Introduction
The G-protein-coupled receptor (GPCR) family is the
largest family in the human genome and the most widely distributed
membrane protein receptor in humans. The ovarian cancer GPCR 1
(OGR1) subfamily is a family of proton-sensing receptor proteins.
The four members of the proton-activated GPCR family, GPCR 1
(OGR1), GPCR 4 (GPR4), T-cell death-associated gene 8 and GPCR 2A
have been also identified as receptors of some specific lipid
molecules, including sphingosine phosphoryl choline and
lysophosphatidyl choline (1–4).
GPR4 is overexpressed in lung tissues, with lower
expression in the kidney, heart, skeletal muscle and pancreatic
tissues (5). GPR4 was firstly
described as a proton-sensing receptor in 2003 (1); it was found to be involved in a variety
of biological processes (1),
including the inhibition of cell apoptosis, the promotion of cell
proliferation and metastasis by initiating different signaling
pathways, and the induction of cytosolic cyclic adenosine
monophosphate (cAMP) in cells by recognizing and accepting protons
via its unique extracellular histidine residues (6). Additionally, GPR4 plays an important
role in angiogenesis, and the proangiogenic effect is independent
of its ligand-hemolytic phospholipids. In previous studies, it was
found that GPR4 induced proliferation and migration of vascular
endothelial cells (ECs), as well as angiogenesis (7). Following GPR4-knockout, vascular ECs
had lower survival, decreased migration and were unable to form
tubular structures. These effects were reversed when GPR4 gene was
re-expressed (8). These findings
suggest that GPR4 plays an important role in angiogenesis.
Furthermore, certain studies have demonstrated the ability of GPR4
to induce angiogenesis in ovarian cancer and squamous cell
carcinoma of the head and neck (SCCHN) (9,10). In
ovarian cancer, the expression level of GPR4 is positively
correlated with the microvessel density (MVD) of vascular ECs,
which is not observed in benign ovarian tissues (10). In SCCHN, GPR4 promotes angiogenesis
by inducing p38, which mediates secretion of vascular endothelial
growth factor A, interleukin (IL)-6 and IL-8 (9). In mice with conditional loss of GPR4
expression, the expression level of vascular endothelial growth
factor (VEGF) receptor 2 was decreased, with suppressed
angiogenesis that remained low following re-expression of VEGF
(11). Furthermore, GPR4-deficient
embryos and neonates had a high perinatal mortality rate (12). Moreover, some GPR4-null embryos and
neonates presented with a tendency for spontaneous bleeding. In
addition, a proportion of subcutaneous blood vessels became dilated
and tortuous with defective vascular smooth muscle cell coverage,
potentially resulting in impaired vascular stability and abnormal
bleeding (12).
Sin et al (13) found that GPR4 was an oncogene that
was overexpressed in human cancer tissues of the breast, ovary,
colon, liver and kidney. Mouse NIH3T3 fibroblasts transfected with
GPR4, resulted in increased survival at low serum concentrations
(13). Furthermore, the neoplastic
transformation of NIH3T3 was found to be successfully induced
through GPR4 transfection (13).
Additionally, a study in a nude mouse model also demonstrated the
carcinogenic ability of GPR4 (11).
Wyder et al (11) reported
that breast cancer and colon carcinoma growth were significantly
inhibited in GPR4-deficient mice. Moreover, cell proliferation,
invasion and metastatic ability were significantly attenuated in
ovarian cancer following GPR4-knockout, suggesting that this gene
plays a role in regulating proliferation, metastasis and invasion
of ovarian cancer.
Hepatocellular carcinoma (HCC) is a malignant solid
tumor enriched with blood vessels, with a unique vascular
distribution. HCC tumors are mainly supplied by the hepatic artery,
and the blood supply in the normal liver parenchyma is mainly
derived from the portal vein and the hepatic artery (14,15).
Tumors of the liver grow fast and are associated with a poor
prognosis due to the abundant blood supply. Thus, angiogenesis is
an important therapeutic target in HCC. Hematogenous and distant
metastases are the major types of metastases in HCC. Under the
microscope, the blood vessels of HCC appear abnormal, mainly
arterial and with sinusoidal capillaries compared with normal blood
vessels (16). Due to the high
metabolism associated with HCC, the tumor tissue is mainly fed by
the arterial system. Overgrowth of the artery can be part of the
non-invasive diagnostic criteria for HCC (17). Hepatic sinusoidal capillarization is
another angiogenic feature that is commonly found in HCC.
Additionally, the liver sinusoidal ECs are characterized by
decreased hepatic sinusoidal fenestration and continuous capillary
formation, along with collagenization of the sinusoids, laminin
deposition near ECs and hepatocytes, and formation of the basement
membrane (18). Certain studies have
suggested a role for GPCRs in tumorigenesis and the development of
HCC (19). Aberrant expression of
GPCRs, such as C-X-C chemokine receptor type 7, promotes HCC tumor
growth by regulating signaling pathways that promote cell
migration, metastases formation and angiogenesis (20). At present, to the best of our
knowledge, there are no studies that have investigated the
association between GPR4 expression and tumor MVD in HCC.
As a member of the superfamily of transforming
growth factor β receptors (21),
endoglin/CD105 is a marker of cell proliferation in vascular ECs,
particularly in the tumor vasculature (21–24). In
human breast cancer, CD105 and CD34 antibodies have been used to
assess MVD. MVD, quantified by CD105, demonstrated an association
between the overall survival time (OS) of the patient and the
expression of CD34 (22). The MVD of
tumor tissues not only reflects tumor blood vessel growth
quantitatively, but also acts as an independent prognostic factor
in some solid tumors (25).
In the present study, CD105 was used to mark blood
vessels and to determine the MVD. Furthermore, the expression of
GPR4 and its co-localization with CD105 was determined in HCC
tumors. The association between expression levels of GPR4 in HCC
cells and the clinicopathological characteristics of patients with
HCC was also investigated.
Materials and methods
Clinical data collection
A total of 47 specimens were obtained from The First
Affiliated Hospital of Xi'an Jiaotong University (Xi'an, Shaanxi,
China) between November 2014 and June 2016. The specimens included
37 cases of HCC and 10 cases of non-HCC (including 6 hepatic
hemangioma samples and 4 normal liver samples obtained 2–5 cm away
from the liver tumor tissue) as controls. In each patient, both
tumor and adjacent normal liver tissue were obtained. The
definition of adjacent normal tissue is generally considered to be
2–5 cm away from the tumor. However, in clinical practice, the
criteria for the diagnosis and radical resection of primary HCC
indicate that the distance between the liver resection margin and
the tumor boundary should be >1 cm. Thus, the ideal distance for
paracancerous tissue was noted in a smaller sample number than
expected. Therefore, liver tissues >2 cm away from the liver
tumor and normal liver tissues obtained from the resection of the
hepatic hemangioma were included in the control group (26). All clinical data of patients with
liver cancer were collected and thoroughly analyzed. Tumor staging
before chemotherapy and radiotherapy was performed according to the
2010 United States Cancer Board (American Joint Committee on
Cancer) system standard (27).
Clinicopathological data, including sex, age, surgical duration,
tumor size, lymph node metastases and pathological type, were
retrieved from the electronic medical records. The 37 patients were
aged between 28 and 81 years, with an average of 55.59±11.14 years.
A total of 8 cases were well-differentiated carcinomas, 24 cases
were moderately differentiated carcinomas and 5 cases were poorly
differentiated carcinomas. The study was approved by the Ethics
Committee of the First Affiliated Hospital of Xi'an Jiaotong
University. The median follow-up time was 14.5 months and the study
endpoint was determined by the patient's death. OS time was used as
a prognostic indicator.
Hematoxylin-eosin staining of frozen
sections
Tissue sections were permeabilized with PBS-Tween-20
(Beijing Dingguo Changsheng Biotechnology Co., Ltd.) and double
distilled water. Hematoxylin nuclei were stained at room
temperature for 3–5 min, and the nuclei were observed to turn blue
under the microscope. After that, the hematoxylin dyes were removed
with double steaming water, followed by 1% hydrochloric acid -
alcohol separation for 3–5 sec. The slices turned blue following
the addition tap water. The slides were stained with eosin for 1–2
min at room temperature, and the slides were dehydrated and
decolorized with different concentrations of ethanol (once with 80%
ethanol, once with 95% ethanol and twice with anhydrous ethanol) at
room temperature for 2–5 min. Finally, xylene permeated the slices
and sealed them with neutral gum at room temperature.
