Introduction
Breast cancer is one of the most common malignant
tumors in females (1). In the Asian
population, triple-negative breast cancer (TNBC) accounts for
10–17% of all breast cancer cases (2). TNBC refers to a type of breast cancer
lacking estrogen receptor (ER), progesterone receptor (PR) and
human epidermal growth factor receptor 2 expression (3). TNBC is associated with a poor
prognosis, a unique metastasis pattern and highly malignant
biological behavior (2). At present,
there is no effective clinical treatment for TNBC, and effective
targets and biomarkers for prognosis are urgently required. The
endothelin family consists of three isoforms (ET-1, ET-2 and ET-3),
which can bind G-coupled protein endothelin A receptor and
endothelin B receptor (EDNRB) via autocrine or paracrine signaling
pathways (4,5). EDNRB is located on chromosome 13 and is
mainly expressed in endothelial cells, macrophages and vascular
smooth muscle cells (6,7). EDNRB may activate numerous
cancer-associated signaling pathways, including the
mitogen-activated protein kinase/Erk 2 and PI3K/AKT signaling
pathways (8,9). In addition, previous studies have noted
that EDNRB, when combined with ET-1, affects cell proliferation and
migration, and is associated with lymph angiogenesis and lymphatic
metastasis (10–12). EDNRB expression exhibits tissue
specificity in cancer. It is highly expressed in glioma, but is
expressed at low levels in prostate and liver cancer, and its high
expression is associated with a favorable prognosis (13–15).
However, the expression and clinical significance of EDNRB in TNBC
remain unclear, and there is a lack of large-scale clinical
studies. The purpose of the present study was to investigate the
association with clinicopathological characteristics and the
prognostic value of EDNRB in TNBC.
Materials and methods
Patient cohorts
The cancer genome atlas (TCGA)
cohort
The present study included tissues from patients
with primary TNBC (n=159) and para-cancerous tissues from patients
with breast cancer (n=112) obtained from TCGA (16). These included 14 pairs of matched
cancerous and para-cancerous tissues. Data regarding the gene
expression levels of EDNRB in each tissue were obtained from the
database, and the expression levels were Log2 transformed to
analyze the difference in EDNRB gene expression between tumor and
normal tissues. Subsequently, 142 patients with primary TNBC with
complete clinical data were included in the analysis of the
association between EDNRB expression and clinicopathological data.
The median value of EDNRB expression was set as the boundary (exact
value, 8.348); expression below the median value was considered
negative; and expression above the median value was considered
positive. In this cohort, the age ranged between 29 and 90 years
(median, 55); 69.0% (n=98) of the patients were postmenopausal;
73.9% (n=105) of the patients had a T stage >2; 86.6% (n=123) of
the patients had an N stage of 0 or 1; and the positive rate of
EDNRB was 52.8%.
Henan cancer hospital (HNCH)
cohort
The present study retrospectively consecutively
collected 99 cases of TNBC between January 2013 and February 2018
at the Department of Breast Surgery of Henan Cancer Hospital
(Zhengzhou, China). The inclusion criteria were as follows: i)
Patients with primary TNBC; ii) no distant metastasis at first
diagnosis; and iii) direct surgical resection or no pathological
complete response was achieved following neoadjuvant chemotherapy.
Patients were followed up using the outpatient registration system
and disease-free survival (DFS) was determined. DFS was defined as
no local or regional recurrence, no distant recurrence and no
contralateral invasive breast cancer. In this cohort, the age
ranged between 27 and 69 years (median, 48); 60.6% (n=60) of
patients were not menopausal; 66.7% (n=66) of patients had a T
stage >2; 72.7% (n=72) of patients had an N stage of 0 or 1; and
the positive rate of EDNRB was 23.2%. The present study was
approved by the Ethics Committee of the Affiliated Cancer Hospital
of Zhengzhou University.
Immunohistochemistry
Tissues were fixed with 10% neutral buffered
formalin at room temperature for 12 h, before being embedded in
paraffin. Rabbit anti-human EDNRB monoclonal antibody (cat. no.
31191; Signalway Antibody LLC, College Park, MD, USA), secondary
antibody (cat. no. sp-9001; OriGene Technologies, Inc., Rockville,
MD, USA) and diaminobenzidine (DAB) chromogenic solution (cat. no.
sp-9001; OriGene Technologies, Inc.) were purchased.
Immunohistochemical staining was performed according to the
streptavidin-peroxidase method. Paraffin-embedded specimens were
cut into 5-µm sections. Following conventional xylene dewaxing and
alcohol gradient dehydration, the specimens were placed in citric
acid buffer (pH 6.0) for antigen repair at 100°C and rinsed in PBS
three times for 5 min each. Sections were incubated with 3%
hydrogen peroxide at room temperature for 25 min (avoiding light)
to block endogenous peroxidase activity. The sections were rinsed
in PBS three times for 5 min each, and normal 10% bovine calf serum
(cat. no. B7446; Sigma-Aldrich; Merck KGaA) was added for 20 min at
room temperature. Subsequently, the serum was dried. EDNRB primary
antibody (dilution, 1:500) was added dropwise to the sections, and
the sections were laid flat in a wet box at 4°C overnight. PBS was
used for three washes of 5 min each. Horseradish peroxidase-labeled
anti-rabbit secondary antibody (dilution, 1:1,000) was added, and
incubated at room temperature for 2 h, followed by DAB color
development, hematoxylin re-dyeing at room temperature for 90 min,
conventional dehydration, drying and sealing. The results were
interpreted as previously described (17,18).
Briefly, a score was assigned according to the staining degree: 0,
basic non-staining (0); 1, light yellow (+); 2, brown (++); and 3,
dark brown (+++). Sections were observed under a bright-field
upright microscope (Olympus Corporation) at 10×40 high
magnification, three fields of view were observed for each section,
the percentage of positively stained tumor cells in each field of
view was calculated and the average value was used for scoring as
follows: 0 points, no positive staining of tumor cells; 1 point,
1–25%; 2 points, 26–50%; 3 points, 51–75%; and 4 points, >75%.
Finally, the percentage was multiplied by the dyeing intensity
score to obtain the total score. A score of 0 was considered
negative, a score of 1–4 was considered weakly positive, a score of
5–8 was considered moderately positive and a score of 9–12 was
considered strongly positive. Finally, in the present study, a
total score £4 was considered negative and a total score >4 was
considered positive. The immunohistochemical results were confirmed
by two blinded pathologists.
