Introduction
Leukemia is a malignant clonal disease of the
heterogeneous hematopoietic system, and its pathogenesis originates
from the disordered differentiation process of hematopoietic stem
cells (1). Leukemia is divided into
lymphocytic leukemia and myeloid leukemia, mainly characterized by
malignant proliferation of lymphoid and myeloid hematopoietic stem
cells (2). The main manifestation of
the body is the disorder in differentiation and apoptosis of
hematopoietic stem cells. Primary and immature leukemia cells
accumulate in the body after malignant proliferation, affecting
normal hematopoietic function, and abnormal cells will be spread to
numerous tissues and organs throughout the body fluid. Hence,
patients with clinical leukemia often have anemia, hemorrhage,
infection and extramedullary infiltration (3–5). The
main cause of hemorrhage is the destruction of platelets caused by
bone marrow hematopoietic dysfunction and chemotherapy drug injury,
leading to a large number of platelet reduction and death of
patients when serious hemorrhage cannot be timely controlled
(6). Some literature has reported
that the average life cycle of leukemia patients is short, and the
treatment is difficult. It is necessary to control the disease
development through timely treatment. In recent years, chemotherapy
is still the main treatment method for leukemia patients. Although
the remission rate of leukemia has been significantly improved, the
clinical efficacy is not ideal. There are problems such as
increased complications, high recurrence rate and reduced immunity
of patients, and the problem of thrombocytopenia has not been
fundamentally solved (7,8).
In order to prevent death caused by excessive blood
loss in patients with leukemia, platelet decline can be prevented
from the perspective of controlling the normal operation of blood
in the body. In this case, patients can be treated with platelet
transfusion repeatedly. Moreover, with the progress of medical
technology, platelet transfusion therapy is gradually getting
mature in the treatment of leukemia patients, but this way does not
have a significant effect on all patients. The incidence of
ineffective platelet transfusion continues to rise, and even leads
to death in severe cases. These problems remain difficult for
clinical researchers and executive physicians (9). It has been reported that interleukin-11
(IL-11) is a kind of cytokine that plays a multipotent role in
various cells including macrophages and T cells, mainly promoting
the production of megakaryocytes and platelets, anti-inflammatory
and other functions (10). At
present, it is known that the intracellular signaling chain of
IL-11 is mainly gp130, which exists in the body in two modes:
humoral and model (11). Therefore,
this study investigated how to improve the efficacy of platelet
transfusion therapy and reduce the risk factors of ineffective
transfusion, so as to achieve the goal of radical treatment of
leukemia patients.
Materials and methods
General data
A total of 105 leukemia patients admitted to The
First Affiliated Hospital of Bengbu Medical College from August
2016 to November 2018 were selected as research subjects. Among
them, 49 cases of patients received transfusion of apheresis
platelet suspension, and were group A. Fifty-six cases of patients
received mixed multi-person platelet suspension, and were group B.
The study was approved by the Ethics Committee of The First
Affiliated Hospital of Bengbu Medical College (Bengbu, China).
Signed informed consents were obtained from the patients and/or the
guardians.
Inclusion and exclusion criteria
Inclusion criteria were as follows: Patients who
were diagnosed with leukemia by pathological features and met the
Diagnostic Criteria for Leukemia (12). Patients who met all platelet
transfusion indexes (13). The
exclusion criteria were as follows: Patients with incomplete
clinical data. Patients with other organ solid lesion. Patients
with hepatic and renal insufficiency. Patients with transfusion
history before transfusion. Patients with cognitive impairment or
communication disorder. The patients and their families agreed to
participate in the experiment and signed informed consents.
Experimental materials
Platelets were from the downtown blood station, and
each pocket of platelets was treated as one quantity (10 units,
200–250 ml). The average number of platelets in each pocket was
2.5×1011, red blood cell count <8.0×1011,
and white blood cell count <5.0×1011. IL-11 antibody
was from Shanghai Hushi medicine technology Co., Ltd. Soluble
glycoprotein 130 (sgp130) antibody was from Shanghai Kanglang
Biotechnology Co., Ltd. ELISA chromogenic reagent was purchased
from Beijing Biotss Biotechnology Co., Ltd. and the microplate
reader was from Jinan Olabo Scientific Instrument Co., Ltd.
Test methods
Platelet transfusion method
The patients received platelet prophylactic
transfusion. Blood typing of patients was checked and recorded, and
blood matching was performed before transfusion. Transfusion was
conducted strictly in accordance with the ABO homologous blood
transfusion standard. During transfusion, patients tolerance was
observed to timely adjust the speed of transfusion. The standard
amount of adult transfusion was one curative dose of platelet
suspension (10 units, 200–250 ml). Dexamethasone (5 mg) intravenous
injection was used to prevent adverse reactions during transfusion,
and the transfusion was completed within 30 min on average.
Furthermore, platelet transfusion was required to be finished 48 h
after collection.
Detection methods of serum IL-11 and
sgp130 levels
After two consecutive full platelet transfusions,
test solution (100 µl) of serum samples of the two groups was added
to 96-well plates. The standard wells and blank wells were set,
incubated at 37°C for 120 min, and then 400 ml washing solution was
added for washing three times. IL-11 (6 ml) goat anti-human
antibody were added, incubated at 37°C for 120 min, and washed
three times. Chromogenic agent (150 µl) were added, developed at
37°C for 30 min. A total of 50 µl was taken out and mixed, and
placed at 500 nm wavelength to measure and record the average
optical density value of each well. Detection of sgp130 level was
also performed in strict accordance with the ELISA kit instructions
and the above operations.
