Introduction
Recent advances in multidisciplinary treatments and
reconstructive surgery have improved the overall survival (OS) of
patients with oral cancer (1,2). The
worldwide incidence rate of oral cancer is 300,400 cases annually
and the 5-year OS rate is 50–60% (1,2).
Nevertheless, the complexities of the process of tumor progression
and tumor recurrence in inoperable cases often cause huge obstacles
in cancer treatment (3). Tegafur, a
component of the oral antitumor drug S-1, is the prodrug of
5-fluorouracil (5-FU) that inhibits DNA synthesis and causes RNA
dysfunction in cells, thereby exerting strong antitumor effects
against solid cancers of the head and neck region (4–7). S-1
with tegafur/uracil exhibited significantly improved treatment
outcome and improved the 3-year survival rate in patients with head
and neck squamous cell carcinoma (HNSCC) who underwent curative
treatment compared with the patients who did not have S1 treatment
(8). Although S-1 is associated with
side effects, including severe leukopenia, neutropenia, nausea,
vomiting and diarrhea, the frequency and degree of side effects are
lower than those reported for other chemotherapeutic agents, such
as docetaxel, taxol and cisplatin (4–11).
Angiogenesis has been identified as an important
determinant of solid tumor growth and metastasis. Several
regulatory factors are involved in tumor angiogenesis, among which
vascular endothelial growth factor (VEGF)-A serves a particularly
important role (12–15). In a clinical trial of HNSCC, strong
VEGF-A expression was negatively associated with OS and
disease-free survival (16–19). Similarly, high VEGF-A expression was
significantly associated with cancer progression and a poor
prognosis (based on T classification, N classification, grade,
clinical stage and cumulative survival) among patients with oral
squamous cell carcinoma (OSCC) (20,21).
VEGF-A-targeting monoclonal antibody therapies have yielded
successful results in various types of cancer including colorectal
cancer and head and neck cancer (10–12,22–24).
Bevacizumab is a molecularly targeted drug with
different properties compared with conventional chemotherapeutic
agents (25). It directly binds to
VEGF-A around the tumor and inhibits tumor angiogenesis (12). Moreover, bevacizumab exerts an
antitumor effect by inhibiting the nutrient supply to tumor cells
(13). Additionally, bevacizumab
normalizes residual blood vessels and improves the drug delivery
system into the tumor so that drugs reach the tumor at a higher
concentration (10,11,22–24). In
addition, the side effects of bevacizumab, which is administered by
intravenous injection, differ from those of conventional
chemotherapeutic agents (26,27).
Common side effects of bevacizumab include bleeding, delayed wound
healing, hypertension and proteinuria, which are rarely observed
with conventional chemotherapy (27,28).
Therefore, bevacizumab can be used in combination with conventional
antitumor drugs with low side effects (10,11,22–24). A
number of clinical trials with patients with recurrent and
metastatic HNSCC and OSCC revealed that bevacizumab in combination
with other molecular-targeted therapies, chemotherapies and/or
radiation therapy led to improved OS and progression-free survival
in numerous types of cancer, including HNSCC (10,11,22–24,29).
Previous studies reported that bevacizumab in combination with S-1
yielded modest to high efficacy against a number of types of
cancer, such as advanced recurrent or metastatic colorectal cancer,
advanced gastric cancer, advanced lung cancer, advanced esophageal
carcinoma with mild and acceptable toxicities, especially as a
second- or third-line therapy (12,23,30–33).
However, to the best of our knowledge, there are no available
reports on the efficacy of bevacizumab plus S-1 treatment in HNSCC
or OSCC.
In the present study, it was hypothesized that
bevacizumab in combination with S-1 may exert stronger antitumor
effect against OSCC cell lines compared with bevacizumab or S-1
alone. In addition, the possibility of fewer side effects of S-1
plus bevacizumab treatment in vivo compared with
conventional chemotherapeutic agents was investigated.
Materials and methods
Cell lines, cell culture and
reagents
The VEGF-A-expressing human oral or tongue cancer
HSC-2, HSC-3, HSC-4 and SAS cell lines were obtained from the RIKEN
BioResource Centre and maintained as monolayer cultures in
DMEM/Ham's F12 with L-glutamine and phenol red medium (FUJIFILM
Wako Pure Chemical Corporation) containing 10% FBS (Thermo Fisher
Scientific, Inc.), 100 µg/ml streptomycin and 100 U/ml penicillin
(Thermo Fisher Scientific, Inc.) at 37°C in a humidified incubator
with 5% CO2.
FBS was not added to the cell culture medium
subjected to western blotting, MTT assays and ELISA in order to
avoid non-specific reactions with VEGF-A present in the FBS. S-1
was obtained from Taiho Pharmaceutical Co., Ltd., while bevacizumab
was purchased from Chugai Pharmaceutical Co., Ltd.
Animals
A total of 12 female athymic BALB/c nu/nu nude mice
(4-week-old) with an average body weight of 20 g were obtained from
Japan SLC, Inc., and were kept under sterile conditions in a
pathogen-free and temperature-controlled (average temperature,
22.1°C) environment with a 12 h light/dark cycle. The mice received
sterilized water and food ad libitum. All manipulations were
conducted aseptically inside a laminar flow hood. All in
vivo experiments were approved by the Institutional Animal Care
and Use Committee of Yamaguchi University (Ube, Japan) (approval
no. 55-010).
Western blotting
HSC-2, HSC-3, HSC-4 and SAS cell lines were grown to
80% confluency in a 100-mm cell culture dish (BD Biosciences).
After adding fresh FBS-free media, cells were incubated at 37°C for
24 and 48 h. The cells were washed, collected by scraping and lysed
in 100 ml lysis buffer (1X formulation comprising 25 mM Tris-HCl pH
7.6, 150 mM NaCl, 1% NP-40, 1% sodium deoxycholate and 0.1% SDS).
Protein concentrations in the whole cell lysates were determined
using NanoDrop™ 1000 (Thermo Fisher Scientific, Inc.). A total of
80 µg protein/lane was loaded into NuPAGE™ 4–12% Bis-Tris gel (cat.
no. NP0322; Thermo Fisher Scientific, Inc.) and was subjected to
SDS-PAGE and then transferred onto PVDF membranes. A blocking
solution was made from Blocker/Diluent part A (cat. no. 46-7003;
Thermo Fisher Scientific, Inc.) and B (cat. no. 46-7004; Thermo
Fisher Scientific, Inc.) according to the manufacturer's protocol,
and the PVDF membranes were incubated in the blocking solution at
room temperature for 30 min. Membranes were treated with VEGF-A
(A-20 rabbit polyclonal; cat. no. SC-15;1:250; Santa Cruz
Biotechnology, Inc.) (or α-tubulin (loading control; B-7 mouse
monoclonal; cat. no. SC-5286; 1:1,000; Santa Cruz Biotechnology,
Inc.) primary antibody at 4°C overnight. The membranes were washed
using 1X wash solution (cat. no. 46-7005; Thermo Fisher Scientific,
Inc.) 3 times at room temperature (5 min/wash) according to
manufacturer's instruction, and then was incubated with either
secondary antibody solution Alk-Phos. conjugated anti-rabbit (cat.
no. 46-7006; neat; Thermo Fisher Scientific, Inc.) or Alk-Phos.
conjugated anti-mouse (cat. no. 46-7006; neat; Thermo Fisher
Scientific Inc.) at room temperature for 30 min. The membranes were
washed 3 times with 1X wash solution at room temperature (5
min/wash) and protein bands were detected by incubating the
membranes into Novex® AP Chromogenic substrate
(BCIP/NBT) (cat. no. 100002902; Thermo Fisher Scientific, Inc.) at
room temperature for 5–15 min. Quantification of protein bands was
performed using ImageJ v1.51h software (National Institutes of
Health). The fold-change of VEGF-A expression was calculated
relative to the control (α-tubulin) and expressed as a
percentage.
MTT assay
SAS and HSC-2 cells were seeded into a 96-well plate
(BD Biosciences) at a density of 5×103 cells/well and incubated at
37°C for 24 h. Subsequently, cells were treated (at 37°C for 24 or
48 h) as follows: Control (serum-free medium without drugs),
bevacizumab alone (1, 10 or 100 µg/ml)or 5-FU alone (0.5, 1 or 2
µg/ml) dissolved in serum-free medium. Cells were also treated with
bevacizumab (1, 10 or 100 µg/ml) plus 5-FU (05, 1 or 2 µg/ml)
dissolved in serum-free medium at 37°C for 48 h. Subsequently, MTT
solution (5mg/ml) was added to each well (25 µl/well) and incubated
for 4 h at 37°C. The purple formazan was dissolved in dimethyl
sulfoxide (100 µl/well) and the absorbance was measured using a
spectrophotometer (Bio-Rad Laboratories, Inc.) at a wavelength of
490 nm. All assays were performed in triplicate.
ELISA
SAS and HSC-2 cells were seeded into a 96-well plate
(BD Biosciences) at a density of 5×103 cells/well, and
wells were treated with one of the following treatments: Control
(serum-free medium without drugs), bevacizumab alone (10 µg/ml),
5-FU alone (1 µg/ml) or bevacizumab (10 µg/ml) plus 5-FU (1 µg/ml).
All cells were cultured at 37°C for 24 and 48 h, then VEGF-A
concentrations in the supernatant from each well were measured via
ELISA Human VEGF Quantikine ELISA kit (cat. no. DVE00; R&D
Systems, Inc.) according to manufacturer's instructions.
