Introduction
Obturator masses have a certain probability of
occurrence in pelvic tumors. The most common origins of obturator
masses are neurological tumors, including schwannoma and
neurofibroma (1–3). Local tumors around the lateral
obturator zone have been reported to be potentially resectable by
laparoscopic lateral pelvic tumor dissection (LLPTD) (4). However, only a limited number of
studies have assessed and confirmed the safety and operability of
such tumors (4). Careful inspection
of CT and MRI is important to determine the tumor positioning
preoperatively. The tumors, locating in the retroperitoneal space,
may be close to iliac vessels, obturator nerve and even spermatic
cords (1,2,5). In
order to gain better exposure for tumor dissection, exploratory
transperitoneal laparoscopy has usually been performed to treat
affected cases (4). Resection of the
tumor was carefully performed to ensure the safe removal of the
specimen with complete and functional preservation of the iliac
vessels and obturator nerve (2,6,7). In particular, cross-obturator masses
may be technically demanding due to the requirement for sufficient
operative space. The aim of the present study was to introduce a
technique modification with the combination of the laparoscopic
approach and hand-assisted (HA) open surgery for patients with
large obturator masses.
The present study reported on the use of a novel
operation procedure for coping with trans-obturator tumor,
combining laparoscopic with open approaches. Due to the limitation
of obturator obstruction and operation space, laparoscopic surgery
alone is not able to fully dissociate obturator tissue to reach the
tumor area below the obturator. In order to ensure the overall
removal of the tumor, the most appropriate method used in the
present study is to push the tumor to the area above the obturator
for laparoscopic dissection. This procedure requires open surgical
assistance. Compared with traditional open surgery, the present
method utilizes minimally invasive laparoscopic surgery and fine
dissection with fewer complications for fast recovery, and due to
these advantages, it may be is deemed more appropriate than the
usual clinical approach to meet the patient's clinical
requirement.
Case report
Case details
In January 2018, a 53-year-old male patient was
admitted to the Department of Urology, Daping Hospital, Army
Medical University (Chongqing, China) with a 1-month history of
abdominal discomfort. The patient was subsequently referred to the
Department of Urological Oncology for resection of the mass.
Ultrasound examination revealed a right pelvic space-occupying
lesion. No obvious palpable lymph nodes were detected. The
laboratory examination and chest X-rays were normal. A
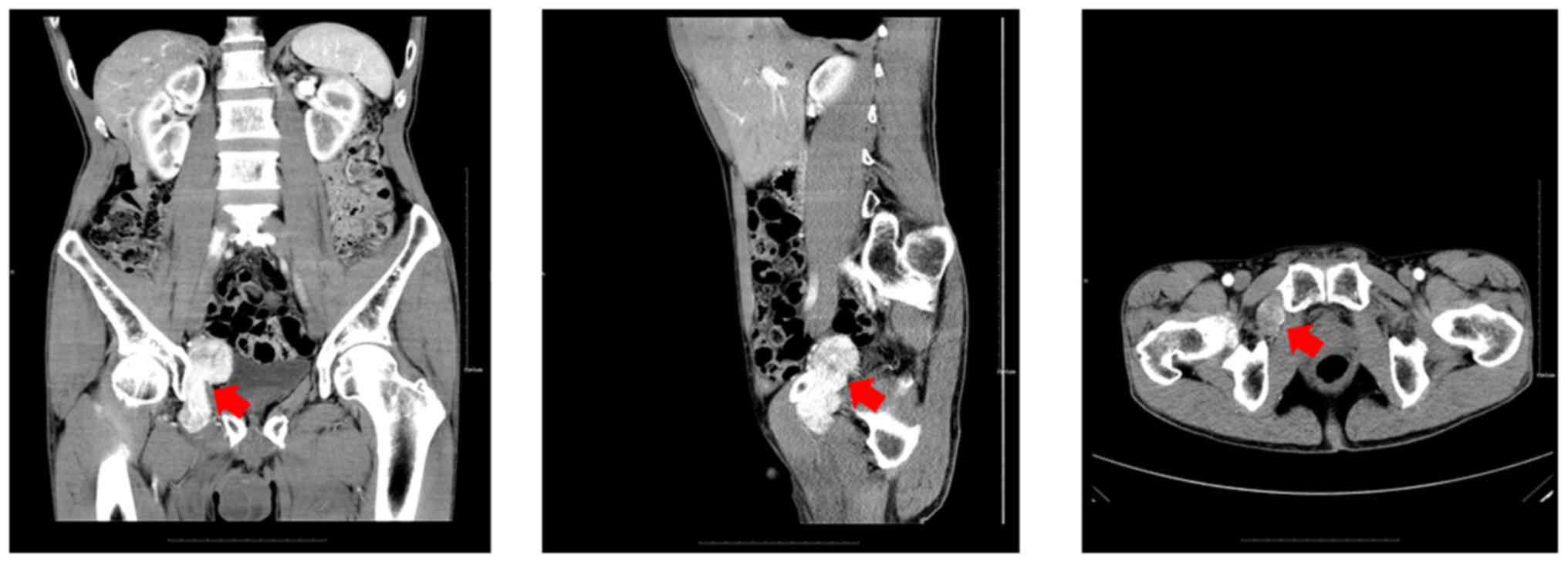
contrast-enhanced CT scan (Fig. 1)
revealed a heterogeneously enhanced mass, measuring 35×37×76 mm,
located in the right pelvic space, with infiltrative growth,
extending into and passing through the obturator foramen, 4 cm
above and 3 cm below the obturator fossa, neighboring the pelvic
wall. Lymph node involvement was not detected on CT examination.
