Introduction
In advanced non-small cell lung cancer (NSCLC),
cytotoxic chemotherapy and epidermal growth factor receptor
(EGFR)-tyrosine kinase inhibitors (TKIs) account for a high
proportion of the treatment regimens (1). Chemotherapy is one of the most
essential treatment strategies for patients without targetable
driver gene mutations and is commonly used following targeted drug
resistance among patients with targetable driver genes (1). Previously, platinum-based doublet
chemotherapy regimens served as the standard first-line treatment;
however, these are considered insufficient, with a response rate of
30–40% and a short progression-free survival (PFS) time ranging
between 5 and 7 months (2–6). Thus, it is crucial to identify and
develop novel markers to predict the efficacy of chemotherapy.
First- and second-generation EGFR-TKIs serve a vital
role in the treatment of advanced NSCLC with EGFR-activating
mutations, demonstrating superior treatment efficacy in this
population compared with traditional chemotherapy (1,7).
However, previous clinical trials have reported that the response
rate of first- or second-generation EGFR-TKIs is ~70%, and PFS time
ranges between 9 and 14 months (7–13). Thus,
numerous patients with EGFR-activating mutations gain limited
treatment benefits from EGFR-TKIs (7–13). In
addition to EGFR-activating mutations, the existing studies
suggested that concomitant mutations may affect the therapeutic
efficacy of first-generation EGFR-TKIs (14).
It was reported that during progression on first- or
second-generation EGFR-TKI treatment, ~60% of patients with initial
EGFR-activating mutations will develop T790M resistance mutations
(15), while the third-generation
EGFR-TKI osimertinib is selective for the T790M mutation. However,
the response rate with osimertinib is 60–70%, and PFS time is ~10
months, while some patients with T790M mutations fail to benefit
from osimertinib treatment (16–18).
Whether concomitant alterations beyond EGFR affect the therapeutic
efficacy of the third-generation EGFR-TKI warrants further
investigation.
Extensive application of next-generation sequencing
(NGS) genotyping in clinical practice and comprehensive genetic
analysis have allowed for the simultaneous discovery of diverse
genetic alterations from only one sample in NSCLC. However, in
addition to the driver genes with targeted agents, the predictive
and prognostic values of other mutated or amplified genes still
remain contradictory. Thus, utilizing genetic alteration profiling
based on NGS, in order to further optimize the selection or
combination of targeted therapy and chemotherapy requires further
research.
Therefore, in addition to sensitive driver gene
status, it is essential to comprehensively take the entire genetic
landscape into account in order to optimize therapeutic strategy.
The present study aimed to retrospectively analyze the association
between the genetic alteration landscape of the tumor and the
treatment outcome of different treatment modalities, including
chemotherapy, and first-, second- and third-generation EGFR-TKIs,
in advanced NSCLC.
Materials and methods
Study design
The present study was approved by The Institutional
Review Board of the Affiliated Tumor Hospital of Guangxi Medical
University (Nanning, China) and conducted in accordance with The
Declaration of Helsinki. Written informed consent was provided by
all patients. The inclusion criteria were as follows: i) IIIB/IV
NSCLC patients; ii) patients received first-line chemotherapy
and/or EGFR-TKIs (either first-, second- or third-generation
EGFR-TKIs) alone or sequentially; and iii) specimens from all
patients were subjected to NGS genotyping prior to specified
treatment. Exclusion criteria were: i) No complete documentation;
ii) specified treatment was adjuvant or neoadjuvant therapy. The
patients' medical records were retrospectively reviewed to identify
eligible patients. A total of 94 patients with advanced NSCLC,
diagnosed between June 2007 and May 2018 at Affiliated Tumor
Hospital of Guangxi Medical University (Nanning, China) were
identified. Fifty-seven (60.6%) were male and 37 (39.4%) were
females, with median age of 58 years (range, 27–80 years). Patients
were grouped into three partially overlapping analysis cohorts
based on treatment regimens, as follows: 64 patients were
classified into the first-line chemotherapy cohort (regardless of
whether targeted therapy was given prior to chemotherapy); 41
patients were classified into the first- or second-generation
EGFR-TKIs cohort (exhibiting EGFR-sensitive mutations prior to
first- or second-generation EGFR-TKIs) and 21 patients were
classified into the third-generation EGFR-TKIs cohort (exhibiting
T790M-positive mutations prior to treatment with osimertinib). A
total of 23 patients were included in two analysis cohorts, while
five patients were simultaneously included in all three analysis
cohorts.
NGS detection
Prior to chemotherapy and/or EGFR-TKI treatment,
baseline peripheral blood, effusion and/or tumor tissues from
included patients were subjected to NGS, targeting 59 genes (ALK,
AKT, APC, AR, ATM, BIM, BRAF, BRCA1, BRCA2, CCND1, CDK4, CDK6,
CDKN2A, CTNNB1, DDR2, EGFR, ERBB2, ESR1, FBXW7, FGFR1, FGFR2,
FGFR3, FLT3, HRAS, IDH1, IDH2, JAK2, KIT, KRAS, MAP2K1, MAP2K2,
MET, MLH1, MSH2, MSH6, MTOR, MYC NF1, NRAS, NTRK1, PDGFRA, PIK3CA,
PMS2, PTCH1, PTEN, PTPN11, RAF1, RB1, RET, ROS1, SMARCA4, SMO, SRC,
STK11, THADA, TP53, TSC1, TSC2, VHL). A median raw average coverage
depth of 600X was achieved for all formalin-fixed paraffin-free
tumor samples and 2,000X was achieved for circulating free DNA
samples. Regarding patients that underwent matched samples NGS
detection at baseline, the genetic alteration status between
matched samples was consistent, with a different variant allele
frequency, of which the higher value was assessed.
Sample collection
For formalin-fixed paraffin-embedded tumor samples,
only samples harbored tumor cell content above 20% were considered
qualified and included. 5–10 ml peripheral blood was collected in
EDTA-coated tubes (BD Biosciences). Plasma was isolated by
fractionating the whole blood by centrifuging at 1,500-2,000 g for
10–15 min at room temperature within 2 h of blood collection and
shipped to Nanjing Geneseeq Technology, Inc., within the next 48 h
(19). Matched malignant pleural
effusion were collected through catheter drainage from the patient.
Samples were also sent to Nanjing Geneseeq Technology Inc.
(Nanjing, Jiangsu, China) for DNA extraction and genetic
testing.
DNA extraction and library
preparation
DNA was extracted from tumor tissue, whole blood or
effusion using the DNeasy Blood & Tissue kit (Qiagen GmbH),
according to the manufacturer's protocol. Purified DNA was
quantified by the Qubit dsDNA HS (High Sensitivity) Assay kit
(Thermo Fisher Scientific, Inc.), according to the manufacturer's
protocols. Sequencing libraries were prepared using the KAPA Hyper
Prep kit (KAPA Biosystems; Roche Diagnostics).
Hybridization capture and
sequencing
Different libraries with unique indices were pooled
together in desirable ratios for up to 2 µg total library input.
Human cot-1 DNA (Thermo Fisher Scientific, Inc.) and xGen Universal
Blocking Oligos (Integrated DNA Technologies, Inc.) were added as
blocking reagents. Customized xGen Lockdown Probes (Integrated DNA
Technologies, Inc.) targeting 59 cancer-associated genes (exons and
selected introns) were used for hybridization enrichment. The
capture reaction was performed with the NimbleGen SeqCap EZ
Hybridization and Wash kit (Roche Applied Science) and Dynabeads
M-270 (Thermo Fisher Scientific, Inc.), according to the
manufacturers' protocols. Captured libraries were on-beads
amplified with Illumina p5 (5′-AATGATACGGCGACCACCGA-3′) and p7
primers (5′-CAAGCAGAAGACGGCATACGAGAT-3′) in KAPA HiFi HotStart
ReadyMix (KAPA Biosystems; Roche Diagnostics). The post-capture
amplified library was purified using Agencourt AMPure XP beads and
quantified via SYBR Green-based qPCR using a KAPA Library
Quantification kit (KAPA Biosystems; Roche Diagnostics). Sequences
of forward and reverse primers were as follows: Forward,
5′-AATGATACGGCGACCACCGA-3′ and reverse,
5′-CAAGCAGAAGACGGCATACGA-3′. Reference gene size of the library
should not exceed 1,000 base pairs (1 kb). The thermocycling
conditions were as follows: Initiation at 95°C for 5 min,
denaturation at 95°C for 30 sec and extension at 60°C for 45
sec repeated for 34 cycles. A total of 0.1X IDTE buffer was used to
dilute the library to 50,000-fold, and this was used as template
for qPCR absolute quantitative detection.