Human cancer xenograft models
HSC-2 cells were used as a xenograft model in BALB/c
nu/nu nude mice (n=12) as they have relatively higher tumorigenic
potential than SAS cells. HSC-2 cell line batches were frozen in
FBS supplemented with 5% dimethyl sulfoxide (v/v) prior to
injection into mice, and then were thawed shortly before injection.
In brief, HSC-2 cells (1×106/mice) were suspended into
0.1 ml PBS (0.05 M phosphate buffer containing 0.145 M sodium
chloride, pH 7.4) and injected into the subcutaneous tissues of
aforementioned nude mice with a 27-gauge needle when they were
5-weeks old. Tumors were allowed to grow for 10 days before
treatment. These tumor-bearing mice were divided into four groups
(n=3; tumor volumes, 40–50 mm3). The humane endpoints of
this in vivo experiment were: Rapid weight loss in treated
mice (≥20% body weight loss compared with the control group), very
large tumor (tumor weight ≥10% of body weight), skin/tumor
ulceration or necrosis, difficulty in ambulation and feeding or
drinking disorder.
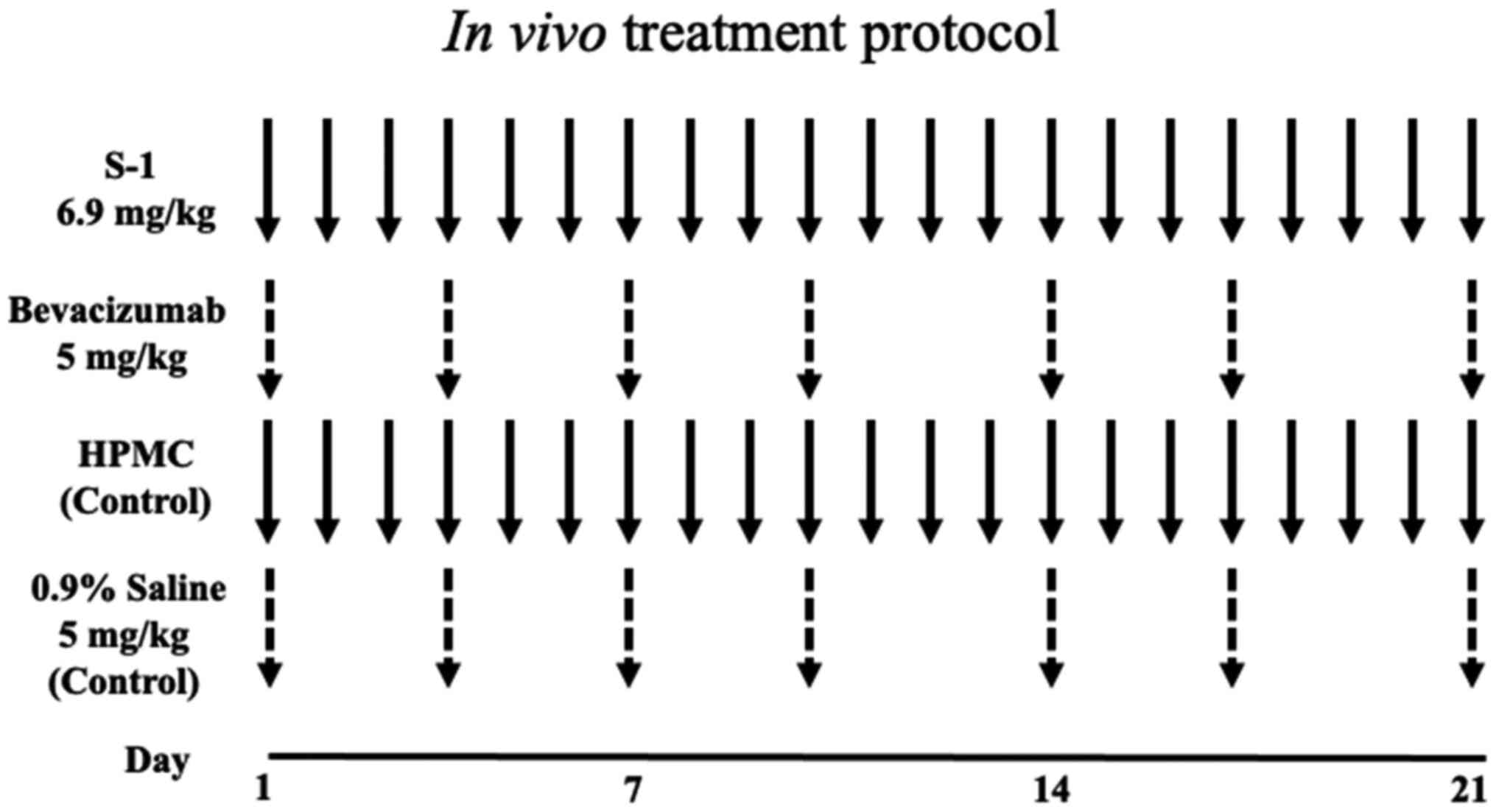
In vivo treatment protocol
Fig. 1 shows the
in vivo treatment protocol. The four treatment groups were:
S-1, bevacizumab, combination therapy and control groups. S-1 was
suspended in autoclaved 0.5% sodium hydroxypropyl methylcellulose
(HPMC; Daiichi Kogyo Seiyaku Co., Ltd.) under sterile conditions to
a concentration of 1.0 mg/ml and homogenized by stirring. The S-1
suspension was administered to mice via gastric lavage at a dosage
of 6.9 mg/kg/day for 3 weeks (S-1 group). Bevacizumab was injected
intraperitoneally (i.p) at a dosage of 5 mg/kg twice/week (on day 1
and 4 of each week) for 3 weeks (bevacizumab group). The
combination group received both S-1 (6.9 mg/kg/day for 21 days) and
bevacizumab 5 mg/kg twice/week (on day 1 and 4 of each week) for 3
weeks. The control mice group received either 5% HPMC (equal volume
of S-1) via gastric lavage or 0.9% saline (i.p) at a dosage of 5
ml/kg twice/week for 3 weeks.
Tumor measurements
HSC-2 ×enograft tumors were inspected twice/week and
measured using a Vernier caliper. Tumor volume (mm3) was
calculated using the standard formula a2 × b/2, where
‘a’ is the width and ‘b’ the length of the horizontal tumor. Body
weights were also measured every 2 days. On day 21, 12 h after the
final drug dosage, the experiment was terminated based on ethical
considerations, and the mice were sacrificed using an overdose of
Somnopentyl (sodium pentobarbital, 200 mg/kg; Merck & Co.,
Inc.). The tumors were dissected, fixed in 10% neutral-buffered
formalin at room temperature for 24 h (Mildform® 10N;
FUJIFILM Wako Pure Chemical Corporation) and embedded in paraffin
for further study. The relative tumor volume was calculated using
the following formula: Tumor volume of the respective tumor on day
n/volume of the same tumor on day 0 (before the treatment
started).
Immunohistochemistry
Avidin-biotin complex-based immunohistochemical
methods were performed to detect CD31 and Ki-67 in tissue specimens
using the EnVision kit™ (Dako; Agilent Technologies, Inc.).
Paraffin-embedded tissue sections (4-µm-thick) were deparaffinized
in xylene and rehydrated through a descending alcohol series at
room temperature. Deparaffinized sections were immersed in absolute
methanol containing 0.3% hydrogen peroxide for 20 min at room
temperature to block endogenous peroxidases. The sections were then
treated with Dako REAL™ peroxidase-blocking solution (cat. no.
S2023 Dako; Agilent Technologies, Inc.,) for 30 min at room
temperature to block non-specific reactions and were incubated
overnight at 4°C with goat anti-mouse CD31 or PECAM-1 (cat. no.
SC-376764; 1:100; Santa Cruz Biotechnology, Inc.) and mouse
anti-human Ki-67 (clone MIB-1; cat. no. M7240; 1:100; Dako; Agilent
Technologies, Inc.). After rinsing the tissue sections in PBS
thrice for 5 min each, 100 µl secondary antibody (Dako REAL™
Envision™ detection system; horse radish peroxidase; rabbit/Mouse;
cat. no. K5007; no dilution; Dako; Agilent Technologies, Inc.) was
added at room temperature for 30 min. Tissue sections were rinsed
thrice in PBS for 5 min each, and incubated with an chromogen
3,3′-diaminobenzidine tetrahydrochloride (DAB) solution for 7 min
at room temperature using Dako REAL™ Envision™ detection system
(cat. no. K5007; Dako; Agilent Technologies, Inc.). Tissue sections
were then counterstained by hematoxylin at room temperature for 1
min. Tissue sections were subsequently dehydrated in graded
ethanol, cleared using Histo-Clear (cat. no. HS200; National
Diagnostics) and mounted with glass coverslips using D.P.X.
(Millipore Sigma). Each experiment included positive controls (for
Ki-67: human tongue squamous cell carnimona tissue; for CD31: human
healthy tongue tissues) and negative controls (same tissue samples
without primary antibody).
Evaluation of microvessel density
(MVD)
Immunohistochemical techniques were used to evaluate
MVD, and vascularity was determined as described previously
(34,35). Unlike immunohistochemical analysis,
tumor vessels were stained with the aforementioned anti-mouse CD31
antibody for 90 min at room temperature. Paraffin sections were
pre-treated with 0.01% protease at 37°C for 20 min. The staining
protocol was otherwise similar to that used for
immunohistochemistry, as aforementioned. The number of vessels per
field was counted in the area of highest vascular density. Vessel
density was recorded as the number of CD31+ vessel
points per field under ×200 magnification using a fluorescence
microscope (BX51; Olympus Corporation). Vascularity was quantified
in the stroma close to the epithelium, up to ~750 µm from the basal
lamina, and microvessels in the tumors were counted. A total of 10
randomly selected fields from non-necrotic tumor tissue were
examined per section, and the results are expressed as the mean
percentage ± SD as previously described (36).
