Introduction
Lung cancer has the highest morbidity and mortality
rate in the male population and the second highest in the female
population among the common malignant tumors in the world (1). There are about 1.8 million new cases of
lung cancer and 1.6 million deaths in the world every year, and the
5-year survival rate is only 15% (2,3). The risk
factors for lung cancer include industrial pollution, air
pollution, genetic factors, and smoking (4).
Lung cancer resection is one of the most important
methods in the treatment of early lung cancer in clinic. However,
postoperative cognitive impairment is a problem that clinicians
have always been trying to overcome. It has been proved that
anesthesia can cause brain cognitive impairment, which can increase
the recovery time and financial burden in mild cases and become
life-threatening in severe cases (5,6). At the
same time, it is easy to cause a certain degree of lung
ischemia-reperfusion injury and affect the pulmonary function, thus
affecting the prognosis of patients because of the need of
resection of partial lung tissue after surgery (7). Serum matrix metalloproteinase-9 (MMP-9)
is one of the proteolytic enzymes released by neutrophils. The
release of MMP-9 by neutrophils is considered to play an important
role in promoting pulmonary inflammation by degrading basement
membrane and migrating neutrophils to lung tissues and airways
(8). According to reports in the
literature, some anaesthetics have effects of cell protection and
are anti-inflammatory (9). Therefore,
how to improve anesthetic methods and reduce the malignant effects
of anesthesia on pulmonary function and cognitive function is a
very important issue.
The purpose of this study was to compare the effects
of sevoflurane and propofol anesthesia on pulmonary function, MMP-9
and postoperative cognition in patients undergoing simple resection
of the lower lobe of left lung, and to provide a theoretical basis
for better clinical choice of anaesthetics.
Patients and methods
Basic information
A total of 58 cases of lung cancer treated by simple
resection of lower lobe of left lung in the Second Hospital of
Dalian Medical University (Dalian, China) from October 2016 to
October 2017 were analyzed retrospectively, including 36 males and
22 females with an average age of 52.68±14.52 years. They were
divided into two groups: Sevoflurane group (n=32) with sevoflurane
anesthesia and propofol group (n=26) with propofol anesthesia.
There was no significant difference in the basic information
between the two groups (P>0.05). Pregnancy and lactation,
autoimmune diseases, chronic inflammation, diabetes, hypertension
and heart disease were excluded in all cases, and all patients had
normal liver and kidney function and did not receive radiotherapy,
chemotherapy, hormones and other drug analgesia, or
anti-inflammatory treatment before surgery.
The study was approved by the Ethics Committee of
the Second Hospital of Dalian Medical University. Patients who
participated in this research had complete clinical data. The
signed informed consents were obtained from the patients or the
guardians (Table I).
 | Table I.Basic information [n (%)]. |
Table I.
Basic information [n (%)].
|
| Groups |
|
|
|---|
|
|
|
|
|
|---|
| Factors | Sevoflurane
(n=32) | Propofol (n=26) | t/χ2 | P-value |
|---|
| Age (years) |
|
| 0.288 | 0.782 |
|
<52 | 12 (37.50) | 8
(30.77) |
|
|
| ≥52 | 20 (62.50) | 18 (69.23) |
|
|
| Sex |
|
| 0.220 | 0.787 |
| Male | 19 (59.38) | 17 (65.38) |
|
|
|
Female | 13 (40.62) | 9
(34.62) |
|
|
| BMI
(kg/m2) | 26.42±1.05 | 25.84±1.17 | 1.988 | 0.052 |
| Operation duration
(min) | 194.52±42.41 | 195.83±45.61 | 0.113 | 0.910 |
| Revival time
(min) | 22.15±8.23 | 23.36±9.42 | 0.522 | 0.604 |
| Smoking status |
|
| 0.620 | 0.543 |
| Used to
smoke | 23 (71.88) | 21 (80.77) |
|
|
| Never
smoke | 9
(28.12) | 5
(19.23) |
|
|
| ASA
classification |
|
| 1.115 | 0.429 |
| I | 18 (56.25) | 11 (42.31) |
|
|
| II | 14 (43.75) | 15 (57.69) |
|
|
| Degree of
education |
|
| 0.130 | 0.778 |
| Junior
secondary school and below | 10 (31.25) | 7
(26.92) |
|
|
| Junior
high school or above | 22 (68.75) | 19 (73.08) |
|
|
| Preoperative heart
rate (time/min) | 78.23±9.13 | 77.84±8.91 | 0.164 | 0.871 |
| Mean arterial
pressure during operation (mmHg) |
88.62±15.22 |
86.28±16.57 | 0.560 | 0.578 |
| Blood loss during
operation (ml) | 102.56±34.85 | 100.17±29.74 | 0.277 | 0.783 |
| Infusion volume
during operation (ml) | 1,263.25±342.12 | 1,186.64±320.73 | 0.872 | 0.387 |
Treatment methods
The patients were prohibited from eating for 8 h and
