Introduction
Lung cancer is considered to be the leading cause of
death, as well as the leading cause of cancer-associated deaths
worldwide (1). It is estimated that
12.7 million new cases of lung cancer are diagnosed each year, and
that it causes 7.6 million deaths worldwide annually (2). Data from the Surveillance, Epidemiology
and End Results database have revealed that >57% of patients
with lung cancer exhibit distant metastasis upon diagnosis
(3). According to the latest data
released by the National Cancer Registration Center, lung cancer is
also the leading cause of cancer-associated deaths in China, with
incidence and mortality rates of 53.86 and 43.41/100,000 people per
year, respectively (4). Among all
lung cancer subtypes, non-small cell lung cancer (NSCLC) accounts
for >80% of lung cancer cases (5–7). The
5-year overall survival rate of patients with NSCLC has remained as
low (~16.1%) over the past two decades due to high rates of
recurrence and distant metastasis (8,9).
Therefore, there is an urgent requirement to identify diagnostic
and prognostic biomarkers for NSCLC to predict the occurrence of
metastasis and to guide treatment strategy.
MicroRNAs (miRNAs) are crucial post-transcriptional
regulators involved in numerous disease processes, including
tumorigenesis and metastasis (10–13).
Altered expression of various miRNAs has been reported in NSCLC and
demonstrated to be associated with carcinogenesis, tumor
progression and treatment outcome (14–17). In
addition, miRNAs can be detected in various human biofluids, such
as blood, serum and plasma, and thus have the potential to be used
as biomarkers for the diagnosis of NSCLC (18–21).
Previous studies have suggested that miRNA expression patterns may
be used to identify different cancer subtypes, for example,
distinguishing lung squamous cell carcinomas (SCCs) from
adenocarcinomas (ADCs) (22–24). However, existing literature regarding
the association of miRNAs with tumorigenesis, outcome of clinical
management and metastasis is considerably varied (25–27); for
example, miR-25 can serve different roles in the pathogenesis of
different types of cancer, exerting both tumor suppressor (26) and cancer promoting effects (25,27).
Furthermore, the underlying mechanisms of miRNA involvement in the
tumorigenesis, metastasis and recurrence of lung cancer are not
well understood, particularly regarding radio-resistance following
radiotherapy of patients with lung cancer. Our previous study
demonstrated that 2- and 4-Gy irradiation induced upregulated
expression of miR-130a, miR-25 and miR-191*, and promoted the
metastatic properties of A549 cells in vitro and in
vivo by upregulating the expression of vascular endothelial
growth factor (VEGF) and C-C chemokine receptor type 7 (CCR-7). The
aim of the present study was to investigate the diagnostic and
functional roles of miR-130a, miR-25 and miR-191* in NSCLC and to
determine their carcinogenic effects that enhance tumor metastasis
in vitro and in vivo.
Materials and methods
Patients
A total of 84 patients diagnosed with NSCLC at the
PLA Rocket Force Characteristic Medical Center between January 2014
and April 2016 were enrolled in the present study. The diagnosis of
all patients was confirmed by cytology or histopathology
assessment. The inclusion criteria were as follows: Complete
medical records, physical examination, fibrobronchoscopy, chest,
head and abdomen CT or abdominal ultrasound scan, whole-body bone
scan, final pathological diagnosis and clear surgical
histopathological diagnosis. The exclusion criteria were as
follows: Neurological abnormality, severe dysfunction of the heart,
liver, kidney or other organs, diabetes and hypertension. The
patient clinicopathological characteristics are presented in
Table I. Parallel information was
collected from 42 age- and sex-matched patients who did not exhibit
abnormalities upon physical examination at the PLA Rocket Force
Characteristic Medical Center in May 2014. The routine laboratory
and imaging tests performed included complete blood count, baseline
electrolyte measurement, blood chemistry profiling and chest
X-rays.
 | Table I.General information and clinical
characteristics of patients with NSCLC, and statistical differences
of miR expression levels in patients with different clinical
characteristics. |
Table I.
General information and clinical
characteristics of patients with NSCLC, and statistical differences
of miR expression levels in patients with different clinical
characteristics.
|
|
| P-value |
|---|
|
|
|
|
|---|
| Category | n (%) | miR-130a | miR-25 | miR-191-3p |
|---|
| Sex |
|
|
|
|
|
Male | 58 (69) | 0.477 | 0.180 | 0.102 |
|
Female | 26 (31) |
|
|
|
| Age, years |
|
|
|
|
|
<60 | 36 (43) | 0.762 | 0.035a | 0.058 |
|
≥60 | 48 (57) |
|
|
|
| Smoking status |
|
|
|
|
|
Yes | 42 (50) | 0.254 | 0.188 | 0.115 |
| No | 42 (50) |
|
|
|
| Radiotherapy |
|
|
|
|
|
Yes | 33 (39) | 0.004b | 0.003b | 0.047a |
| No | 51 (61) |
|
|
|
| Histological
type |
|
|
|
|
|
Adenocarcinoma | 46 (55) | 0.584 | 0.013a | 0.006b |
|
Squamous cell carcinoma | 38 (45) |
|
|
|
| Lymph node
metastasis |
|
|
|
|
|
Yes | 66 (79) | 0.887 | 0.200 | 0.639 |
| No | 18 (21) |
|
|
|
| Extracranial
metastasis |
|
|
|
|
|
Yes | 67 (80) | 0.777 | 0.534 | 0.773 |
| No | 17 (20) |
|
|
|
| BM |
|
|
|
|
|
Yes | 22 (26) | 0.559 | 0.542 | 0.535 |
| No | 62 (74) |
|
|
|
| No. of BM |
|
|
|
|
| 0 | 62 (74) | 0.529 | 0.871 | 0.670 |
| 1 | 5 (6) |
|
|
|
| ≥2 | 17 (20) |
|
|
|
| Maximum diameter of
BM, cm |
|
|
|
|
| 0 | 62 (74) | 0.448 | 0.305 | 0.121 |
| ≤2 | 11 (13) |
|
|
|
|
>2 | 11 (13) |
|
|
|
| TNM T stage |
|
|
|
|
| T1 | 3 (4) | 0.378 | 0.733 | 0.157 |
| T2 | 0 (0) |
|
|
|
| T3 | 5 (6) |
|
|
|
| T4 | 76 (90) |
|
|
|
| N stage |
|
|
|
|
| N0 | 18 (21) | 0.235 | 0.222 | 0.234 |
| N1 | 17 (20) |
|
|
|
| N2 | 24 (29) |
|
|
|
| N3 | 25 (30) |
|
|
|
| Survival
status |
|
|
|
|
|
Death | 26 (31) | 0.054 | 0.016a | 0.033a |
|
Survival | 58 (69) |
|
|
|
| ECOG performance
status |
|
|
|
|
| 1 | 47 (56) | 0.836 | 0.989 | 0.935 |
| 2 | 37 (44) |
|
|
|
Follow-up
All patients were followed up by outpatient visits
or telephone between June 2016 and June 2018, and no patients were
lost to the follow-up. The date of diagnosis was set as the start
of follow-up, and survival time was assessed monthly. The period
between the date of diagnosis and death due to any cause was
considered as the overall survival time. Patients who passed away
due to non-neoplastic causes and those who were alive at the end of
follow-up were included as censored data that met statistical
requirements.
Cell culture
The human bronchioloalveolar lung carcinoma cell
line A549 was obtained from the cell bank of Peking Union Medical
College Hospital. A549 cells were cultured at 37°C in RPMI-1640
medium (Gibco; Thermo Fisher Scientific, Inc.) supplemented with
10% fetal bovine serum (FBS; Gibco; Thermo Fisher Scientific, Inc.)
and antibiotics (100 U/ml penicillin and 100 µg/ml streptomycin;
Gibco; Thermo Fisher Scientific, Inc.) in a humidified chamber at
5% CO2. Cells were seeded at 5×105 cells per
60-mm culture dish.
Irradiation and experimental
groups
Following 24-h culture, A549 cells in the
exponential growth phase were irradiated with 2 or 4 Gy at a rate
of 442.89 cGy/min in a linear accelerator (source distance, 100 cm;
6 MeV; Elekta Instrument AB). The A549 cells treated with each dose
of radiation were divided into 3 subgroups and cultured for 2, 12
or 24 h. Non-irradiated A549 cells were collected at the indicated
time points and used as negative controls.
