-10 ratio prior
to treatment. |
Table I.
Association between the expression
levels of IL-2, IL-10, IgG and sIgA, and the IL-2/IL-10 ratio prior
to treatment.
|
| IL-2 | IL-10 | IL-2/IL-10 | sIgA | IgG |
|---|
|
|
|
|
|
|
|
|---|
| Group | HPV (−) | HPV (+) | HPV (−) | HPV (+) | HPV (−) | HPV (+) | HPV (−) | HPV (+) | HPV (−) | HPV (+) |
|---|
| Control | 64.35±16.84 | 57.06±21.15 | 30.78±22.41 | 30.19±21.06 | 4.91±5.97 | 8.11±17.36 | 1.67±0.94 | 1.41±0.62 | 2.85±1.57 | 3.12±1.62 |
| LSIL |
63.36±18.67a |
63.59±22.74a |
12.70±8.35a |
13.59±6.52a |
12.72±16.28a |
9.25±14.33a |
1.36±16.69a |
1.02±1.24a | 4.22±4.42 | 3.81±6.29 |
| HSIL |
44.33±16.84a |
45.27±17.15a |
18.85±9.69a |
18.35±8.69a |
4.28±5.54a |
4.45±6.40a |
1.36±1.28a |
1.28±1.15a | 5.52±8.30 | 6.87±8.38 |
| SCC |
70.33±44.22a |
81.92±74.70a |
30.99±24.63a |
47.37±15.36a |
3.74±2.78a |
2.21±2.40a |
1.02±0.55a |
1.46±1.04a | 7.47±8.84 | 6.71±9.80 |
Associations between HPV
seroconversion and IL-2, IL-10, IgG and sIgA expression levels and
the IL-2/IL-10 ratio in patients with different severities of
cervical lesions following treatment
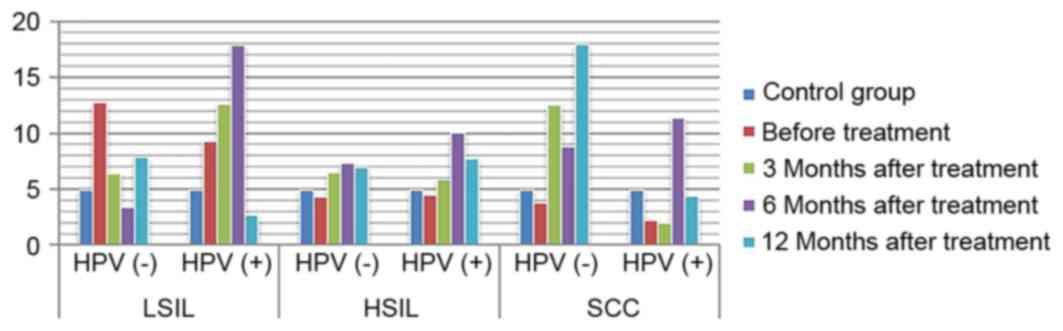
ANOVA in a factorial design revealed that, following
treatment, differences in IL-2 and IL-10 expression levels, as well
as differences in the IL-2/IL-10 ratio, between patients with
varying degrees of disease and the presence or absence of infection
were statistically significant (P<0.05). For IL-2 expression
level, the highest level of expression was found in high-grade
lesions. IL-10 expression level increased with the severity of the
disease increased. The ratio of IL-2 to IL-10 was the highest in
low-grade lesions, and decreased gradually with the increase of
disease severity, and was the lowest in HPV positive cervical
cancer. The expression of IL-2 in HPV negative patients with
low-grade lesions increased gradually with the treatment, while the
expression of IL-2 in HPV positive patients increased
insignificantly. The expression of IL-2 in HPV negative patients
