Introduction
Desmoid-type fibromatosis is a tumor-like
proliferating fibrous tissue disorder, composed of clonal
proliferation of fibroblasts and myofibroblasts (1). It is a rare soft-tissue tumor
originating from connective tissue of the fascia or aponeurosis.
Genetic, endocrine and physical factors, such as pregnancy and
trauma, play an important role in the etiology of the disease
(2). Desmoid-type fibromatosis is
characterized by aggressive growth, high likelihood of relapse and
less frequent distant metastasis (3). The recurrence rate after complete tumor
resection is between 20 and 60%, about 8% of patients die due to
rapid recurrence, and 20 to 30% of patients achieve tumor
stabilization or spontaneous remission (4). The peak incidence of desmoid-type
fibromatosis is from 35–40 years old, whereas for women it is
mainly during the reproductive age (5). Although rare, it is a highly atopic
tumor with unpredictable biological behavior that may occur in any
part of the body (6). According to
its anatomic location, desmoid-type fibromatosis is generally
divided into three types: Abdominal external type (trunk and
limbs), abdominal wall type and intra-abdominal type (7). Due to the variety of location and
clinical symptoms of desmoid-type fibromatosis, it often leads to
difficult diagnosis, and there are many diseases that need to be
differentiated, such as inflammatory lesions, liposarcoma and
fibrosarcoma (8). The most common
complaints of patients are painless progressive growth of the mass,
neurological dysfunction, joint stiffness and abdominal discomfort
due to the tumor growth (9). The
imaging findings of desmoid-type fibromatosis depend on the number
of fibroblasts proliferating in the tumor, as well as the fiber
composition, collagen content and tumor supply (10). Areas of dense fibrous tissue and
scar-like collagen fiber deposition usually show low signal for
T1WI and T2WI, and no enhancement after injection of contrast agent
(11). In areas where tumor cells
are concentrated, there is a moderate to significant enhancement
following the injection of contrast agent, whereas the matrix
portion is weakly enhanced (12).
Certain cases of desmoid-type fibromatosis remain stable following
surgery, while others progress rapidly (13). Therefore, it is important to choose
the appropriate treatment. Currently, treatments for desmoid-type
fibromatosis include surgical tumor resection, radiation therapy,
hormonal therapy, and non-steroidal anti-inflammatory therapy.
Surgery is currently the preferred treatment for desmoid-type
fibromatosis. The incidence of desmoid-type fibromatosis is ~2–4
cases per 1 million, accounting for 0.03% of all tumors (14,15).
Since the cases are rare, the factors that can accurately predict
tumor recurrence have not been confirmed. In the present study,
through the assessment of tissue samples and regression analysis
using the Cox proportional hazards model, factors significantly
affecting the recurrence rate and time of desmoid-type fibromatosis
were identified.
Materials and methods
General patient data
A total of 102 cases of pathologically confirmed
desmoid-type fibromatosis were collected from Jiaxing Traditional
Chinese Medicine Hospital between January 2011 and May 2017. The
cohort comprised of 73 females and 29 males, with mean age of
32.86±12.64 years (range, 6–78 years). The data collected included
clinical data [sex, age, relapse status at the end of the follow-up
(every 3 months) in May 2017 and recurrence time], imaging data
[tumor type, maximum diameter, tumor margin, computed tomography
(CT) enhancement ratio, magnetic resonance (MR) enhancement ratio
and T2 signal ratio] and pathological data (Ki-67 and endoscopic
margin). Among them, 71 cases (21 males and 50 females) experienced
a relapse and 31 cases (8 males and 23 females) had no relapse. A
total of 89 cases had an unexplained mass, 2 had a mass identified
on physical examination, 7 cases were identified after trauma, 23
cases had pain associated with the lesions, 2 cases had joint
deformities, 5 cases had limited joint activity, 5 cases had
abdominal pain and 2 cases had intestinal obstruction. Furthermore,
2 cases were identified during pregnancy, 1 case following surgical
resection of the thyroid carcinoma, 1 case following surgical
resection of endometrial carcinoma, 1 following surgical resection
of ovarian cyst, 2 after appendectomy, 1 after splenectomy and 1
following intestinal polyp removal on colonoscopy. Ethics approval
was obtained from the Medical Ethics Committee of Jiaxing Chinese
Medicine Hospital (no. 2016-JZLK-005). All patients were informed
and provided oral consent to participate.
CT examination
CT scans were performed using a Siemens SOMATOM
Sensation 16-slice spiral CT (Siemens AG) with a layer thickness of
2.5 mm and a layer spacing of 2.5 mm. The 0.625-mm standard
algorithm was used for reconstruction. The coronal plane and
sagittal plane were reconstructed with a layer thickness of 2.0 mm.
Enhanced scanning was performed at 25, 70 and 300 sec,
respectively, after injection of ioversol (300 mg/100 ml; Medtronic
Ltd.) at a rate of 2.5 ml/sec and a dose of 80 ml.
MR imaging (MRI) examination
MRI was performed with a GE Signal 1.5T or 3.0T MRI
scanner (GE Healthcare Life Sciences). TOSOPA phased array coils,
EXTREM surface coils or GPFLEX surface coils were used, depending
on the scan site. The scanning sequences were: T1-weighted imaging
[(T1WI) Repetition time (TR), 360–560 msec; echo time (TE), 9–18
msec]; T2WI (TR, 2,200-3,600 msec; TE, 108–127 msec); proton
density-WI (TR, 2,200-3,600 msec; TE, 11–29 msec); and short time
inversion recovery (TR, 4,500-5,400 msec; TE, 48–53 msec),
including sagittal, coronal and transverse sections, with a layer
thickness of 4.0 mm, layer spacing of 1.0 mm, a field of view of
18×18 cm and a matrix of (160–192) × (200–256). Coronary,
transverse and sagittal T1WI and T1WI fat-suppressed scanning were
performed after injection of Gd-diethylenetriamine penta-acetic
acid (0.2 mmol/kg).