Evaluation of cell proliferation
Immunohistochemical techniques were also used to
evaluate the cell proliferative ability. Tumor cells were stained
with mouse anti-human Ki-67 by immunohistochemistry as
aforementioned, and Ki-67+ nuclei were counted under
×200 magnification from a total of 1,000 cells to determine the
distribution of cell proliferation using a fluorescence microscope
(BX51; Olympus Corporation) as previously described (37).
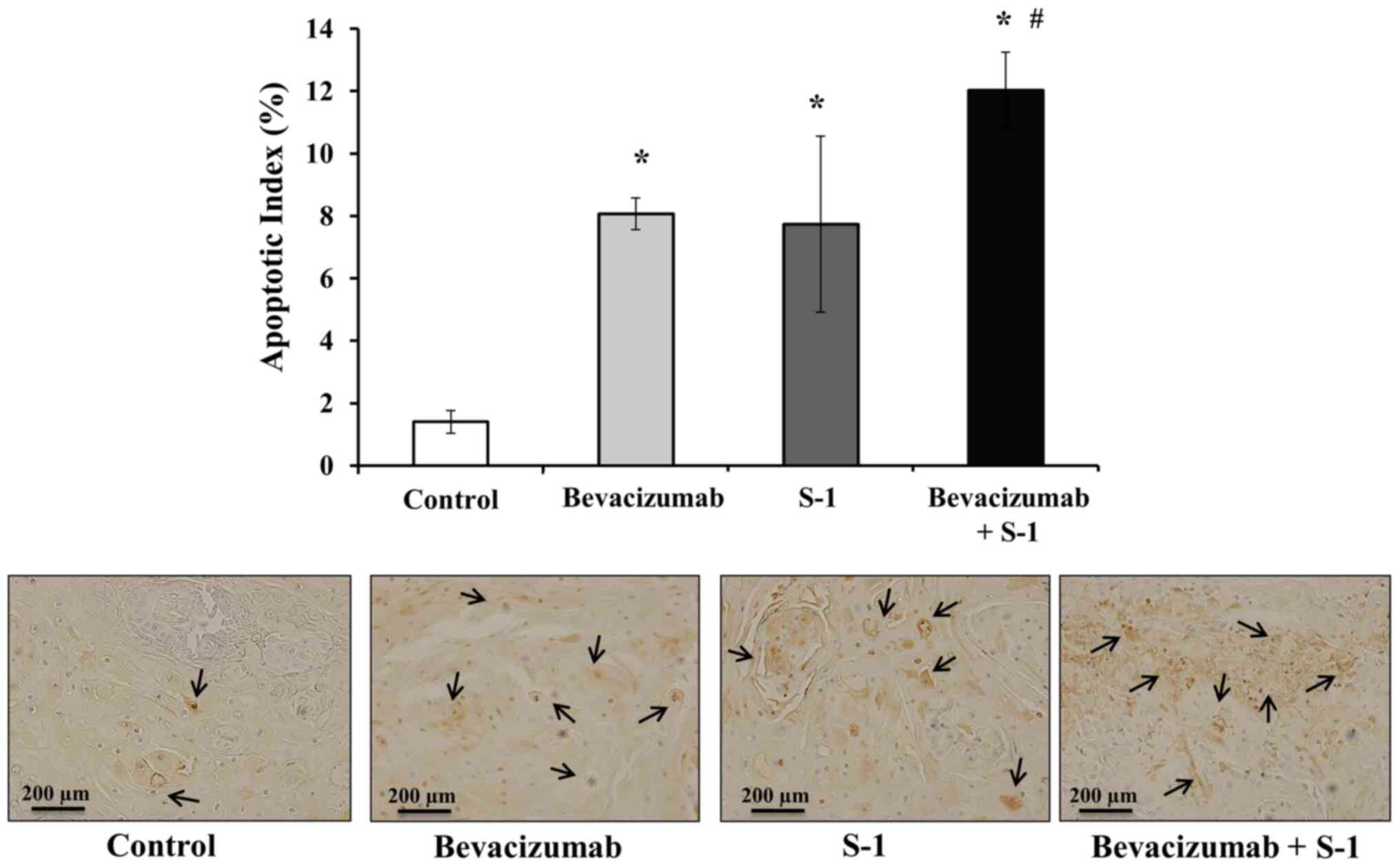
Evaluation of apoptotic index
Tissue sections were subjected to TUNEL assay to
examine apoptosis using the DeadEnd™ Fluorometric TUNEL system
(cat. no. G3250; Promega, Corporation) according to manufacturer's
instructions. Paraffin-embedded tumor sections (4-µm-thick) were
deparaffinized in xylene, rehydrated using a graded ethanol series
and incubated with 20 µg/ml proteinase K (Dako; Agilent
Technologies, Inc.) at room temperature for 15 min. The sections
were then rinsed with distilled water and incubated in a 3%
hydrogen peroxide solution at room temperature for 5 min to block
endogenous peroxidases. The sections were then washed with PBS,
incubated in an equilibration buffer and treated with TdT enzyme in
a humidified chamber at 37°C for 60 min. Slides were subsequently
placed in working strength stop wash buffer at room temperature for
10 min, rinsed with PBS and incubated with an
anti-digoxigenin-peroxidase conjugate at room temperature for 30
min. Diaminobenzidine (Peroxidase Substrate kit; Vector
Laboratories, Inc.) was then applied to each section to reveal
peroxidase activity. Hematoxylin was used at room temperature for 1
min as the counterstain. TUNEL-positive cells were counted under
×200 magnification from a minimum of 5 microscopic fields per
section using a fluorescence microscope (BX51; Olympus Corporation)
to determine the distribution of apoptotic cells. The apoptotic
index was reported as the percentage of TUNEL-positive cells per
1,000 total cells as previously described (38).
Statistical analysis
MTT and ELISA data of drug-treated cells, tumor
measurements, MVD, cell proliferative ability and apoptotic index
were compared using one-way ANOVA followed by the post hoc Tukey's
test. All data were presented as the mean ± SD. The
Statcels2® 4-Step Excel Statistics software application
was used for the analyses (OMS Publishing, Inc.; http://oms-publ.memo.jp/main/). P<0.05 was
considered to indicate a statistically significant difference.
Results
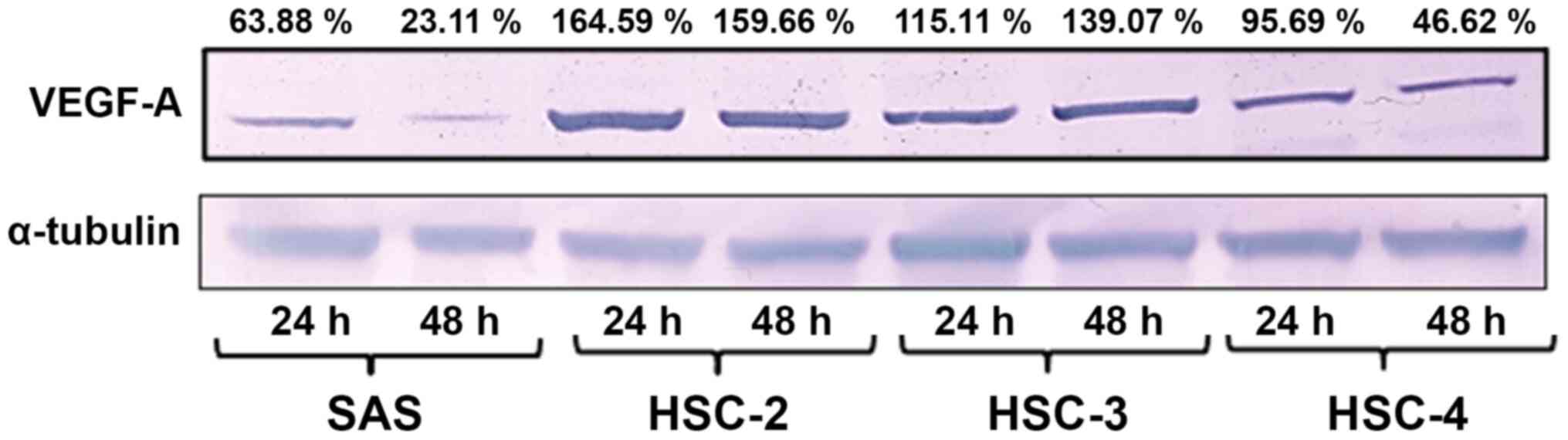
Endogenous VEGF-A expression in four
OSCC cell lines in vitro
Western blotting of the cultured cell lines revealed
the highest levels of VEGF-A expression in HSC-2 cells after 24 and
48 h of culture, followed by HSC-3, HSC-4 and SAS cells (Fig. 2).