Library fragment size was determined using the
Agilent Technologies 2100 Bioanalyzer (Agilent Technologies, Inc.).
The target-enriched library was then sequenced on the HiSeq4000 NGS
platform (Illumina, Inc.), according to the manufacturer's
protocol.
Sequencing data processing
Trimmomatic was used for FASTQ file quality control
(below 15 or N bases were removed) (20). Reads were then mapped to the
reference Human Genome (hg19) using Burrows-Wheeler Aligner
(BWA-mem, version 0.7.12) (github.com/lh3/bwa/tree/master/bwakit). Local
realignment around the indels and base quality score recalibration
was applied with the Genome Analysis Toolkit version 3.4.0
(software.broadinstitute.org/gatk/), which was also
applied to detect germline mutations. VarScan2 was used for somatic
mutation detection (21). Common
SNPs were filtered out using dbSNP version 137 software (22) and the 1,000 Genomes database,
followed by annotation using ANNOVAR version 2016Apr25 (23). Genomic fusions were identified using
FACTERA version 1.4 with default parameters (24). Copy number variations were detected
using ADTEx version 2.0 (adtex.sourceforge.net) with default parameters
(19).
Study endpoint
The assessed clinical endpoints were as follows:
Objective response rate (ORR), PFS and overall survival (OS). ORR
was defined as the proportion of patients who achieved complete or
partial response, according to the Response Evaluation Criteria in
Solid Tumors (RECIST) guideline (version 1.1) (25). PFS was calculated from the time of
treatment initiation to the progression of the disease (as
determined by means of the RECIST guidelines) or mortality for any
reason. OS was assessed from the date of diagnosis to mortality for
any reason. The date of last follow-up was 1st July 2019.
Statistical analysis
In this study, continuous variables are presented as
median (range) and binary variables were presented as frequency.
Fisher's exact test was used to compare categorical characteristics
between molecular groups, and age was analyzed using the Wilcoxon
rank-sum test. The association between predictive factors and ORR
was assessed using logistic regression. The Kaplan-Meier method and
multivariate Cox proportional hazards regression analysis were
performed to detect predictive factors in PFS and OS. All
statistical analyses were two-sided. P<0.05 was considered to
indicate a statistically significant difference. All analyses were
performed using SPSS version 17.0 (SPSS Inc.).
Results
Association between genetic alteration
status and treatment outcome of first-line chemotherapy
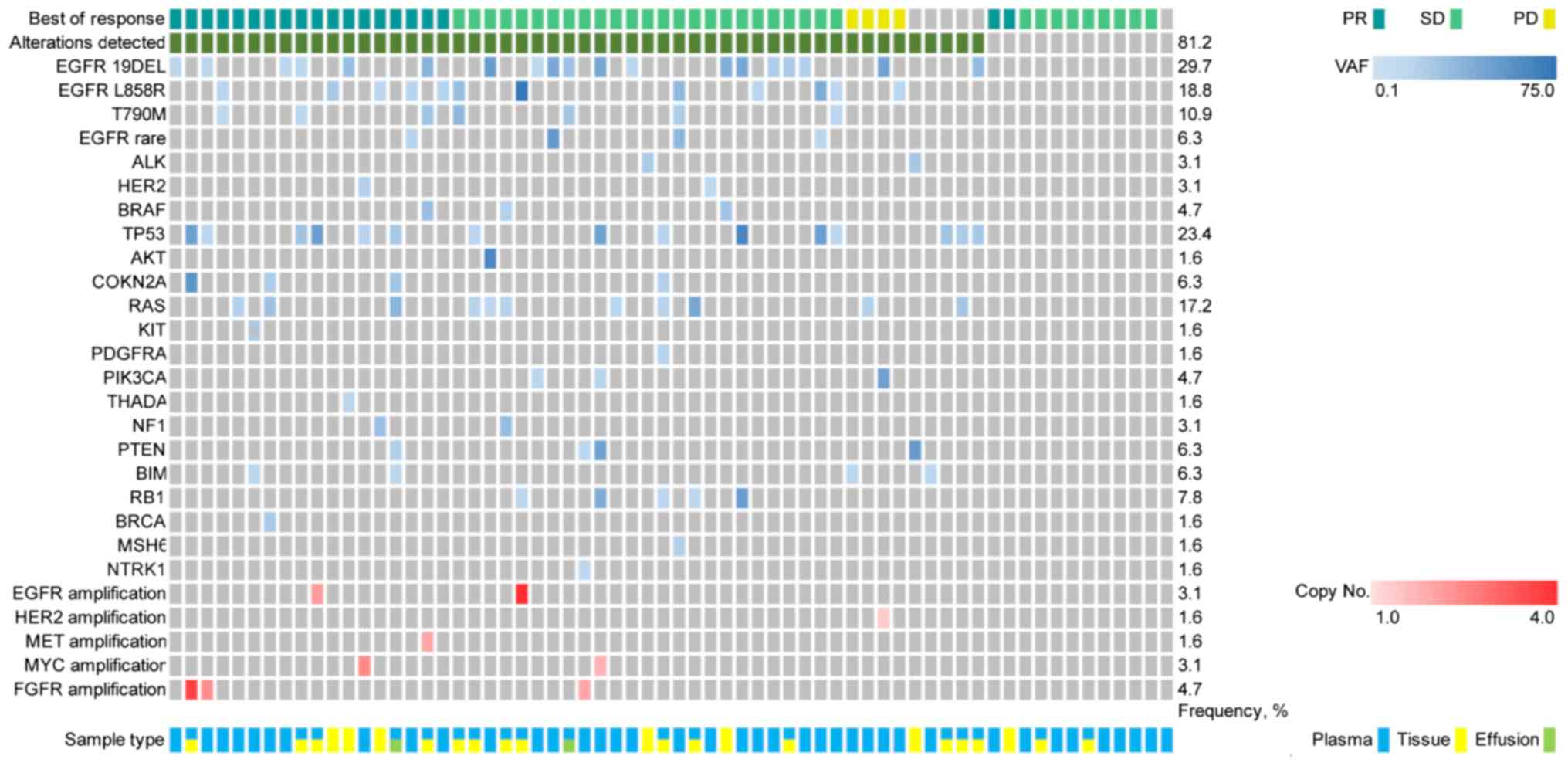
The first-line chemotherapy cohort included 64
patients with advanced NSCLC receiving platinum-based doublet
first-line chemotherapy. The median follow-up on first-line
chemotherapy was 20.3 months (range, 3.0–135.6 months). A total of
52 patients (81.3%) exhibited genetic alterations, whereas 12
patients (18.8%) did not present with any genetic alterations
(Fig. 1). The baseline
characteristics for patients with advanced NSCLC are presented in
Table SI.
The following treatment variables were assessed:
Genetic alterations status (detected or not detected), sex, age
(≤65 or >65 years), smoking status, Eastern Cooperative Oncology
Group (ECOG) performance status (0–1 or 2) (26), histology (squamous or non-squamous
cell carcinoma), clinical stage, number of previous anticancer
regimens for advanced disease (0 or ≥1) and central nervous system
(CNS) metastases (Table SI). The
ORR of first-line chemotherapy was 29.7% (19/64), while no
significant difference was observed between patients with or
without genetic alterations (32.7 vs. 16.7%; P=0.29; Table I).
 | Table I.Treatment outcome for patients with
advanced non-small cell lung cancer receiving first-line
chemotherapy. |
Table I.
