|
1
|
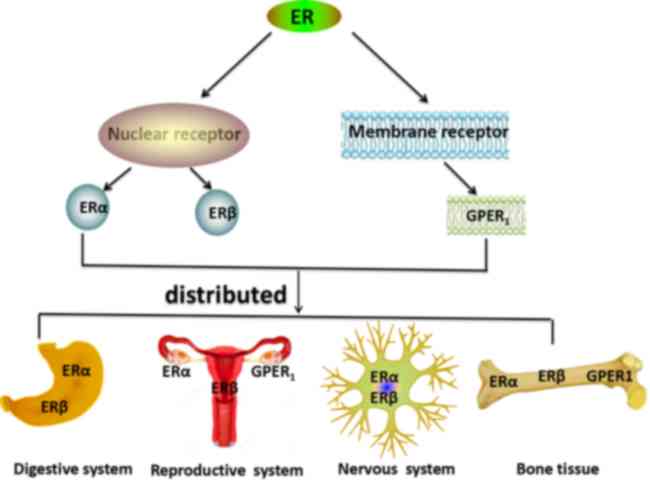
Simpson ER: Sources of estrogen and their
importance. J Steroid Biochem Mol Biol. 86:225–230. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Guyton AC and Hall J: Guyton and Hall
Textbook of Medical Physiology. 957–999. 2011.
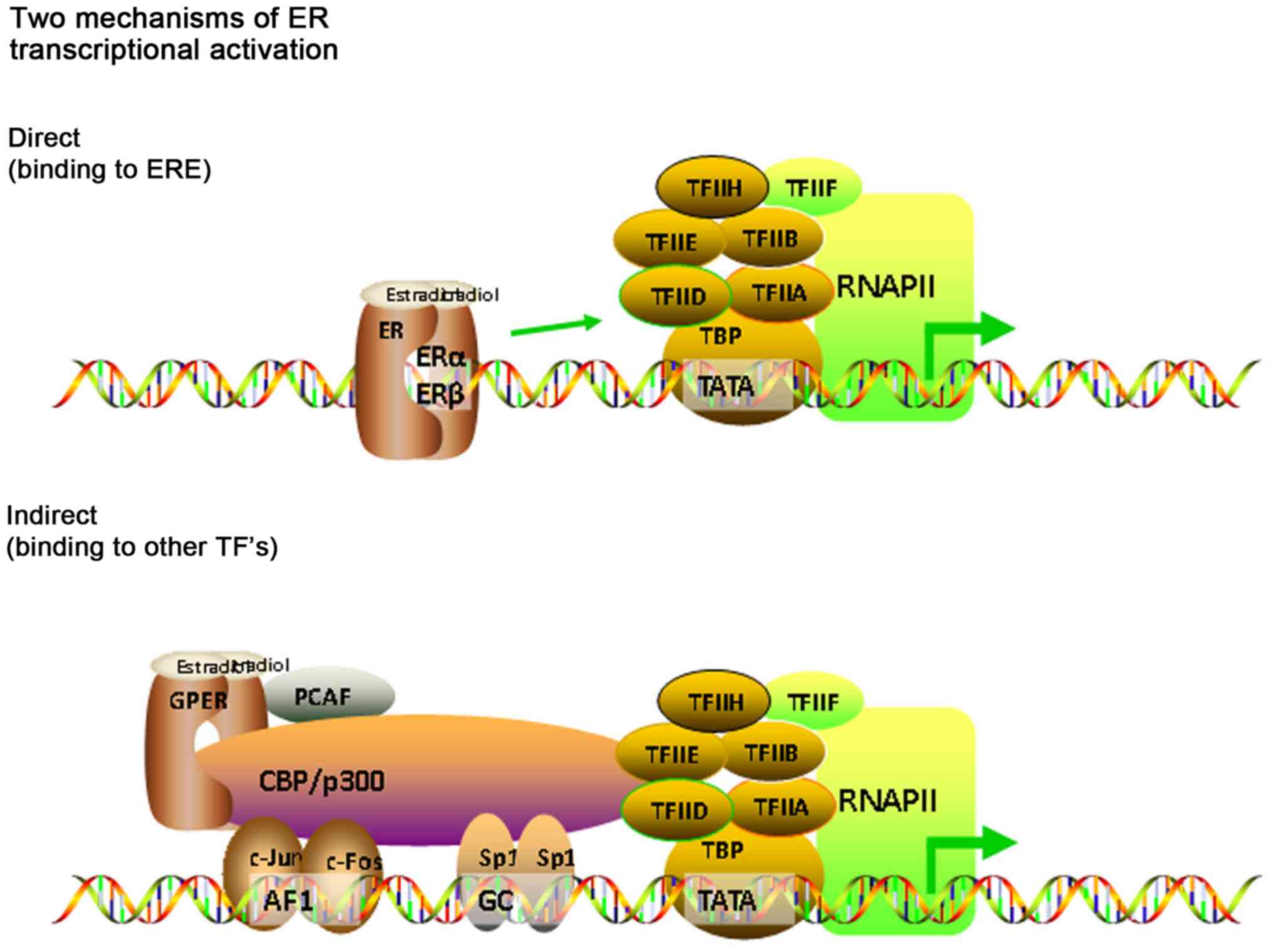
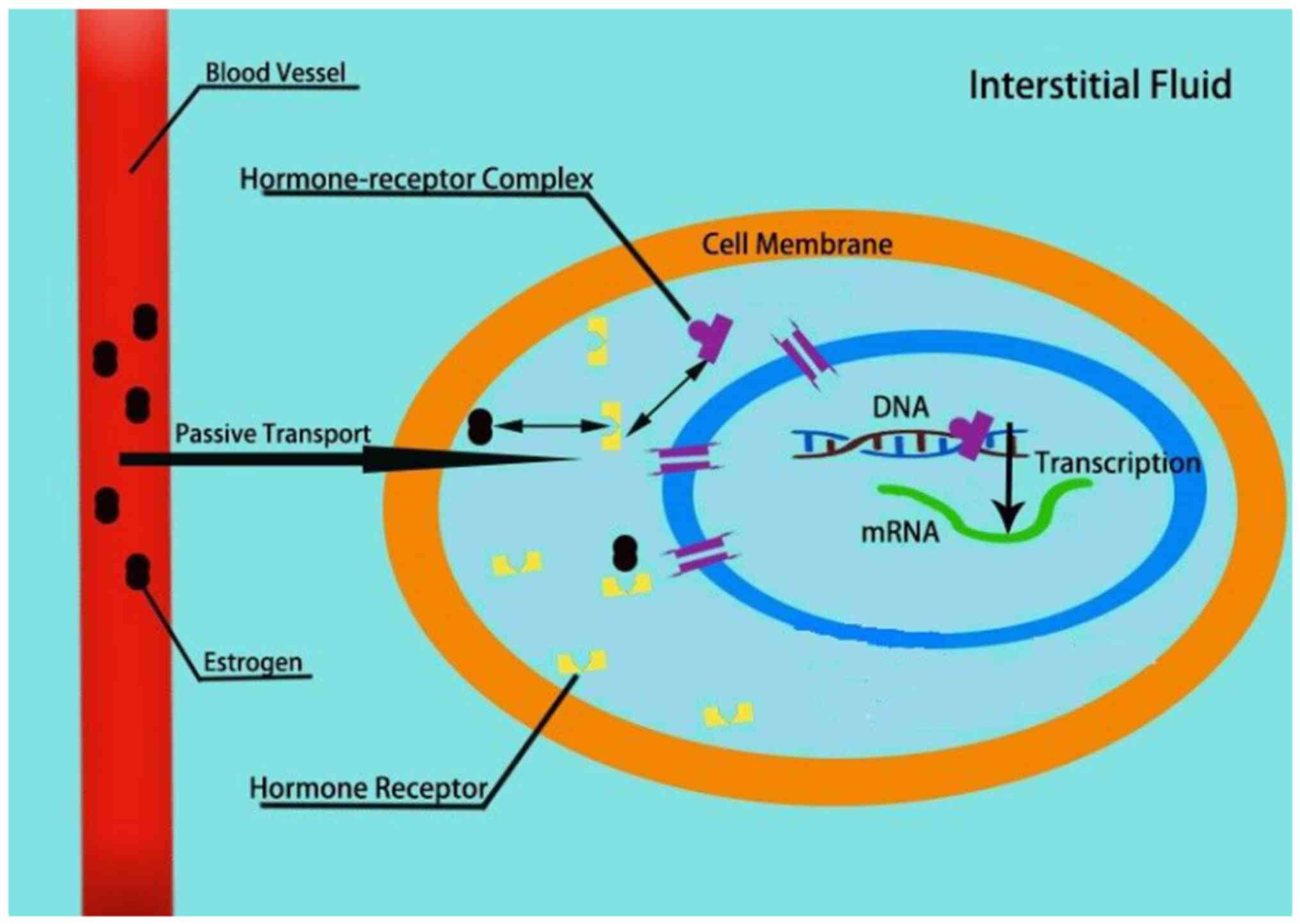
|
|
3
|
Nilsson S and Gustafsson JA: Estrogen
receptors: Therapies targeted to receptor subtypes. Clin Pharmacol
Ther. 89:44–55. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Labrie F: Extragonadal synthesis of sex
steroids: Intracrinology. Ann Endocrinol (Paris). 64:95–107.
2003.PubMed/NCBI
|
|
5
|
Kim YS, Kim N and Kim GH: Sex and gender
differences in gastroesophageal reflux disease. J
Neurogastroenterol Motil. 22:575–588. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kurt D, Saruhan BG, Kanay Z, Yokus B,
Kanay BE, Unver O and Hatipoglu S: Effect of ovariectomy and female
sex hormones administration upon gastric ulceration induced by cold
and immobility restraint stress. Saudi Med J. 28:1021–1027.
2007.PubMed/NCBI
|
|
7
|
Meleine M and Matricon J: Gender-related
differences in irritable bowel syndrome: Potential mechanisms of
sex hormones. World J Gastroenterol. 20:6725–6743. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Batistatou A, Stefanou D, Goussia A,
