Introduction
Breast cancer is one of the most common female
malignancies. Although the prognosis of breast cancer has improved
with early detection and advances in systemic treatment, 20–30% of
patients still experience distant metastasis. Patients with
advanced disease have a median survival of only ~2 years (1). As one of the most aggressive breast
malignancies, human epidermal growth factor receptor 2
(HER2)-positive breast cancer exhibits frequent recurrence and
metastasis during or after treatment (2). In advanced HER2-positive breast cancer,
chemotherapy combined with trastuzumab is currently widely used in
practice and is recognized as a valid approach for improving
patient survival (1). Although
chemotherapy is effective in most patients, some patients relapse
and develop resistance (3). Cancer
stem cells (CSCs) have numerous abilities, including a self-renewal
ability, an invasive ability and resistance ability to numerous
antitumor agents, including chemotherapy and targeted therapy, all
of which are thought to contribute to recurrence or metastasis and
to overall aggressiveness of the disease (4).
Chemotherapy can inhibit tumor growth and also leads
to hypoxia, which might induce an increase in the proportion of
CSCs. CSCs can survive by increasing the expression of
hypoxia-inducible factors (5).
Previous studies have demonstrated that following treatment of
breast cancer cells with chemotherapy, the surviving cells exhibit
enrichment in CSCs (6,7). Li et al (8) reported that
CD44+/CD24−/low breast cancer cells could
separate from primary breast cancer tissues after chemotherapy. In
addition, the proportion of stem cell subsets after chemotherapy
increased compared with that before chemotherapy, and the formation
of mammospheres was enhanced. Previous studies in breast cancer
mouse models also suggested that combining chemotherapy with drugs
targeting CSCs or metastatic progression could improve survival
(7,9).
Niclosamide is an anthelmintic agent that has been
approved by the Food and Drug Administration (FDA) and used in
humans for nearly 50 years (10).
Chen et al (11) identified
niclosamide (trade name, Niclocide) as a potentially effective
antitumor drug that could alter the hepatocellular carcinoma gene
expression pattern. The underlying mechanism of niclosamide has not
been well characterized, although it has been reported that it
could inhibit mitochondrial oxidative phosphorylation and stimulate
ATPase activity (12). Our previous
studies revealed that niclosamide exerts anticancer effects in
triple-negative and HER2-positive breast cancers by reversing
epithelial-mesenchymal transition (EMT) and inhibiting stem cell
phenotype (13,14). Furthermore, we previously
demonstrated that niclosamide monotherapy alone or combined with
cisplatin can significantly inhibit the Akt, ERK and Src signaling
pathways (13,14). Thus, the inhibitory effect of
niclosamide on tumor cells is well-documented, although the
mechanism has not yet been clarified.
The present study aimed to determine the inhibitory
effects of niclosamide on the growth, invasion and EMT of
chemoresistant HER2-positive breast cancer cells. The molecular
mechanisms of niclosamide-mediated inhibition of Bcl-2 and signal
transducer and activator of transcription 3 (STAT3) were also
investigated.
Materials and methods
Cell culture and cisplatin
treatment
The BT474 cell line, estrogen receptor (ER) and
HER2-positive breast cancer cell line, was purchased from the
American Type Culture Collection. Cells were cultured in RPMI-1640
medium (Gibco; Thermo Fisher Scientific, Inc.) supplemented with
10% FBS (Gibco; Thermo Fisher Scientific, Inc.) and 1%
penicillin/streptomycin in at 37°C in a humidified incubator
containing 5% CO2. Cisplatin and niclosamide were
purchased from Sigma-Aldrich (Merck KGaA). Cisplatin was prepared
in DMSO to obtain a stock solution of 200 mM at −20°C. Niclosamide
was prepared in DMSO to obtain a stock solution of 10 mM at −20°C.
BT474 cells were continuously treated with increasing
concentrations of cisplatin (5-20 µmol/l) for >6 months to
acquire a stable cisplatin-resistant cell line (13). Before each experiment, cisplatin was
removed from the media for at least 72 h.
Cell viability and combination index
(CI) analysis
Alamar Blue (resazurin solution), purchased from
Sigma-Aldrich; Merck KGaA, was used to assess cell viability as
previously described by Liu et al (13). The results are displayed as the ratio
of viable treated cells to viable 1% DMSO control treated cells.
CompuSyn software (version 1.0; ComboSyn) was utilized to calculate
the CI value for niclosamide and cisplatin. The fraction affected
value was calculated as the portion of cells inhibited after drug
exposure.
Apoptosis analysis
Cells were exposed to DMSO (1%) control, cisplatin
(20 µM) or niclosamide (1 µM) for 48 h. Cells in suspension (100
µl) were stained with 100 µl of Muse Annexin V & Dead Cell
reagent (Merck KGaA) according to the manufacturer's instructions
and incubated in the dark for 20 min at room temperature. The Muse
Cell Analyzer (Merck KGaA) was used to analyze fluorescence.
Western blotting
After cisplatin resistant BT474 cells were treated
with 1% DMSO (control), 1 µM niclosamide or 1 µM niclosamide
combined with 20 µM cisplatin for 48 h, proteins were extracted
using RIPA buffer (cat. no. 89900, Thermo Fisher Scientific, Inc.).
The bicinchoninic acid assay was used to measure the protein
concentration. Total proteins (20 µg/lane) were separated by
SDS-PAGE on a 10% gel. The separated proteins were transferred onto
PVDF membranes and blocked with 5% fat-free milk in TBST buffer
(0.1% Tween-20) for 2 h at room temperature. The membranes were
incubated with primary antibodies (diluted at 1:1,000, except for
GAPDH, which was diluted at 1:10,000) overnight at 4°C. Antibodies
against E-cadherin (cat. no. 3195), N-cadherin (cat. no. 13116),
vimentin (cat. no. 3390), Bcl-2 (cat. no. 4223), phosphorylated
(p)-STAT3 (Tyr705) (cat. no. 9145), STAT3 (cat. no. 30835) and
GAPDH (cat. no. 8884) were purchased from Cell Signaling
Technology, Inc. The membranes were washed three times with TBST
(TBS with 0.05% Tween-20), and subsequently incubated with
anti-rabbit HRP-conjugated IgG (cat. no. 7074) or anti-mouse
HRP-conjugated IgG (cat. no. 7076) secondary antibodies (both
diluted at 1:5,000; Cell Signaling Technology, Inc.) at room
temperature for 1 h and re-washed. The immunoreactive signals were
visualized using a peroxide solution with an
electrochemiluminescent HRP substrate and luminol reagent (Merck
Millipore; cat. no. WBKLS0500). Data were analyzed using ImageJ
software (version 1.52v, National Institutes of Health) and
normalized to GAPDH.
Mammosphere formation assay
A total of 3,000 cells/ml were plated in
ultralow-attachment plates (Corning). The medium contained
serum-free DMEM/F12 supplemented with 20 ng/ml human recombinant
epidermal growth factor (Invitrogen; Thermo Fisher Scientific,
Inc.), 10 ng/ml basic fibroblast growth factor (Invitrogen; Thermo
Fisher Scientific, Inc.) and 1X B27 supplement (Gibco; Thermo
Fisher Scientific, Inc.). The mammosphere formation assay procedure
was performed as previously described (14). Mammosphere-forming efficiency (MFE)
was calculated as the mammosphere number (diameter ≥50 µm) divided
by the number of seeded cells.
Cell invasion assay
The cell invasion assay was conducted using
Matrigel®-coated invasion chambers (BD Biosciences). A
total of 5×104 cells in 0.5 ml serum-free medium were
seeded into the top chambers of the transwell. Medium containing
10% FBS medium was then added to the bottom chamber. After 12 h
incubation, cells in the top chambers were wiped whereas cells on
the bottom of the chamber were fixed with 10% neutral formalin at
room temperature for 30 min and stained with 1% crystal violet at
room temperature for 30 min. The stained cells were observed under
a microscope (Zeiss GmbH) with a 10X objective lens in five random
regions per sample. Results were presented as the average cell
number across fields of view.
