Introduction
Having a high incidence worldwide (1), lung adenocarcinoma brain metastasis is
one of the most common distant metastases. The occurrence of brain
metastasis is an important cause of treatment failure and death in
patients (2). Patients with lung
adenocarcinoma brain metastasis have poor prognoses. The median
survival time of untreated patients with brain metastasis is 1 to 2
months, with only ~6 months in treated patients (3). In recent years, radiotherapy technology
has been developed at a high speed, and systemic treatment has
become increasingly standardized. In particular, small molecule
targeted drugs and chemotherapeutic drugs are widely used in
clinical practice. Therefore, the prognoses of patients with lung
adenocarcinoma brain metastasis have greatly improved (4,5).
Studies have shown that, compared with simple
radiotherapy, targeted or chemotherapeutic drug treatment combined
with radiotherapy can have a better synergistic effect and improve
the control rate of brain metastasis, prolonging the survival time
of patients (6). Having prolonged the
survival time of patients with lung cancer brain metastasis to a
certain degree, the comprehensive application of treatment methods
has significantly improved their quality of life (7). In recent years, extensive attention has
been paid by researchers and scholars to stereotactic radiotherapy,
especially gamma knife radiotherapy that is minimally invasive and
highly integrated, which can avoid the expansion of radiation
damage (8). Related studies have
proven that (9–11) gamma knife has better efficacy and
longer survival time in the treatment of lung cancer brain
metastasis tumor than conventional whole brain radiotherapy.
Pemetrexed is the first-line medication for lung adenocarcinoma
brain metastasis chemotherapy (12).
As a new generation of folic acid antagonist, it blocks thymidylate
synthase (TS), glycinamide nucleotide transferase (GARFT) and
dihydrofolate reductase (DH-FR), further affecting the DNA and RNA
syntheses of tumor cells, so as to inhibit their growth and treat
tumors (13).
Clinical practice has shown that the expression
level of tumor serum markers in vivo is important for the
diagnosis and efficacy judgment of lung adenocarcinoma tumors
(14). The comprehensive detection of
multiple tumor markers can improve the accuracy rate of lung cancer
diagnosis (15). Related studies have
shown that the use of multiple lung adenocarcinoma tumor markers
for detection can improve the early diagnostic rate of lung cancer
patients, providing reliable data support for subsequent efficacy
judgment and treatment (16). In this
study, cytokeratin fragment antigen 21-1 (CYFRA21-1) and
carcinoembryonic antigen (CEA) were selected as markers of lung
adenocarcinoma brain metastasis. CEA was first discovered in colon
cancer. Subsequent studies have shown that it is highly expressed
in epithelial-derived tumors such as lung cancer and esophagus
cancer (17). It also plays a very
important role in tumor growth and metastasis (18). CYFRA21-1, an acidic protein that
constitutes cells, is mainly found in patients with lung cancer and
breast cancer. Rare in normal subjects, it is mainly released from
the cancerous epithelium and then enters blood circulation
(19). A large number of studies have
shown that, as the most valuable serum tumor marker in patients
with lung cancer brain metastasis, CYFRA21-1 has higher clinical
value in the diagnosis, disease monitoring and efficacy judgment of
non-small cell lung cancer (20).
The efficacy of pemetrexed combined with
stereotactic gamma-ray radiotherapy in the treatment of 67 patients
with lung adenocarcinoma brain metastasis was compared with that of
simple gamma knife radiotherapy in the traetment of 53 patients, to
investigate the clinical significance and safety of pemetrexed
combined with radiotherapy in the treatment of lung adenocarcinoma
brain metastasis.
Patients and methods
Research subjects
A retrospective analysis method was used to analyze
the cases of 67 patients with lung adenocarcinoma brain metastasis,
who were treated with pemetrexed combined with radiotherapy in The
First People's Hospital of Yunnan Province (Kunming, China) from
May 2013 to December 2015. They were used as experimental group,
including 36 males and 31 females, aged 32–78 years, with an
average age of 57.48±16.12 years, a follow-up time of 1–24 months
and an average follow-up time of 15.1±6.24 months. At the same
time, 53 patients (control group) with lung adenocarcinoma brain
metastasis treated with simple gamma knife radiotherapy were
selected, including 30 males and 23 females, aged 30–76 years, with
an average age of 55.73±15.83 years and an average follow-up time
of 14.8±6.12 months.
Inclusion criteria: i) patients diagnosed with lung
adenocarcinoma brain metastasis by pathology, and with
adenocarcinoma by pathological examination of brain metastasis or
primary lesions; ii) patients with normal electrocardiogram, urine
routine, liver and kidney function, coagulation function, blood
pressure and blood routine before treatment; iii) patients with no
history of operation and trauma within 4 weeks; iv) patients with
no hemoptysis, epistaxis or other kind of bleeding; v) patients
with no severe vascular invasion observed in imaging examination
results; and vi) patients with survival time estimated to be ≥3
months.
Exclusion criteria: i) patients who refused
operation or who could not have operation; ii) patients with other
cancers; iii) patients with liver dysfunction; iv) those with
autoimmune system defects; v) long-term smokers; vi) pregnant or
lactating women; and vii) patients receiving any other anti-tumor
treatment than brain metastasis radiotherapy during treatment.
The study was approved by the Ethics Committee of
The First People's Hospital of Yunnan Province. Patients who
participated in this research, signed an informed consent.