Observational indexes
i) Percentage plate recovery (PPR) and corrected
count increment (CCI) were compared between patients in the two
groups before and after platelet transfusion. ii) Serum IL-11 and
sgp130 levels were compared between patients in the two groups
before and after platelet transfusion. iii) Correlation of PPR and
CCI with IL-11 and sgp130 levels in leukemia patients after
transfusion treatment was analyzed. iv) Patients were divided into
an effective group and an ineffective group in accordance with
clinical efficacy of patients, and logistic regression was used to
analyze the related risk factors of ineffective transfusion of the
patients.
Statistical analysis
SPSS 19.0 statistical software (Beijing Qingsi
technology Co., Ltd.) was used for statistical analysis of the
experimental data. Enumeration data were qualified by Chi-square
test. Measurement data were expressed as mean ± standard deviation.
t-test was used for comparison between the two groups, and paired
t-test was used between the two groups before and after
transfusion. Pearson's was used for correlation analysis and
Multivariate logistic regression to analyze the risk factors
affecting the ineffective transfusion of leukemia patients.
GraphPad Prism 8 was employed to draw the illustrations, and
P<0.05 was considered statistically significant.
Results
Comparison of general data
There were no significant differences between the
two groups in sex, age, disease course, anemia, infection and fever
(P>0.05) (Table I).
 | Table I.Comparison of general data of patients
in the two groups. |
Table I.
Comparison of general data of patients
in the two groups.
| Factors | Group A (n=49) | Group B (n=56) | t/χ2
value | P-value |
|---|
| Sex (n) |
|
| 0.006 | 0.938 |
| Male | 24 (48.98) | 27 (48.21) |
|
|
|
Female | 25 (51.02) | 29 (51.79) |
|
|
| Age (years) | 57.35±5.45 | 57.83±5.62 | 0.443 | 0.659 |
| Disease course