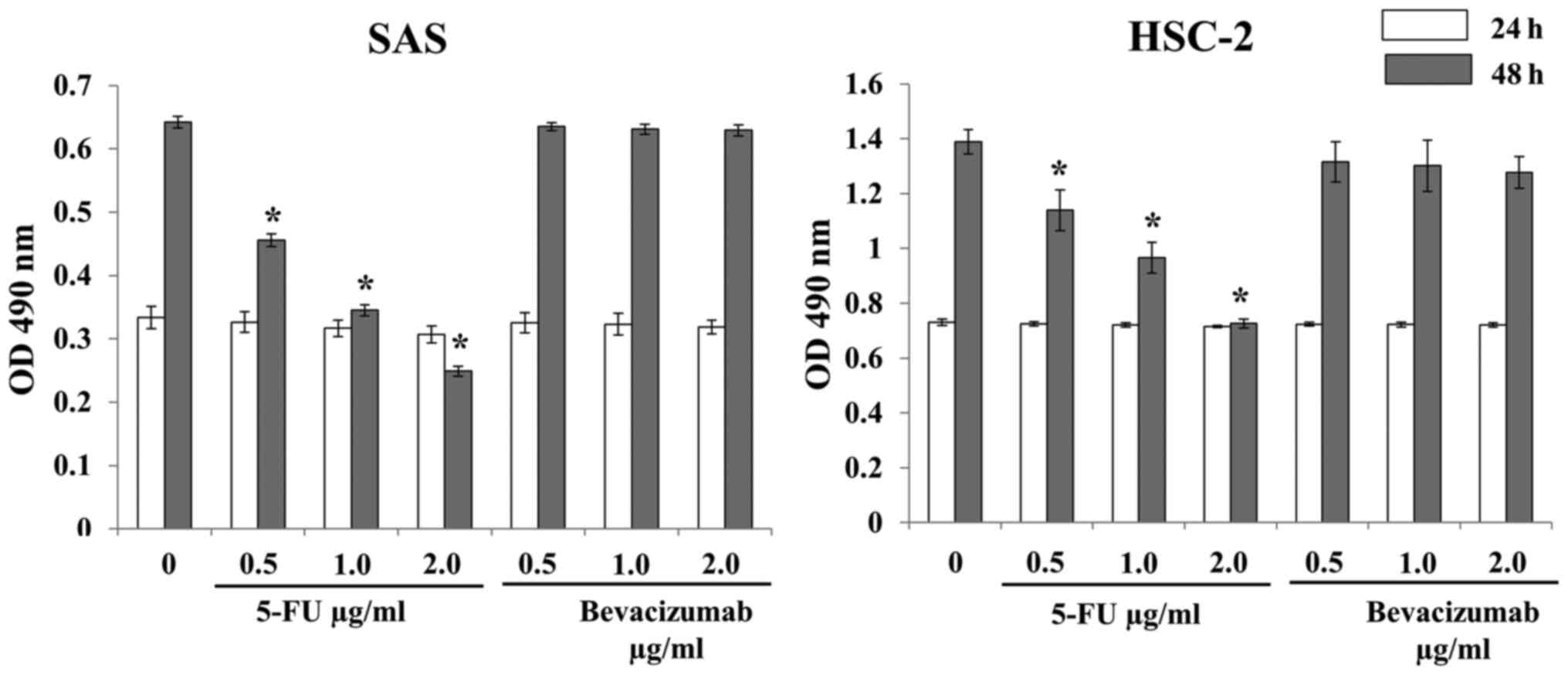
Inhibitory effects of 5-FU and
bevacizumab on SAS and HSC-2 cell proliferation in vitro
No significant decrease in SAS and HSC-2 cell
proliferation was observed after treatment with 5-FU alone or
bevacizumab alone for 24 h compared with no treatment (Fig. 3). Treatment with 5-FU alone for 48 h
significantly inhibited the proliferation of SAS and HSC-2 cells
compared with no treatment; however, bevacizumab treatment alone
for 48 h did not exert any effect (Fig.
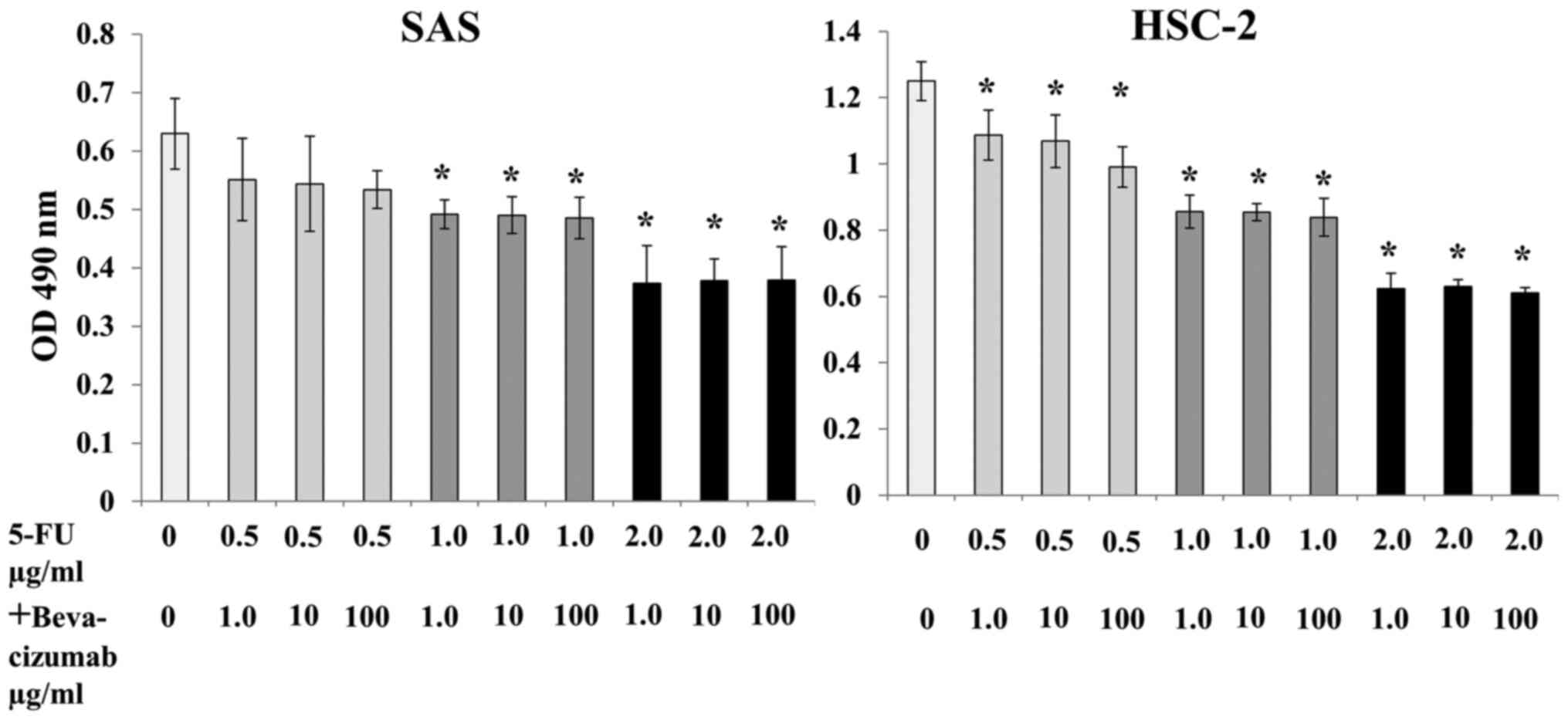
3). Although combined treatment with 5-FU and bevacizumab
significantly inhibited the proliferation of both SAS and HSC-2
cells, no synergistic or additive effects were observed (Fig. 4).
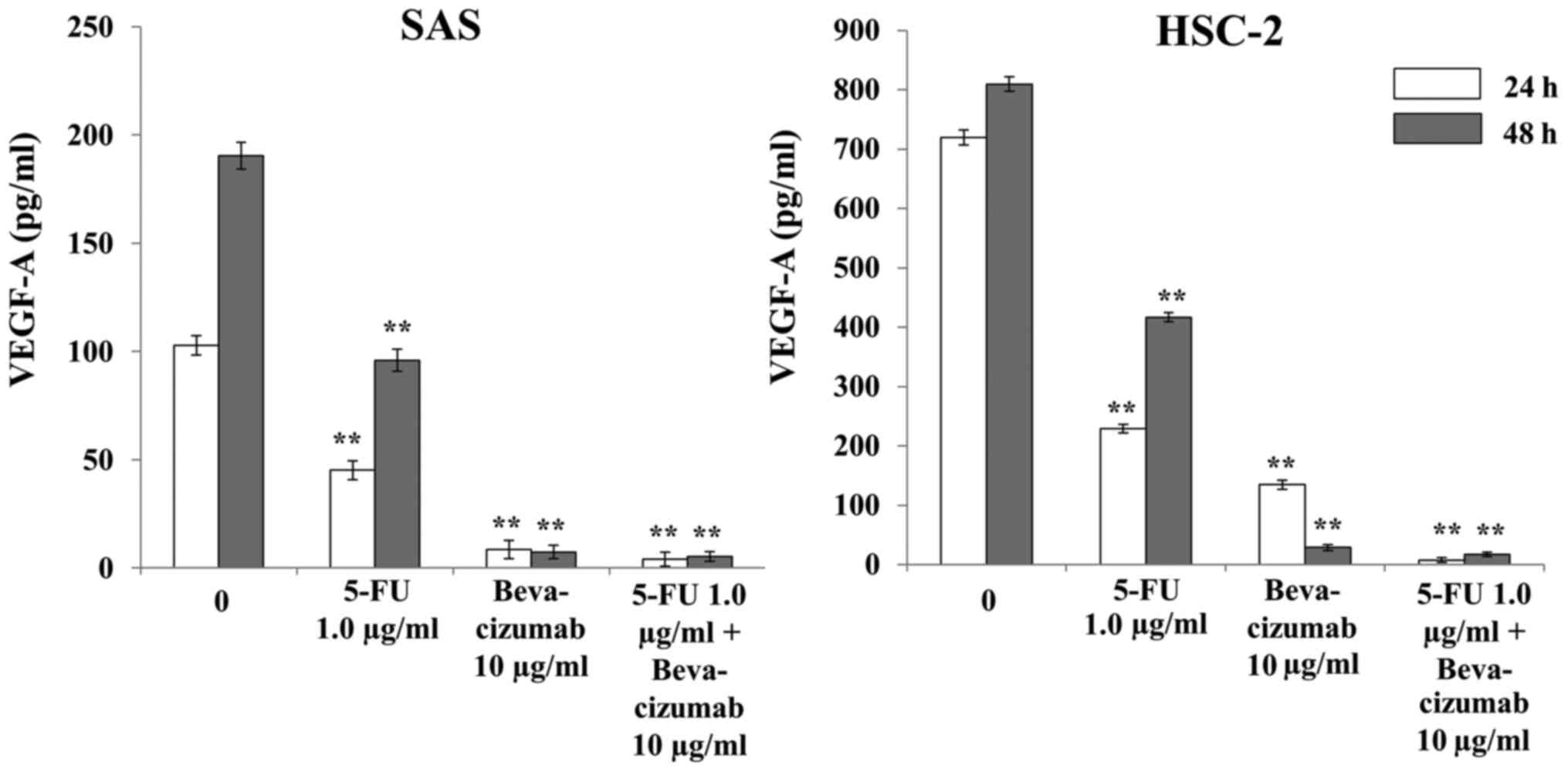
Effects of 5-FU and bevacizumab on
VEGF-A production by SAS and HSC-2 cells in vitro
Treatment with 5-FU alone significantly decreased
VEGF-A production in both SAS and HSC-2 cells compared with the
control, and further decreases were observed with bevacizumab alone
and in combination with 5-FU after 24 and 48 h of treatment
(Fig. 5). In both cell lines,
significant differences were observed after 24 and 48 h of
treatment with either agent, alone or in combination, compared with
the control (Fig. 5).