Experimental methods
Treatment plan
Control group: gamma knife was used in the
treatment. Local anesthesia was performed on the patients prior to
the installation of Leksell stereotactic stent (Elekta Instrument
AB, Stockholm, Sweden). A 1.5-T magnetic resonance imaging (MRI)
system (MAGNETOM Avanto; Siemens AG, Munich, Germany) was used to
perform non-interval and enhanced scans on the thin layer (3 mm) of
the lesion area. The obtained high-resolution image was transmitted
to the treatment planning system (TPS) in a private network for
three-dimensional image reconstruction display and stereoscopic
positioning of the target area. The tumor was encased with a 50%
isodose curve, with a peripheral dose of 22–26 Gy and an average of
18.5 Gy for treatment, and the stereotactic frame was removed after
the treatment. Experimental group: A total of 500 mg/m2
pemetrexed (SFDA approval no. H20080177, 500 mg/branch; Nanjing
Pharmaceutical Co., Ltd., Nanjing, China) was added to 100 ml of
saline for dissolution. After pemetrexed treatment given for 2
cycles, stereotactic gamma-ray radiation system (OUR New Med.,
Shenzhen, China) was used. In order to minimize the difference
between source skin distance and source tumor distance, CT scans
were performed in the prone or supine position. The image was input
to the WBS-TPS workstation to confirm the clinical target volume
and adjust the exposure field. According to the size of the
lesions, 50–70% isodose curve was used to enclose the clinical
target area. The optimization was conducted according to the
probability of complications and tumor control in normal tissues.
The isodose curve was 60–70% for wrapping, the peripheral dose was
5–7 Gy/time, and the total dose was 40–56 Gy. The operation was the
same as gamma knife treatment in control group. Pemetrexed
chemotherapy for 2 cycles was performed after radiotherapy.
Altogether 21 days were considered to be 1 treatment
cycle for both groups. The two groups of patients received
symptomatic supportive treatments such as glucocorticoids and
mannitol dehydration, intracranial pressure before and after gamma
knife treatment. Experimental group was given folic acid (SFDA
approval no. H32023302, 400 µg/tablet; Changzhou Pharmaceutical
Factory Co., Ltd., Changzhou, China) on the 7th day before
chemotherapy, 400 µg/time, orally administered once/day, until the
21st day after chemotherapy. Vitamin B12 (SFDA approval no.
H32021841, 500 µg/branch; Jinling Pharmaceutical Co., Ltd.,
Nanjing, China) was supplemented 1,000 µg/time, intramuscularly
injected, with injection once every 4 chemotherapy cycles.
Dexamethasone acetate tablet (SFDA approval no. H22023498, 0.75
mg/tablet; Changchun Dirui Pharmaceutical Co., Ltd., Changchun,
China) was orally administered once daily, 7.5 mg/time before the
1st day of pemetrexed, on the day and on the 2nd day of medication.
Blood routine, liver and kidney function and electrolyte
examinations were required weekly during treatment. The clinical
efficacy and adverse reactions in the pemetrexed combined with
radiotherapy group and simple gamma knife group were observed and
recorded.
CEA and CYFRA21-1 determination
In the morning, 3 ml of fasting venous blood were
collected from all subjects with a vacuum blood lancet, before and
after treatment, and were placed in a centrifuge. Centrifugation
was performed at 3,000 × g for 15 min at 4°C. The slurry in the
test tube was then carefully aspirated to obtain serum. The
instruments used were Roche Cobas E601 electrochemical luminescence
immunoassay analyzer (Roche Diagnostics Co., Ltd., Shanghai,
China), CEA detection kit (xy-302; Shanghai Xinyu Biotechnology
Co., Ltd., Shanghai, China) and CYFRA21-1 (JK-EA00523; Shanghai
Jingkang Bioengineering Co., Shanghai, China).
Electrochemiluminescence was used to detect serum CEA and CYFRA21-1
levels in the two groups.
Follow-up and observation
indicators
After treatment, patients in the two groups were
followed up by visiting the hospital and by telephone. Their
survival times and diameter rates of survival lesion were recorded
at 6th, 12th, and 24th months after treatment. Therapeutic effects
were evaluated according to the evaluation criteria in solid tumors
of the World Health Organization (WHO), and the overall efficacy
was recorded. If the disease mutated, the patient was promptly
treated. The magnetic resonance examination was strengthened at
each time of follow-up in clinic. Survival time was recorded from
the 1st day of patients with lung adenocarcinoma brain metastasis
treated with gamma knife to the death or follow-up deadline. The
last follow-up time of this study was December 23, 2017.
Response evaluation criteria (21)
The evaluation was based on the Response Evaluation
Criteria in Solid Tumors (RECIST). Complete response (CR): all
lesions disappear and this is maintained for 4 weeks. Partial
response (PR): the total lesion diameter decreases by ≥30% and
maintained for 4 weeks. Progressive disease (PD): the total lesion
diameter increases by ≥20% or new lesions occur. Stable disease
(SD): the total lesion diameter decreases but does not reach PR, or
increases but does not reach PD. The effective rate = (CR+PR)/total
number of cases ×100%. The tumor local control rate =
(CR+PR+SD)/total number of cases ×100%.