(month) | 11.43±2.45 | 11.51±2.47 | 0.166 | 0.868 |
| Anemia (n) |
|
| 0.207 | 0.650 |
| With | 18 (36.73) | 23 (41.07) |
|
|
|
Without | 31 (63.27) | 33 (58.93) |
|
|
| Hemorrhage (n) |
|
| 0.223 | 0.637 |
| With | 12 (24.49) | 16 (28.57) |
|
|
|
Without | 37 (75.51) | 40 (71.43) |
|
|
| Infection (n) |
|
| 0.094 | 0.760 |
| With | 11 (22.45) | 14 (25.00) |
|
|
|
Without | 38 (77.55) | 42 (75.00) |
|
|
| Fever (n) |
|
| 0.016 | 0.898 |
| With | 10 (20.41) | 12 (21.43) |
|
|
|
Without | 39 (79.59) | 44 (78.57) |
|
|
| Skeletal arthralgia
(n) |
|
| 0.371 | 0.543 |
| With | 9 (18.37) | 13 (23.21) |
|
|
|
Without | 40 (81.63) | 43 (76.79) |
|
|
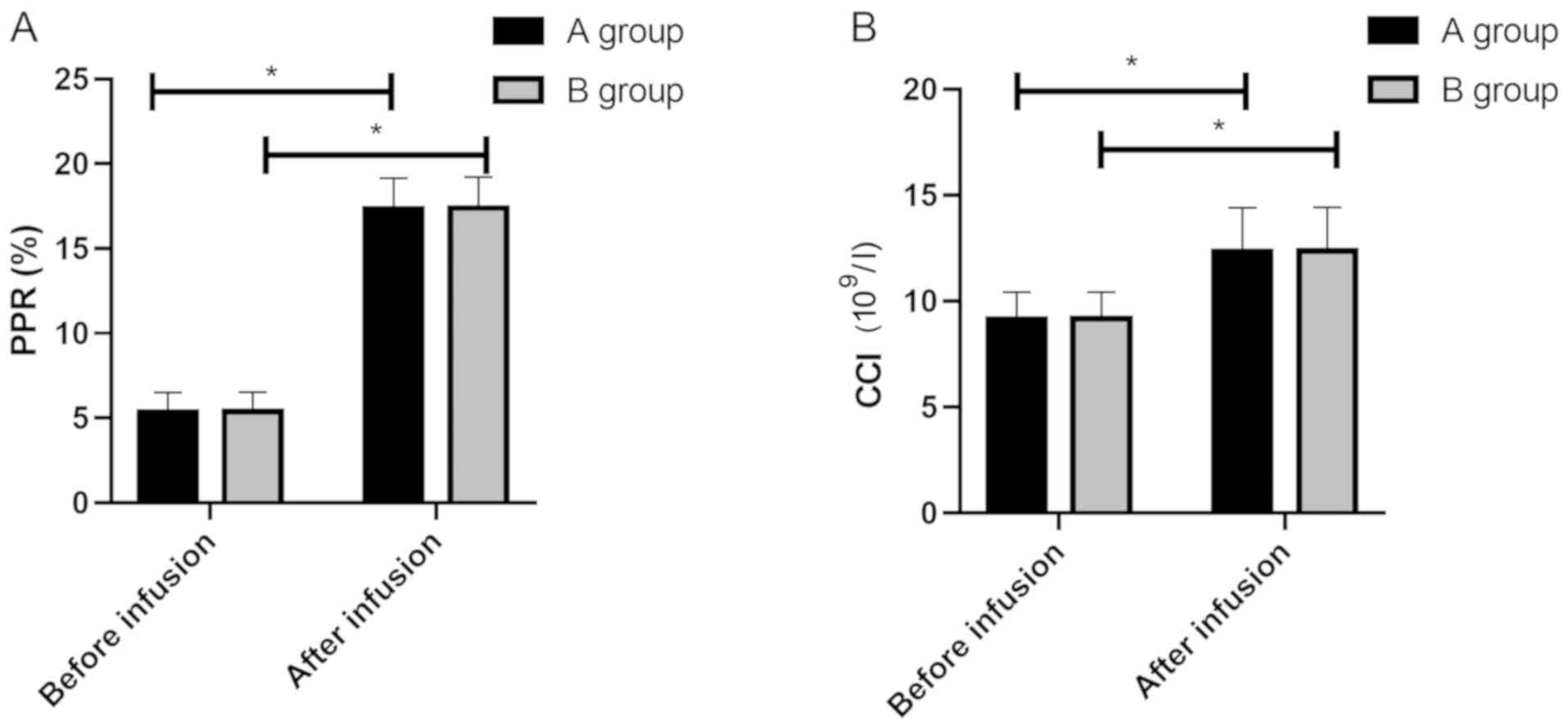
Comparison of PPR and CCI of patients
between the two groups before and after platelet transfusion
There were no significant differences in PPR and CCI
between the two groups before transfusion (P>0.05). There were
no significant differences in PPR between group A (17.34±1.82) and
group B (17.39±1.83) after transfusion, and no significant
differences in CCI between group A (12.32±2.09) and group B
(12.36±2.07) after transfusion (P>0.05). However, the factors in
both groups were significantly higher than those before
transfusion, with statistically significant differences (P<0.05)
(Fig. 1).
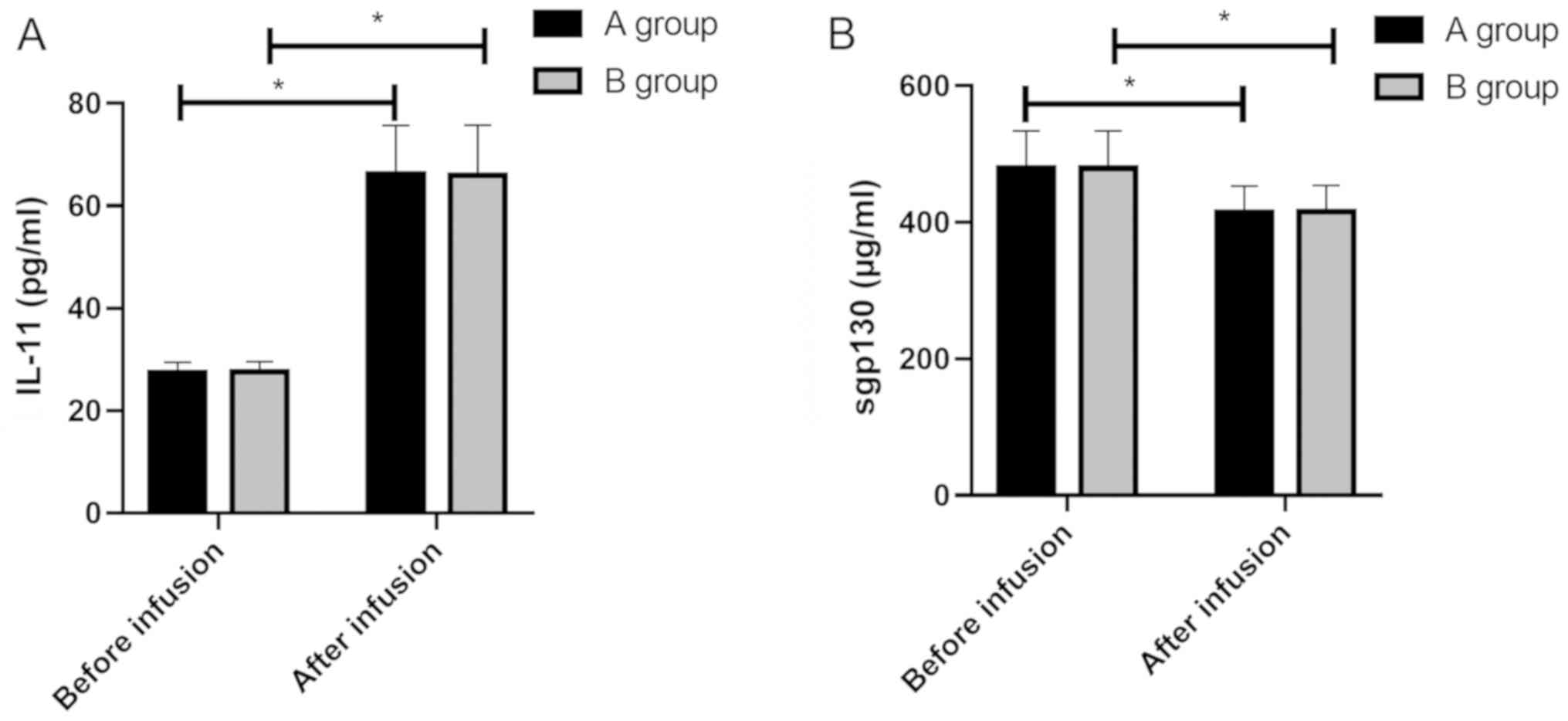
Comparison of IL-11 and sgp130 of
patients between the two groups before and after platelet
transfusion
There were no significant differences in IL-11 and
spg130 between the two groups before transfusion (P>0.05). There
were no significant differences in IL-11 between group A
(66.14±2.08) and group B (65.98±9.76) after transfusion, and no
differences in spg130 between group A (414.32±39.09) and group B
(415.36±38.94) after transfusion (P>0.05). The factors in both
groups were significantly higher than those before transfusion,
with statistically significant differences (P<0.05) (Fig. 2).