Animal model
A total of 30 female athymic BALB/c nu/nu mice (6–8
weeks; weight, ~18 g) were obtained from Vital River Laboratories
and housed in specific pathogen-free conditions with free access to
food and water, temperature of 20–25°C, relative humidity of 55–65%
and a 12-h light/dark cycle in the Beijing Laboratory Animal
Research Center (Beijing Institute of Science and Technology,
Beijing, China). Mice were injected with 5×105 A549
cells irradiated with 0-, 2- or 4-Gy X-rays via the tail vein, and
were separated into the 0-, 2- and 4-Gy groups. The mice in the
0-Gy group were divided into 3 groups according to the time point
of observation, with 6 mice in each group, and mice that did not
undergo inoculation of A549 were used as controls. Mice were
sacrificed 3, 6 or 10 weeks after inoculation, and lung and sera
samples were harvested and stored at −80°C.
RNA isolation
RNA isolation from serum
Total RNA were extracted from the serum of patients
and nude mice using a mirVana™PARIS™ Kit (cat. no. 1556;
Ambion; Thermo Fisher Scientific, Inc.), according to the
manufacturer's protocol. Briefly, ≤625 µl serum was mixed with an
equal volume of 2X denaturing solution at room temperature and
incubated on ice for 5 min. Subsequently, an equal volume of
acid-phenol: Chloroform was added for extraction of the aqueous
phase.
RNA extraction from A549 cells and
lung tissue of nude mice
The cells were washed twice with PBS prior to the
addition of 600 µl lysis/binding buffer (mirVana miRNA
Isolation kit; cat. no. 1561; Ambion; Thermo Fisher Scientific,
Inc.) directly to the culture plate or flask. The lysates were
manually harvested using a sterile cell scraper and transferred to
a 2-ml tube. The samples were stored at −80°C unless RNA was
immediately extracted according to the manufacturer's instructions
(Ambion; Thermo Fisher Scientific, Inc.).
For murine lung tissue, 0.2 g tissue was ground into
a powder in liquid nitrogen with a pre-cooled mortar and pestle.
The tissue was mixed with 1 ml lysis/binding buffer, followed by
acid-phenol: Chloroform extraction. Ethanol was added to the
samples prior to passing them through a filter cartridge containing
a glass-fiber filter for RNA immobilization. The filter was washed
with miRNA wash solution 1/2/3 three times, and the RNA was eluted
with 30 µl elution solution (low ionic-strength solution), with
both solutions included in the aforementioned kit.
Reverse transcription-quantitative
(RT-q)PCR quantification of miRNA expression
To quantify miRNA expression in A549 cells, the
TaqMan miRNA assay (Applied Biosystems; Thermo Fisher Scientific,
Inc.) was performed according to the manufacturer's instructions.
The template cDNA was synthesized from total miRNA using a TaqMan™
MicroRNA Reverse Transcription kit (cat. no. 4366596; Applied
Biosystems; Thermo Fisher Scientific, Inc.) and quantified by qPCR
using the following parameters: Hold at 50°C for 2 min,
denaturation at 95°C for 10 min, followed by 40 cycles at 95°C for
15 sec and 60°C for 60 sec. The TaqMan® Universal PCR
Master mix II (cat. no. 4440038; Applied Biosystems; Thermo Fisher
Scientific, Inc.) was used with a LightCycler 480 real-time PCR
system (Roche Molecular Systems, Inc.). The primers and probes of
the three miRNAs were purchased from Thermo Fisher Scientific, Inc.
(TaqMan® microRNA assay; cat. no. 4427975; Applied
Biosystems; Thermo Fisher Scientific, Inc.) U6 RNA was used for
internal normalization. Relative expression was calculated using
the following equations: Relative gene
expression=2−∆∆Cq; -∆∆Cq=(Cq gene of
interest-Cq internal control
gene)treated -(Cq gene of
interest-Cq internal control
gene)untreated (6,28).
miRNA transfection
A total of 5×105 A549 cells were seeded
per 60-mm plate 18–24 h prior to the transfection. The medium was
replaced with antibiotic-free medium 6–12 h before transfection.
Synthetic miRNA mimics and inhibitors (miR-130a, miR-25 and
miR-191*) and the negative control (cat. nos. 4464084, 4464066,
4464058 and 4464076; Thermo Fisher Scientific, Inc.) were
transfected into 70–80% confluent A549 cells using the
Lipofectamine® RNAiMAX (cat. no. 13778030; Invitrogen;
Thermo Fisher Scientific, Inc.) reagent according to the
manufacturer's instructions. The prepared mixtures of
Lipofectamine® RNAiMAX and miRNA mimics/inhibitor
diluted in Opti-MEM (cat. no. 31985-062; Invitrogen; Thermo Fisher
Scientific, Inc.) were incubated separately for 5 min at room
temperature, then added to adherent A549 cells and incubated at
37°C for 24 h. After 24 h transfection, cells were harvested for
the extraction of total RNA and protein.
Transwell invasion assay
Cell invasion was measured using 24-well micro
chemotaxis chambers with a membrane pore size of 8.0 µm (EMD
Millipore) pre-coated with 10 µg/ml Matrigel at 37°C for 30 min (BD
Biosciences). A549 cells transfected with miRNA mimics or
inhibitors were resuspended in 100 µl serum-free DMEM (cat. no.
10566016; Gibco; Thermo Fisher Scientific, Inc.) and seeded into
the upper well of each chamber. A total of 100 µl DMEM containing
10% FBS and 10% fibronectin (BD Biosciences) was loaded into the
lower well.
Cells were incubated at 37°C for 22 h. Cells in the
upper well that had not migrated were scraped off using a cotton
swab, and the cells that had migrated through the membrane were
fixed with 4% paraformaldehyde for 20 min and stained with Giemsa
for 10 min, both at room temperature. Fixed cells were imaged under
a phase-contrast microscope (magnification ×400) for six fields and
counted for statistical analysis.
Protein extraction and western
blotting
Transfected A549 cells were washed twice in ice-cold
PBS and lysed in RIPA lysis buffer with protease inhibitors (50
nmol/l HEPES, pH 7.5, 150 nmol/l NaCl, 1% glycerol, 1% Triton,
protease inhibitor cocktail). The protein concentration was
determined using a BCA Protein Assay kit (Beyotime Institute of
Biotechnology). A total of 25 µg protein was loaded per sample for
SDS-PAGE (12% acrylamide) and transferred to polyvinylidene
difluoride membranes (EMD Millipore). The membranes were blocked
using 5% skimmed milk in TBS-Tween (TBST; 0.05% Tween-20) at room
temperature for 1 h, and then incubated with antibodies against
VEGF (1:800; cat. no. 34-4300; Sigma-Aldrich; Merck KGaA), CCR-7
(1:2,000; cat. no. ab32527; Abcam) or tubulin (1:2,000; cat. no.
SC-12462; Santa Cruz Biotechnology, Inc.) for 2 h at room
temperature, the membrane was washed 3 times with TBST (10 min
each), followed by incubation with horseradish
peroxidase-conjugated mouse anti-rabbit secondary antibody for 1 h
at room temperature (1:1,000; cat. no. sc-2357; Santa Cruz
Biotechnology, Inc.). The signal was captured using a Super Signal
West Pico chemiluminescent substrate (cat. no. 34080; Pierce;
Thermo Fisher Scientific, Inc.) to visualize the bands, and
Image-Pro Plus 6.0 software (Media Cybernetics, Inc.) was used for
grayscale analysis.
Statistical analysis
Data are presented as the mean ± SD. Data were
processed using SPSS version 19.0 (IBM Corp.). The Mann-Whitney U
test was used to determine the statistical difference between the
expression levels of the three miRNAs and different clinical
characteristics. Associations between clinical characteristics and
miRNA expression were assessed by logistic regression analysis, and
survival was analyzed using the Kaplan-Meier method with Cox
regression. One-way ANOVA followed by Dunnett's post hoc test was
used to evaluated the statistical differences of the expression
levels of the three miRNAs or VEGF or CCR-7 mRNA/protein expression
at different time points of A549 cells with 0-, 2- and 4-Gy X-ray
irradiation or with miRNA transfection. Kruskal-Wallis test
followed by Tukey's or Dunnett's post hoc tests was used to
evaluate the statistical differences of three miRNAs expression in
lung tissues and serum of nude mice injected with A549 cells with
different doses of X-ray irradiation. Receiver operating
characteristic curves were used to evaluate the diagnostic value of
miR-130a, miR-25 and miR-191* in patients with NSCLC. P<0.05 was
considered to indicate a statistically significant difference.
