|
1
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin. 68:394–424. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Domper Arnal MJ, Ferrandez Arenas A and
Lanas Arbeloa A: Esophageal cancer: Risk factors, screening and
endoscopic treatment in Western and Eastern countries. World J
Gastroenterol. 21:7933–7943. 2015. View Article : Google Scholar
|
|
3
|
Chen W, Zheng R, Baade PD, Zhang S, Zeng
H, Bray F, Jemal A, Yu XQ and He J: Cancer statistics in China,
2015. CA Cancer J Clin. 66:115–132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zheng R, Zeng H, Zhang S and Chen W:
Estimates of cancer incidence and mortality in China, 2013. Chin J
Cancer. 36:662017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sohda M and Kuwano H: Current status and
future prospects for esophageal cancer treatment. Ann Thorac
Cardiovasc Surg. 23:1–11. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Berry MF: Esophageal cancer: Staging
system and guidelines for staging and treatment. J Thorac Dis.
6:S289–S297. 2014.PubMed/NCBI
|
|
7
|
Xi M and Lin SH: Recent advances in
intensity modulated radiotherapy and proton therapy for esophageal
cancer. Expert Rev Anticancer Ther. 17:635–646. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fenkell L, Kaminsky I, Breen S, Huang S,
Van Prooijen M and Ringash J: Dosimetric comparison of IMRT vs. 3D
conformal radiotherapy in the treatment of cancer of the cervical
esophagus. Radiother Oncol. 89:287–291. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bollschweiler E, Plum P, Monig SP and
Holscher AH: Current and future treatment options for esophageal
cancer in the elderly. Expert Opin Pharmacother. 18:1001–1010.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Berry SD, Ngo L, Samelson EJ and Kiel DP:
