Introduction
As a common malignant tumor in the head and neck,
laryngeal cancer (LC) is more common in males over the age of 40
and has a higher incidence rate in Asia compared with other regions
(1). The incidence of LC accounts
for 1% of malignant tumors in the whole body and >5% of head and
neck cancer cases. Despite its low incidence, LC is a threat to
patient quality of life if not treated in a timely manner (2). Current treatment methods include
surgery, radiotherapy, chemotherapy and immunotherapy (3,4). In
clinical practice, patients with LC are often treated with a
combination of different methods; however, surgical excision
remains the main clinical method for treating LC (5). Advancements in laryngectomy procedures
have improved the initial survival rate of patients with LC, and
preserve laryngeal function, which has an impact on quality of life
(6).
Pharyngeal fistula (PF), one of the complications
that occurs after laryngectomy, refers to the formation of an
abscess cavity after surgical resection. PF originates from the
saliva or pus, stored under the subcutaneous or incision tissue
that connects the hypopharynx, esophagus and skin to the sinus
tract, through which saliva or food flows out (7). PF does not only prolong the treatment
time of patients, but also impacts the financial burden of their
family (8). Due to the influence of
laryngectomy on deglutition, patients cannot eat within a short
period of time post-surgery, which leads to slow recovery,
malnutrition and post-operative infection (9). Enteral nutrition support is provided to
patients using a nasogastric feeding tube (NFT), the main method of
nutrition support after laryngectomy, which has a beneficial effect
on post-operative recovery; however, patients using NFT long-term
are prone to malnutrition, which hinders the growth of granulation
tissue (10).
A previous study demonstrated that early oral
feeding provides nutritional support for patients with LC.
Furthermore, the coordination between the muscle groups of the oral
floor and neck during oral feeding is a form of exercise, which
promotes the blood circulation and wound healing. Moreover, the
secretion of saliva and washing of the food passage during feeding
cleans the inner wall of the fistula and promotes the maintenance
of normal bacterial flora in the oral and pharyngeal cavity. This
allows the normal bacterial flora to inhibit the growth of
pathogenic bacteria in the fistula and decreases inflammation
(11). However, the time to commence
oral feeding and whether it has an impact on PF treatment is
unknown.
In the present study, the effect of post-operative
enteral nutrition support nursing combined with early oral feeding
(following a laryngectomy) on the post-operative efficacy and PF
healing of patients with LC was analyzed.
Materials and methods
Patients
The clinical data of 133 patients with LC who
underwent a laryngectomy in The Third Affiliated Hospital, Sun
Yat-Sen University, between May 2014 and September 2016, were
retrospectively analyzed. All patients were diagnosed with LC,
based on the pathology of biopsies, and tumor-node-metastasis (TNM)
staging was performed on patients in accordance with The American
Joint Committee on Cancer criteria (12). Patients (n=133) were divided into two
groups: Control and observation groups. The control group included
61 patients (39 males and 22 females; mean age, 55.84±8.64 years;
age range, 45–68 years). The observation group included 72 patients
(49 males and 23 females; mean age, 56.25±9.35 years; age range,
42–69 years). The present study was approved by the Medical Ethics
Committee of the Third Affiliated Hospital, Sun Yat-Sen University,
and written informed consent was obtained from the
participants.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (i) Patients
>18 years; (ii) patients who had not received preoperative
radiotherapy and chemotherapy; and (iii) patients who complied with
the treatment administered. The exclusion criteria were as follows:
Patients with (i) a family history of genetic diseases; (ii) close
relatives with history of LC; (iii) autism, memory disorders,
hearing disorders and physical disabilities; and (iv) recurrence
and metastasis post-surgery.