Immunofluorescence double
staining
Rabbit anti-human GPR4 polyclonal antibody (Abcam),
mouse anti-human CD105 monoclonal antibody (Abcam), goat
anti-rabbit Alexa Fluor 488 IgG (Jackson ImmunoResearch; http://www.jacksonimmuno.com/#) and goat
anti-mouse Cy3 IgG (Jackson) were used in immunohistochemistry
assays. Tissue sections (10 µm tissue sections embedded with SAKURA
Tissue-Tek O.C.T. Compound) were fixed in ice cold acetone (−20°C)
for 10 min and permeabilized with PBS-Tween-20 (PBST; 0.1%) at room
temperature. Non-specific binding sites were blocked with blocking
buffer (10% goat serum; Zsbio Commerce Store) for 1 h at room
temperature. Incubation was performed with a rabbit anti-human GPR4
polyclonal antibody (catalog no. ab188606; 1:100) and a mouse
anti-human CD105 monoclonal antibody (catalog no. ab14114; 1:100),
stored overnight at 4°C (>16 h), followed by four washes with
PBST and incubated with goat anti-rabbit Alexa Fluor 488 IgG
(ab2338840; 1:100) and goat anti-mouse Cy3 IgG (ab2338000; 1:100).
The secondary antibody was placed in an opaque wet box for 1 h at
room temperature for incubation. Sections were observed by laser
confocal microscopy. PBS was used as a negative control instead of
the primary antibody. Immunofluorescence staining of GPR4 and CD105
expression was detected by confocal laser scanning microscopy using
488- and 561 nm wavelengths to excite green and red fluorescence,
respectively.
Laser scanning confocal
microscopy
Immunofluorescence staining of GPR4 and CD105
expression was detected by confocal laser scanning microscopy
(TCS-SP5; Leica Microsystems GmbH). Wavelengths of 488 and 561 nm
were used to excite the green and red fluorescence, respectively.
The scanning resolution was 1024×1024 pixels. At ×200
magnification, three images were randomly captured for each slice.
New microvascular ECs (CD105-labeled) appeared green, GPR4-labeled
cells appeared red, and CD105- and GPR4-labeled cells appeared
yellow.
MVD determination
CD105-positivity was defined by capillaries
appearing green upon CD105 staining. These were counted based on
the Weidner's standard (28,29). MVD was observed in fields of ×100
magnification in the most vascularized areas, termed hotspots. The
average vessel count in the three fields at ×200 magnification was
used as the final MVD value. ECs or EC clusters stained green were
counted as a separate blood vessel. A clear separation was required
between these vessels. Lumen formation and the presence of red
blood cells in the cavity were not included.
GPR4 staining observation
GPR4 expression level was detected by ImageJ
analysis software (verison 2.0; National Institutes of Health). The
software was used to analyze each images of sections captured at
×200 magnification in the three fields. Parameter settings included
a selection of parameters commonly used in the literature: Positive
area (area), average optical density (mean density) and integrated
optical density (IOD). Image analysis results consisted of the
average grayscale value: IOD/area (30).
Analysis of co-expression and
co-localization of GPR4 and CD105
Image pro-plus software (version 6.0; Media
Cybernetics) was used to analyze confocal images, with correlation
coefficients and overlap coefficients. Pearson's correlation
coefficients were assigned to colocalization degrees used to
measure the linear relationship between distance variables as
follows: 0.6–0.8, Strong correlation; 0.4–0.6, medium correlation;
0.2–0.4 weak correlation; and 0.0–0.2 extremely weak correlation or
no correlation.
Controls
Non-HCC tissues were collected as the control group.
According to the protocol from the antibodies obtained from Abcam,
human lung tissues were used as the GPR4 positive control, mice
brain tissues as the CD105 positive control and PBS as the negative
control. The tissues were derived from surgical excision of lung
tissue from a patient that provided written informed consent prior
to the study, and from laboratory mice. The use of the mice was
approved by the Ethics Committee of the First Affiliated Hospital
of Xi'an Jiaotong University (Xi'an, China).
Statistical analysis
The statistical analysis was processed with the
statistical software programs Prism (version 7.0; GraphPad) and
SPSS (version 18.0; IBM Corp.). Measurement data are expressed as
the mean ± standard deviation. Statistical comparisons of data
between two groups were performed with the paired or unpaired
Student's t-test; comparisons between different parts of the same
specimen were performed with the paired Student's t-test. ANOVA was
used to compare multiple mean values. LSD, S-N-K and Tamhane's T2
test was used for the post hoc test following ANOVA. Under other
conditions, comparisons were carried out by non-parametric
analysis. Pearson's correlation coefficients were used to assess
the linear correlation between distant variables. Univariate
log-rank test and Kaplan-Meier survival curve were used for the
survival analysis.
Results
Expression of CD105 in HCC and control
tissues
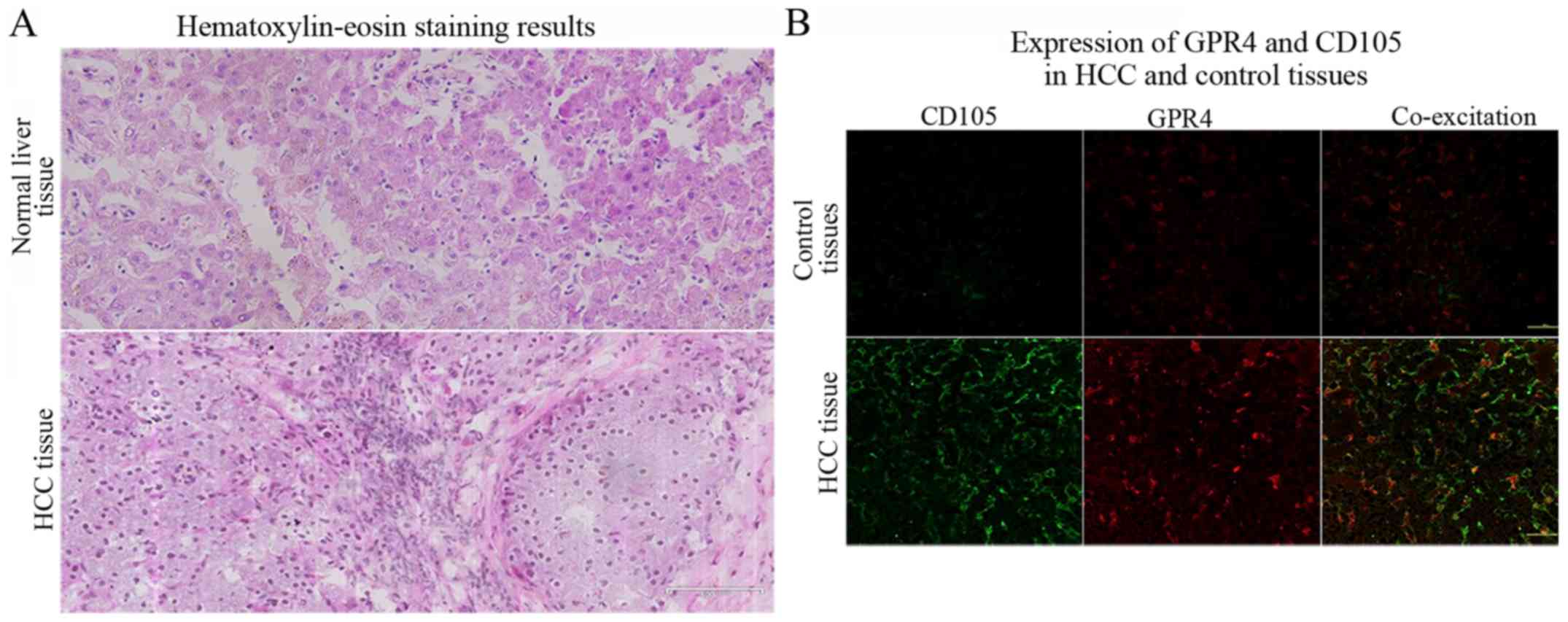
Human HCC tumors and normal liver tissues were
compared following hematoxylin staining (Fig. 1A). The tissues were stained for CD105
and GPR4 by immunofluorescence double staining (Fig. 1B). A low level of CD105 was expressed
in the control tissues, and was mainly expressed on the cell
membrane in HCC tumor tissues. Green fluorescent staining was
strongly scattered in tumor tissues and in the ECs of liver tissue
within 2 cm of the tumor. These positively stained single cell or
cell clusters mainly formed four types of shapes: Sinus, branching,
oval and sprouting. Most of these positively stained ECs formed
thin and irregular walls without smooth muscle tissue. The mean
MVD, determined using CD105, of the 37 liver tumor tissues was
significantly higher than that of the 10 control tissues
(P<0.05; mean, 61.51±28.09 and 12.90±11.72, respectively;
Table I).
 | Table I.Expression of CD105 in HCC and
control tissues. |
Table I.