using medication before the surgery, and 0.2 mg/kg midazolam
intravenous injection (H20031037; Jiangsu Enhua Pharmaceutical
Group Co., Ltd., Jiangsu, China) was conducted 30 min prior to
surgery. Invasive monitoring of angiosthenia, central venous
pressure, electrocardiogram, blood pressure, heart rate, pulse and
oxygen protection was established. In propofol group, propofol
(H20030114; Sichuan Guorui Pharmaceutical Co., Ltd., Sichuan,
China) target-controlled infusion (plasma concentration 3 µg/ml), 3
µg/kg fentanyl (H20030197; Yichang Humanwell Pharmaceutical Co.,
Ltd., Yichang, China), and 0.3 mg/kg atracurium (H20060869; Jiangsu
Hengrui Pharmaceutical Co., Ltd., Jiangsu, China) rapidly induced
endotracheal intubation by intravenous injection. After intubation,
the flow of inhaled oxygen was 2.0 l/min, the tidal volume was 8–10
ml/kg, the respiratory rate was 10–12 times/min, and the
respiratory ratio was 1:1.5. TCI pump (cp-660tci pump; Shanghai
Huanxi Medical equipment Co., Ltd., Shanghai, China) propofol
target controlled infusion (plasma concentration 4 µg/ml) was used
to maintain anesthesia. In sevoflurane group, 6% sevoflurane
(H35020148; Fujian Gutian Pharmaceutical Co., Ltd., Fujian, China)
with 5 l/min oxygen flow was initially inhaled. The patients were
asked to take a deep breath and applied positive pressure manual
ventilation when their consciousness disappeared. The oxygen flow
was reduced to 2 l/min, and the concentration of sevoflurane in the
volatile tank was adjusted to maintain the end-expiratory
sevoflurane concentration in the gas monitor at 1.0 MAC, fentanyl 3
µg/kg, atracurium 0.5–0.6 mg/kg rapidly induced endotracheal
intubation by intravenous injection, and 3% sevoflurane was inhaled
continuously for maintenance of anesthesia. Both groups received
continuous infusion of atracurium and fentanyl with micro-infusion
pump during surgery, and the average BIS was maintained between 40
and 60%.
Observation index
The moment before induction of anesthesia (T1),
before the start of one-lung ventilation (T2), before the end of
one-lung ventilation (T3), after closed chest surgery (T4), 24 h
after surgery (T5), calculate alveolar-arterial oxygen difference
(A-aD02), respiratory index (RI) and intrapulmonary shunt ratio
(Qs/Qt) were compared between the two groups (10).
The MMP-9 concentration in patients at T1, T4 and T5
was detected by ELISA (Shanghai Xinfan Biotechnology Co., Ltd.,
Shanghai, China). Then, 3 ml peripheral venous blood was drawn from
all patients at T1, T4 and T5 and centrifuged with 3,000 × g for 8
min at 4°C. The serum was collected and the level of MMP-9 was
detected by ELISA. The specific operation methods were strictly in
accordance with the instructions.
The cognitive function of two groups was assessed
according to Mini-Mental State Examination (MMSE) 1 day before
surgery and 1 and 10 days after surgery. The total score of MMSE is
30 points, and the normal range is 27–30 points. A decrease of 2
points is statistically significant. A total score of 23 or less
can be diagnosed as POCD. In addition, the occurrence of
restlessness in patients was recorded after surgery (11).
Statistical analysis
The data was analyzed by SPSS 20.0 statistical
software (IBM Corp., Armonk, NY, USA). Chi-square test was used for
count data. t-test was used for paired comparisons, and οne-way
ANOVA was used for multiple comparisons. The repetitive measure
analysis of variance (ANOVA) was used in the comparison of
different times within the group with Least Significant Difference
test. P<0.05 was considered to indicate a statistically
significant difference.
Results
Comparison of pulmonary function
between two groups
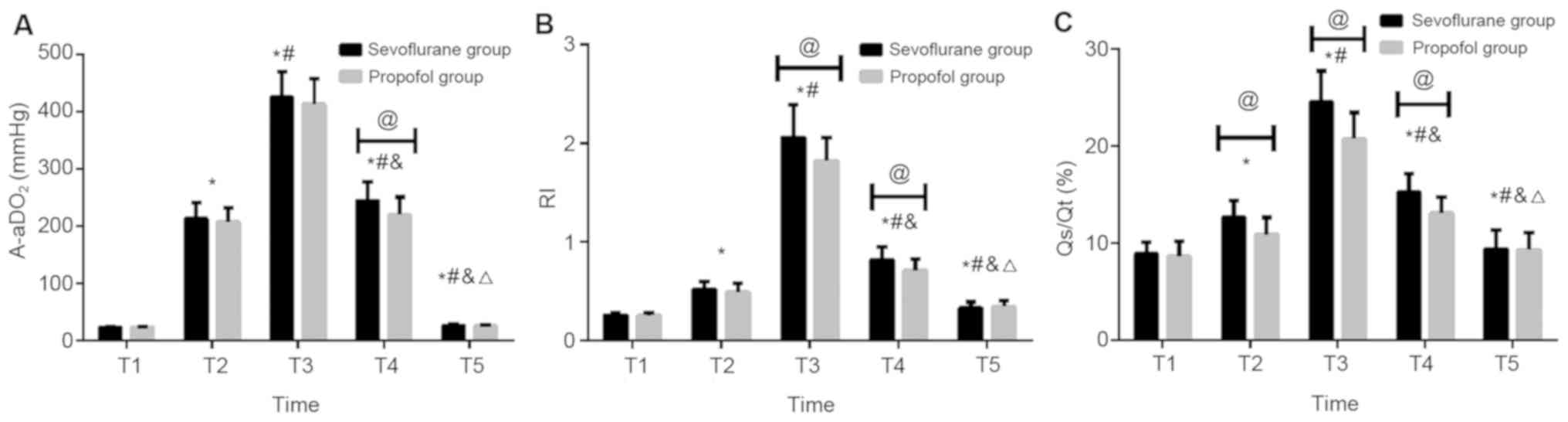
There was no significant difference in A-aDO2 level
at T1, T2, T3, T5 between sevoflurane and propofol groups
(P>0.05). The A-aDO2 level at T4 in sevoflurane group was
significantly higher than that in propofol group, and the
difference was statistically significant (P<0.05). Both
sevoflurane and propofol groups had significantly higher A-aDO2
level at T2, T3, T4 and T5 than that at T1. Both sevoflurane and
propofol groups had significantly higher A-aDO2 level at T3 and T4
than that at T2, and both sevoflurane and propofol groups had
significantly lower A-aDO2 level at T5 than that at T2. Both
sevoflurane and propofol groups had significantly lower A-aDO2
level at T4 and T5 than that at T3. Both sevoflurane and propofol
groups had significantly lower A-aDO2 level at T5 than that at T4,
and the difference was statistically significant (P<0.05).