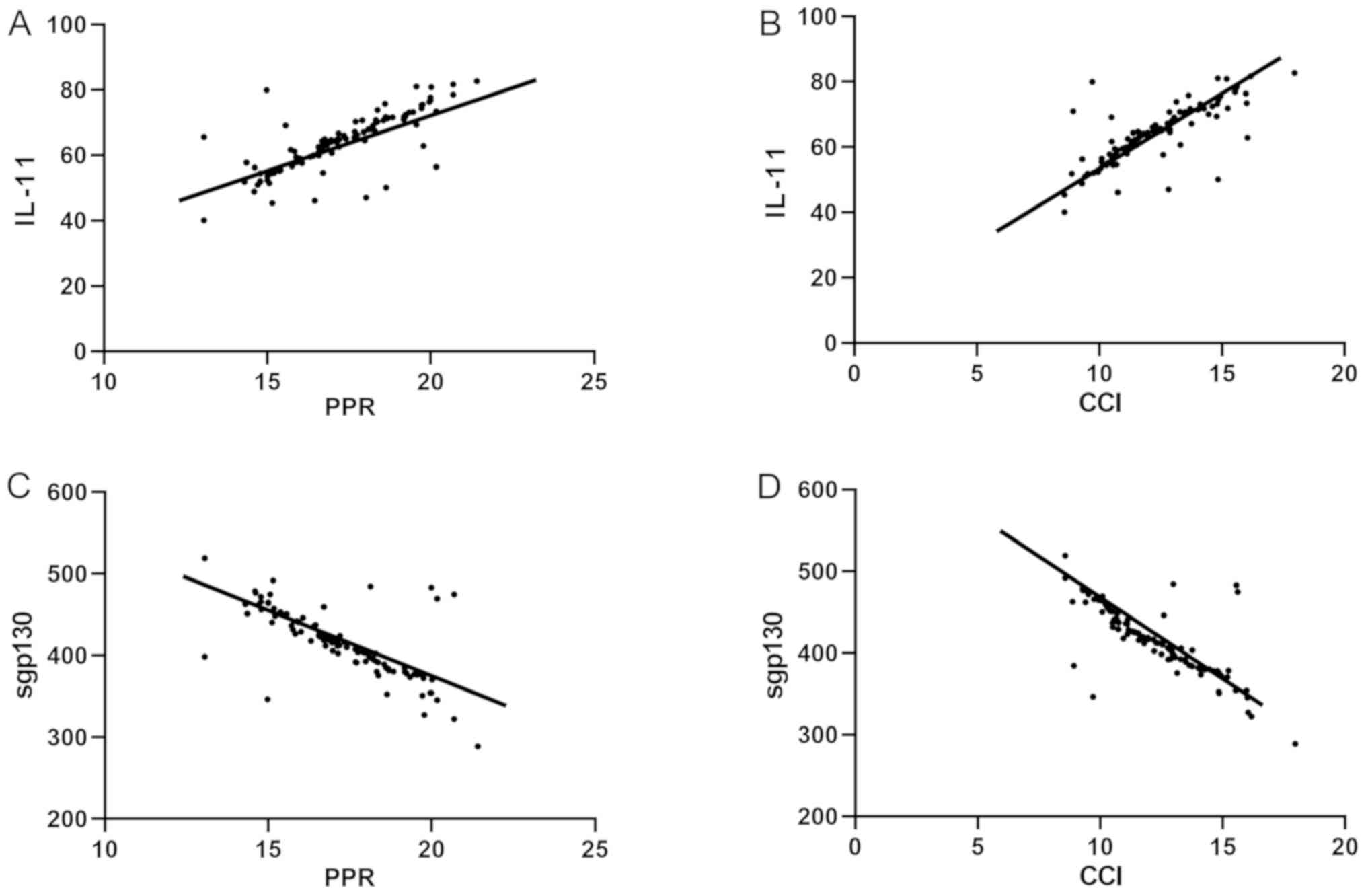
Correlation analysis of PPR and CCI
with serum IL-11 and sgp130 levels in leukemia patients
Pearson's correlation analysis showed that PPR in
leukemia patients was positively correlated with serum IL-11 level
(r=0.7693, P<0.001), CCI in leukemia patients was positively
correlated with serum IL-11 level (r=0.7760, P<0.001), PPR in
leukemia patients was negatively correlated with serum sgp130 level
(r=−0.7086, P<0.001), and CCI in leukemia patients was
negatively correlated with serum sgp130 level (r=−0.7733,
P<0.001) (Fig. 3).