Expression of CD105 in HCC and
control tissues.
| Pathological
group | Cases, n | MVDa | P-value | t |
|---|
| HCC tissues | 37 | 61.51±28.09 | <0.05 | 8.210 |
| Control
tissues | 10 | 12.90±11.72 |
|
|
Similar to CD105, GPR4 was mainly expressed on the
cell membrane and exhibited a lumen-like structure. The expression
of GPR4 was significantly lower in the control tissues compared
with that in the HCC tissues (P<0.05; mean, 0.0259±0.0041 and
0.0386±0.0125, respectively; Table
II).
 | Table II.Expression of GPR4 in HCC and control
tissues. |
Table II.
Expression of GPR4 in HCC and control
tissues.
| Pathological
group | Cases, n | Fluorescence
intensitya | P-value | t |
|---|
| HCC tissues | 37 | 0.0386±0.0125 | <0.05 | 5.210 |
| Control
tissues | 10 | 0.0259±0.0041 |
|
|
Correlation between GPR4 and CD105 in
HCC and control tissues
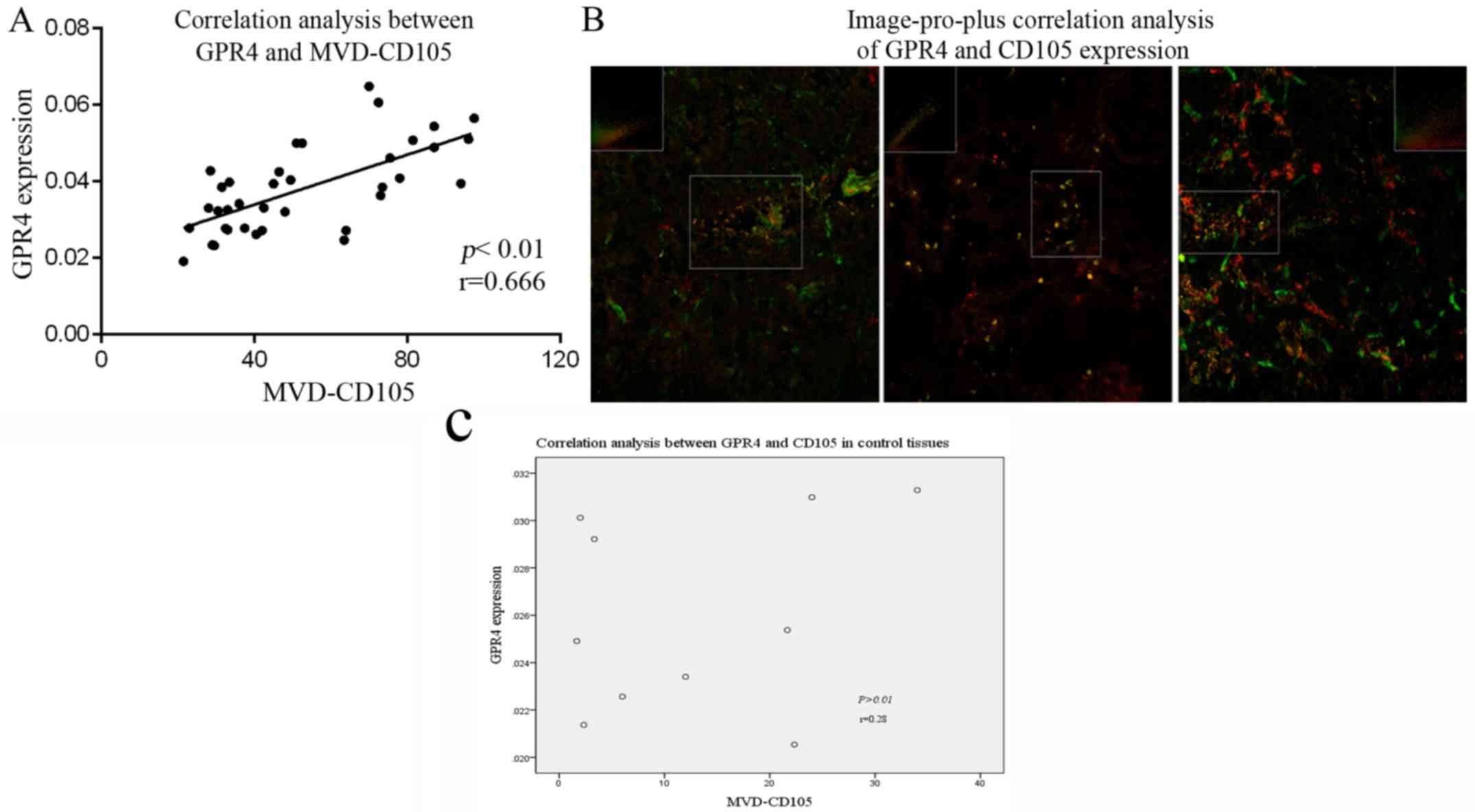
In control tissues, laser confocal imaging revealed
very weak and low co-localized expression of CD105 and GPR4.
Pearson's correlation analysis revealed no significant correlation
between CD105 and GPR4 co-localization (P>0.01; r=0.28; Fig. 2C) in control tissues.
Laser confocal imaging revealed that the region with
high GPR4 expression was consistent with high expression of CD105,
particularly in the sinusoidal and oval ECs of liver tissues <2
cm adjacent to the tumor. Co-localization of GPR4 and CD105 was
detected as yellow fluorescence. Pearson's correlation analysis
revealed a positive correlation between the expression of CD105 and
GPR4 (P<0.01; r=0.666; Fig. 2A).
The Image-pro-plus software was used to analyze three
representative confocal images (Fig.
2B). The Pearson's correlation coefficients indicated strong
correlations calculated by the Image-pro-plus software (r=0.65,
r=0.88 and r=0.62). These results corroborated the previous
observation, further illustrating the association between GPR4 and
microvessel formation.
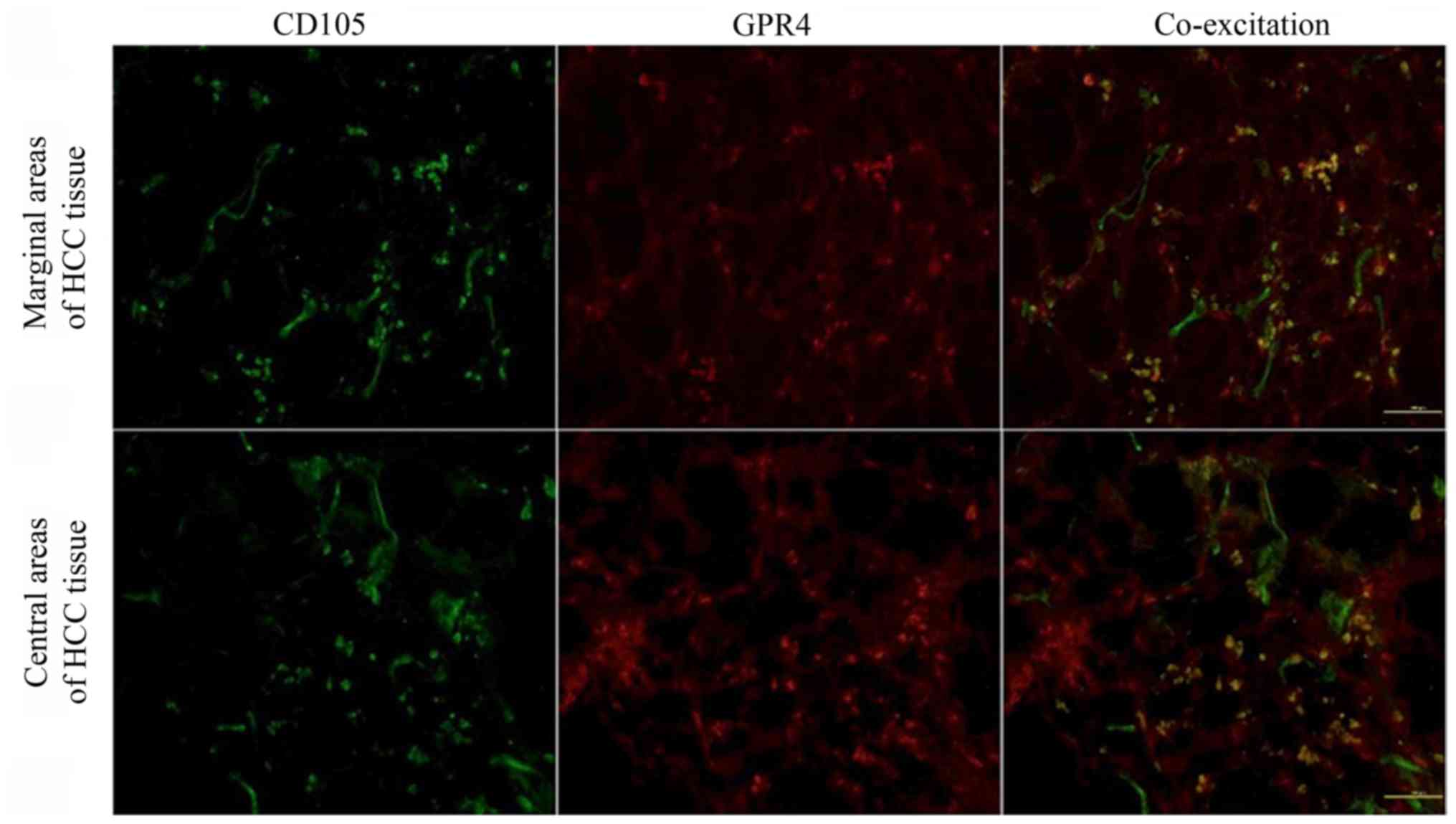
Expression of CD105 in the marginal
and central areas of HCC tissues
The positively stained regions for CD105 were found
to be scattered in the cancer tissues, particularly in the margin
of the invasion extension. However, a lower expression of CD105 was
found in the central areas of the neoplastic tissues or in areas of
necrosis (Fig. 3). The expression of
CD105 in the tumor edge was significantly higher than that in the
central area (P<0.05; Table
III). This observation could be explained by the higher number
of new blood vessels in the peripheral regions of HCC tissues, with
intensive neovascularization.