Determination of toxic and side
effects
Following the common chemotherapeutic drugs grading
criteria of the WHO (22), the
adverse reactions observed in patients with lung adenocarcinoma
brain metastasis, such as nausea and vomiting, fatigue and
myelosuppression caused by drug use were graded. Then, the
incidence of toxic and side effects was compared between the
pemetrexed combined with radiotherapy group and the simple gamma
knife group.
Statistical methods
SPSS 17.0 statistical software (SPSS, Inc., Chicago,
IL, USA) was used to statistically analyze the experimental data.
Enumeration data were expressed as n (%). The Chi-square test was
used for the comparison between groups. Measurement data were
expressed as mean ± standard deviation. Paired t-test was used for
data comparison before and after treatment in the group. The paired
t-test was used for the comparison in the group before and after
treatment. Multiple comparisons were performed using ANOVA followed
by the SNK test which was used as the post hoc test. The Kaplan
Meier test for the survival analysis and log-rank test were also
used. P<0.05 was considered to indicate a statistically
significant difference.
Results
Comparison of clinical basic
conditions between two groups of patients with lung adenocarcinoma
brain metastasis
The clinical basic conditions of patients were
analyzed, as shown in Table I. There
was no significant difference between the experimental and control
group, in sex, age, smoking, number of brain metastasis lesions,
maximum diameter of brain metastasis lesion, primary tumor number,
primary tumor site and ECOG score factors in patient behavioral
status (P>0.05).
 | Table I.Comparison of clinical basic
conditions between two groups of patients with lung adenocarcinoma
brain metastasis [n (%)]. |
Table I.
Comparison of clinical basic
conditions between two groups of patients with lung adenocarcinoma
brain metastasis [n (%)].
| Clinical
characteristics | Experimental group
(n=67) | Control group
(n=53) | χ2 | P-value |
|---|
| Sex |
|
| 0.099 | 0.753 |
| Male | 36 (53.73) | 30 (56.60) |
|
|
|
Female | 31 (46.27) | 23 (43.40) |
|
|
| Age (years) |
|
| 0.203 | 0.653 |
| ≤65 | 39 (58.21) | 33 (62.26) |
|
|
|
>65 | 28 (41.79) | 20 (37.74) |
|
|
| Smoking |
|
|
|
|
| Yes | 12 (17.91) | 10 (18.87) | 0.018 | 0.893 |
| No | 55 (82.09) | 43 (81.13) |
|
|
| Number of brain
metastasis lesions (1–10 lesions) |
|
| 1.315 | 0.251 |
| ≤3 | 40 (59.70) | 37 (69.81) |
|
|
|
>3 | 27 (40.30) | 16 (30.19) |
|
|
| Maximum diameter of
brain metastasis lesion (cm) |
|
| 1.079 | 0.299 |
| ≤3 | 38 (56.72) | 35 (66.04) |
|
|
|
>3 | 29 (43.28) | 18 (33.96) |
|
|
| Primary tumor
number |
|
| 0.056 | 0.813 |
|
Simple | 48 (71.64) | 39 (73.58) |
|
|
|
Multiple | 19 (28.36) | 14 (26.42) |
|
|
| Primary tumor
site |
|
| 2.033 | 0.154 |
|
Peripheral type | 44 (65.67) | 28 (52.83) |
|
|
| Central
type | 23 (34.33) | 25 (47.17) |
|
|
| ECOG score |
|
| 0.007 | 0.934 |
| ≤2 | 51 (76.12) | 40 (75.47) |
|
|
|
>2 | 16 (23.88) | 13 (24.53) |
|
|
Comparison of clinical efficacy
between two groups of patients
All treatments and follow-ups were performed on both
groups of patients. The treatment effective rate and tumor local
control rate of patients were compared between experimental and
control group, and were found to be significantly different
(P<0.05). The results showed that the treatment effective rate
and tumor local control rate were significantly higher in
experimental group than those in control group, and the clinical
efficacy was better in experimental group than that in control
group (Table II).
 | Table II.Comparison of clinical efficacy
between two groups of patients [n (%)]. |
Table II.
Comparison of clinical efficacy
between two groups of patients [n (%)].