Tumor xenograft model
Xenograft experiments were approved by the Tongji
University School of Medicine Committee for the Use and Care of
Animals and performed in strict accordance with institutional
requirements. A total of 5×106 BT474-resistant cells in
100 µl Matrigel (BD Biosciences) mixed with 100 µl RPMI-1640 medium
were subcutaneously injected into 12 four-six-week-old female
BALB/c nude mice (Slaccas Laboratory Animal; Shanghai, China). Nude
mice were housed in a temperature-controlled (24-25°C and 50%
humidity) pathogen-free environment with a 12:12 h light:dark
cycle. After 14 days, tumor-bearing mice with tumor volumes between
50 and 100 mm3 were evenly divided into four groups
according to tumor size. Each group contained 3 mice, which were
injected intraperitoneally from day 14 to day 56 with one of the
following treatments: i) Vehicle; ii) cisplatin; iii) niclosamide;
or iv) niclosamide with cisplatin. The dosage of niclosamide was 20
mg/kg/day five days a week, and the dosage of cisplatin was 2
mg/kg/week. The mice were sacrificed on day 56 by cervical
dislocation. Tumor size was measured every seven days and tumor
volume was calculated after collection using the following formula:
Volume = length × width2 / 2.
Immunohistochemistry
The immunohistochemistry procedure has been
described by Liu et al (13).
Antibodies against Ki67 (1:100; cat. no. ab15580), HER2 (1:2,000;
cat. no. ab237715) and Bcl-2 (1:250; cat. no. ab32124) were
purchased from Abcam. The primary antibody incubation step was
skipped in one group as a negative control. Images were acquired
using a microscope (magnification, ×40; Zeiss GmbH).
Statistical analysis
Statistical analysis was performed using SPSS
software (version 19; IBM Corp.) or GraphPad Prism (version 5;
GraphPad Software Inc.). Cell viability, apoptosis, western
blotting, mammosphere formation and cell invasion assays were
performed in triplicate. Data are presented as the mean ± standard
deviation (SD). Statistical significance was analyzed by two-way
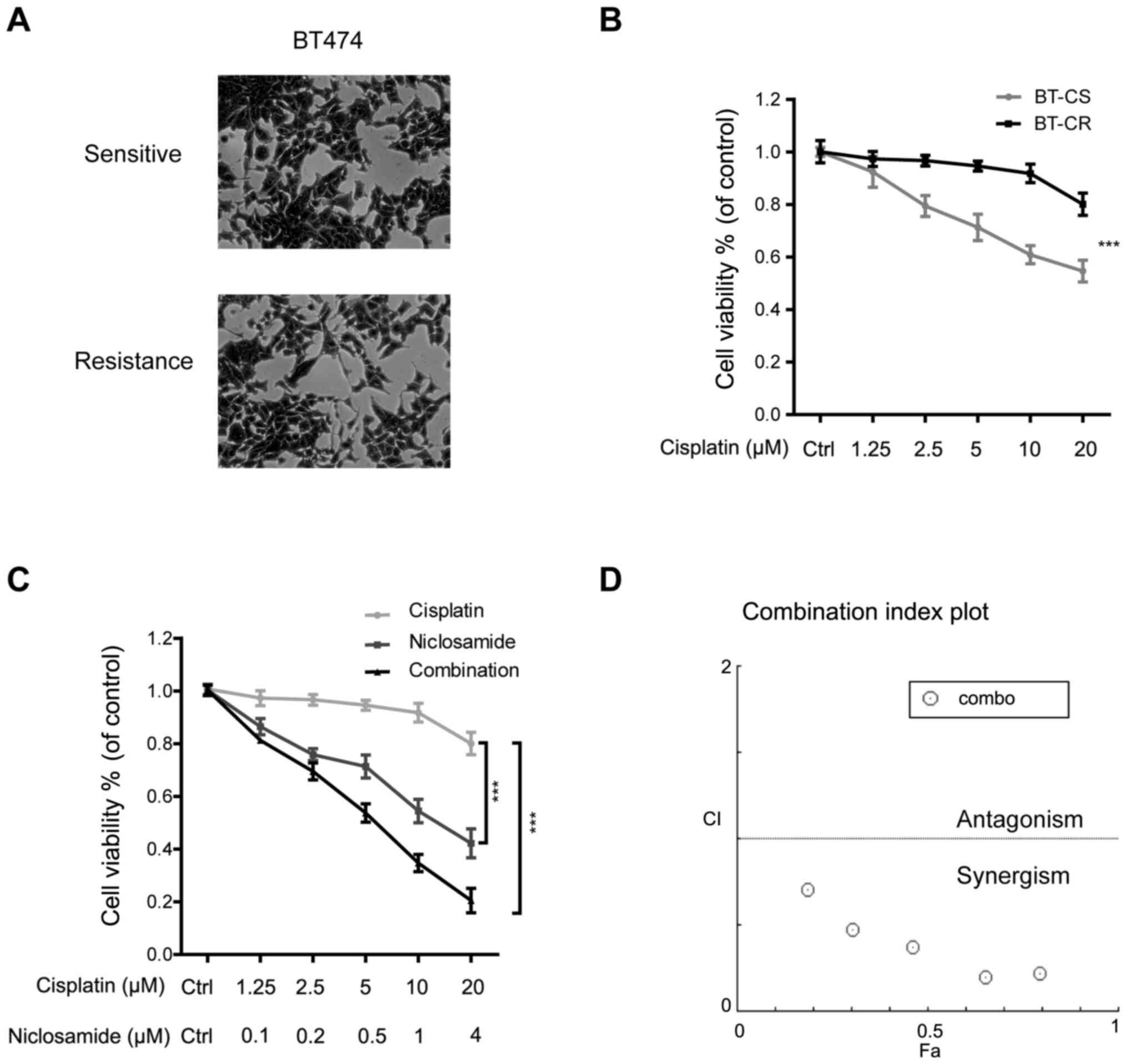
ANOVA followed by Tukey's post hoc test (Fig. 1) or one-way ANOVA followed by Tukey's
post hoc test (Figs. 2–5). Data from the in vivo study were
analyzed using mixed two-way ANOVA method regarding time as a
repeated measure and Tukey's post hoc test. P<0.05 was
considered to indicate a statistically significant difference.