Competing risk of death: An important consideration in studies of
older adults. J Am Geriatr Soc. 58:783–787. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
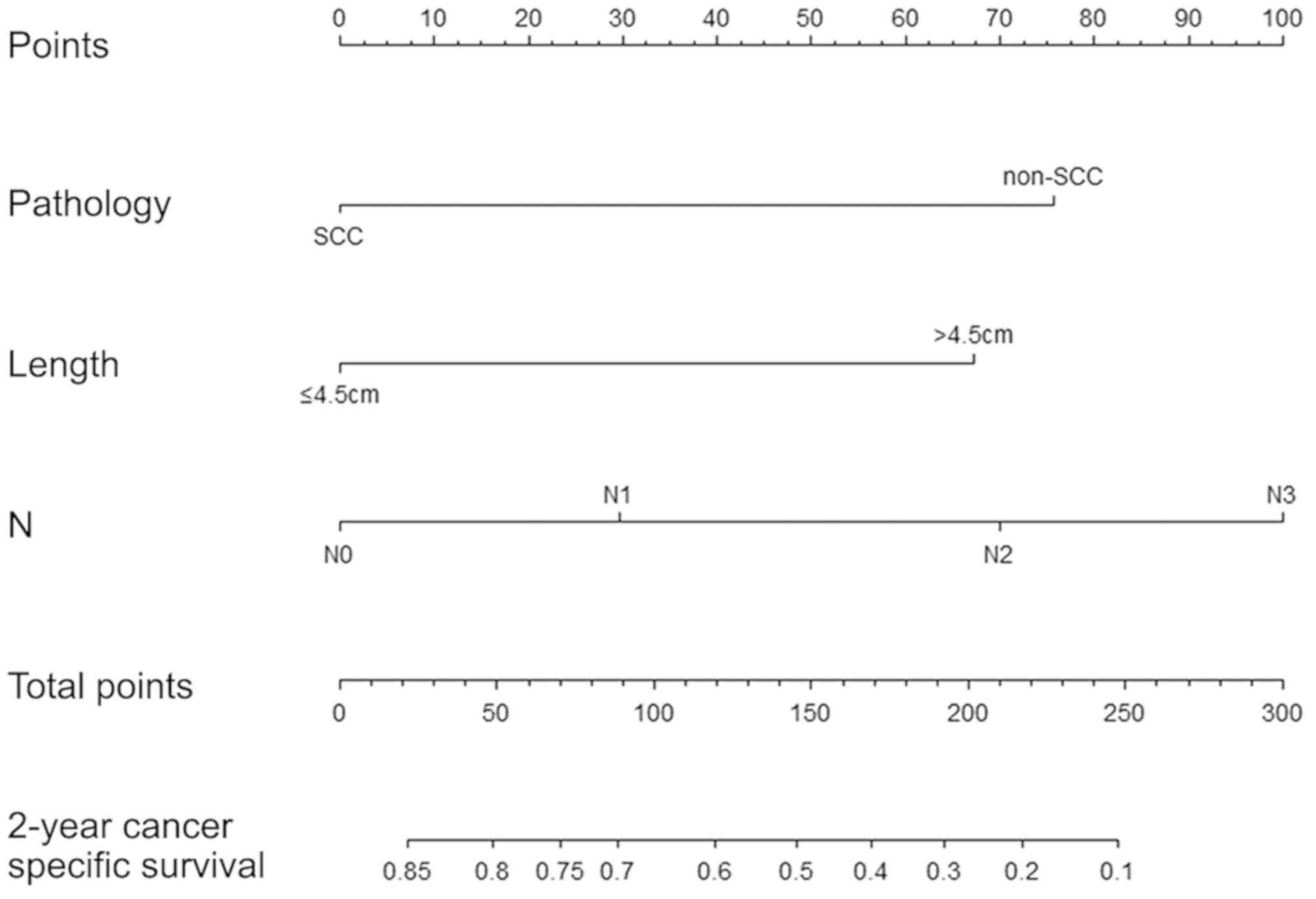
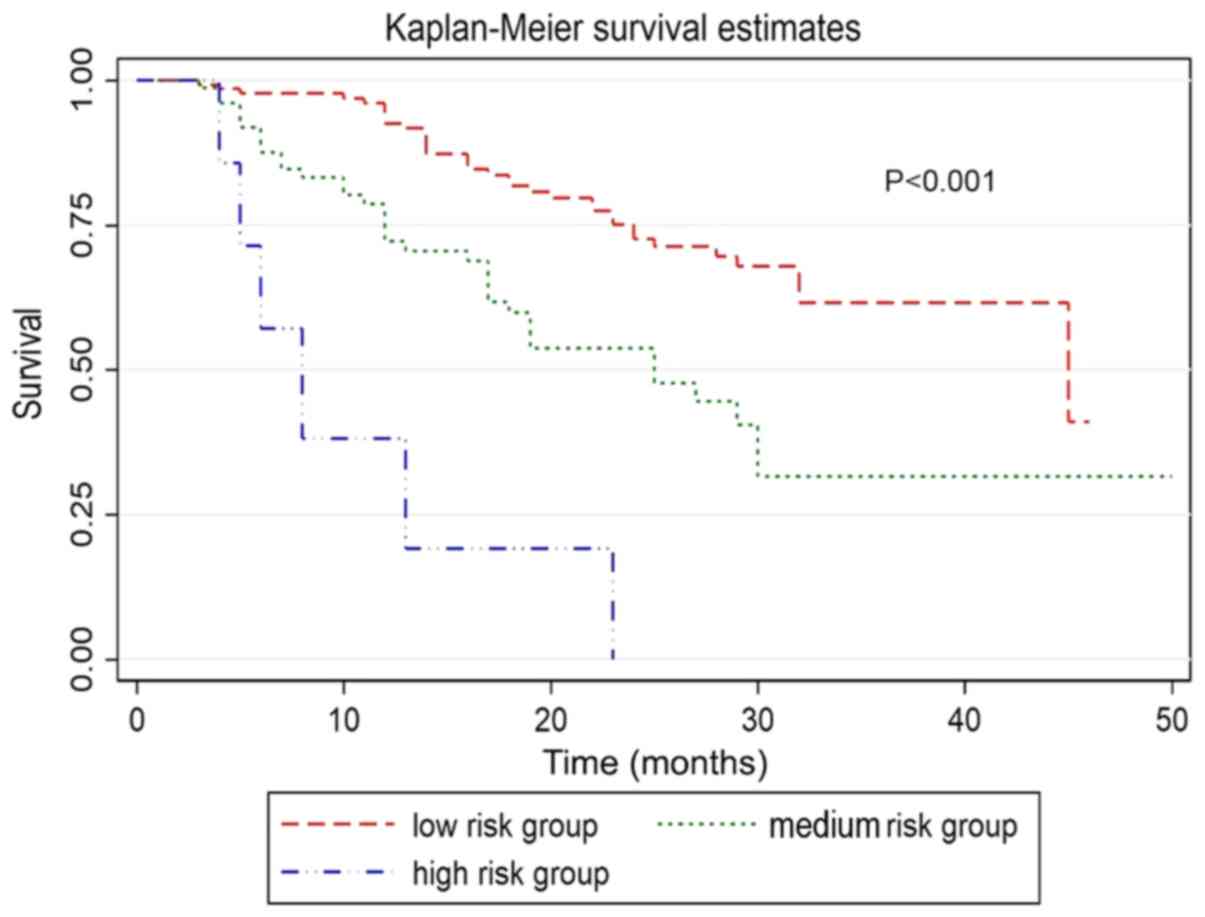
Zhang Z, Geskus RB, Kattan MW, Zhang H and
Liu T: Nomogram for survival analysis in the presence of competing
risks. Ann Transl Med. 5:4032017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Carmona R, Zakeri K, Green G, Hwang L,
Gulaya S, Xu B, Verma R, Williamson CW, Triplett DP, Rose BS, et
al: Improved method to stratify elderly patients with cancer at
risk for competing events. J Clin Oncol. 34:1270–1277. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Simpson MC, Massa ST, Boakye EA, Antisdel
JL, Stamatakis KA, Varvares MA and Osazuwa-Peters N: primary cancer
vs. competing causes of death in survivors of head and neck cancer.
JAMA Oncol. 4:257–259. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Eguchi T, Bains S, Lee MC, Tan KS, Hristov
B, Buitrago DH, Bains MS, Downey RJ, Huang J, Isbell JM, et al:
Impact of increasing age on cause-specific mortality and morbidity
in patients with stage I non-small-cell lung cancer: A competing
risks analysis. J Clin Oncol. 35:281–290. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Grobman WA and Stamilio DM: Methods of
clinical prediction. Am J Obstet Gynecol. 194:888–894. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kutikov A, Egleston BL, Wong YN and Uzzo
RG: Evaluating overall survival and competing risks of death in
patients with localized renal cell carcinoma using a comprehensive
nomogram. J Clin Oncol. 28:311–317. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Huang XD, Zhou GQ, Lv JW, Zhou HQ, Zhong