| Group | n | CR | PR | SD | PD | Effective rate | Tumor local control
rate |
|---|
| Experimental
group | 67 | 16 (23.88) | 39 (58.21) | 7 (10.45) | 5 (7.46) | 82.09% | 92.54% |
| Control group | 53 | 13 (24.53) | 20 (37.74) | 9 (16.98) | 11 (20.75) | 62.26% | 79.25% |
| χ2 |
|
|
|
|
| 5.948 | 4.524 |
| P-value |
|
|
|
|
| <0.05 | <0.05 |
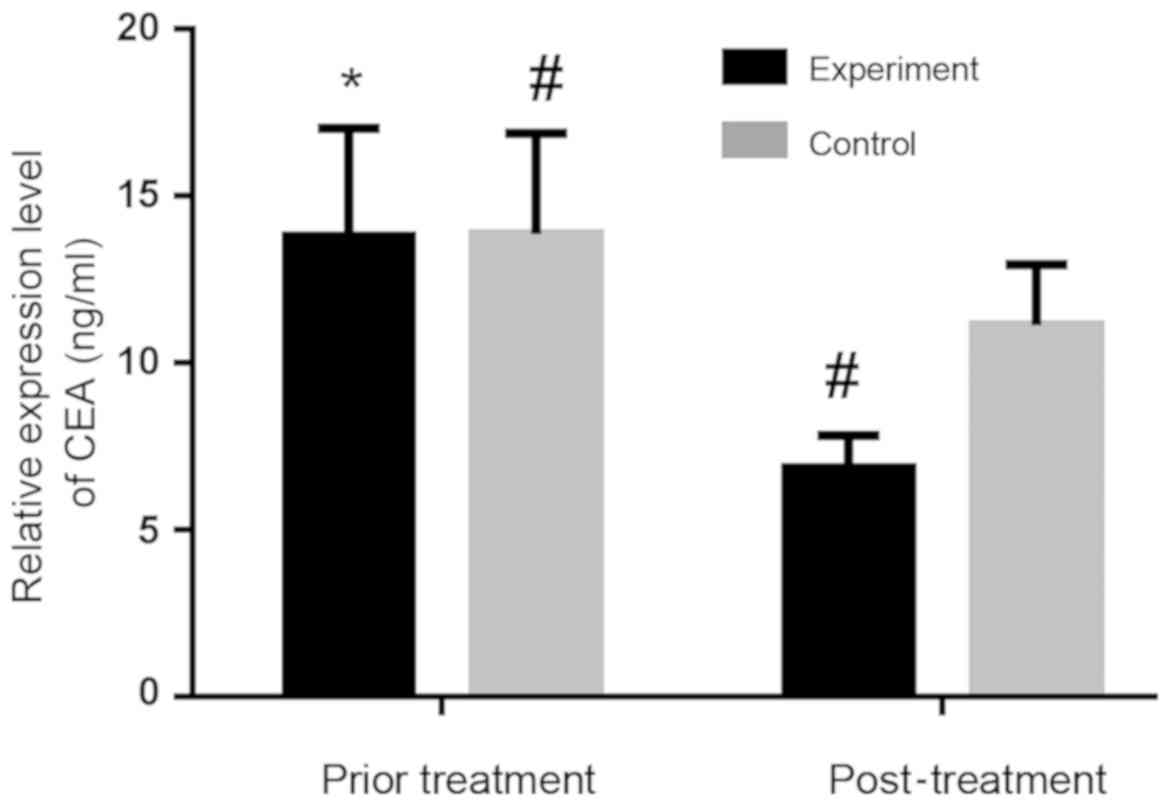
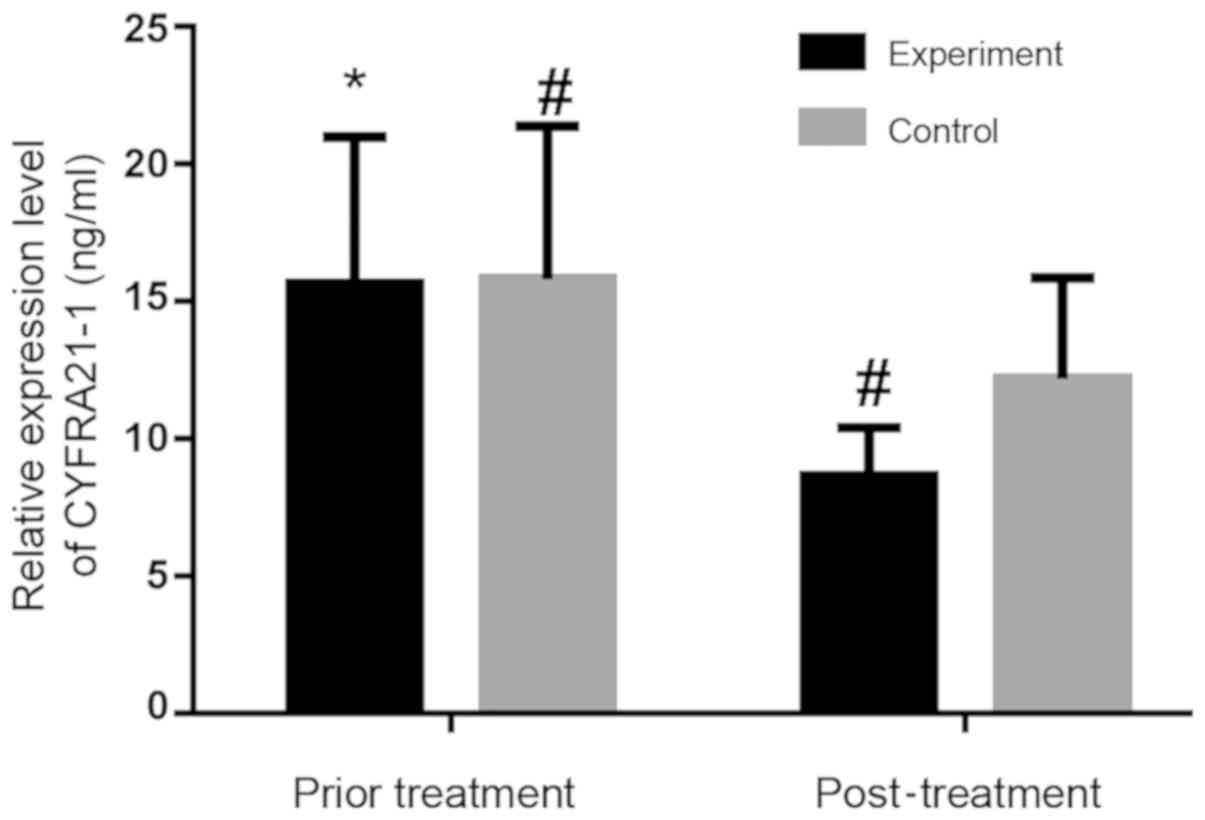
Comparison of the serum levels
In experimental group, serum CEA and CYFRA21-1
concentrations before treatment were 13.78±3.24 and 15.67±5.32
ng/ml, respectively. Those after treatment were 6.85±0.98 and
8.65±1.75 ng/ml, respectively. Serum levels of CEA and CYFRA21-1
after treatment were significantly lower than those before
treatment in the experimental group (P<0.05). In control group,
the serum CEA and CYFRA21-1 levels before treatment were 13.85±3.02
and 15.82±5.56 ng/ml, respectively. Those after treatment were
11.12±1.82 and 11.12±1.82 ng/ml, respectively. Serum levels after
treatment were lower than those before treatment in the control
group (P=0.0004, 0.0033). After treatment, the expression of serum
CEA and CYFRA21-1 in the experimental group was significantly lower
than those in the control group (P<0.05). Figs. 1 and 2
show that the overall decrease is more obvious in the experimental
group than that in the control group.