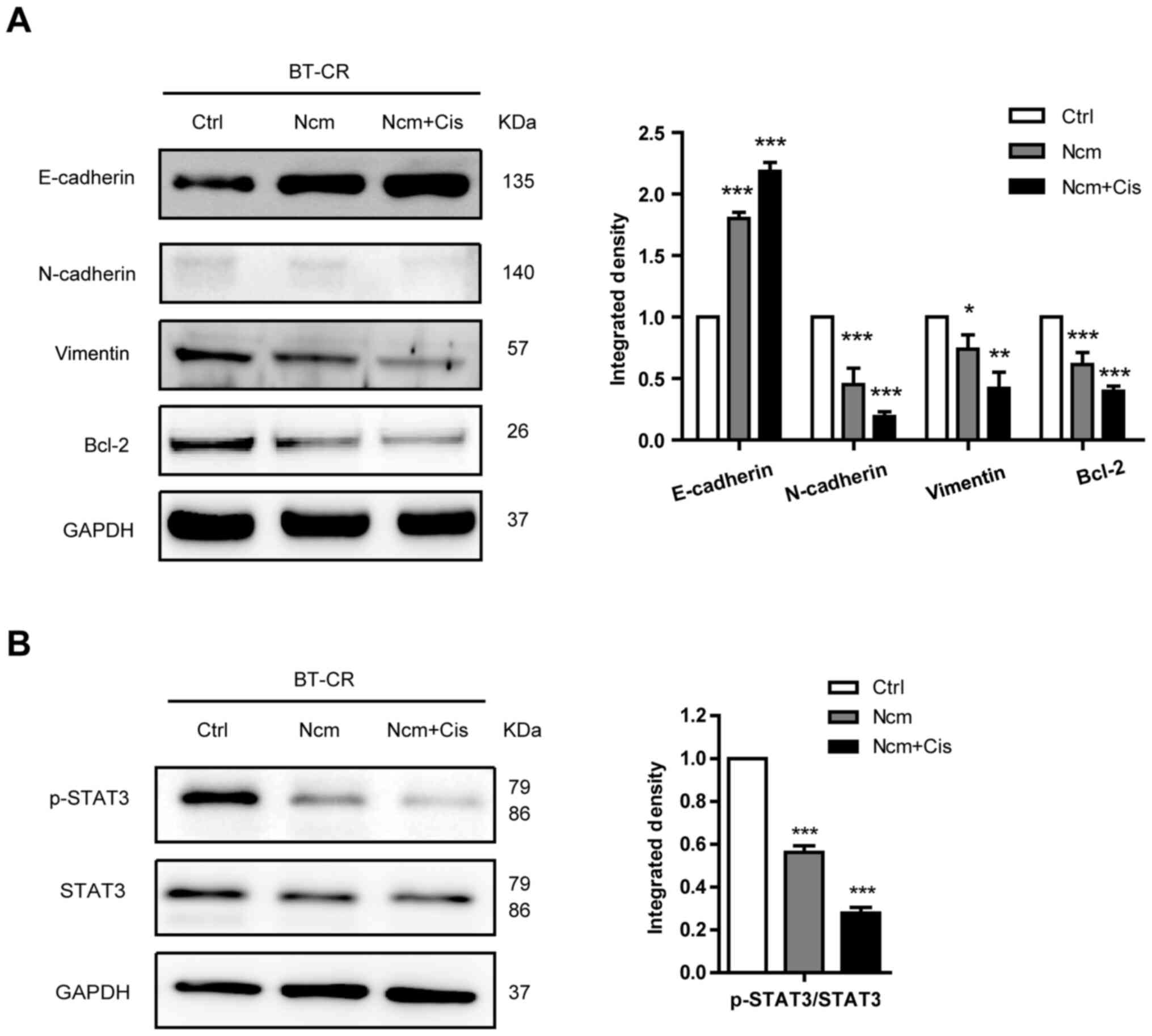
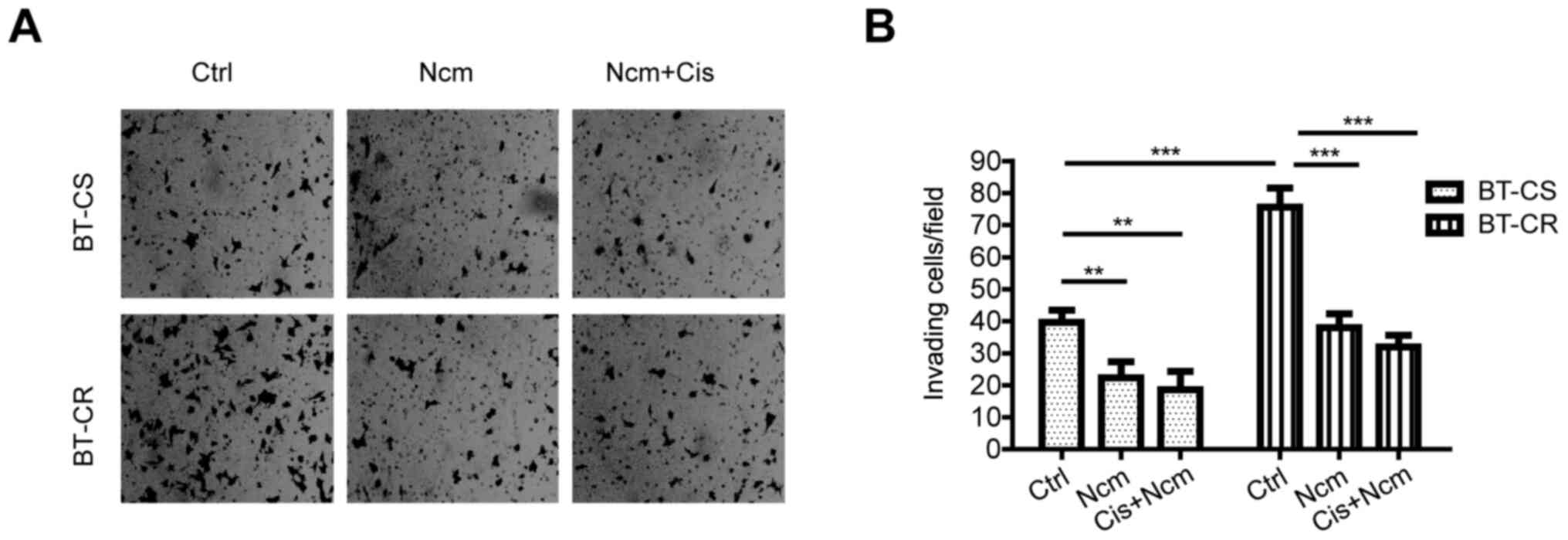
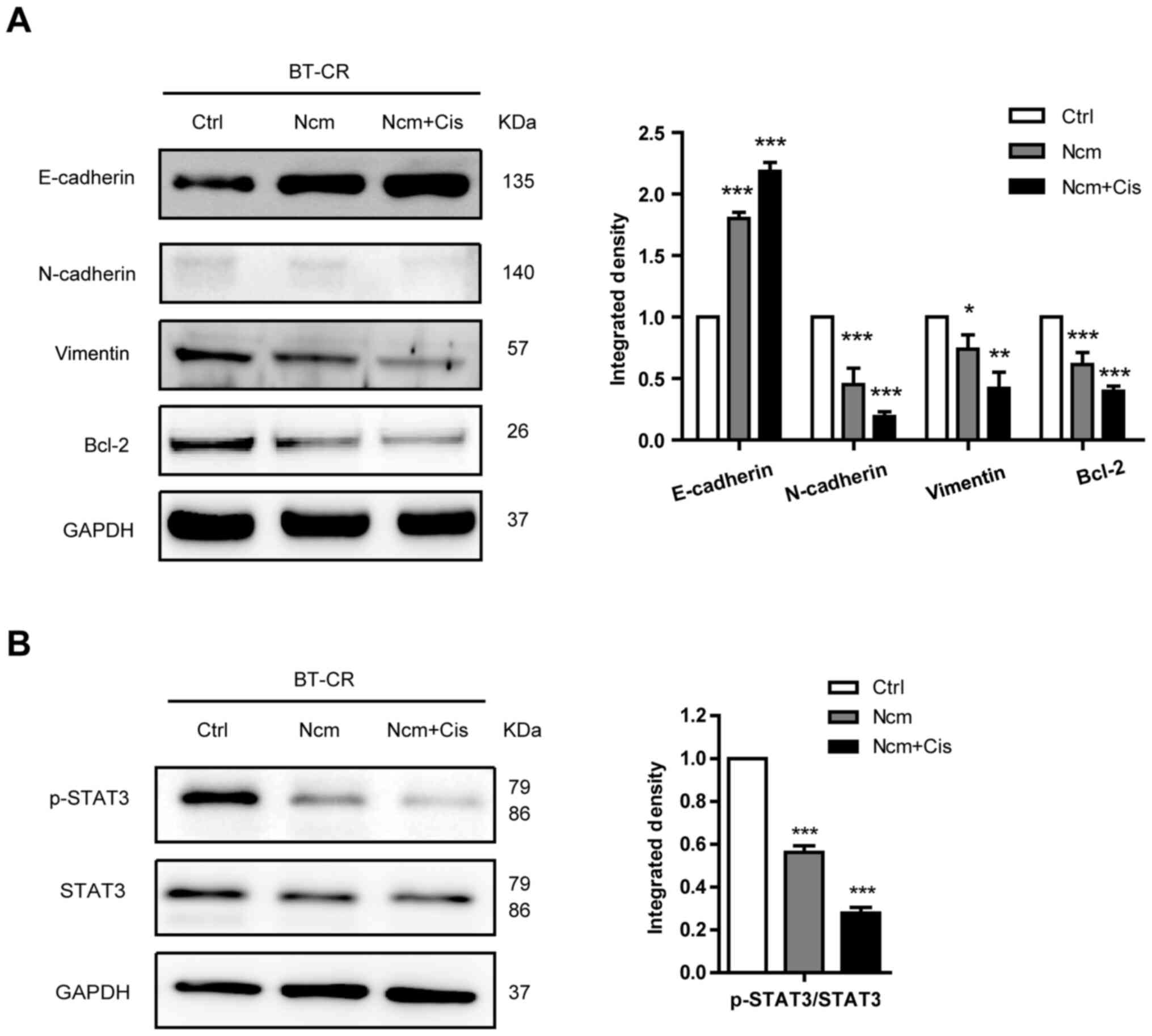 | Figure 5.Niclosamide and cisplatin suppress
EMT and inhibit the Stat3 signaling pathway. (A) Expression of
E-cadherin, N-cadherin, vimentin and Bcl-2 evaluated by western
blotting in lysates of BT-CR cells treated with DMSO (control), 1
µM niclosamide or 1 µM niclosamide combined with 20 µM cisplatin
for 48 h. Histogram represents the density values of each protein.
