Introduction
Undifferentiated embryonal sarcoma of the liver
(UESL) is an aggressive disease that accounts for <0.2% of all
primary liver tumors (1). UESL was
first described as a mesenchymoma by Donovan and Santulli (2) in 1946, and was subsequently termed
malignant mesenchymoma by Stout (3)
in 1948 before being first recognized as a distinct form of sarcoma
by Stocker and Ishak (4) in
1978.
UESL predominantly develops in the childhood, with a
peak incidence between 6 and 10 years of age (4); however, it also occasionally occurs in
adults (5). UESL usually manifests
with nonspecific clinical presentations and preoperative
examination results (3–5). The majority of the relevant studies
involve pediatric cases and have reported a poor prognosis, even in
patients who undergo complete surgical resection of the tumor
(4,5). However, patient prognosis has recently
been improved using therapeutic strategies combining surgery with
chemotherapy, especially with neoadjuvant chemotherapy.
UESL in adults is extremely rare; to the best of our
knowledge, the currently available literature includes only 108
reported cases of UESL in adult patients. Due to the low incidence
of UESL, especially among adults, the majority of the literature
comprises case reports, with a limited number of small case series.
Therefore, limited data are available regarding the prognosis of
adults patients with UESL, especially in terms of 1-, 3- and 5-year
survival rates. The effects of chemotherapy or neoadjuvant
chemotherapy on UESL in the adult population also remain unclear.
To improve the prognosis of these patients, more cases and
treatment experiences should be reported.
The present study aimed to analyze a
single-institution retrospective case series of UESL in adults,
which was one of the largest reported series to date and included
the first report of overall survival in this population, as well as
to perform a systematic review of the literature to investigate the
presentation, treatment modalities and outcomes of this rare
tumor.
Materials and methods
Retrospective analysis
A retrospective review was conducted of three cases
of UELS in patients >15 years of age treated at the Center of
Hepatopancreatobiliary Diseases of Beijing Tsinghua Changgung
Hospital between 2015 and 2018. The recorded data included the
demographic (age and sex) and clinical characteristics of the
patients, including the year of diagnosis, signs and symptoms at
presentation, laboratory data, imaging results, tumor extension,
type of surgery, tumor size, pathology reports, use of chemotherapy
and interventional therapy, presence and location of recurrence,
and the duration of overall survival in months. These results are
presented as a descriptive analysis of a case series.
Systematic review
A systematic review of the available literature was
performed using MEDLINE, Web of Science, Embase, the Google Scholar
database and the Cochrane Library to search for all published
studies regarding UELS. The PRISMA guidelines were followed
(http://www.prisma-statement.org/). The
search terms were ‘undifferentiated embryonal sarcoma’ and ‘adult’.
The inclusion criteria were as follows: English or Chinese
language, human studies, adult patients (≥15 years), full-text
availability and completeness of clinical data. Studies lacking
primary data were excluded, but were examined to identify any
relevant citations. Data extraction from relevant studies was
performed to search for additional studies. The search was
independently performed by two authors, and disagreements regarding
study inclusion were resolved through discussion among all authors.
The aforementioned clinical parameters from the cases in the
included studies were evaluated.
Statistical analysis
Statistical analyses and graphing were performed
using GraphPad Prism 7.0 software (GraphPad Software, Inc.).
Survival was estimated using the Kaplan-Meier method, and the
results were compared using the two-sided log-rank test. P<0.05
was considered to indicate a statistically significant
difference.
Results
Retrospective analysis of a case
series
Demographic and clinical characteristics
As presented in Table
I, the three adult patients with UELS were female, with a mean
age of 21 years at diagnosis (range, 15–25 years). Symptoms upon
admission included fever, chills, nausea, vomiting and weight loss
(patient A), and abdominal pain and mass (patients B and C).
Laboratory analysis revealed elevated levels of alkaline
phosphatase (ALP, patient A), activated partial thromboplastin
time/prothrombin time (patients B and C), aspartate
aminotransferase, alanine aminotransferase, direct bilirubin, ALP
and γ-glutamyl transpeptidase (patient C), as well as decreased
albumin, red blood cell count, hemoglobin and red blood
cell-specific volume (patient C). Tumor marker levels were normal
in patients A and C, whereas the level of protein induced by
vitamin K absence or antagonist-II (PIVKA-II) was elevated outside
of the normal range in patient C. In all patients, ultrasound
examination and computed tomography revealed a cystic and solid
mass.
 | Table I.Demographic and clinical
characteristics of the patients with undifferentiated embryonal
sarcoma of the liver in the retrospective case series. |
Table I.