with high-grade lesions and cervical cancer patients increased
slightly with the treatment. The amount of expression increased
significantly, while the expression level of HPV persistently
decreased (P<0.05). The expression of IL-10 in patients with
HPV-negative and HPV-positive cervical cancer was increased with
the treatment. The expression of IL-10 in patients with
HPV-negative and HPV-positive cervical cancer decreased with the
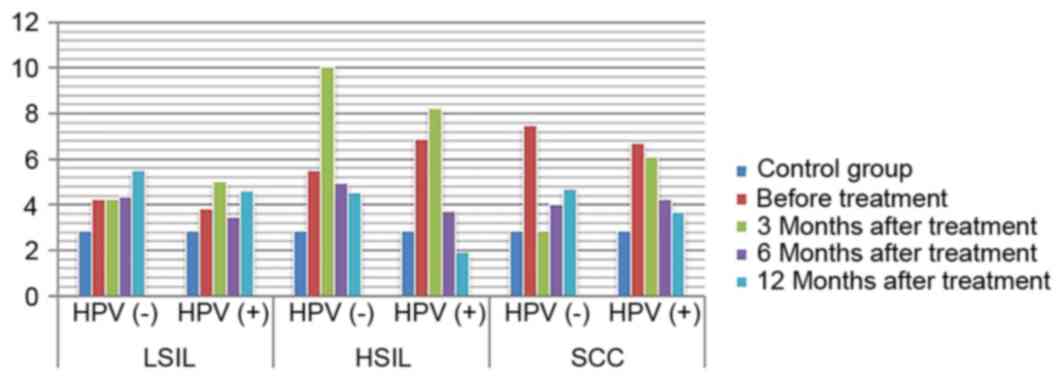
treatment (P<0.05). IL-2/IL-10 ratio of HPV-negative patients in
low-grade and high-grade lesions increased gradually with the
treatment, while that of HPV-positive patients showed an increasing
trend. However, the expression of IL-2/IL-10 in HPV-negative
patients and HPV-persistent patients in cervical cancer increased
gradually with the treatment (P<0.05) (Figs. 1–4).
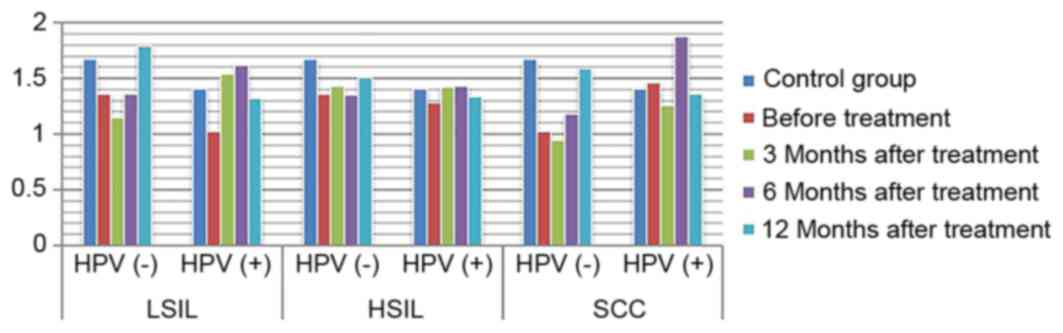
The difference in IgG expression was not statistically significant
(P>0.05). In the LSIL group, expression of sIgA was increased in
the HPV negative after infection group, and decreased gradually
through the treatment of HPV persistent infection. By comparing the
difference in sIgA expression between patients with different
degrees of disease as statistically significant (P<0.05), while
the difference in IgG expression in the HSIL group and the cervical
SCC group was not statistically significant (P>0.05; Figs. 5, 6).
Discussion
The immunity of the tumor microenvironment is a
novel concept regarding the mutual resistance of the immunity of
malignant tumors and tumor cells. A previous study demonstrated
that the immunological function of the local microenvironment may
have been inhibited when systemic immunity had not undergone any
significant change in the early stages of cancer (7). The cervix is exposed in the vagina and
thus, cervical HPV infection and cervical lesions are associated
with the influence of the vaginal microenvironment. The vaginal
microenvironment is composed of the vaginal local immunity, the
vaginal microbial flora and the endocrine regulation of the body.