(B) Expression of p-STAT3 (Tyr705) and STAT 3 evaluated by western
blotting in lysates of BT-CR cells treated with DMSO (control), 1
µM niclosamide or the combination of 1 µM niclosamide and 20 µM
cisplatin for 48 h. Histogram represents the integrated density
values of p-STAT3/STAT3 ratio. *P<0.05; **P<0.01;
***P<0.001. BT-CS, cisplatin sensitive BT474 cells; BT-CR,
cisplatin resistant BT474 cells; Ctrl, control; Cis, cisplatin;
Ncm, niclosamide; EMT, epithelial-mesenchymal transition; p,
phosphorylated; STAT3, signal transducer and activator of
transcription 3. |
Results
Niclosamide combined with cisplatin
reverses cisplatin resistance
BT474 cells, which were originally isolated from a
case of HER2-positive breast cancer, were cultured with increasing
concentrations of cisplatin (5-20 µM) for >6 months. As
presented in Fig. 1A, cisplatin
resistant BT474 cells (BT-CR) had a morphology similar to that of
cisplatin sensitive BT474 cells (BT-CS) but had more membrane
protrusions than BT-CS cells. To verify the difference in cisplatin
sensitivity between BT-CS and BT-CR cells, Alamar Blue assay was
performed on cells following treatment with different cisplatin
concentrations (0, 1.25, 2.5, 5, 10 and 20 µM) for 48 h. The
results demonstrated that cisplatin cytotoxicity was significantly
inhibited in BT-CR cells compared with the sensitive parental cell
line BT-CS (Fig. 1B;
P<0.001).
BT-CR cells were treated with the indicated
concentrations of cisplatin and niclosamide or a combination of
these two drugs (combination group) for 48 h (Fig. 1C). The results demonstrated that both
niclosamide and the combination treatment decreased the viability
of BT-CR cells (P<0.001). To determine whether the antitumor
effect of niclosamide combined with cisplatin was synergistic,
additive or antagonistic, the CI was calculated using CompuSyn
software. The median inhibitory concentration of cisplatin in BT-CR
cells was 169.5 µM, whereas the median inhibitory concentration of
niclosamide was 2.4 µM. The CI value of combination treatment with
niclosamide and cisplatin was <1 µM, indicating that niclosamide
and cisplatin exerted a synergistic effect on the resistant cells
BT-CR (Fig. 1D).
Niclosamide and cisplatin induce
resistant cell apoptosis
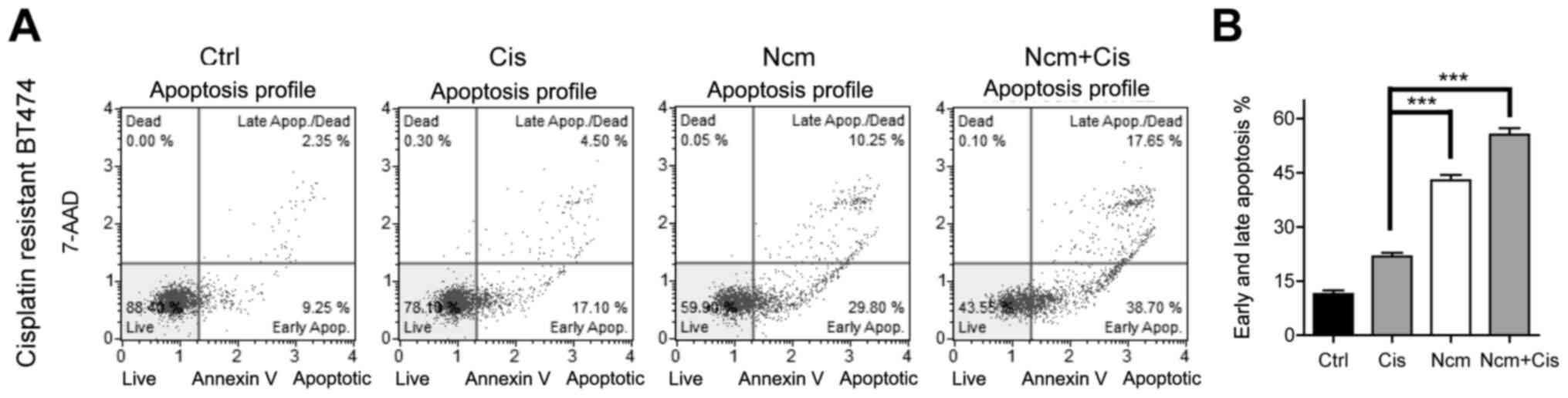
The apoptosis of BT-CR cells treated with cisplatin
(20 µM) and niclosamide (1 µM) was evaluated. The niclosamide
concentration was selected according to previous research (11). Since the serum concentration of
niclosamide is 0.25–6.0 µg/ml (corresponding to 0.76–18.35 µM), the
concentration of 1 µM chosen was within the serum concentration
range (7). Annexin V/7-AAD staining
was detected by flow cytometry. Niclosamide (1 µM) treatment for 48
h increased the apoptosis rate compared with that of 20 µM
cisplatin treatment in resistant BT474 cells (Fig. 2A). Furthermore, niclosamide combined
with cisplatin significantly increased the apoptosis rate,
suggesting that niclosamide alone or combined with cisplatin
increased cytotoxicity by inducing apoptosis. The histogram
represents the percentage of early and late apoptotic cells
detected by flow cytometry (Fig.
2B).