 | Table III.Expression of CD105 in HCC. |
Table III.
Expression of CD105 in HCC.
| Region | Cases, n | MVDa | P-value | t |
|---|
| Central part of HCC
tissues | 37 | 44.49±19.95 | <0.05 | 6.863 |
| Marginal part of
HCC tissues | 37 | 61.51±28.09 |
|
|
Expression of GPR4 in the marginal and
central areas of HCC tissues
The expression of GPR4 in HCC tissues was not
significantly different between the marginal and central areas
(P>0.05; Fig. 3; Table IV). This may be due to the hypoxic
environment in the center of the tumor leading to high GPR4
expression.
 | Table IV.Expression of GPR4 in HCC. |
Table IV.
Expression of GPR4 in HCC.
| Region | Cases, n | Fluorescence
intensitya | P-value | t |
|---|
| Central part of HCC
tissues | 37 | 0.0375±0.0114 | 0.350 | −0.947 |
| Marginal part of
HCC tissues | 37 | 0.0386±0.0125 |
|
|
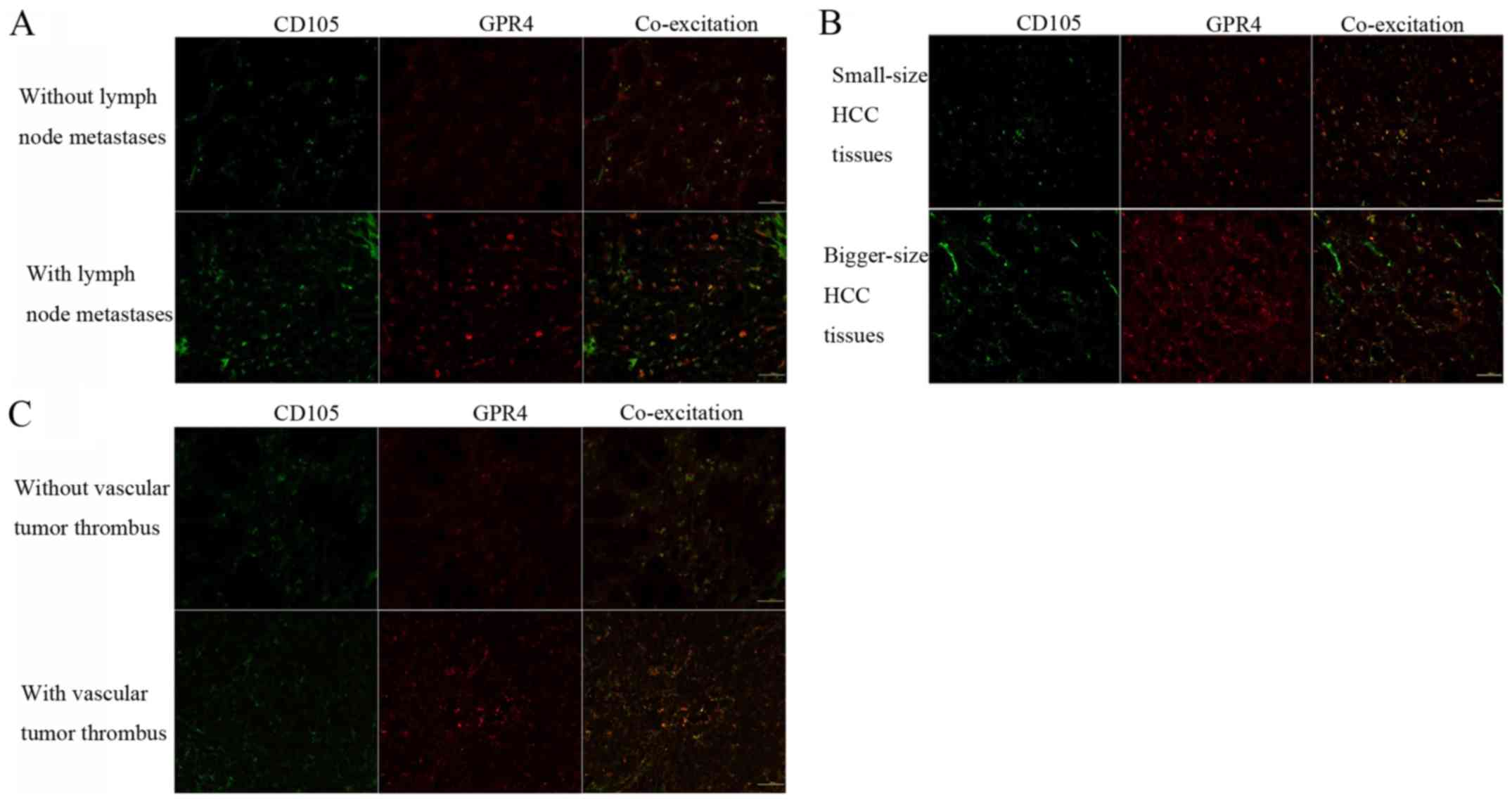
Association between CD105 and
clinicopathological features
MVD, determined by staining for CD105, was compared
between different clinicopathological factors of patients (Table V). This demonstrated that CD105
expression was independent of sex, age, tumor differentiation
degree, cirrhosis and ascites (P>0.05). Conversely, CD105 was
associated with lymphatic invasion (Fig.
4A), tumor size (Fig. 4B),
intravascular tumor thrombus (Fig.
4C) and TNM staging (all P<0.05)
 | Table V.Association between expression of
CD105 in hepatocellular carcinoma tumor tissues and
clinicopathological features. |
Table V.
Association between expression of
CD105 in hepatocellular carcinoma tumor tissues and
clinicopathological features.
| Clinicopathological
features | Cases, n | MVDa | P-value | t/F |
|---|
| Age, years |
|
| 0.110 | 1.641 |
|
<60 | 23 | 67.00±29.63 |
|
|
|
≥60 | 14 | 52.50±23.62 |
|
|
| Sex |
|
| 0.604 | −0.532 |
|
Male | 30 | 60.53±29.65 |
|
|
|
Female | 7 | 65.71±21.41 |
|
|
| Tumor size, cm |
|
| <0.01 | 3.975 |
|
<5 | 19 | 46.47±17.34 |
|
|
| ≥5 | 18 | 77.39±28.85 |
|
|
| Differentiated
degree |
|
| 0.857 | 0.155 |
|
High | 8 | 56.75±22.96 |
|
|
|
Middle | 24 | 63.25±31.20 |
|
|
|
Poor | 5 | 60.80±22.742 |
|
|
| Lymph node
metastasis |
|
| <0.01 | −6.861 |
| No | 35 | 59.69±27.78 |
|
|
|
Yes | 2 | 93.50±2.12 |
|
|
| Ascites |
|
| 0.197 | −1.337 |
| No | 26 | 57.58±27.97 |
|
|
|
Yes | 11 | 70.82±27.36 |
|
|
| Cirrhosis of the
liver |
|
| 0.517 | 0.671 |
| No | 8 | 67.88±30.97 |
|
|
|
Yes | 29 | 59.76±27.56 |
|
|
| Intravascular tumor
thrombus |
|
| <0.01 | −4.530 |
| No | 28 | 52.50±24.14 |
|
|
|
Yes | 9 | 89.56±20.37 |
|
|
| TNM staging |
|
| 0.003 | −3.258 |
|
I–II | 21 | 49.62±22.70 |
|
|
|
III–IV | 16 | 77.13±27.35 |
|
|
Association between GPR4 and
clinicopathological features
GPR4 expression was significantly associated with
tumor size (Fig. 4B) and blood
vessel invasion (Fig. 4C) (both
P<0.05; Table VI). This may be
explained by the high nutrient and oxygen requirements to maintain
the biological activity associated with larger tumors and blood
vessel invasion, which leads to induction of angiogenesis and GPR4
expression.
 | Table VI.Association between expression of
GPR4 in hepatocellular carcinoma tumor tissues and
clinicopathological features. |
Table VI.