Image data collection methods and
measurement standards
The following parameters were used. The maximum
diameter of the tumor was measured after an enhanced scan. The CT
enhancement ratio was defined as (CT valueenhanced
scan-CT valueplain scan)/CT valueplain
scan. The signal intensity (SI) prior to and after the MR
enhanced scan of the same region of interest (ROI) was measured by
3-dimensional localization. The ROI (away from cystic change,
calcification and fat area) was enhanced in the lesion. The MR
enhancement ratio was defined as (SIenhanced
scan-SIplain scan)/SIplain scan. The SI
of the most enhanced region of the lesion (away from cystic change,
calcification and fat area) and adjacent muscle on the T2WI
fat-suppressed sequence was measured. The T2 signal ratio was
defined as
(SItumor-SImuscle)/SImuscle. Low,
high and iso-density were all relatively defined by CT examination,
when the major parts of the tumor (non-necrotic sites) were
compared with that in the surrounding muscle or other soft tissue.
Lesions were considered as mildly, moderately or significantly
enhanced after CT enhanced scan when the CT values of the lesions
were increased by 0–20, 21–40 or >40 Hounsfield unit (HU),
respectively. The MR signal level was the signal within the tumor
relative to the surrounding muscle. Tumor recurrence was defined as
the original pathologically confirmed desmoid-type fibromatosis
relapsing after surgery, confirmed by imaging and pathology. A new
tumor was defined as the first appearance of desmoid-type
fibromatosis. Recurrence-free survival was defined as the absence
of recurrence from the time the lesion was surgically removed to
the end of follow-up. The recurrence time was the time between the
surgery and the time-point when a recurrent tumor was identified by
the patient. All the measurements were performed by two experienced
radiologists who had no prior knowledge of the relapse status of
the patients, and the results were subsequently analyzed.
Histopathological analysis
All the tissues were fixed with 3.7% neutral
buffered formalin, routinely dehydrated, embedded in paraffin and
serially sectioned. Cells positive for the Ki-67 protein were
observed by immunohistochemical staining. The 3-µm-thick sections
were blocked with 3% hydrogen peroxide at room temperature for 6
min. The primary antibody (MyoD1; ready-to-use, no dilution; clone
number: EP212; Beijing Zhongshang Jinqiao Biotechnology Co., Ltd.)
was incubated overnight at 4°C. The secondary antibody (Envision
Immunochromogenic Reagent; ready-to-use, no dilution; cat. no.
K-5007; Zhejiang Medical Biotechnology Co., Ltd.) was incubated for
30 min at room temperature and developed for 5 min. Positivity for
Ki-67 was confirmed by the presence of brown stained nuclei. A DP70
Digital Camera (Olympus Corp.) image acquisition system was used to
select 2–5 high-power fields of view (magnification, ×200) to
capture images. The number of Ki-67 positive tumor cells and the
total number of tumor cells were counted using the Image-pro Plus
image analysis software (v6.0; Media Cybernetics Inc.). The Ki-67
positive index was calculated as: (number of Ki-67 positive tumor
cells/total number of tumor cells) ×100%.
Statistical analysis
SPSS (v19.0; IBM Corp.) was used for all statistical
analyses. The Kaplan-Meier method and log-rank test were used for
univariate analysis to identify significantly associated
indicators. By using the Cox proportional hazard regression model,
stepwise regression analysis was used to determine the independent
risk factors of recurrence time, while the hazard ratio and 95%
confidence interval were also calculated. All values were expressed
as the mean ± standard error of the mean.
Results
Recurrence time and rate
Of the 102 patients, 71 exhibited local recurrence
(70%) with a recurrence time of 20.59±23.98 months (range, 3–123
months), including 21 males for whom the recurrence time was
23.04±23.48 months (range, 3–73 months) and 50 females with a
recurrence time of 19.53±24.69 months (range, 4–123 months). The
overall 1-year recurrence rate was 31% and the 2-year recurrence
rate was 54%. The median age at recurrence was 29 years. In all
cases of relapse, the recurrence occurred in situ.
Clinicopathological data
A total of 67 lesions were located outside of the
abdomen, of which 27 lesions were located in the limbs (6 in the
upper limbs and 21 in the lower limbs), 25 in the joint girdle (13
in the shoulder girdle and 12 in the pelvic girdle), 12 in the
trunk (4 cases in the chest wall and 8 cases in the back) and 3 in
the head and neck. A total of 28 lesions were located in the
abdominal wall, including 19 lesions in anterior lower abdominal
wall. Furthermore, 7 lesions were located inside of the abdomen,
including 3 cases in the mesentery of the small intestine, 1 case
in the small intestine, 1 case in the ileocecal region and 2 cases
in the anterior bladder. Relapse of desmoid-type fibromatosis
occurred in 71 cases (70%). The follow-up time was 30.53±22.57
months (range, 24–123 months). The tumor size was 7.71±3.59 cm
(range, 1.6–19.0 cm). The tumor margin was clear in 29 cases and
unclear in 73 cases visually. Of the 19 cases that were positive
for desmoid-type fibromatosis in the margin, based on histology
with hemotoxylin and eosin (H&E) staining, 16 cases relapsed.