Statistical analysis
GraphPad Prism 7 (GraphPad Software, Inc., La Jolla,
CA, USA), SPSS v23.0 software (IBM Corp., Armonk, NY, USA) and R
software 3.6.1 (Lucent Technologies) were used for statistical
analysis. P<0.05 was considered to indicate a statistically
significant difference. Independent sample correction t-test was
used to compare the difference in EDNRB gene expression between
tumor and normal tissues in the TCGA cohort, and a paired t-test
was used to compare the differences in expression levels between
paired tissues. The stromal, immune and ESTIMATE scores were
calculated using the ‘ESTIMATE’ package in R software (19). The correlation between EDNRB
expression and the score was analyzed using Spearman's correlation
analysis. A two-sided χ2 test was used to analyze the
association between EDNRB expression and clinicopathological data.
Binary logistics regression analysis was used for multivariate
analysis. Survival analysis was performed using the Kaplan-Meier
method and a log-rank test. Based on the results of the
multivariate Cox regression analysis, the present study established
two prediction models to further illustrate the predictive value of
EDNRB expression for prognosis. Model 1 consisted of N stage and
NAC, while model 2 also included EDNRB expression as a parameter.
Integrated area under the curve (iAUC) of time-dependent receiver
operating characteristic (ROC) curves, concordance index (C-index),
integrated discriminant improvement (IDI) and decision curve
analyses were performed using the model to determine the model
discrimination and the prediction accuracy for survival, and to
determine the value of EDNRB for clinical net benefit.
Results
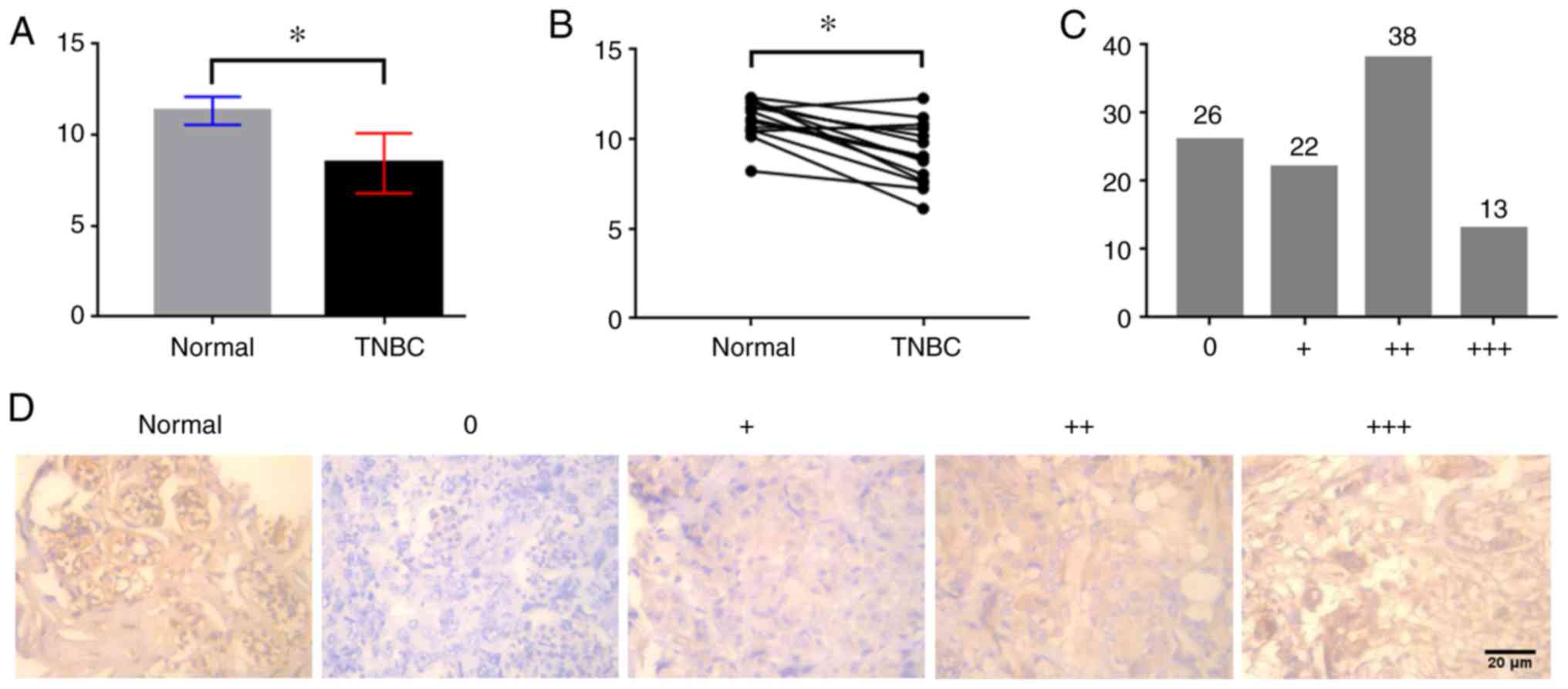
Expression levels of EDNRB in TNBC are
lower than those in normal tissues
The present study investigated the difference in
EDNRB expression between TNBC and normal breast tissues in the TCGA
cohort. As shown in Fig. 1A, the
expression levels of EDNRB in TNBC tissues were lower than those in
normal breast tissues (P<0.01). Similarly, analysis of the
difference between 14 cases of TNBC and adjacent normal tissues in
the TCGA cohort indicated that the expression levels of EDNRB in
TNBC were relatively low (P<0.01; Fig. 1B). Additionally, in
immunohistochemical analysis of 99 cases, 26 cases were uncolored,
and 13 cases exhibited dark brown staining (Fig. 1C). EDNRB was mainly expressed in the
cytoplasm and was highly expressed in normal breast tissues
(Fig. 1D).
Association between EDNRB expression
and clinicopathological data of patients with TNBC
In order to study the association between EDNRB and
clinicopathological data of patients with TNBC, the present study
collected clinicopathological data of the TCGA and HNCH cohorts
(Table I). The TCGA cohort included
142 patients with TNBC with complete clinicopathological data.
Univariate analysis revealed that EDNRB expression was associated
with T stage and N stage (P=0.04 and P=0.01, respectively).