Arkoumani E, Papavassiliou AG and Agnantis NJ: Estrogen receptor
beta (ERbeta) is expressed in brain astrocytic tumors and declines
with dedifferentiation of the neoplasm. J Cancer Res Clin Oncol.
130:405–410. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yang H, Sukocheva OA, Hussey DJ and Watson
DI: Estrogen, male dominance and esophageal adenocarcinoma: Is
there a link? World J Gastroenterol. 18:393–400. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Enmark E, Pelto-Huikko M, Grandien K,
Lagercrantz S, Lagercrantz J, Fried G, Nordenskjold M and
Gustafsson JA: Human estrogen receptor beta-gene structure,
chromosomal localization, and expression pattern. J Clin Endocrinol
Metab. 82:4258–4265. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rochira V, Granata AR, Madeo B, Zirilli L,
Rossi G and Carani C: Estrogens in males: What have we learned in
the last 10 years? Asian J Androl. 7:3–20. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Heldring N, Pike A, Andersson S, Matthews
J, Cheng G, Hartman J, Tujague M, Strom A, Treuter E, Warner M and
Gustafsson JA: Estrogen receptors: How do they signal and what are
their targets. Physiol Rev. 87:905–931. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Carmeci C, Thompson DA, Ring HZ, Francke U
and Weigel RJ: Identification of a gene (GPR30) with homology to
the G-protein-coupled receptor superfamily associated with estrogen
receptor expression in breast cancer. Genomics. 45:607–617. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Filardo EJ and Thomas P: Minireview: G
protein-coupled estrogen receptor-1, GPER-1: Its mechanism of
action and role in female reproductive cancer, renal and vascular
physiology. Endocrinology. 153:2953–2962. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sanden C, Broselid S, Cornmark L,
Andersson K, Daszkiewicz-Nilsson J, Martensson UE, Olde B and
Leeb-Lundberg LM: G protein-coupled estrogen receptor 1/G
protein-coupled receptor 30 localizes in the plasma membrane and
traffics intracellularly on cytokeratin intermediate filaments. Mol
Pharmacol. 79:400–410. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Filardo EJ, Quinn JA, Bland KI and
Frackelton AR Jr: Estrogen-induced activation of Erk-1 and Erk-2
requires the G protein-coupled receptor homolog, GPR30, and occurs
via trans-activation of the epidermal growth factor receptor
through release of HB-EGF. Mol Endocrinol. 14:1649–1660. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Revankar CM, Cimino DF, Sklar LA,
Arterburn JB and Prossnitz ER: A transmembrane intracellular
estrogen receptor mediates rapid cell signaling. Science.