Association between expression of
GPR4 in hepatocellular carcinoma tumor tissues and
clinicopathological features.
| Clinicopathological
features | Cases, n | Fluorescence
intensitya | P-value | t/F |
|---|
| Age, years |
|
| 0.184 | 1.357 |
|
<60 | 23 | 0.0406±0.0137 |
|
|
|
≥60 | 14 | 0.0353±0.0099 |
|
|
| Sex |
|
| 0.051 | 2.073 |
|
Male | 30 | 0.0399±0.0133 |
|
|
|
Female | 7 | 0.0330±0.0062 |
|
|
| Tumor size, cm |
|
| <0.01 | 4.349 |
|
<5 | 19 | 0.0314±0.0064 |
|
|
| ≥5 | 18 | 0.0462±0.01302 |
|
|
| Differentiated
degree |
|
| 0.520 | 0.667 |
|
High | 8 | 0.0428±0.0039 |
|
|
|
Middle | 24 | 0.0370±0.0027 |
|
|
|
Poor | 5 | 0.0398±0.0049 |
|
|
| Lymph node
metastasis |
|
| 0.223 | −1.850 |
| No | 35 | 0.0382±0.0127 |
|
|
|
Yes | 2 | 0.0462±0.0053 |
|
|
| Ascites |
|
| 0.286 | −1.103 |
| No | 26 | 0.0371±0.0119 |
|
|
|
Yes | 11 | 0.0423±0.0138 |
|
|
| Cirrhosis of the
liver |
|
| 0.596 | −0.543 |
| No | 8 | 0.0367±0.0105 |
|
|
|
Yes | 29 | 0.0392±0.0131 |
|
|
| Intravascular tumor
thrombus |
|
| <0.01 | −4.457 |
| No | 28 | 0.0349±0.0114 |
|
|
|
Yes | 9 | 0.0502±0.008 |
|
|
| TNM staging |
|
| <0.01 | −4.820 |
|
I–II | 21 | 0.0318±0.0094 |
|
|
|
III–IV | 16 | 0.0476±0.0102 |
|
|
Association between GPR4 and CD105
expression and the prognosis of patients with HCC
Postoperative clinical data were retrieved from
outpatient medical records or telephone calls. Overall, 91.89% of
patients successfully completed follow-up, with a median follow-up
time of 14.5 months (range, 2–36 months). The remaining three
patients were lost to follow up. OS time was calculated as the
period from surgery until death.
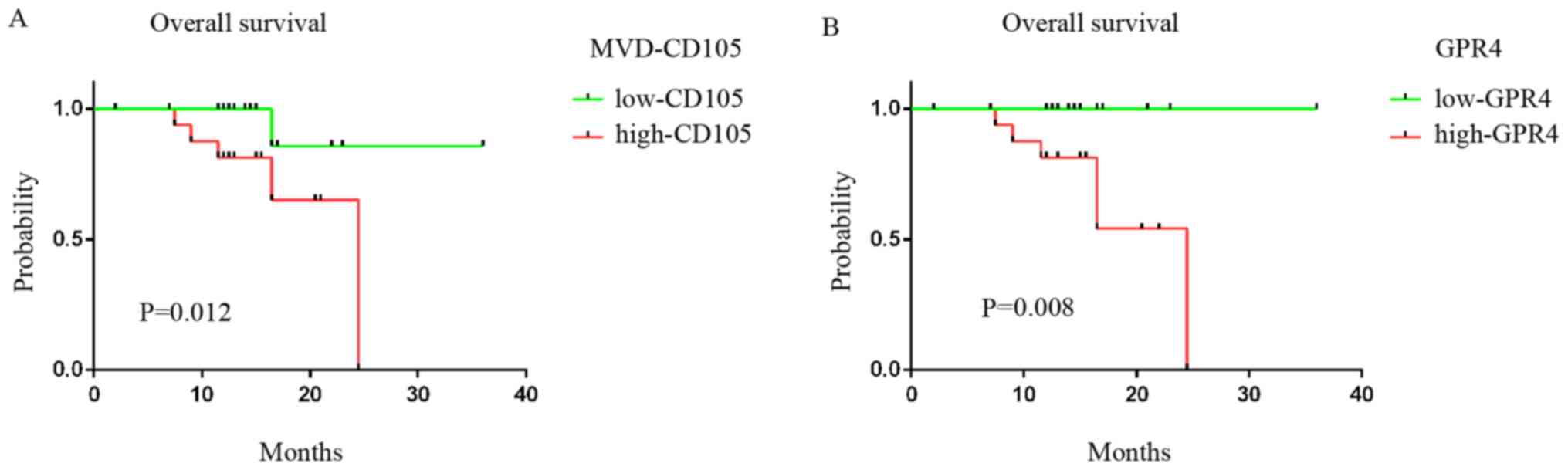
Prognostic significance was investigated by using
the average GPR4 expression (mean, 0.0386) and MVD-CD105 (mean,
61.51) levels as the cut-offs to divide patients into low- and
high-CD105/GPR4 groups (Fig. 5). OS
time was significantly shorter in the high-CD105/GPR4 group
compared with that in the low-CD105/GPR4 group.
Survival analysis with the univariate log-rank test
showed that MVD-CD105 and GPR4 expression affect the prognosis of
patients with HCC, and this was statistically significant
(P<0.05). Kaplan-Meier survival curves suggested that increased
MVD-CD105 and GPR4 expression were associated with a higher risk of
death in HCC.
Discussion
In the present study, MVD (based on CD105-labeled
ECs) and GPR4 expression were significantly higher in HCC than in
control tissues. This suggests the involvement of CD105 and GPR4 in
the neovascularization of HCC, and the GPR4 role of HCC in
angiogenesis. Previous studies have shown that traditional vascular
markers, such as CD31, are expressed in both small and large blood
vessels, and that CD105 is weakly expressed in blood vessels of
non-cancerous tissues (24). CD105
is highly expressed in blood vessel ECs both within and surrounding
the tumor (23,24). CD105 is mainly expressed during
neovascularization, particularly in the ECs of immature tumor
vasculature, and is believed to inhibit tumor angiogenesis. This
makes it an ideal therapeutic target in cancer (24,31,32).
Certain previous studies compared CD105-labeled MVD with
CD31-labeled tumor MVD and concluded that CD105-labeled MVD was a
risk factor for tumor progression compared with CD31 [P=0.020;
hazard ratio, 1.873; 95% confidence interval, 1.102–3.184)
(33). Moreover, CD105-labeled MVD
in tumor tissue was associated with tumor progression and
prognosis, as established in several solid tumor studies (32–37),
such as prostate cancer, primary hepatocellular carcinomas,
non-small cell lung cancer, rectal cancer and oral squamous cell
carcinoma. Therefore, CD105 may be more representative and
sensitive as a tumor vascular marker compared with a pan-vascular
marker in predicting tumor prognosis. Therefore, the expression and
clinical significance of CD105 in microvessels may be more
sensitive than that of CD31 or CD34. Honda et al (14) reported that neovascularization
density was increased in liver cancer, which was consistent the
result from previous studies (23,24,31,32).