Of the 83 cases that were negative on histology with H&E
staining, 55 cases relapsed. A total of 87 cases of hard-textured
lesions and 15 cases of medium-grade lesions were encountered. A
total of 35 lesions invaded the peripheral vessels. Envelopes on
the lesions were seen in 1 case. In 19 cases, pathologically
positive margins of desmoid-type fibromatosis were observed. On
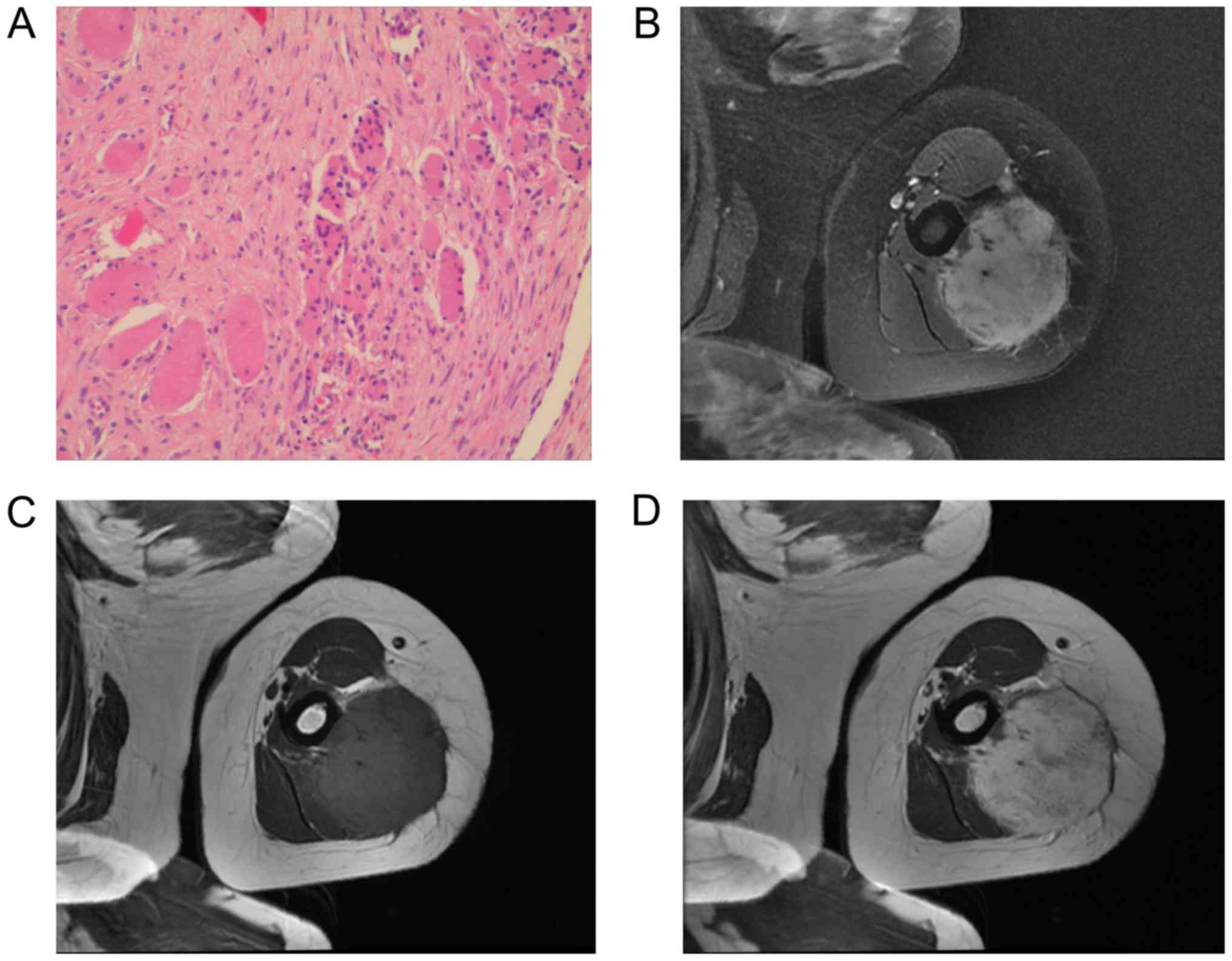
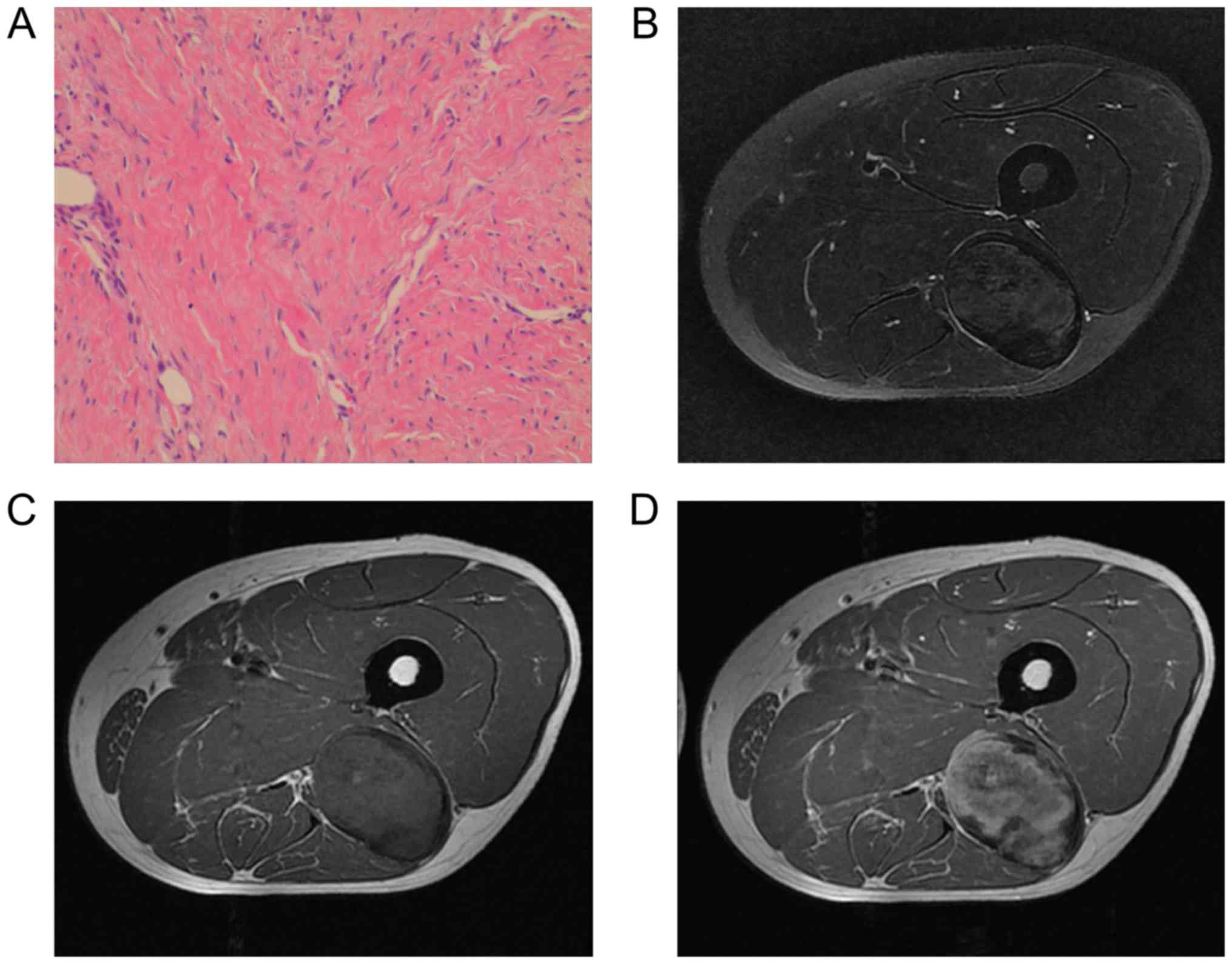
microscopy, the sections exhibited a bundle of spindle-shaped cells
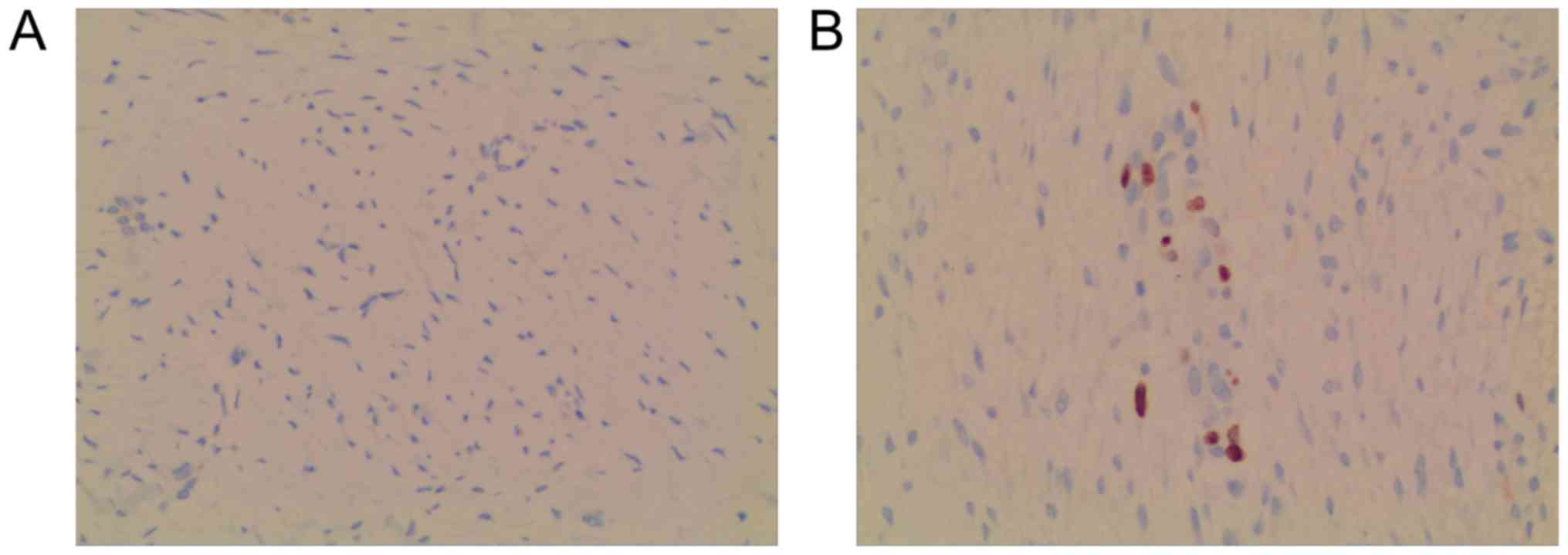
with uniform nuclei and clear nucleoli (Figs. 1A and 2A). A total of 60 cases had positive
staining for Ki-67, with the positive index ranging between 1 and
20%. Representative images for Ki-67 staining are presented in
Fig. 3.
Imaging data
The minimum size of the tumors was 1.3×2.1×2.0 cm
and the maximum size was 15×14×8 cm. The lesions included
calcification in 8 cases, cystic degeneration in 3 cases, fat in 1
case, peripheral nerve and vessel invasion in 35 cases, bone
destruction in 17 cases and ascites in 1 case. Lesions displayed
using CT had a lower density compared with that of the muscles. The
CT value ranged between 33 and 47 HU, and the mean CT value was