Univariate analysis of ineffective
transfusion of patients
Patients were divided into an effective treatment
group (n=83) and an ineffective group (n=22) according to the
clinical efficacy. The clinical data of patients in both the
effective group and ineffective group were collected for univariate
analysis. There were no significant differences in age, sex,
antibiotic use, or blood sampling method (P>0.05), but there
were differences in number of transfusion, fever, infection,
hemorrhage, and splenomegaly (P<0.05) (Table II).
 | Table II.Univariate analysis. |
Table II.
Univariate analysis.
| Clinicopathologic
features | Effective group
(n=83) | Ineffective group
(n=22) | χ2
value | P-value |
|---|
| Age (years) |
|
| 0.108 | 0.742 |
|
<57 | 41 (49.40) | 10 (45.45) |
|
|
| ≥57 | 42 (50.60) | 12 (54.55) |
|
|
| Sex (n) |
|
| 0.023 | 0.880 |
| Male | 40 (48.19) | 11 (50.00) |
|
|
|
Female | 43 (51.81) | 11 (50.00) |
|
|
| Transfusion frequency
(n) |
|
| 12.373 | 0.006 |
| 1 | 36 (43.37) | 3 (13.64) |
|
|
| 2–5 | 24 (28.92) | 5 (22.73) |
|
|
| 6–9 | 14 (16.87) | 6 (27.27) |
|
|
| ≥10 | 9 (10.84) | 8 (36.36) |
|
|
| Fever (n) |
|
| 6.693 | 0.010 |
| With | 13 (15.66) | 9 (40.91) |
|
|
|
Without | 70 (84.34) | 13 (59.09) |
|
|
| Hemorrhage (n) |
|
| 7.748 | 0.005 |
| With | 17 (20.48) | 11 (50.00) |
|
|
|
Without | 66 (79.52) | 11 (50.00) |
|
|
| Splenomegaly (n) |
|
| 4.220 | 0.040 |
| With | 11 (13.25) | 7 (31.82) |
|
|
|
Without | 72 (86.75) | 15 (68.18) |
|
|
| Infection (n) |
|
| 19.101 | <0.001 |
|
With | 12 (14.46) | 13 (59.09) |
|
|
|
Without | 71 (85.54) | 9 (40.91) |
|
|
| Antibiotic use
(number) |
|
| 0.315 | 0.575 |
|
With | 25 (30.12) | 8 (36.36) |
|
|
|
Without | 58 (69.88) | 14 (63.64) |
|
|
| Blood sampling
methods |
|
| 0.016 | 0.898 |
|
Apheresis platelet | 39 (46.99) | 10 (45.45) |
|
|
| Mixed
multi-person platelet | 44 (53.01) | 12 (54.55) |
|
|
| Anemia
(number) |
|
| 0.041 | 0.841 |
|
With | 32 (38.55) | 9 (40.91) |
|
|
|
Without | 51 (61.45) | 13 (59.09) |
|
|
| Bone pain |
|
| 0.053 | 0.818 |
|
With | 17 (20.48) | 5 (22.73) |
|
|
|
Without | 66 (79.52) | 17 (77.27) |
|
|
Multivariate analysis of
treatment
Indicators with differences in univariate analysis
were included in the assignments (Table III). Multivariate logistic
regression analysis was performed, the results showed that
transfusion frequency, hemorrhage and splenomegaly were not related
risk factors for ineffective transfusion, while fever (OR, 0.382;
95% CI, 0.183–0.972) and infection (OR, 0.367; 95% CI, 0.140–0.956)
were related risk factors for ineffective transfusion (Table IV).
 | Table III.Assignments. |
Table III.
Assignments.
| Factors | Assignment |
|---|
| Transfusion
frequency (n) | One time=0, 2–5
times=1, 6–9 times=2, ≥10 times=3 |
| Fever | With=1,
without=0 |
| Hemorrhage | With=1,
without=0 |
| Splenomegaly | With=1,
without=0 |
| Infection | With=1,
without=0 |
| Transfusion | Effective=1,
ineffective=0 |
 | Table IV.Multivariate analysis. |
Table IV.