A significant and positive correlation was
demonstrated between GPR4 expression level and MVD in the present
study. The localization of high GPR4 expression was consistent with
the CD105 expression hotspot in tissues of hepatic sinusoidal and
oval ECs <2 cm adjacent to the tumor. GPR4 was highly expressed
in liver tumor tissues, not only in marginal region. Moreover, the
expression of GPR4 was co-localized with CD105, which demonstrates
the presence of neovascularization-associated ECs. Therefore, the
high expression of GPR4 in the endothelium of neovascularization
may be involved in tumor angiogenensis. A review of the relevant
literature found no studies on the expression of GPR4 in liver
tumor tissues and blood vessels. In the present study, the
expression of GPR4 in liver tumor tissues and blood vessels was
preliminarily detected. Initially, immunofluorescence histochemical
study was conducted on frozen sections. IHC and co-staining with
classical markers for tumor angiogenesis was conducted for a
detailed morphological study on the paraffin sections of tumors.
GPR4 expression was observed in the microvessels of the tumors,
indicating its involvement in the microvessel angiogenesis in HCC.
Furthermore, the findings also indicated the potential of GPR4 and
CD105 as therapeutic targets, and as effective and sensitive
markers of tumors in HCC. Certain studies have demonstrated the
role of GPR4 in the process of angiogenesis. Jing et al
(9) revealed the promotion of
angiogenesis by GPR4 in head and neck cancer, and Ren et al
(10) reported that the
overexpression of GPR4 may be required for angiogenesis in
epithelial ovarian carcinomas. The expression of VEGFR2 and the
angiogenic response to VEGF was found to be decreased in
GPR4-deficient mice (11). Certain
studies reported a high perinatal mortality rate and a spontaneous
bleeding tendency in embryos and neonates that lacked GPR4
expression (12). Additionally, it
was observed that a proportion of subcutaneous blood vessels that
were covered with defective vascular smooth muscle cells became
dilated and tortuous, resulting in impaired vascular stability and
abnormal bleeding (12).
Angiogenesis may be associated with the
proton-sensor function of GPR4. The angiogenesis effect is
stimulated, and proton concentration is increased in hypoxic or
ischemic tissues (38–41). Subsequently, GPR4 senses a change in
pH and induces angiogenesis; the histidine on the GPR4 protein can
sense the change in the extracellular pH. At acidic pH levels,
activated GPR4 can stimulate the adenylate cyclase to produce a
large amount of cyclic AMP, with cAMP subsequently activating the
downstream pathway of protein kinase A and cyclic adenylate
response element binding to the protein. Ultimately, this process
activates the transcription of certain genes, including those
coding for angiogenic factors such as VEGF, among others (42,43).
Therefore, the role of GPR4 in angiogenesis may be due to the
function of its H+ receptors. In an extracorporeal
aortic ring experiment, microvessel products of GPR4-deficient
adult mice were less dependent on the pH of the culture medium
compared with wild-type mice (44).
Moreover, the ischemic and hypoxic conditions of the tumor
microenvironment activates GPR4 and thereby promotes angiogenesis.
Another study with ECs demonstrated that GPR4 promotes angiogenesis
via the regulation of C/EBP homologous protein (CHOP) in an acidic
environment (45). Although these
studies have shown that GPR4 promotes angiogenesis, the role of
GPR4 in liver cancer was not investigated.
In the present study, GPR4 expression was observed
in liver tumor tissues. Previous studies have also shown the
expression of GPR4 in a number of tumor tissues, including high
expression in HCC (11,13), suggesting its association with
tumorigenesis. The study by Sin et al (13) indicated that GPR4 is an oncogene and
that it was overexpressed in human cancer tissues, including those
of the breast, ovary, colon, liver and kidney. It was also shown
that the ectopic overexpression of GPR4 led to oncogenic
transformation of NIH3T3 fibroblasts. Although the effect of pH was
not assessed in the study, GPR4 was shown to have tumor-promoting
activity (13). Furthermore, high
expression of GPR4 in hepatoma cells indicated its role in the
development of HCC in the present study. In the present study, GPR4
expression was also found to be associated with the
clinicopathological features of HCC patients, indicating the
involvement of GPR4 in angiogenesis, tumor growth and the
development of HCC. Dong et al (46) observed that the inhibition of cell
apoptosis led to decreased expression of CHOP by GPR4, following
hypoxia/reoxygenation treatment in human umbilical vein ECs.
Moreover, the inhibition of GPR4 resulted in decreased renal injury
following ischemia-reperfusion and inhibition of cell apoptosis
through the suppression of CHOP expression (46) Therefore, GPR4 has potential as a
diagnostic marker for the diagnosis of liver cancer, and as a
therapeutic target in HCC. However, further studies are
required.
Another finding from the present study was that
CD105 expression was closely associated with tumor size, lymph node
metastasis, intravascular tumor thrombus and TNM staging in the
patients with HCC, highlighting its potential as a marker of
vascular EC proliferation. It is highly relevant to determine novel
targets of antiangiogenesis and CD105 may be a prognostic factor
for patients with HCC. The association between increased
neovascularization and clinical characteristics in patients with
HCC indicated the highly vascularized nature of this malignancy and
the part played by angiogenesis. Thus, uncovering the mechanisms
underlying angiogenesis in HCC may provide effective and sensitive
markers for HCC diagnosis and a specific target for antiangiogenic
therapy.
In the present study, differences in mean CD105
values were found between the tumor edge and central area. However,
no such difference was observed with GPR4 expression. Furthermore,
a higher number of new blood vessels was observed in the peripheral
region of HCC tissues, where the proliferation of ECs was more
active. Intensive neovascularization elicits hypoxic conditions,
inducing the expression of CD105 predominantly in the tumor
marginal edge (47). On the other
hand, no significant differences in GPR4 expression were observed
between the tumor edge and the tumor center in the present study.
It is acknowledged that an extracellular acidic environment induces
the expression of GPR4 (12). The
hypoxic environment in the central tumor area may lead to high GPR4
expression, leading to an absence of differences in GPR4 expression
between the neovascular-rich edge compared with the central area of
the tumor. GPR4 has dual effects of tumor promotion and inhibition,
depending on the cell type and biological background. In the
present study, GPR4 expression was affected by different
clinicopathological factors, although the potential impact of
sample differences should also be considered.
Analysis of survival curves showed shorter survival
times in patients with liver cancer exhibiting high GPR4 and CD105
expression levels. Notably, the expression levels of CD105 and GPR4
were consistent with the prognostic trend of these patients. This
suggests the potential value of using CD105 and GPR4 as predictive
markers of prognosis in cancer patients, and this is worth pursuing
in further investigations.
Previous studies have implicated GPR4 in two main
processes, which were corroborated in the present study. On one
hand, GPR4 is involved in angiogenesis in ovarian cancer (10). On the other hand, it is an oncogene
associated with tumor progression (13). However, it is worth mentioning that
the present study was the first to suggest a role for GPR4 in liver
cancer, as, to the best of our knowledge, previous studies have not
investigated GPR4 in this type of tumor. The present study was the
first to investigate the association between GPR4 and MVD in liver
tumor tissues, as well as the association between GPR4 and the
clinicopathological features of patients with liver cancer.
Due to the limited number of specimens collected,
the association between GPR4 and tumor angiogenesis needs to be
validated and further studied. Western blot analysis will be
carried out in future studies to further assess the expression
levels of the proteins investigated in the present study.
Furthermore, future studies should focus on the effect of
inhibiting and promoting angiogenesis in vitro on GPR4
expression.
Several therapeutic options are available for HCC,
including surgical resection, chemotherapy, radiofrequency
ablation, transarterial chemoperfusion, selective internal
radiation therapy, transarterial chemoembolization, percutaneous
ethanol instillation, monoclonal antibody therapy and liver
transplantation (48–54). Tumor vascular-targeting therapy has
been widely considered in medical research. The rich vascularity of
HCC suggests the inhibition of angiogenesis as a therapeutic target
in this tumor and indicates that antiangiogenic therapy may be a
relevant option for advanced HCC. Angiogenesis in HCC is regulated
by both proangiogenic and antiangiogenic factors. Proangiogenic
factors include VEGF, matrix metalloproteases, angiopoietin-2 and
basic fibroblast growth factor, and angiogenesis inhibitors include
tissue inhibitor of metalloproteinases 1, angiostatin, endostatin
and thrombospondin (55–58) Some inflammatory molecules, such as
signal transducer and activator of transcription 3, nuclear
factor-κB, tumor necrosis factor-α and interleukin-8, also have
potential roles in liver cancer angiogenesis (56–59).
Antiangiogenesis therapy of HCC has been gradually diversified,
with VEGF inhibitors, tyrosinase receptor inhibitors and drugs that
directly inhibit ECs. The targeted drug sorafenib has been widely
recognized as a first-line treatment with good clinical efficacy.