Demographic and clinical
characteristics of the patients with undifferentiated embryonal
sarcoma of the liver in the retrospective case series.
| No. | Age, years | Sex | Symptoms | Laboratory test
results | Tumor markers | US findings | CT findings |
|---|
| A | 15 | F | Fever, chill,
nausea, vomiting, weight loss | ↑ALP | Normal | N.A. | Cystic and solid
mass |
| B | 24 | F | Abdominal pain and
mass | ↑PT, APTT | Normal | Cystic and solid
mass | Mass with
enhancement in solid parts |
| Ca | 25 | F | Abdominal pain and
mass | ↑PT, APTT, AST,
ALT, DBIL, ALP, GGT; ↓ALB, RBC, HGB, HCT | ↑PIVKA-II | N.A. | Lobulated low
enhancement mass |
Treatment and outcome
Table II summarizes
the treatments and outcomes of the three patients. One patient was
admitted to the hospital for recurrent UESL. The lesions involved
the right lobe in two cases and the left lobe in one case. One
patient had undergone biopsy and neoadjuvant chemotherapy
(vincristine, cytoxan and cis-platinum) prior to admission. Two
patients received preoperative transarterial chemoembolization.
Surgical treatment involved right trisectionectomy in two cases,
and extended left hemihepatectomy in one case. Two patients
received postoperative chemotherapy (dacarbazine plus lobaplatin or
doxorubicin, ifosfamide, mesna and dacarbazine). One patient
underwent postoperative hepatic artery infusion chemotherapy.
 | Table II.Treatment and outcome of the patients
with undifferentiated embryonal sarcoma of the liver in the
retrospective case series. |
Table II.
Treatment and outcome of the patients
with undifferentiated embryonal sarcoma of the liver in the
retrospective case series.
| No. | Year of
diagnosis | Tumor
extension | Biopsy | Treatment before
surgery | Type of
surgery | Treatment after
surgery | Recurrence | Outcome | OS, months |
|---|
| A | 2016 | R + L | + | VCR + CTX + PDD;
TACE | Right
trisectionectomy | – | No | Alive | 41 |
| B | 2017 | L | – | – | Extended left
hemihepatectomy | DTIC + LBP; HAIC
(EPI + L-OHP) | Lung | Dead | 17 |
| C | 2018 | R + La | – | TACE | Right
trisectionectomy | AIM, AIDM | Lung, inguinal
LN | Alive | 9 |
Two patients experienced recurrence, with one in the
lung and the other in the lung plus inguinal lymph nodes. Two
patients are currently alive after follow-up, one after 9 months of
follow-up and the other after 41 months of follow-up. One patient
succumbed to pulmonary recurrence at 17 months.
Pathological characteristics
In one case, the tumor size was <10 cm; in the
other two cases, the tumor size was >20 cm. The tumor in one
case exhibited visible capsule infiltration and tumor thrombus
(portal vein and hepatic vein). Immunohistochemical results
revealed expression of the cytokeratin antibody AE1/AE3, the
melanoma antibody HMB45 and DESMIN in one case; vimentin, CD31 and
periodic acid-schiff stain (PAS) positive in two cases; and CD34
and smooth muscle actin in all three cases. The rate of Ki-67
expression was >60% in all cases. The results are presented in
Table III.
 | Table III.Pathological characteristics of the
patients with undifferentiated embryonal sarcoma of the liver in
the retrospective case series. |
Table III.
Pathological characteristics of the
patients with undifferentiated embryonal sarcoma of the liver in
the retrospective case series.
| No. | Size, cm | Infiltration of
capsule | Tumor thrombus | Necrosis, % | AE1/AE3 | Vimentin | HMB45 | CD31 | CD34 | KI-67 | SMA | DESMIN | PAS |
|---|
| A | 9×7×8 | – | – | 100 | N.A. | N.A. | N.A. | + | + | 70%+ | + | + | N.A. |
| B | 20×15×12.5 | + | + | N.A. | + | + | N.A. | N.A. | + | 60%+ | + | – | + |
| C | 22×19×10 | – | – | N.A. | – | + | + | + | + | 60%+ | + | – | + |
Systematic literature review
Demographic data
The literature search identified 108 reported adult
cases of UESL. Of these cases, 75 were reported and summarized by
Pachera et al (6) and Chen
et al (7) between 1955 and
2011. An additional 33 cases were reported between 2011 and 2019
(Table IV) (8–36). Thus,
including the present case series, a total of 111 adult cases of
UESL have been reported to date. Among all cases, the median age
was 29 years (range, 15–86 years), and the peak incidence was
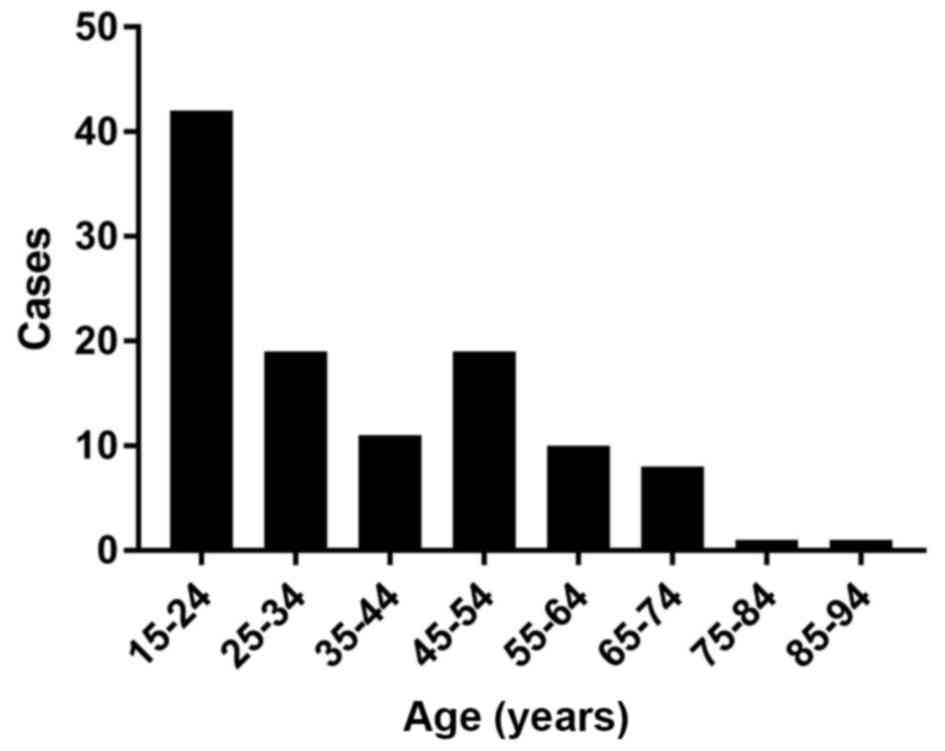
between the ages of 15 and 24 years (Fig. 1). Sex was reported for 107 patients;
of these, 44 (41%) were men and 63 (59%) were women, with a male:
Female ratio of 1:1.4 (Table
IV).