Treatment outcome for patients with
advanced non-small cell lung cancer receiving first-line
chemotherapy.
|
|
|
|
| PFS | OS |
|---|
|
|
|
|
|
|
|
|---|
|
|
| ORR | Univariate | Multivariate | Univariate | Multivariate |
|---|
|
|
|
|
|
|
|
|
|---|
| Variable | No., % | No., % | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value |
|---|
| Gene alternation
status |
|
| 0.29 |
| 0.001a |
| 0.0003b |
| 0.87 |
| 0.51 |
| Not
detected | 12 (18.8) | 2 (16.7) |
| 6.68
(2.25–19.82) |
| 4.43
(1.97–10.00) |
| 1.12
(0.31–4.07) |
| 1.64
(0.38–7.17) |
|
|
Detected | 52 (81.3) | 17 (32.7) |
| 1 (Reference) |
| 1 (Reference) |
| 1 (Reference) |
| 1 (Reference) |
|
| ECOG performance
status |
|
| 0.36 |
| 0.02a |
| 0.21 |
| 0.02a |
| 0.03a |
|
0-1 | 57 (89.1) | 18 (31.6) |
| 3.06
(0.57–16.6) |
| 2.32
(0.62–8.70) |
| 2.94
(0.69–12.56) |
| 3.05
(1.10–8.47) |
|
| 2 | 7
(10.9) | 1 (14.3) |
| 1 (Reference) |
| 1 (Reference) |
| 1 (Reference) |
| 1 (Reference) |
|
| CNS metastasis |
|
| 0.22 |
| 0.68 |
| 0.84 |
| 0.04a |
| 0.25 |
| No | 51 (79.7) | 17 (33.3) |
| 1.15 (0.55-
2.38 |
| 0.90
(0.33–2.44) |
| 2.22
(0.68–7.30) |
| 2.03
(0.60–6.82) |
|
|
Yes | 13 (20.3) | 2 (15.4) |
| 1 (Reference) |
| 1 (Reference) |
| 1 (Reference) |
| 1 (Reference) |
|
| Previous anticancer
regimens |
|
| 0.70 |
| 0.07 |
| 0.02a |
| − |
| − |
| 0 | 45 (70.3) | 14 (31.1) |
| 1.80
(0.80–4.06) |
| 2.47
(1.17–5.20) |
| − |
| − |
|
| ≥1 | 19 (29.7) | 5 (26.3) |
| 1 (Reference) |
| 1 (Reference) |
| – |
| – |
|
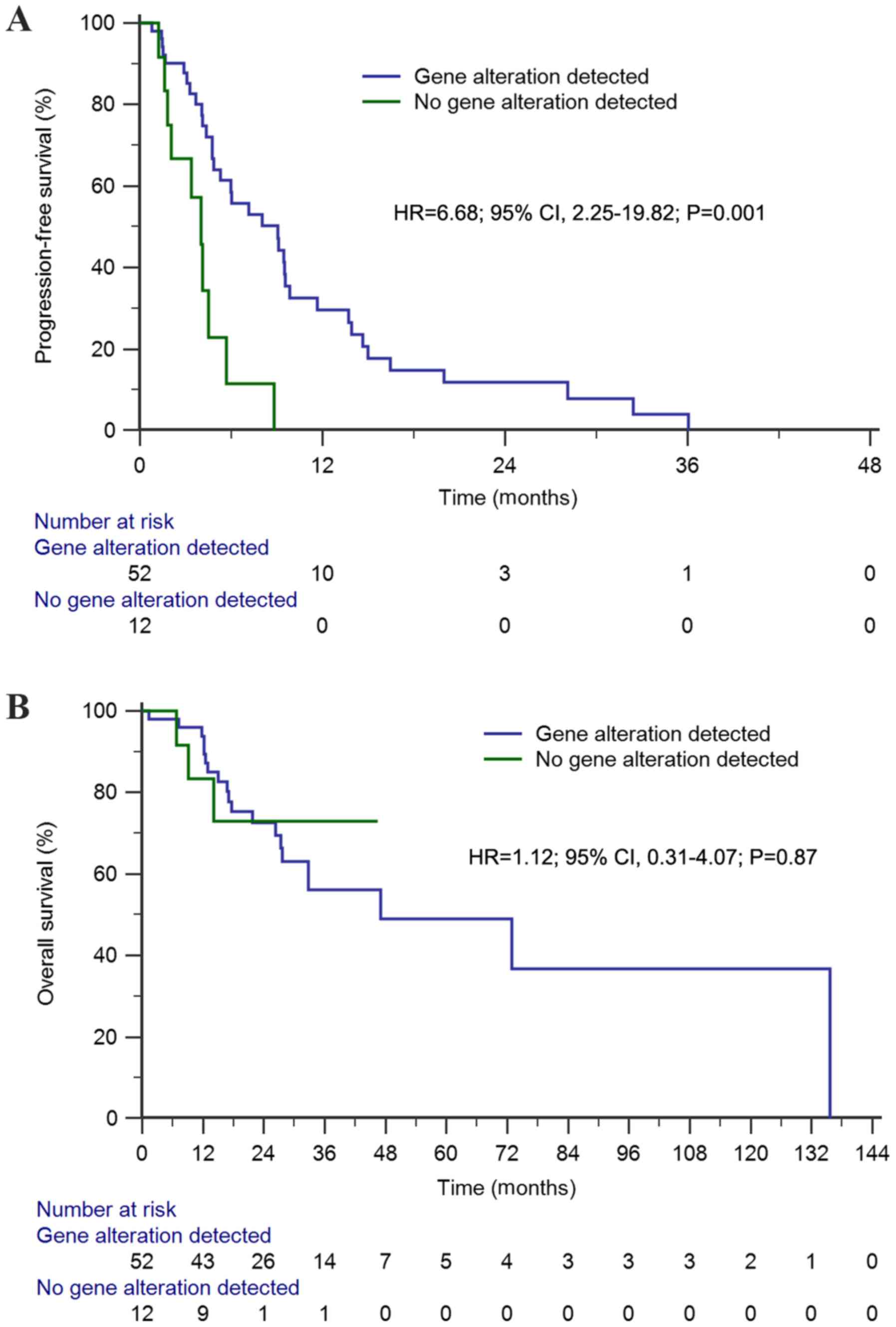
The median PFS time of this cohort was 6.0 months
(95% CI, 3.1–8.9 months). Univariate analysis demonstrated that the
median PFS time of first-line chemotherapy among patients with
genetic alterations was significantly longer than that of patients
without genetic alterations [9.1 vs. 4.0 months; hazard ratio
(HR)=6.68; 95% CI, 2.25–19.82; P=0.001; Fig. 2A). Conversely, genetic alteration
status (HR=4.43; 95% CI, 1.97–10.00; P=0.0003) and receiving
previous anticancer regimens (HR=2.47; 95% CI, 1.17–5.20; P=0.02)
were predictive factors of PFS time in the multivariate analysis
(Table I).
The median OS time of the first-line chemotherapy
cohort was 47.0 months (95% CI, 8.2–85.7 months). Univariate
analysis demonstrated that OS for patients with genetic alterations
was similar to that of patients without genetic alterations (47.0
vs. 47.0 months; HR=1.12; 95% CI, 0.31–4.07; P=0.87; Fig. 2B). Similarly, multivariate analysis
demonstrated that there was no significant difference observed in
OS time (HR=1.64; 95% CI, 0.38–7.17; P=0.51; Table I).