However, inhibitors of angiogenesis do not completely inhibit or
suppress liver cancer angiogenesis (59). The investigation of the various
mechanisms of HCC angiogenesis, both at the molecular and genetic
levels, is hence highly recommended.
Overall, the results from the present study allow
the conclusion that both CD105 and GPR4 are positively expressed in
benign and malignant liver tissues. Compared with control tissues,
tumor tissues exhibited high CD105 and GPR4 expression. There was a
strong positive correlation between the average fluorescence
intensities of GPR4 and CD105 (MVD). GPR4 and CD105 were
co-localized in the vascular endothelium of cancer tissues. GPR4
was preferentially expressed in the margin compared with the
central area of the tumors, suggesting its expression in HCC tumor
microvessels and its potential implication in HCC angiogenesis and
development. These results indicated the therapeutic relevance of
investigating novel antiangiogenic targets. The association between
the expression of GPR4 and the clinicopathological features of
patients with HCC further indicated its role in angiogenesis,
growth and the prognosis of patients with HCC. The mechanism
underlying the role of GPR4 in HCC angiogenesis will be further
investigated in future studies.
Acknowledgements
Not applicable.
Funding
This manuscript was supported by the National
Natural Science Foundations of China (grant no. 81772793/H1621,
31201060/C0709, 30973175/C1701 and 81172490/H1621), the Program for
New Century Excellent Talents in University (grant no.
NCET-12-0440), the Scientific and Technological Research Foundation
of Shaanxi Province (grant no. 2012K13-01-06), the Research
Foundation of Health Department of Shaan'xi Province (grant no.
2010D41), the Fundamental Research Funds for the Central
Universities, First Affiliated Hospital of Xi'an Jiaotong
University, and the Clinical Research Award of the First Affiliated
Hospital of Xi'an Jiaotong University (grant no.
XJTU1AHCR2014-041).
Availability of data and materials
The datasets used and/or analysed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
JR conceived and supervised the study; JR and CFX
designed the experiments; JR, CFX, SS, YLY, SY, SHB and YYW
performed the experiments; LYC, JZZ, RL, XZZ and HLM analyzed the
data; JR, CFX, SS and HLM wrote the manuscript; JR and XZZ revised
the manuscript. All authors have read and approved the final
version of this submission.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Xi'an Jiaotong University. Written informed consent was obtained
from each patient, including consent for their samples to be taken
and used for research purposes, before surgery.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ludwig MG, Vanek M, Guerini D, Gasser JA,
Jones CE, Junker U, Hofstetter H, Wolf RM and Seuwen K:
Proton-sensing G-protein-coupled receptors. Nature. 425:93–98.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Liang B, Lei W and Gaole A: Relationship
between proton-sensing G-protein coupled receptors and
tumorigenesis and tumor metastasis. Chin J Biochem Mol Biol.
2011.(In Chinese).
|
|
3
|
Murakami N, Yokomizo T, Okuno T and
Shimizu T: G2A is a proton-sensing G-protein-coupled receptor
antagonized by lysophosphatidylcholine. J Biol Chem.
279:42484–42491. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wang JQ, Kon J, Mogi C, Tobo M, Damirin A,
Sato K, Komachi M, Malchinkhuu E, Murata N, Kimura T, et al: TDAG8
is a proton-sensing and psychosine-sensitive G-protein-coupled
receptor. J Biol Chem. 279:45626–45633. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mahadevan MS, Baird S, Bailly JE, Shutler
GG, Sabourin LA, Tsilfidis C, Neville CE, Narang M and Korneluk RG:
Isolation of a novel G protein-coupled receptor (GPR4) localized to
chromosome 19q13.3. Genomics. 30:84–88. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Justus CR, Dong L and Yang LV: Acidic
tumor microenvironment and pH-sensing G protein-coupled receptors.
Front Physiol. 4:3542013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ren J, Zhang Y, Cai H, Ma H, Zhao D, Zhang
X, Li Z, Wang S, Wang J, Liu R, et al: Human GPR4 and the notch
signaling pathway in endothelial cell tube formation. Mol Med Rep.
14:1235–1240. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kim KS, Ren J, Jiang Y, Ebrahem Q, Tipps
R, Cristina K, Xiao YJ, Qiao J, Taylor KL, Lum H, et al: GPR4 plays
a critical role in endothelial cell function and mediates the
effects of sphingosylphosphorylcholine. FASEB J. 19:819–821. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jing Z, Xu H, Chen X, Zhong Q, Huang J,
Zhang Y, Guo W, Yang Z, Ding S, Chen P and Huang Z: The
proton-sensing G-protein coupled receptor GPR4 promotes
angiogenesis in head and neck cancer. PLoS One. 11:e01527892016.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ren J, Jin W, Gao YE, Zhang Y, Zhang X,
Zhao D, Ma H, Li Z, Wang J, Xiao L, et al: Relations between GPR4
expression, microvascular density (MVD) and clinical pathological
characteristics of patients with epithelial ovarian carcinoma
(EOC). Curr Pharm Des. 20:1904–1916. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wyder L, Suply T, Ricoux B, Billy E,
Schnell C, Baumgarten BU, Maira SM, Koelbing C, Ferretti M, Kinzel
B, et al: Reduced pathological angiogenesis and tumor growth in
mice lacking GPR4, a proton sensing receptor. Angiogenesis.
14:533–544. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yang LV, Radu CG, Roy M, Lee S, McLaughlin
J, Teitell MA, Iruela-Arispe ML and Witte ON: Vascular
abnormalities in mice deficient for the G protein-coupled receptor
GPR4 that functions as a pH sensor. Mol Cell Biol. 27:1334–1347.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sin WC, Zhang Y, Zhong W, Adhikarakunnathu
S, Powers S, Hoey T, An S and Yang J: G protein-coupled receptors
GPR4 and TDAG8 are oncogenic and overexpressed in human cancers.
Oncogene. 23:6299–6303. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Honda H, Tajima T, Kajiyama K, Kuroiwa T,
Yoshimitsu K, Irie H, Aibe H, Shimada M and Masuda K: Vascular
changes in hepatocellular carcinoma: Correlation of radiologic and
pathologic findings. AJR Am J Roentgenol. 173:1213–1217. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Matsui O, Kobayashi S, Sanada J, Kouda W,
Ryu Y, Kozaka K, Kitao A, Nakamura K and Gabata T: Hepatocelluar
nodules in liver cirrhosis: Hemodynamic evaluation
(angiography-assisted CT) with special reference to multi-step
hepatocarcinogenesis. Abdom Imaging. 36:264–272. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hui LI, Qing YE, Yin XJ and Li YM: The
research of angiogenesis in hepatocellular carcinoma. Chin Clin
Oncol. 4:2009.(In Chinese).
|
|
17
|
Yamamoto K: Clinical management of
hepatocellular carcinoma. J Okayama Med Association. 120:279–284.
2008.
|
|
18
|
Kin M, Torimura T, Ueno T, Inuzuka S and
Tanikawa K: Sinusoidal capillarization in small hepatocellular
carcinoma. Pathol Int. 4:771–778. 1994.
|
|
19
|
Peng WT, Sun WY, Li XR, Sun JC, Du JJ and
Wei W: Emerging roles of G protein-coupled receptors in
hepatocellular carcinoma. Int J Mol Sci. 19:13662018. View Article : Google Scholar
|
|
20
|
Chen Y, Teng F, Wang G and Nie Z:
Overexpression of CXCR7 induces angiogenic capacity of human
hepatocellular carcinoma cells via the AKT signaling pathway. Oncol
Rep. 36:2275–2281. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Nassiri F, Cusimano MD, Scheithauer BW,
Rotondo F, Fazio A, Yousef GM, Syro LV, Kovacs K and Lloyd RV:
Endoglin (CD105): A review of its role in angiogenesis and tumor
diagnosis, progression and therapy. Anticancer Res. 31:2283–2290.
2011.PubMed/NCBI
|
|
22
|
Kumar S, Ghellal A, Li C, Byrne G, Haboubi
N, Wang JM and Bundred N: Breast carcinoma: Vascular density
determined using CD105 antibody correlates with tumor prognosis.
Cancer Res. 59:856–861. 1999.PubMed/NCBI
|
|
23
|
Fonsatti E, Altomonte M, Nicotra MR,
Natali PG and Maio M: Endoglin (CD105): A powerful therapeutic
target on tumor-associated angiogenetic blood vessels. Oncogene.
22:6557–6563. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Dallas NA, Samuel S, Xia L, Fan F, Gray
MJ, Lim SJ and Ellis LM: Endoglin (CD105): A marker of tumor
vasculature and potential target for therapy. Clin Cancer Res.