There was no significant difference in RI level at
T1, T2, T5 between sevoflurane and propofol groups (P>0.05). The
RI level at T3, T4 in sevoflurane group was significantly higher
than that in propofol group, and the difference was statistically
significant (P<0.05). Both sevoflurane and propofol groups had
significantly higher RI level at T2, T3, T4 and T5 than that at T1.
Both sevoflurane and propofol groups had significantly higher RI
level at T3 and T4 than that at T2, and both sevoflurane and
propofol groups had significantly lower RI level at T5 than that at
T2. Both sevoflurane and propofol groups had significantly lower RI
level at T4 and T5 than that at T3. Both sevoflurane and propofol
groups had significantly lower RI level at T5 than that at T4, and
the difference was statistically significant (P<0.05).
There was no significant difference in Qs/Qt at T1,
T5 between sevoflurane and propofol groups (P>0.05). The Qs/Qt
at T2, T3 and T4 in sevoflurane group was significantly higher than
that in propofol group, and the difference was statistically
significant (P<0.05). Both sevoflurane and propofol groups had
significantly higher Qs/Qt at T2, T3, T4 and T5 than that at T1.
Both sevoflurane and propofol groups had significantly higher Qs/Qt
at T3 and T4 than that at T2, and both sevoflurane and propofol
groups had significantly lower Qs/Qt at T5 than that at T2. Both
sevoflurane and propofol groups had significantly lower Qs/Qt at T4
and T5 than that at T3. Both sevoflurane and propofol groups had
significantly lower Qs/Qt at T5 than that at T4, and the difference
was statistically significant (P<0.05; Fig. 1 and Table
II).
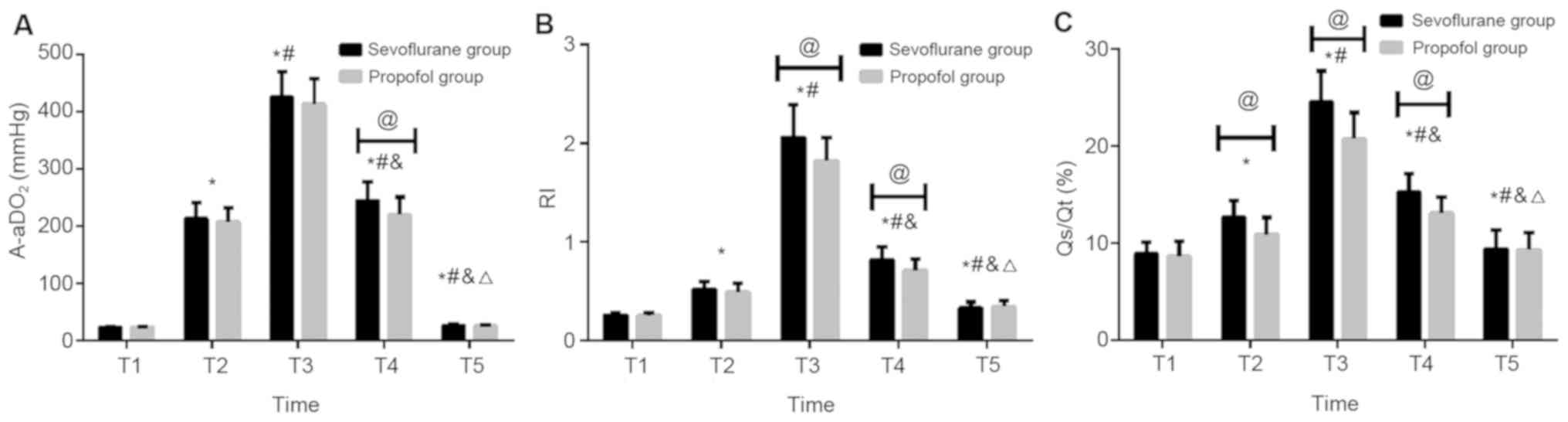 | Figure 1.Comparison of pulmonary function
between two groups. (A) There was no significant difference in
A-aDO2 level at T1, T2, T3 and T5 between sevoflurane and propofol
groups (P>0.05). The A-aDO2 level at T4 in sevoflurane group was
significantly higher than that in propofol group, and the
difference was statistically significant (P<0.05). Both
sevoflurane and propofol groups had significantly higher A-aDO2
level at T2, T3, T4 and T5 than that at T1. Both sevoflurane and
propofol groups had significantly higher A-aDO2 level at T3 and T4
than that at T2, and both sevoflurane and propofol groups had
significantly lower A-aDO2 level at T5 than that at T2. Both
sevoflurane and propofol groups had significantly lower A-aDO2
level at T4 and T5 than that at T3. Both sevoflurane and propofol
groups had significantly lower A-aDO2 level at T5 than that at T4,
and the difference was statistically significant (P<0.05). (B)
There was no significant difference in RI level at T1, T2 and T5
between sevoflurane and propofol groups (P>0.05). The RI level
at T3 and T4 in sevoflurane group was significantly higher than
that in propofol group, and the difference was statistically
significant (P<0.05). Both sevoflurane and propofol groups had
significantly higher RI level at T2, T3, T4 and T5 than that at T1.