Association between concomitant
alterations and treatment outcome of the first- or
second-generation EGFR-TKIs cohort
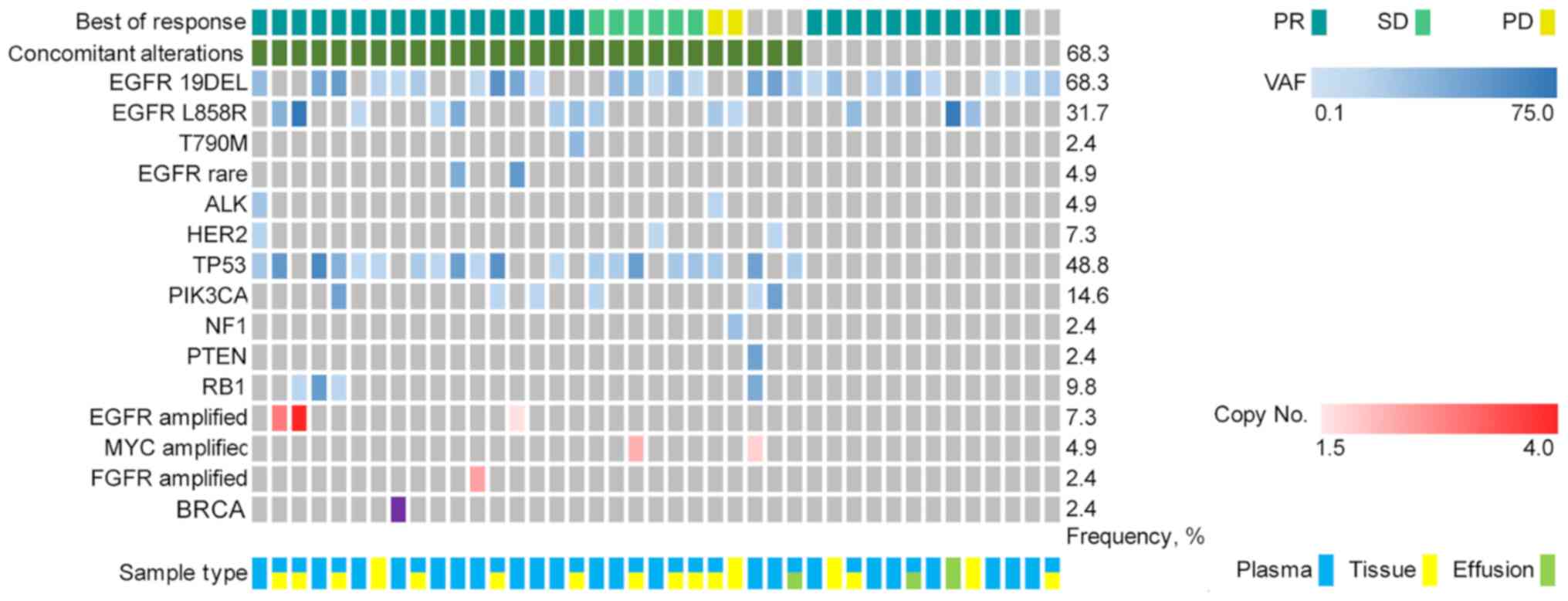
The first- or second-generation EGFR-TKI cohort
included 41 patients with advanced NSCLC exhibiting a positive
EGFR-activating mutation based on NGS and received first- or
second-generation EGFR-TKI targeted therapy. The median follow-up
for the first- or second-generation EGFR-TKIs cohort was 20.4
months (range, 6.0–121.5 months). A total of 28 patients (68.3%)
exhibited concomitant alterations (Fig.
3). The baseline characteristics for patients with EGFR-mutant
advanced NSCLC are presented in Table
SII.
The following treatment variables were assessed:
Genetic alterations, sex, age, smoking status, clinical stage,
number of previous anticancer regimens for advanced disease, EGFR
mutation site (exon 19 deletion or exon 21 mutation) and CNS
metastases (Table SII). The ORR of
the first- or second-generation EGFR-TKIs cohort was 73.2% (30/41).
Although the ORR among patients with concomitant alterations was
lower than that in patients without concomitant alterations, no
significant difference was observed between the two groups (64.3
vs. 92.3%; P=0.07; Table II).
 | Table II.Treatment outcome for patients with
EGFR-mutant advanced non-small cell lung cancer receiving EGFR
tyrosine kinase inhibitors. |
Table II.
Treatment outcome for patients with
EGFR-mutant advanced non-small cell lung cancer receiving EGFR
tyrosine kinase inhibitors.
|
|
|
|
| PFS | OS |
|---|
|
|
|
|
|
|
|
|---|
|
|
| ORR | Univariate | Multivariate | Univariate | Multivariate |
|
|
|
|
|
|
|
|
| Variable | No., % | No., % | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value |
|---|
| Concomitant
alternation status |
|
| 0.07 |
| 0.04a |
| 0.047a |
| 0.01a |
| 0.03a |
| Not
detected | 13 (31.7) | 12 (92.3) |
| 2.14 (95% CI,
1.03–4.44) |
| 2.30
(1.01–5.23) |
| 4.30
(1.41–13.16) |
| 9.20
(1.18–71.50) |
|
|
Detected | 28 (68.3) | 18 (64.3) |
| 1 (Reference) |
| 1 (Reference) |
| 1 (Reference) |
| 1 (Reference) |
|
| Smoking status |
|
| 0.48 |
| 0.04a |
| 0.10 |
| 0.04a |
| 0.13 |
| No | 26 (63.4) | 20 (76.9) |
| 2.02
(0.86–4.76) |
| 2.71
(0.83–8.87) |
| 2.87
(0.87–9.53) |
| 3.95
(0.74–21.10) |
|
|
Yes | 15 (36.6) | 10 (66.7) |
| 1 (Reference) |
| 1 (Reference) |
| 1 (Reference) |
| 1 (Reference) |
|
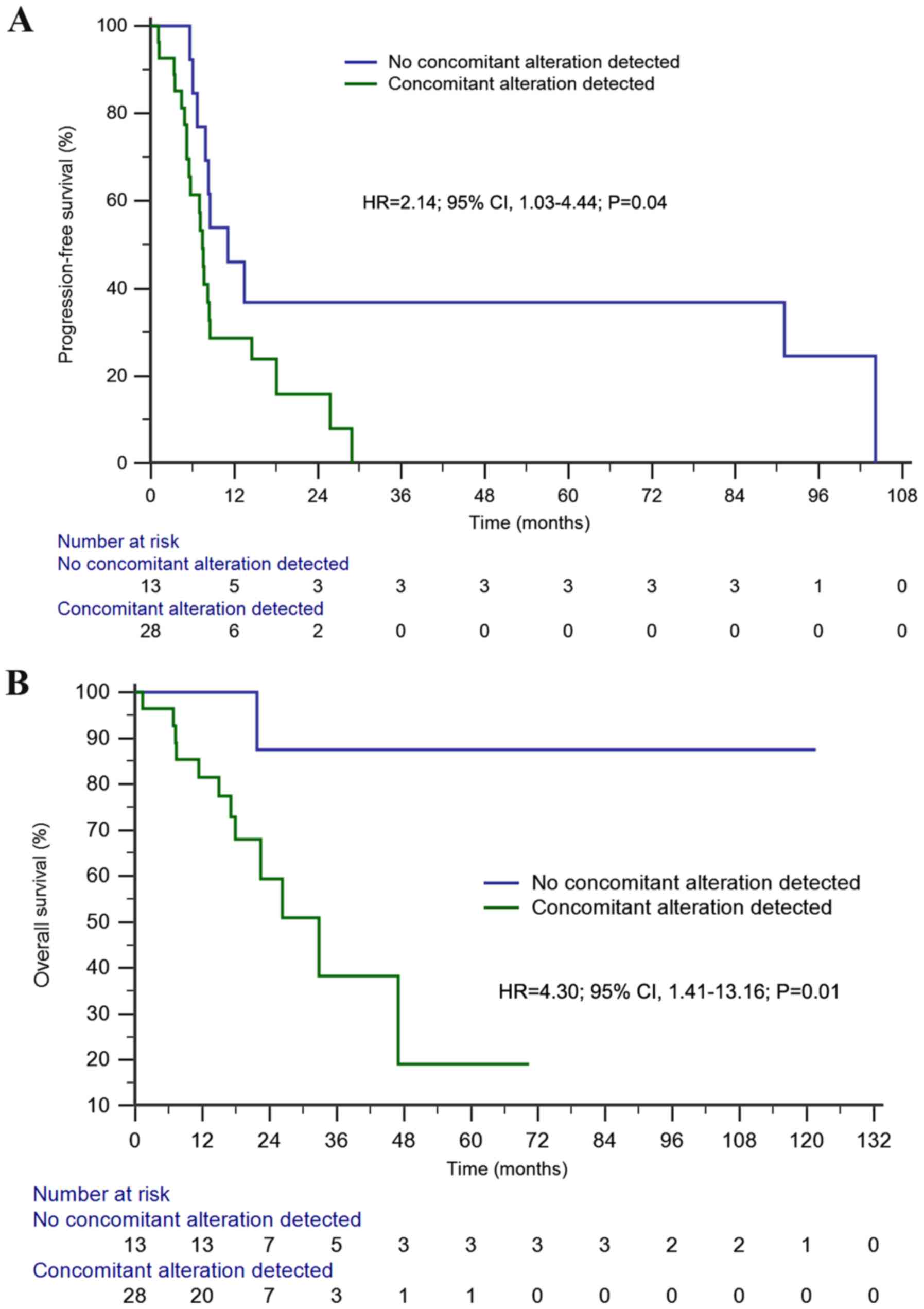
The median PFS time in the first- or
second-generation EGFR-TKIs cohort was 8.1 months (95% CI, 7.1–9.2
months). Univariate analysis demonstrated a significantly longer
PFS time in patients without concomitant alterations than in those
with concomitant alterations (11.1 vs. 7.4 months; HR=2.14; 95% CI,
1.03–4.44; P=0.04; Fig. 4A).