The suspected preoperative diagnosis included vagal nerve
schwannoma, fibroid tumor, paraganglioma, inflammatory pseudotumor
or non-Hodgkin lymphoma. The baseline characteristics of the
patient are presented in Table I.
The clinical samples and images were provided by the Department of
Pathology and Medical Imaging following approval by the Research
Ethics Committee of Daping Hospital, Army Medical University
(Chongqing, China) and obtaining written informed consent from the
patient. The treatment plan was discussed by the multidisciplinary
board of the hospital.
 | Table I.Characteristics of the patient. |
Table I.
Characteristics of the patient.
| Item |
Value/description |
|---|
| Sex | Male |
| Age (years) | 53 |
| BMI
(kg/m2) | 30.5 |
| Operation | Laparoscopic LPTD and
Open |
| Histology | Solitary fibrous
tumor |
| Pathological
stage | I |
Surgical technique
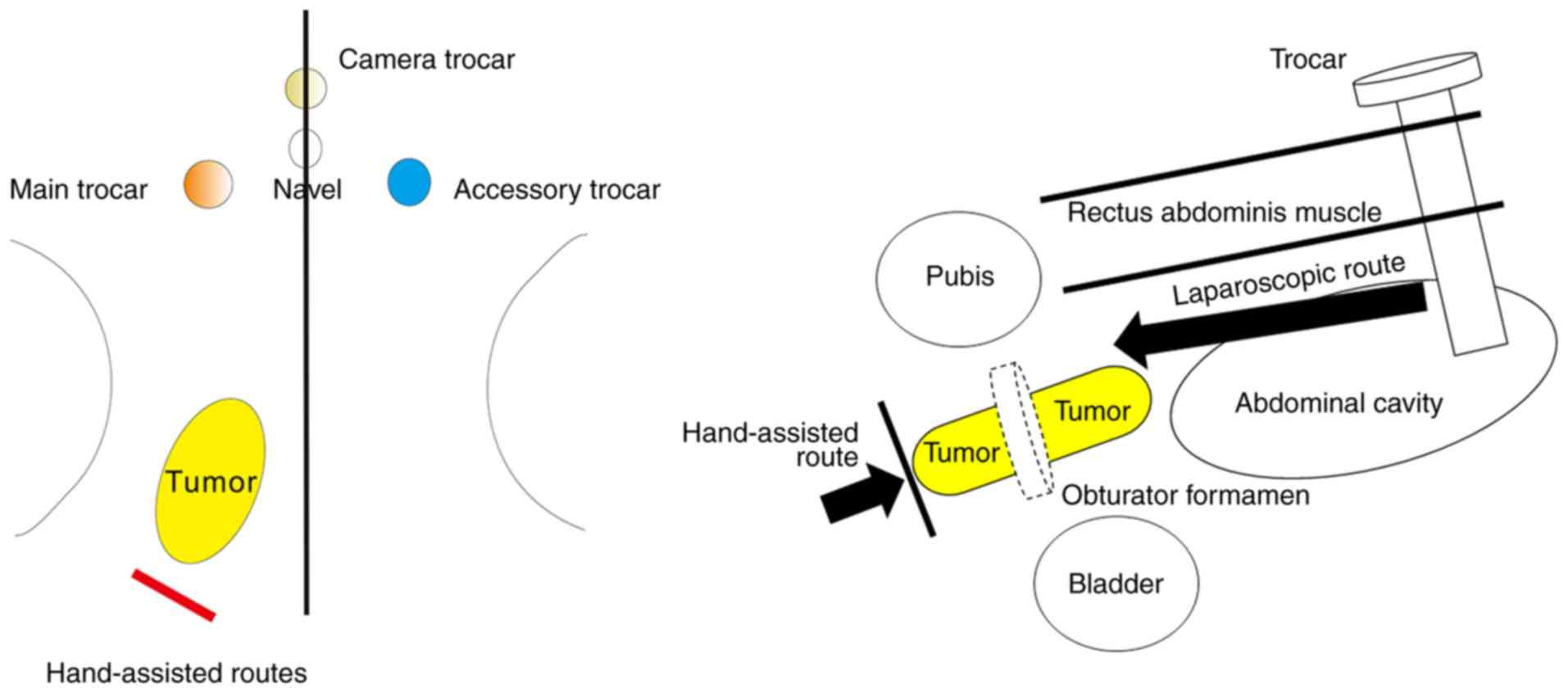
The surgical procedure was based on the combination
of laparoscopic and open surgery. The mass was planned to be
removed by transabdominal laparoscopic dissection with the aim of
achieving better exposure, complete dissection and sufficient
hemostasis to stem bleeding.
First, a small 15-mm incision was made above the
umbilicus. The anterior rectus sheath was then incised, followed by
parting the rectus abdominis muscle exactly in the middle. A 12-mm
trocar was inserted into the abdominal space through the posterior
rectus sheath, which was used as the camera port. Two 12-mm ports
were also inserted laterally to the rectus abdominis muscle, one on
each side.
The procedure was performed according to the
previous description for LLPTD surgery (4). The external iliac vein was first