307:1625–1630. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Thomas P, Pang Y, Filardo EJ and Dong J:
Identity of an estrogen membrane receptor coupled to a G protein in
human breast cancer cells. Endocrinology. 146:624–632. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sharma G and Prossnitz ER:
G-protein-coupled estrogen receptor (GPER) and sex-specific
metabolic homeostasis. Adv Exp Med Boil. 1043:427–453. 2017.
View Article : Google Scholar
|
|
20
|
Vakil N, van Zanten SV, Kahrilas P, Dent J
and Jones R; Globale Konsensusgruppe, : The Montreal definition and
classification of gastroesophageal reflux disease: A global,
evidence-based consensus paper. Z Gastroenterol. 45:1125–1140.
2007.(Article in German). View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Katzka DA, Pandolfino JE and Kahrilas PJ:
Phenotypes of gastroesophageal reflux disease: Where rome, lyon,
and montreal meet. Clin Gastroenterol Hepatol. July 15–2019.(Epub
ahead of print). View Article : Google Scholar
|
|
22
|
Nam SY, Choi IJ, Ryu KH, Park BJ, Kim YW,
Kim HB and Kim JS: The effect of abdominal visceral fat,
circulating inflammatory cytokines, and leptin levels on reflux
esophagitis. J Neurogastroenterol Motil. 21:247–254. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Pohl H, Wrobel K, Bojarski C, Voderholzer
W, Sonnenberg A, Rosch T and Baumgart DC: Risk factors in the
development of esophageal adenocarcinoma. Am J Gastroenterol.
108:200–207. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Asanuma K, Iijima K and Shimosegawa T:
Gender difference in gastro-esophageal reflux diseases. World J
Gastroenterol. 22:1800–1810. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Iijima K and Shimosegawa T: Involvement of
luminal nitric oxide in the pathogenesis of the gastroesophageal
reflux disease spectrum. J Gastroenterol Hepatol. 29:898–905. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Masaka T, Iijima K, Endo H, Asanuma K, Ara
N, Ishiyama F, Asano N, Koike T, Imatani A and Shimosegawa T:
Gender differences in oesophageal mucosal injury in a reflux
oesophagitis model of rats. Gut. 62:6–14. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Boeckxstaens G, El-Serag HB, Smout AJ and
Kahrilas PJ: Symptomatic reflux disease: The present, the past and
the future. Gut. 63:1185–1193. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Jacobson BC, Moy B, Colditz GA and Fuchs
CS: Postmenopausal hormone use and symptoms of gastroesophageal
reflux. Arch Intern Med. 168:1798–1804. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Van Thiel DH, Gavaler JS and Stremple J:
Lower esophageal sphincter pressure in women using sequential oral
contraceptives. Gastroenterology. 71:232–234. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Nilsson M, Lundegardh G, Carling L, Ye W
and Lagergren J: Body mass and reflux oesophagitis: An
oestrogen-dependent association? Scand J Gastroenterol. 37:626–630.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Nilsson M, Johnsen R, Ye W, Hveem K and
Lagergren J: Obesity and estrogen as risk factors for
gastroesophageal reflux symptoms. JAMA. 290:66–72. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Nordenstedt H, Zheng Z, Cameron AJ, Ye W,
Pedersen NL and Lagergren J: Postmenopausal hormone therapy as a
risk factor for gastroesophageal reflux symptoms among female
twins. Gastroenterology. 134:921–928. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
el-Serag HB: The epidemic of esophageal
adenocarcinoma. Gastroenterol Clin North Am. 31421–440. (viii)2002.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Vizcaino AP, Moreno V, Lambert R and