Multivariate analysis.
|
|
|
|
|
|
| 95% CI Of Exp
(B) |
|---|
|
|
|
|
|
|
|
|
|---|
| Factors | B | SE | Wals | Sig. | Exp (B) | Lower limit | Upper limit |
|---|
| Transfusion
frequency | 0.423 | 0.297 | 2.047 | 0.157 | 1.526 | 0.867 | 2.724 |
| Fever | −0.997 | 0.396 | 4.623 | 0.039 | 0.382 | 0.183 | 0.972 |
| Hemorrhage | 0.372 | 0.284 | 1.783 | 0.185 | 1.460 | 0.841 | 2.589 |
| Splenomegaly | −1.118 | 0.604 | 3.458 | 0.067 | 0.324 | 0.148 | 0.957 |
| Infection | −0.994 | 0.487 | 4.245 | 0.037 | 0.367 | 0.140 | 0.956 |
Discussion
The process of infiltration of leukemia cells in
patients with leukemia in extramedullary and extramedullary
lymphocytes includes leukemia cells spilling from the bone marrow
and lymphocytes to the peripheral blood, and migrating to the
tissues and organs suitable for their growth. It involves complex
pathological process such as leukocyte chemotaxis, adhesion,
migration and degradation of vascular endothelial cells (14–16). In
addition, some studies have shown that both the abnormal function
and the decrease in the number of platelets in patients with
leukemia would have secondary onset to the hemorrhage of the
patient's body (17). Platelet is
the most influential clotting factor in the human body, which can
significantly improve the condition of hemorrhage caused by
platelet dysfunction or decreased platelet transfusion in patients
with blood diseases, and is an effective treatment method (18). IL-11 can bind to IL-11Ra, a binding
chain of cell-surface specific receptor-ligand, and then connect to
gp130 (a signaling chain), to activate the biological function of
IL-11 and mediate inflammatory response (19). sgp130 is a receptor and signal
transmitter shared by IL-11 and leukemia suppressor factors. sgp130
is one of the soluble proteins in various forms and is related to
the prognosis of leukemia (20).
This study mainly investigated the changes in platelet count and
the expression of IL-11 and sgp130 in patients with leukemia after
platelet transfusion, and analyzed their correlation, to explore
the influencing factors of ineffective platelet transfusion.
PPR and CCI were studied in two groups of patients
and it was found that PPR and CCI in both groups were significantly
higher after transfusion than before transfusion. This indicated
that the platelet count in the two groups was effectively increased
after different blood sampling methods. Some studies have shown
that the disorder of the body's internal environment and the
production and release of platelet antibodies in patients with
leukemia would affect the maturation of platelets and cause damage
to them, leading to a decrease in the number of platelets in
patients (21). Platelet transfusion
therapy can enhance the intracellular platelet density of patients
through matching of blood after transfusion, to prevent the
deterioration of patients' condition caused by hemorrhage (22). In clinical practice, CCI, PPR and
patients' hemorrhage status were used as the criteria to assess the
efficacy of platelet transfusion (23). It is concluded that platelet
transfusion can effectively control the hemorrhage rate of leukemia
patients, and different blood sampling methods have little effect
on the transfusion treatment. This study on IL-11 and sgp130 levels
showed that IL-11 levels increased while sgp130 levels decreased in
the two groups after transfusion, but there were no significant
differences in IL-11 and sgp130 levels between group A and group B
after transfusion. Previous studies have shown that (24,25)
membrane gp130 is involved in mediating the platelet production,
inflammatory response and other biological activities of IL-6
family cytokines. sgp130, as a negative regulator, blocks their
biological effects and is involved in immune response, hemopoiesis,
inflammation, endocrine and nervous system functions. The
literature is consistent with our results to some extent. The
anti-inflammatory mechanism of the body is stimulated by the
increase in the number of platelets, and the same target causes the
IL-11 level to rise and the gp130 level to decrease under the
inflammatory action. Pearson's correlation analysis was conducted
to further study the relationship of IL-11 and sgp130 with changes
of platelet number after platelet transfusion in leukemia patients.
The results showed that serum IL-11 level in leukemia patients was
positively correlated with PPR and CCI, while serum sgp130 level in
leukemia patients was negatively correlated with PPR and CCI. It
further indicates that with the treatment of platelet transfusion,
the number of platelets in the body can be effectively increased,
which has a good effect on improving the inflammatory response and
hemopoiesis in the body. Previous literature (26) have reported that the failure of
long-term platelet transfusion therapy in clinical practice is
particularly prominent, and the clinical efficacy on hemorrhage of
patients with blood diseases is poor, and the related factors
causing ineffective transfusion have become difficult points and
concerns of the academic community. Univariate analysis in this
study showed that there were differences in transfusion frequency,
fever, infection and splenomegaly between the effective group and
ineffective group. From the perspective of efficacy, the treatment
success rate decreased with the increase of transfusion times.
However, the results of multivariate logistic regression analysis
in this study showed that transfusion frequency was not considered
as a risk factor for ineffective transfusion, it was speculated
that the transfusion of platelet samples and the interval time
between transfusions in this study might have influenced the
results. Previous studies (27) have
shown that with the increase of transfusion times, platelet
antibodies will develop in patients, hindering the efficacy of
platelet transfusion. The results may be different from the effect
of transfusion on the number of transfusion in patients with
different physical conditions. Splenomegaly and hemorrhage will
cause platelet consumption and loss, affecting the efficacy of
platelet transfusion (28,29). In the results of multivariate
logistic regression analysis of this study, however, the above two
factors were not considered as risk factors for ineffective
transfusion. It was analyzed that this was a confounding factor as
well as transfusion frequency, which may be related to the fact
that the pathological manifestations of patients with splenomegaly
were not significant and the cause of hemorrhage was not leukemic
immune system damage. Multivariate logistic regression analysis
showed that fever and infection were independent risk factors
leading to ineffective transfusion. Previous literature (30) have indicated that platelet of
patients with hematological system diseases and fever exposure to
recessive antigen would absorb antibody, which may lead to
accelerated circulation in patients. When circulation is performed
to the reticuloendothelial system, platelet survival time is
shortened and depletion is increased, affecting the effectiveness
of platelet transfusion.