Furthermore, multivariate analysis demonstrated that T stage [odds
ratio (OR), 0.40; P=0.03] and N stage (OR, 4.3; P=0.02) were
independent predictors of EDNRB expression. The lower the T stage
and the higher the N stage, the more positive EDNRB expression was.
The present study collected 99 samples from patients with TNBC in
the HNCH cohort. Univariate analysis revealed that age and
menopausal status were associated with EDNRB expression (P=0.01 and
P=0.02, respectively). Multivariate analysis demonstrated that age
was an independent predictor of EDNRB expression (OR, 3.37;
P=0.01), and higher age was associated with positive EDNRB
expression.
 | Table I.Correlation between EDNRB and
clinicopathological data. |
Table I.
Correlation between EDNRB and
clinicopathological data.
|
|
| EDNRB |
|
|
|
|
| EDNRB |
|
|
|
|
|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|---|
| Variable | HNCH number | Negative | Positive | P-value | OR | 95% CI | P | TCGA number | Negative | Positive | P-value | OR | 95% CI | P-value |
|---|
| Age |
|
|
| 0.01 | 3.37 | 1.28–8.87 | 0.01 |
|
|
|
|
|
| 0.62 |
|
<50 | 61 (61.6) | 52 (85.2) | 9 (14.8) |
|
|
|
| 50 (35.2) | 25 (50.0) | 25 (50.0) |
|
|
|
|
|
≥50 | 38 (38.4) | 24 (63.2) | 14 (36.8) |
|
|
|
| 92 (64.8) | 42 (45.7) | 50 (54.3) |
|
|
|
|
| Menopausal
status |
|
|
| 0.02 |
|
|
|
|
|
| 0.78 |
|
|
|
|
Premenopausal | 60 (60.6) | 51 (85.0) | 9 (15.0) |
|
|
|
| 44 (31.0) | 20 (45.5) | 24 (54.5) |
|
|
|
|
|
Postmenopausal | 39 (39.4) | 25 (64.1) | 14 (35.9) |
|
|
|
| 98 (69.0) | 47 (48.0) | 51 (52.0) |
|
|
|
|
| Tumor size, cm |
|
|
| 0.50 |
|
|
|
|
|
| 0.04 | 0.40 | 0.18–0.90 | 0.03 |
| ≤2 | 33 (33.3) | 24 (72.7) | 9 (27.3) |
|
|
|
| 37 (26.1) | 12 (32.4) | 25 (67.6) |
|
|
|
|
|
>2 | 66 (66.7) | 52 (78.8) | 14 (21.2) |
|
|
|
| 105 (73.9) | 55 (52.4) | 50 (47.6) |
|
|
|
|
| Pathological N
stage |
|
|
| 0.23 |
|
|
|
|
|
| 0.01 | 4.30 | 1.33–13.89 | 0.02 |
|
0-1 | 72 (72.7) | 53 (73.6) | 19 (26.4) |
|
|
|
| 123 (86.6) | 63 (51.2) | 60 (48.8) |
|
|
|
|
|
2-3 | 27 (27.3) | 23 (85.2) | 4 (14.8) |
|
|
|
| 19 (13.4) | 4 (21.1) | 15 (78.9) |
|
|
|
|
| NAC |
|
|
| 0.95 |
|
|
|
|
|
|
|
|
|
|
|
Yes | 35 (35.4) | 27 (77.1) | 8 (22.9) |
|
|
|
|
|
|
|
|
|
|
|
| No | 64 (64.6) | 49 (76.6) | 15 (23.4) |
|
|
|
|
|
|
|
|
|
|
|
EDNRB expression is positively
correlated with stromal score
In order to analyze the correlation between EDNRB
expression and non-tumor components in the tumor microenvironment,
the immune, stromal and ESTIMATE scores of TNBC tissues from the
TCGA cohort (n=159) were calculated. Each patient had a stromal
score, an immune score and an ESTIMATE score. Stromal scores ranged
between-1,525.21 and 1,571.25 (mean, 145.89), immune scores ranged
between-1,684.49 and 2,529.03 (mean, 546.82) and ESTIMATE scores
ranged between-3,068.11 and 3,258.92 (mean, 692.72). EDNRB
expression was correlated with stromal score (rs=0.44; P<0.01),
immune score (rs=0.19; P=0.02) and ESTIMATE score (rs=0.35;
P<0.01; Table II).
 | Table II.Correlation between EDNRB and tumor
microenvironment. |
Table II.
Correlation between EDNRB and tumor
microenvironment.
| Variable | Score | rs | 95% CI | P-value |
|---|
| Stromal score | 145.89±693.84 | 0.44 | 0.30~0.56 | <0.01 |
| Immune score | 546.82±901.60 | 0.19 | 0.03~0.34 | 0.02 |
| ESTIMATE score | 692.72±1411.76 | 0.35 | 0.20~0.49 | <0.01 |
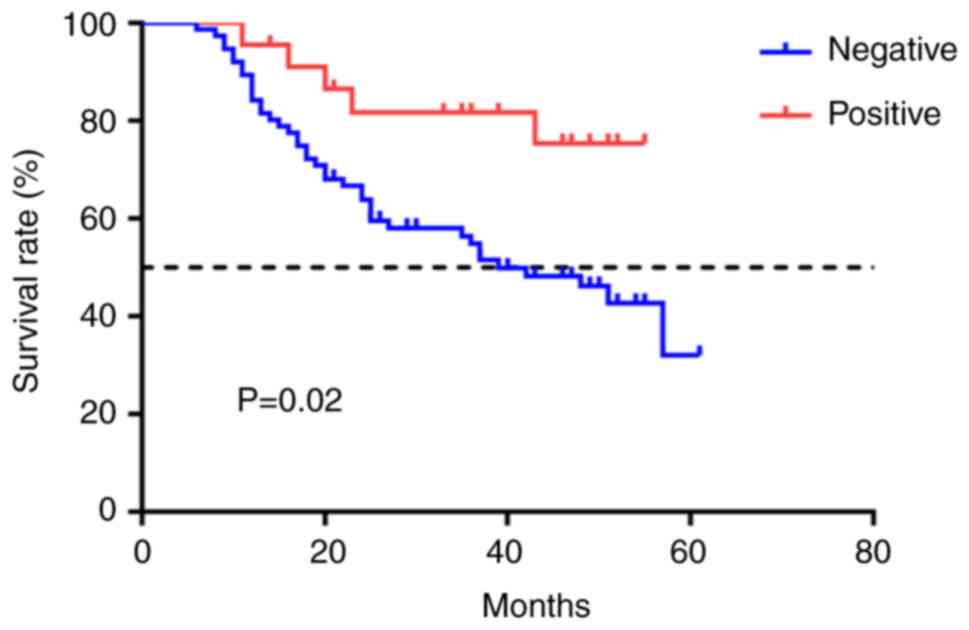
EDNRB expression is associated with a
favorable prognosis
Using the outpatient registration system, the HNCH
cohort was followed up (median follow-up time, 36 months). Among
them, 78.3% (n=18) of the patients in the EDNRB-positive group had
DFS events, while 47.4% (n=36) of the patients in the
EDNRB-negative group had DFS events. Univariate Cox regression
analysis revealed that N stage (P=0.01), neoadjuvant chemotherapy
(NAC; P=0.01) and EDNRB expression (P=0.03) may be associated with
the prognosis of patients with TNBC (Table III). Furthermore, when adjusted for
confounding factors, multivariate Cox regression analysis
demonstrated that EDNRB expression (P=0.04), N stage (P=0.01) and
NAC (P=0.02) were independent predictors of prognosis in patients
with TNBC (Table III).