Niclosamide and cisplatin inhibit the
stem-like phenotype in resistant cells
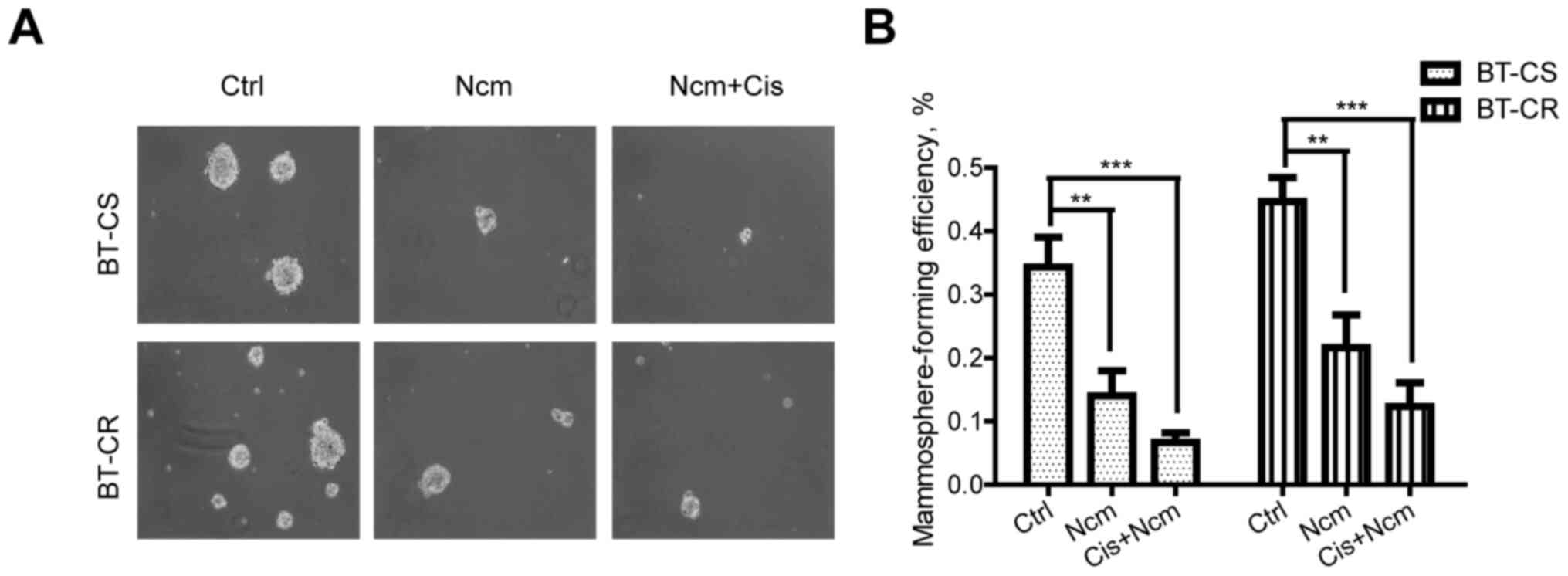
The mammosphere assay was used to assess the cell
stem-like phenotype of BT-CS and BT-CR cells. As presented in
Fig. 3, a prominent decrease in the
number and diameter of spheres treated with niclosamide was
noticed, either alone or combined with cisplatin, in the BT-CS and
BT-CR cell lines. Exposure to niclosamide (P<0.01) or combined
with cisplatin (P<0.001) significantly decreased the MFE of both
BT-CS and BT-CR cells. This result indicated that niclosamide alone
or combined with cisplatin could effectively decrease the cell
ability to form mammospheres.
Niclosamide and cisplatin inhibit cell
invasion ability
Because niclosamide combined with cisplatin was
found to induce apoptosis and significantly decrease the MFE,
subsequent experiments were carried out to investigate whether cell
invasion was also inhibited by niclosamide or combination
treatment. Transwell invasion assays were performed to determine
the invasive ability of BT-CS and BT-CR cells. The results
demonstrated that BT-CR cells had a higher invasive ability
compared with BT-CS cells. Furthermore, niclosamide alone and
combined with cisplatin significantly attenuated the invasive
ability of BT-CS and BT-CR cells (Fig.
4).
Niclosamide and cisplatin suppress EMT
and inhibit the STAT3 signaling pathway
Previous studies demonstrated that EMT is a possible
mechanism of cell metastasis (15,16).
Niclosamide treatment may also suppress EMT in resistant
HER2-positive breast cancer cells. To test this hypothesis,
epithelial (E-cadherin) and mesenchymal (N-cadherin and vimentin)
markers were detected by western blotting. As presented in Fig. 5A, E-cadherin expression significantly
increased whereas N-cadherin and vimentin expression significantly
decreased in cells treated with niclosamide alone or combined with
cisplatin compared with the control group. Moreover, treatment with
niclosamide alone or combined with cisplatin decreased the
expression level of the antiapoptotic protein Bcl-2 (Fig. 5A). The phosphorylation level (Tyr705)
of STAT3 was analyzed by western blotting and the results
demonstrated that p-STAT3 levels significantly decreased following
niclosamide treatment (Fig. 5B).
These findings suggested that niclosamide may inactivate STAT3 to
downregulate the expression of Bcl-2 and increase the cisplatin
sensitivity of HER2-positive cells.
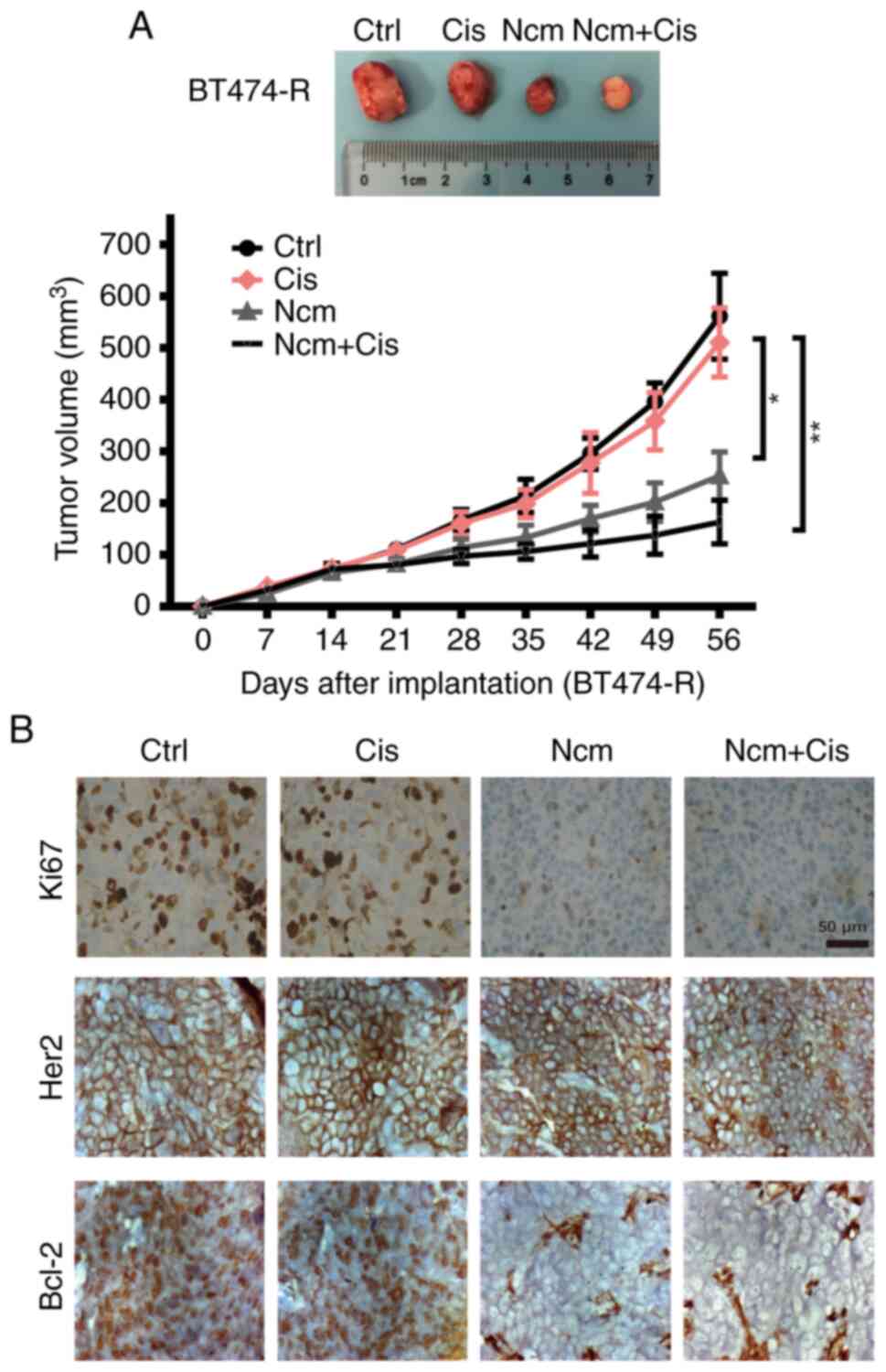
Antitumor efficacy of niclosamide in
vivo
To verify the inhibitory effect of niclosamide in
vivo, xenografts generated from BT474-resistant cells were
treated as described in the Materials and methods. As presented in
Fig. 6A, niclosamide alone and
combined with cisplatin significantly inhibited the growth of
xenograft tumors derived from resistant cells compared with
cisplatin alone (P<0.05). There was no significant difference
between the niclosamide group and the combination treatment group.
Tumor tissues were stained for Ki67, HER2 and Bcl-2 by
immunohistochemistry. As shown in Fig.