 | Table IV.New cases of undifferentiated
embryonal sarcoma of the liver between 2011 and 2019 in the
literature. |
Table IV.
New cases of undifferentiated
embryonal sarcoma of the liver between 2011 and 2019 in the
literature.
| Author, year | Age, years | Sex | Site | Biopsy | Treatment before
surgery | Surgery | Treatment after
surgery | Recurrence
(treatment) | Outcome | OS, mos | (Refs.) |
|---|
| Gerson et
al, 2019 | 71 | M | L | – | – | Left lobectomy | – | N.A. | N.A. | N.A. | (8) |
| Capozza et
al, 2019 | 20 | F | Rc | – | – | Right
hepatectomy | VAIA | No | Alive | 177 | (9) |
| Capozza et
al, 2019 | 17 | M | R | + | – | Right
hepatectomy | IFO + VCR +
ACTD | No | Alive | 20 | (9) |
| Esteban et
al, 2018 | 53 | F | Ra | + | Radiotherapy | Not performed | – | – | DOD | N.A. | (10) |
| Esteban et
al, 2018 | 35 | F | R+L | – | – | Extended right
hepatectomy | – | LR in 24 mos
(ADR+IFO) | Alive | 60 | (10) |
| Pandit et
al, 2019 | 34 | M | R+Lb | – | – | Mass
enucleation | – | No | Alive | 6 | (11) |
| Pandit et
al, 2019 | 29 | F | R | + | – | Radical
resection | – | LR, peritonea in 4
mos | DOD | 8 | (12) |
| Pinamonti et
al, 2018 | 60 | F | R | – | – | Segmentectomy | VCR + ACTD +
CTX | No | Alive | 30 | (13) |
| Beksac et
al, 2018 | 26 | F | L | + | – | Nonanatomic
resection | PTX + CDDP +
IFO | No | Alive | 72 | (14) |
| Khan et al,
2017 | 21 | M | R | + | IFO + ADR | LTx | – | No | Alive | 18 | (15) |
| Mori et al,
2017 | 65 | F | R+L | – | – | Right
trisectionectomy | – | LR in 18 mos
(resection) | Alive | 26 | (16) |
| Lee et al,
2016 | 51 | M | R | – | – | Right
hemihepatectomy | – | N.A. | N.A. | N.A. | (17) |
| Giakoustidis et
al, 2016 | 29 | F | R+L | + | PVE | Right
trisectionectomy | CTX + CDDP +
ADR | 1st LR in 12 mos
(CTX + CDDP + ADR), 2nd LR and spine metastasis | DOD | 28 | (18) |
| Treitl et
al, 2016 | 30 | M | L | + | – | Left
hepatectomy | ADR + IFO | No | Alive | 3 | (19) |
| Zanwar et
al, 2017 | 20 | M | R | + | IVA | Right
hepatectomy | IVA | No | Alive | 24 | (20) |
| Masuda et
al, 2015 | 52 | F | R+L | – | – | Right
trisectionectomy | – | LR in
12/19/25/35/42/47 mos (resections and RFA); bone metastases and TT
in azygos vein | DOD | 62 | (21) |
| Masuda et
al, 2015 | 53 | F | L+R | – | – | Extended left
hepatectomy | – | LR in 4/14 mos
(resections and RFA) | Alive | 65 | (21) |