Kaplan-Meier analysis demonstrated that negative EDNRB expression
was associated with an adverse prognosis in patients with TNBC
(P=0.02; Fig. 2).
 | Table III.Univariate and multivariate Cox
regression analysis of disease-free survival. |
Table III.
Univariate and multivariate Cox
regression analysis of disease-free survival.
|
| Univariate | Multivariate |
|---|
|
|
|
|
|---|
| Variable | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Age | 0.54 | 0.28–1.04 | 0.06 |
|
|
|
| Menopausal
status | 0.54 | 0.28–1.03 | 0.06 |
|
|
|
| Tumor size | 1.13 | 0.81–1.58 | 0.46 |
|
|
|
| Pathological N
stage | 4.04 | 2.23–7.31 | 0.01 | 2.45 | 1.23–4.92 | 0.01 |
| NAC | 3.46 | 1.87–6.40 | 0.01 | 2.45 | 1.19–5.02 | 0.02 |
| EDNRB | 0.36 | 0.14–0.91 | 0.03 | 0.38 | 0.15–0.98 | 0.04 |
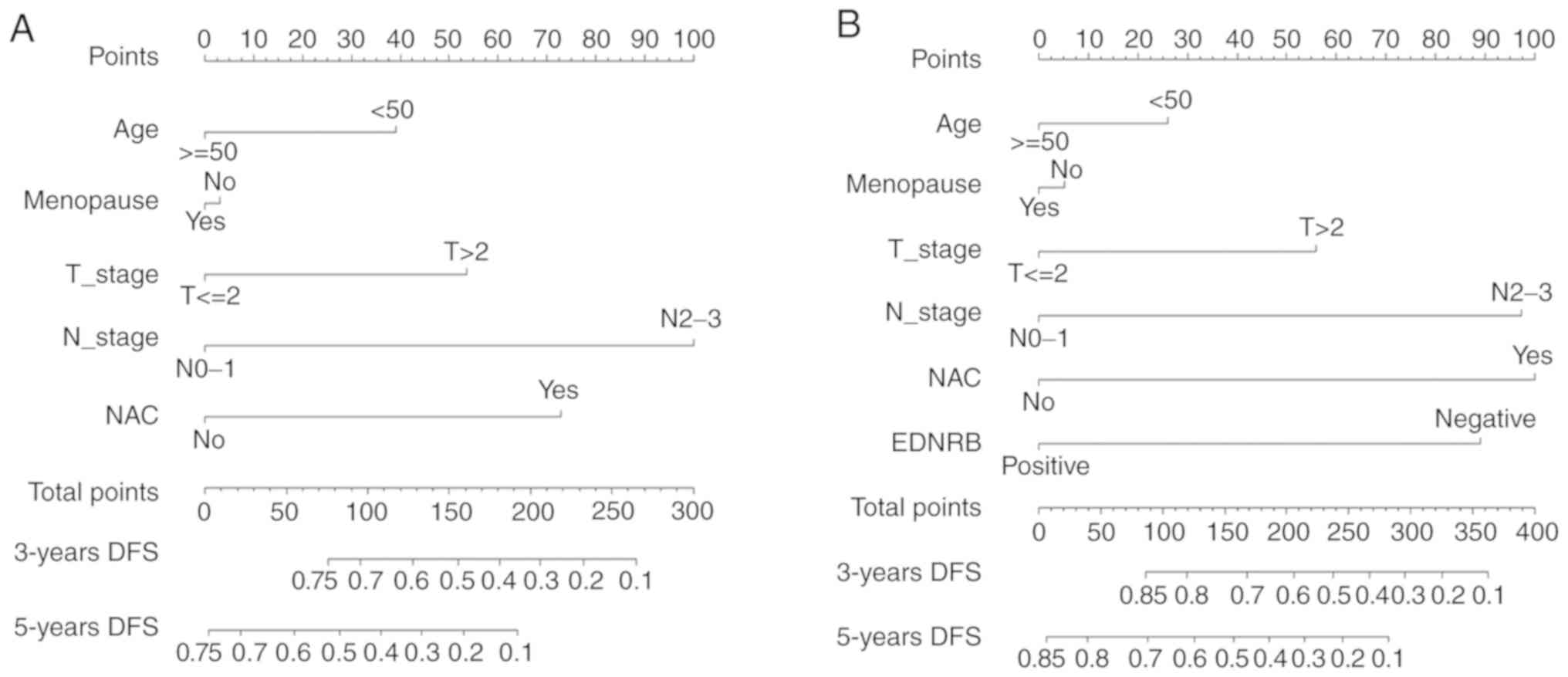
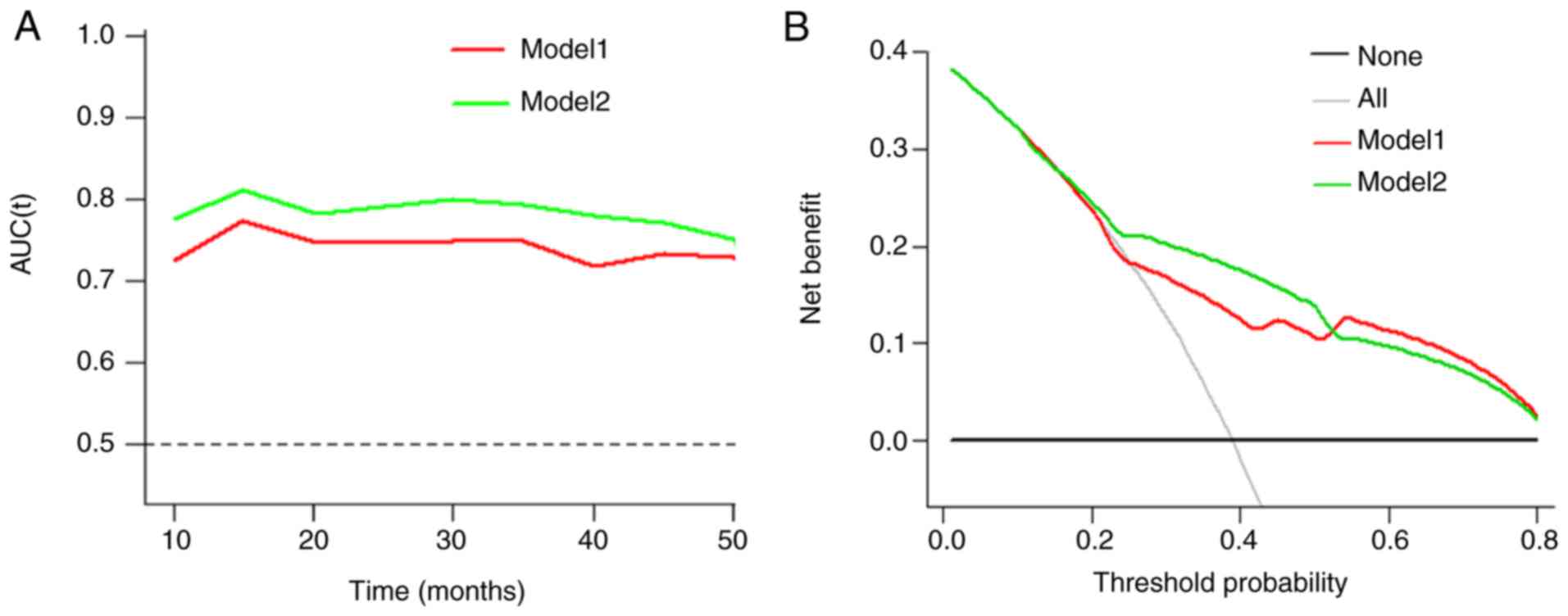
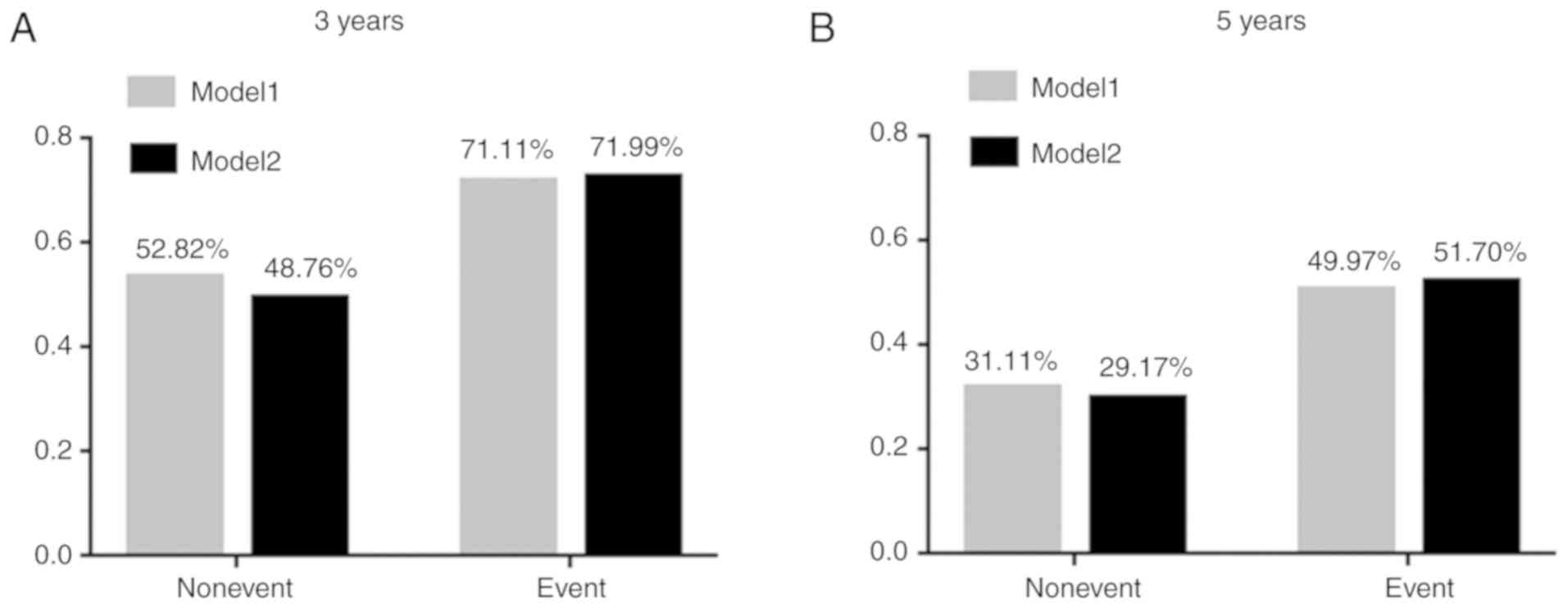
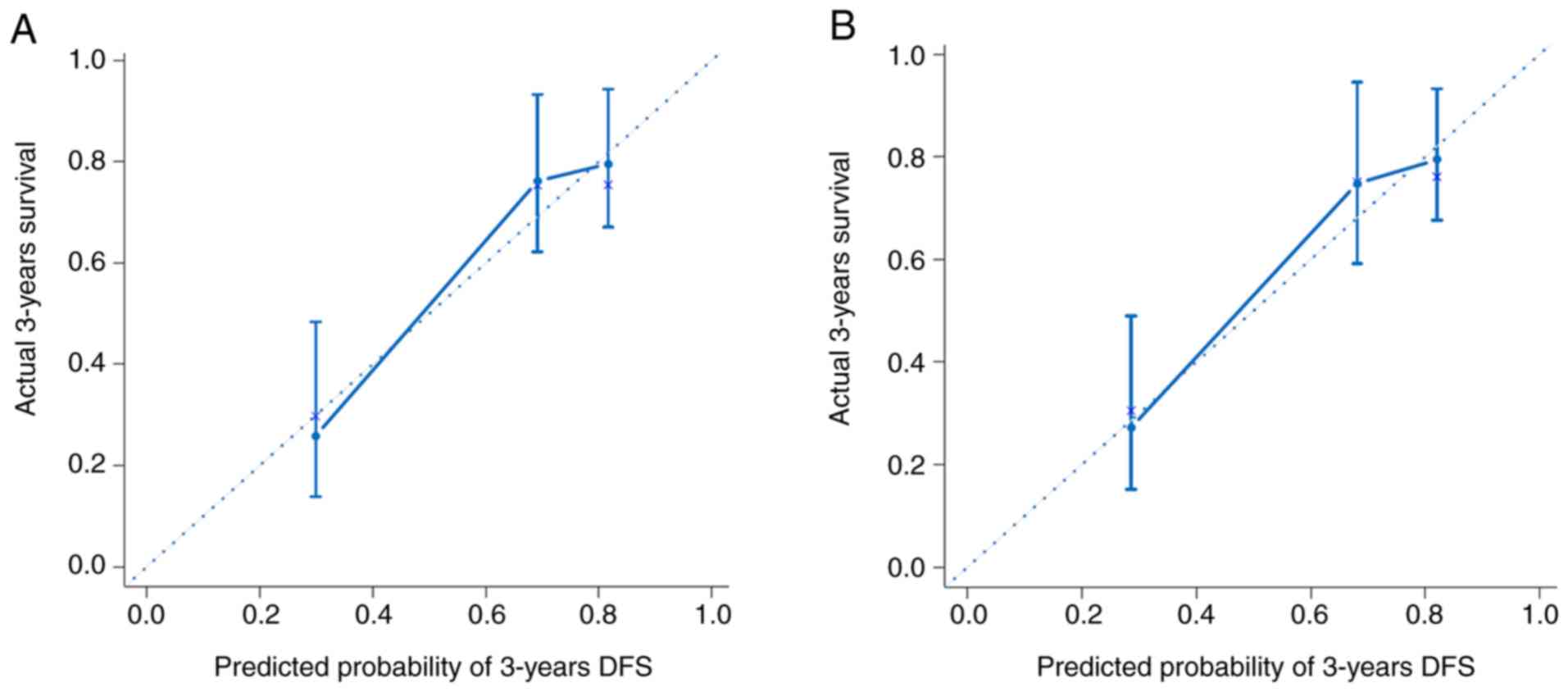
Addition of EDNRB expression improves
the predictive ability of model 1 for prognosis
These models were presented as a nomogram (Fig. 3). When calculating the iAUC value of
the ROC curve between 5 and 50 months to evaluate the model
discrimination, the results revealed that the iAUC value of model 2
was larger than that of model 1 after adding EDNRB expression as a
parameter (0.78 vs. 0.74; Fig. 4A;
Table IV). Similarly, the C-index
of model 2 was greater than that of model 1 (0.73 vs. 0.69;
Table IV), which indicated that the
model discrimination degree was improved after the EDNRB expression
parameter was added. Furthermore, the clinical significance of