Among these, the vaginal local immunity and the systemic immunity
have similar compositions and primarily include humoral immunity
and cellular immunity (8). When HPV
infection occurs, the sIgA level in the genital tract may directly
reflect the status and outcome of the local immune function in the
cervix and vagina (9). When mucosal
immunity occurs, it may induce IgG production in the blood, which
leaks into the genital tract, and IgA in the genital tract
secretion is primarily produced from the local mucosa in the
genital tract. Changes in IL-2 and IL-10 expression in the serum of
patients with cervical cancer indicate that the immune response may
change accordingly (10).
The process through which cervical HPV infection
induces cervical cancer is long-term and dynamic. In the process of
HPV infection, a corresponding immune response mechanism may be
produced to resist the infection and invasion of the virus.
Therefore, the infection in the majority of people would disappear
over time (11). Only 5–10% of
infected patients develop persistent infections when the immune
function of the body is damaged or inhibited (12). Whether HPV infection will be
eliminated or will develop into cervical lesions primarily depends
upon the systemic and vaginal local immune functions. In the
present study, the results of the HPV test in patients with
cervical lesions in Inner Mongolia revealed that, prior to
treatment, the infection rate of HPV in patients with cervical
lesions increased gradually with an increase in the grade of
cervical lesions. Furthermore, the proportion of patients with
high-risk HPV infection increased with an increase in the grade of
cervical lesions; this means that high-level (HSIL) lesions have a
higher rate of high-risk HPV infection. During persistent HPV
infection, the balance of type 1 T helper (Th1)/Th2 cell functions
is dysrupted. In a previous study, Th2 cells served erethitic
functions and inhibited the immune response of the body (13). Furthermore, the integration of HPV in
host cells may further damage or impair immune function, leading to
a cycle of viral infection and immune function damage in patients
with HPV infection (14). IL-2
expression was highest in the cervical SCC group prior to treatment
and was lowest in the HSIL group. In patients without HPV
infection, the expression of IL-2 was not significantly different
to that of the healthy controls. IL-10 expression gradually
increased with the increase in the grade of cervical lesions, which
was highest in the cervical SCC group. When sustained cervical HPV
infection causes an imbalance in the Th1/Th2 ratio in the vaginal
microenvironment, its adaptive immune response tends toward Th2
(15), causing continuous changes in
the vaginal microecology and immune status. In the present study,
the IL-2/IL-10 ratio gradually decreased prior to treatment and was
lowest in the cervical SCC group, suggesting that the immune status
drifted toward Th2 with the rise in the severity of the cervical
lesions, for example, when comparing low and high level lesions.
The main humoral immune mechanism is the activation of B cells
following virus invasion and the B cell-induced production of
plasma cells, which secrete corresponding antibodies to bind with
antigens, thereby eliminating viruses. Compared with cellular
immunity, humoral immunity occurs later and often elicits a lesser
effect. The results of the present study revealed that IgG
expression level in vaginal secretion increased with an increase in
the grade of cervical lesions, and the sIgA expression in patients
with all grades of lesions was significantly lower than in the
healthy controls.