Parkin DM: Time trends incidence of both major histologic types of
esophageal carcinomas in selected countries, 1973–1995. Int J
Cancer. 99:860–868. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Mathieu LN, Kanarek NF, Tsai HL, Rudin CM
and Brock MV: Age and sex differences in the incidence of
esophageal adenocarcinoma: Results from the surveillance,
epidemiology, and end results (SEER) registry (1973–2008). Dis
Esophagus. 27:757–763. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Wang BJ, Zhang B, Yan SS, Li ZC, Jiang T,
Hua CJ, Lu L, Liu XZ, Zhang DH, Zhang RS and Wang X: Hormonal and
reproductive factors and risk of esophageal cancer in women: A
meta-analysis. Dis Esophagus. 29:448–454. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Wang QM, Qi YJ, Jiang Q, Ma YF and Wang
LD: Relevance of serum estradiol and estrogen receptor beta
expression from a high-incidence area for esophageal squamous cell
carcinoma in China. Med Oncol. 28:188–193. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Zhang Z, He Q, Fu S and Zheng Z: Estrogen
receptors in regulating cell proliferation of esophageal squamous
cell carcinoma: Involvement of intracellular Ca(2+) signaling.
Pathol Oncol Res. 23:329–334. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Hennessy BA, Harvey BJ and Healy V:
17beta-Estradiol rapidly stimulates c-fos expression via the MAPK
pathway in T84 cells. Mol Cell Endocrinol. 229:39–47. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Zuguchi M, Miki Y, Onodera Y, Fujishima F,
Takeyama D, Okamoto H, Miyata G, Sato A, Satomi S and Sasano H:
Estrogen receptor α and β in esophageal squamous cell carcinoma.
Cancer Sci. 103:1348–1355. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Ueo H, Matsuoka H, Sugimachi K, Kuwano H,
Mori M and Akiyoshi T: Inhibitory effects of estrogen on the growth
of a human esophageal carcinoma cell line. Cancer Res.
50:7212–7215. 1990.PubMed/NCBI
|
|
42
|
Menon S, Nightingale P and Trudgill N: Is
hormone replacement therapy in post-menopausal women associated
with a reduced risk of oesophageal cancer? United European
Gastroenterol J. 2:374–382. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Lanas A and Chan FKL: Peptic ulcer
disease. Lancet. 390:613–624. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Kanotra R, Ahmed M, Patel N, Thakkar B,
Solanki S, Tareen S, Fasullo MJ, Kesavan M, Nalluri N, Khan A, et
al: Seasonal variations and trends in hospitalization for peptic
ulcer disease in the United States: A 12-year analysis of the
nationwide inpatient sample. Cureus. 8:e8542016.PubMed/NCBI
|
|
45
|
Suleyman H, Albayrak A, Bilici M, Cadirci
E and Halici Z: Different mechanisms in formation and prevention of
indomethacin-induced gastric ulcers. Inflammation. 33:224–234.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Feldman M, Richardson CT and Walsh JH:
Sex-related differences in gastrin release and parietal cell
sensitivity to gastrin in healthy human beings. J Clin Invest.
71:715–720. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Sangma TK, Jain S and Mediratta PK: Effect
of ovarian sex hormones on non-steroidal anti-inflammatory
drug-induced gastric lesions in female rats. Indian J Pharmacol.
46:113–116. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Okada K, Inamori M, Imajyo K, Chiba H,
Nonaka T, Shiba T, Sakaguchi T, Atsukawa K, Takahashi H, Hoshino E
and Nakajima A: Gender differences of low-dose aspirin-associated
gastroduodenal ulcer in Japanese patients. World J Gastroenterol.