In conclusion, platelet transfusion can
significantly increase the number of platelets after treatment and
improve the hemorrhage of patients with leukemia. In this study, it
was found that infection and fever were the influencing factors
affecting the efficacy of transfusion. Patients should be
transfused after the basic clinical inflammatory symptoms are
controlled and the causes of ineffective transfusion should be
identified and solved timely.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
LC and ZG conceived and designed the study. LC, HZ,
BG and ZG were responsible for the collection, analysis and
interpretation of the data. HZ drafted the manuscript. BG revised
the manuscript critically for important intellectual content. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
The First Affiliated Hospital of Bengbu Medical College (Bengbu,
China). Signed informed consents were obtained from the patients
and/or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Maertens J, Marchetti O, Herbrecht R,
Cornely OA, Flückiger U, Frêre P, Gachot B, Heinz WJ, Lass-Flörl C,
Ribaud P, et al Third European Conference on Infections in
Leukemia, : European guidelines for antifungal management in
leukemia and hematopoietic stem cell transplant recipients: Summary
of the ECIL 3–2009 update. Bone Marrow Transplant. 46:709–718.
2011.PubMed/NCBI
|
|
2
|
Takami A, Yano S, Yokoyama H, Kuwatsuka Y,
Yamaguchi T, Kanda Y, Morishima Y, Fukuda T, Miyazaki Y, Nakamae H,
et al: Donor lymphocyte infusion for the treatment of relapsed
acute myeloid leukemia after allogeneic hematopoietic stem cell
transplantation: A retrospective analysis by the Adult Acute
Myeloid Leukemia Working Group of the Japan Society for
Hematopoietic Cell Transplantation. Biol Blood Marrow Transplant.
20:1785–1790. 2014.PubMed/NCBI
|
|
3
|
Roe JS, Mercan F, Rivera K, Pappin DJ and
Vakoc CR: BET bromodomain inhibition suppresses the function of
hematopoietic transcription factors in acute myeloid leukemia. Mol
Cell. 58:1028–1039. 2015.PubMed/NCBI
|
|
4
|
Liu W and Freedman HI: A
reaction-diffusion model of leukemia treatment by chemotherapy. Can
Appl Math Q. 11:249–282. 2003.
|
|
5
|
Jiang L, Yu G, Meng W, Wang Z, Meng F and
Ma W: Overexpression of amyloid precursor protein in acute myeloid
leukemia enhances extramedullary infiltration by MMP-2. Tumour
Biol. 34:629–636. 2013.PubMed/NCBI
|
|
6
|
Houwerzijl EJ, Blom NR, van der Want JJ,
Louwes H, Esselink MT, Smit JW, Vellenga E and de Wolf JT:
Increased peripheral platelet destruction and caspase-3-independent
programmed cell death of bone marrow megakaryocytes in
myelodysplastic patients. Blood. 105:3472–3479. 2005.PubMed/NCBI
|
|
7
|
Frinc I, Dima D, Chitic M, Berce C,
Berindan-Neagoe I, Tat T, Tanase A, Tomuleasa C and Bojan A:
Transthoracic ultrasonography for the follow-up of a chronic
lymphocytic leukemia patient with chemotherapy-induced
immunosuppression prior to allogeneic stem cell transplantation. A
case report. Med Ultrason. 19:330–332. 2017.PubMed/NCBI
|
|
8
|
Just Vinholt P, Højrup Knudsen G, Sperling
S, Frederiksen H and Nielsen C: Platelet function tests predict
bleeding in patients with acute myeloid leukemia and
thrombocytopenia. Am J Hematol. 94:891–901. 2019.PubMed/NCBI
|
|
9
|
Apelseth TO, Tor Hervig MD and Øystein
Bruserud MD: Platelet transfusion in acute leukemia patients with
severe chemotherapy-induced thrombocytopenia: The possible
importance of hemoglobin levels and red blood cell transfusions for
evaluation of clinical effects of transfusion. Transfusion.
50:2505–2506. 2010.
|
|
10
|
Wang Q, Du X, Yang M, Xiao S, Cao J, Song
J and Wang L: LncRNA ZEB1-AS1 contributes to STAT3 activation by
associating with IL-11 in B-lymphoblastic leukemia. Biotechnol
Lett. 39:1801–1810. 2017.PubMed/NCBI
|
|
11
|
Richards PJ, Nowell MA, Horiuchi S,
McLoughlin RM, Fielding CA, Grau S, Yamamoto N, Ehrmann M,
Rose-John S, Williams AS, et al: Functional characterization of a
soluble gp130 isoform and its therapeutic capacity in an
experimental model of inflammatory arthritis. Arthritis Rheum.
54:1662–1672. 2006.PubMed/NCBI
|
|
12
|
Mason J and Griffiths M: Molecular
diagnosis of leukemia. Expert Rev Mol Diagn. 12:511–526.