CW, Wu CF, Zheng ZQ, He XJ, Peng L, Ma J and Sun Y: Competing risk
nomograms for nasopharyngeal carcinoma in the intensity-modulated
radiotherapy era: A big-data, intelligence platform-based analysis.
Radiother Oncol. 129:389–395. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Luo C, Zhong X, Deng L, Xie Y, Hu K and
Zheng H: Nomogram predicting locoregional recurrence to assist
decision-making of postmastectomy radiotherapy in patients with
T1-2N1 breast cancer. Int J Radiat Oncol Biol Phys. 103:905–912.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yang L, Shen W and Sakamoto N:
Population-based study evaluating and predicting the probability of
death resulting from thyroid cancer and other causes among patients
with thyroid cancer. J Clin Oncol. 31:468–474. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Edge SB and Compton CC: The American Joint
Committee on Cancer: The 7th edition of the AJCC cancer staging
manual and the future of TNM. Ann Surg Oncol. 17:1471–1474. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Li X, Wan J, Wu Z, Tu J, Hu Y, Wu S and
Lou L: Fatal adverse events with molecular targeted agents in the
treatment of advanced hepatocellular carcinoma: A meta-analysis of
randomized controlled trials. Drug Des Devel Ther. 12:3043–3049.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sfumato P, Filleron T, Giorgi R, Cook RJ
and Boher JM: Goftte: A R package for assessing goodness-of-fit in
proportional (sub) distributions hazards regression models. Comput
Methods Programs Biomed. 177:269–275. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chen Y, Jia Z, Mercola D and Xie X: A
gradient boosting algorithm for survival analysis via direct
optimization of concordance index. Comput Math Methods Med.