Feeding
Patients in the control and observation groups were
observed for a total of 14 days. Patients in the control group were
fed through a NFT for 14 days. In the observation group, the NFT
was removed on the 7th day of nasogastric feeding, and oral feeding
was initiated if no PF appeared within 7 days. Patients in the
observation group were also trained to perform dry swallowing
(swallowing without saliva) six times a day for 10–15 min each
time, depending on their condition. In the early stage of feeding,
patients in the observation group were mainly fed soft food, and
gradually transitioned to normal food (from small and soft food to
large and hard food), under the guidance and training of nursing
staff. Mouthwash (0.9% sodium chloride solution; Hunan Jinjian
Pharmaceutical Co., Ltd.) was used to wash after feeding. Patients
in both groups received routine cefuroxime infusions (1.5 g/8 h;
Sinopharm Zhijun Pharmaceutical Co., Ltd.,), for prophylactic
anti-infective treatment, as well as compound electrolytes and
nutrient solution (intravenous drip (ivgtt), each 1,000 ml contains
5.26 g sodium chloride, 5.02 g sodium gluconate, 3.68 g sodium
acetate, 0.37 g potassium chloride and 0.30 g magnesium chloride;
China Sichuan Kelun Pharmaceutical Co., Ltd.).
Nursing
Patients in the control and observation groups
received nursing care as follows. Routine nursing consisted of
nurses: i) Visiting the patients every hour to observe their
condition; ii) monitoring the vital signs of the patients,
depending on their condition; and iii) cleaning the wound as
appropriate and maintaining its sterility. Nutrition support
nursing consisted of the following: i) Strictly controlling the
rate of nutrient infusion to 25 ml/h in the first 6 h on the 1st
post-operative day to avoid the occurrence of gastric retention;
ii) observing the clinical manifestations in patients and
increasing the infusion rate to 30–60 ml/h if the patient appeared
comfortable; iii) adjusting the patients to a semi-reclining
position to avoid regurgitation of nutrients and maintaining the
gastric tube fixed and unobstructed; iv) maintaining the
temperature of the nutrient solution between 38–40°C using a
heater; and v) rinsing the nasogastric tube with warm water after
infusion and once every 4 h during infusion.
PF processing
In case of PF formation, the necrotic tissues were
cleaned and drained immediately. The airway-associated care was
strengthened, by maintaining the ventilation of the patient and
using auxiliary equipment, when breathing was difficult. The wound
was cleaned using saline (0.9% sodium chloride solution; Hunan
Jinjian Pharmaceutical Co., Ltd.) and hydrogen peroxide (3%). An
in-house antibiotic gauze (applying 400 mg of different antibiotic
ointment evenly on the sterile gauze block with sterile scraper to
cover the PF position) was used to fill the wound with pressure
dressing, depending on the susceptibility of the patient to
infection indicated by their test results of drug sensitivity.
Patients who did not respond to medication were additionally
treated with surgery.
Detection method
Serum albumin (ALB) and pre-albumin (PA) were
detected with a Beckman 5800 system (Beckman Coulter, Inc.). ALB
was detected by bromocresol green method. The principle of this
method is that bromocresol green reacts with albumin to form a
green complex and then the absorbance is read at 600 nm (13). The immunoturbidimetric method was
used to detect PA. The principle of this detection method is that
the antibody (prealbumin PA; cat. no. C079-h; incubated at 37°C for
60 min; China Jilin Changchun Huili Biotechnology Co., Ltd.) reacts
with the soluble antigen to form an immune complex, which becomes
the particle suspended in the reaction solution. The absorbance is
read at 340 nm for the main wave and at 750 nm for the secondary
wave. The kit was purchased from Beijing Jiuqiang Biotechnology
Co., Ltd. (cat. no. GS631M) and was used according to the
manufacturer's instructions. Hemoglobin (Hb) and lymphocyte count
(LYM) were measured with automatic blood routine analyzer XT-2000i
(5 classification; Sysmex Corporation).
Outcome measures
The primary outcome measures were ALB, PA, Hb, LYM
levels and PF healing time. The secondary outcome measures were
occurrences of post-operative infection, adverse reactions, weight,
upper arm muscle circumference (UAMC) and triceps skinfold (TSF).
The primary and secondary outcomes were measured before surgery and
on the 7 and the 14th post-operative days.
Statistical analysis
All statistical analyses were performed using SPSS
software (version 20.0; IBM Corp.) and graphs were drawn using
GraphPad Prism software (version 7.0; GraphPad Software, Inc.).
Measurement data are expressed as the mean ± SD. Data expressed as
rate (%) were assessed by the χ2 and Fisher exact tests.