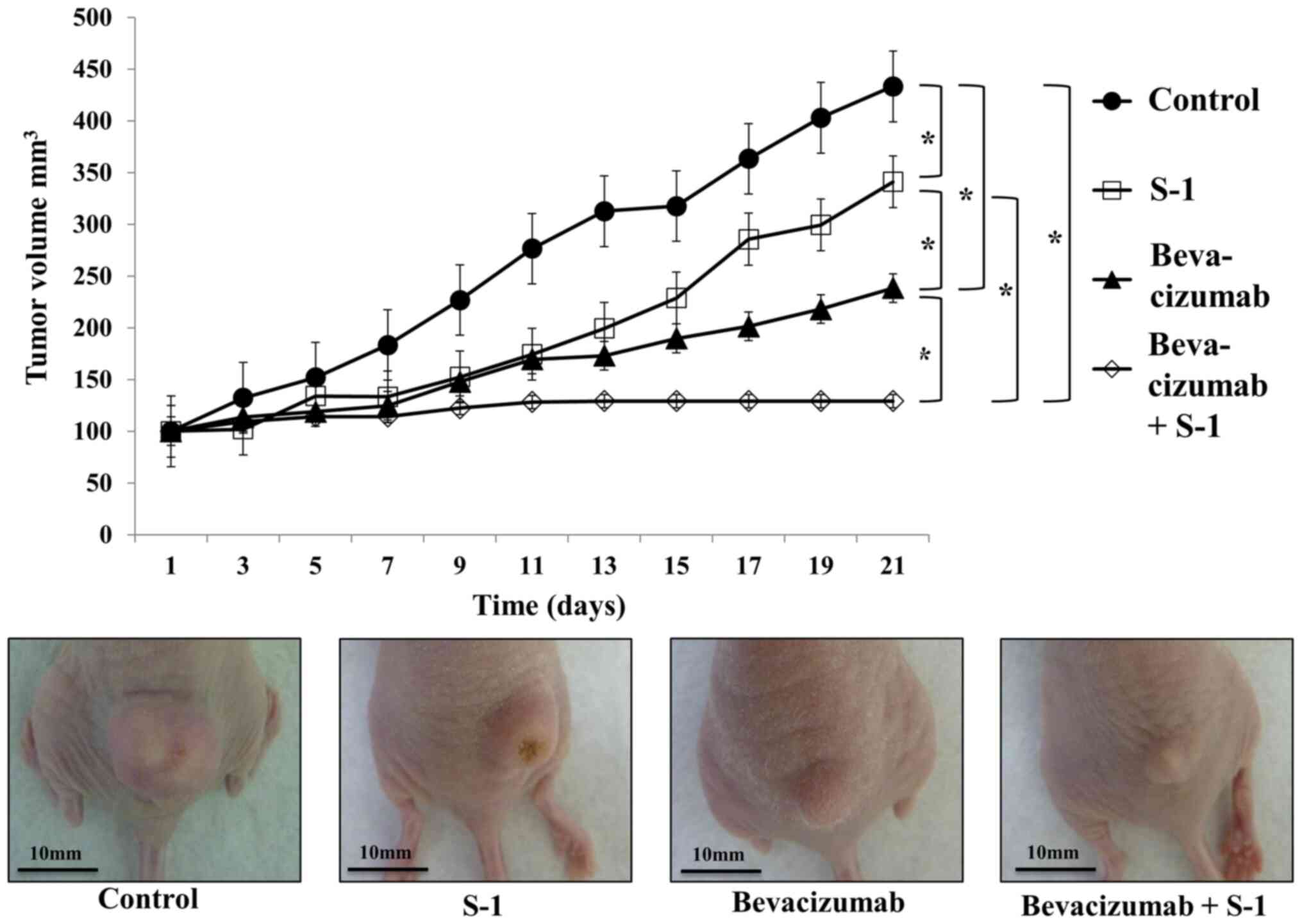
Relative changes in tumor volume over
time
On average, tumor growth inhibition was observed
with bevacizumab alone, S-1 alone or both agents in combination,
and this inhibition was significantly different compared with that
in the control group (Fig. 6).
Bevacizumab was more effective than S-1 at decreasing tumor volume,
and the combination of bevacizumab and S-1 was significantly more
effective than either agent alone (Fig.
6). No increase in tumor volume was observed in mice treated
with the combination of bevacizumab and S-1 after day 13 (Fig. 6). No loss of body weight was observed
in any treated mice during the experimental period (data not
shown). Furthermore, no abnormalities were observed in the heart,
lung, liver and kidney of mice by the naked eye (data not
shown).
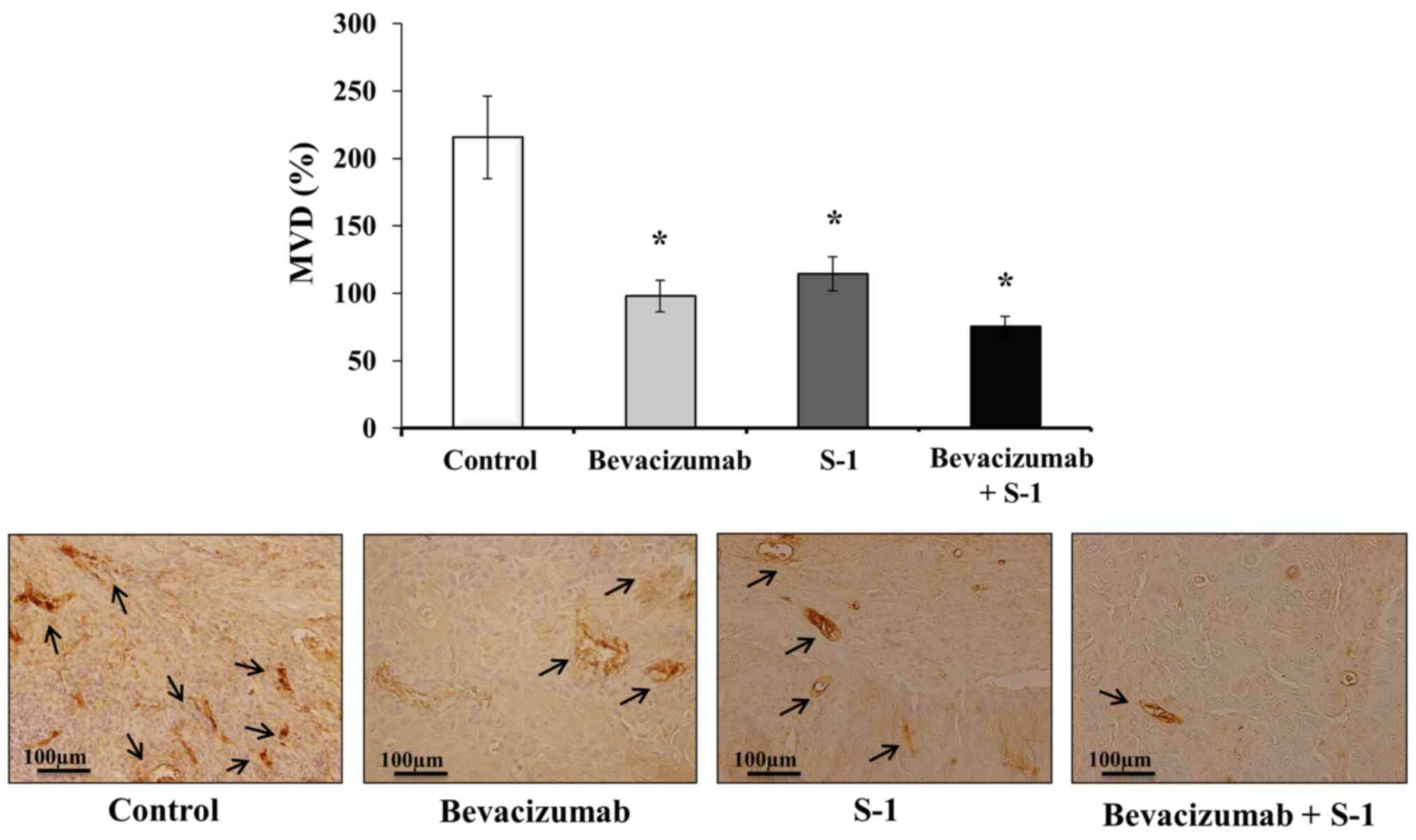
Effects of S-1 and bevacizumab on
residual tumor MVD in vivo
Mice tumor sections were subjected to
immunohistochemical staining with CD31 to clarify the antitumor
mechanisms affecting MVD. The following MVD values were recorded
for each group: Control group, 215.67±30.55%; bevacizumab group,
98.00±11.79%; S-1 group, 114.33±12.66%; and combination group,
75.33±7.57% (Fig. 7). The MVDs of
the S-1 alone, bevacizumab alone and combination groups were
significantly lower than that of the control group (Fig. 7). Although the MVD value of
bevacizumab alone was lower than that of S-1 alone, and the MVD of
the combination group was lower than bevacizumab or S-1 alone, no
significant differences were observed among the treatment groups
(Fig. 7).