Results
Associations between clinical features
of patients with NSCLC and the expression of miR-130a, miR-25 and
miR-191*
A total of 84 patients (58 male and 26 female) with
lung cancer with a mean age of 60.78 years (range, 37–87) were
enrolled in the present study. According to the International
Association for the Study of Lung Cancer Staging Project (29), various clinical stages were present
among the enrolled patients, including three cases at stage I, five
cases at stage III and 76 cases at stage IV. Detailed clinical
characteristics of the patients are presented in Table I. Notably, the expression of miR-25
and miR-191* was significantly higher in patients treated with
radiotherapy compared with those who did not receive radiotherapy
treatment, in patients with SCC compared with those with ADC, and
in patients who succumbed to NSCLC or the associated complications
during the follow-up period compared with those who survived
(P<0.05 and P<0.01; Table I;
Fig. S1B and C). miR-130a
expression levels were significantly different between the
radiotherapy and non-radiotherapy groups (P=0.004; Fig. S1A), and there was also a significant
difference in miR-25 expression between patients aged ≥60 and
<60 years (P=0.035; Table I;
Fig. S1B). There was no association
between miR-130a, miR-25 or miR-191* expression and sex, smoking
status, lymph node metastasis, extracranial metastasis, brain
metastasis (BM), number of BMs, maximum diameter of BM,
Tumor-Node-Metastasis (TNM) T stage (30), node (N) stage (30) or Eastern Cooperative Oncology Group
(ECOG) (31,32) performance status (P>0.05; Table I).
Logistic regression analysis of
clinical characteristics and the expression of miR-130a, miR-25 and
miR-191* in the serum of patients with NSCLC
Based on the optimal cut-off values for miR-130a,
miR-25 and miR-191* (Data S1 and Fig.
S2), logistic regression analysis was performed to determine
the association between the expression of each miRNA and clinical
characteristics. The results indicated that miR-130a expression was
associated with radiotherapy (P=0.021), but not sex, age, smoking
status, histological type, survival status, lymph-node metastasis,
BM, extracranial metastasis or ECOG value. By contrast, miR-25 and
miR-191* expression levels were associated with radiotherapy
(P=0.026 and P=0.014, respectively), histological type (P=0.010 and
P=0.005, respectively) and survival status (P=0.020 and P=0.043,
respectively) (Table II). The
expression of miR-25 was also significantly associated with age
(P=0.019).
 | Table II.Logistic regression analysis of
factors that affect the expression of miR-130a, miR-25 and miR-191*
in the serum of patients with non-small cell lung cancer. |
Table II.
Logistic regression analysis of
factors that affect the expression of miR-130a, miR-25 and miR-191*
in the serum of patients with non-small cell lung cancer.
|
|
|
|
|
|
|
| 95% CI of
Exp(B) |
|---|
|
|
|
|
|
|
|
|
|
|---|
| microRNA | Clinical
characteristic | B | SE | Wald | P-value | Exp(B) | Lower | Upper |
|---|
| miR-130a | Radiotherapy | −1.228 | 0.533 | 5.315 | 0.021a | 0.293 | 0.103 | 0.832 |
|
| Age | 1.252 | 0.534 | 5.486 | 0.019a | 3.496 | 1.227 | 9.963 |
|
| Radiotherapy | −1.268 | 0.570 | 4.948 | 0.026a | 0.282 | 0.092 | 0.860 |
| miR-25 | Histological
type | 1.551 | 0.605 | 6.570 | 0.010a | 4.715 | 1.440 | 15.431 |
|
| Survival
status | −1.118 | 0.480 | 5.428 | 0.020a | 0.327 | 0.128 | 0.837 |
| miR-191* | Histological
type | 1.344 | 0.483 | 7.750 | 0.005b | 3.836 | 1.489 | 9.884 |
|
| Radiotherapy | −1.326 | 0.537 | 6.101 | 0.014a | 0.266 | 0.093 | 0.761 |
|
| Survival
status | −1.034 | 0.511 | 4.097 | 0.043a | 0.356 | 0.131 | 0.968 |
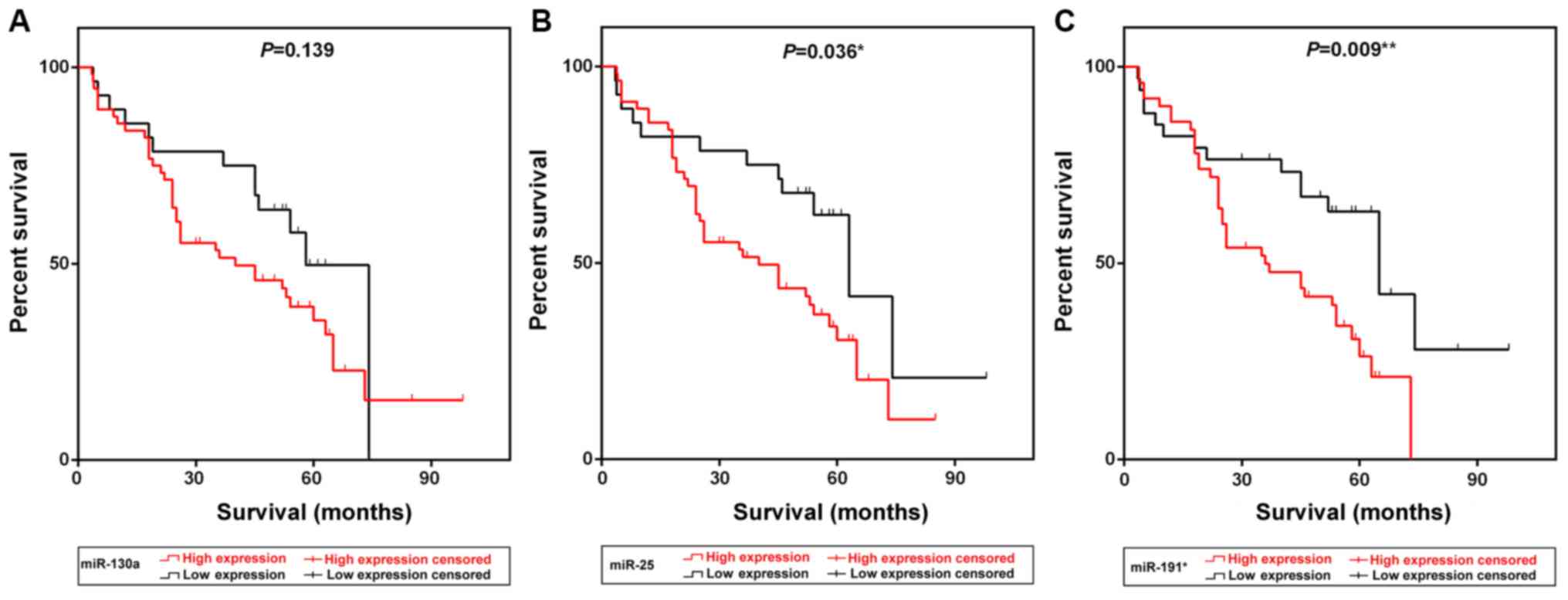
Kaplan-Meier survival curve analysis demonstrated
that patients exhibiting high expression of miR-25 and miR-191*
presented with low survival rates compared with patients with low
expression of the two miRNAs (P=0.036 and P=0.009, respectively;
Fig. 1B and C). The median survival
time of patients in the high miR-25 and miR-191* expression groups
was 40 and 36 months, respectively, which was notably lower
compared with the survival times of patients in the low expression
groups [63 (P=0.036) and 65 (P=0.009) months, respectively;
Table III]. Multivariate Cox
survival analysis indicated that radiotherapy (P=0.024), ECOG
status (P=0.008) and miR-191* expression (P=0.034) were independent
prognostic factors for NSCLC in this cohort (Table IV).
 | Table III.Analysis of miR-130a, miR-25 and
miR-191* expression and survival time of patients with non-small
cell lung cancer. |
Table III.