Furthermore, concomitant alterations were the only prognostic
factor of PFS in the multivariate analysis (HR=2.30; 95% CI,
1.01–5.23; P=0.047; Table II).
The median OS time of the first- or
second-generation EGFR-TKIs cohort was not reached. However,
patients without concomitant alterations exhibited a significantly
longer OS time than those with concomitant alterations in both
univariate [not reached (NR) vs. 32.8 months; HR=4.30; 95% CI,
1.41–13.16; P=0.01; Fig. 4B] and
multivariate (HR=9.20; 95% CI, 1.18–71.50; P=0.03) analyses.
Subgroup analysis of the 28 patients with exon 19
deletions indicated a significantly longer PFS (11.1 vs. 7.5
months; HR=2.75; 95% CI, 1.12–6.74; P=0.027; Fig. S1A) and OS time (NR vs. 32.8 months;
HR=6.62; 95% CI, 1.69–26.01; P=0.007; Fig. S1B) in patients without concomitant
alterations compared with those with concomitant alterations.
Multivariate analyses demonstrated that concomitant alterations
were the only prognostic factor of PFS (HR=2.86; 95% CI, 1.08–7.60;
P=0.034) and OS time (HR=11.09; 95% CI, 1.34–91.98; P=0.026) in
patients with exon 19 deletions. Univariate and multivariate
analyses in patients with exon 21 mutations demonstrated that
concomitant alterations had no significant effect on PFS time,
while median OS was not reached (Fig.
S2).
Association between concomitant
alterations and treatment outcome of osimertinib
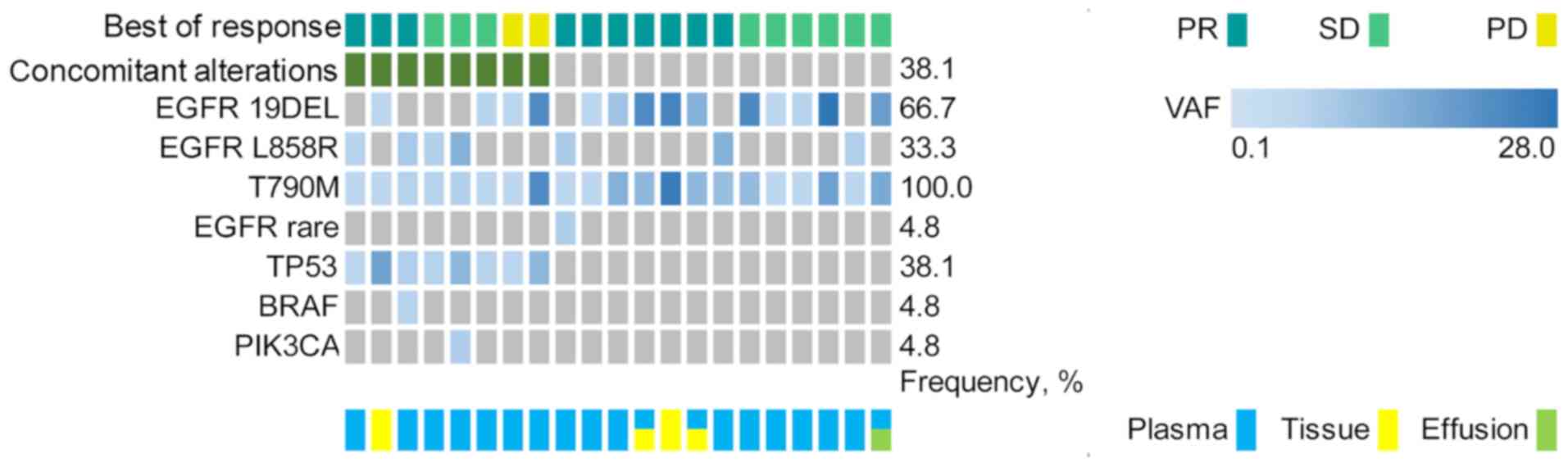
The third-generation EGFR-TKIs cohort included 21
patients with T790M-positive advanced NSCLC who had progressed
disease following exposure to first- or second-generation
EGFR-TKIs. All patients received third-generation EGFR-TKI
osimertinib treatment, with a median follow-up of 32.8 months
(range, 10.7–121.5 months). A total of 8 patients (38.1%) presented
with concomitant alterations beyond EGFR (Fig. 5). Co-occurring EGFR mutation
detection was identified in 14 patients (66.7%) with exon 19
deletions and 7 patients (33.3%) with exon 21 mutations. The
baseline characteristics for patients with T790M-mutant advanced
NSCLC are presented in Table
SIII.
The following treatment variables were assessed:
Concomitant genetic alterations, sex, age, smoking status,
co-occurring EGFR mutation sites and CNS metastases (Table SIII). The ORR of the
third-generation EGFR-TKI osimertinib treatment cohort was 47.6%
(10/21), while the ORRs among patients with and without concomitant
alterations were 37.5% (3/8) and 53.8% (7/13), respectively
(Table III).
 | Table III.Treatment outcome for patients with
T790M-positive advanced non-small cell lung cancer receiving
osimertinib. |
Table III.
Treatment outcome for patients with
T790M-positive advanced non-small cell lung cancer receiving
osimertinib.
|
|
|
|
| PFS | OS |
|---|
|
|
|
|
|
|
|
|---|
|
|
| ORR | Univariate | Multivariate | Univariate | Multivariate |
|---|
|
|
|
|
|
|
|
|
|---|
| Variable | No., % | No., % | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value |
|---|
| Concomitant
alternation status |
|
| 0.47 |
| 0.002a |
| 0.001a |
| 0.03a |
| 0.05 |
| Not
detected | 13 (61.9) | 7 (53.8) |
| 9.48
(2.29–39.28) |
| 24.4
(3.42–174.6) |
| 4.85
(1.16–20.29) |
| 4.93
(0.99–24.52) |
|
|
Detected | 8 | 3 |
| 1 (Reference) |
| 1 (Reference) |
| 1 (Reference) |
| 1 (Reference) |
|
| Co-occurring EGFR
mutation sites |
|
| 0.54 |
| 0.83 |
| 0.04a |
| 0.66 |
| 0.66 |
| Exon 21
mutation | 7 (33.3) | 4 (57.1) |
| 0.89
(0.30–2.62) |
| 0.17
(0.03–0.96) |
| 0.71
(0.16–3.11) |
| 0.69
(0.13–3.56) |
|
| Exon 19
deletion | 14 (66.7) | 6 (42.9) |
| 1 (Reference) |
| 1 (Reference) |
| 1 (Reference) |
| 1 (Reference) |
|
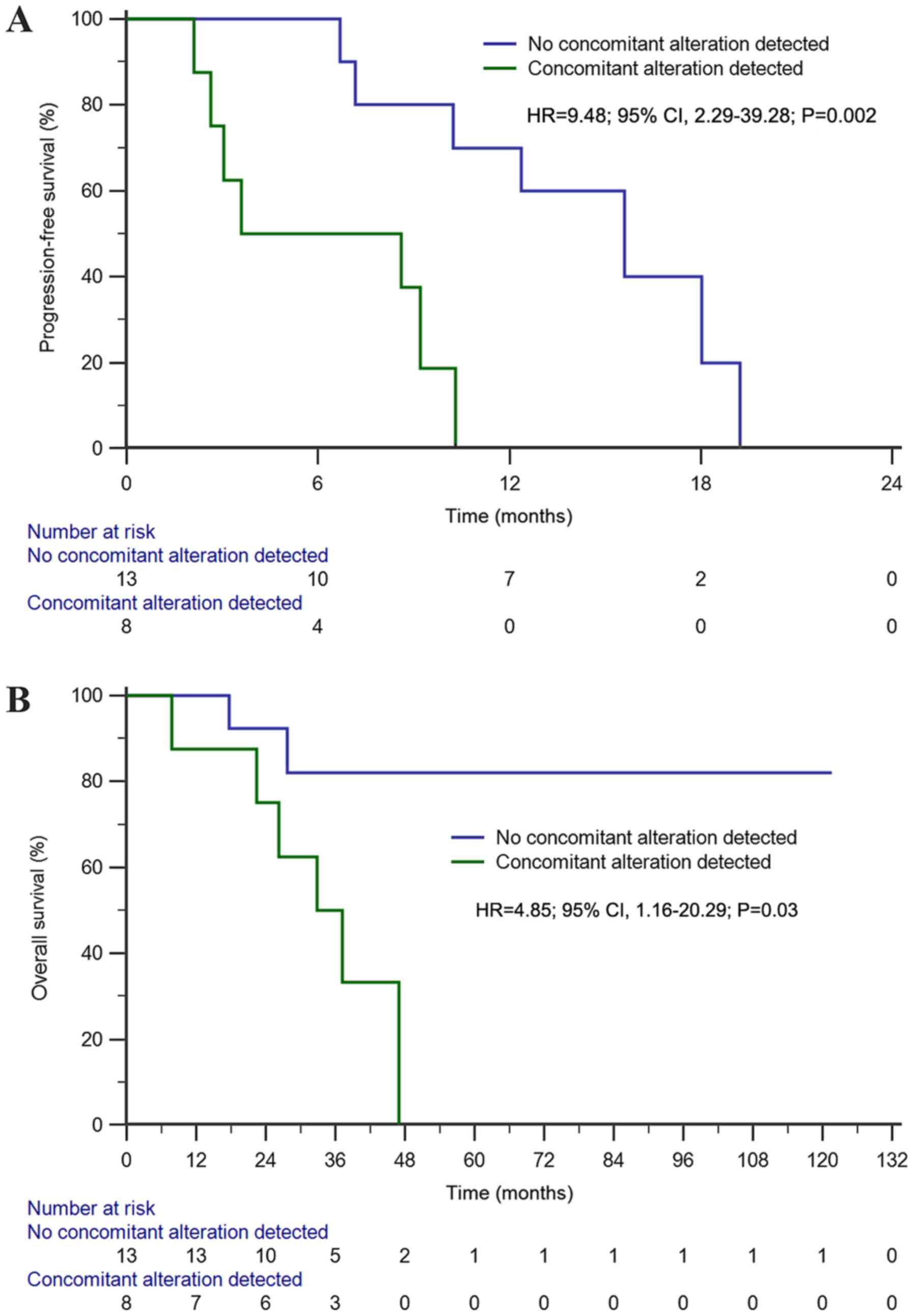
The median PFS time of this cohort was 10.3 months
(95% CI, 8.2–12.4 months). Univariate analysis indicated that
patients without concomitant alterations had a significantly longer
PFS time than those with concomitant alterations (15.6 vs. 3.6
months; HR=9.48; 95% CI, 2.29–39.28; P=0.002; Fig. 6A). Furthermore, concomitant
alterations (HR=24.4; 95% CI, 3.42–174.6; P=0.001) and co-occurring
EGFR mutation sites (HR=0.17; 95% CI, 0.03–0.96; P=0.04) were both
prognostic factors affecting PFS in the multivariate analysis.
The median OS time of the third-generation EGFR-TKI
osimertinib treatment cohort was 47.0 months (95% CI, 29.3–64.6
months). Univariate analysis demonstrated that patients without
concomitant alterations exhibited a significantly longer OS time
than those with concomitant alterations (NR vs. 32.8 months;
HR=4.85; 95% CI, 1.16–20.29; P=0.03; Fig. 6B). Furthermore, concomitant
alterations were the only prognostic factor of OS in the
multivariate analysis (HR=4.93; 95% CI, 0.99–24.52; P=0.05).
Discussion
Analysis of the NGS genotyping results prior to
chemotherapy and EGFR-TKI treatment in the present study
demonstrated that tumor genetic alteration profiling serves vital
roles in both targeted therapy and cytotoxic chemotherapy. A
positive genetic alteration status may significantly prolong PFS