| Kallam et
al, 2015 | 47 | M | L | – | – | Left lobectomy
(R1) | – | Lung metastases in
2 mos (ADR+ IFO, GEM+ DXT) | Death
(pneumonia) | 8 | (22) |
| Xie et al,
2014 | 39 | M | R | + | – | Tumor
resection | – | LR in 2 mos | Alive | 2 | (23) |
| Cao et al,
2014 | 37 | M | L | – | – | Lobectomy | – | LR in 19 mos
(TACE); Lung and mediastinum LN metastasis in 24 mos | DOD | 34 | (24) |
| Cao et al,
2014 | 24 | F | R | – | – | Lobectomy | MAID | LR in 4 mos
(N.A.) | Alive | 24 | (24) |
| Hanafiah et
al, 2014 | 20 | M | R+L | + | – | Extended right
hepatectomy | – | LR in 6 mos
(ADM) | Alive | 6 | (25) |
| Hong et al,
2014 | 67 | M | R | – | – | Segmentectomy | – | LR in 6 mos
(MAID) | Death (sepsis) | 8 | (26) |
| Ismail et
al, 2013 | 16 | F | R+L | + | CAV/ETIF/IF +
ADR | Right extended
hemihepatectomy | IVADO, VP-16/CDDP,
VRB/CTX | No | Alive | 50 | (27) |
| Jia et al,
2013 | 46 | F | R | – | – | Segmentectomy | – | LR in 6 mos | DOD | 12 | (28) |
| Hu et al,
2012 | 19 | F | R | – | – | Right
hemihepatectomy | – | No | Alive | 40 | (29) |
| Varol et al,
2012 | 33 | F | L | + | – | Not performed | – | – | DOD | N.A. | (30) |
| Dhanasekaran et
al, 2012 | 54 | M | L | + | ADR+ IFO, DTIC;
TACE | LTx | – | No | Alive | 167 | (31) |
| Lightfoot et
al, 2012 | 78 | F | R | – | – | Partial right
hepatectomy | – | No | Alive | 6 | (32) |
| Noguchi et
al, 2012 | 27 | F | R | – | – | Right
trisectionectomy | VADRCA+ CDDP, MCVC;
radiotheraphy | No | Alive | 60 | (33) |
| Tanaka et
al, 2012 | 51 | F | R | – | – | Segmentectomy | – | LR, lung and spine
metastasis in 48 mos | DOD | 60 | (34) |
| Tucker et
al, 2012 | 74 | F | L | – | – | Left
hepatectomy | – | No | Alive | 9 | (35) |
| Kim et al,
2011 | 47 | F | L | – | – | Left lateral
sectionectomy | MAID | Lumbar spine in 2
years (radiotheraphy) | DOD | 48 | (36) |
Treatment and outcome
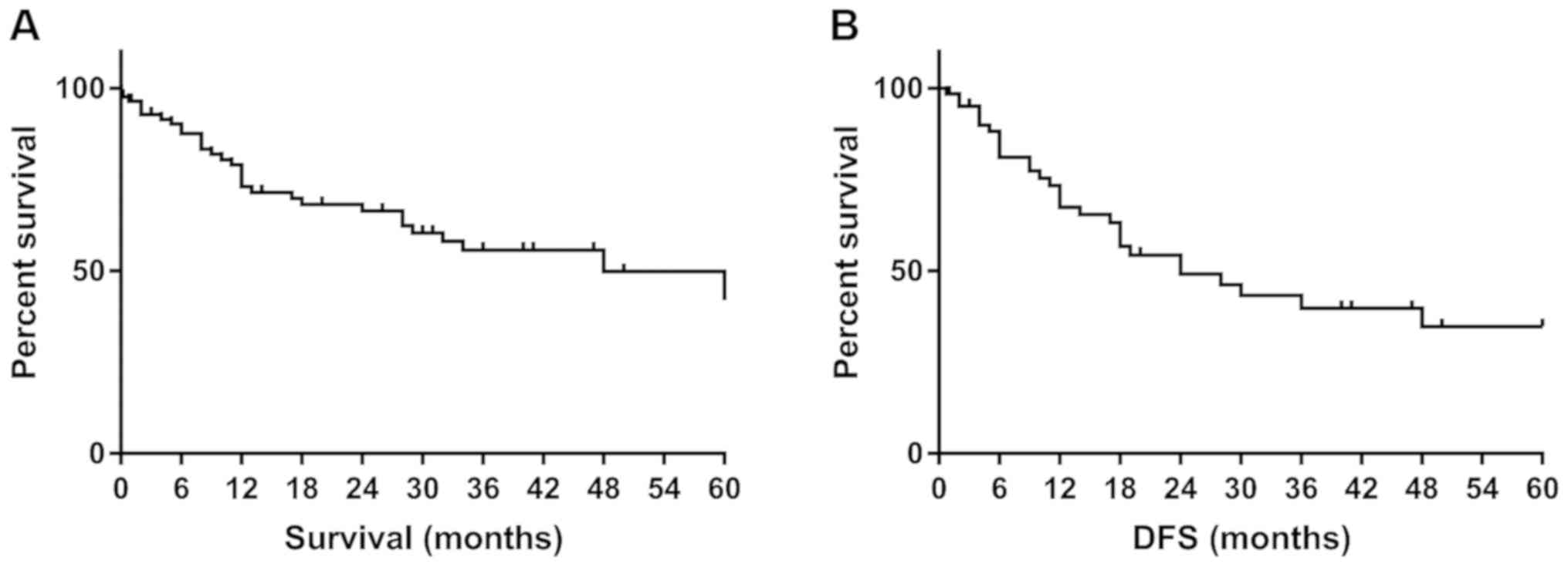
Complete treatment and survival data were available
for 83 patients. Among these patients, the median follow-up was 18
months (range, 2 days to 204 months), and median survival was 48
months (range, 2 days to 204 months). Among all the 83 patients,
the 1-, 3- and 5-year overall survival rates were 72, 56 and 47%,
respectively (Fig. 2A), and the 1-,
3- and 5-year disease-free survival rates were 67, 40 and 35%,
respectively (Fig. 2B).