39.0±2.0 HU. The CT enhanced scan exhibited mild enhancement in 11
cases, moderate enhancement in 69 cases and marked enhancement in
22 cases. With MRI, the SI of the lesions on the T2WI
fat-suppressed sequence was higher (Fig.
1B) or slightly higher (Fig. 2B)
compared with that of the surrounding muscle. The SI of the lesions
on T1WI was equal to or lower compared with that of the surrounding
muscle, and the SI was at times uneven with a clear or blurred
margin (Figs. 1C and 2C). The lesions exhibited a marked and
non-uniform enhancement in the arterial phase of the enhanced scan
(Figs. 1D and 2D), which was higher compared with that of
the surrounding muscle. The lesions continued to intensify in the
delayed phase and were still partially enhanced until 600 sec
later. The area of low SI on T1WI and the T2WI fat-suppressed
sequence corresponded to the higher collagen content. Of the 102
cases, 25 of the lesions were uniformly enhanced (24.5%).
Measurement indices
The maximum diameter of the tumors was 7.71±3.59 cm
(range, 2–19 cm) and the CT enhancement ratio was 0.78±0.38 (range,
0.18–1.88). Furthermore, the T2 signal ratio was 2.32±1.42 (range,
0.13–5.05) and the MR enhancement ratio was 1.17±0.77
(0.14–4.62).