EDNRB was analyzed by comparing the net benefits of model 1 and
model 2 using decision curve analysis. As shown in Fig. 4B, compared with model 1, in the
interval where the 3-year survival rate threshold was <0.52, the
net benefit of model 2 was higher according to the decision curve
analysis. IDI was calculated to judge the improvement of the model.
The results demonstrated that the IDI values of the model to
predict the 3- and 5-year survival rates were 0.04 (P=0.02) and
0.05 (P=0.01; Fig. 5; Table IV), respectively. These results
demonstrated that adding EDNRB expression as a parameter may
increase the accuracy of prognosis prediction. Additionally, the
calibration plot for the prediction of 3-year DFS in patients with
TNBC exhibited good agreement between nomogram predictions and
actual observation (Fig. 6).
 | Table IV.Validation of the prognostic value of
EDNRB. |
Table IV.
Validation of the prognostic value of
EDNRB.
| Variable | iAUC | C-index (95%
CI) | IDI for 3
years | P1 | IDI for 5
years | P2 |
|---|
| Model 1 | 0.74 | 0.69
(0.61–0.76) | 0.04 | 0.02 | 0.05 | 0.01 |
| Model 2 | 0.78 | 0.73
(0.65–0.81) |
|
|
|
|
Discussion
TNBC is highly heterogeneous, with a high risk of
local recurrence and distant metastasis. At present, chemotherapy
is the main clinical treatment method (20,21).
EDNRB serves an important role in cancer development and lymphatic
metastasis (8–11,22). At
present, the expression and clinical significance of EDNRB in TNBC
remain unclear. The results of the present study demonstrated that