Analysis of miR-130a, miR-25 and
miR-191* expression and survival time of patients with non-small
cell lung cancer.
|
|
|
| 95% CI of HR |
|
|
|---|
|
|
|
|
|
|
|
|---|
| Expression
levels | Median survival
time, months | HR | Lower | Upper | Chi-square | P-value |
|---|
| miR-130a |
|
|
|
|
|
|
|
High | 40 | 1.584 | 0.878 | 2.77 | 2.188 | 0.139 |
|
Low | 58 | 0.631 | 0.361 | 1.14 |
|
|
| miR-25 |
|
|
|
|
|
|
|
High | 40 | 1.942 | 1.057 | 3.287 | 4.409 | 0.036a |
|
Low | 63 | 0.515 | 0.304 | 0.945 |
|
|
| miR-191* |
|
|
|
|
|
|
|
High | 36 | 2.12 | 1.235 | 3.71 | 6.789 | 0.009b |
|
Low | 65 | 0.472 | 0.27 | 0.81 |
|
|
 | Table IV.Multivariate analysis of
clinicopathological features, miR-130a, miR-25 and miR-191*
expression and prognosis of patients with non-small cell lung
cancer. |
Table IV.
Multivariate analysis of
clinicopathological features, miR-130a, miR-25 and miR-191*
expression and prognosis of patients with non-small cell lung
cancer.
|
|
|
|
|
|
| 95% CI of
Exp(B) |
|---|
|
|
|
|
|
|
|
|
|---|
| Factor | B | SE | Wald | P-value | Exp(B) | Lower | Upper |
|---|
| Age (<60 years
vs. ≥60 years) | −0.093 | 0.338 | 0.075 | 0.784 | 0.912 | 0.470 | 1.767 |
| Sex (male vs.
female) | −0.506 | 0.455 | 1.238 | 0.266 | 0.603 | 0.247 | 1.470 |
| Smoking status (yes
vs. no) | −0.360 | 0.404 | 0.707 | 0.372 | 0.697 | 0.316 | 1.538 |
| Radiotherapy (yes
vs. no) | 0.808 | 0.357 | 5.110 | 0.024a | 2.242 | 1.113 | 4.516 |
| Histological type
(LAD vs. LSCC) | −0.215 | 0.394 | 0.298 | 0.585 | 0.806 | 0.372 | 1.746 |
| Lymph node
metastasis (yes vs. no) | −0.173 | 0.385 | 0.202 | 0.653 | 0.841 | 0.395 | 1.789 |
| Extracranial
metastasis (yes vs. no) | −0.273 | 0.410 | 0.443 | 0.506 | 0.761 | 0.340 | 1.701 |
| Brain metastasis
(yes vs. no) | −0.261 | 0.396 | 0.436 | 0.509 | 0.770 | 0.355 | 1.672 |
| ECOG (score 1 vs.
2) | −0.876 | 0.328 | 7.133 | 0.008b | 0.416 | 0.219 | 0.792 |
| miR-130a expression
(up- vs. downregulation) | −0.406 | 0.450 | 0.812 | 0.368 | 0.666 | 0.276 | 1.611 |
| miR-25 expression
(up- vs. downregulation) | −0.723 | 0.487 | 2.200 | 0.138 | 0.485 | 0.187 | 1.261 |
| miR-191* expression
(up- vs. downregulation) | −0.825 | 0.389 | 4.509 | 0.034a | 0.438 | 0.205 | 0.938 |
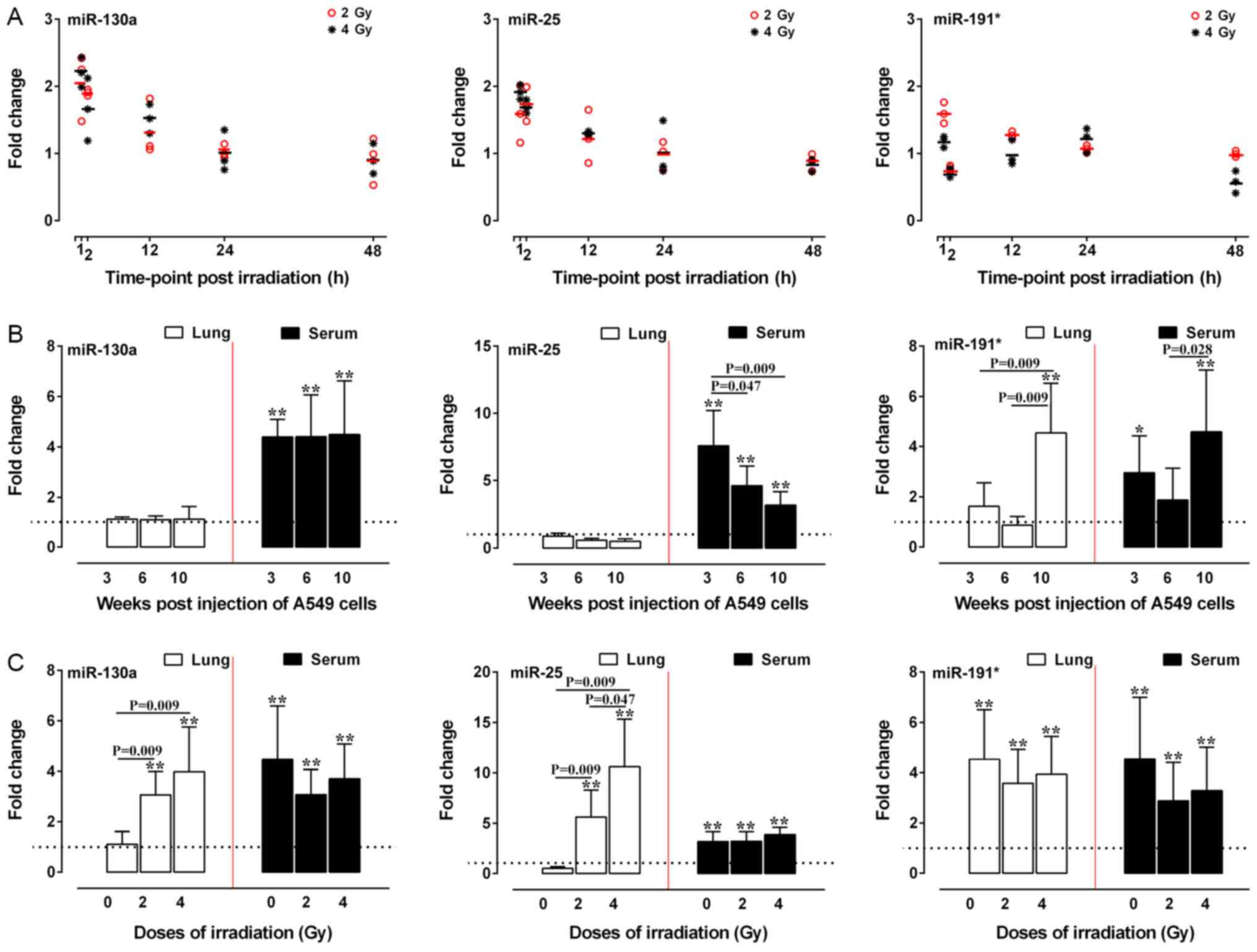
Two- and 4-Gy X-ray irradiation
upregulates the expression of miR-130a, miR-25 and miR-191* in A549
cells in vitro and in vivo
The aforementioned results indicated that
radiotherapy, histological type and prognosis were associated with
the expression of miR-130a, miR-25 and miR-191* in patients with
NSCLC. Therefore, the expression levels of miR-130a, miR-25 and
miR-191* in A549 cells treated with different doses of irradiation
were examined in vitro and in vivo. At 2 h post-2-Gy
irradiation, the expression levels of miR-130a and miR-25 were
significantly increased in A549 cells (P<0.05 and P<0.01),
whereas the expression levels of miR-191* were significantly
increased at 12 h post-irradiation compared with those in the
respective control groups (Fig. 2A).
At 2 h post-4-Gy irradiation, the expression levels of miR-191* and
miR-25 were also significantly increased (P<0.05 and P<0.01),
whereas the expression levels of miR-130a were significantly
increased at 12 h post-irradiation compared with those in the
respective control groups (P<0.05) (Fig. 2A).
For the in vivo study, 6 mice each in the
0-Gy group were sacrificed at 3, 6 and 10 weeks, and 5 mice each in
the 2- and 4-Gy groups were sacrificed at 10 weeks after injection.
At 3, 6 and 10 weeks after A549 cell injection, miR-130a and miR-25
expression was significantly increased in mice serum samples, but
there was no significant increase in lung tissue expression of
these miRNAs compared with in the control mice. The expression
levels of miR-191* were increased in the serum of nude mice at 3
and 10 weeks after injection when the mice exhibited visible tumors
scattered in the lungs (data not shown), while the miR-191*
expression in the lung tissues of nude mice was upregulated at 10
weeks after injection compared with that of the control group
(P<0.05; Fig. 2B). Both 2- or
4-Gy irradiation resulted in significant upregulation of the
expression levels of all three miRNAs at 10 weeks post injection in
the serum and lung tissue compared with those in the control group
(P<0.01; Fig. 2C). Notably, the
expression levels of miR-130a and miR-25 in the lung tissues of
mice treated with 2- and 4-Gy irradiation exhibited a
dose-dependent tendency to increase compared with those of mice
injected with non-irradiated A549 cells (P<0.05 and P<0.01;
Fig. 2C).