exposed upon identifying the pubic bone and Cooper's ligament as
anatomical landmarks, which was followed by opening the peritoneum
and separating the vessels in the obturator canal. The tumor
completely occupied the obturator space and the obturator nerve was
closely associated with the tumor. The obturator nerve was
carefully isolated and preserved. The internal iliac vessel
branches supplying the tumor, including artery and vein, were
dissected and then clamped.
However, during surgery, the upper part of the tumor
extending above the obturator fossa fully occupied the obturator
space; therefore, there was insufficient space for exploring and
excising the lower part of the tumor below the obturator foramen.
In order to solve this problem and achieve complete resection, an
open exploratory incision was made on the inner side of the
inguinal ligaments in order to push the lower part of the tumor
upwards. By combining the laparoscopic and open routes, the tumor
was fully excised. No intraoperative complications occurred
(Fig. 2). The dissected mass was
placed into the sample bag and extracted through the 12-mm port
trocar.
Outcome
The perioperative baseline information of the
patient is presented in Table II.
The operative time was 210 min. The estimated blood loss was 200
ml. R0 resection was achieved. Laparoscopic imaging revealed an
8-cm mass spanning the obturator fossa and compressing the
obturator nerve. The postoperative hospital stay was 11 days. There
were no severe postoperative complications except transient low
intestinal obstruction and weakness of the adductor muscle.
 | Table II.Perioperative data. |
Table II.
Perioperative data.