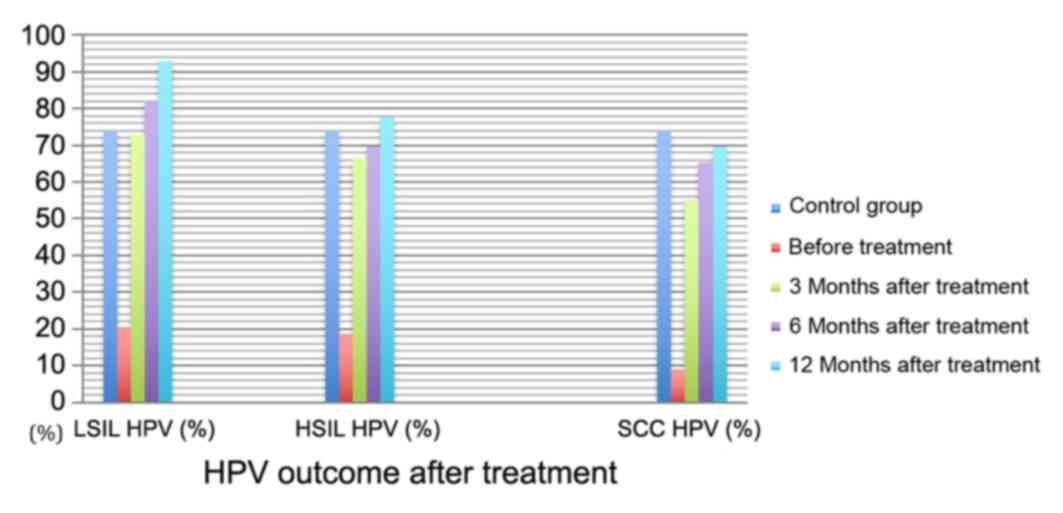
The results of the present study suggest that HPV
infection is an important factor in the occurrence of high-grade
cervical lesions. However, HPV clears up and the grade of lesions
gradually decreases when the lesion tissue is removed or local
immunotherapy is performed. HPV seroconversion occurs in patients
with HPV infection 6 months after treatment, and patients with
cervical lesions recover to a healthy state an average of 32 months
after treatment (16). The present
study revealed that the scavenging rate of local HPV infection in
patients gradually increased with treatment time (Table I). The infection rate in patients in
the LSIL group was similar to that in the control group at 3 months
after treatment, while in the HSIL group, this time was 12 months
after treatment. This revealed that the occurrence of cervical
lesions was associated with HPV infection, and that HPV outcome was
associated with the grade of cervical lesions during post-treatment
follow-up. The higher the grade of the disease, the later the HPV
seroconversion occurred following treatment. With the same
treatment time, the higher the grade of cervical lesion, the lower
the HPV seroconversion rate. The risks of lesions and recurrence
were significantly increased in patients with persistent HPV
infection following treatment (17).
Therefore, promoting the seroconversion of HPV infection has become
the focus of research internationally.
A study revealed that the immune evasion mechanism
of HPV may occur at the early stage of infection (18). The vaginal anti-inflammatory
microenvironment creates the conditions in which virus infection
occurs. However, promoting HPV seroconversion and improving the
outcome of cervical lesions following treatment through changing
the status of immune drift has become the principal target of
present studies (19). In a study on
cellular immunity in patients with cervical cancer following
surgery (20), it was revealed that
the secretion of Th1 cells was significantly decreased in patients
with cervical cancer, suggesting that the ability of immune cells
to secrete cytokine was inhibited, and cellular immune function
recovered following surgery. The present study revealed that
recovery was not significant at 3–12 months after treatment in the
LSIL group. This may be due to the fact that the planting and
invasion of the HPV virus to the basal layer of cervical epithelial
cells was unstable in patients with low-grade lesions. Therefore,
there was no significant change in the immune response over a short
period of time following treatment. In the HSIL and cervical SCC
groups, patients with HPV seroconversion presented with
significantly increased IL-2 expression following treatment, while
IL-2 expression decreased in patients with persistent HPV
infection. These results indicated that Th1 cell function gradually
recovered following treatment in patients without HPV infection.
IL-2 expression significantly increased 1 year after treatment, but
this was not recovered in patients with persistent HPV infection.