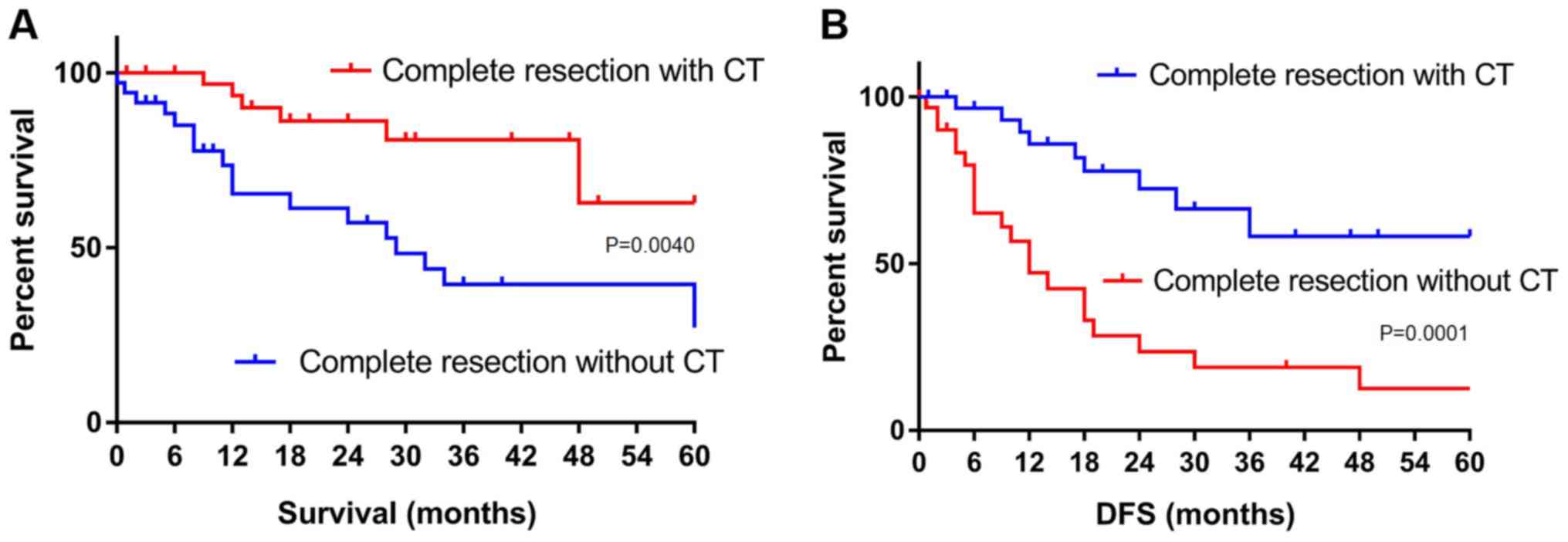
Patients who underwent complete tumor resection with
adjuvant and/or neoadjuvant chemotherapy exhibited significantly
higher survival rates compared with those in patients who underwent
surgery alone. For patients treated with chemotherapy plus surgery
vs. surgery alone, the overall survival rates were as follows:
1-year, 93% vs. 65%; 3-year, 80% vs. 40%; and 5-year, 63% vs. 34%
(P=0.0040; Fig. 3A). The
corresponding disease-free survival rates were as follows: 1-year,
86% vs. 47%; 3-year, 58% vs. 19%; and 5-year, 58% vs. 13%
(P=0.0001; Fig. 3B).
Discussion
In the present study, one of largest case series of
adult UESL to date was analyzed. The literature review confirmed
that a higher survival rate was associated with treatment
strategies combining complete tumor resection and chemotherapy
compared with radical tumor resection alone. To the best of our
knowledge, 111 adult cases of UESL have been reported to date,
including the present case series. The present analysis is the
first to include a thorough 1-, 3- and 5-year survival rate
analysis in this population.
UESL is rare and usually occurs in children; its
incidence decreases with increasing age, with peak incidence
occurring between the ages of 6 and 10 years (3,5). Among
adult patients, the present study identified another peak between
the ages of 15 and 24 years. It is possible that UESL is similar to
embryonal tumors, and thus may predominantly occur in young adults.
In addition, a female preponderance was observed in the present
systematic review, with a male: Female ratio of 1:1.4. In the
present case series, all three patients were female, and the median
age at diagnosis was 21 years (range, 15–25 years).
UESL exhibits a nonspecific clinical presentation.