2013:8735952013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Hong SM, Cho H, Moskaluk CA and Yu E:
Measurement of the invasion depth of extrahepatic bile duct
carcinoma: An alternative method overcoming the current T
classification problems of the AJCC staging system. Am J Surg
Pathol. 31:199–206. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
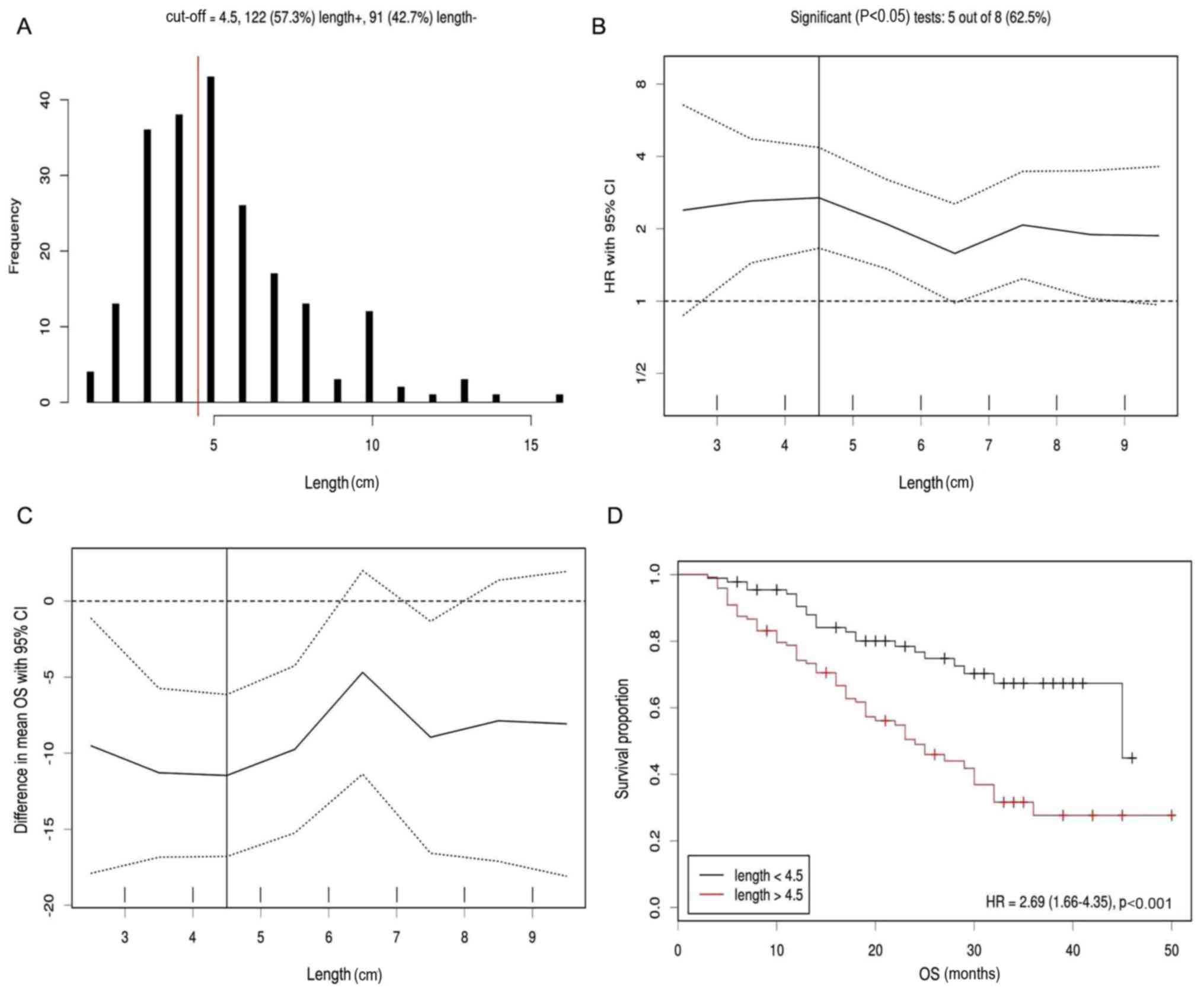
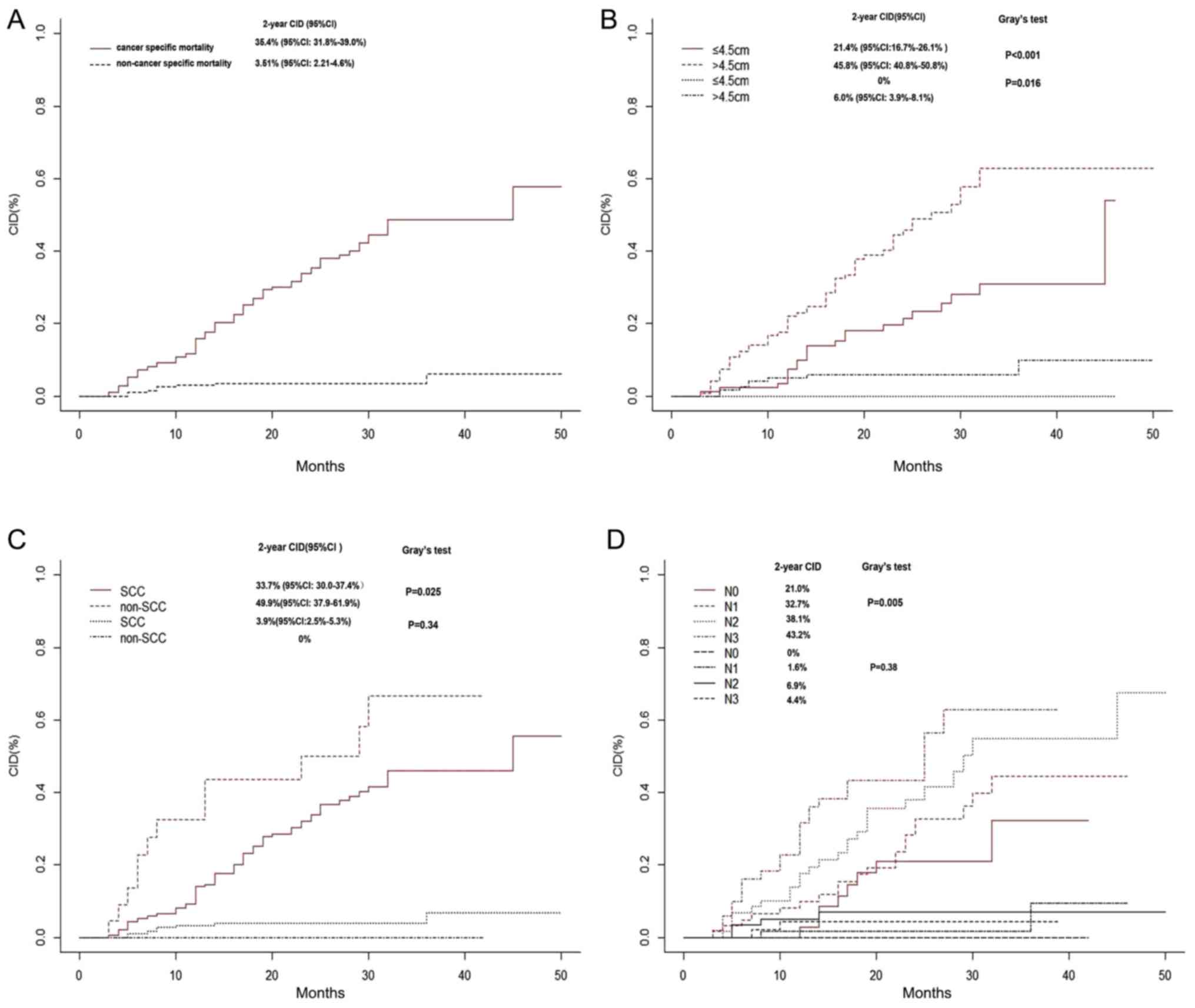
Zhang X, Wang Y, Qu P, Liu-Helmersson J,
Zhao L, Zhang L and Sang S: Prognostic value of tumor length for
cause-specific death in resectable esophageal cancer. Ann Thorac
Surg. 106:1038–1046. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhang X, Wang Y, Jiang Y, Wang Z, Zhao L,
Xue X, Sang S and Zhang L: The prognostic impact of tumor length in
esophageal cancer: Protocol for a systematic review and
meta-analysis. Medicine (Baltimore). 97:e129022018. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wang BY, Liu CY, Lin CH, Hsu PK, Hsu WH,
Wu YC and Cheng CY: Endoscopic tumor length is an independent
prognostic factor in esophageal squamous cell carcinoma. Ann Surg
Oncol. 19:2149–2158. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Gaur P, Sepesi B, Hofstetter WL, Correa
AM, Bhutani MS, Watson TJ and Swisher SG; M. D. Anderson Esophageal
Cancer Group and University of Rochester School of Medicine and