| Item |
Value/description |
|---|
| Operative time
(min) | 210 |
| Blood loss (ml) | 200 |
| Adjacent structures
removed en bloc | None |
| Post-operative
complications | Low intestinal
obstruction/weakness of the adductor muscle |
| Post-operative
hospital stay (days) | 10 |
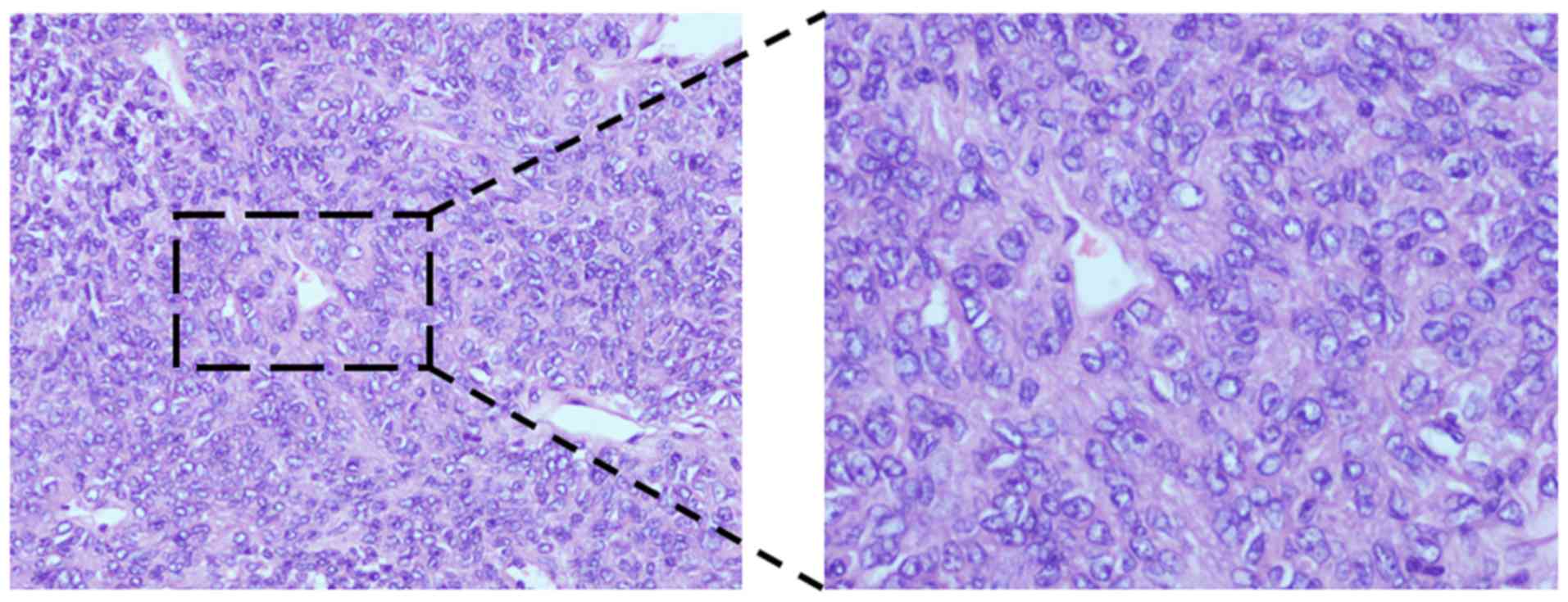
The cut surface of the tumor had a white to tan
appearance. Hematoxylin and eosin staining and immunohistochemical
examination revealed significantly increased cellular
proliferation, locally scattered mast cells, 2 mitotic figures per
10 high-power fields and positive CD117, CD34 and STAT6 staining,
findings consistent with solitary fibrous tumor (SFT), which is a
mesenchymal neoplasm without typical symptoms (Fig. 3). The patient reported postoperative
short-term dysfunction of hip joint adduction and right leg pain
due to mild obturator nerve damage during the dissection. At the
hospital, the patient received timely neurotrophic therapy based on
methylcobalamin. The 2-month follow-up revealed no residual disease
based on CT evaluation.