Independent or paired t-test was used for comparison between and
within two groups, respectively. Repeated measures ANOVA was used
for analysis between more than two groups; Bonferroni correction
was used for post hoc test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Patient characteristics
Comparisons of the clinical data, between patients
in the control and observation groups, revealed no significant
differences in the sex, age, BMI, smoking history, hypertension
history, diabetes history and TNM stage (all P>0.05; Table I). The surgical treatment plans of
two groups were significantly different (P<0.05).
 | Table I.Characteristics of patients in the
control (n=61) and observation (n=72) groups. |
Table I.
Characteristics of patients in the
control (n=61) and observation (n=72) groups.
| Characteristics | Control group, n
(%) | Observation group, n
(%) | t/χ2 | P-value |
|---|
| Sex |
|
| 0.251 | 0.617 |
| Male | 39 (63.93) | 49 (68.06) |
|
|
|
Female | 22 (36.04) | 23 (31.94) |
|
|
| Age, years |
|
| 0.006 | 0.937 |
| ≥55 | 36 (59.02) | 42 (58.33) |
|
|
|
<55 | 25 (40.98) | 30 (41.67) |
|
|
| BMI,
kg/m2 | 22.36±1.25 | 22.84±1.84 | 1.727 | 0.087 |
| Smoking habit |
|
| 0.453 | 0.501 |
| Yes | 39 (63.93) | 50 (69.44) |
|
|
| No | 22 (36.04) | 22 (30.56) |
|
|
| Hypertension |
|
| 1.320 | 0.251 |
| Yes | 50 (81.97) | 53 (73.61) |
|
|
| No | 11 (18.03) | 19 (26.39) |
|
|
| Diabetes
mellitus |
|
| 0.226 | 0.634 |
| Yes | 40 (65.57) | 50 (69.44) |
|
|
| No | 21 (34.43) | 22 (30.56) |
|
|
| TNM stage |
|
| 1.114 | 0.291 |
| T1 | 30 (49.18) | 42 (58.33) |
|
|
| T2 | 31 (50.82) | 30 (41.67) |
|
|
| Surgical program |
|
| 3.957 | 0.047 |
| Total
laryngectomy | 7 (11.48) | 18 (25.00) |
|
|
| Partial
resection | 54 (88.52) | 54 (75.00) |
|
|
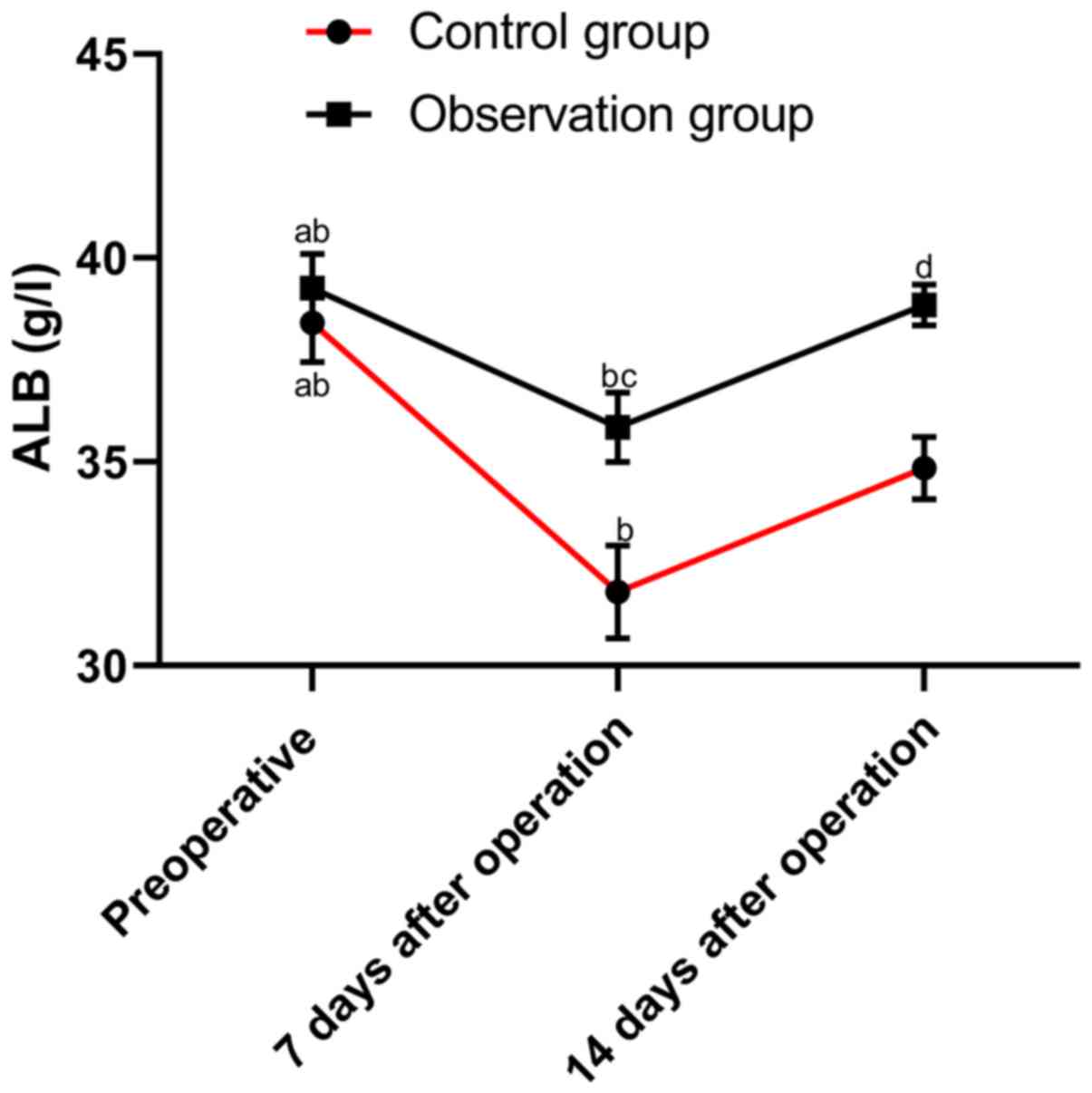
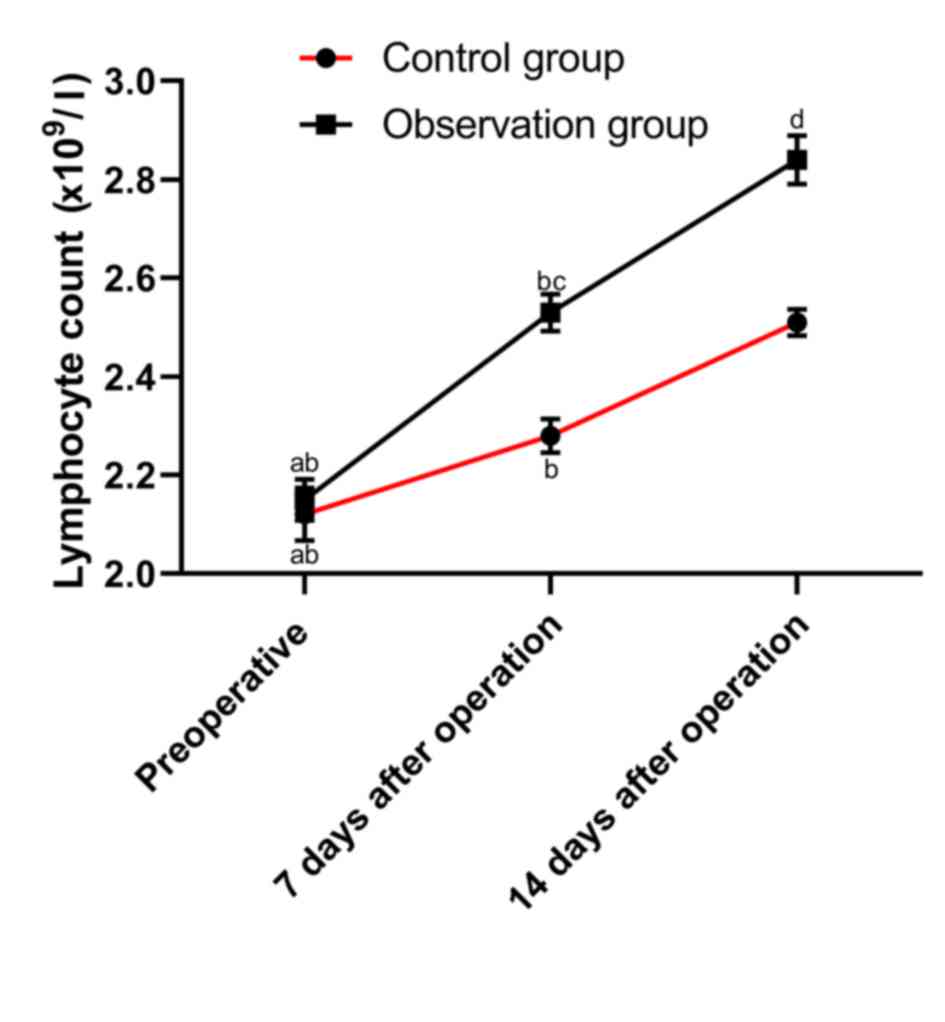