Both sevoflurane and propofol groups had significantly higher RI
level at T3 and T4 than that at T2, and both sevoflurane and
propofol groups had significantly lower RI level at T5 than that at
T2. Both sevoflurane and propofol groups had significantly lower RI
level at T4, T5 than that at T3. Both sevoflurane and propofol
groups had significantly lower RI level at T5 than that at T4, and
the difference was statistically significant (P<0.05). (C) There
was no significant difference in Qs/Qt at T1, T5 between
sevoflurane and propofol group (P>0.05). The Qs/Qt at T2, T3 and
T4 in sevoflurane group was significantly higher than that in
propofol group, and the difference was statistically significant
(P<0.05). Both sevoflurane and propofol groups had significantly
higher Qs/Qt at T2, T3, T4 and T5 than that at T1. Both sevoflurane
and propofol groups had significantly higher Qs/Qt at T3 and T4
than that at T2, and both sevoflurane and propofol groups had
significantly lower Qs/Qt at T5 than that at T2. Both sevoflurane
and propofol groups had significantly lower Qs/Qt at T4 and T5 than
that at T3. Both sevoflurane and propofol groups had significantly
lower Qs/Qt at T5 than that at T4, and the difference was
statistically significant (P<0.05). *P<0.05 compared with T1;
#P<0.05 compared with T2; &P<0.05
compared with T3; △P<0.05 compared with T4;
@P<0.05. A-aDO2, alveolar-arterial oxygen difference;
RI, respiratory index; Qs/Qt, intrapulmonary shunt ratio. |
 | Table II.Comparison of pulmonary function
between two groups. |
Table II.
Comparison of pulmonary function
between two groups.
| Index | No. | T1 | T2 | T3 | T4 | T5 | F | P-value |
|---|
| A-aDO2 (mmHg) |
|
Sevoflurane | 32 | 23.56±1.72 |
213.54±28.46a |
426.52±43.26a,b |
244.73±33.25a–c |
26.49±1.93a–d | 1201.00 | <0.05 |
|
Propofol | 26 | 23.41±1.47 |
207.16±25.31a |
413.64±44.82a,b |
219.67±31.48a–c |
25.64±1.75a–d | 938.10 | <0.05 |
| t |
| 0.352 | 0.892 | 1.110 | 2.923 | 1.738 |
|
|
|
P-value |
| 0.726 | 0.376 | 0.272 | 0.005 | 0.088 |
|
|
| RI |
|