Literature review
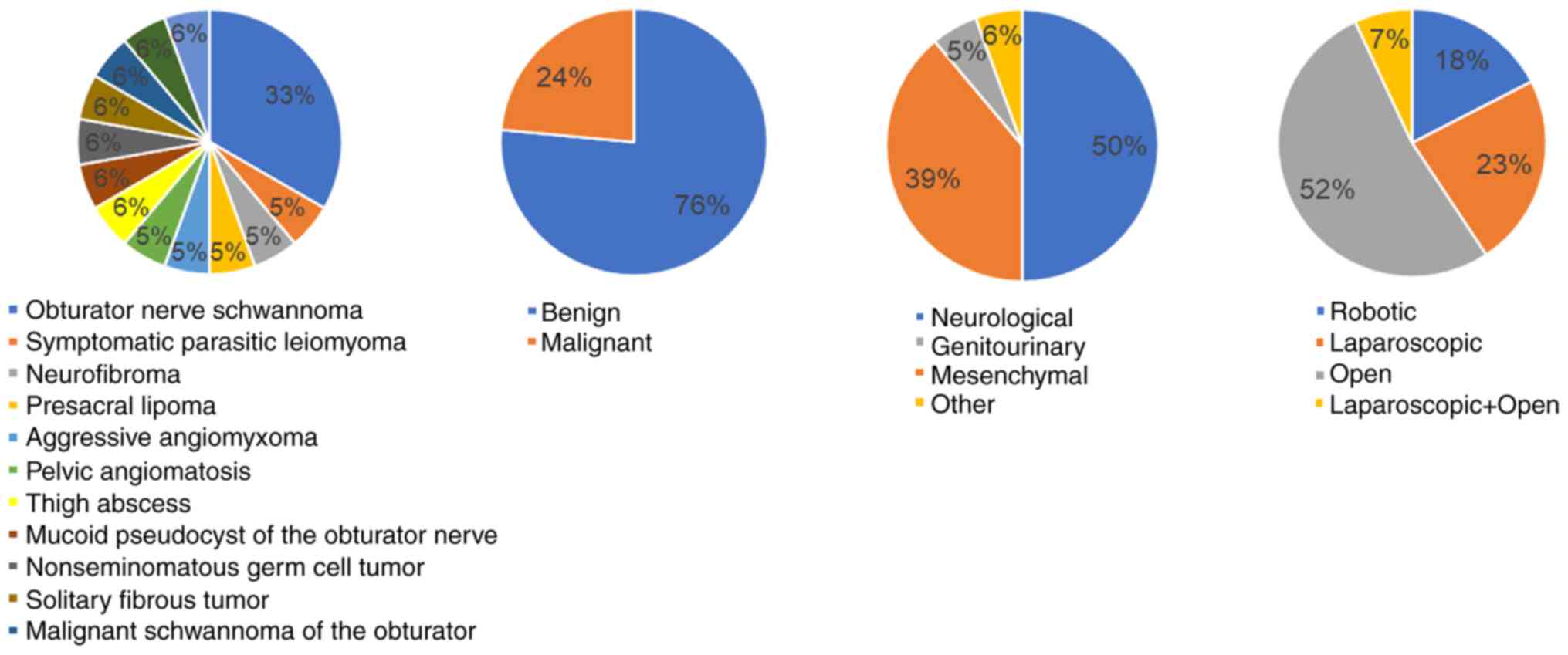
A total of 186 articles were retrieved by searching
the PubMed database for studies published between January 13, 2006
and December 20, 2019 using the search term ‘mass in obturator’.
Publications were included in the review if they met the following
list of preset inclusion criteria: i) The mass was located in the
obturator fossa; ii) the mass was a solid tumor based on surgical
biopsy diagnosis or imaging diagnosis; iii) lymph node or tumor
metastasis was excluded. A total of 17 publications, mainly case
reports, were included in the review of the present study. A total
of 6 cases were diagnosed as obturator nerve schwannoma (2,6–10) and 1 case was a malignant schwannoma
of the obturator nerve treated with neoadjuvant chemotherapy
followed by neurosurgery (1). Other
types of tumor (1 case each) included retroperitoneal extragonadal
germ cell tumor (5), pelvic
angiomatosis (11), parasitic
leiomyoma (12), neurofibroma
(3), presacral lipoma (13), aggressive angiomyxoma (14), mucoid pseudocyst of the obturator
nerve (15), thigh abscess
mistakenly diagnosed as sarcoma (16), fibroblastic osteosarcoma (17) and desmoid tumor (18). The patients' characteristics are
summarized in Table III. From the
previous studies and the present study, data on the cases of
obturator tumor were extracted and further analyzed based on
composition ratio and are presented in Table IV and Fig. 4. The majority of the cases were
benign (~75%) and originated from neural tissue (~50%). The
selected operative approach was either open or minimally invasive
(50% each).
 | Table III.Cases of tumors in the obturator
region reported in the literature. |
Table III.
Cases of tumors in the obturator
region reported in the literature.