Univariate analysis
Kaplan-Meier survival analysis was used to analyze
10 variables to investigate recurrence time (Table I). The differences between 1-year and
2-year postoperative tumor-free survival rates were analyzed by the
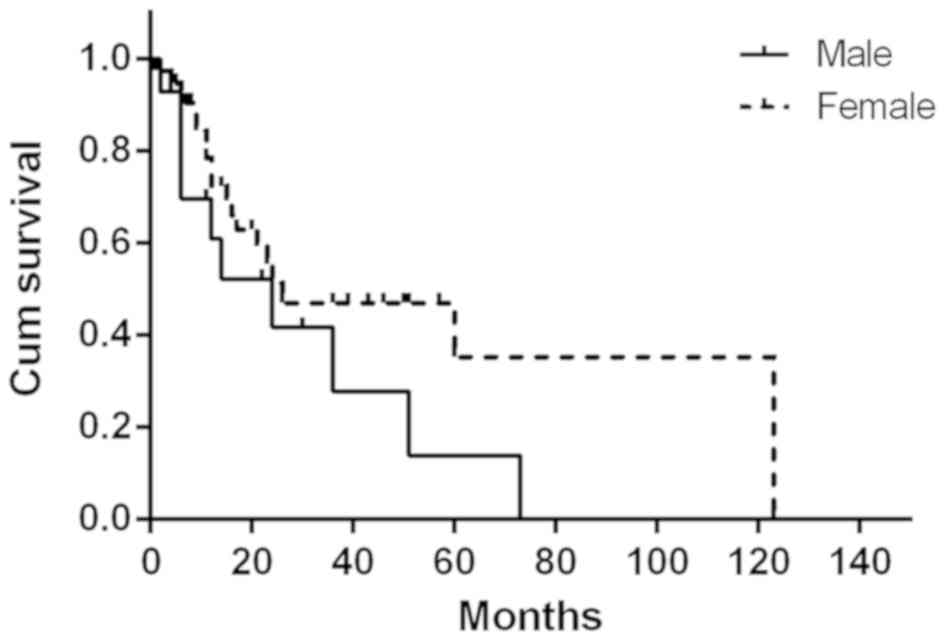
log-rank test. The results revealed that sex (P=0.038), tumor
diameter (P=0.005), CT enhancement ratio (P=0.016) and Ki-67 status
(P<0.001) had a significant effect on the recurrence time
(Table II).
 | Table I.Influencing factors on the recurrence
rate of desmoid-type fibromatosis. |
Table I.
Influencing factors on the recurrence
rate of desmoid-type fibromatosis.
|
| Score |
|---|
|
|
|
|---|
| Variables | 1 | 2 | 3 |
|---|
| Sex | Male | Female |
|
| Age, years | <20 | 20–40 | >40 |
| Tumor location | Abdominal
external | Abdominal wall | Intra-abdominal |
| Maximum tumor
diameter, cm | <5 | 5–9 | >9 |
| Border | Clear | Unclear |
|
| CT enhancement
ratio | <0.6 | 0.6–0.9 | >0.9 |
| MR enhancement
ratio | <0.8 | 0.8–1.5 | >1.5 |
| T2 signal ratio | <1.8 | 1.8–2.5 | >2.5 |
| Ki-67 | Negative | Positive |
|
| Pathological
margin | Negative | Positive |
|
 | Table II.Univariate analysis of each variable
on recurrence time. |
Table II.
Univariate analysis of each variable
on recurrence time.
|
|
| Postoperative
tumor-free survival rate, % |
|
|---|
|
|
|
|
|
|---|
| Variables | Number | 1-year | 2-year | P-value |
|---|
| Sex |
|
|
| 0.038 |
|
Male | 29 | 57 | 43 |
|
|
Female | 73 | 73 | 49 |
|
| Age, years |
|
|
| 0.208 |
|
<20 | 15 | 71 | 57 |
|
|
20–40 | 62 | 64 | 42 |
|
|
>40 | 25 | 82 | 55 |
|
| Types |
|
|
| 0.159 |
|
Abdominal external | 67 | 64 | 24 |
|
|
Abdominal wall | 28 | 46 | 38 |
|
|
Intra-abdominal | 7 | 86 | 71 |
|
| Maximum diameter,
cm |
|
|
| 0.005a |
|
<5 | 24 | 75 | 50 |
|
|
5–9 | 49 | 68 | 56 |
|
|
>9 | 29 | 64 | 29 |
|
| Border |
|
|
| 0.591 |
|
Clear | 29 | 64 | 50 |
|
|
Unclear | 73 | 70 | 46 |
|
| CT enhancement
ratio |
|
|
| 0.016a |
|
<0.6 | 27 | 65 | 50 |
|
|
0.6–0.9 | 37 | 56 | 39 |
|
|
>0.9 | 38 | 84 | 53 |
|
| MR enhancement
ratio |
|
|
| 0.759 |
|
<0.8 | 29 | 79 | 64 |
|
|
0.8–1.50 | 42 | 62 | 43 |
|
|
>1.50 | 31 | 69 | 38 |
|
| T2 signal
ratio |
|
|
| 0.073 |
|
<1.8 | 32 | 87 | 69 |
|
|
1.8–2.50 | 36 | 50 | 33 |
|
|
>2.50 | 34 | 71 | 41 |
|
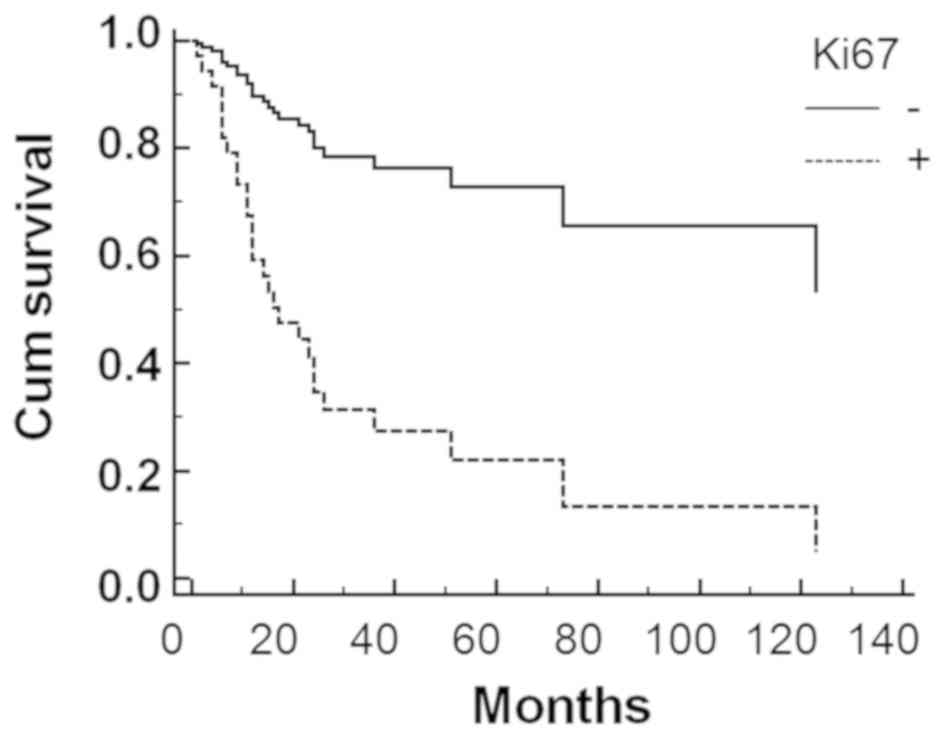
| Ki67 |
|
|
| <0.001a |
|
Negative | 42 | 79 | 74 |
|
|
Positive | 60 | 63 | 31 |
|
| Pathological
margin |
|
|
| 0.068 |
|
Negative | 83 | 71 | 52 |
|
|
Positive | 19 | 44 | 11 |
|
Multivariate analysis
The 10 variables (Table
I) were analyzed using the multivariate Cox regression model,
and the stepwise regression method to eliminate the mutual
influence among the various factors to obtain four independently
associated variables with recurrence (Table III). These four variables were sex,
maximum diameter, Ki-67 status and T2 signal ratio.
 | Table III.Data from multivariate Cox
proportional hazard regression model. |
Table III.