6B, both niclosamide and combination therapy inhibited Ki67 and
Bcl-2 expression. Taken together, these findings demonstrated that
niclosamide may inhibit cisplatin-resistant BT474 tumor growth
in vivo.
Discussion
The present study demonstrated that niclosamide, an
FDA-approved anthelmintic agent, might also be considered as a
potential chemotherapeutic agent for HER2-positive chemoresistant
breast cancer. The results demonstrated that niclosamide induced
apoptosis and was more effective when combined with cisplatin.
Furthermore, niclosamide overcame chemotherapy resistance in
HER2-positive cells via Bcl-2 inhibition and STAT3 activation.
These results suggested that niclosamide might be considered as a
potential antitumor drug and used in combination with chemotherapy
in the treatment of HER2-positive breast cancer. A recent study
reported that niclosamide, a potent radiosensitizer, acts by
inhibiting STAT3 and Bcl-2 and by increasing the production of
reactive oxygen species (ROS) in triple-negative breast cancer
(17). Another study demonstrated
that niclosamide inhibits the growth of melanoma cell lines (A375
and B16-F10) and induces mitochondrial apoptosis, which impairs
cell migration and invasion, reduces expression of phosphorylated
STAT3 at Tyr705 and inhibits matrix metalloproteinase-2 and −9
expression (18). Conversely, the
present study demonstrated that the anthelmintic agent niclosamide
may be repurposed to treat chemoresistant HER2-positive breast
cancer. To the best our knowledge, the present study was the first
to suggest that niclosamide could be used for the treatment of
chemoresistant HER2-positive breast cancer.
Niclosamide is administered orally in parasitic
patients but is only partially absorbed through the
gastrointestinal tract. In anthelmintic therapy, niclosamide is
administered orally in adults at a single dose of 2 g. Due to
differences in individual absorption rates, the maximum serum
concentration of niclosamide in humans is 0.25–6.0 µg/ml
(corresponding to 0.76–18.35 µM), which is well within the
concentration range of its anticancer activity and within the
concentration range we previously observed for the treatment of
chemoresistance in HER2-positive breast cancer (10). In addition, in rodent xenograft
models, oral administration of niclosamide has been shown to lead
to an accumulation of the drug in tumor tissue at concentrations
even higher than those in plasma (19). However, additional stage I–III
randomized clinical trials are needed to demonstrate the antitumor
effect of niclosamide before it could be approved for any cancer
treatment.
Niclosamide is increasingly studied in cancer
research and has been demonstrated to effectively inhibit a variety
of cancer-related signaling pathways. A previous study suggested
that niclosamide could inhibit PI3K/Akt, Wnt/β-catenin signaling
and β-catenin/T-cell factor complex formation, and promote
degradation of the Wnt co-receptor low-density lipoprotein
receptor-related protein 6 (20).
Jak-STAT and NF-κB signaling have also been identified as potential
targets of niclosamide in lung cancer and multiple myeloma
(21). Furthermore, niclosamide has
been shown to enhance the efficacy of programmed cell death
1/programmed cell death ligand 1 immune checkpoint blockade and
cisplatin cytotoxicity in non-small cell lung cancer models
(22). Furthermore, Snail family
transcriptional repressor 1 is known as a transcriptional repressor
of cadherin-1, which encodes E-cadherin. Downregulation of
E-cadherin is vital to the migration and invasion of cancer cells.
This process might facilitate breast cancer metastasis (23,24).
Previous studies have demonstrated that CSCs forming tumor spheres
in vitro are more likely to develop tumors in vivo
and to become resistant to standard radiation or chemotherapy than
differentiated cells (25,26). This, along with our previous studies
(13,14), indicates that niclosamide can inhibit
EMT in both lapatinib-resistant and chemoresistant breast cancer.
In addition, niclosamide alone or in combination with cisplatin
successfully decreased MFE in the present study, indicating that
niclosamide may be used as an effective anticancer agent by
inhibiting EMT and the breast cancer stem-like phenotype.
Cellular metabolic reprogramming is one of the
hallmarks of tumor cells, and Dr Otto Warburg reported that tumor
cells convert glucose to lactate to support cell growth, even in a
normoxic state. This aerobic glycolysis is known as the ‘Warburg
effect’ (27). In normal cells,
almost all pyruvate produced by glycolysis enters the mitochondria
for oxidative phosphorylation, maximizing the energy extraction
from glucose, whereas in cancer cells, only ~5% of pyruvate enters
the mitochondria (28). Aerobic
glycolysis in cancer cells is accompanied by elevated glucose
uptake, and only a small fraction of glucose is used for oxidative
phosphorylation (27). This explains
the energy deficit of cancer cells. Niclosamide is an anthelmintic
drug with mitochondrial uncoupling function (29). Previous studies have demonstrated
that mitochondrial uncoupling increases the pyruvate influx into
mitochondria, upregulates mitochondrial oxidation, reduces lactate
production and decreases the biosynthetic pentose phosphate
pathway, implying that mitochondrial uncoupling may be considered
as an effective way to antagonize aerobic glycolysis and that
mitochondrial uncoupling agents could potentially be developed for
the treatment of malignancies (29,30).
Niclosamide has been shown to be associated with glycolysis and
glucose uptake regulation, setting tumor cells at rest. Park et
al (31) and Khanim et al
(32) confirmed that niclosamide
could induce mitochondrial disintegration and induce the production
of mitochondrial superoxide, leading to mitochondrial damage. In
the present study, niclosamide induced apoptosis in chemoresistant
cells by downregulating Bcl-2, which was consistent with previous
studies (33,34).
Numerous malignant tumors express activated STAT3
and are resistant to apoptosis induction and chemotherapy (35). A previous study reported that STAT3
may be a key downstream mediator of HER2 signaling (36). Duru et al (37) showed that HER2-STAT3 crosstalk
increases aggressiveness and radioresistance in breast CSCs. HER2
also promotes radioresistance in HER2-positive breast cancer
through STAT3-survivin regulation (38). Chung et al (39) reported that in HER2-overexpressing
breast cancer, STAT3 activation promotes CSC characteristics of
which phenotype is associated with tumor drug resistance. In
addition, Li et al (40)
reported that trastuzumab resistance is regulated by
STAT3-dependent feedback activation in HER2-positive breast cancer
and gastric cancer. STAT3 activation is therefore a critical
pathway for the survival of drug-resistant tumors in HER2-positive
breast cancer. A proportion of STAT3 protein is localized in the
mitochondria. STAT3 functions as a promoter of the mitochondrial
electron transport chain in the mitochondria (41), decreases mitochondrial ROS production
and inhibits apoptosis (42).
Conversely, a lack of STAT3 decreases ATP levels and increases ROS
production in tumor cells (43).
Niclosamide has been reported to be a potent STAT3 suppressor that
inhibits STAT3 phosphorylation at Tyr705 (44). The inhibitory effect of niclosamide
on STAT3 phosphorylation also influences other pathways, including
the Wnt/β-catenin pathway, which is relevant to cancer initiation
and progression (45). Previously,
we reported that niclosamide induces growth inhibition and
apoptosis in MDA-MB-231 cisplatin-resistant cells (ER-negative) and
suppresses tumor invasion and stem-like phenotype, suggesting that
niclosamide might function through the Akt, ERK and Src pathways
(13). In the present study,
niclosamide induced growth inhibition and apoptosis in ER and
HER2-positive cells.
Cisplatin is a chemotherapeutic agent that has not
been routinely used in breast cancer; however, an increasing number
of studies have reported favorable responses in subgroups of breast
cancer (46–48). The National Comprehensive Cancer
Network have listed platinum-based agents, such as cisplatin and
carboplatin, as the preferred treatment for patients with
triple-negative recurrent/stage IV breast cancer who carry the
germline BRCA1/2 mutation (49).