16:1896–1900. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Speir E, Yu ZX, Takeda K, Ferrans VJ and
Cannon RO III: Antioxidant effect of estrogen on
cytomegalovirus-induced gene expression in coronary artery smooth
muscle cells. Circulation. 102:2990–2996. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Jiang F and Shen X: Current prevalence
status of gastric cancer and recent studies on the roles of
circular RNAs and methods used to investigate circular RNAs. Cell
Mol Biol Lett. 24:532019. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Chung HW, Noh SH and Lim JB: Analysis of
demographic characteristics in 3242 young age gastric cancer
patients in Korea. World J Gastroenterol. 16:256–263. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Tokunaga A, Kojima N, Andoh T, Matsukura
N, Yoshiyasu M, Tanaka N, Ohkawa K, Shirota A, Asano G and Hayashi
K: Hormone receptors in gastric cancer. Eur J Cancer Clin Oncol.
19:687–689. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Lindblad M, Ye W, Rubio C and Lagergren J:
Estrogen and risk of gastric cancer: A protective effect in a
nationwide cohort study of patients with prostate cancer in Sweden.
Cancer Epidemiology Biomarkers Prev. 13:2203–2207. 2004.
|
|
54
|
Furukawa H, Iwanaga T, Koyama H and
Taniguchi H: Effect of sex hormones on the experimental induction
of cancer in rat stomach-a preliminary study. Digestion.
23:151–155. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Kim MJ, Cho SI, Lee KO, Han HJ, Song TJ
and Park SH: Effects of 17β-estradiol and estrogen receptor
antagonists on the proliferation of gastric cancer cell lines. J
Gastric Cancer. 13:172–178. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Chandanos E and Lagergren J: Oestrogen and
the enigmatic male predominance of gastric cancer. Eur J Cancer.
44:2397–2403. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Sunakawa Y, Cao S, Berger MD, Matsusaka S,
Yang D, Zhang W, Ning Y, Parekh A, Stremitzer S, Mendez A, et al:
Estrogen receptor-beta genetic variations and overall survival in
patients with locally advanced gastric cancer. Pharmacogenomics J.
17:36–41. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Matsuyama S, Ohkura Y, Eguchi H, Kobayashi
Y, Akagi K, Uchida K, Nakachi K, Gustafsson JA and Hayashi S:
Estrogen receptor beta is expressed in human stomach
adenocarcinoma. J Cancer Res Clin Oncol. 128:319–324. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Takano N, Iizuka N, Hazama S, Yoshino S,
Tangoku A and Oka M: Expression of estrogen receptor-alpha and
-beta mRNAs in human gastric cancer. Cancer Lett. 176:129–135.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Wang M, Pan JY, Song GR, Chen HB, An LJ
and Qu SX: Altered expression of estrogen receptor alpha and beta
in advanced gastric adenocarcinoma: Correlation with prothymosin
alpha and clinicopathological parameters. Eur J Surg Oncol.
33:195–201. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Ryu WS, Kim JH, Jang YJ, Park SS, Um JW,
Park SH, Kim SJ, Mok YJ and Kim CS: Expression of estrogen
receptors in gastric cancer and their clinical significance. J Surg
Oncol. 106:456–461. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Qin J, Liu M, Ding Q, Ji X, Hao Y, Wu X
and Xiong J: The direct effect of estrogen on cell viability and
apoptosis in human gastric cancer cells. Mol Cell Biochem.
395:99–107. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Zhang BG, Du T, Zang MD, Chang Q, Fan ZY,
Li JF, Yu BQ, Su LP, Li C, Yan C, et al: Androgen receptor promotes
gastric cancer cell migration and invasion via AKT-phosphorylation
dependent upregulation of matrix metalloproteinase 9. Oncotarget.