Sevoflurane | 32 | 0.26±0.02 |
0.52±0.08a |
2.06±0.33a,b |
0.82±0.13a–c |
0.33±0.06a–d | 639.90 | <0.05 |
|
Propofol | 26 | 0.25±0.03 |
0.49±0.09a |
1.82±0.24a,b |
0.71±0.12a–c |
0.34±0.07a–d | 616.10 | <0.05 |
| t |
| 1.517 | 1.343 | 3.100 | 3.316 | 0.586 |
|
|
|
P-value |
| 0.135 | 0.185 | 0.003 | 0.002 | 0.560 |
|
|
| Qs/Qt (%) |
|
Sevoflurane | 32 | 8.92±1.24 |
12.68±1.72a |
24.56±3.17a,b |
15.28±1.93a–c |
9.43±1.92a–d | 294.10 | <0.05 |
|
Propofol | 26 | 8.67±1.52 |
10.93±1.74a |
20.73±2.73a,b |
13.15±1.62a–c |
9.34±1.75a–d | 167.50 | <0.05 |
| t |
| 0.690 | 3.834 | 4.865 | 4.486 | 0.185 |
|
|
|
P-value |
| 0.493 | <0.05 | <0.05 | <0.05 | 0.854 |
|
|
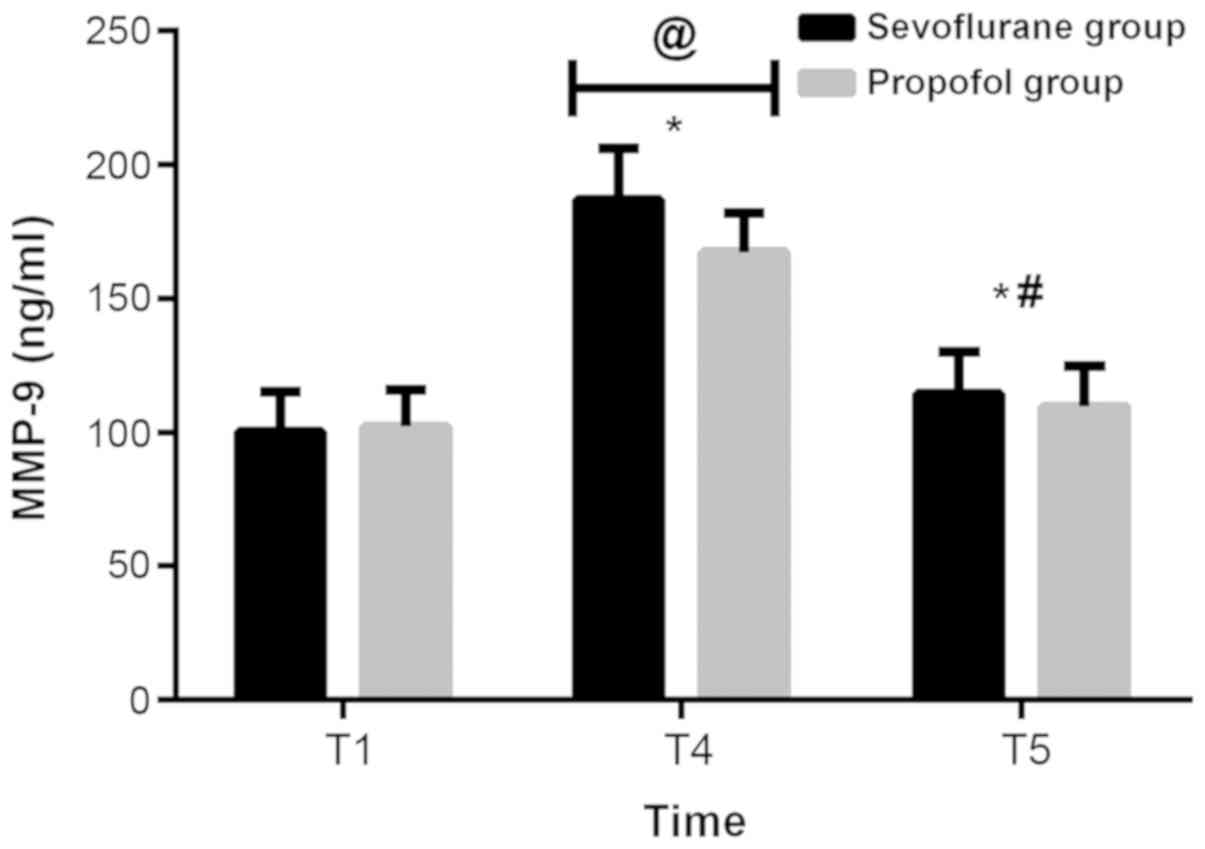
Comparison of MMP-9 between the two
groups
There was no significant difference in MMP-9 level
at T1 and T5 between sevoflurane and propofol group (P>0.05).
The MMP-9 level at T4 in the sevoflurane group was significantly
higher than that in the propofol group, and the difference was
statistically significant (P<0.05). Both sevoflurane and
propofol groups had significantly higher MMP-9 level at T4 and T5
than that at T1. Both sevoflurane and propofol groups had
significantly lower MMP-9 level at T5 than that at T4, and the
difference was statistically significant (P<0.05; Fig. 2 and Table
III).
 | Table III.Comparison of MMP-9 between the two
groups. |
Table III.
Comparison of MMP-9 between the two
groups.
| Index | No. | T1 | T4 | T5 | F | P-value |
|---|
| MMP-9 (ng/ml) |
|
Sevoflurane | 32 | 100.26±14.85 |
186.72±19.42a |
114.56±15.61a,b | 245.100 | <0.05 |
|
Propofol | 26 | 102.14±13.76 |
167.25±14.73a |
109.68±15.26a,b | 154.800 | <0.05 |
| t | 0.495 | 4.218 | 1.196 |
|
|
|
|
P-value | 0.622 | <0.05 | 0.237 |
|
|
|
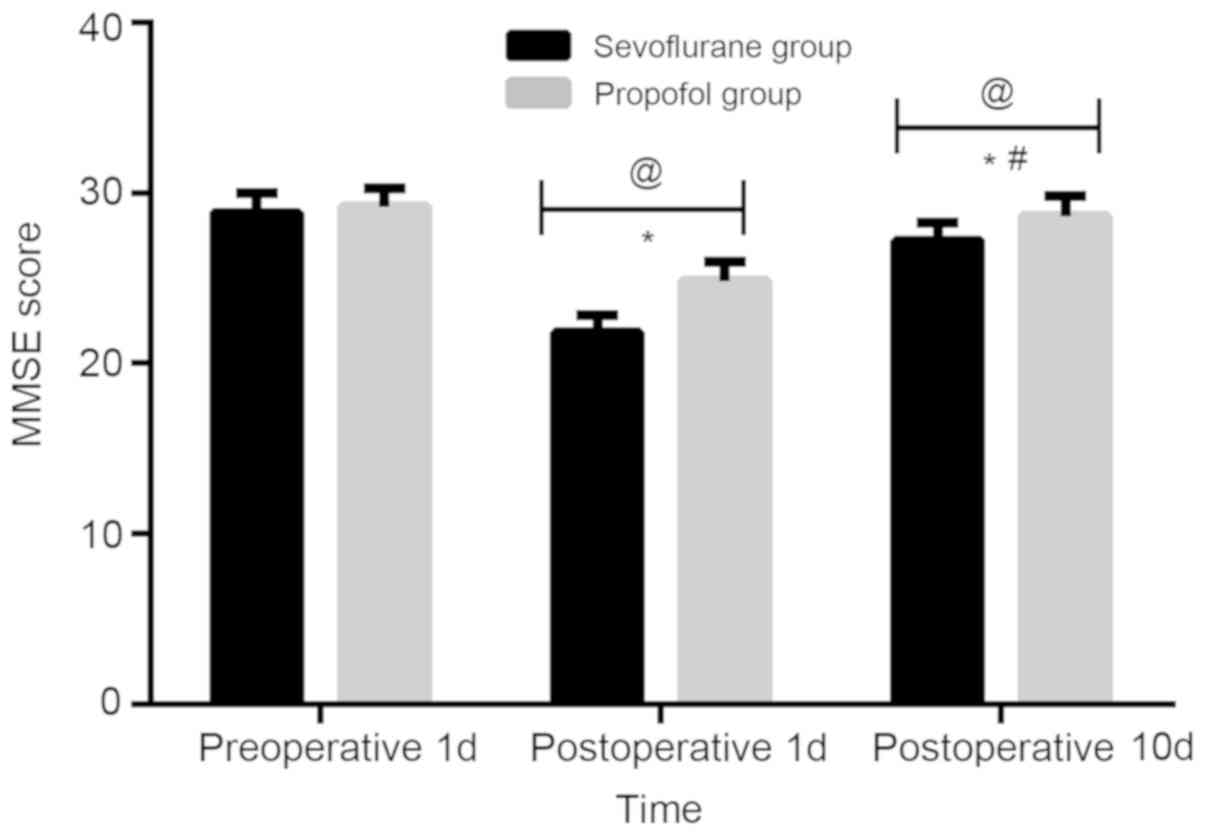
Comparison of cognitive function
between the two groups
There was no significant difference in MMSE score
between sevoflurane and propofol groups 1 day before surgery
(P>0.05). The MMSE score in sevoflurane group was significantly
lower than that in propofol group 1 and 10 days after surgery, and