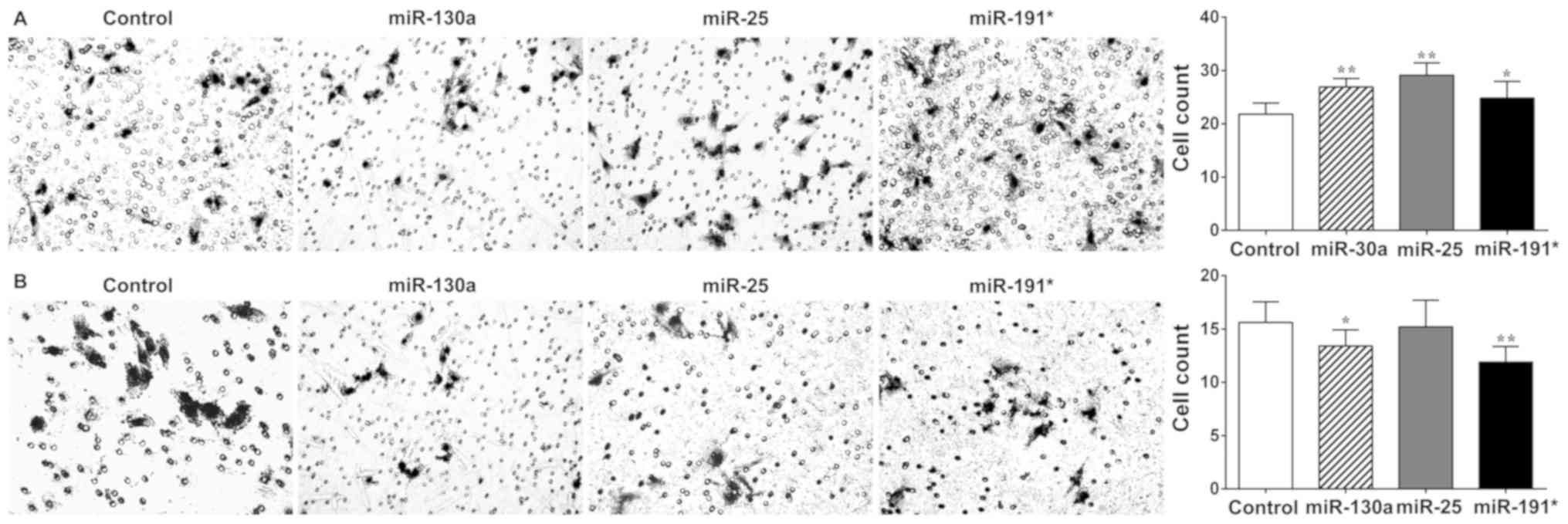
Roles of miR-130a, miR-25 and miR-191*
in A549 cell invasion in vitro
To delineate the roles of the three miRNAs in
response to X-ray irradiation, the effects of miR-130a, miR-25 and
miR-191* on the invasive capability of A549 cells were assessed
in vitro following transfection with miRNA mimics and
inhibitors. Transfection efficiency was verified by qPCR (data not
shown). The results of the cell invasion assay demonstrated that
the invasiveness of A549 cells transfected with miR-130a, miR-25
and miR-191* mimics was significantly increased compared with that
of the control group (P<0.05 and P<0.01; Fig. 3A). Additionally, transfection of A549
cells with miR-130a and miR-191* inhibitors significantly reduced
invasiveness (P<0.05; Fig. 3B),
while transfection of A549 cells with miR-25 inhibitor had no
significant effect on cell invasiveness.
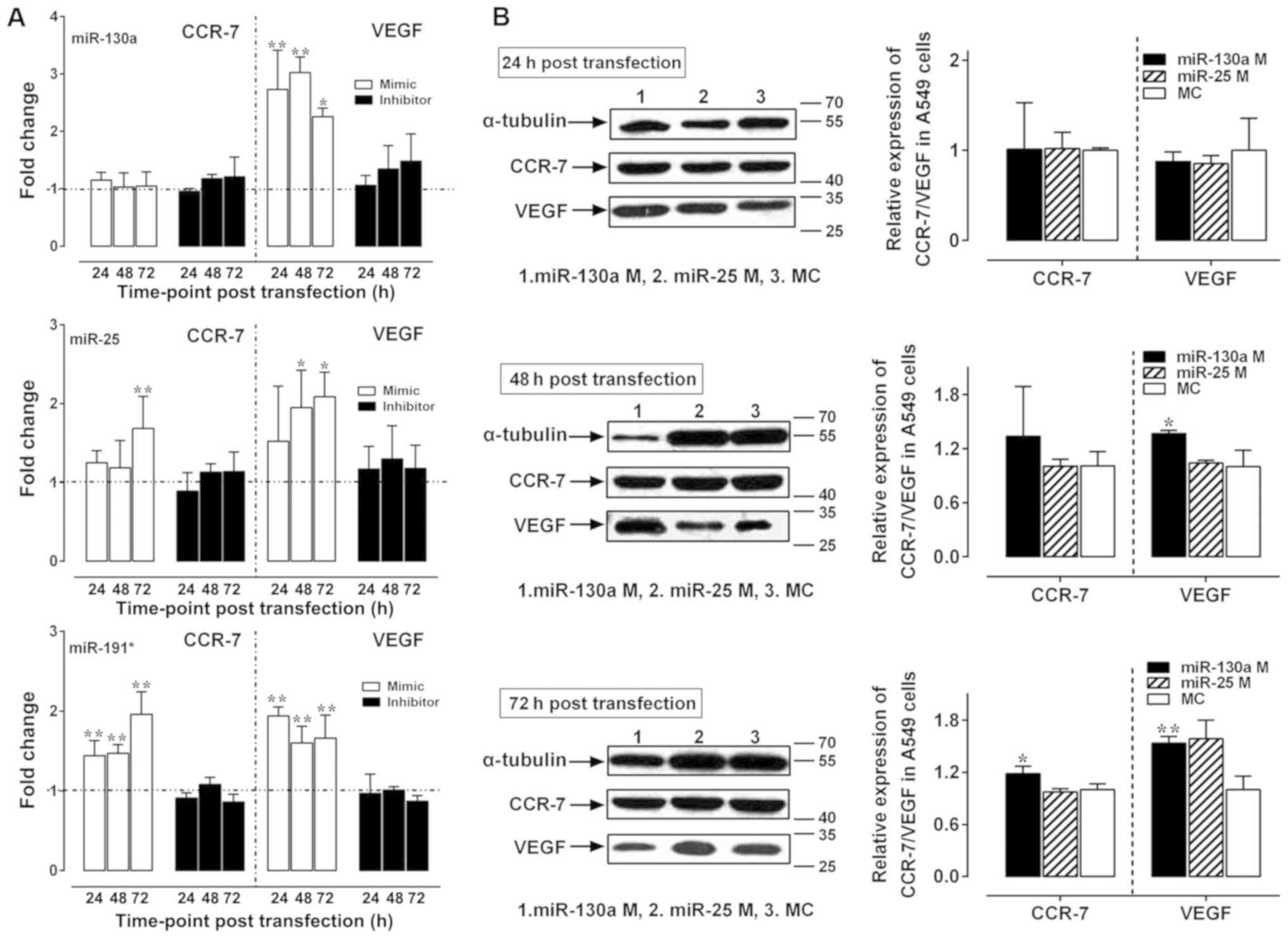
Our previous study has demonstrated that 2- and 4-Gy
X-rays promote the invasion of A549 cells in vitro and in
vivo mainly by upregulating the expression of VEGF and CCR-7
mRNA (33). Following A549 cell
exposure to 2- and 4-Gy X-ray irradiation, the expression of
miR-130a was positively correlated with the expression of VEGF and
CCR-7 mRNA (P<0.05), while the expression of miR-25 and miR-191*
was not significantly correlated with the expression of VEGF/CCR-7
mRNA (P>0.05) (34). Therefore,
the effects of miR-130a, miR-25 and miR-191* on the expression of
VEGF and CCR-7 in X-ray-irradiated A549 cells were subsequently
investigated. Upregulation of VEGF expression levels was observed
following transfection of all three miRNA mimics compared with
those in the control groups (P<0.05 and P<0.01; Fig. 4A), whereas upregulation of CCR-7
expression was observed in the miR-25 mimics group at 72 h and in
the miR-191* mimics group at 24, 48 and 72 h post-transfection
(P<0.05 and P<0.01; Fig. 4A).