5:10584–10595. 2014.PubMed/NCBI
|
|
64
|
Wesolowska M, Pawlik P and Jagodzinski PP:
The clinicopathologic significance of estrogen receptors in human
gastric carcinoma. Biomed Pharmacother. 83:314–322. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Zhou J, Teng R, Xu C, Wang Q, Guo J, Xu C,
Li Z, Xie S, Shen J and Wang L: Overexpression of ERα inhibits
proliferation and invasion of MKN28 gastric cancer cells by
suppressing β-catenin. Oncol Rep. 30:1622–1630. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Wang X, Deng H, Zou F, Fu Z, Chen Y, Wang
Z and Liu L: ER-α36-mediated gastric cancer cell proliferation via
the c-Src pathway. Oncol Lett. 6:329–335. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Tang W, Liu R, Yan Y, Pan X, Wang M, Han
X, Ren H and Zhang Z: Expression of estrogen receptors and androgen
receptor and their clinical significance in gastric cancer.
Oncotarget. 8:40765–40777. 2017.PubMed/NCBI
|
|
68
|
Wakui S, Motohashi M, Muto T, Takahashi H,
Hano H, Jutabha P, Anzai N, Wempe MF and Endou H: Sex-associated
difference in estrogen receptor β expression in
N-methyl-N′-nitro-N-nitrosoguanidine-induced gastric cancers in
rats. Comp Med. 61:412–418. 2011.PubMed/NCBI
|
|
69
|
Choung RS and Locke GR III: Epidemiology
of IBS. Gastroenterol Clin North Am. 40:1–10. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Heitkemper M, Jarrett M, Bond EF and Chang
L: Impact of sex and gender on irritable bowel syndrome. Biol Res
Nurs. 5:56–65. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Longstreth GF and Wolde-Tsadik G:
Irritable bowel-type symptoms in HMO examinees. Prevalence,
demographics, and clinical correlates. Dig Dis Sci. 38:1581–1589.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Toner BB and Akman D: Gender role and
irritable bowel syndrome: Literature review and hypothesis. Am J
Gastroenterol. 95:11–16. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Heitkemper MM and Chang L: Do fluctuations
in ovarian hormones affect gastrointestinal symptoms in women with
irritable bowel syndrome? Gender Med. 2 (Suppl 6):152–167. 2009.
View Article : Google Scholar
|
|
74
|
Chaloner A and Greenwood-Van Meerveld B:
Sexually dimorphic effects of unpredictable early life adversity on
visceral pain behavior in a rodent model. J Pain. 14:270–280. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Cao DY, Ji Y, Tang B and Traub RJ:
Estrogen receptor β activation is antinociceptive in a model of
visceral pain in the rat. J Pain. 13:685–694. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Jacenik D, Cygankiewicz AI, Fichna J,
Mokrowiecka A, Malecka-Panas E and Krajewska WM: Estrogen signaling
deregulation related with local immune response modulation in
irritable bowel syndrome. Mol Cell Endocrinol. 471:89–96. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Qin B, Dong L, Guo X, Jiang J, He Y, Wang
X, Li L and Zhao J: Expression of G protein-coupled estrogen
receptor in irritable bowel syndrome and its clinical significance.
Int J Clin Exp Pathol. 7:2238–2246. 2014.PubMed/NCBI
|
|
78
|
Zielinska M, Fichna J, Bashashati M,
Habibi S, Sibaev A, Timmermans JP and Storr M: G protein-coupled
estrogen receptor and estrogen receptor ligands regulate colonic
motility and visceral pain. Neurogastroenterol Motil. 29:2017.
View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Mizoguchi A, Takeuchi T, Himuro H, Okada T
and Mizoguchi E: Genetically engineered mouse models for studying
inflammatory bowel disease. J Pathol. 238:205–219. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Xavier RJ and Podolsky DK: Unravelling the
pathogenesis of inflammatory bowel disease. Nature. 448:427–434.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Molodecky NA, Soon IS, Rabi DM, Ghali WA,
Ferris M, Chernoff G, Benchimol EI, Panaccione R, Ghosh S, Barkema
HW and Kaplan GG: Increasing incidence and prevalence of the
inflammatory bowel diseases with time, based on systematic review.