Changes in primary outcomes of
patients with LC
Comparisons between the two groups revealed no
significant differences in ALB, PA, Hb and LYM before surgery (all
P>0.05). ALB, Hb and PA levels were significantly decreased,
whereas LYM was significantly increased, on the 7th post-operative
day in both groups compared with those before surgery (all
P<0.05). ALB, Hb, PA levels and the LYM in the control group
were significantly decreased on the 7th post-operative day compared
with those of the observation group (all P<0.05). On the 14th
post-operative day, PA levels were significantly decreased, whereas
LYM was significantly increased, in both groups compared with those
before surgery (all P<0.05). There were no differences in ALB
and Hb levels in the observation group on the 14th post-operative
day compared with those before surgery (both P>0.05). Meanwhile,
ALB and Hb levels in the control group were significantly decreased
on the 14th post-operative day compared with those before surgery
(both P<0.05). Finally, ALB, Hb, PA levels and LYM were
significantly decreased in the control group on the 14th
post-operative day compared with those in the observation group
(all P<0.05; Figs. 1–4).
PF healing
In the present study, patients presented with PF in
both groups, including five patients in the control group and seven
patients in the observation group. There were no differences in the
average healing times between the control (7.54±2.35 days) and the
observation (7.25±2.01 days) groups, following the treatment for PF
(P>0.05; data not shown).
Analysis of adverse reactions
The number of patients with post-operative
infection, PF, diarrhea, bloating, nausea and vomiting in the
control and observation groups during treatment was not
statistically different (all P>0.05; Table II).
 | Table II.Analysis of adverse reactions in