This suggests that there was an association between HPV
seroconversion and the recovery of vaginal local immunity, while
patients with persistent HPV infection presented with continuous
immune damage. IL-10 expression was lower in patients without HPV
in the LSIL and HSIL groups at different treatment times, and this
expression level increased with an increase in treatment time. In
the cervical SCC group, IL-10 expression gradually decreased in the
presence of HPV infection. The IL-2/IL-10 ratio increased with
treatment time in patients with all grades of cervical lesions and
negative HPV. This suggests that the local immunity tended toward
Th1 when HPV seroconversion occurred. The IL-2/IL-10 ratio in
patients with all grades of lesions increased at 6 months after
treatment, but decreased again at 12 months after treatment,
suggesting that vaginal local immunity may recover again and may
resist HPV infection at 6 months after treatment.
There are certain stable lymphocytes and macrophages
in the vagina, which simultaneously serve a role in immune
phagocytosis in the invasion of exogenous pathogens, promote
cellular immune response and activate humoral immunity; and this
forms the first line of defense for preventing the invasion of
pathogens (21). IgG is the main
antibody in the serum and the extracellular fluid, and may
persistently exist in the vaginal local immunity throughout the
process of HPV infection (22). Lee
et al (23) reported that
serum IgG expression was lower in HPV-positive cervical cancer
patients than in HPV-negative patients at 1-year follow-up. This
suggests that immune factors may serve an important role in
promoting HPV seroconversion in patients in different grades of
cervical lesions. A number of studies revealed that when mild
inflammation occurred in the genital tract, sIgA secretion
increased to remove pathogens (21,24).
When inflammation continued to progress and the mucosal epithelial
cells and plasma cells were damaged, the defense function was
weakened and sIgA secretion was decreased. Therefore, the local
sIgA level in the vagina has become an index for the diagnosis and
prognosis of HPV infection in the genital tract. This may partly
reflect the severity of cervical lesions (25,26), and
may be used as an index for the diagnosis and classification of
diseases. The present study revealed that the difference in IgG
expression between the LSIL group and the control group prior to
and following treatment was statistically significant.
Additionally, the expression level in patients without HPV
infection returned to a level similar to that in the control group
at 12 months after treatment. This suggests that the immune
inhibitory state in patients with low-grade cervical lesions prior
to treatment may return to normal levels following treatment. IgG
expression significantly increased following treatment in the HSIL
group. The difference in sIgA expression level between the cervical
cancer group and the control group was not statistically
significant, and the reason for this may be associated with the
significant immune response in the serum. In the LSIL group, sIgA
expression decreased prior to treatment and gradually increased
following treatment, suggesting that there was an immune inhibitory
state in the patients with low-grade cervical lesions prior to
treatment and that immune function may recover following treatment.
The difference in sIgA expression between the HSIL group and the
cervical SCC group prior to and following treatment was not
statistically significant, but the increase was faster in
HPV-negative patients than in HPV-positive patients. This may be
due to the fact that the immune response time was long and sIgA
secretion from the mucosa was reduced compared with that at the
initial stage of anti-infection treatment.
The present study demonstrated that, as the HPV
infection rate decreases in cervical lesions following treatment,
the immune response in the vagina gradually recovers from the
inhibitory state, and humoral immunity also reverts back to its
normal state. Furthermore, immune recovery in patients with HPV
seroconversion is more ideal compared with that in patients with
persistent HPV infection. These results further confirm the role
served by HPV infection in damaging the vaginal local immunity and
that, in the treatment of HPV infection, purposefully improving the
immune function of the patients may have a synergistic effect on
HPV seroconversion. Therefore, the expression of immune factors and
the presence of HPV infection in the vaginal microenvironment are
associated with the occurrence of cervical lesions. Therefore, in
the process of detection and follow-up, understanding the cervical
and vaginal immune status may have important clinical significance
in the prevention and treatment of cervical HPV infection, and in
the treatment of patients with cervical lesions. However, the
present study on the vaginal local immunity mechanism has
limitations. In order to improve the ability of the vaginal
microenvironment to prevent virus invasion, improving the immune
microenvironment and state has become a reasonable novel direction
in the study of HPV infection and cervical lesions.
Acknowledgements
Not applicable.