the difference was statistically significant (P<0.05). Both
sevoflurane and propofol groups had significantly lower MMSE score
of 1 and 10 days after surgery than that of 1 day before surgery.
Both sevoflurane and propofol groups had significantly higher MMSE
score of 10 days after surgery than that of 1 day after surgery,
and the difference was statistically significant (P<0.05;
Fig. 3 and Table IV).
 | Table IV.Comparison of cognitive function
between the two groups. |
Table IV.
Comparison of cognitive function
between the two groups.
| Index | No. | 1 day before
surgery | 1 day after
surgery | 10 day after
surgery | F | P-value |
|---|
| MMSE score |
|
Sevoflurane | 32 | 28.86±1.13 |
21.84±1.02a |
27.21±1.03a,b | 311.100 | <0.05 |
|
Propofol | 26 | 29.23±1.05 |
24.86±1.08a |
28.65±1.18a,b | 147.700 | <0.05 |
| t |
| 1.290 | 10.860 | 4.889 |
|
|
|
P-value |
| 0.202 | <0.05 | <0.05 |
|
|
Discussion
According to literature reports, A-aDO2 and RI are
the main indicators of pulmonary diffusion function. There is a
positive correlation between the index value and the degree of lung
injury. The larger the value is, the more serious the lung injury
is (12). Qs/Qt is associated with
planing defects, causing arterial blood flow into the pulmonary
vein to cause Qs/Qt to rise (13).
MMP-9 is a proteolytic enzyme that activates inflammatory mediators
and cells in the lung and increases the permeability of pulmonary
capillaries, which leads to pneumonedema (14). The total score of MMSE is 30 points
and less than 23 points are regarded as cognitive dysfunction
(15). Propofol is the most widely
used intravenous anesthesia in clinical surgical treatment and has
the function of antioxidation and inhibition of inflammation. It is
generally more stable when inducing anesthesia and rarely
irritation symptoms appear (16).
Sevoflurane is a new type of inhaled anesthesia with no irritation
of upper respiratory tract, low inhibition of respiration, rapid
recovery after surgery and short recovery time (17).