EDNRB was expressed at low levels in TNBC, and is associated with
favorable prognostic and predictive value.
The positive expression rate of EDNRB in the present
study was 23.2%, which was close to the positive expression rate of
22.2% in all breast cancer types in a previous study (23). In line with the results of studies on
prostate and liver cancer (14,15), the
present study revealed that EDNRB expression was low in TNBC
samples, and this was also observed in the TCGA cohort. This
indicated that EDNRB may serve an anticancer role in TNBC.
The tumor microenvironment is a complex milieu,
which includes endothelial cells, fibroblasts, immune cells and
mesenchymal stem cells (24). Immune
cells and stromal cells are the main non-tumor components of the
tumor microenvironment (24).
Stromal cells are considered to serve an important role in tumor
growth, progression and spread (25,26). The
present study demonstrated that EDNRB expression was moderately
positively correlated with the matrix score (rs=0.44; P<0.01),
but weakly correlated with the immune score (rs=0.19; P=0.02). This
suggested that the role of EDNRB in the occurrence and development
of TNBC may be associated with stromal cells rather than immune
cells, and this should be validated in future studies.
Several studies have demonstrated that EDNRB may be
associated with the occurrence and development of tumors (13–15). In
the HNCH cohort, multivariate analysis revealed that age was an
independent predictor of EDNRB expression (OR, 3.37; 95% CI,
1.28–8.87; P=0.01). This result was verified in the TCGA cohort.