| Author (year) | Sex | Age at onset
(years) | Single tumor | Tumor type | Operative
approach | Operation time
(min) | Post-operative
Complications | Hospital stay
(days) | (Refs.) |
|---|
| Menderes (2018) | F | 48 | Yes | Symptomatic parasitic
leiomyoma (3.3 cm) | Robotic | NS | None | 1 | (12) |
| Chao (2018) | F | 33 | Yes | Neurofibroma (3.7
cm) | Open | 450 | Mild weakness and
paresthesia affecting the leg | 15 | (3) |
| Gleason (2017) | F | 63 | Yes | Obturator nerve
schwannoma (4.5 cm) | Open | NS | Neurologic deficits
with resolution of pelvic pain | 3 | (9) |
| Poskus (2018) | F | 42 | Yes | Presacral lipoma (15
cm) | Laparoscopic | 80 | None | 2 | (13) |
| Kanao (2019) | F | 46 | Yes | Aggressive
angiomyxoma (8 cm) | Laparoscopic and
Open | NS | None | NS | (14) |
| Chopra (2017) | M | 46 | Yes | Pelvic schwannoma (6
cm) | Robotic | 240 | None | 2 | (8) |
| Takahashi (2016) | F | 68 | Yes | Obturator nerve
schwannoma (3 cm) | Laparoscopic | NS | Weakness of the
adductor muscle | NS | (6) |
| Tobias-Machado
(2017) | M | 60 | Yes | Prescral and
obturator fossa schwannoma | Laparoscopic | 150 | None | 2 | (2) |
| Ghosh (2011) | F | 26 | Yes | Pelvic
angiomatosis | Open | NS | None | NS | (11) |
| Yeung Jr
(2007) | F | 44 | Yes | Thigh abscess | Open | NS | None | NS | (16) |
| Uchida (2006) | M | 71 | Yes | Mucoid pseudocyst
of the obturator nerve | Open | NS | Impaired adduction
and partial loss of sensation at the inner thigh | NS | (15) |
| Tanaka (2006) | M | 29 | Yes | Nonseminomatous
germ cell tumor (10.5 cm) | Open | NS | None | NS | (5) |
| Kanta (2013) | F | 69 | Yes | Malignant
schwannoma of the obturator nerve (12 cm) | Open | NS | Minimal weakness of
adduction of the right thigh | NS | (1) |
| Park (2007) | F | 44 | Yes | Schwannoma | Laparoscopic | NS | None | NS | (7) |
| Perrin (2017) | M | 27 | Yes | Obturator
schwannoma | Robotic | NS | None | NS | (10) |
| Pachowicz
(2017) | M | 33 | Yes | Fibroblastic
osteosarcoma | Open | NS | None | NS | (17) |
| Sueishi (2016) | F | 21 | Yes | Desmoid-type
fibromatosis (8 cm) | Open | NS | Left lower limb
weakness and menstrual colic | NS | (18) |
| Present study | M | 53 | Yes | Solitary fibrous
tumor | Laparoscopic and
Open | 210 | Low intestinal
obstruction/weakness of the adductor muscle | 10 |
|
 | Table IV.Different types of tumors reported in
the previous studies included in Table
III. |
Table IV.
Different types of tumors reported in
the previous studies included in Table
III.
| Tumor type | N |
|---|
| Obturator nerve
schwannoma | 6 |
| Symptomatic
parasitic leiomyoma | 1 |
| Neurofibroma | 1 |
| Presacral
lipoma | 1 |
| Aggressive
angiomyxoma | 1 |
| Pelvic
angiomatosis | 1 |
| Thigh abscess | 1 |
| Mucoid pseudocyst
of the obturator nerve | 1 |
| Non-seminomatous
germ cell tumor | 1 |
| Solitary fibrous
tumor | 1 |
| Malignant
schwannoma of the obturator | 1 |
| Desmoid-type
fibromatosis | 1 |
| Fibroblastic
osteosarcoma | 1 |
Discussion
Laparoscopic surgery provides surgeons with a clear
and magnified view of the operative field (19). Therefore, it is useful for complex
surgical procedures, particularly in deep locations in the narrow
lateral pelvic space (4,14). It appears that only a limited number
of studies have explored surgical dissection of obturator masses
and these lacked systematic conclusions (2,5).
LLPTD, as a minimally invasive pelvic surgical
technique, has been applied in the clinical setting due its
feasibility and reduced associated blood loss (4). However, the effect of the limited space
must be taken into consideration. In the present case, occupation
of the obturator fossa by a large tumor made LLPTD more difficult.
The combined open approach with HA-LLPTD allows experienced LLPTD
surgeons to modify the tumor location and perform complete tumor
dissection without any complications (14).
This approach may be performed via surgical
cooperation and without the requirement for an assistant port
(1). LLPTD combined with an open
approach has been previously reported (14,20).
Surgeons must have a comprehensive anatomical understanding to use
this approach. The technique reported in the present study included
LLPTD combined with the open method for pelvic and inguinal
surgery, and it appears to be more useful for such cases as
compared with the conventional approach.