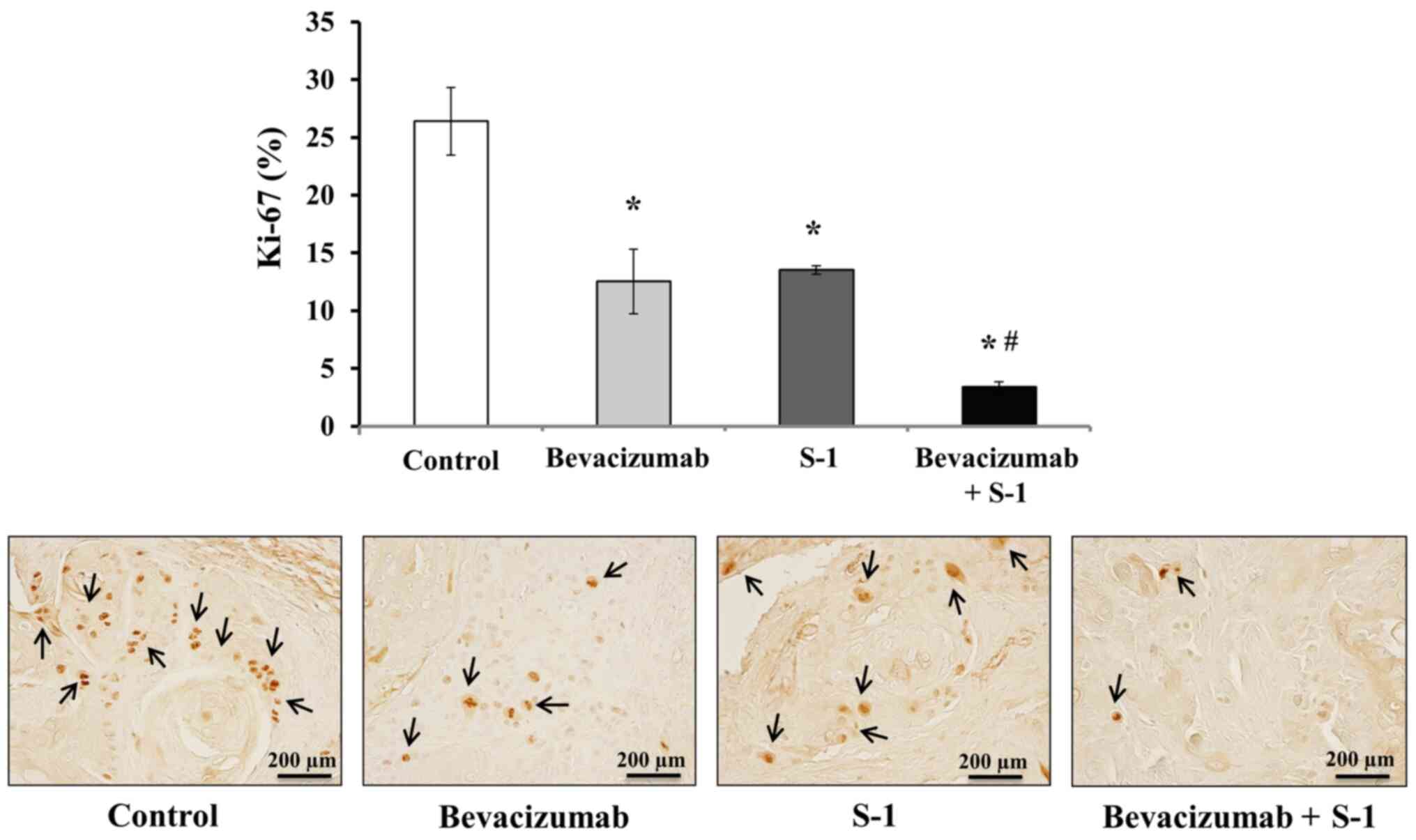
Inhibitory effects of S-1 and
bevacizumab on cell proliferation in vivo
Tumor sections were stained with Ki-67 via
immunohistochemistry, and the numbers of Ki-67+ nuclei
were quantified to analyze the degree of inhibition of cell
proliferation. Tumors treated with either bevacizumab or S-1 alone
exhibited significantly decreased cell proliferative abilities
compared with the control group (Fig.
8). Additionally, the number of Ki-67+ nuclei was
significantly lower in tumors treated with both bevacizumab and S-1
compared with that of tumors in the control or individual treatment
groups (Fig. 8). The number of
Ki-67+ nuclei in different treatment groups was: Control
group, 26.40±2.91%; bevacizumab group, 12.53±2.80%; S-1 group,
13.53±0.38%; combination group, 3.40±0.46% (Fig. 8).
Effects of S-1 and bevacizumab on
apoptosis induction in vivo
Next, the rate of apoptosis in nude mice tumors was
analyzed after treatment with bevacizumab or S-1, alone or in
combination. The number of apoptotic cells in each harvested tumor
was quantified using a TUNEL assay. A significantly higher degree
of apoptosis was observed in tumors treated with either bevacizumab
or S-1 alone compared with the control group (Fig. 9). However, the highest number of
apoptotic cells was observed in tumors treated with bevacizumab and
S-1 in combination; this combination treatment significantly
induced apoptosis compared with each agent alone, as well as
compared with the control (Fig. 9).
The apoptotic indexes were as follows: Control group, 1.4±0.36%;
bevacizumab group, 8.07±0.5%; S-1 group, 7.73±2.82%; and
combination group, 12.0±1.22% (Fig.
9).
Discussion
A number of mice xenografts studies have revealed
that 5-FU metabolized from S-1 exerts significant antitumor effects
and inhibits tumor angiogenesis by inducing apoptosis of the tumor
vascular endothelial cells in various types of tumor, including
human OSCC (6–8,38–40).
Additionally, bevacizumab monotherapy exhibited antitumor effects
in nude mice with OSCC and HNSCC tumors (12). Moreover, this antitumor effect of
bevacizumab was enhanced when administered in combination with
paclitaxel, irinotecan, cisplatin, interleukin-8, irradiation or
cetuximab (36,41–44).
In the present study, a synergistic and suppressive
antitumor effect of bevacizumab plus S-1 combination therapy was
observed against OSCC in vivo. Although the combined
treatment with 5-FU and bevacizumab inhibited the proliferation of
SAS and HSC-2 cells in vitro, it did not exhibit any
synergistic effect. On the other hand, the results of the current
in vivo experiments suggested that the anti-angiogenic
action of bevacizumab and the antitumor effect of S-1
synergistically inhibited tumor cell proliferation and promoted
apoptosis. Although VEGF-A expression was not analyzed in mice
tumors, it may be possible that S-1/5-FU downregulated VEGF
expression by suppressing NF-κB, which finally resulted in
decreased MVD and inhibited angiogenesis (8,45).
Similar results were obtained in two types of OSCC
cell lines in vitro: HSC-2, which expressed high levels of
VEGF-A, and SAS, which expressed low levels of VEGF-A; however,
there was no synergistic effect of the combination treatment. HSC-2
cells are derived from squamous cell carcinoma of the mouth; it has
an epithelial cell-like morphology and no metastatic potential
(46). On the other hand, SAS is a
poorly differentiated squamous cell carcinoma cell line from a
human tongue primary lesion (47).
5-FU inhibited cell proliferation and directly decreased VEGF-A
expression. By contrast, bevacizumab alone did not inhibit cell
proliferation and did not exhibit a synergistic suppressive effect
when administered in combination with 5-FU; in other words, it did
not have a direct antitumor effect in vitro. However,
bevacizumab neutralized VEGF-A expression in the culture
supernatant, thus decreasing the concentration of VEGF-A around the
neoplastic cells. The reason why bevacizumab alone did not exert
antitumor effect or apoptosis in vitro remains unknown and
should be further clarified in the future.
Based on the present results, it can be assumed that
bevacizumab alone cannot exert antitumor effects in an in
vitro environment (48).
However, it can possibly exert antitumor effects in an in
vivo environment, which is a complex mixture of tumor cells,
tumor blood vessels and interstitial cells. In the present study,
HSC-2 cells were used for the in vivo experiments, as this
cell line had a higher tumorigenic potential and it strongly
expressed VEGF-A compared with the SAS cell line.