Comparison of side reactions between
two groups
Both groups had better tolerance and fewer adverse
reactions in grades III–IV. Severe side reactions in grades I–II
were compared between experimental and control groups. The
proportion of toxic and side effects was significantly lower in
experimental group than that in control group, and there was a
significant difference in the incidence of toxic and side effects
between the two groups (P<0.05; Table III).
 | Table III.Comparison of side reactions between
two groups [n (%)]. |
Table III.
Comparison of side reactions between
two groups [n (%)].
|
|
| I–II |
|---|
|
|
|
|
|---|
| Group | n |
Myelosuppression | Fatigue
vomiting | Nausea and
esophagitis | Radiation | Radiation
pneumonitis |
|---|
| Experimental
group | 67 | 18 (26.87) | 39 (58.21) | 34 (50.75) | 9 (13.43) | 4 (5.97) |
| Control group | 53 | 26
(49.06)a | 41
(77.36)a | 46
(86.79)a | 15
(28.30)a | 10
(18.87)a |
| χ2 |
| 6.28 | 4.88 | 17.30 | 4.09 | 4.78 |
| P-value |
|
0.012 |
0.027 |
<0.001 |
0.043 |
0.029 |
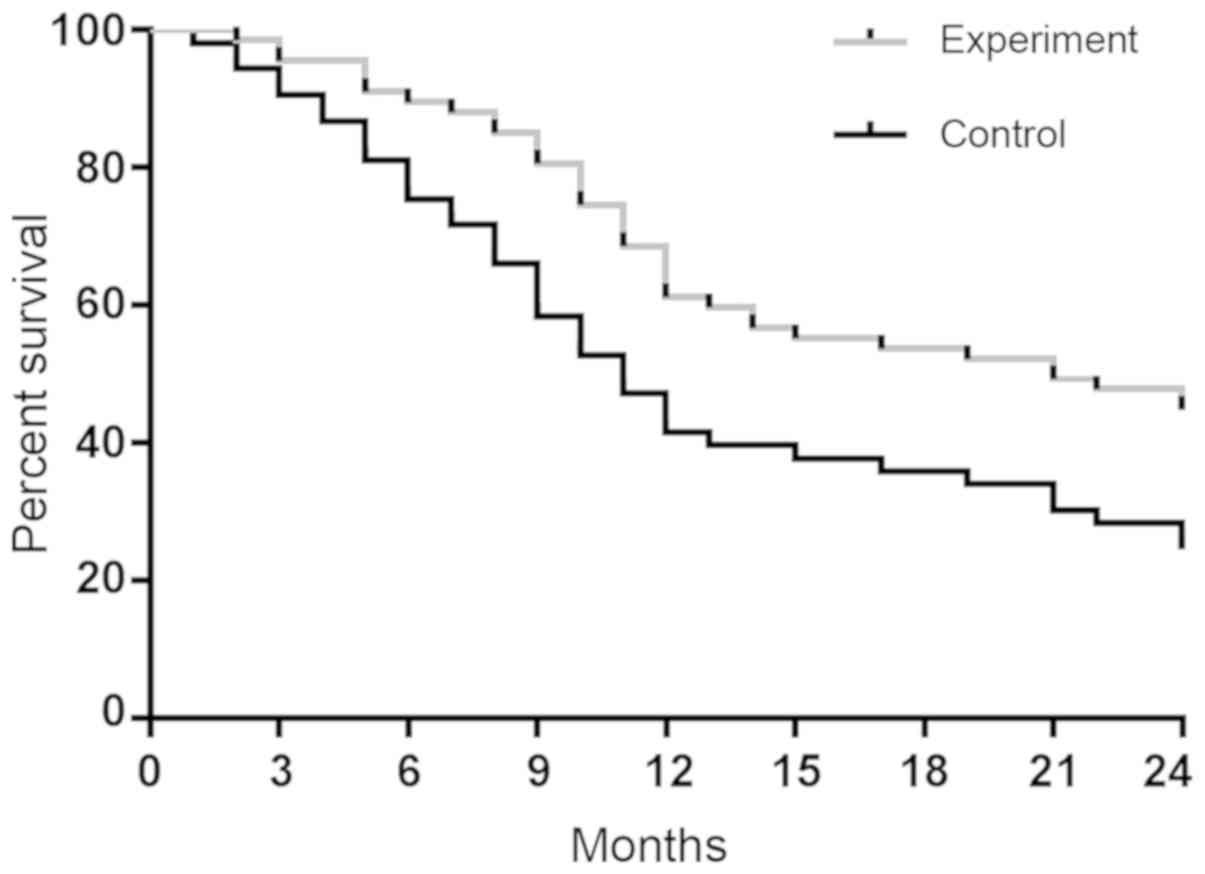
Comparison of survival analysis
between two groups
The 6-, 12- and 24-month survival rates in the
experimental group were 89.55% (60/67), 61.19% (41/67) and 44.78%
(30/67), respectively, with a median survival time of 13.1 months.