control and observation groups, n (%). |
Table II.
Analysis of adverse reactions in
control and observation groups, n (%).
| Group | Infection | PF | Diarrhea | Bloating | Nausea | Vomiting |
|---|
| Control group | 2 (3.28) | 5 (8.20) | 2 (3.28) | 1 (1.64) | 3 (4.92) | 2 (3.28) |
| Observation
group | 1 (1.39) | 7 (9.72) | 2 (2.78) | 0 | 1 (1.39) | 2 (2.78) |
| P-value | 0.999 | 0.999 | 0.999 | 0.459 | 0.333 | 0.999 |
Nutritional status indicators
Before surgery, there were no differences in the
weight, UAMC and TSF of patients between the control and
observation groups (all P>0.05). On the 14th post-operative day,
the weight and UAMC in the observation group were significantly
higher than those before surgery (both P<0.05), whereas no
difference in TSF was observed (P>0.05). In the control group,
no differences in weight, UAMC and TSF were demonstrated on the
14th post-operative day compared with those before surgery
(P>0.05). On the 14th post-operative day, the weight and UAMC in
the control group were significantly lower than those of the
observation group (all P<0.05), while there was no difference in
TSF (P>0.05; Table III).
 | Table III.Nutritional status indicators in
control and observation groups before and after surgery. |
Table III.
Nutritional status indicators in
control and observation groups before and after surgery.
|
| Control group | Observation
group |
|---|
|
|
|
|
|---|
| Indicators | Before surgery | Preoperative 7th
day | Before surgery | Preoperative 14th
day |
|---|
| Weight, kg | 50.65±8.64 | 51.35±9.53 | 51.38±10.84 |
55.64±8.62a |
| UAMC, l/cm | 20.53±4.86 | 19.84±4.63 | 20.84±4.66 |
22.81±5.37a |
| TSF, d/mm | 7.62±3.20 | 7.25±2.15 | 7.54±2.93 | 7.15±2.11 |
Discussion
With the development of social economy and industry,
the number of smokers is increasing, which leads to a number of
types of respiratory diseases (14).