Cisplatin is a DNA-damaging drug. Based on clinical trials,
cisplatin has become the backbone drug for the treatment of primary
breast cancer, as well as brain metastases (50). The combination of cisplatin,
bevacizumab and etoposide was used in a phase 2 trial in eight
patients with breast cancer and brain metastasis in Taiwan, and the
treatment was effective in five patients (46). In a previous study on neoadjuvant
therapy, the paclitaxel plus cisplatin (PC) regimen combined with
trastuzumab was shown to have a high pathological complete response
rate in HER2-positive breast cancer (47). In addition, the results from TBCRC009
clinical trial demonstrated that patients with metastatic
triple-negative breast cancer receiving cisplatin every 3 weeks had
numerically higher objective response rates than those receiving
carboplatin (48). Our present study
creates the possibility for future clinical trials targeting DNA
damage-resistant tumors with niclosamide in the treatment of
HER2-positive breast cancer. The combination of these two classes
of drug may therefore be considered as a novel option to treat
cancer.
In the present study, the sample size of each group
in the in vivo experiment was relatively small. When the
experiment was conducted, cells were injected into nude mice for 14
days and tumor-bearing mice with tumor volumes of 50–100
mm3 were evenly divided into four groups according to
tumor size. Before treatment, the mean tumor volume in each group
was consistent and not significantly different. We also controlled
factors (mice weight, age, the mean tumor volume and housing
conditions) other than the intervention that were perfectly
balanced across the groups. The four groups of xenograft tumors
showed different growth rates after treatment, which may reflect
the antitumor effect of niclosamide in vivo. However, the
small sample size remains a limitation of this research.
Furthermore, there was no significant difference between the
niclosamide group and the combination group. However, there was a
trend of higher antitumor effect in the combination group. To
determine whether the effect of combination treatment is greater
than that of niclosamide alone, clinical trials need to be
conducted in cisplatin-resistant patients.
The development and clinical application of oncology
drugs is a long and expensive process. New drugs applied in
practice account for a very small portion of investigated drugs.
Niclosamide is already available in the clinic, and the side
effects and other data related to its clinical use are already
documented.
In conclusion, the present study offered new ideas
for the treatment of chemoresistant HER2-positive breast cancer.
The results from this study were in accordance with existing
results showing that niclosamide can inhibit EMT and STAT3
phosphorylation, leading to cytotoxicity against chemoresistant
cells and breast CSCs. Niclosamide combined with cisplatin may be
considered as a novel treatment therapy for chemoresistant
HER2-positive breast cancer.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Fundamental
Research Funds for the Central Universities (grant no.
22120180601).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author upon reasonable
request.
Authors' contributions
JL and JH contributed to the design of the study.
HD, HQ and JL performed the experiments. HD and JL analyzed the
data. JL drafted the initial manuscript. JL and HD confirmed the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
Animal experiments were approved by the Tongji
University School of Medicine Committee for the Use and Care of
Animals (Shanghai, China; approval no. 11115043) and performed in
strict accordance with institutional requirements.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kennecke H, Yerushalmi R, Woods R, Cheang
MC, Voduc D, Speers CH, Nielsen TO and Gelmon K: Metastatic
behavior of breast cancer subtypes. J Clin Oncol. 28:3271–3277.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Camejo N, Castillo C, Alonso R, Correa F,
Rivero E, Mezquita C, Rosich A, Dellacasa F, Silveira L and Delgado
L: Effectiveness of Trastuzumab for Human Epidermal Growth Factor
Receptor 2-Positive Breast Cancer in a Real-Life Setting: One
Decade of Experience Under National Treatment Coverage Regulations.
JCO Glob Oncol. 6:217–223. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Diaby V, Tawk R, Sanogo V, Xiao H and
Montero AJ: A review of systematic reviews of the
cost-effectiveness of hormone therapy, chemotherapy, and targeted
therapy for breast cancer. Breast Cancer Res Treat. 151:27–40.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Geng SQ, Alexandrou AT and Li JJ: Breast
cancer stem cells: Multiple capacities in tumor metastasis. Cancer
Lett. 349:1–7. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Semenza GL: Targeting HIF-1 for cancer
therapy. Nat Rev Cancer. 3:721–732. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dean M, Fojo T and Bates S: Tumour stem
cells and drug resistance. Nat Rev Cancer. 5:275–284. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Samanta D, Gilkes DM, Chaturvedi P, Xiang
L and Semenza GL: Hypoxia-inducible factors are required for
chemotherapy resistance of breast cancer stem cells. Proc Natl Acad
Sci USA. 111:E5429–E5438. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Li X, Lewis MT, Huang J, Gutierrez C,
Osborne CK, Wu MF, Hilsenbeck SG, Pavlick A, Zhang X, Chamness GC,
et al: Intrinsic resistance of tumorigenic breast cancer cells to
chemotherapy. J Natl Cancer Inst. 100:672–679. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gao J, Liu J, Xie F, Lu Y, Yin C and Shen
X: Co-Delivery of Docetaxel and Salinomycin to Target Both Breast
Cancer Cells and Stem Cells by PLGA/TPGS Nanoparticles. Int J
Nanomedicine. 14:9199–9216. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Andrews P, Thyssen J and Lorke D: The
biology and toxicology of molluscicides, Bayluscide. Pharmacol
Ther. 19:245–295. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chen B, Wei W, Ma L, Yang B, Gill RM, Chua
MS, Butte AJ and So S: Computational Discovery of Niclosamide
Ethanolamine, a Repurposed Drug Candidate That Reduces Growth of
Hepatocellular Carcinoma Cells In Vitro and in Mice by Inhibiting
Cell Division Cycle 37 Signaling. Gastroenterology. 152:2022–2036.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Al-Hadiya BM: Niclosamide: Comprehensive
profile. Profiles Drug Subst Excip Relat Methodol. 32:67–96. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Liu J, Chen X, Ward T, Pegram M and Shen
K: Combined niclosamide with cisplatin inhibits
epithelial-mesenchymal transition and tumor growth in
cisplatin-resistant triple-negative breast cancer. Tumour Biol.
37:9825–9835. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Liu J, Chen X, Ward T, Mao Y, Bockhorn J,
Liu X, Wang G, Pegram M and Shen K: Niclosamide inhibits
epithelial-mesenchymal transition and tumor growth in
lapatinib-resistant human epidermal growth factor receptor
2-positive breast cancer. Int J Biochem Cell Biol. 71:12–23. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Taliaferro-Smith L, Oberlick E, Liu T,
McGlothen T, Alcaide T, Tobin R, Donnelly S, Commander R, Kline E,
Nagaraju GP, et al: FAK activation is required for IGF1R-mediated
regulation of EMT, migration, and invasion in mesenchymal triple
negative breast cancer cells. Oncotarget. 6:4757–4772. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Schieber MS and Chandel NS: ROS links
glucose metabolism to breast cancer stem cell and EMT phenotype.
Cancer Cell. 23:265–267. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lu L, Dong J, Wang L, Xia Q, Zhang D, Kim
H, Yin T, Fan S and Shen Q: Activation of STAT3 and Bcl-2 and
reduction of reactive oxygen species (ROS) promote radioresistance
in breast cancer and overcome of radioresistance with niclosamide.
Oncogene. 37:5292–5304. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhu Y, Zuo W, Chen L, Bian S, Jing J, Gan
C, Wu X, Liu H, Su X, Hu W, et al: Repurposing of the
anti-helminthic drug niclosamide to treat melanoma and pulmonary
metastasis via the STAT3 signaling pathway. Biochem Pharmacol.