The most common symptoms are right upper quadrant abdominal pain
and mass. Other symptoms include vomiting, diarrhea, weight loss,
fever, and jaundice (3,6,7). Among
the cases included in the present retrospective analysis, the
symptoms upon admission were fever, chills, nausea, vomiting and
weight loss in one patient, and abdominal pain and mass in the
other two patients. Laboratory findings, including liver function
and tumor markers, are usually normal at the time of UESL
presentation (6,7). Among the present cases, one patient
exhibited obviously altered liver function, and tumor markers,
including α-fetoprotein, carcinoembryonic antigen, carbohydrate
antigen (CA)199 and CA125, were negative in all patients. Only one
of the three patients exhibited elevated PIVKA-II. In the
ultrasound examination and CT scans, UESL often presents as a large
solid or cystic mass, with enhancement in the solid parts (33,37).
This is similar to the cases in the present study.
From its first recognition as a unique
clinicopathologic entity in 1978 until the early 1990s, UESL has
been associated with a poor prognosis, even in patients who
underwent complete surgical resection of the tumor (1,2,37). Due to its low incidence, especially
among adults, UESL survival data are mainly from case reports or
small case series of childhood patients. In the initial report by
Stocker and Ishak (4), the median
survival was <1 year, and only 19% (6/31) of the reported
patients were alive and disease-free after resection for the median
follow-up of 9 months (range, 2–52 months). Among the 40 patients
reported in the literature between 1950 and 1988, 47.5% died after
a mean duration of 11.9 months, 15.0% survived with disease, and
37.5% were alive and disease-free (average, 37.5 months) (38).
In the recent two decades, an increasing number of
long-term survivors have been reported. These cases have mainly
included children who underwent surgical tumor resection,
especially with postoperative chemotherapy (39–42). In
a review of 68 adult patients between 1995 and 2007, Lenze et
al (5) observed a median
survival of 29 months among all patients, and that patients who
underwent complete tumor resection followed by adjuvant
chemotherapy exhibited significantly improved survival compared
with that of patients who underwent surgery alone. Similarly, the
present results demonstrated significantly improved survival among
patients treated with complete tumor resection plus adjuvant and/or
neoadjuvant chemotherapy compared with patients treated with
surgery alone. In addition, in pediatric cases, neoadjuvant
chemotherapy can reduce the tumor size and stage, making complete
surgical resection possible (25,42,43).
However, due to insufficient data, the effect of neoadjuvant
chemotherapy in adult patients with UESL and its influence on
survival cannot be currently assessed.
The present findings were limited by the
retrospective study design and the low number of cases. The rarity
of UESL, especially in adults, precludes large prospective
single-institution studies. In addition, the effects of neoadjuvant
treatment of UESL could not be evaluated in this study due to the
limited relevant data in adult patients. However, this may be
confirmed as a useful method in the future, based on the results of
studies on pediatric UESL.
In conclusion, the present study reports one of
largest case series of adult UESL to date. The results of our
systematic literature review were the first to report the survival
rates, which confirmed significantly improved survival following
treatment with complete tumor resection plus chemotherapy compared
with radical tumor resection alone. In the future,
multi-institutional or global collaborative studies may represent
the best approach to investigating adult UESL and standardizing its
treatment.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
BS and LG conceived and designed the study. BS, XH
and SY performed the bioinformatics analysis and wrote the initial
manuscript. LC, ZY and LG were involved in the conception of the
study and edited the manuscript. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the Beijing Tsinghua Changgung Hospital, and written
informed consent was obtained from all patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
UESL
|
undifferentiated embryonal sarcoma of
the liver
|
|
ALP
|
alkaline phosphatase
|
|
APTT
|
activated partial thromboplastin
time
|
|
PT
|
prothrombin time
|
|
AST
|
aspartate aminotransferase
|
|
ALT
|
alanine aminotransferase
|
|
DBIL
|
direct bilirubin
|
|
GGT
|
γ-glutamyl transpeptidase
|
|
ALB
|
albumin
|
|
RBC
|
red blood cell
|
|
HGB
|
hemoglobin
|
|
HCT
|
red blood cell specific volume
|
|
PIVKA-II
|
protein induced by vitamin K absence
or antagonist-II
|
|
HAIC
|
hepatic artery infusion
chemotherapy
|
|
CA
|
carbohydrate antigen
|
References
|
1
|
Liver Cancer Study Group of Japan, .
Primary liver cancer in Japan. Clinicopathologic features and
results of surgical treatment. Ann Surg. 211:277–287.
1990.PubMed/NCBI
|
|
2
|
Donovan EJ and Santulli TV: Resection of
the left lobe of the liver for mesenchymoma: Report of case. Ann
Surg. 124:90–93. 1946. View Article : Google Scholar
|
|
3
|
Stout AP: Mesenchymoma, the mixed tumor of
mesenchymal derivatives. Ann Surg. 127:278–290. 1948. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Stocker JT and Ishak KG: Undifferentiated
(embryonal) sarcoma of the liver: Report of 31 cases. Cancer.