LC is a common malignant tumor in the head and neck, most common in
males, and is associated with poor living conditions and smoking
(15). As an important organ in the
respiratory process, the larynx has three functions: Respiration,
deglutition and vocalization. The larynx also plays a role in
protecting the lower respiratory tract (16).
At present, the treatment of early LC is primarily
surgical; however, the direct exposure of the wound to the air
after surgery and the lack of laryngeal protection easily leads to
infection and complications (17).
Furthermore, a previous study has shown that malnutrition is an
important cause of poor wound healing following surgery for head
and neck cancer (18).
Post-operative enteral nutrition support is an
important type of post-operative nutritional care for patients with
LC, and ensures the delivery of nutrients via a feeding tube to
support their daily metabolism and is beneficial for their
prognosis (19). A recent study
demonstrated that early oral feeding provides nutrition for
patients, and has no effect on PF healing; furthermore, this type
of nutritional intake promotes early post-operative rehabilitation,
following resection of tumors in patients with colorectal cancer
(20). Therefore, the present study
investigated the effects of post-operative enteral nutrition
support nursing combined with early oral feeding on the
post-operative efficacy and PF healing time in patients with LC and
identified the optimal treatment and nursing options for the
clinical setting.
In the present study, ALB, PA, Hb levels and LYM
were measured before and after surgery in the control and
observation groups. ALB maintains blood colloid osmotic pressure,
inhibits platelet aggregation and eliminates free radicals in the
body, and is a good indicator of general health (21). The concentration of serum PA reflects
the nutritional status of the body, which is often used as an
important indicator of changes in post-operative nutritional
status. Blood Hb levels partially reflect the nutritional status of
patients (22,23). Furthermore, when the immunity of a
patient is weakened, LYM is decreased and the patient becomes prone
to infections, inhibiting wound healing (24).
The present study demonstrated that the levels of
ALB, Hb, PA and LYM in the control group were significantly reduced
on the 7 and 14th post-operative days compared with those in the
observation group. This indicated improvement in the post-operative
condition of the patients, following nutrition support nursing
combined with early oral feeding, in contrast to the combination
with nasogastric feeding. This finding was consistent with the
study by Süslü and Şefik Hoşal (25), which reported ameliorative effects on
the immune system and nutritional status of patients following
early oral feeding. Furthermore, the present study demonstrated no
difference in the average PF healing time between the two groups.
However, it was speculated that the cause of PF in patients may be
associated with the surgical method and the age of the patient. A
study by Seven et al (26)
indicated there was no effect on PF in patients following oral
feeding on the 7th post-operative day. Additionally, a study by
Kishikova and Fleming (27) also
demonstrated that early oral feeding had no effect on PF healing.
The aforementioned studies are consistent with the results obtained
in the present study. Statistical analysis on the adverse reactions
of patients in the two groups demonstrated no differences between
the two groups post-operatively, which might be influenced by the
small sample size.
Finally, the weight, UAMC and TSF of patients in the
two groups were compared. UAMC and TSF were important indicators
that determine the development of subcutaneous fat and total
protein storage (28). It was
demonstrated that there were no changes in the weight, UAMC and TSF
in the control group following surgery. In the observation group,
no differences were observed in TSF before and after surgery.
Meanwhile, the weight and UAMC in the observation group were
significantly increased after surgery compared with those before
surgery and those in the control group. These results suggested
that early oral feeding exhibited beneficial effects compared with
enteral nutrition support nursing combined with nasogastric
feeding.
However, the short observation time, lack of
long-term follow-up, lack of complete understanding of the details
of the patient's change in condition, and the small sample size are
limitations of the present study. Moreover, the scope of surgical
resection and the chemoradiation regimens of phase 1 and 2 were not
consistent, which may affect the results. In addition, the main
cause of PF in patients is unclear. Therefore, future studies
including a longer follow-up time and larger sample size are
warranted. Furthermore, patient grouping according to the scope of
surgical resection is required and risk factors of PF require
further investigation. This will allow the investigation of
independent risk factors and the verification of the findings from
the present study.