Those in control group were 75.47% (40/53), 41.51% (22/53) and
24.53% (13/53), respectively, with a median survival time of 10.8
months. The survival rate and median survival time were higher in
experimental group than those in control group, and there were
significant differences in the 6-, 12- and 24-month survival rates
between the two groups (P<0.05). Survival curves were plotted
according to the survival data of experimental and control groups
(Fig. 3).
Discussion
Lung adenocarcinoma is one of the most common
malignant tumors in respiratory diseases, and the incidence of
brain metastasis is lower than that of other types of metastases.
Nevertheless, once occurring, it causes serious consequences, which
is also an important reason for poor prognosis and death in
patients with advanced lung adenocarcinoma (2). In clinic, the use of a simple treatment
method is not ideal. Gamma knife radiotherapy is often used in
patients with lung adenocarcinoma brain metastasis, mainly because
its application can improve the poor positioning of whole brain
radiotherapy and the shortage of radiation dose to some extent
(23). In addition, gamma knife has
the advantages of no craniotomy and small damage. The damage degree
of the tissue near the target is significantly reduced, with the
edge of the lesion after operation being sharper (24). Pemetrexed is the first-line of
chemotherapy for lung adenocarcinoma (12). It has a stronger ability of blood
brain barrier penetration. Pemetrexed has multiple targets, so it
shows broad-spectrum anti-tumor effect in clinical application,
with exact efficacy (25).
Serum CEA is one of the most widely used tumor
markers in clinical practice, and changes in CEA level have a
certain judgment value for predicting the therapeutic efficacy and
prognoses of patients with lung adenocarcinoma brain metastasis
(26). CYFRA21-1, having higher
sensitivity and specificity for lung cancer brain metastasis than
CEA, is the preferred tumor marker (27). Commonly used to monitor lung
adenocarcinoma brain metastasis, the expression levels of serum CEA
and CYFRA21-1 in patients are often considered to be positively
correlated with tumor recurrence and metastasis, but negatively
correlated with the survival rate of lung adenocarcinoma patients
(28). In this study, the expression
levels of both kinds of serum before treatment were higher than
those after treatment in experimental and control group. The serum
levels after treatment were significantly lower than those before
treatment in the experimental group (P<0.05), as well as in the
control group (P<0.05). Additionally, the decrease of serum CEA
and CYFRA21-1 levels after treatment was more obvious in
experimental group than that in control group. The detection of CEA
and CYFRA21-1 indicates that pemetrexed combined with radiotherapy
is more effective than simple gamma knife treatment. Therefore, the
detection of tumor marker content in serum has certain guiding
significance in judging the efficacy of drug treatment (29).
In this study, there was no significant difference
between experimental and control group, in sex, age, smoking,
number of brain metastasis lesions, maximum diameter of brain
metastasis lesion, primary tumor number, primary tumor site and
ECOG score factors in patient behavioral status (P>0.05). It was
found that the effective rate and local control rate in the
experimental group were significantly higher than those in the
control group. The differences between the groups were
statistically significant (P<0.05), suggesting that this
combination regimen can improve patients' quality of life to some
extent. This is mainly due to the fact that pemetrexed can reduce
the incidence of lung adenocarcinoma brain metastasis (12). By regulating multiple enzymes in the
folate-dependent metabolic pathway, pemetrexed mainly acts on
multiple targets in the body to act as an anti-folate, further
effectively inhibiting the synthesis and metabolism of tumor cells
in vivo (30,31). The present study showed that the
incidence of adverse reactions such as toxic and side effects was
lower in the experimental group than that in the control group,
with a statistically significant difference (P<0.05). This
indicates that the safety of the combination treatment is higher
than that of the simple radiotherapy. The survival time was
compared between the experimental and control group. The results
showed that the median survival time of patients was longer in the
experimental group than that in the control group, and there were
significant differences in the 6-, 12- and 24-month survival rates
of patients between the two groups (P<0.05). This suggests that
pemetrexed combined with radiotherapy can prolong the survival time
of lung adenocarcinoma patients to some extent. The study of Tiseo
et al (32) has shown that
pemetrexed-disodium combined with gamma knife in the treatment of
non-small cell lung cancer brain metastasis has better clinical
efficacy and safety than simple gamma knife treatment, with certain
clinical promotion and application value. This is consistent with
the findings of our study.