Obturator nerve injury is the most common surgical
complication reported in the literature (6,15). The
reasons are as follows: i) The combination of sharp and blunt
dissection of the tumor causes injury to the nerve, as it is
situated in close proximity to the tumor; ii) tumor tissue may be
dissected along with the obturator nerve, irrespective of whether
the nerve is infiltrated by the tumor; iii) pelvic lymph node
dissection may cause injury. It is noteworthy that caution should
be taken intraoperatively to protect the nerve against mechanical
and thermal injury; in addition, the treatment process should
include close observation of perioperative symptoms and signs,
postoperative follow-up and neurotrophic support (1,3).
Recent studies have reported on cases of SFT located
in the pelvic region (21,22). However, to the best of our knowledge,
SFTs spanning the obturator fossa with involvement of obturator
nerve have not been reported to date. SFTs may be misdiagnosed as
other tumor types occurring in this area, such as neurological
tumors. Furthermore, the assessment of malignancy should
incorporate the biological behavior of the tumor and not rely on
histopathological examination alone. Atypical SFTs may undergo
malignant transformation and recurrence (23). Therefore, a rigorous follow-up is
crucial for assessing the efficacy of surgical treatment.
Several types of tumor have been reported to be
located in the obturator fossa, the majority of which are benign,
mainly derived from neurological and mesenchymal tissues (7,12). In
particular, obturator nerve schwannoma is more commonly reported
compared with other types. The operative approach may be either
open or minimally invasive (1,6,7,9).
However, in recent years, robotic and laparoscopic surgery have
become mainstay surgical options (6,8). In the
present case, a combined approach was used to treat a
transobturator tumor, which appeared to be the optimal choice.
HA-LLPTD allows experienced laparoscopic surgeons to
safely perform complete resection of tumors located in the
obturator fossa with fewer complications. The combination of
laparoscopic and open surgery is an innovative method for the
excision of obturator foramen masses, which provides clinical
solutions for extracting tumors of the obturator region. Although
the short-term outcome appears to be favorable, due to the small
sample size, further investigations with larger sample sizes are
still required to assess and explore the long-term outcome of this
approach.
Acknowledgements
Not applicable.
Funding
This work was supported in part by the Dali Tong
Chongqing Science and Technology Bureau (Basic and Frontier
Research Project; grant no. cstc2018jcyjA2133) and the Chongqing
Municipal Health and Health Committee (Science and Health Joint
Medical Research Project; grant no. 2018QNXM041).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author upon reasonable
request.
Authors' contributions
DT acquired the data, performed the literature
review, performed the surgery and pre-operative administration, and
drafted, reviewed and edited the manuscript for intellectual
content. JJ contributed to the conceptualization, analysis of the
present study and revised the manuscript for important intellectual
content. JZ performed the surgery, contributed to data and image
analysis and manuscript editing. PZ made pathological staining and
recognize pathological diagnosis. HT took radiological images and
recognize radiological diagnosis. All authors have read and
approved the manuscript.
Ethics approval and consent to
participate
The present study was approved by the Research
Ethics Committee of Daping Hospital, Army Medical University. The
patient provided informed consent.
Patient consent for publication
Written informed consent was provided by the
patients for the publication of the study, including personal data
and images in all formats.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kanta M, Petera J, Ehler E, Prochazka E,
Lastovicka D, Habalova J, Valis M and Rehak S: Malignant schwannoma
of the obturator nerve. Bratisl Lek Listy. 114:584–586.
2013.PubMed/NCBI
|
|
2
|
Tobias-Machado M, Hidaka AK, Sato LLK,
Silva IN, Mattos PAL and Pompeo ACL: Laparoscopic resection of
prescral and obturator fossa schwannoma. Int Braz J Urol.
43:5662017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chao WT, Liu CH, Chen YJ, Wu HH, Chuang CM
and Wang PH: Neurofibroma involving obturator nerve mimicking an
adnexal mass: A rare case report and PRISMA-driven systematic
review. J Ovarian Res. 11:142018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Masubuchi S, Okuda J, Hamamoto H, Ishii M,
Osumi W, Yamamoto M, Inoue Y, Tanaka K and Uchiyama K: Totally
extraperitoneal approach to laparoscopic lateral lymph node
dissection for patients with recurrent lateral pelvic lymph nodes
after rectal cancer surgery: A novel technique-M TEP LLND. Surg
Today. 49:981–984. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tanaka T, Kitamura H, Masumori N,
Tsukamoto T and Kimura M: Retroperitoneal extragonadal germ cell
tumor presenting as a bulky pelvic mass of the obturator fossa. Int
J Urol. 13:180–182. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Takahashi H, Hara M, Tsuboi K, Sagawa H,
Ishiguro H, Matsuo Y and Takeyama H: Laparoscopically resected
obturator nerve schwannoma: A case report. Asian J Endosc Surg.