Dentistry Foregut Group, : Endoscopic esophageal tumor length: A
prognostic factor for patients with esophageal cancer. Cancer.
117:63–69. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Koyanagi K, Kato F, Kanamori J, Daiko H,
Ozawa S and Tachimori Y: Clinical significance of esophageal
invasion length for the prediction of mediastinal lymph node
metastasis in Siewert type II adenocarcinoma: A retrospective
single-institution study. Ann Gastroenterol Surg. 2:187–196. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Arigami T, Uchikado Y, Omoto I, Sasaki K,
Kita Y, Owaki T, Yanagita S, Mori S, Kurahara H, Okumura H, et al:
Primary tumor score based on tumor depth and length predicts
prognosis in esophageal squamous cell carcinoma. Anticancer Res.
38:5447–5452. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zhang X, Wang Y, Li C, Helmersson J, Jiang
Y, Ma G, Wang G, Dong W, Sang S and Du J: The prognostic value of
tumor length to resectable esophageal squamous cell carcinoma: A
retrospective study. Peer J. 5:e29432017. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Vadhwana B, Zosimas D, Lykoudis PM, Phen
HM, Martinou M and Khoo D: Tumour length as an independent
prognostic factor in resectable oesophageal carcinoma. Ann R Coll
Surg Engl. 22:1–6. 2019.
|
|
33
|
Xu H, Wu S, Luo H, Chen C, Lin L, Huang H
and Xue R: Prognostic value of tumor length and diameter for