The clinical significance and safety evaluation of
pemetrexed combined with radiotherapy were explored by efficacy
evaluation, tumor marker detection, side reaction judgment, and
survival analysis. The investigation and analysis are more
comprehensive, so the results are convincing, conducive to
providing reference for the clinic. However, in the screening of
lung adenocarcinoma patients and collection of relevant data,
subjective factors are inevitable. Also, there is a limitation in
the design. Four further experimental groups could be included in
future experiments to validate the data: i) simple gamma-knife
only, ii) whole body gamma knife only, iii) pemetrexed only, and
iv) a combination of pemetrexed and whole body gamma knife. In
addition, in subsequent studies, the staging of lung adenocarcinoma
brain metastasis should be studied, to compare the efficacy
difference between pemetrexed combined with radiotherapy and simple
gamma knife and the incidence of adverse reactions in the
staging.
In summary, pemetrexed combined with stereotactic
gamma-ray radiotherapy in the treatment of patients with lung
adenocarcinoma brain metastasis is more effective, with lighter
adverse reactions and higher safety. Having certain clinical value,
it can provide reference for clinically selecting treatment methods
of lung adenocarcinoma brain metastasis.
Acknowledgements
Not applicable.
Funding
This study was supported by the Yunnan Province
Health Science and Technology Project (no. 2014NS266).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
GZ and RZ assisted with CEA and CYFRA21-1
determination. KW and YA collected and analyzed the general
information of patients. LL and KG were responsible for the
surgery. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
The First People's Hospital of Yunnan Province (Kunming, China).
Patients who participated in this research, signed an informed
consent and had complete clinical data.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ning M, Chunhua M, Rong J, Yuan L, Jinduo
L, Bin W and Liwei S: Diagnostic value of circulating tumor cells
in cerebrospinal fluid. Open Med (Wars). 11:21–24. 2016.PubMed/NCBI
|
|
2
|
Kawabe T, Phi JH, Yamamoto M, Kim DG,
Barfod BE and Urakawa Y: Treatment of brain metastasis from lung
cancer. Prog Neurol Surg. 25:148–155. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Fidler IJ: The biology of brain
metastasis: challenges for therapy. Cancer J. 21:284–293. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Johung KL, Yeh N, Desai NB, Williams TM,
Lautenschlaeger T, Arvold ND, Ning MS, Attia A, Lovly CM, Goldberg
S, et al: Extended survival and prognostic factors for patients
with ALK-rearranged non-small-cell lung cancer and brain
metastasis. J Clin Oncol. 34:123–129. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Jamal-Hanjani M and Spicer J: Epidermal
growth factor receptor tyrosine kinase inhibitors in the treatment
of epidermal growth factor receptor-mutant non-small cell lung
cancer metastatic to the brain. Clin Cancer Res. 18:938–944. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Liu WJ, Zeng XT, Qin HF, Gao HJ, Bi WJ and
Liu XQ: Whole brain radiotherapy plus chemotherapy in the treatment
of brain metastases from lung cancer: A meta-analysis of 19
randomized controlled trails. Asian Pac J Cancer Prev.
13:3253–3258. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shi Y, Sun Y, Yu J, Ding C, Ma Z, Wang Z,
Wang D, Wang Z, Wang M, Wang Y, et al: China experts consensus on
the diagnosis and treatment of brain metastases of lung cancer
(2017 version). Zhongguo Fei Ai Za Zhi. 20:1–13. 2017.(In Chinese).
PubMed/NCBI
|
|
8
|
Rahn DA III, Ray DK, Schlesinger DJ,
Steiner L, Sheehan JP, O'Quigley JM and Rich T: Gamma knife
radiosurgery for brain metastasis of nonsmall cell lung cancer: Is
there a difference in outcome between morning and afternoon
treatment? Cancer. 117:414–420. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Peacock KH and Lesser GJ: Current
therapeutic approaches in patients with brain metastases. Curr
Treat Options Oncol. 7:479–489. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pan HC, Sheehan J, Stroila M, Steiner M
and Steiner L: Gamma knife surgery for brain metastases from lung
cancer. J Neurosurg. 102 Suppl:128–133. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gerosa M, Nicolato A, Foroni R, Tomazzoli
L and Bricolo A: Analysis of long-term outcomes and prognostic
factors in patients with non-small cell lung cancer brain
metastases treated by gamma knife radiosurgery. J Neurosurg. 102
Suppl:75–80. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ortuzar W, Hanna N, Pennella E, Peng G,
Langer C, Monberg M and Scagliotti G: Brain metastases as the
primary site of relapse in two randomized phase III pemetrexed
trials in advanced non-small-cell lung cancer. Clin Lung Cancer.
13:24–30. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shimizu T, Nakanishi Y, Nakagawa Y,
Tsujino I, Takahashi N, Nemoto N and Hashimoto S: Association
between expression of thymidylate synthase, dihydrofolate
reductase, and glycinamide ribonucleotide formyltransferase and
efficacy of pemetrexed in advanced non-small cell lung cancer.
Anticancer Res. 32:4589–4596. 2012.PubMed/NCBI
|
|
14
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2016. CA Cancer J Clin. 66:7–30. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Shi Y, Sun Y, Ding C, Wang Z, Wang C, Bai
C, Bai C, Feng J, Liu X, Li F, et al: China experts consensus on
icotinib for non-small cell lung cancer treatment (2016 version).