Funding
The present study was funded by the National Natural
Science Foundation of China (grant no. 81260095).
Availability of data and materials
The datasets used and/or analysed during the present
study available from the corresponding author on reasonable
request.
Authors' contributions
JM provided substantial contributions to the
conception and design of the work; JM and JS undertook the
acquisition, analysis, and interpretation of data for the work. JM
and JS undertook manuscript drafting and revisions and are
accountable for all aspects of the work in ensuring that questions
related to the accuracy or integrity of any part of the work are
appropriately investigated and resolved.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the Inner Mongolia Medical University of China (Inner
Mongolia, China). Written informed consent was obtained from all
patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kurman RJ, Carcangiu ML, Herrington CS and
Young RH: World Health Organization classification of tumours of
female reproductive organs4th. Lyon: IARC Press; pp. 8–25. 2014
|
|
2
|
Tavassoli FA and Devilee P: World Health
Organization Classification of Tumors, Pathology and Genetics of
Tumors of the Breast and Female Genital Organs2014
|
|
3
|
Jensen KE, Schmiedel S, Norrild B,
Frederiksen K, Iftner T and Kjaer SK: Parity as a cofactor for
high-grade cervical disease among women with persistent human
papillomavirus infection: A 13-year follow-up. Br J Cancer.
108:234–239. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Luhn P, Walker J, Schiffman M, Zuna RE,
Dunn ST, Gold MA, Smith K, Mathews C, Allen RA, Zhang R, Wang S and
Wentzensen N: The role of co-factors in the progression from human
papillomavirus infection to cervical cancer. Gynecol Oncol.
128:265–270. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Griffin C, Harding J and Sutton C: Re: The
vaginal microbiome, vaginal anti-microbial defence mechanisms and
the clinical challenge of reducing infection-related preterm birth.
BJOG. 122:10332015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nguyen ML and Flowers L: Cervical cancer
screening in immunocompromised women. Obstet Gynecol Clin North Am.
40:339–357. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Stanley M: Immunobiology of HPV and HPV
vaccines. Gynecol Oncol. 109 (Suppl 2):S15–S21. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Prata TT, Bonin CM, Ferreira AM, Padovani
CT, Fernandes CE, Machado AP and Tozetti IA: Local
immunosuppression induced by high viral load of human
papillomavirus: Characterization of cellular phenotypes producing
interleukin-10 in cervical neoplastic lesions. Immunology.
146:113–121. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hwang TS, Jeong JK, Park M, Han HS, Choi
HK and Park TS: Detection and typing of HPV genotypes in various
cervical lesions by HPV oligonucleotide microarray. Gynecol Oncol.
90:51–56. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pineo CB, Hitzeroth II and Rybicki EP:
Immunogenic assessment of plant-produced human papillomavirus type
16 L1/L2 chimaeras. Plant Biotechnol J. 11:964–975. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chen Y: The changes of local immunity,
microcirculation status and serum immune status in patients with
cervical cancer. J Hainan Med Univ. 20:226–228. 2014.
|
|
12
|
Rodríguez AC, Schiffman M, Herrero R,
Hildesheim A, Bratti C, Sherman ME, Solomon D, Guillén D, Alfaro M,
Morales J, et al: Longitudinal study of human papillomavirus
persistence and cervical intraepithelial neoplasia grade 2/3:
Critical role of duration of infection. J Natl Cancer Inst.
102:315–324. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kobayashi A, Greenblatt RM, Anastos K,
Minkoff H, Massad LS, Young M, Levine AM, Darragh TM, Weinberg V
and Smith-McCune KK: Functional attributes of mucosal immunity in
cervical intraepithelial neoplasia and effects of HIV infection.