esophageal squamous cell cancer patients treated with definitive
(chemo)radiotherapy: Potential indicators for nonsurgical T
staging. Cancer Med. 8:6326–6334. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Yin H, Li D, Zhu C, Wang M and Wei N:
Factors relevant to the prognosis of patients with esophageal
cancer who received intensity-modulated radiotherapy. Thorac
Cancer. 9:1215–1219. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Shiozaki H, Sudo K, Xiao L, Wadhwa R,
Elimova E, Hofstetter WL, Skinner HD, Lee JH, Weston B, Bhutani MS,
et al: Distribution and timing of distant metastasis after local
therapy in a large cohort of patients with esophageal and
esophagogastric junction cancer. Oncology. 86:336–339. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Sakanaka K, Ishida Y, Itasaka S, Ezoe Y,
Aoyama I, Miyamoto S, Horimatsu T, Muto M and Hiraoka M:
Identification of a predictive factor for distant metastasis in
esophageal squamous cell carcinoma after definitive
chemoradiotherapy. Int J Clin Oncol. 21:899–908. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Chen GZ, Zhu HC, Dai WS, Zeng XN, Luo JH
and Sun XC: The mechanisms of radioresistance in esophageal
squamous cell carcinoma and current strategies in radiosensitivity.
J Thorac Dis. 9:849–859. 2017. View Article : Google Scholar : PubMed/NCBI
|