Compared with those in the negative control group, protein
expression levels of VEGF were upregulated at 48 and 72 h
post-transfection with miR-130a mimics (P<0.05 and P<0.01,
respectively; Fig. 4B), whereas the
expression of CCR-7 was upregulated only at 72 h post-transfection
with miR-130a mimics (P<0.05; Fig.
4B). By contrast, no significant changes in the mRNA (Fig. 4A) or protein expression levels (data
not shown) of VEGF or CCR-7 were observed in the three miRNA
inhibitor transfection groups.
Discussion
Although a large number of circulating miRNAs have
been studied as potential biomarkers for NSCLC (7,20,35,36),
the value of detecting miRNAs in the blood for predicting the
prognosis of patients following radiotherapy has not yet been
defined. The results of the present study demonstrated that
upregulation of miR-130a, miR-25 and miR-191* expression in the
serum of patients with NSCLC was associated with radiotherapy,
histological type, low survival rate and low median survival time.
These results suggested that these miRNAs may serve roles in
predicting the prognosis of NSCLC. Existing miRNA biomarkers are
used as indicators for the early diagnosis in NSCLC (36,37),
carcinogenesis in gastric cancer and NSCLC (38,39),
metastasis (40,41) in lung adenocarcinoma and NSCLC,
disease recurrence in adrenocortical cancer (42), drug/radiotherapy-resistance (43) and prognosis in NSCLC (39). Geng et al (37) have identified five miRNAs (miR-20a,
miR-223, miR-21, miR-221 and miR-45) in the plasma for early-stage
NSCLC screening. Xu et al (44) have reported that miR-130a is
upregulated in the plasma of patients with NSCLC compared with
healthy controls, but not associated with poor prognosis. The
expression of miR-25 is increased in lung tissues of patients with
ADC with an epidermal growth factor receptor mutation, which is
frequent in non-smoking patients (45). In addition, previous studies have
indicated that the expression of miR-25 is significantly
upregulated in NSCLC tissues compared with in paired adjacent
tissues and negatively correlated with the protein expression of
regulator of G protein signaling 3 (46,47). In
consistence with previous reports, the results of the present study
suggested that patients with NSCLC exhibiting high expression of
miR-25 and miR-191* in the serum exhibited lower survival rates
compared with patients with low expression of these miRNAs. The
shorter median survival times of patients exhibiting high
expression of miR-25 and miR-191* indicates a role for these miRNAs
in predicting poor prognosis. In addition, miR-191* expression was
demonstrated to be an independent prognostic factor in patients
with NSCLC in the present study.
Further analysis demonstrated that the expression of
the three miRNAs in patients with SCCs or those who had undergone
radiotherapy was significantly higher compared with that in
patients with ADCs or those who had not undergone radiotherapy,
respectively. This suggested that miR-130a, miR-25 and miR-191* may
have a potential role in predicting the response to radiotherapy
and in differentiating SCCs from ADCs among patients with NSCLC.
Radiotherapy remains essential as a tool for the treatment of lung
cancer, particularly in patients with local or advanced metastases
for whom surgical treatment is not an option (48). However, radiotherapy of primary
tumors has been demonstrated to accelerate metastasis in mice
(49), thus limiting the efficacy of
radiotherapy. In addition, ionizing radiation promotes the
migration and invasion of a variety of tumor cells, including
glioma, neck squamous cell carcinoma, pancreatic cancer and lung
cancer cells (50). The underlying
mechanisms of this effect may involve the tumor microenvironment,
cell-cell junctions, extracellular matrix junction, protease
secretion and induction of epithelial-mesenchymal transition
(51–56). To investigate the potential role of
miRNAs in regulating the response to radiotherapy, the present
study analyzed the effects of 2- and 4-Gy X-ray irradiation on the
expression of miR-130a, miR-25 and miR-191* in A549 cells in
vitro and in vivo. The results demonstrated that 2- and
4-Gy irradiation promoted the expression of these three miRNAs, as
well as the invasiveness of A549 cells in vitro. Further
in vivo experiments revealed that irradiation promoted
metastasis in A549-cell xenograft mice, accompanied by high
expression of miR-130a, miR-25 and miR-191* in the serum. These
results indicated functional roles of the three miRNAs in
radiation-mediated metastasis and suggested that they may be
potential biomarkers of lung cancer metastasis induced by
radiotherapy.
miRNAs have been demonstrated to regulate invasion
and metastasis via a variety of mechanisms, including the
regulation of oncogene and/or tumor suppressor gene expression
(57,58), tumor metastasis-related gene
expression (59,60) and tumor angiogenesis-related gene
expression (61). VEGF and CCR-7 are
involved in metastasis, and have been clinically demonstrated to be
associated with metastasis and prognosis (62–65). The
present study aimed to further study the involvement of miR-130a,
miR-25 and miR-191* in radiation-mediated metastasis using A549
cells in vitro. miR-130a, miR-25 and miR-191* mimics
promoted the invasion of A549 cells, whereas miR-130a and miR-191*
inhibitors impeded their invasiveness. The miR-130a mimics also
increased the expression of VEGF mRNA and protein in A549 cells at
24, 48 and 72 h post-transfection, and the expression of CCR-7
protein was upregulated at 72 h post-transfection. miR-25 and
miR-191* mimic transfection increased the expression of CCR-7 and
VEGF only at the mRNA level. Overall, these results suggested that
miR-130a, miR-25 and miR-191* may promote the invasion of A549
cells by increasing VEGF and CCR-7 expression.
The results of the present study demonstrated the
significance of miR-130a, miR-25 and miR-191* in NSCLC,
particularly regarding diagnosis and tumor metastasis. However,
certain limitations remain in the present study. The number of
patients included in this study was relatively small, and the stage
distribution of the patients was uneven, which may have caused
selection bias. Furthermore, due to the large time-span of sample
collection, the follow-up time was extended accordingly, which may
also introduce bias. To address these issues, a larger cohort of
patients should be included in future studies, with a shorter
follow-up duration. In addition, the present study only used one
cell line, and including multiple cell lines in future studies will
help eliminate concerns that the observations made in the in
vitro and xenograft experiments were cell line-specific.
In conclusion, the results of the present study
demonstrated that the expression levels of miR-130a, miR-25 and
miR-191* were elevated in the serum of patients with NSCLC compared
with that of healthy control subjects, and that this was associated
with patient prognosis and response to radiotherapy. Therefore,
these miRNAs exhibit potential for use as biomarkers to predict the
prognosis and radiotherapy outcome for patients with NSCLC. In
vitro and in vivo study confirmed the tumorigenic roles
of miR-130a, miR-25 and miR-191* in radiation-mediated xenograft
metastasis in mice, supporting their possible clinical and
functional roles in radiation-mediated metastasis of lung
cancer.
Supplementary Material
Supporting Data
Acknowledgements
The authors would like to thank Dr Na Jia (Beijing
Institute of Microbiology and Epidemiology, Beijing, China) for
critical review of this manuscript, Ms. Ying Yang (Biolancet
Technology, Ltd., Beijing, China) for performing the microRNA
profile assay and Mr. Li-gang An (Beijing Laboratory Animal
Research Center, Beijing, China) for technical assistance.
Funding
The present study was supported by the China
Postdoctoral Science Foundation (grant no. 2014M552667), the
National Natural Science Foundation of China (grant no. 31770914)
and the Major Program of Military Logistics (grant no.