Data from multivariate Cox
proportional hazard regression model.
| Variables | HR (95% CI) | P-value |
|---|
| Sex | 0.424
(0.203–0.938) | 0.032 |
| Maximum tumor
diameter | 1.100
(1.001–1.218) | 0.045 |
| T2 signal
ratio | 1.268
(0.993–1.560) | 0.044 |
| Ki-67 | 1.084
(1.003–1.139) | 0.001 |
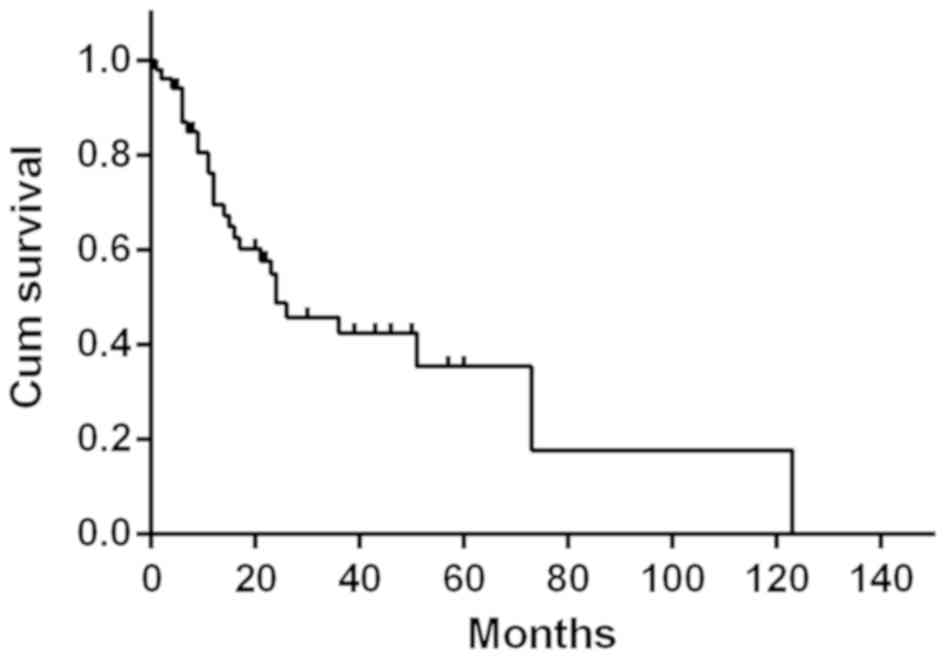
Recurrence-free survival
The Kaplan-Meier curve for cumulative
recurrence-free survival time within the study population is
presented in Fig. 4. The number of
recurrence-free patients decreased over time. At the median of 35
months, 50% of the patients had relapsed. As males had a higher
risk of recurrence compared with that in females (P=0.032),
recurrence-free survival was stratified by sex (Fig. 5). Furthermore, the recurrence-free
survival curves for patients with Ki-67-positive and -negative
lesions are presented in Fig. 6. At
the same time-points on the horizontal axis, the number of
Ki-67-positive cases without recurrence was significantly lower
compared with that in the Ki-67-negative cases (P=0.001).
Discussion
Desmoid-type fibromatosis is also known as invasive
fibromatosis. Under normal physiological conditions, fibroblasts
have a crucial role in wound healing and protecting vital organs,
including the lung, liver, blood vessels, heart and kidney, but
when certain cells undergo gene mutations, neoplasms may be formed,
leading to the occurrence of desmoid-type fibromatosis (16,17).
With an incidence rate of approximately five per million people
annually, it is uncommon, representing approximately 0.3 per cent
of all soft tissue neoplasms (18,19).
While the exact causes remain elusive, desmoid-type fibromatosis is
currently considered to be associated with surgical history,
traumatic injury, familial adenomatous polyposis and Gardner's
syndrome (10). Women were more
likely to develop the disease compared with men (20), and therefore, estrogen is an
influencing factor. The most common sign is a painless, progressive
mass, but symptoms/complaints including neurological disorders,
joint stiffness or abdominal discomfort due to tumor growth may
also occur (9). Desmoid-type
fibromatosis is likely to recur after surgery. Despite complete
resection of the tumor, the recurrence rate remains 20–60%
(21). The overall recurrence rate
in the present study was 70%, which is higher than that reported by
previous studies (3,22–24).
Whether gender affects the recurrence of desmoid-type fibromatosis
is also controversial. A study by Wang et al (25) indicated that sex and recurrence of
desmoid-type fibromatosis had no significant association. In the
present study the overall incidence in females (73/102; 71.6%) was
higher than that in males (29/102; 28.4%), but the two-year
recurrence rate was higher in males (57%) compared with that in
females (51%), and male gender was a significant risk factor for
recurrence. Multivariate analysis also revealed that sex was a
major influencing factor of tumor recurrence. Female patients had a
0.424-fold risk of recurrence compared with that for male patients.
Analysis of the reasons suggested that this may be due to hormone
levels. This may also be associated with each patient's individual
genetic mutations, and genetic studies with this regard are
therefore desirable. It has also been reported that age may be a
prognostic factor (26). However, in
the present study, the patient age had no effect on the
prognosis.
The present study indicated that the maximum
diameter of the tumor affected postoperative recurrence. A larger
primary tumor in size was significantly associated with a higher
probability of recurrence and a shorter recurrence time.