Gastroenterology. 142:46–54.e42; quiz e30. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Cook LC, Hillhouse AE, Myles MH, Lubahn
DB, Bryda EC, Davis JW and Franklin CL: The role of estrogen
signaling in a mouse model of inflammatory bowel disease: A
Helicobacter hepaticus model. PLoS One. 9:e942092014. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Barzi A, Lenz AM, Labonte MJ and Lenz HJ:
Molecular pathways: Estrogen pathway in colorectal cancer. Clin
Cancer Res. 19:5842–5848. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Principi M, Barone M, Pricci M, De Tullio
N, Losurdo G, Ierardi E and Di Leo A: Ulcerative colitis: From
inflammation to cancer. Do estrogen receptors have a role? World J
Gastroenterol. 20:11496–11504. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Pierdominici M, Maselli A, Varano B,
Barbati C, Cesaro P, Spada C, Zullo A, Lorenzetti R, Rosati M,
Rainaldi G, et al: Linking estrogen receptor β expression with
inflammatory bowel disease activity. Oncotarget. 6:40443–40451.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Armstrong CM, Allred KF, Weeks BR, Chapkin
RS and Allred CD: Estradiol has differential effects on acute
colonic inflammation in the presence and absence of estrogen
receptor β expression. Dig Dis Sci. 62:1977–1984. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Looijer-van Langen M, Hotte N, Dieleman
LA, Albert E, Mulder C and Madsen KL: Estrogen receptor-β signaling
modulates epithelial barrier function. Am J Physiol Gastrointest
Liver Physiol. 300:G621–G626. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Saleiro D, Murillo G, Benya RV,
Bissonnette M, Hart J and Mehta RG: Estrogen receptor-β protects
against colitis-associated neoplasia in mice. Int J Cancer.
131:2553–2561. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Bustos V, Nolan AM, Nijhuis A, Harvey H,
Parker A, Poulsom R, McBryan J, Thomas W, Silver A and Harvey BJ:
GPER mediates differential effects of estrogen on colon cancer cell
proliferation and migration under normoxic and hypoxic conditions.
Oncotarget. 8:84258–84275. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Konstantinopoulos PA, Kominea A, Vandoros
G, Sykiotis GP, Andricopoulos P, Varakis I, Sotiropoulou-Bonikou G
and Papavassiliou AG: Oestrogen receptor beta (ERbeta) is
abundantly expressed in normal colonic mucosa, but declines in
colon adenocarcinoma paralleling the tumour's dedifferentiation.
Eur J Cancer. 39:1251–1258. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Delellis Henderson K, Duan L,
Sullivan-Halley J, Ma H, Clarke CA, Neuhausen SL, Templeman C and
Bernstein L: Menopausal hormone therapy use and risk of invasive
colon cancer: The california teachers study. Am J Epidemiol.
171:415–425. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Manson JE, Chlebowski RT, Stefanick ML,
Aragaki AK, Rossouw JE, Prentice RL, Anderson G, Howard BV, Thomson
CA, LaCroix AZ, et al: Menopausal hormone therapy and health
outcomes during the intervention and extended poststopping phases
of the Women's Health Initiative randomized trials. JAMA.
310:1353–1368. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Design of the Women's Health Initiative
clinical trial and observational study. The Women's Health
Initiative Study Group. Control Clin Trials. 19:61–109. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Calle EE, Miracle-McMahill HL, Thun MJ and
Heath CW Jr: Estrogen replacement therapy and risk of fatal colon
cancer in a prospective cohort of postmenopausal women. J Natl
Cancer Inst. 87:517–523. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Simon MS, Chlebowski RT, Wactawski-Wende
J, Johnson KC, Muskovitz A, Kato I, Young A, Hubbell FA and
Prentice RL: Estrogen plus progestin and colorectal cancer
incidence and mortality. J Clin Oncol. 30:3983–3990. 2012.
View Article : Google Scholar : PubMed/NCBI
|