AEP17J001).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
JL, JA and QSJ conceived and designed the study. JL,
JA, AML and JG performed the experiments. ZXL, GLZ, WWH and HMC
participated in the acquisition and interpretation of data, drafted
the work and revised it critically for important intellectual
content. JL, YDZ, WWH and QSJ analyzed the data. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
All studies involving animals were performed
according to a protocol approved by the Animal Welfare Ethics
Committee of Beijing Experimental Animal Research Center [Beijing,
China; approval no. ShiYanXueKe (SYXK) (Beijing) 2011-0006]. Ethics
approval for the study involving human samples was provided by the
PLA Rocket Force Characteristic Medical Center Ethics Committee
(approval no. KeYan 2015038). Written informed consent was obtained
from all participants who donated lung tissue and serum
samples.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
ADC
|
adenocarcinoma
|
|
BM
|
brain metastasis
|
|
CCR-7
|
C-C chemokine receptor type 7
|
|
ECOG
|
Eastern Cooperative Oncology Group
|
|
miRNA
|
microRNA
|
|
NSCLC
|
non-small-cell lung cancer
|
|
SCC
|
squamous cell carcinoma
|
|
TNM
|
Tumor-Node-Metastasis
|
|
VEGF
|
vascular endothelial growth factor
|
References
|
1
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Torre LA, Siegel RL and Jemal A: Lung
cancer statistics. Adv Exp Med Biol. 893:1–19. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hayat MJ, Howlader N, Reichman ME and
Edwards BK: Cancer statistics, trends, and multiple primary cancer
analyses from the surveillance, epidemiology, and end results
(SEER) program. Oncologist. 12:20–37. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chen W, Zheng R, Baade PD, Zhang S, Zeng
H, Bray F, Jemal A, Yu XQ and He J: Cancer statistics in China,
2015. CA Cancer J Clin. 66:115–132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lortet-Tieulent J, Soerjomataram I, Ferlay
J, Rutherford M, Weiderpass E and Bray F: International trends in
lung cancer incidence by histological subtype: Adenocarcinoma
stabilizing in men but still increasing in women. Lung Cancer.
84:13–22. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Jemal A, Siegel R, Ward E, Hao Y, Xu J,
Murray T and Thun MJ: Cancer statistics, 2008. CA Cancer J Clin.
58:71–96. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Xu FX, Su YL, Zhang H, Kong JY, Yu H and
Qian BY: Prognostic implications for high expression of miR-25 in
lung adenocarcinomas of female non-smokers. Asian Pac J Cancer
Prev. 15:1197–1203. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yang L, Yang G, Zhou M, Smith M, Ge H,
Boreham J, Hu Y, Peto R, Wang J and Chen Z: Body mass index and
mortality from lung cancer in smokers and nonsmokers: A nationally
representative prospective study of 220,000 men in China. Int J
Cancer. 125:2136–2143. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Siegel R, Ward E, Brawley O and Jemal A:
Cancer statistics, 2011: The impact of eliminating socioeconomic
and racial disparities on premature cancer deaths. CA Cancer J
Clin. 61:212–236. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mitra R, Sun J and Zhao Z: MicroRNA
regulation in cancer: One arm or two arms? Int J Cancer.
137:1516–1518. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Worley LA, Long MD, Onken MD and Harbour
JW: Micro-RNAs associated with metastasis in uveal melanoma
identified by multiplexed microarray profiling. Melanoma Res.
18:184–190. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Paul P, Chakraborty A, Sarkar D, Langthasa
M, Rahman M, Bari M, Singha RS, Malakar AK and Chakraborty S:
Interplay between miRNAs and human diseases. J Cell Physiol.
233:2007–2018. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Budhu A, Jia HL, Forgues M, Liu CG,
Goldstein D, Lam A, Zanetti KA, Ye QH, Qin LX, Croce CM, et al:
Identification of metastasis-related microRNAs in hepatocellular
carcinoma. Hepatology. 47:897–907. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jiang LP, Zhu ZT, Zhang Y and He CY:
Downregulation of microRNA-330 correlates with the radiation
sensitivity and prognosis of patients with brain metastasis from
lung cancer. Cell Physiol Biochem. 42:2220–2229. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Dong J, Zhang Z, Gu T, Xu SF, Dong LX, Li
X, Fu BH and Fu ZZ: The role of microRNA-21 in predicting brain
metastases from non-small cell lung cancer. Onco Targets Ther.
10:185–194. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wang XC, Wang W, Zhang ZB, Zhao J, Tan XG
and Luo JC: Overexpression of miRNA-21 promotes
radiation-resistance of non-small cell lung cancer. Radiat Oncol.
8:1462013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Jiang LP, He CY and Zhu ZT: Role of
microRNA-21 in radiosensitivity in non-small cell lung cancer cells
by targeting PDCD4 gene. Oncotarget. 8:23675–23689. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Powrozek T, Krawczyk P, Kowalski DM,
Kuźnar-Kamińska B, Winiarczyk K, Olszyna-Serementa M,
Batura-Gabryel H and Milanowski J: Application of plasma
circulating microRNA-448, 506, 4316, and 4478 analysis for
non-invasive diagnosis of lung cancer. Tumour Biol. 37:2049–2055.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Matikas A, Syrigos KN and Agelaki S:
Circulating biomarkers in non-small-cell lung cancer: Current
status and future challenges. Clin Lung Cancer. 17:507–516. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Li W, Wang Y, Zhang Q, Tang L, Liu X, Dai
Y, Xiao L, Huang S, Chen L, Guo Z, et al: MicroRNA-486 as a
biomarker for early diagnosis and recurrence of non-small cell lung
cancer. PLoS One. 10:e01342202015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Greystoke A, Ayub M, Rothwell DG, Morris
D, Burt D, Hodgkinson CL, Morrow CJ, Smith N, Aung K, Valle J, et
al: Development of a circulating miRNA assay to monitor tumor
burden: From mouse to man. Mol Oncol. 10:282–291. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yanaihara N, Caplen N, Bowman E, Seike M,
Kumamoto K, Yi M, Stephens RM, Okamoto A, Yokota J, Tanaka T, et
al: Unique microRNA molecular profiles in lung cancer diagnosis and
prognosis. Cancer Cell. 9:189–198. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Volinia S, Calin GA, Liu CG, Ambs S,
Cimmino A, Petrocca F, Visone R, Iorio M, Roldo C, Ferracin M, et
al: A microRNA expression signature of human solid tumors defines
cancer gene targets. Proc Natl Acad Sci USA. 103:2257–2261. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Takamizawa J, Konishi H, Yanagisawa K,
Tomida S, Osada H, Endoh H, Harano T, Yatabe Y, Nagino M, Nimura Y,
et al: Reduced expression of the let-7 microRNAs in human lung
cancers in association with shortened postoperative survival.
Cancer Res. 64:3753–3756. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wu T, Hu H, Zhang T, Jiang L, Li X, Liu S,
Zheng C, Yan G, Chen W, Ning Y, et al: MiR-25 promotes cell
proliferation, migration, ad invasion of non-small cell lung cancer
by targeting the LATS2/YAP signaling pathway. Oxid Med cell Longev.
18:97197232019.
|
|
26
|
Li Q, Zou C, Zou C, Han Z, Xiao H, Wei H,
Wang W, Zhang L, Zhang X, Tang Q, et al: MicroRNA-25 functions as a
potential tumor suppressor in colon cancer by targeting smad7.
Cancer Lett. 335:168–174. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chen H, Pan H, Qian Y, Zhou W and Liu X:
miR-25-3p promotes the proliferation of triple negative breast
cancer by targeting BTG2. Mol Cancer. 17:42018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Schmittgen TD, Lee EJ and Jiang J:
High-throughput real-time PCR. Methods Mol Biol. 429:89–98. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Funai K, Kawase A, Mizuno K, Koyama S and
Shiiya N: 8th edition tumor, node, and metastasis T-stage prognosis
discrepancies: Solid component diameter predicts prognosis better
than invasive component diameter. Cancer (Basel). 12:15772020.
View Article : Google Scholar
|
|
30
|
Rami-Porta R, Bolejack V, Crowley J, Ball
D, Kim J, Lyons G, Rice T, Suzuki K, Thomas CF Jr, Travis WD, et
al: The IASLC lung cancer staging project: Proposals for the
revisions of the T descriptors in the forthcoming eighth edition of
the TNM classification for lung cancer. J Thorac Oncol.
10:990–1003. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Schiller JH, Harrington D, Belani CP,
Langer C, Sandler A, Krook J, Zhu J and Johnson DH; Eastern
Cooperative Oncology Group, : Comparison of four chemotherapy
regimens for advanced non-small-cell lung cancer. N Engl J Med.
346:92–98. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Sandler A, Gray R, Perry MC, Brahmer J,
Schiller JH, Dowlati A, Lilenbaum R and Johnson DH:
Paclitaxel-Carboplatin alone or with bevacizumab for non-small-cell
lung cancer. N Engl J Med. 355:2542–2550. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Lv J, Jiang QS, Song XJ, Wang CL, Guo LJ,
Wang SN, Li FS and Hu WW: Role of VEGF-A/C and CCR-7 in the
enhanced metastasis of A549 cells induced by 2 and 4 Gy X-rays in
vitro and in vivo. Sci China Tech Sci. 57:990–997. 2014. View Article : Google Scholar
|
|
34
|
Lv J, Wang SN, Song XJ, Li X, He R, Yu HJ,
Chen S, Wang L and Jiang QS: The impact of X-rays on the
expressions of miR-130a/miR-25 and its potential role in the
enhanced metastasis of A549 cell lines in vitro induced by X-rays.