14:1931–1937. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Fonsatti E, Nicolay HJ, Altomonte M, Covre
A and Maio M: Targeting cancer vasculature via endoglin/CD105: A
novel antibody-based diagnostic and therapeutic strategy in solid
tumours. Cardiovasc Res. 86:12–19. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Robboy SJ: Surgical Pathology Dissection,
an Illustrated Guide. International Journal of Gynecological
Pathology. 16–86. 1997.
|
|
27
|
Edge SB and Compton CC: The American joint
committee on cancer: The 7th edition of the AJCC cancer staging
manual and the future of TNM. Ann Surg Oncol. 17:1471–1474. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chen A, Dong L, Leffler NR, Asch AS, Witte
ON and Yang LV: Activation of GPR4 by acidosis increases
endothelial cell adhesion through the cAMP/Epac pathway. PLoS One.
6:e275862011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Le D: Tumor angiogenesis and
metastasis-correlation in invasive breast carcinoma. N Engl J Med.
324:1–8. 1991. View Article : Google Scholar
|
|
30
|
Yu P, Bu H, Wang H, Zhao G, Zhang J and
Zhou Q: Comparative study on image analysis and manual counting of
immunohistochemistry. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi.
20:288–290. 2003.(In Chinese). PubMed/NCBI
|
|
31
|
Henry-Berger J, Mouzat K, Baron S,
Bernabeu C, Marceau G, Saru JP, Sapin V, Lobaccaro JM and Caira F:
Endoglin (CD105) expression is regulated by the liver X receptor
alpha (NR1H3) in human trophoblast cell line JAR. Biol Reprod.
78:968–975. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Wikström P, Lissbrant IF, Stattin P,
Egevad L and Bergh A: Endoglin (CD105) is expressed on immature
blood vessels and is a marker for survival in prostate cancer.
Prostate. 51:268–275. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Darcy KM and Birrer MJ: Translational
research in the gynecologic oncology group: Evaluation of ovarian
cancer markers, profiles, and novel therapies. Gynecol Oncol.
117:429–439. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Yao Y, Pan Y, Chen J, Sun X, Qiu Y and
Ding Y: Endoglin (CD105) expression in angiogenesis of primary
hepatocellular carcinomas: Analysis using tissue microarrays and
comparisons with CD34 and VEGF. Ann Clin Lab Sci. 37:39–48.
2007.PubMed/NCBI
|
|
35
|
Tanaka F, Otake Y, Yanagihara K, Kawano Y,
Miyahara R, Li M, Yamada T, Hanaoka N, Inui K and Wada H:
Evaluation of angiogenesis in non-small cell lung cancer:
Comparison between anti-CD34 antibody and anti-CD105 antibody. Clin
Cancer Res. 7:3410–3415. 2001.PubMed/NCBI
|
|
36
|
Goldiş DS, Sferdian MF, Tarţă C, Fulger
LO, Totolici BD and Neamţu C: Comparative analysis of microvessel
density quantified through the immunohistochemistry expression of
CD34 and CD105 in rectal cancer. Rom J Morphol Embryol. 56:419–424.
2015.PubMed/NCBI
|
|
37
|
Mărgăritescu C, Simionescu C, Mogoantă L,
Badea P, Pirici D, Stepan A and Ciurea R: Endoglin (CD105) and
microvessel density in oral squamous cell carcinoma. Rom J Morphol
Embryol. 49:321–326. 2008.PubMed/NCBI
|
|
38
|
Nedergaard M, Kraig RP, Tanabe J and
Pulsinelli WA: Dynamics of interstitial and intracellular pH in
evolving brain infarct. Am J Physiol. 260:R581–R588.
1991.PubMed/NCBI
|
|
39
|
Lardner A: The effects of extracellular pH
on immune function. J Leukoc Biol. 69:522–530. 2001.PubMed/NCBI
|
|
40
|
Wahl ML and Grant DS: Effects of
microenvironmental extracellular pH and extracellular matrix
proteins on angiostatin's activity and on intracellular pH. Gen
Pharmacol. 35:277–285. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Gatenby RA and Gillies RJ: Why do cancers
have high aerobic glycolysis? Nat Rev Cancer. 4:891–899. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Wang X and Klein RD: Prostaglandin E 2
induces vascular endothelial growth factor secretion in prostate
cancer cells through EP2 receptor-mediated cAMP pathway. Mol
Carcinog. 46:912–923. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Ristori C, Ferretti ME, Pavan B,
Cervellati F, Casini G, Catalani E, Dal Monte M and Biondi C:
Adenylyl Cyclase/cAMP System involvement in the antiangiogenic
effect of somatostatin in the retina. Results from transgenic mice.
Neurochem Res. 33:12472008. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Rozengurt E: Mitogenic signaling pathways
induced by G protein-coupled receptors. J Cell Physiol.
213:589–602. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Dong L, Krewson EA and Yang LV: Acidosis
activates endoplasmic reticulum stress pathways through GPR4 in
human vascular endothelial cells. Int J Mol Sci. 18:2782017.
View Article : Google Scholar
|
|
46
|
Dong B and Zhang X, Fan Y, Cao S and Zhang
X: GPR4 knockout improves renal ischemia-reperfusion injury and
inhibits apoptosis via suppressing the expression of CHOP. Biochem
J. 474:4065–4075. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Li C, Guo B, Wilson PB, Stewart A, Byrne
G, Bundred N and Kumar S: Plasma levels of soluble CD105 correlate
with metastasis in patients with breast cancer. Int J Cancer.
89:122–126. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Abou-Alfa GK, Amadori D, Santoro A, Figer
A, De Greve J, Lathia C, Voliotis D, Anderson S, Moscovici M and
Ricci S: Safety and efficacy of sorafenib in patients with
hepatocellular carcinoma (HCC) and child-pugh A versus B cirrhosis.
Gastrointest Cancer Res. 4:40–44. 2011.PubMed/NCBI
|
|
49
|
Branco F, Bru C, Vilana R, Bianchi L and
Alvas de Mattos AA: Percutaneous ethanol injection before liver
transplantation in the hepatocellular carcinoma. Ann Hepatol.
8:220–227. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Kawai S, Okamura J, Ogawa M, Ohashi Y,
Tani M, Inoue J, Kawarada Y, Kusano M, Kubo Y and Kuroda C:
Prospective and randomized clinical trial for the treatment of
hepatocellular carcinoma-a comparison of lipiodol-transcatheter
arterial embolization with and without adriamycin (first
cooperative study). The cooperative study group for liver cancer
treatment of Japan. Cancer Chemother Pharmacol. 31 (Suppl):S1–S6.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Lau WY, Lai EC and Leung TW: Current role
of selective internal irradiation with yttrium-90 microspheres in
the management of hepatocellular carcinoma: A systematic review.
Int J Rad Oncol Biol Phys. 81:460–467. 2011. View Article : Google Scholar
|
|
52
|
Livraghi T, Goldberg SN, Lazzaroni S,
Meloni F, Solbiati L and Gazelle GS: Small hepatocellular
carcinoma: Treatment with radio-frequency ablation versus ethanol
injection. Radiology. 210:655–661. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Nicolini A, Fasani P, Manini MA,
Martinetti L, Forzenigo LV, Iavarone M, Crespi S, Rossi G,
Biondetti P, Colombo M and Sangiovanni A: Transarterial
embolization with microspheres in the treatment of monofocal HCC.
Dig Liver Dis. 41:143–149. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Sun W: Treatment of inoperable HCC after
sorafenib: Where will the new paradigm take Us? Gastrointest Cancer
Res. 2:49–50. 2008.PubMed/NCBI
|
|
55
|
Germano G, Allavena P and Mantovani A:
Cytokines as a key component of cancer-related inflammation.
Cytokine. 43:374–379. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Sakurai T, He G, Matsuzawa A, Yu GY, Maeda
S, Hardiman G and Karin M: Hepatocyte necrosis induced by oxidative
stress and IL-1α release mediate carcinogen-induced compensatory
proliferation and liver tumorigenesis. Cancer Cell. 14:156–165.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Sun HC and Tang ZY: Angiogenesis in
hepatocellular carcinoma: The retrospectives and perspectives. J
Cancer Res Clin. 130:307–319. 2004. View Article : Google Scholar
|
|
58
|
Zhu AX: Systemic treatment of
hepatocellular carcinoma: Dawn of a new era? Ann Surg Oncol.
17:1247–1256. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Abdel-Rahman O and Cheung WY: The
expanding role of systemic therapy in the management of
hepatocellular carcinoma. Can J Gastroenterol Hepatol. 2018:1–4.
2018. View Article : Google Scholar
|