42:336–348. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lenze F, Birkfellner T, Lenz P, Hussein K,
Länger F, Kreipe H and Domschke W: Undifferentiated embryonal
sarcoma of the liver in adults. Cancer. 112:2274–2282. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pachera S, Nishio H, Takahashi Y, Yokoyama
Y, Oda K, Ebata T, Igami T and Nagino M: Undifferentiated embryonal
sarcoma of the liver: Case report and literature survey. J
Hepatobiliary Pancreat Surg. 15:536–544. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chen JH, Lee CH, Wei CK, Chang SM and Yin
WY: Undifferentiated embryonal sarcoma of the liver with focal
osteoid picture-a case report. Asian J Surg. 36:174–178. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gerson G, Valença JT, Cavalcante JM and
Coêlho RAB: Undifferentiated embryonal sarcoma of the liver in
elderly: Case report and review of the literature. Indian J Pathol
Microbiol. 62:129–131. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Capozza MA, Ruggiero A, Maurizi P,
Mastrangelo S, Attinà G, Triarico S, Vellone M and Giuliante F:
Undifferentiated embryonal sarcoma of the liver (UESL) in
adolescents: An unexpected diagnosis. J Pediatr Hematol Oncol.
41:e132–e134. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Esteban SG, Emilio CU, Emmanuel AF, Oscar
SJ, Paulina CE and Angel MM: Undifferentiated embryonal sarcoma of
the liver in adult patient: A report of two cases. Ann
Hepatobiliary Pancreat Surg. 22:269–273. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pandit N, Jaiswal LS, Shrestha V, Awale L
and Adhikary S: Undifferentiated embryonal sarcoma of liver in an
adult with spontaneous rupture and tumour thrombus in the right
atrium. ANZ J Surg. 89:E396–E397. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pandit N, Deo KB, Jaiswal LS, Pradhan A
and Adhikary S: Hanging undifferentiated embryonal sarcoma of the
liver in adult: An unusual presentation of an aggressive tumor. J
Gastrointest Cancer. 50:689–692. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pinamonti M, Vittone F, Ghiglione F,
Borasi A, Silvestri S and Coverlizza S: Unexpected liver embryonal
sarcoma in the adult: Diagnosis and treatment. Case Rep Surg.
2018:83620122018.PubMed/NCBI
|
|
14
|
Beksac K, Mammadov R, Ciftci T, Guner G,
Akyol A and Kaynaroglu V: Undifferentiated embryonal sarcoma of the
liver in an adult patient. Cureus. 10:e30372018.PubMed/NCBI
|
|
15
|
Khan ZH, Ilyas K, Khan HH, Ghazanfar H,
Hussain Q, Inayat F, Yasir M and Asim R: Unresectable
undifferentiated embryonal sarcoma of the liver in an adult male
treated with chemotherapy and orthotopic liver transplantation.
Cureus. 9:e17592017.PubMed/NCBI
|
|
16
|
Mori A, Fukase K, Masuda K, Sakata N,
Mizuma M, Ohtsuka H, Morikawa T, Nakagawa K, Hayashi H, Motoi F, et
al: A case of adult undifferentiated embryonal sarcoma of the liver
successfully treated with right trisectionectomy: A case report.
Surg Case Rep. 3:192017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lee KH, Maratovich MN and Lee KB:
Undifferentiated embryonal sarcoma of the liver in an adult
patient. Clin Mol Hepatol. 22:292–295. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Giakoustidis DE, Gargavanis AA, Katsiki
ED, Salveridis NT, Antoniadis NA and Papanikolaou V:
Undifferentiated embryonal sarcoma of the liver in a young female:
Treatment with portal vein embolization and liver trisectonectomy.
Korean J Hepatobiliary Pancreat Surg. 20:144–147. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Treitl D, Roudenko A, El Hussein S, Rizer
M and Bao P: Adult embryonal sarcoma of the liver: Management of a
massive liver tumor. Case Rep Surg. 2016:56257622016.PubMed/NCBI
|
|
20
|
Zanwar S, Goel M, Patkar S, Ramaswamy A,
Shetty N, Ramadwar M and Ostwal V: A case of ruptured adult
embryonal sarcoma of the liver with excellent outcome after
neoadjuvant chemotherapy. J Gastrointest Cancer. 48:100–102. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Masuda T, Beppu T, Doi K, Miyata T,
Nakagawa S, Okabe H, Hayashi H, Ishiko T, Iyama K and Baba H:
Repeated hepatic resections and radio-frequency ablations may
improve the survival of adult undifferentiated embryonal sarcoma of
the liver: Report of two cases. Surg Case Rep. 1:552015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kallam A, Krishnamurthy J, Kozel J and
Shonka N: Undifferentiated embryonal sarcoma of liver. Rare Tumors.
7:60092015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Xie ZY, Li LP, Wu WJ, Sun DY, Zhou MH and
Zhao YG: Undifferentiated embryonal sarcoma of the liver mistaken
for hepatic abscess in an adult. Oncol Lett. 8:1184–1186. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cao Q, Ye Z, Chen S, Liu N, Li S and Liu
F: Undifferentiated embryonal sarcoma of liver: A
multi-institutional experience with 9 cases. Int J Clin Exp Pathol.