Sci China Technol Sci. 56:2243–2249. 2013. View Article : Google Scholar
|
|
35
|
Doval DC, Deshpande R, Dhabhar B, Babu KG,
Prabhash K, Chopra R, Sripada PV, Deshmukh C and Suryavanshi M:
Liquid biopsy: A potential and promising diagnostic tool for
advanced stage non-small cell lung cancer patients. Indian J
Cancer. 54 (Suppl):S25–S30. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Han Y and Li H: miRNAs as biomarkers and
for the early detection of non-small cell lung cancer (NSCLC). J
Thorac Dis. 10:3119–3131. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Geng Q, Fan T, Zhang B, Wang W, Xu Y and
Hu H: Five microRNAs in plasma as novel biomarkers for screening of
early-stage non-small cell lung cancer. Respir Res. 15:1492014.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Zhou Y, Li R, Yu H, Wang R and Shen Z:
MicroRNA-130a is an oncomir suppressing the expression of CRMP4 in
gastric cancer. Onco Targets Ther. 10:3893–3905. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Wang K, Chen M and Wu W: Analysis of
microRNA (miRNA) expression profiles reveals 11 key biomarkers
associated with non-small cell lung cancer. World J Surg Oncol.
15:1752017. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Daugaard I, Veno MT, Yan Y, Kjeldsen TE,
Lamy P, Hager H, Kjems J and Hansen LL: Small RNA sequencing
reveals metastasis-related microRNAs in lung adenocarcinoma.
Oncotarget. 8:27047–27061. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Li Y, Li Y, Liu J, Fan Y, Li X, Dong M,
Liu H and Chen J: Expression levels of microRNA-145 and
microRNA-10b are associated with metastasis in non-small cell lung
cancer. Cancer Biol Ther. 17:272–279. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Chabre O, Libe R, Assie G, Barreau O,
Bertherat J, Bertagna X, Feige JJ and Cherradi N: Serum miR-483-5p
and miR-195 are predictive of recurrence risk in adrenocortical
cancer patients. Endocr Relat Cancer. 20:579–594. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Acunzo M, Visone R, Romano G, Veronese A,
Lovat F, Palmieri D, Bottoni A, Garofalo M, Gasparini P, Condorelli
G, et al: miR-130a targets MET and induces TRAIL-sensitivity in
NSCLC by downregulating miR-221 and 222. Oncogene. 31:634–642.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Xu X, Zhu S, Tao Z and Ye S: High
circulating miR-18a, miR-20a, and miR-92a expression correlates
with poor prognosis in patients with non-small cell lung cancer.
Cancer Med. 7:21–31. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Dacic S, Kelly L, Shuai Y and Nikiforova
MN: miRNA expression profiling of lung adenocarcinomas: Correlation
with mutational status. Mod Pathol. 23:1577–1582. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Wu T, Chen W, Kong D, Li X, Lu H, Liu S,
Wang J, Du L, Kong Q, Huang X and Lu Z: miR-25 targets the
modulator of apoptosis 1 gene in lung cancer. Carcinogenesis.
36:925–935. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Chen Z, Wu Y, Meng Q and Xia Z: Elevated
microRNA-25 inhibits cell apoptosis in lung cancer by targeting
RGS3. In vitro cell. Dev Biol Anim. 52:62–67. 2016. View Article : Google Scholar
|
|
48
|
Deek MP, Kim S, Yue N, Baby R, Ahmed I,
Zou W, Langenfeld J, Aisner J and Jabbour SK: Modern radiotherapy
using image guidance for unresectable non-small cell lung cancer
can improve outcomes in patients treated with chemoradiation
therapy. J Thorac Dis. 8:2602–2609. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Hartford AC, Gohongi T, Fukumura D and
Jain RK: Irradiation of a primary tumor, unlike surgical removal,
enhances angiogenesis suppression at a distal site: Potential role
of host-tumor interaction. Cancer Res. 60:2128–2131.
2000.PubMed/NCBI
|
|
50
|
Moncharmont C, Levy A, Guy JB, Falk AT,
Guilbert M, Trone JC, Alphonse G, Gilormini M, Ardail D, Toillon
RA, et al: Radiation-Enhanced cell migration/invasion process: A
review. Crit Rev Oncol Hematol. 92:133–142. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Wang H, Tan G, Dong L, Cheng L, Li K, Wang
Z and Luo H: Circulating miR-125b as a marker predicting
chemoresistance in breast cancer. PLoS One. 7:e342102012.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Farazi TA, Spitzer JI, Morozov P and
Tuschl T: miRNAs in human cancer. J Pathol. 223:102–115. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Manne U, Shanmugam C, Bovell L, Katkoori
VR and Bumpers HL: miRNAs as biomarkers for management of patients
with colorectal cancer. Biomark Med. 4:761–770. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Cha HJ, Shin S, Yoo H, Lee EM, Bae S, Yang
KH, Lee SJ, Park IC, Jin YW and An S: Identification of ionizing
radiation-responsive microRNAs in the IM9 human B lymphoblastic
cell line. Int J Oncol. 34:1661–1668. 2009.PubMed/NCBI
|
|
55
|
Baffa R, Fassan M, Volinia S, O'Hara B,
Liu CG, Palazzo JP, Gardiman M, Rugge M, Gomella LG, Croce CM and
Rosenberg A: MicroRNA expression profiling of human metastatic
cancers identifies cancer gene targets. J Pathol. 219:214–221.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Simone NL, Soule BP, Ly D, Saleh AD,
Savage JE, Degraff W, Cook J, Harris CC, Gius D and Mitchell JB:
Ionizing radiation-induced oxidative stress alters miRNA
expression. PLoS One. 4:e63772009. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Li N, Fu H, Tie Y, Hu Z, Kong W, Wu Y and
Zheng X: miR-34a inhibits migration and invasion by down-regulation
of c-Met expression in human hepatocellular carcinoma cells. Cancer
Lett. 275:44–53. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Sayed D, Rane S, Lypowy J, He M, Chen LY,
Vashistha H, Yan L, Malhotra A, Vatner D and Abdellatif M:
MicroRNA-21 targets Sprouty2 and promotes cellular outgrowths. Mol
Biol Cell. 19:3272–3282. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Valastyan S, Reinhardt F, Benaich N,
Calogrias D, Szász AM, Wang ZC, Brock JE, Richardson AL and
Weinberg RA: A pleiotropically acting microRNA, miR-31, inhibits
breast cancer metastasis. Cell. 137:1032–1046. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Valastyan S, Benaich N, Chang A, Reinhardt
F and Weinberg RA: Concomitant suppression of three target genes
can explain the impact of a microRNA on metastasis. Genes Dev.
23:2592–2597. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Chen Y and Gorski DH: Regulation of
angiogenesis through a microRNA (miR-130a) that down-regulates
antiangiogenic homeobox genes GAX and HOXA5. Blood. 111:1217–1226.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Yang X, Zhang Y, Hosaka K, Andersson P,
Wang J, Tholander F, Cao Z, Morikawa H, Tegnér J, Yang Y, et al:
VEGF-B promotes cancer metastasis through a VEGF-A-independent
mechanism and serves as a marker of poor prognosis for cancer
patients. Proc Natl Acad Sci USA. 112:E2900–E2909. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Jean C, Chen XL, Nam JO, Tancioni I, Uryu
S, Lawson C, Ward KK, Walsh CT, Miller NL, Ghassemian M, et al:
Inhibition of endothelial FAK activity prevents tumor metastasis by
enhancing barrier function. J Cell Biol. 204:247–263. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Ji RC: Lymph nodes and cancer metastasis:
New perspectives on the role of intranodal lymphatic sinuses. Int J
Mol Sci. 18:512016. View Article : Google Scholar
|
|
65
|
Liu Y, Wu BQ, Geng H, Xu ML and Zhong HH:
Association of chemokine and chemokine receptor expression with the
invasion and metastasis of lung carcinoma. Oncol Lett.
10:1315–1322. 2015. View Article : Google Scholar : PubMed/NCBI
|