In conclusion, post-operative enteral nutrition
support nursing combined with early oral feeding significant
improved the post-operative outcomes of patients with LC and had no
effect on PF healing.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AL was the guarantor of integrity of the entire
study, and contributed to the study concepts, study design, data
acquisition and manuscript preparation. JY was responsible for data
collection and analysis as well as manuscript writing and revision.
ZW contributed to the experimental studies, literature research and
clinical studies. PL performed the statistical analysis and data
analysis. The final version of the manuscript has been read and
approved by all authors.
Ethical approval and consent to
participate
The present study was approved by the Ethics
Committee of the Third Affiliated Hospital, Sun Yat-Sen University.
All patients provided informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
PF
|
pharyngeal fistula
|
|
LC
|
laryngeal cancer
|
|
ALB
|
albumin
|
|
PA
|
pre-albumin
|
|
Hb
|
hemoglobin
|
|
LYM
|
lymphocyte count
|
|
UAMC
|
upper arm muscle circumference
|
|
TSF
|
triceps skinfold
|
|
TNM
|
tumor-node-metastasis
|
References
|
1
|
Xuan L, Qu L, Zhou H, Wang P, Yu H, Wu T,
Wang X, Li Q, Tian L, Liu M and Sun Y: Circular RNA: A novel
biomarker for progressive laryngeal cancer. Am J Transl Res.
8:932–939. 2016.PubMed/NCBI
|
|
2
|
Siegel R, Ma J, Zou Z and Jemal A: Cancer
statistics, 2014. CA Cancer J Clin. 64:9–29. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yang R: Corruption in China's higher
education system: A malignant tumor. US-China Educ Rev. 2:18–21.
2015.
|
|
4
|
Metelmann HR, Woedtke TV, Kai M, Hyckel P
and Podmelle F: Immunotherapy and immunosurveillance of oral
cancers: Perspectives of plasma medicine and mistletoe. Cancer
Immunol. 313–318. 2015.
|
|
5
|
Timme DW, Jonnalagadda S, Patel R, Rao K
and Robbins KT: Treatment selection for T3/T4a laryngeal cancer:
Chemoradiation versus primary surgery. Ann Otol Rhinol Laryngol.
124:845–851. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Elegbede AI, Rybicki LA, Adelstein DJ,
Kaltenbach JA, Lorenz RR, Scharpf J and Burkey BB: Oncologic and
functional outcomes of surgical and nonsurgical treatment of
advanced squamous cell carcinoma of the supraglottic larynx. JAMA
Otolaryngol Head Neck Surg. 141:1111–1117. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dedivitis RA, Aires FT, Cernea CR and
Brandão LG: Pharyngocutaneous fistula after total laryngectomy:
Systematic review of risk factors. Head Neck. 37:1691–1697. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Goepfert RP, Hutcheson KA, Lewin JS, Desai
NG, Zafereo ME, Hessel AC, Lewis CM, Weber RS and Gross ND:
Complications, hospital length of stay, and readmission after total
laryngectomy. Cancer. 123:1760–1767. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Stankovic M, Milisavljevic D, Zivic M,
Stojanov D and Stankovic P: Primary and salvage total laryngectomy.
Influential factors, complications, and survival. J BUON.
20:527–539. 2015.PubMed/NCBI
|
|
10
|
van der Linden NC, Kok A,
Leermakers-Vermeer MJ, de Roos NM, de Bree R, van Cruijsen H and
Terhaard CH: Indicators for enteral nutrition use and prophylactic
percutaneous endoscopic gastrostomy placement in patients with head
and neck cancer undergoing chemoradiotherapy. Nutr Clin Pract.