It has been reported that 5-FU inhibits tumor cell
proliferation and has an anti-angiogenic effect, which is not as
strong as bevacizumab (32,33,36,38,40,41). In
the present study, it was observed that in the S-1 alone group,
5-FU metabolized from S-1 exerted an antitumor effect by inhibiting
cell proliferation and inducing apoptosis in vivo, as well
as by decreasing MVD. However, we assumed that bevacizumab alone
led to the regression of immature tumor blood vessels and a
negative feedback loop involving continuous reduction of the
nutrient supply to cancer cells; these factors ultimately led to
the inhibition of cell proliferation and induction of
apoptosis.
Tumor progression was slowed down by S-1 or
bevacizumab alone, but was not completely inhibited in mice. It can
be hypothesized that, in the combination group, the marked
decreases in tumor progression, MVD and cell proliferative ability,
and the increase in the apoptotic index may be attributed to an
improved ability to maintain homeostasis, which was absent in the
S-1 or bevacizumab alone groups. Hence, we suggest the following
mechanism behind the antitumor effect of S-1 and bevacizumab
combination therapy. Bevacizumab binds to VEGF-A secreted from
tumor cells and may induce the regression of immature tumor blood
vessels and a negative feedback cycle that disrupts the continuous
nutrient supply to cancer cells, thus inhibiting cell proliferation
and promoting apoptosis. At the same time, it may be assumed that
S-1 exerts direct antitumor effects, as well as promoting
continuous indirect antitumor angiogenesis inhibition, thereby
exerting marked antitumor effects. This may be a reason for the
marked antitumor effect of the combination treatment on cell
proliferation and apoptosis, but not for the direct effect on
angiogenesis. However, the underlying mechanisms of S-1 and
bevacizumab combination treatment in OSCC are not completely
understood, and there may be other unknown underlying factors
responsible for the efficacy of this combination treatment.
Additionally, the present study did not analyze VEGF-A expression
in mice tumors nor the concentrations of drugs within tumor
tissues, adjacent tissues or plasma. Therefore, this should be
further investigated in future studies.
Recent findings have indicated that once a solid
tumor reaches a certain size, it begins to secrete various
angiogenic factors to promote the neovasculature (49,50).
Tumor growth can be suppressed by blocking blood vessels that feed
tumors, which can then disappear via tumor dormancy without
metastasis (51,52). Given the lack of further increase in
tumor volume after day 13 of the bevacizumab and S-1 combination
therapy in the present study, the potential need for tumor dormancy
therapy in OSCC should be considered, as proposed by Folkman and
Hochberg (53). In other words,
bevacizumab inhibits VEGF-A secretion from tumor cells and causes
simultaneous inhibition of tumor growth and angiogenesis.
Bevacizumab exerts a significant antitumor effect by improving drug
delivery and thus allowing high concentrations of 5-FU to diffuse
into the tumor (54). Therefore,
conventional chemotherapy can directly exert antitumor effect on
tumor cells, whereas bevacizumab can indirectly inhibit cell
proliferation and increase apoptosis by decreasing nutrition supply
to the tumor (55). In addition,
bevacizumab can be expected to have further antitumor effects if
combined with conventional antitumor agents (56). Hence, the current combination therapy
may be used as a new treatment for OSCC due to its enhanced
antitumor effects.
In conclusion, the combined treatment of S-1 and
bevacizumab was effective against OSCC cells in vitro and
exhibited marked synergistic antitumor effects in vivo. This
combination therapy seemed to inhibit cell proliferation and
promote apoptosis by controlling tumor angiogenesis. The present
results indicated that S-1 and bevacizumab combination therapy may
be a useful and promising treatment for refractory, highly
angiogenic OSCC tumors.
Acknowledgements
Not applicable.
Funding
The present study was supported in part by
Grant-in-Aid from the Japanese Ministry of Education, Science and
Culture (grant nos. 21890168 and 15K11292).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YI and KH designed the study. YI and TT performed
the experiments. YI, TF and KH analyzed the data, wrote and revised
the manuscript. YI, TF and KH confirmed the authenticity of all the
raw data. YU and KM helped in analysis and interpretation of data,
revised the manuscript and provided valuable suggestions during the
study. All authors have read and approved the final version of the
manuscript and are fully responsible for its content.
Ethics approval and consent to
participate
All in vivo experiments were approved by the
Institutional Animal Care and Use Committee of Yamaguchi University
(approval no. 55-010; Ube, Japan).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Joo YH, Cho JK, Koo BS, Kwon M, Kwon SK,
Kwon SY, Kim MS, Kim JK, Kim H, Nam I, et al: Guidelines for the
surgical management of oral cancer: Korean society of thyroid-head
and neck surgery. Clin Exp Otorhinolaryngol. 12:107–144. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chi AC, Day TA and Neville BW: Oral cavity
and oropharyngeal squamous cell carcinoma - an update. CA Cancer J
Clin. 65:401–421. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Vermorken JB, Remenar E, van Herpen C,
Gorlia T, Mesia R, Degardin M, Stewart JS, Jelic S, Betka J, Preiss
JH, et al EORTC 24971/TAX 323 Study Group, : Cisplatin,
fluorouracil, and docetaxel in unresectable head and neck cancer. N
Engl J Med. 357:1695–1704. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tsukuda M, Kida A, Fujii M, Kono N,
Yoshihara T, Hasegawa Y and Sugita M; Chemotherapy Study Group of
Head and Neck Cancer, : Randomized scheduling feasibility study of
S-1 for adjuvant chemotherapy in advanced head and neck cancer. Br
J Cancer. 93:884–889. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Harada K, Sato M, Ueyama Y, Nagayama M,
Hamakawa H, Nagahata S, Yoshimura Y, Osaki T and Ryoke K; Oral
Cancer Study Group of Chugoku-Shikoku, : Multi-institutional phase
II trial of S-1 in patients with oral squamous cell carcinoma.
Anticancer Drugs. 19:85–90. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yokoe H, Kasamatsu A, Ogawara K, Ishigami
T, Sato Y, Shibata M, Tanzawa H and Uzawa K: Neoadjuvant
chemotherapy with S-1 for patients with oral squamous cell
carcinoma. J Cancer Sci Ther. 2:132–135. 2010. View Article : Google Scholar
|
|
7
|
Tsukahara K, Kubota A, Hasegawa Y,
Takemura H, Terada T, Taguchi T, Nagahara K, Nakatani H, Yoshino K,
Higaki Y, et al: Randomized phase III trial of adjuvant
chemotherapy with S-1 after curative treatment in patients with
squamous-cell carcinoma of the head and neck (ACTH-HNC). PLoS One.
11:1–15. 2015.
|
|
8
|
Harada K, Ferdous T and Ueyama Y:
Therapeutic strategies with oral fluoropyrimidine anticancer agent,
S-1 against oral cancer. Jpn Dent Sci Rev. 53:61–77. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sakuramoto S, Sasako M, Yamaguchi T,
Kinoshita T, Fujii M, Nashimoto A, Furukawa H, Nakajima T, Ohashi
Y, Imamura H, et al ACTS-GC Group, : Adjuvant chemotherapy for
gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med.
357:1810–1820. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yamada Y, Takahari D, Matsumoto H, Baba H,
Nakamura M, Yoshida K, Yoshida M, Iwamoto S, Shimada K, Komatsu Y,
et al: Leucovorin, fluorouracil, and oxaliplatin plus bevacizumab
versus S-1 and oxaliplatin plus bevacizumab in patients with
metastatic colorectal cancer (SOFT): An open-label,
non-inferiority, randomised phase 3 trial. Lancet Oncol.
14:1278–1286. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Presta LG, Chen H, O'Connor SJ, Chisholm
V, Meng YG, Krummen L, Winkler M and Ferrara N: Humanization of an
anti-vascular endothelial growth factor monoclonal antibody for the
therapy of solid tumors and other disorders. Cancer Res.
57:4593–4599. 1997.PubMed/NCBI
|
|
12
|
Yoshida H, Yoshimura H, Matsuda S, Ryoke
T, Kiyoshima T, Kobayashi M and Sano K: Effects of peritumoral
bevacizumab injection against oral squamous cell carcinoma in a
nude mouse xenograft model: A preliminary study. Oncol Lett.
15:8627–8634. 2018.PubMed/NCBI
|
|
13
|
Willett CG, Boucher Y, di Tomaso E, Duda
DG, Munn LL, Tong RT, Chung DC, Sahani DV, Kalva SP, Kozin SV, et
al: Direct evidence that the VEGF-specific antibody bevacizumab has
antivascular effects in human rectal cancer. Nat Med. 10:145–147.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tong M, Lloyd B, Pei P and Mallery RS:
Human head and neck squamous cell carcinoma cells are both targets
and effectors for the angiogenic cytokine, VEGF. J Cell Biochem.
105:1202–1210. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Vassilakopoulou M, Psyrri A and Argiris A:
Targeting angiogenesis in head and neck cancer. Oral Oncol.
51:409–415. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Mineta H, Miura K, Ogino T, Takebayashi S,
Misawa K, Ueda Y, Suzuki I, Dictor M, Borg A and Wennerberg J:
Prognostic value of vascular endothelial growth factor (VEGF) in
head and neck squamous cell carcinomas. Br J Cancer. 83:775–781.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Smith BD, Smith GL, Carter D, Sasaki CT
and Haffty BG: Prognostic significance of vascular endothelial
growth factor protein levels in oral and oropharyngeal squamous
cell carcinoma. J Clin Oncol. 18:2046–2052. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tse GM, Chan AW, Yu KH, King AD, Wong KT,
Chen GG, Tsang RK and Chan AB: Strong immunohistochemical
expression of vascular endothelial growth factor predicts overall
survival in head and neck squamous cell carcinoma. Ann Surg Oncol.