Pulmonary lobectomy often results in patients
breathing only through one lobe. Currently, hypoxic pulmonary
vasoconstriction of non-ventilated lung is an important factor
affecting arterial partial pressure of oxygen. Therefore, A-aDO2,
RI and Qs/Qt can be used as indicators for evaluating pulmonary
function of patients (18). In this
study, there was no significant difference in the clinical data of
patients (P>0.05), thus the data was comparable. The A-aDO2
level at T4 in sevoflurane group was significantly higher than that
in propofol group, the difference was statistically significant
(P<0.05). The RI level at T3 and T4 in sevoflurane group was
significantly higher than that in propofol group, and the
difference was statistically significant (P<0.05). The Qs/Qt
level at T2 and T3 and T4 in sevoflurane group was significantly
higher than that in propofol group, and the difference was
statistically significant (P<0.05). The MMP-9 level at T4 in the
sevoflurane group was significantly higher than that in the
propofol group, and the difference was statistically significant
(P<0.05). Combined with the above results, the lung injury of
patients undergoing lung cancer resection with propofol was lower
than that of sevoflurane, especially at T4. The level of A-aDO2,
RI, Qs/Qt and MMP-9 in the serum of the patients of the two groups
showed a trend of first increase and then decrease, but the level
of A-aDO2, Qs/Qt and MMP-9 in propofol group was significantly
lower than that in sevoflurane group. Findings of Tian et al
(19) were basically consistent with
ours, possibly because inhalation of sevoflurane released
inflammatory mediators and made inflammatory cytokines highly
expressed, leading to more severe lung injury in patients (20). Other studies have shown that
inhalation of anaesthesia may cause reversible pulmonary alveolar
fluid and a decrease of lung water clearance by affecting
biomembrane, leading to perioperative pulmonary edema and thus
affecting oxygen diffusion function (21). Animal experiments have shown that
inhalation of anaesthesia can inhibit type II alveolar epithelial
cells (AECII) from synthetizing pulmonary surfactant or decrease
their activities (22).
MMSE scale is one of the most important evaluation
indicators, which has the advantages of simple operation, high
efficiency and high reliability (23). Especially, lung cancer resection
impairs the cognitive function of patients to a certain extent.
Under the influence of surgical resection of lung tissue, lung
cancer resection can reduce the ratio of ventilation volume to
blood flow to a certain extent, resulting in hypoxemia and
impairment of cognitive function of patients (24). In this study, there was no significant
difference in MMSE score between sevoflurane and propofol group 1
day before surgery (P>0.05). The MMSE score in sevoflurane group
was significantly lower than that in propofol group 1 and 10 days
after surgery, and the difference was statistically significant
(P<0.05). Both sevoflurane and propofol groups had significantly
lower MMSE score of 1 and 10 days after surgery than that of day 1
before surgery. Both sevoflurane and propofol groups had
significantly higher MMSE score of 10 days after surgery than that
of 1 day after surgery, and the difference was statistically
significant (P<0.05). Combined with the above results, it showed
that the use of propofol was beneficial to the recovery of
cognitive function in patients, which was consistent with the
results of Jin et al (25).
The reason may be that sevoflurane can make increased permeability
of mitochondrial membrane, activity of oxygen free radical, and
enzyme concentration of inducing apoptosis, leading to
postoperative amnesia in patients (26).
However, there are still some limitations in this
study. We hope that in the future, the research can be further
deepened, and additional univariate analysis can be performed to
compare the relationship between each clinical parameter and the
A-aDO2, RI, MMP-9 and MMSE scores, or the multivariate analysis
involving each clinical parameter as an independent variable.
In conclusion, propofol has little effect on
pulmonary function and can reduce inflammation. Both sevoflurane
and propofol have an effect on cognitive function after lung cancer
resection. However, propofol can reduce cognitive impairment in
patients, and provide theoretical basis for better clinical choice
of anaesthesia.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
GW was responsible for the conception and design of
the work. GW and JL collected general data of patients. JG was
responsible for the treatment. GW and XZ analyzed observation
index, and drafted and revised the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
The Second Hospital of Dalian Medical University (Dalian, China).
Patients who participated in this research had complete clinical
data. The signed informed consents were obtained from the patients
or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Herbst RS, Heymach JV and Lippman SM: Lung
cancer. N Engl J Med. 359:1367–1380. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pope CA III, Burnett RT, Thun MJ, Calle
EE, Krewski D, Ito K and Thurston GD: Lung cancer, cardiopulmonary
mortality, and long-term exposure to fine particulate air
pollution. JAMA. 287:1132–1141. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shepherd FA, Rodrigues Pereira J, Ciuleanu
T, Tan EH, Hirsh V, Thongprasert S, Campos D, Maoleekoonpiroj S,
Smylie M, Martins R, et al; National Cancer Institute of Canada
Clinical Trials Group, . Erlotinib in previously treated
non-small-cell lung cancer. N Engl J Med. 353:123–132. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Engelman JA, Zejnullahu K, Mitsudomi T,
Song Y, Hyland C, Park JO, Lindeman N, Gale CM, Zhao X, Christensen
J, et al: MET amplification leads to gefitinib resistance in lung
cancer by activating ERBB3 signaling. Science. 316:1039–1043. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bekker A, Korban A and Esochaghi S:
Long-term cognitive decline in the elderly is not attributable to
surgery/anesthesia. Int J Anesthesiol Res. 5:490–493. 2017.
|
|
6
|
Shi HJ, Xue XH, Wang YL, Zhang WS, Wang ZS
and Yu AL: Effects of different anesthesia methods on cognitive
dysfunction after hip replacement operation in elder patients. Int
J Clin Exp Med. 8:3883–3888. 2015.PubMed/NCBI
|
|
7
|
Tian HT, Duan XH, Yang YF, Wang Y, Bai QL
and Zhang X: Effects of propofol or sevoflurane anesthesia on the
perioperative inflammatory response, pulmonary function and
cognitive function in patients receiving lung cancer resection. Eur
Rev Med Pharmacol Sci. 21:5515–5522. 2017.PubMed/NCBI
|
|
8
|
Hsu AT, Barrett CD, DeBusk GM, Ellson CD,
Gautam S, Talmor DS, Gallagher DC and Yaffe MB: Kinetics and role
of plasma matrix metalloproteinase-9 expression in acute lung
injury and the acute respiratory distress syndrome. Shock.