32:225–232. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hay A, Pitkin L and Gurusamy K: Early
versus delayed oral feeding in patients following total
laryngectomy. Adv Otolaryngol. 2014:P1–P10. 2015. View Article : Google Scholar
|
|
12
|
Yang X, Ren GX, Zhang CP, Zhou GY, Hu YJ,
Yang WJ, Guo W, Li J and Zhong LP: Neck dissection and
post-operative chemotherapy with dimethyl triazeno imidazole
carboxamide and cisplatin protocol are useful for oral mucosal
melanoma. Bmc Cancer. 10:6232010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lang L, Li X, Luo X, Du J, Huang Y, Cao D
and Li M: Comparison of test results and performances of hitachi
7600 and beckman olympus 5800 automatic biochemical analyzers. Int
J Clin Exp Med. 11:5095–5102. 2018.
|
|
14
|
Holland AE, Spruit MA, Troosters T, Puhan
MA, Pepin V, Saey D, McCormack MC, Carlin BW, Sciurba FC, Pitta F,
et al: An official European Respiratory Society/American Thoracic
Society technical standard: Field walking tests in chronic
respiratory disease. Eur Respir J. 44:1428–1446. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Møller PK, Tolstrup JS, Olsen MH, Dalton
SO, Overgaard J and Johansen J: Predictors of continuous tobacco
smoking in a clinical cohort study of Danish laryngeal cancer
patients smoking before treated with radiotherapy. Acta Oncologica.
54:685–692. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Mattsson P, Hydman J and Svensson M:
Recovery of laryngeal function after intraoperative injury to the
recurrent laryngeal nerve. Gland Surg. 4:27–35. 2015.PubMed/NCBI
|
|
17
|
Sotirović J, Šuljagić V, Baletić N,
Pavićević L, Bijelić D, Erdoglija M, Perić A and Soldatović I: Risk
factors for surgical site infection in laryngeal cancer surgery.
Acta Clin Croat. 54:57–64. 2015.PubMed/NCBI
|
|
18
|
Ackerman D, Laszlo M, Provisor A and Yu A:
Nutrition management for the head and neck cancer patient. Cancer
Treat Res. 174:187–208. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wiggs CM: Case study: Baby John-nursing
reflections on moral angst. Nurs Ethics. 18:606–612. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sousa AA, Porcaro-Salles JM, Soares JM,
Meyer de Moraes G, Souza Silva G, Abreu Sepulcri R, Rezende
Carvalho J and Savassi-Rocha PR: Tolerance of early oral feeding in
patients subjected to total laryngectomy. Head Neck. 38 (Suppl
1):E643–E648. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Huang J, Lin L, Sun D, Chen H, Yang D and
Li Q: ChemInform abstract: Bio-inspired synthesis of metal
nanomaterials and applications. Chem Soc Rev. 44:6330–6374. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Isshiki M, Hirayama S, Ueno T, Ito M,
Furuta A, Yano K, Yamatani K, Sugihara M, Idei M and Miida T:
Apolipoproteins C-II and C-III as nutritional markers unaffected by
inflammation. Clin Chim Acta. 481:225–230. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Minekus M, Alminger M, Alvito P, Balance
S, Bohn T, Bourlieu C, Carrière F, Boutrou R, Corredig M, Dupont D,
et al: A standardised static in vitro digestion method suitable for
food-an international consensus. Food Funct. 5:1113–1124. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Iwata E, Shigematsu H, Yamamoto Y, Tanaka
M, Okuda A, Morimoto Y, Masuda K, Nakajima H, Koizumi M and Tanaka
Y: Lymphocyte count at 4 days postoperatively: A reliable screening
marker for surgical site infection following posterior lumbar
decompression surgery. Spine (Phila Pa 1976). 43:E1096–E1101.
2018.PubMed/NCBI
|
|
25
|
Süslü N and Şefik Hoşal A: Early oral
feeding after total laryngectomy: Outcome of 602 patients in one
cancer center. Auris Nasus Larynx. 43:546–550. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Seven H, Calis AB and Turgut S: A
randomized controlled trial of early oral feeding in
laryngectomized patients. Laryngoscope. 113:1076–1079. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kishikova L and Fleming JC: Oral feeding
following laryngectomy: Early or delayed? Int J Surg. 12:1137–1140.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Anoop S, Misra A, Bhatt SP, Gulati S,
Mahajan H and Prabakaran G: High plasma glucagon levels correlate
with waist-to-hip ratio, suprailiac skinfold thickness, and deep
subcutaneous abdominal and intraperitoneal adipose tissue depots in
nonobese Asian Indian males with type 2 diabetes in North India. J
Diabetes Res. 2017:23760162017. View Article : Google Scholar : PubMed/NCBI
|