Furthermore, larger lesions tended to invade the surrounding
vessels and nerves, therefore the lesion was not completely removed
during surgery to preserve the local tissue function, and some
tumor cells remained in the surrounding tissue, leading to
short-term recurrence. Multivariate analysis revealed the CT
enhancement and the MR enhancement ratios were not significantly
associated with postoperative tumor recurrence. The imaging
findings of desmoid-type fibromatosis were dependent on the number
of proliferating fibroblasts in the tumor as well as the fibrous,
collagen and vascular components (11). The CT value mainly reflects the
difference in tissue density. Differences in the CT values of the
fibrous, collagen and vascular components within the tumor were
small, as all of them are soft tissues. The difference in the
increase of CT values after the enhanced scan was small and not
sufficient to reflect the difference between these tissues. On
plain scanning, it was difficult to display the exact border of the
desmoid-type fibromatosis, but on the CT enhancement scan, the
border was clearly visible. Although the MR enhancement ratio had
no effect on postoperative tumor recurrence, an MR enhanced scan is
important, as it may help determine the size of the tumor, tumor
composition and infiltration of the surrounding tissue, as well as
to identify the presence of a tumor envelope and edema around the
tumor, the observation and comprehensive evaluation of which is
important for the surgical treatment and prognostication of the
patient. On T2WI, the SI of desmoid-type fibromatosis was higher
compared with that of the surrounding muscle, whereas on T1WI, the
SI was equal to or lower compared with that of the surrounding
muscle. The lesions exhibited invasive growth with unclear margins.
The internal lesion with low SI (lower compared with that of the
muscle) was unevenly enhanced, while the remainder of the lesion
was consistently enhanced. Different modes of MR help distinguish
the internal tissue components of the tumor. The area of
band-shaped low SI on T1WI was usually not enhanced on the T1WI
enhanced scan, corresponding to the dense fibrous tissue and
scar-like collagen deposition area, and the results were similar to
those studied by Xu et al (12). After injection of the contrast agent,
the lesion was moderately to markedly enhanced, particularly in the
concentration area of the tumor cells, while the stromal area
exhibited mild enhancement and the results were similar to those
studied by Kim et al (27).
The T2WI SI was associated with the number of tumor cells in the
collagen matrix (27). A stronger
T2WI SI was associated with a higher cell proliferation and a
shorter time to tumor recurrence (27). The results from the present study
suggested that the T2 signal ratio was a risk factor affecting
recurrence time. An increase of the T2 signal ratio was
significantly associated with an increase in the risk of
recurrence.
It is controversial whether the pathological margin
of desmoid-type fibromatosis has any effect on recurrence. A
multidisciplinary research institute in France (15) retrospectively analyzed and
demonstrated that an infiltrated margin, including tumor cells of
desmoid-type fibromatosis, had no significant effect on the
prognosis of patients. However, Wang et al (25) reported that invasion of major vessels
and nerves and invasion of the surgical margin were risk factors
for postoperative recurrence. In the present study, univariate and
multivariate analyses indicated no association between the
pathological margin and tumor recurrence. This may be due to the
small number of samples. Ki-67 is a proliferating cell-associated
nuclear antigen that is a marker for cell proliferation (26). The present study demonstrated that
Ki-67 is a key factor influencing tumor recurrence time. Patients
with positive Ki-67 are more likely to relapse.
The causes of recurrence of desmoid-type
fibromatosis are complex and diverse and may be affected by
numerous factors. A number of imaging findings that may affect the
recurrence were assessed in the present study, which revealed that
sex, maximum tumor diameter, T2 signal ratio and Ki-67 were
independent risk factors using the Cox proportional hazard
regression analysis; sex and Ki-67 status were not associated with
imaging. Therefore, when imaging findings are used to predict the
recurrence of desmoid-type fibromatosis, clinical and pathological
indicators must be combined.
While having identified several factors that affect
postoperative recurrence, it must be noted that the present study
had certain limitations. Due to the different locations of the
tumors, it was not possible to measure the SI in the same muscle.
Only the corresponding SI around the lesion was selected as a
reference. Furthermore, as the size of the lesions was
inconsistent, it was not possible to uniformly determine the ROI,
which may have affected the present results. In addition, as the
present study was retrospective, patients were lost to follow-up
and/or their clinical data were incomplete.
At present, MRI is the preferred method for the
preoperative evaluation of tumors and postoperative detection of
recurrence. Based on the results of the present study, an objective
assessment of postoperative recurrence of desmoid-type fibromatosis
may be made based on the imaging findings. The sex of the patients,
tumor diameter, Ki-67 expression status and T2 signal ratio were
identified to affect postoperative recurrence. The T2 signal ratio
and the maximum diameter of the tumor were the most significant
indicators of post-operative recurrence. Long-term follow-up after
surgery is necessary. Clinical and imaging examination should be
performed every 3–6 months for 2–3 years prior to annual follow-up.
For high-risk cases with a Ki-67-positive status or a high T2
signal ratio, close follow-up with short intervals is required.
Acknowledgements
Not applicable.
Funding
The present study was supported in part by Zhejiang
Provincial Natural Science Foundation of China (grant. no.
LQ19H220001).
Availability of data and material
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
Study design, data collection, statistical analysis,
data interpretation, manuscript preparation and literature search
was performed by JW. Statistical analysis, data interpretation,
manuscript preparation, manuscript revision and the literature
search were performed by YH. Data collection, statistical analysis,
data interpretation, literature search and manuscript revision were
performed by YS. Statistical analysis, data interpretation and the
literature search were performed by YG. Study design, statistical
analysis and data interpretation were performed by MZ. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
All procedures performed in studies involving human
participants were in accordance with the ethical standards of the
institutional and/or national research committee and with the 1964
Helsinki declaration and its later amendments or comparable ethical
standards. Ethics approval was obtained from the Medical Ethics
Committee of Jiaxing Chinese Medicine Hospital (no.
2016-JZLK-005).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Fletcher CDM: WHO classification of
tumours of soft tissue and bone/[M]//WHO classification of tumours
of soft tissue and bone. IARC Press; pp. 95–104. 2013
|
|
2
|
Teixeira LE, Arantes EC, Villela RF,
Soares CB, Costa RB and Andrade MA: Extra-abdominal desmoid tumor:
Tocal recurrence and treatment options. Acta Ortop Bras.