time in patients undergoing first-line chemotherapy. Furthermore,
the presence of concomitant alterations was negatively associated
with therapeutic outcomes of first- and second-generation EGFR-TKIs
treatment. Similarly, concomitant alterations were demonstrated to
affect PFS and OS time for third-generation EGFR-TKIs treatment.
Understanding tumor genetic alteration profiling may improve the
facilitation and development of effective and personalized
therapeutic strategies, and will aid in predicting the therapeutic
outcome either for cytotoxic chemotherapy or EGFR-TKIs in advanced
NSCLC. Thus, genetic sequencing is essential in advanced NSCLC as
it may be insufficient to develop treatment strategies based on
limited genetic information.
Previous studies have reported conflicting results
regarding the association between single gene mutations and
chemotherapy efficacy. It has been demonstrated that patients with
EGFR mutations tend to exhibit longer PFS time than patients
without mutations for first-line chemotherapy (7,27,28).
Regarding KRAS, BRAF and other genetic mutations, the predictive
effect of these genetic alterations on the efficacy of chemotherapy
is also controversial (29–31). However, to the best of our knowledge,
existing evidence has only considered the alteration of a single
gene and came to inconsistent conclusions. To the best of our
knowledge, no study has taken comprehensive genetic profiling into
account to investigate the effect on chemotherapy efficacy in
advanced NSCLC. However, various prognostic models based on genetic
profiling were demonstrated to successfully predict responders to
adjuvant chemotherapy (32,33). With controversy concerning the test
method, study design or sample selection and inconvenience as
multiple specified genes were requested for testing in each model,
the reported genetic models were not widely utilized in clinical
practice. Nevertheless, as cytotoxic agents, chemotherapeutic drugs
exhibit global regulation activities in more than one signaling
pathway (34,35). Notably, in the present study,
categorizing the population receiving first-line chemotherapy based
on the alteration status of the detected genes demonstrated that
patients with genetic alterations exhibited a significantly longer
PFS time following first-line chemotherapy. Currently, the
molecular mechanism by which genetic alterations affect the
treatment outcome of chemotherapy remains unclear, thus further
research is required.
The predictive value of concomitant mutations for
targeted therapy in advanced NSCLC is gaining recognition. Hong
et al (14) reported that
co-occurring mutations beyond EGFR affect the therapeutic efficacy
of first-generation EGFR-TKIs, with lower ORR and shorter PFS and
OS time (14). Furthermore, Wang
et al (36) demonstrated that
accompanied gene aberrations may predict resistance to treatment
with TKIs. Recently, Chen et al (37) confirmed the negative predictive role
of co-occurring driver gene mutations in TKI therapy. Consistent
with these findings, the results of the present study confirmed
that PFS and OS time were significantly shorter in patients with
concomitant alterations than those without concomitant
alterations.
Notably, stratified analysis among patients with
exon 19 deletions indicated that PFS and OS time were significantly
longer among patients without concomitant alterations. However,
analysis among patients with exon 21 mutations failed to
demonstrate a significant effect of concomitant alterations on the
efficacy of EGFR-TKI therapy. However, it is difficult to reach a
definitive conclusion as the small number of cases with exon 21
mutations in the present study may have limited the ability to
detect the impact of concomitant alterations on the efficacy of
EGFR-TKI treatment. It was hypothesized that patients with exon 21
mutations may be more likely to develop other genetic alterations
and activate signaling pathways responsible for TKI resistance,
which is not associated with concomitant alterations. Regarding the
population with exon 19 deletions, the results of the present study
support the notion that the bypass signaling pathway activated by
concomitant alterations may affect the efficacy of TKIs, ultimately
affecting the survival of advanced EGFR-mutant NSCLC (14).
To the best of our knowledge, the present study was
the first to reveal the predictive role of concomitant alterations
on third-generation EGFR-TKI therapy. Among patients with T790M
mutation receiving osimertinib treatment, concomitant alterations
predicted significantly shortened PFS and OS time as compared with
those without concomitant alterations. It was hypothesized that the
bypass pathway activated by concomitant alterations may initiate
rapid drug resistance as even the EGFR pathway is inhibited by
osimertinib, ultimately resulting in poor treatment efficacy and
prognosis among patients with T790M mutation receiving osimertinib.