The average age in the TCGA cohort was higher than that in the HNCH
cohort (55.79 years vs. 48.76 years), and the positive rate of
EDNRB was higher (52.8% vs. 23.2%). Wülfing et al (12), revealed that EDNRB expression is
associated with tumor size in breast cancer. The present study
reported that EDNRB expression was also associated with T stage in
TNBC. A previous study has demonstrated that EDNRB is involved in
lymph angiogenesis following activation by ET-1 (11). In line with this, in the present
study, multivariate analysis in the TCGA cohort revealed that N
stage was an independent predictor of EDNRB expression (OR, 4.30;
95% CI, 1.33–13.89; P=0.02). Lymph node involvement is usually
associated with the prognosis of patients, and the worse the
involvement, the poorer the prognosis (27). In the present study, EDNRB expression
was positively associated with lymph node stage, while the DFS time
was longer in patients with high EDNRB expression. This indicated
that EDNRB may serve different roles in different stages of tumor
occurrence and development, which requires further research and
verification at the molecular level.
EDNRB is associated with the prognosis of various
types of cancer (13–15). A previous study had demonstrated that
high expression levels of EDNRB were associated with a poor
prognosis in breast cancer (18),
and this conclusion was based on prognosis analysis of the
difference in expression of EDNRB in all types of breast cancer, of
which only 25.1% were TNBC. In the present studym with a median
follow-up time of 36 months, Kaplan-Meier survival analysis
revealed that the relapse risk of EDNRB-positive patients was 0.36
times that of EDNRB-negative patients [hazard ratio (HR), 0.36; 95%
CI, 0.14–0.91; P=0.03]. In contrast to a study by Gu et al
(18), all cases in the HNCH cohort
in the present study were classified as TNBC, with 61.6% of
patients being younger than 50 years. The difference between the
two conclusions was due to the difference in the characteristics of
the patients involved. Multivariate Cox regression analysis was
used to further correct for confounding factors. The results
revealed that EDNRB expression was an independent predictor of
prognosis (HR, 0.38; 95% CI, 0.15–0.98; P=0.04). Subsequently, two
models were established using the multivariate Cox regression
analysis results, and the accuracy of EDNRB for the prediction of
prognosis was analyzed using multiple indicators and angles. IDI
indicated the extent to which a new marker reclassifies subjects,
and it is a method to evaluate the ability of a new marker to
predict a binary outcome of interest (28). The results suggested that the IDI
values of the model for predicting the 3- and 5-year survival rates
were 0.04 and 0.05, respectively, following the addition of the
EDNRB parameter, and the difference was statistically significant.
This indicated that EDNRB may improve the prediction accuracy of
the model for prognosis. Decision curve analysis is a method for
the evaluation of clinical net benefit (29). In the present study, the decision
curves of models 1 and 2 intersected at the 3-year survival rate
threshold of 0.52, below which model 2 had a higher net benefit.
Additionally, the analysis revealed that the result was of clinical
significance. The model predicted a 3-year survival rate of 0.52 as
a high-risk threshold in clinical decision-making. Intervention
measures should be implemented within the range where the threshold
is <0.52, and there was no clinical value in the range
>0.52.
The present study had certain advantages and
disadvantages. To the best of our knowledge, the present study was
the first large-scale study to analyze the association between
EDNRB and clinicopathological data, and the prognosis of patients
with TNBC. However, the disadvantages were as follows: This was a
retrospective clinical study with low evidence level; the end point
of the present study was DFS, but no overall survival analysis was
performed; the follow-up time of this study was short, so the
accuracy of predicting 5-year DFS was low, meaning that the
calibration plot and decision curve analysis results for predicting
5-year DFS could not be obtained; and the present study lacked
molecular mechanism research at the cellular level.
In conclusion, the present study investigated EDNRB
expression in TNBC and its association with prognosis. EDNRB
expression was correlated with stromal scores. Patients with TNBC
with low EDNRB expression had a shorter DFS time, and EDNRB may
improve the ability to predict prognosis. This suggests that EDNRB
may be used as a novel biomarker for the prognosis of TNBC.
Acknowledgements
Not applicable.
Funding
The present study was supported by a grant from
Henan Province Medical Science and Technology Research Project
(SBGJ2018088).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SL performed the immunohistochemical experiment,
analyzed the experimental results and wrote the manuscript; JYZ
assisted in the immunohistochemical experiment; JJZ and DJ assisted
in analyzing the experimental results and revising the manuscript;
ZL designed the experiment and corrected the final manuscript. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the Affiliated Cancer Hospital of Zhengzhou
University. Written informed consent was obtained from the patients
when their samples were first collected.
Patient consent for publication
All patients provided informed consent for
publication of data.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
TNBC
|
triple-negative breast cancer
|
|
ER
|
estrogen receptor
|
|
PR
|
progesterone receptor
|
|
HER2
|
human epidermal growth factor
receptor
|
|
EDNRA
|
endothelin A receptor
|
|
EDNRB
|
endothelin B receptor
|
|
MAPK
|
mitogen-activated protein kinase
|
|
Erk
|
extracellular signal-regulated kinase
2
|
|
PI3K/AKT
|
phosphatidylinositol 3-kinase/protein
kinase B
|
|
DFS
|
disease-free survival
|
|
iAUC
|
Integrated area under the curve
|
|
C-index
|
concordance index
|
|
IDI
|
integrated discriminant
improvement
|
|
OR
|
odds ratio
|
|
HNCH
|
Henan Cancer Hospital
|
|
NAC
|
neoadjuvant chemotherapy
|
|
CI
|
confidence interval
|
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2018. CA Cancer J Clin. 68:7–30. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wang C, Kar S, Lai X, Cai W, Arfuso F,
Sethi G, Lobie PE, Goh BC, Lim LHK, Hartman M, et al: Triple
negative breast cancer in Asia: An insider's view. Cancer Treat
Rev. 62:29–38. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dent R, Trudeau M, Pritchard KI, Hanna WM,
Kahn HK, Sawka CA, Lickley LA, Rawlinson E, Sun P and Narod SA:
Triple-negative breast cancer: Clinical features and patterns of
recurrence. Clin Cancer Res. 13:4429–4434. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Inoue A, Yanagisawa M, Kimura S, Kasuya Y,
Miyauchi T, Goto K and Masaki T: The human endothelin family: Three
structurally and pharmacologically distinct isopeptides predicted
by three separate genes. Proc Natl Acad Sci USA. 86:2863–2867.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bagnato A and Natali PG: Endothelin
receptors as novel targets in tumor therapy. J Transl Med.