24:147–150. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kuhnen C, Helwing M, Rabstein S, Homann HH
and Müller KM: Desmoid-type fibromatosis (aggressive fibromatosis).
Pathologe. 26:117–126. 2005.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
4
|
de Bree E, Keus R, Melissas J, Tsiftsis D
and van Coevorden F: Desmoid tumors: Need for an individualized
approach. Expert Rev Anticancer Ther. 9:525–535. 2014. View Article : Google Scholar
|
|
5
|
Penel N, Coindre JM, Bonvalot S, Italiano
A, Neuville A, Le Cesne A, Terrier P, Ray-Coquard I, Ranchere-Vince
D, Robin YM, et al: Management of desmoid tumours: A nationwide
survey of labelled reference centre networks in France. Eur J
Cancer. 58:90–96. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gronchi A, Colombo C, Le Péchoux C, Dei
Tos AP, Le Cesne A, Marrari A, Penel N, Grignani G, Blay JY, Casali
PG, et al: Sporadic desmoid-type fibromatosis: A stepwise approach
to a non-metastasising neoplasm-a position paper from the Italian
and the French Sarcoma Group. Ann Oncol. 25:578–583. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sugrue JJ, Cohen SB, Marshall RM and Riker
AI: Palliative resection of a giant mesenteric desmoid tumor.
Ochsner J. 15:468–472. 2015.PubMed/NCBI
|
|
8
|
Chaudhary P: Mesenteric fibromatosis. Int
J Colorectal Dis. 29:1445–1451. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jenayah AA, Bettaieb H, Saoudi S, Gharsa
A, Sfar E, Boudaya F and Chelli D; Desmoid tumors, : Clinical
features and treatment options: A case report and a review of
literature'. Pan Afr Med J. 21:932015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Weschenfelder W, Lindner R, Spiegel C,
Hofmann GO and Vogt M: Desmoid tumor of the popliteal fossa during
pregnancy. Case Rep Surg. 2015:2626542015.PubMed/NCBI
|
|
11
|
Kim YW, Choi SJ, Jeon UB and Choo KS:
Retroperitoneal fibromatosis presenting as a presacral mass. Acta
Radiol Short Rep. 3:20479816145237602014.PubMed/NCBI
|
|
12
|
Xu H, Koo HJ, Lim S, Lee JW, Lee HN, Kim
DK, Song JS and Kim MY: Desmoid-type fibromatosis of the thorax:
CT, MRI, and FDG PET characteristics in a large series from a
tertiary referral center. Medicine (Baltimore). 94:e15472015.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fiore M, Rimareix F, Mariani L, Domont J,
Collini P, Le Péchoux C, Casali PG, Le Cesne A, Gronchi A and
Bonvalot S: Desmoid-type fibromatosis: A front-line conservative
approach to select patients for surgical treatment. Ann Surg Oncol.
16:2587–2593. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Basha MS, Dutt SC, Murthy SN and Syed G:
Juvenile fibromatosis of the temporomandibular joint: A rare case
report. Dent Res J (Isfahan). 11:284–287. 2014.PubMed/NCBI
|
|
15
|
Salas S, Dufresne A, Bui B, Blay JY,
Terrier P, Ranchere-Vince D, Bonvalot S, Stoeckle E, Guillou L, Le
Cesne A, et al: Prognostic factors influencing progression-free
survival determined from a series of sporadic desmoid tumors: A
wait-and-see policy according to tumor presentation. J Clin Oncol.
29:3553–3558. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Efthimiopoulos GA, Chatzifotiou D,
Drogouti M and Zafiriou G: Primary asymptomatic desmoid tumor of
the mesentery. Am J Case Rep. 16:160–163. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ali R, Parthiban N and O'Dwyer T: Desmoid
fibromatosis of submandibular region. J Surg Tech Case Rep.
6:21–25. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Reitamo JJ, Häyry P, Nykyri E and Saxén E:
The desmoid tumor. I. Incidence, sex-, age- and anatomical
distribution in the Finnish population. Am J Clin Pathol.
77:665–673. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
van Broekhoven DL, Grünhagen DJ, den
Bakker MA, van Dalen T and Verhoef C: Time trends in the incidence
and treatment of extra-abdominal and abdominal aggressive
fibromatosis: A population-based study. Ann Surg Oncol.
22:2817–2823. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Bn A, Cd JK, Ps S, M M and Urs R: Giant
aggressive mesenteric fibromatosis-a case report. J Clin Diagn Res.
9:PD07–PD08. 2015.PubMed/NCBI
|
|
21
|
Briand S, Barbier O, Biau D,
Bertrand-Vasseur A, Larousserie F, Anract P and Gouin F:
Wait-and-see policy as a first-line management for extra-abdominal
desmoid tumors. J Bone Joint Surg Am. 96:631–638. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Cates JM: Pregnancy does not increase the
local recurrence rate after surgical resection of desmoid-type
fibromatosis. Int J Clin Oncol. 20:617–622. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cates JM, Stricker TP, Sturgeon D and
Coffin CM: Desmoid-type fibromatosis-associated Gardner fibromas:
Prevalence and impact on local recurrence. Cancer Lett.
353:176–181. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Yang JL, Wang J, Zhou XY, Li XQ, Hou YY
and Zhu XZ: Clinicopathologic and genetic studies of desmoid-type
fibromatosis. Zhonghua Bing Li Xue Za Zhi. 35:145–150. 2006.(In
Chinese). PubMed/NCBI
|
|
25
|
Wang YF, Guo W, Sun KK, Yang RL, Tang XD,
Ji T and Tang S: Postoperative recurrence of desmoid tumors:
Clinical and pathological perspectives. World J Surg Oncol.
13:262015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Prodinger PM, Rechl H, Keller M, Pilge H,
Salzmann M, von Eisenhart-Rothe R and Holzapfel BM: Surgical
resection and radiation therapy of desmoid tumours of the
extremities: Results of a supra-regional tumour centre. Int Orthop.
37:1987–1993. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kim SJ, Ha DH, Lee SM and Kang H: Desmoid
type fibromatosis in the facet joint of lumbar spine: Case report
and review of literature. Korean J Radiol. 14:818–822. 2013.
View Article : Google Scholar : PubMed/NCBI
|