7:8647–8656. 2014.PubMed/NCBI
|
|
25
|
Hanafiah M, Yahya A, Zuhdi Z and Yaacob Y:
A case of an undifferentiated embryonal sarcoma of the liver
mimicking a liver abscess. Sultan Qaboos Univ Med J. 14:e578–e581.
2014.PubMed/NCBI
|
|
26
|
Hong WJ, Kang YN and Kang KJ:
Undifferentiated embryonal sarcoma in adult liver. Korean J Pathol.
48:311–314. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ismail H, Dembowska-Bagińska B,
Broniszczak D, Kaliciński P, Maruszewski P, Kluge P, Swięszkowska
E, Kościesza A, Lembas A and Perek D: Treatment of undifferentiated
embryonal sarcoma of the liver in children-single center
experience. J Pediatr Surg. 48:2202–2206. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Jia C, Zhao W, Dai C, Wang X, Bu X, Peng
S, Xu F, Xu Y and Zhao Y: Undifferentiated embryonal sarcoma of the
liver in a middle-aged adult with systemic lupus erythematosus.
World J Surg Oncol. 11:2442013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Hu X, Chen H, Jin M, Wang X, Lee J, Xu W,
Zhang R, Li S and Niu J: Molecular cytogenetic characterization of
undifferentiated embryonal sarcoma of the liver: A case report and
literature review. Mol Cytogenet. 5:262012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Varol U, Karaca B, Muslu U, Doğanay L,
Değirmenci M, Uslu R and Göker E: Undifferentiated embryonal
sarcoma of the liver in an adult patient: Case report. Turk J
Gastroenterol. 23:279–283. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Dhanasekaran R, Hemming A, Salazar E and
Cabrera R: Rare case of adult undifferentiated (embryonal) sarcoma
of the liver treated with liver transplantation: Excellent
long-term survival. Case Reports Hepatol. 2012:5197412012.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Lightfoot N and Nikfarjam M: Embryonal
sarcoma of the liver in an adult patient. Case Rep Surg.
2012:3827232012.PubMed/NCBI
|
|
33
|
Noguchi K, Yokoo H, Nakanishi K, Kakisaka
T, Tsuruga Y, Kamachi H, Matsushita M and Kamiyama T: A long-term
survival case of adult undifferentiated embryonal sarcoma of liver.
World J Surg Oncol. 10:652012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Tanaka S, Takasawa A, Fukasawa Y, Hasegawa
T and Sawada N: An undifferentiated embryonal sarcoma of the liver
containing adipophilin-positive vesicles in an adult with massive
sinusoidal invasion. Int J Clin Exp Pathol. 5:824–829.
2012.PubMed/NCBI
|
|
35
|
Tucker SM, Cooper K, Brownschidle S and
Wilcox R: Embryonal (undifferentiated) sarcoma of the liver with
peripheral angiosarcoma differentiation arising in a mesenchymal
hamartoma in an adult patient. Int J Surg Pathol. 20:297–300. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Kim HH, Kim JC, Park EK, Hur YH, Koh YS,
Cho CK, Kim HS and Kim HJ: Undifferentiated embryonal sarcoma of
the liver presenting as a hemorrhagic cystic tumor in an adult.
Hepatobiliary Pancreat Dis Int. 10:657–660. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Li XW, Gong SJ, Song WH, Zhu JJ, Pan CH,
Wu MC and Xu AM: Undifferentiated liver embryonal sarcoma in
adults: A report of four cases and literature review. World J
Gastroenterol. 16:4725–4732. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Leuschner I, Schmidt D and Harms D:
Undifferentiated sarcoma of the liver in childhood: Morphology,
flow cytometry, and literature review. Hum Pathol. 21:68–76. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Walker NI, Horn MJ, Strong RW, Lynch SV,
Cohen J, Ong TH and Harris OD: Undifferentiated (embryonal) sarcoma
of the liver. Pathologic findings and long-term survival after
complete surgical resection. Cancer. 69:52–59. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Urban CE, Mache CJ, Schwinger W, Pakisch
B, Ranner G, Riccabona M, Schimpl G, Brandesky G, Messner H,
Pobegen W, et al: Undifferentiated (embryonal) sarcoma of the liver
in childhood. Successful combined-modality therapy in four
patients. Cancer. 72:2511–2516. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Weitz J, Klimstra DS, Cymes K, Jarnagin
WR, D'Angelica M, La Quaglia MP, Fong Y, Brennan MF, Blumgart LH
and Dematteo RP: Management of primary liver sarcomas. Cancer.
109:1391–1396. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Bisogno G, Pilz T, Perilongo G, Ferrari A,
Harms D, Ninfo V, Treuner J and Carli M: Undifferentiated sarcoma
of the liver in childhood: A curable disease. Cancer. 94:252–257.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Kim DY, Kim KH, Jung SE, Lee SC, Park KW
and Kim WK: Undifferentiated (embryonal) sarcoma of the liver:
Combination treatment by surgery and chemotherapy. J Pediatr Surg.
37:1419–1423. 2002. View Article : Google Scholar : PubMed/NCBI
|