169:1136102019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Osada T, Chen M, Yang XY, Spasojevic I,
Vandeusen JB, Hsu D, Clary BM, Clay TM, Chen W, Morse MA, et al:
Antihelminth compound niclosamide downregulates Wnt signaling and
elicits antitumor responses in tumors with activating APC
mutations. Cancer Res. 71:4172–4182. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Londoño-Joshi AI, Arend RC, Aristizabal L,
Lu W, Samant RS, Metge BJ, Hidalgo B, Grizzle WE, Conner M,
Forero-Torres A, et al: Effect of niclosamide on basal-like breast
cancers. Mol Cancer Ther. 13:800–811. 2014. View Article : Google Scholar
|
|
21
|
You S, Li R, Park D, Xie M, Sica GL, Cao
Y, Xiao ZQ and Deng X: Disruption of STAT3 by niclosamide reverses
radioresistance of human lung cancer. Mol Cancer Ther. 13:606–616.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Luo F, Luo M, Rong QX, Zhang H, Chen Z,
Wang F, Zhao HY and Fu LW: Niclosamide, an antihelmintic drug,
enhances efficacy of PD-1/PD-L1 immune checkpoint blockade in
non-small cell lung cancer. J Immunother Cancer. 7:2452019.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Schmalhofer O, Brabletz S and Brabletz T:
E-cadherin, beta-catenin, and ZEB1 in malignant progression of
cancer. Cancer Metastasis Rev. 28:151–166. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wu Q, Li J, Zhu S, Wu J, Chen C, Liu Q,
Wei W, Zhang Y and Sun S: Breast cancer subtypes predict the
preferential site of distant metastases: A SEER based study.
Oncotarget. 8:27990–27996. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Fillmore CM and Kuperwasser C: Human
breast cancer cell lines contain stem-like cells that self-renew,
give rise to phenotypically diverse progeny and survive
chemotherapy. Breast Cancer Res. 10:R252008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Grimshaw MJ, Cooper L, Papazisis K,
Coleman JA, Bohnenkamp HR, Chiapero-Stanke L, Taylor-Papadimitriou
J and Burchell JM: Mammosphere culture of metastatic breast cancer
cells enriches for tumorigenic breast cancer cells. Breast Cancer
Res. 10:R522008. View
Article : Google Scholar : PubMed/NCBI
|
|
27
|
Levine AJ and Puzio-Kuter AM: The control
of the metabolic switch in cancers by oncogenes and tumor
suppressor genes. Science. 330:1340–1344. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Vander Heiden MG, Cantley LC and Thompson
CB: Understanding the Warburg effect: The metabolic requirements of
cell proliferation. Science. 324:1029–1033. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Alasadi A, Chen M, Swapna GVT, Tao H, Guo
J, Collantes J, Fadhil N, Montelione GT and Jin S: Effect of
mitochondrial uncouplers niclosamide ethanolamine (NEN) and
oxyclozanide on hepatic metastasis of colon cancer. Cell Death Dis.
9:2152018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Lu J, Tan M and Cai Q: The Warburg effect
in tumor progression: Mitochondrial oxidative metabolism as an
anti-metastasis mechanism. Cancer Lett. 356 (2 Pt A):156–164. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Park SJ, Shin JH, Kang H, Hwang JJ and Cho
DH: Niclosamide induces mitochondria fragmentation and promotes
both apoptotic and autophagic cell death. BMB Rep. 44:517–522.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Khanim FL, Merrick BA, Giles HV, Jankute
M, Jackson JB, Giles LJ, Birtwistle J, Bunce CM and Drayson MT:
Redeployment-based drug screening identifies the anti-helminthic
niclosamide as anti-myeloma therapy that also reduces free light
chain production. Blood Cancer J. 1:e392011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Yu K, Wang T, Li Y, Wang C, Wang X, Zhang
M, Xie Y, Li S, An Z and Ye T: Niclosamide induces apoptosis
through mitochondrial intrinsic pathway and inhibits migration and
invasion in human thyroid cancer in vitro. Biomed Pharmacother.
92:403–411. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ye T, Xiong Y, Yan Y, Xia Y, Song X, Liu
L, Li D, Wang N, Zhang L, Zhu Y, et al: The anthelmintic drug
niclosamide induces apoptosis, impairs metastasis and reduces
immunosuppressive cells in breast cancer model. PLoS One.
9:e858872014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Yu H, Lee H, Herrmann A, Buettner R and
Jove R: Revisiting STAT3 signalling in cancer: New and unexpected
biological functions. Nat Rev Cancer. 14:736–746. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Duru N, Candas D, Jiang G and Li JJ:
Breast cancer adaptive resistance: HER2 and cancer stem cell
repopulation in a heterogeneous tumor society. J Cancer Res Clin
Oncol. 140:1–14. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Duru N, Fan M, Candas D, Menaa C, Liu HC,
Nantajit D, Wen Y, Xiao K, Eldridge A, Chromy BA, et al:
HER2-associated radioresistance of breast cancer stem cells
isolated from HER2-negative breast cancer cells. Clin Cancer Res.
18:6634–6647. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Kim JS, Kim HA, Seong MK, Seol H, Oh JS,
Kim EK, Chang JW, Hwang SG and Noh WC: STAT3-survivin signaling
mediates a poor response to radiotherapy in HER2-positive breast
cancers. Oncotarget. 7:7055–7065. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Chung SS, Giehl N, Wu Y and Vadgama JV:
STAT3 activation in HER2-overexpressing breast cancer promotes
epithelial-mesenchymal transition and cancer stem cell traits. Int
J Oncol. 44:403–411. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Li G, Zhao L, Li W, Fan K, Qian W, Hou S,
Wang H, Dai J, Wei H and Guo Y: Feedback activation of STAT3
mediates trastuzumab resistance via upregulation of MUC1 and MUC4
expression. Oncotarget. 5:8317–8329. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Wegrzyn J, Potla R, Chwae YJ, Sepuri NB,
Zhang Q, Koeck T, Derecka M, Szczepanek K, Szelag M, Gornicka A, et
al: Function of mitochondrial Stat3 in cellular respiration.
Science. 323:793–797. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Yang R and Rincon M: Mitochondrial Stat3,
the Need for Design Thinking. Int J Biol Sci. 12:532–544. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Gough DJ, Corlett A, Schlessinger K,
Wegrzyn J, Larner AC and Levy DE: Mitochondrial STAT3 supports
Ras-dependent oncogenic transformation. Science. 324:1713–1716.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Ren X, Duan L, He Q, Zhang Z, Zhou Y, Wu
D, Pan J, Pei D and Ding K: Identification of Niclosamide as a New
Small-Molecule Inhibitor of the STAT3 Signaling Pathway. ACS Med
Chem Lett. 1:454–459. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Chen H, Yang Z, Ding C, Chu L, Zhang Y,
Terry K, Liu H, Shen Q and Zhou J: Discovery of O-Alkylamino
Tethered Niclosamide Derivatives as Potent and Orally Bioavailable
Anticancer Agents. ACS Med Chem Lett. 4:180–185. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Wu PF, Lin CH, Kuo CH, Chen WW, Yeh DC,
Liao HW, Huang SM, Cheng AL and Lu YS: A pilot study of bevacizumab
combined with etoposide and cisplatin in breast cancer patients
with leptomeningeal carcinomatosis. BMC Cancer. 15:2992015.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Zhou L, Xu S, Yin W, Lin Y, Du Y, Jiang Y,
Wang Y, Zhang J, Wu Z and Lu J: Weekly paclitaxel and cisplatin as
neoadjuvant chemotherapy with locally advanced breast cancer: A
prospective, single arm, phase II study. Oncotarget. 8:79305–79314.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Isakoff SJ, Mayer EL, He L, Traina TA,
Carey LA, Krag KJ, Rugo HS, Liu MC, Stearns V, Come SE, et al:
TBCRC009: A Multicenter Phase II Clinical Trial of Platinum
Monotherapy With Biomarker Assessment in Metastatic Triple-Negative
Breast Cancer. J Clin Oncol. 33:1902–1909. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Silver DP, Richardson AL, Eklund AC, Wang
ZC, Szallasi Z, Li Q, Juul N, Leong CO, Calogrias D, Buraimoh A, et
al: Efficacy of neoadjuvant Cisplatin in triple-negative breast
cancer. J Clin Oncol. 28:1145–1153. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Shah N, Mohammad AS, Saralkar P, Sprowls
SA, Vickers SD, John D, Tallman RM, Lucke-Wold BP, Jarrell KE,
Pinti M, et al: Investigational chemotherapy and novel
pharmacokinetic mechanisms for the treatment of breast cancer brain
metastases. Pharmacol Res. 132:47–68. 2018. View Article : Google Scholar : PubMed/NCBI
|