44:128–136. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shan JG, Xue S, Xu GX, Wang WJ, Lian F,
Liu S, Hu ZL and Huang RT: Effects of acupuncture-drug compound
anesthesia on perioperative inflammatory factors in patients
undergoing cardiac surgery. Zhongguo Zhenjiu. 30:585–588. 2010.(In
Chinese).
|
|
10
|
Luo YX, Huang B and Ying LI: Effects of
anesthetics on inflammatory response and lung function of patients
undergoing radical esophageal cancer surgery. Zhongguo Yiyuan
Ganranxue Zazhi. 4:877–879, (In Chinese).
|
|
11
|
Zhang L, Chen C, Wang L, Cheng G, Wu WW
and Li YH: Awakening from anesthesia using propofol or sevoflurane
withepidural block in radical surgery for senile gastric cancer.
Int J Clin Exp Med. 8:19412–19417. 2015.PubMed/NCBI
|
|
12
|
Zhao X, Jin YW, Li HB, Wang ZG, Feng H and
Feng C: Effects of maintaining intravenous infusion of remifentanil
or propofol on anesthesia and palinesthesia during anesthesia and
analepsia. Genet Mol Res. 13:2865–2872. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jin Y, Zhao X, Li H, Wang Z and Wang D:
Effects of sevoflurane and propofol on the inflammatory response
and pulmonary function of perioperative patients with one-lung
ventilation. Exp Ther Med. 6:781–785. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hu XL, Tang HH, Zhou ZG, Yin F and Liu WJ:
The effect of sevoflurane inhalation anesthesia only and propofol
total intravenous anesthesia on perioperative cytokine balance
inlung cancer patients. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi.
27:659–661. 2011.(In Chinese). PubMed/NCBI
|
|
15
|
Suemitsu R, Takeo S, Hamatake M, Morokuma
A, Suemori Y and Tanaka H: The results of surgery under general
anesthesia in patients with lung cancer. Surg Today. 41:60–66.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Qiu Q, Choi SW, Wong SS, Irwin MG and
Cheung CW: Effects of intra-operative maintenance of general
anaesthesia with propofol on postoperative pain outcomes - a
systematic review and meta-analysis. Anaesthesia. 71:1222–1233.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sorour K, Vyas PA, Raval DS, Donovan LM
and Vyas AA: Successful treatment of severe asthma exacerbation
with sevoflurane inhalation in the intensive care unit. J Anesth
Crit Care. 3:000922015.
|
|
18
|
Stiles BM, Poon A, Giambrone GP,
Gaber-Baylis LK, Wu X, Lee PC, Port JL, Paul S, Bhat AU, Zabih R,
et al: Incidence and factors associated with hospital readmission
after pulmonary lobectomy. Ann Thorac Surg. 101:434–443. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tian HT, Duan XH, Yang YF, Wang Y, Bai QL
and Zhang X: Effects of propofol or sevoflurane anesthesia on the
perioperative inflammatory response, pulmonary function and
cognitive function in patients receiving lung cancer resection. Eur
Rev Med Pharmacol Sci. 21:5515–5522. 2017.PubMed/NCBI
|
|
20
|
Dai AL, Fan LH, Zhang FJ, Yang MJ, Yu J,
Wang JK, Fang T, Chen G, Yu LN and Yan M: Effects of sevoflurane
preconditioning and postconditioning on rat myocardial stunning in
ischemic reperfusion injury. J Zhejiang Univ Sci B. 11:267–274.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Rezaiguia-Delclaux S, Jayr C, Luo DF,
Saïdi NE, Meignan M and Duvaldestin P: Halothane and isoflurane
decrease alveolar epithelial fluid clearance in rats.
Anesthesiology. 88:751–760. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Molliex S, Crestani B, Dureuil B, Bastin
J, Rolland C, Aubier M and Desmonts JM: Effects of halothane on
surfactant biosynthesis by rat alveolar type II cells in primary
culture. Anesthesiology. 81:668–676. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zarogoulidis P, Darwiche K, Tsakiridis K,
Teschler H, Yarmus L, Zarogoulidis K and Freitag L: Learning from
the cardiologists and developing eluting stents targeting the mTOR
pathway for pulmonary application; a future concept for tracheal
stenosis. J Mol Genet Med. 7:652013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhai HR, Yang XN, Nie Q, Liao RQ, Dong S,
Li W, Jiang BY, Yang JJ, Zhou Q, Tu HY, et al: Different dissecting
orders of the pulmonary bronchus and vessels during right upper
lobectomy are associated with surgical feasibility and
postoperative recovery for lung cancer patients. Chin J Cancer.
36:532017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Jin Y, Zhao X, Li H, Wang Z and Wang D:
Effects of sevoflurane and propofol on the inflammatory response
and pulmonary function of perioperative patients with one-lung
ventilation. Exp Ther Med. 6:781–785. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Liang H, Gu MN, Yang CX, Wang HB, Wen XJ
and Zhou QL: Sevoflurane inhibits proliferation, induces apoptosis,
and blocks cell cycle progression of lung carcinoma cells. Asian
Pac J Cancer Prev. 12:3415–3420. 2011.PubMed/NCBI
|