Zhongguo Fei Ai Za Zhi. 19:489–494. 2016.(In Chinese). PubMed/NCBI
|
|
16
|
Wang XF, Wu YH, Wang MS and Wang YS: CEA,
AFP, CA125, CA153 and CA199 in malignant pleural effusions predict
the cause. Asian Pac J Cancer Prev. 15:363–368. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nagashima T, Sakao Y, Mun M, Ishikawa Y,
Nakagawa K, Masuda M and Okumura S: A clinicopathological study of
resected small-sized squamous cell carcinomas of the peripheral
lung: Prognostic significance of serum carcinoembryonic antigen
levels. Ann Thorac Cardiovasc Surg. 19:351–357. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kulpa J, Wójcik E, Reinfuss M and
Kołodziejski L: Carcinoembryonic antigen, squamous cell carcinoma
antigen, CYFRA 21-1, and neuron-specific enolase in squamous cell
lung cancer patients. Clin Chem. 48:1931–1937. 2002.PubMed/NCBI
|
|
19
|
Sertić Milić H, Franjević A, Bubanović G,
Marušić A, Nikolić I and Puljić I: Size, edge, and stage of NSCLC
determine the release of CYFRA 21-1 in bloodstream. Wien Klin
Wochenschr. 127:465–471. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Szturmowicz M, Rudziński P, Kacprzak A,
Langfort R, Bestry I, Broniarek-Samson B and Orłowski T: Prognostic
value of serum C-reactive protein (CRP) and cytokeratin 19
fragments (Cyfra 21-1) but not carcinoembryonic antigen (CEA) in
surgically treated patients with non-small cell lung cancer.
Pneumonol Alergol Pol. 82:422–429. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ramalingam S and Belani C: Systemic
chemotherapy for advanced non-small cell lung cancer: recent
advances and future directions. Oncologist. 13 Suppl 1:5–13. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Muallaoglu S, Disel U, Mertsoylu H, Besen
A, Karadeniz C, Taner Sumbul A, Abali H and Ozyilkan O: Acute
infusion reactions to chemotherapeutic drugs: a single institute
experience. J BUON. 18:261–267. 2013.PubMed/NCBI
|
|
23
|
Lindvall P, Bergström P, Löfroth PO,
Henriksson R and Bergenheim AT: Hypofractionated conformal
stereotactic radiotherapy alone or in combination with whole-brain
radiotherapy in patients with cerebral metastases. Int J Radiat
Oncol Biol Phys. 61:1460–1466. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Park SJ, Kim HT, Lee DH, Kim KP, Kim SW,
Suh C and Lee JS: Efficacy of epidermal growth factor receptor
tyrosine kinase inhibitors for brain metastasis in non-small cell
lung cancer patients harboring either exon 19 or 21 mutation. Lung
Cancer. 77:556–560. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Al-Saleh K, Quinton C and Ellis PM: Role
of pemetrexed in advanced non-small-cell lung cancer: meta-analysis
of randomized controlled trials, with histology subgroup analysis.
Curr Oncol. 19:e9–e15. 2012.PubMed/NCBI
|
|
26
|
Arrieta O, Villarreal-Garza C,
Martínez-Barrera L, Morales M, Dorantes-Gallareta Y, Peña-Curiel O,
Contreras-Reyes S, Macedo-Pérez EO and Alatorre-Alexander J:
Usefulness of serum carcinoembryonic antigen (CEA) in evaluating
response to chemotherapy in patients with advanced non small-cell
lung cancer: a prospective cohort study. BMC Cancer. 13:2542013.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Hoang T, Xu R, Schiller JH, Bonomi P and
Johnson DH: Clinical model to predict survival in chemonaive
patients with advanced non-small-cell lung cancer treated with
third-generation chemotherapy regimens based on eastern cooperative
oncology group data. J Clin Oncol. 23:175–183. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Muley T, Fetz TH, Dienemann H, Hoffmann H,
Herth FJ, Meister M and Ebert W: Tumor volume and tumor marker
index based on CYFRA 21-1 and CEA are strong prognostic factors in
operated early stage NSCLC. Lung Cancer. 60:408–415. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Guo J, Yu J, Song X and Mi H: Serum CA125,
CA199 and CEA combined detection for epithelial ovarian cancer
diagnosis: A meta-analysis. Open Med (Wars). 12:131–137.
2017.PubMed/NCBI
|
|
30
|
Zhao R, Qiu A, Tsai E, Jansen M, Akabas MH
and Goldman ID: The proton-coupled folate transporter: Impact on
pemetrexed transport and on antifolates activities compared with
the reduced folate carrier. Mol Pharmacol. 74:854–862. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Chattopadhyay S, Moran RG and Goldman ID:
Pemetrexed: biochemical and cellular pharmacology, mechanisms, and
clinical applications. Mol Cancer Ther. 6:404–417. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Tiseo M, Giovannetti E, Tibaldi C,
Camerini A, Di Costanzo F, Barbieri F, Burgers JA, Vincent A,
Peters GJ, Smit EF and Ardizzoni A: Pharmacogenetic study of
patients with advanced non-small cell lung cancer (NSCLC) treated
with second-line pemetrexed or pemetrexed-carboplatin. Lung Cancer.
78:92–99. 2012. View Article : Google Scholar : PubMed/NCBI
|