9:307–310. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Park NY, Chong GO and Lee YS: Laparoscopic
resection of schwannoma in the anomaly of obturator nerve. J
Laparoendosc Adv Surg Tech A. 17:769–773. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chopra S, Dharmaraja A, Satkunasivam R and
Gill IS: Robot-assisted laparoscopic resection of a pelvic
schwannoma. Urol Case Rep. 11:63–65. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gleason T, Le BH, Parthasarathy K and
Robinson-Bennett B: Obturator nerve schwannoma as a mimic of
ovarian malignancy. Case Rep Obstet Gynecol.
2017:97248272017.PubMed/NCBI
|
|
10
|
Perrin H, Brunner P, Ortega JC, Mercier B,
Clement N, Robino C and Chazal M: Robotic resection of an obturator
schwannoma with preservation of normal nerve fascicles and
function. J Robot Surg. 11:479–483. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ghosh SB, Mala YM, Tripathi R and Singh A:
Pelvic angiomatosis: An unusual cause of recurrent obstructed
labor: A case report and review of literature. Arch Gynecol Obstet.
283:127–129. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Menderes G, Nhundu B, Levy K and Silasi
DA: Robotic resection of a symptomatic parasitic leiomyoma from the
obturator fossa. J Minim Invasive Gynecol. 25:232018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Poskus E, Makunaite G, Kubiliute I and
Danys D: Case report: Laparoscopic approach in the treatment of
presacral lipoma. Ann Med Surg (Lond). 35:64–66. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kanao H, Aoki Y, Tanigawa T, Matoda M,
Okamoto S, Nomura H, Omatsu K, Kato K, Utsugi K and Takeshima N: En
bloc resection of an aggressive angiomyxoma by a novel combination
laparoscopic and open perineal approach. J Minim Invasive Gynecol.
26:598–599. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Uchida A, Horiguchi A, Ide H, Hatakeyama
N, Yoshimura I and Ogawa Y: Mucoid pseudocyst of the obturator
nerve. Int J Urol. 13:471–472. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yeung P Jr, Sokol A, Walton B and Iglesia
C: Thigh abscess mistaken for sarcoma following transobturator
tape: A case report and literature review. J Minim Invasive
Gynecol. 14:657–659. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Pachowicz M, Drelich-Zbroja A, Szumilo J,
Skwarcz S and Chrapko B: A mysterious tumor in the obturator
internus muscle-a case report. Nucl Med Rev Cent East Eur.
20:62–63. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sueishi T, Arizono T, Nishida K, Hamada T
and Inokuchi A: A case of spontaneous regression of recurrent
desmoid tumor originating from the internal obturator muscle after
delivery. World J Oncol. 7:75–80. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Goel M, Kurunkar SR, Kanetkar A and Patkar
S: Outcome of robot-assisted radical cholecystectomy in a
high-volume tertiary cancer center in India. J Laparoendosc Adv
Surg Tech Part B Videoscop. 29:vor.2018.0539. 2019.PubMed/NCBI
|
|
20
|
Blank JJ, Gibson EK, Peterson CY, Ridolfi
TJ and Ludwig KA: Retroileal anastomosis in hand-assisted
laparoscopic left colectomy: Experience at a single institution.
Surg Endosc. 34:3408–3413. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wang Y, Wei R, Ji T, Chen Z and Guo W:
Surgical treatment of primary solitary fibrous tumors involving the
pelvic ring. PLoS One. 13:e02075812018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Fernandez A, Conrad M, Gill RM, Choi WT,
Kumar V and Behr S: Solitary fibrous tumor in the abdomen and
pelvis: A case series with radiological findings and treatment
recommendations. Clin Imaging. 48:48–54. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Huang SC and Huang HY: Solitary fibrous
tumor: An evolving and unifying entity with unsettled issues.
Histol Histopathol. 34:313–334. 2019.PubMed/NCBI
|