2:162004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Davenport AP, Hyndman KA, Dhaun N, Southan
C, Kohan DE, Pollock JS, Pollock DM, Webb DJ and Maguire JJ:
Endothelin. Pharmacol Rev. 68:357–418. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Namiki A, Hirata Y, Fukazawa M, Ishikawa
M, Moroi M, Aikawa J, Yabuki S and Machii K: Endothelin-1- and
endothelin-3-induced vasorelaxation via endothelium-derived nitric
oxide. Jpn J Pharmacol. 58 (Suppl 2):326P1992.PubMed/NCBI
|
|
8
|
Vacca F, Bagnato A, Catt KJ and Tecce R:
Transactivation of the epidermal growth factor receptor in
endothelin-1-induced mitogenic signaling in human ovarian carcinoma
cells. Cancer Res. 60:5310–5317. 2000.PubMed/NCBI
|
|
9
|
Green DS, Rupasinghe C, Warburton R,
Wilson JL, Sallum CO, Taylor L, Yatawara A, Mierke D, Polgar P and
Hill N: A cell permeable peptide targeting the intracellular loop 2
of endothelin B receptor reduces pulmonary hypertension in a
hypoxic rat model. PLoS One. 8:e813092013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Morbidelli L, Orlando C, Maggi CA, Ledda F
and Ziche M: Proliferation and migration of endothelial cells is
promoted by endothelins via activation of ETB receptors. Am J
Physiol. 269:H686–H695. 1995.PubMed/NCBI
|
|
11
|
Spinella F, Caprara V, Garrafa E, Castro
V, Rosanò L, Natali PG and Bagnato A: Endothelin axis induces
metalloproteinase activation and invasiveness in human lymphatic
endothelial cells. Can J Physiol Pharmacol. 88:782–787. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wülfing P, Diallo R, Kersting C, Wülfing
C, Poremba C, Rody A, Greb RR, Böcker W and Kiesel L: Expression of
endothelin-1, endothelin-A, and endothelin-B receptor in human
breast cancer and correlation with long-term follow-up. Clin Cancer
Res. 9:4125–4131. 2003.PubMed/NCBI
|
|
13
|
Vasaikar S, Tsipras G, Landázuri N, Costa
H, Wilhelmi V, Scicluna P, Cui HL, Mohammad AA, Davoudi B, Shang M,
et al: Overexpression of endothelin B receptor in glioblastoma: A
prognostic marker and therapeutic target? BMC Cancer. 18:1542018.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bastian PJ, Ellinger J, Heukamp LC, Kahl
P, Müller SC and von Rücker A: Prognostic value of CpG island
hypermethylation at PTGS2, RAR-beta, EDNRB, and other gene loci in
patients undergoing radical prostatectomy. Eur Urol. 51:665–674.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhang L, Luo B, Dang YW, He RQ, Chen G,
Peng ZG and Feng ZB: The clinical significance of endothelin
receptor type B in hepatocellular carcinoma and its potential
molecular mechanism. Exp Mol Pathol. 107:141–157. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cancer Genome Atlas Network, .
Comprehensive molecular portraits of human breast tumours. Nature.
490:61–70. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ren G, Tian Q, An Y, Feng B, Lu Y, Liang
J, Li K, Shang Y, Nie Y, Wang X and Fan D: Coronin 3 promotes
gastric cancer metastasis via the up-regulation of MMP-9 and
cathepsin K. Mol Cancer. 11:672012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gu X, Han S, Cui M, Xue J, Ai L, Sun L,
Zhu X, Wang Y and Liu C: Knockdown of endothelin receptor B
inhibits the progression of triple-negative breast cancer. Ann N Y
Acad Sci. 1448:5–18. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yoshihara K, Shahmoradgoli M, Martinez E,
Vegesna R, Kim H, Torres-Garcia W, Treviño V, Shen H, Laird PW,
Levine DA, et al: Inferring tumour purity and stromal and immune
cell admixture from expression data. Nat Commun. 4:26122013.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Belkacemi Y, Hanna NE, Besnard C, Majdoul
S and Gligorov J: Local and regional breast cancer recurrences:
Salvage therapy options in the new era of molecular subtypes. Front
Oncol. 8:1122018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bianchini G, Balko JM, Mayer IA, Sanders
ME and Gianni L: Triple-negative breast cancer: Challenges and
opportunities of a heterogeneous disease. Nat Rev Clin Oncol.
13:674–690. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Berger Y, Bernasconi CC and
Juillerat-Jeanneret L: Targeting the endothelin axis in human
melanoma: Combination of endothelin receptor antagonism and
alkylating agents. Exp Biol Med (Maywood). 231:1111–1119.
2006.PubMed/NCBI
|
|
23
|
Wülfing P, Kersting C, Tio J, Fischer RJ,
Wülfing C, Poremba C, Diallo R, Böcker W and Kiesel L:
Endothelin-1-, endothelin-A-, and endothelin-B-receptor expression
is correlated with vascular endothelial growth factor expression
and angiogenesis in breast cancer. Clin Cancer Res. 10:2393–2400.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Joyce JA and Pollard JW:
Microenvironmental regulation of metastasis. Nat Rev Cancer.
9:239–252. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hanahan D and Weinberg RA: Hallmarks of
cancer: The next generation. Cell. 144:646–674. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kalluri R and Zeisberg M: Fibroblasts in
cancer. Nat Rev Cancer. 6:392–401. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Beenken SW, Urist MM, Zhang Y, Desmond R,
Krontiras H, Medina H and Bland KI: Axillary lymph node status, but
not tumor size, predicts locoregional recurrence and overall
survival after mastectomy for breast cancer. Ann Surg. 237:732–739.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kerr KF, McClelland RL, Brown ER and
Lumley T: Evaluating the incremental value of new biomarkers with
integrated discrimination improvement. Am J Epidemiol. 174:364–374.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Vickers AJ and Elkin EB: Decision curve
analysis: A novel method for evaluating prediction models. Med
Decis Making. 26:565–574. 2006. View Article : Google Scholar : PubMed/NCBI
|