2012.PubMed/NCBI
|
|
13
|
Gmür J, Burger J, Schanz U, Fehr J and
Schaffner A: Safety of stringent prophylactic platelet transfusion
policy for patients with acute leukaemia. Lancet. 338:1223–1226.
1991.PubMed/NCBI
|
|
14
|
Hasegawa H, Nomura T, Kohno M, Tateishi N,
Suzuki Y, Maeda N, Fujisawa R, Yoshie O and Fujita S: Increased
chemokine receptor CCR7/EBI1 expression enhances the infiltration
of lymphoid organs by adult T-cell leukemia cells. Blood. 95:30–38.
2000.PubMed/NCBI
|
|
15
|
Makaryus AN, Tung F, Liu W, Mangion J and
Kort S: Extensive neoplastic cardiac infiltration in a patient with
acute myelogenous leukemia: Role of echocardiography.
Echocardiography. 20:539–544. 2003.PubMed/NCBI
|
|
16
|
Li Y, Azuma A, Takahashi S, Usuki J,
Matsuda K, Aoyama A and Kudoh S: Fourteen-membered ring macrolides
inhibit vascular cell adhesion molecule 1 messenger RNA induction
and leukocyte migration: Role in preventing lung injury and
fibrosis in bleomycin-challenged mice. Chest. 122:2137–2145.
2002.PubMed/NCBI
|
|
17
|
Noguchi T, Ikeda K, Yamamoto K, Ashiba A,
Yoshida J, Munemasa M, Takenaka K, Shinagawa K, Ishimaru F, Yoshino
T, et al: Severe bleeding tendency caused by leukemic infiltration
and destruction of vascular walls in chronic neutrophilic leukemia.
Int J Hematol. 74:437–441. 2001.PubMed/NCBI
|
|
18
|
Li JJ, Chen BA, Huang CY, Li CP, Shi GY,
Xiao JY, Ding JH, Gao C, Sun YY, Wan J, et al: Test of activated
plasma clotting time to assess efficacy of platelet transfusion.
Exp Hematol. 15:108–111. 2007.
|
|
19
|
Balic JJ, Garbers C, Rose-John S, Yu L and
Jenkins BJ: Interleukin-11-driven gastric tumourigenesis is
independent of trans-signalling. Cytokine. 92:118–123.
2017.PubMed/NCBI
|
|
20
|
Zhang QR, Wu DP and Miao M: Level and
clinical value of the plasma IL-11 and soluble gp130 in the
patients with acute leukemia during the treatment of the induced
remission. Zhongguo Shiyong Neike Zazhi. 17:1376–1378. 2007.(In
Chinese).
|
|
21
|
Yan M and Jurasz P: The role of platelets
in the tumor microenvironment: From solid tumors to leukemia.
Biochim Biophys Acta. 1863:392–400. 2016.PubMed/NCBI
|
|
22
|
Ishikura H and Kitamura T: Trauma-induced
coagulopathy and critical bleeding: The role of plasma and platelet
transfusion. J Intensive Care. 5:22017.
|
|
23
|
Julmy F, Ammann RA, Mansouri Taleghani B,
Fontana S, Hirt A and Leibundgut K: Effects of high-yield
thrombocytapheresis on the quality of platelet products.
Transfusion. 48:442–450. 2008.PubMed/NCBI
|
|
24
|
Wolf J, Waetzig GH, Chalaris A, Reinheimer
TM, Wege H, Rose-John S and Garbers C: Different soluble forms of
the interleukin-6 family signal transducer gp130 fine-tune the
blockade of interleukin-6 Trans-signaling. J Biol Chem.
291:16186–16196. 2016.PubMed/NCBI
|
|
25
|
Lemmers A, Gustot T, Durnez A, Evrard S,
Moreno C, Quertinmont E, Vercruysse V, Demetter P, Franchimont D,
Le Moine O, et al: An inhibitor of interleukin-6 trans-signalling,
sgp130, contributes to impaired acute phase response in human
chronic liver disease. Clin Exp Immunol. 156:518–527.
2009.PubMed/NCBI
|
|
26
|
Gerstner JB, Smith MJ, Davis KD, Cimo PL
and Aster RH: Post-transfusion purpura: Therapeutic failure of
PlAl-negative platelet transfusion. Am J Hematol. 6:71–75.
1979.PubMed/NCBI
|
|
27
|
Tzadok S, Gurevich A, Inbal A, Bar-Natan
M, Wolaj O and Raanani P: Continuous platelet transfusion increases
platelet increment in refractory hemato-oncological patients. A
Single Center Experience. Blood. 124:2888. 2014.
|
|
28
|
Yates SG and Sarode R: Is platelet
transfusion necessary in cirrhotic patients with splenomegaly?
Liver Int. 34:164–165. 2014.PubMed/NCBI
|
|
29
|
Hennewig U, Laws HJ, Eisert S and Göbel U:
Bleeding and surgery in children with Glanzmann thrombasthenia with
and without the use of recombinant factor VIIa. Klin Padiatr.
217:365–370. 2005.PubMed/NCBI
|
|
30
|
Beardsley DS, Chen BG and Kruglov O: A
Mechanism for exacerbation of chronic ITP by infection: Toll-like
receptor 4 (TLR4) activation enhances antibody-mediated platelet
phagocytosis by human macrophages. Blood. 108:4802006.PubMed/NCBI
|