Cancer Res. 64:6766–74. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Baussano I, Ronco G, Segnan N, French K,
Vineis P and Garnett GP: HPV-16 infection and cervical cancer:
Modeling the influence of duration of infection and precancerous
lesions. Epidemics. 2:21–28. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Torres-Poveda K, Bahena-Román M,
Madrid-González C, Burguete-García AI, Bermúdez-Morales VH,
Peralta-Zaragoza O and Madrid-Marina V: Role of IL-10 and TGF-β1 in
local immunosuppression in HPV-associated cervical neoplasia. World
J Clin Oncol. 5:753–763. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kim YT, Lee JM, Hur SY, Cho CH, Kim YT,
Kim SC and Kang SB: Clearance of human papillomavirus infection
after successful conization in patients with cervical
intraepithelial neoplasia. Int J Cancer. 126:1903–1909. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Park JY, Bae J, Lim MC, Lim SY, Lee DO,
Kang S, Park SY, Nam BH and Seo SS: Role of high risk-human
papilloma virus test in the follow-up of patients who underwent
conization of the cervix for cervical intmepithelial neoplasia. J
Gynecol Oncol. 20:86–90. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tsuda K, Yamanaka K, Kitagawa H, Akeda T,
Naka M, Niwa K, Nakanishi T, Kakeda M, Gabazza EC and Mizutani H:
Calcineurin inhibitors suppress cytokine production from memory T
cells and differentiation of naïve T cells into cytokine-producing
mature T cells. PLoS One. 7:e314652012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Vidal AC, Skaar D, Maguire R, Dodor S,
Musselwhite LW, Bartlett JA, Oneko O, Obure J, Mlay P, Murphy SK
and Hoyo C: IL-10, IL-15, IL-17, and GMCSF levels in cervical
cancer tissue of Tanzanian women infected with HPV16/18 vs.
non-HPV16/18 genotypes. Infect Agents Cancer. 10:102015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tang XF, Xu HJ, Guo LH, Gu YF, Tai LZ and
Duan Y: Changes and clinical significance of T lymphocyte immune
function in cervical cancer patients after operation. Chin J
Nosocomiol. 25:1270–1272. 2015.
|
|
21
|
van de Ven AA, Janssen WJ, Schulz LS, van
Loon AM, Voorkamp K, Sanders EA, Kusters JG, Nierkens S, Boes M,
Wensing AM and van Montfrans JM: Increased prevalence of
gastrointestinal viruses and diminished secretory immunoglobulin a
levels in antibody deficiencies. J Clin Immunol. 34:962–970. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
de Gruijl TD, Bontkes HJ, Walboomers JM,
Schiller JT, Stukart MJ, Groot BS, Chabaud MM, Remmink AJ,
Verheijen RH, Helmerhorst TJ, et al: Immunoglobulin G responses
against human papillomavirus type 16 virus-like particles in a
prospective nonintervention cohort study of women with cervical
intraepithelial neoplasia. J Natl Cancer I nst. 89:630–663. 1997.
View Article : Google Scholar
|
|
23
|
Lee SR, Zhang SY, Liu DQ and Han CL:
Effects of IgG, INF- and CD4+/CD8+T cells on the prognosis of high
risk HPV infection in different cervical lesions. Chin Matern Child
Health Care. 30:5125–5126. 2015.
|
|
24
|
Passmore JA, Marais DJ, Sampson C, Allan
B, Parker N, Milner M, Denny L and Williamson AL: Cervicovaginal,
oral, and serum IgG and IgA responses to human papillomavirus type
16 in women with cervical intraepithelial neoplasia. J Med Virol.
79:1375–1380. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hurlimann J, Dayal R and Gloor E:
Immunoglobulins and secretory component in endometrium and cervix.
Influence of inflammation and carcinoma. Virchows Arch A Pathol
Anat Histol. 377:211–223. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Warner RH, Stevens FM and McCarthy CF:
Salivary SIgA and SIgA 1 in coeliac disease, inflammatory bowel
disease and controls. Ir J Med Sci. 168:33–35. 1999. View Article : Google Scholar : PubMed/NCBI
|