Patients with T790M-resistant mutations and co-occurring exon 19
deletions exhibited a longer PFS time with osimertinib than
patients with co-occurring exon 21 mutations. Furthermore,
co-occurring EGFR-activating genetic mutation type was one of the
independent prognostic factors for PFS. Similarly, pooled analysis
of two osimertinib studies in T790M-positive NSCLC revealed a trend
toward an increased response rate (70% vs. 57%) and a prolonged PFS
time (11.1 vs. 9.5 months) among patients with co-occurring exon 19
deletions (17,38,39). The
underlying molecular mechanisms of poorer efficacy among patients
with co-occurring exon 21 mutations compared with exon 19 deletions
may be due to a higher number of concomitant genetic alterations
(57.1 vs. 28.6%), which may contribute to the bypass pathway
activation responsible for resistance as we speculation
Several limitations exist within the present study.
First, as it was a retrospective study, patient selection bias may
have attributed to somewhat longer PFS time in the first-line
chemotherapy cohort, while patients receiving different treatments
were included in the three analysis cohorts. Secondly, relatively
small sample sizes of each analysis cohort were used, thus
affecting the reliability of the results. Furthermore, NGS results
based on the targeted gene panel have the potential to miss
information of non-target genes in non-preselected regions, as well
as the possible inability of plasma NGS to detect genetic
alterations, and of tissue NGS to detect genetic heterogeneity in
some cases, which may have affected the accuracy of the results
(40,41).
In conclusion, diverse genetic alteration profiling
in patients with advanced NSCLC identified by NGS resulted in the
discovery of different therapeutic efficacies for different
treatment modes. Positive genetic alterations statuses prior to
first-line chemotherapy were predictive of favorable treatment
outcomes, whereas concomitant alterations indicated poor
therapeutic effect and survival with either first- or
second-generation EGFR-TKI, or third-generation EGFR-TKI treatment.
How genetic alteration profiling of tumors using NGS could guide
the selection and combination of treatment regimens for advanced
NSCLC remains an area for further investigation. Dynamic monitoring
of genetic alteration evolution patterns caused by different
therapeutic drugs, such as chemotherapy or EGFR-TKIs, may help
understand the underlying molecular mechanisms affecting the
efficacy of chemotherapy or EGFR-TKIs, in order to predict and
improve treatment efficacy, and ultimately overcome drug
resistance.
Supplementary Material
Supporting Data
Acknowledgements
The authors would like to thank Dr Dongqing Zhu, Dr
Qiuxiang Ou, Mr. Yong Wu and Miss Lijuan Liu (Nanjing Geneseeq
Technology Inc.) for their technical support.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
WJ, QY, AZ and RN conceived and designed the present
study. WJ, QY, AZ, WZ and HW collected the data, and HW, WZ, CS and
SZ analyzed the data. RN and QY supervised the present study. WJ
drafted the initial manuscript, while QY, AZ, CS and RN
subsequently reviewed and edited the manuscript. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by The Institutional
Review Board of the Affiliated Tumor Hospital of Guangxi Medical
University (Nanning, China), and conducted in accordance with The
Declaration of Helsinki. Written informed consent was provided by
all patients prior to the study start.
Patient consent for publication
Written informed consent was provided by all
patients for their data to be published in the present study.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
NGS
|
next-generation sequencing
|
|
PFS
|
progression-free survival
|
|
OS
|
overall survival
|
|
NSCLC
|
non-small cell lung cancer
|
|
EGFR
|
epidermal growth factor receptor
|
|
TKI
|
tyrosine kinase inhibitor
|
|
ORR
|
objective response rate
|
|
RECIST
|
Response Evaluation Criteria in Solid
Tumors
|
|
CNS
|
central nervous system
|
|
ECOG
|
Eastern Cooperative Oncology Group
|
References
|
1
|
Doroshow DB and Herbst RS: Treatment of
advanced non-small cell lung Cancer in 2018. JAMA Oncol. 4:569–570.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ohe Y, Ohashi Y, Kubota K, Tamura T,
Nakagawa K, Negoro S, Nishiwaki Y, Saijo N, Ariyoshi Y and Fukuoka
M: Randomized phase III study of cisplatin plus irinotecan versus
carboplatin plus paclitaxel, cisplatin plus gemcitabine, and
cisplatin plus vinorelbine for advanced non-small-cell lung cancer:
Four-Arm cooperative study in Japan. Ann Oncol. 18:317–323. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Fossella F, Pereira JR, von Pawel J,
Pluzanska A, Gorbounova V, Kaukel E, Mattson KV, Ramlau R, Szczesna
A, Fidias P, et al: Randomized, multinational, phase III study of
docetaxel plus platinum combinations versus vinorelbine plus
cisplatin for advanced non-small-cell lung cancer: The TAX 326
study group. J Clin Oncol. 21:3016–3024. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Scagliotti GV, Parikh P, von Pawel J,
Biesma B, Vansteenkiste J, Manegold C, Serwatowski P, Gatzemeier U,
Digumarti R, Zukin M, et al: Phase III study comparing cisplatin
plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-I
patients with advanced-stage non-small-cell lung cancer. J Clin
Oncol. 26:3543–3551. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Rodrigues-Pereira J, Kim JH, Magallanes M,
Lee DH, Wang J, Ganju V, Martinez-Barrera L, Barraclough H, van
Kooten M and Orlando M: A randomized phase 3 trial comparing
pemetrexed/carboplatin and docetaxel/carboplatin as first-line
treatment for advanced, nonsquamous non-small cell lung cancer. J
Thorac Oncol. 6:1907–1914. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Scagliotti GV, Gridelli C, de Marinis F,
Thomas M, Dediu M, Pujol JL, Manegold C, San Antonio B, Peterson
PM, John W, et al: Efficacy and safety of maintenance pemetrexed in
patients with advanced nonsquamous non-small cell lung cancer
following pemetrexed plus cisplatin induction treatment: A
cross-trial comparison of two phase III trials. Lung Cancer.
85:408–414. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mok TS, Wu YL, Thongprasert S, Yang CH,
Chu DT, Saijo N, Sunpaweravong P, Han B, Margono B, Ichinose Y, et
al: Gefitinib or carboplatin-paclitaxel in pulmonary
adenocarcinoma. N Engl J Med. 361:947–957. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Maemondo M, Inoue A, Kobayashi K, Sugawara
S, Oizumi S, Isobe H, Gemma A, Harada M, Yoshizawa H, Kinoshita I,
et al: Gefitinib or chemotherapy for non-small-cell lung cancer
with mutated EGFR. N Engl J Med. 362:2380–2388. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mitsudomi T, Morita S, Yatabe Y, Negoro S,
Okamoto I, Tsurutani J, Seto T, Satouchi M, Tada H, Hirashima T, et
al: Gefitinib versus cisplatin plus docetaxel in patients with
non-small-cell lung cancer harboring mutations of the epidermal
growth factor receptor (WJTOG3405): An open label, randomised phase
3 trial. Lancet Oncol. 11:121–128. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhou C, Wu YL, Chen G, Feng J, Liu XQ,
Wang C, Zhang S, Wang J, Zhou S, Ren S, et al: Erlotinib versus
chemotherapy as first-line treatment for patients with advanced
EGFR mutation-positive non-small-cell lung cancer (OPTIMAL,
CTONG-0802): A multicenter, open-label, randomised, phase 3 study.
Lancet Oncol. 12:735–742. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rosell R, Carcereny E, Gervais R,
Vergnenegre A, Massuti B, Felip E, Palmero R, Garcia-Gomez R,
Pallares C, Sanchez JM, et al: Erlotinib versus standard
chemotherapy as first-line treatment for European patients with
advanced EGFR mutation-positive non-small-cell lung cancer
(EURTAC): A multicenter, open-label, randomised multicenter phase 3
trial. Lancet Oncol. 13:239–246. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sequist LV, Yang JC, Yamamoto N, O'Byrne
K, Hirsh V, Mok T, Geater SL, Orlov S, Tsai CM, Boyer M, et al:
Phase III study of afatinib or cisplatin plus pemetrexed in
patients with metastatic lung adenocarcinoma with EGFR mutations. J
Clin Oncol. 31:3327–3334. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wu YL, Cheng Y, Zhou X, Lee KH, Nakagawa
K, Niho S, Tsuji F, Linke R, Rosell R, Corral J, et al: Dacomitinib
versus gefitinib as first-line treatment for patients with
EGFR-mutation-positive non-small-cell lung cancer (ARCHER 1050): A,
randomised open-label, phase 3 trial. Lancet Oncol. 18:1454–1466.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hong S, Gao F, Fu S, Wang Y, Fang W, Huang
Y and Zhang L: Concomitant genetic alterations with response to
treatment and epidermal growth factor receptor tyrosine kinase
inhibitors in patients with EGFR-mutant advanced non-small CELL
lung cancer. JAMA Oncol. 4:739–742. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yu HA, Arcila ME, Rekhtman N, Sima CS,
Zakowski MF, Pao W, Kris MG, Miller VA, Ladanyi M, Riely GJ, et al:
Analysis of tumor specimens at the time of acquired resistance to
EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers.
Clin Cancer Res. 19:2240–2247. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Janne PA, Yang JC, Kim DW, Planchard D,
Ohe Y, Ramalingam SS, Ahn MJ, Kim SW, Su WC, Horn L, et al: AZD9291
in EGFR inhibitor-resistant non-small-cell lung cancer. N Engl J
Med. 372:1689–1699. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ahn MJ, Tsai CM, Shepherd FA, Bazhenova L,
Sequist LV, Hida T, Yang JCH, Ramalingam SS, Mitsudomi T, Jänne PA,
et al: Osimertinib in patients with T790M mutation-positive,
advanced non-small cell lung cancer: Long-Term follow-up from a
pooled analysis of 2 phase 2 studies. Cancer. 15:892–901. 2018.
|
|
18
|
Mok TS, Wu YL, Ahn MJ, Garassino MC, Kim
HR, Ramalingam SS, Shepherd FA, He Y, Akamatsu H, Theelen WS, et
al: Osimertinib or platinum-pemetrexed in EGFR T790M-positive lung
cancer. N Engl J Med. 376:629–640. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yang Z, Yang N, Ou Q, Xiang Y, Jiang T, Wu
X, Bao H, Tong X, Wang X, Shao YW, et al: Investigating novel
resistance mechanisms to third-generation EGFR tyrosine kinase
inhibitor osimertinib in non-small cell lung cancer patients. Clin
Cancer Res. 24:3097–3107. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Bolger AM, Lohse M and Usadel B:
Trimmomatic: A flexible trimmer for Illumina sequence data.
Bioinformatics. 30:2114–2120. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Koboldt DC, Zhang Q, Larson DE, Shen D,
McLellan MD, Lin L, Miller CA, Mardis ER, Ding L and Wilson RK:
VarScan 2: Somatic mutation and copy number alteration discovery in
cancer by exome sequencing. Genome Res. 22:568–576. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sherry ST, Ward MH, Kholodov M, Baker J,
Phan L, Smigielski EM and Sirotkin K: Dbsnp: The NCBI database of
genetic variation. Nucleic Acids Res. 29:308–311. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wang K, Li M and Hakonarson H: ANNOVAR:
Functional annotation of genetic variants from high-throughput
sequencing data. Nucleic Acids Res. 38:e1642010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Newman AM, Bratman SV, Stehr H, Lee LJ,
Liu CL, Diehn M and Alizadeh AA: FACTERA: A practical method for
the discovery of genomic rearrangements at breakpoint resolution.
Bioinformatics. 30:3390–3393. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Eisenhauer EA, Therasse P, Bogaerts J,
Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S,
Moone M, et al: New response evaluation criteria in solid tumours:
Revised RECIST guideline (version 1.1). Eur J Cancer. 45:228–247.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zubrod CG, Schleiderman M, Frei S,
Brindley C, Gold GL, Shnider B, Oviedo R, Gorman J, Jones Jr R,
Jonsson U, et al: Appraisal of methods for the study of
chemotherapy of cancer in man: Comparative therapeutic trial of
nitrogen mustard and triethylene thiophosphoramide. J Chronic Dis.
11:7–33. 1960. View Article : Google Scholar
|
|
27
|
Fukuoka M, Wu YL, Thongprasert S,
Sunpaweravong P, Leong SS, Sriuranpong V, Chao TY, Nakagawa K, Chu
DT, Saijo N, et al: Biomarker analyses and final overall survival
results from a phase III, randomized, open-label, first-line study
of gefitinib versus carboplatin/paclitaxel in clinically selected
patients with advanced non-small-cell lung cancer in Asia (IPASS).
J Clin Oncol. 29:2866–2874. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wu M, Zhao J, Song SW, Zhuo M, Wang X, Bai
H, Wang S, Yang L, An T, Zhang Y, et al: EGFR mutations are
associated with prognosis but not with the response to front-line
chemotherapy in the Chinese patients with advanced non-small cell
lung cancer. Lung Cancer. 67:343–347. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Marabese M, Ganzinelli M, Garassino MC,
Shepherd FA, Piva S, Caiola E, Macerelli M, Bettini A, Lauricella
C, Floriani I, et al: KRAS mutations affect prognosis of
non-small-cell lung cancer patients treated with first-line
platinum containing chemotherap. Oncotarget. 6:34014–34022. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Macerelli M, Caramella C, Faivre L, Besse
B, Planchard D, Polo V, Ngo Camus M, Celebic A, Koubi-Pick V,
Lacroix L, et al: Does KRAS mutational status predict
chemoresistance in advanced non-small cell lung cancer (NSCLC)?
Lung Cancer. 83:383–388. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Cardarella S, Ogino A, Nishino M, Butaney
M, Shen J, Lydon C, Yeap BY, Sholl LM, Johnson BE and Jänne PA:
Clinical, pathologic, and biologic features associated with BRAF
mutations in non-small cell lung cancer. Clin Cancer Res.
19:4532–4540. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Van Laar RK: Genomic signatures for
predicting survival and adjuvant chemotherapy benefit in patients
with non-small-cell lung cancer. BMC Med Genomics. 5:302012.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Zhu CQ, Ding K, Strumpf D, Weir BA,
Meyerson M, Pennell N, Thomas RK, Naoki K, Ladd-Acosta C, Liu N, et
al: Prognostic and predictive gene signature for adjuvant
chemotherapy in resected non-small-cell lung cancer. J Clin Oncol.
28:4417–4424. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Booth L, Poklepovic A and Dent P: Not the
comfy chair! Cancer drugs that act against multiple active sites.
Expert Opin Ther Targets. 23:893–901. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Mun H, Lee SH, Lee CH, Jo SY, Oh JH, Lee
A, Lee B, Jang SJ and Suh YA: Taxotere induces dephosphorylation of
MET in patient-derived tumor models. Anticancer Res. 40:109–119.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Wang Z, Cheng Y, An T, Gao H, Wang K, Zhou
Q, Hu Y, Song Y, Ding C, Peng F, et al: Detection of EGFR mutations
in plasma circulating tumour DNA as a selection criterion for
first-line gefitinib treatment in patients with advanced lung
adenocarcinoma (BENEFIT): A phase 2, single-arm, multicenter
clinical trial. Lancet Respir Med. 6:681–690. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Chen M, Xu Y, Zhao J, Zhong W, Zhang L, Bi
Y and Wang M: Concurrent driver gene mutations as negative
predictive factors in epidermal growth factor receptor-positive
non-small cell lung cancer. Ebiomedicine. 42:304–310. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Yang JCH, Ahn MJ, Kim DW, Ramalingam SS,
Sequist LV, Su WC, Kim SW, Kim JH, Planchard D, Felip E, et al:
Osimertinib in pretreated T790M-positive advanced non-small-cell
lung cancer: AURA study phase II extension component. J Clin Oncol.
35:1288–1296. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Goss G, Tsai CM, Shepherd FA, Bazhenova L,
Lee JS, Chang GC, Crino L, Satouchi M, Chu Q, Hida T, et al:
Osimertinib for pretreated EGFR Thr790Met-positive advanced
non-small-cell lung cancer (AURA2): A multicenter, open-label,
single-arm, phase 2 study. Lancet Oncol. 17:1643–1652. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Marusyk A, Almendro V and Polyak K:
Intra-tumour heterogeneity: A looking glass for cancer? Nat Rev
Cancer. 12:323–334. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Almendro V, Marusyk A and Polyak K:
Cellular heterogeneity and molecular evolution in cancer. Ann Rev
Pathol. 8:277–302. 2013. View Article : Google Scholar
|