14:3558–3565. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
O-charoenrat P, Rpys-Evans P and Eccles S:
Expression of vascular endothelial growth family members in head
and neck squamous cell carcinoma correlates with lymph node
metastasis. Cancer. 92:556–568. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Shang ZJ, Li JR and Li ZB: Circulating
levels of vascular endothelial growth factor in patients with oral
squamous cell carcinoma. Int J Oral Maxillofac Surg. 31:495–498.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Cheng SJ, Lee JJ, Kok SH, Chou CH, Chang
HH, Yang H, Chiang ML and Kuo MY: Expression of vascular
endothelial growth factor is significantly associated with
progression and prognosis of oral squamous cell carcinomas in
Taiwan. J Formos Med Assoc. 110:50–57. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hurwitz H, Fehrenbacher L, Novotny W,
Cartwright T, Hainsworth J, Heim W, Berlin J, Baron A, Griffing S,
Holmgren E, et al: Bevacizumab plus irinotecan, fluorouracil, and
leucovorin for metastatic colorectal cancer. N Engl J Med.
350:2335–2342. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Seiwert TY, Haraf DJ, Cohen EE, Stenson K,
Witt ME, Dekker A, Kocherginsky M, Weichselbaum RR, Chen HX and
Vokes EE: Phase I study of bevacizumab added to fluorouracil- and
hydroxyurea-based concomitant chemoradiotherapy for poor-prognosis
head and neck cancer. J Clin Oncol. 26:1732–1741. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Yao M, Galanopoulos N, Lavertu P, Fu P,
Gibson M, Argiris A, Rezaee R, Zender C, Wasman J, Machtay M, et
al: Phase II study of bevacizumab in combination with docetaxel and
radiation in locally advanced squamous cell carcinoma of the head
and neck. Head Neck. 37:1665–1671. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ferrara N and Davis-Smyth T: The biology
of vascular endothelial growth factor. Endocr Rev. 18:4–25. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Monk BJ, Sill MW, McMeekin DS, Cohn DE,
Ramondetta LM, Boardman CH, Benda J and Cella D: Phase III trial of
four cisplatin-containing doublet combinations in stage IVB,
recurrent, or persistent cervical carcinoma: A Gynecologic Oncology
Group study. J Clin Oncol. 27:4649–4655. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wright JD, Viviano D, Powell MA, Gibb RK,
Mutch DG, Grigsby PW and Rader JS: Bevacizumab combination therapy
in heavily pretreated, recurrent cervical cancer. Gynecol Oncol.
103:489–493. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Monk BJ, Sill MW, Burger RA, Gray HJ,
Buekers TE and Roman LD: Phase II trial of bevacizumab in the
treatment of persistent or recurrent squamous cell carcinoma of the
cervix: A gynecologic oncology group study. J Clin Oncol.
27:1069–1074. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Suzuki S, Shimazaki J, Morishita K, Koike
N, Harada N, Hayashi T and Suzuki M: Efficacy and safety of
oxaliplatin, bevacizumab and oral S-1 for advanced recurrent
colorectal cancer. Mol Clin Oncol. 5:391–394. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Fang J, Wang H and Xu Q: Bevacizumab
combined with low-dose S-1 as maintenance therapy with a long
progression-free survival in an elderly patient with heavily
pre-treated advanced gastric cancer: A case report. Biomed Rep.
1:239–242. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Yamada K, Ichiki M, Takahashi K, Hisamatsu
Y, Takeoka H, Azuma K, Shukuya T, Nishikawa K, Tokito T, Ishii H,
et al: A multicenter phase II trial of S-1 combined with
bevacizumab after platinum-based chemotherapy in patients with
advanced non-squamous non-small cell lung cancer. Cancer Chemother
Pharmacol. 78:501–507. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Nie K, Geng C, Zhang L, Liu S, Zhang Z,
Wang R, Zou X and Ji Y: Clinical observation of bevacizumab
combined with S-1 in the treatment of pretreated advanced
esophageal carcinoma. Chin Med Sci J. 31:221–227. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Yoshida M, Takagane A, Miyake Y, Shimada
K, Nagata N, Sato A, Ogata Y, Fukunaga M, Otsuka K, Takahashi T, et
al: A phase II study of third-line combination chemotherapy with
bevacizumab plus S-1 for metastatic colorectal cancer with mutated
KRAS (SAVIOR Study). Oncology. 91:24–30. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Weidner N, Semple JP, Welch WR and Folkman
J: Tumor angiogenesis and metastasis - correlation in invasive
breast carcinoma. N Engl J Med. 324:1–8. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Harada K, Baillie R, Lu S, Syrjänen S and
Schor AM: VEGF expression in skin warts. Relevance to angiogenesis
and vasodilation. Arch Dermatol Res. 293:233–238. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Fujita K, Sano D, Kimura M, Yamashita Y,
Kawakami M, Ishiguro Y, Nishimura G, Matsuda H and Tsukuda M:
Anti-tumor effects of bevacizumab in combination with paclitaxel on
head and neck squamous cell carcinoma. Oncol Rep. 18:47–51.
2007.PubMed/NCBI
|
|
37
|
Roland NJ, Caslin AW, Bowie GL and Jones
AS: Has the cellular proliferation marker Ki67 any clinical
relevance in squamous cell carcinoma of the head and neck? Clin
Otolaryngol Allied Sci. 19:13–18. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Itashiki Y, Harada K, Ferdous T and
Yoshida H: Effects of tumor necrosis factor-related
apoptosis-inducing ligand alone and in combination with
fluoropyrimidine anticancer agent, S-1, on tumor growth of human
oral squamous cell carcinoma xenografts in nude mice. Anticancer
Res. 27:2365–2375. 2007.PubMed/NCBI
|
|
39
|
Harada K, Supriatno, Kawashima Y, Yoshida
H and Sato M: S-1 inhibits tumorigenicity and angiogenesis of human
oral squamous cell carcinoma cells by suppressing expression of
phoshorylated Akt, vascular endothelial growth factor and
fibroblast growth factor-2. Int J Oncol. 30:365–374.
2007.PubMed/NCBI
|
|
40
|
Shirasaka T, Nakano K, Takechi T, Satake
H, Uchida J, Fujioka A, Saito H, Okabe H, Oyama K, Takeda S, et al:
Antitumor activity of 1 M tegafur-0.4 M
5-chloro-2,4-dihydroxypyridine-1 M potassium oxonate (S-1) against
human colon carcinoma orthotopically implanted into nude rats.
Cancer Res. 56:2602–2606. 1996.PubMed/NCBI
|
|
41
|
Yoshida M, Muro K, Tsuji A, Hamamoto Y,
Yoshino T, Yoshida K, Shirao K, Miyata Y, Takahari D, Takahash T,
et al: Combination chemotherapy with bevacizumab and S-1 for
elderly patients with metastatic colorectal cancer (BASIC trial).
Eur J Cancer. 51:935–941. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Cao S, Durrani FA, Toth K, Rustum YM and
Seshadri M: Bevacizumab enhances the therapeutic efficacy of
Irinotecan against human head and neck squamous cell carcinoma
xenografts. Oral Oncol. 47:459–466. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Wang Y, Dong L, Bi Q, Li X, Wu D, Ge X,
Zhang X, Fu J, Zhang C, Wang C, et al: Investigation of the
efficacy of a bevacizumab-cetuximab-cisplatin regimen in treating
head and neck squamous cell carcinoma in mice. Target Oncol.
5:237–243. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Gyanchandani R, Sano D, Ortega Alves MV,
Klein JD, Knapick BA, Oh S, Myers JN and Kim S: Interleukin-8 as a
modulator of response to bevacizumab in preclinical models of head
and neck squamous cell carcinoma. Oral Oncol. 49:761–770. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Ferdous T, Harada K, Kin T, Harada T and
Ueyama Y: Efficacy of schedule-dependent metronomic S-1
chemotherapy in human oral squamous cell carcinoma cells. Int J
Oncol. 43:271–279. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
CELL BANK Website: HSC-2 cell, .
https://cellbank.brc.riken.jp/cell_bank/CellInfo/?cellNo=RCB1945
|
|
47
|
Takahashi K, Kanazawa H, Akiyama Y, Tazaki
S, Takahara M, Muto T, Tanazawa H and Sato K: Establishment and
characterization of a cell line (SAS) from poorly differentiated
human squamous cell carcinoma of the tongue. J Jpn Stomatol Soc.
38:20–28. 1989.(In Japanese).
|
|
48
|
Heydar H, Mansouri K, Norooznezhad M,
Norooznezhad F, Mohamadnia A and Bahrami N: Bevacizumab inhibits
angiogenic cytokines in head and neck squamous cell carcinoma: From
gene to the protein. Int J Hematol Oncol Stem Cell Res. 12:136–141.
2018.PubMed/NCBI
|
|
49
|
Wary KK: Molecular targets for
anti-angiogenic therapy. Curr Opin Mol Ther. 6:54–70.
2004.PubMed/NCBI
|
|
50
|
Gimbrone MA Jr, Leapman SB, Cotran RS and
Folkman J: Tumor dormancy in vivo by prevention of
neovascularization. J Exp Med. 136:261–276. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Holmgren L, O'Reily MS and Folkman J:
Dormancy of micrometastasis, balanced proliferation and apoptosis
in the presence of angiogenesis suppression. Nat Med. 1:149–153.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
O'Reilly MS, Holmgren L, Chen C and
Folkman J: Angiostatin induces and sustains dormancy of human
primary tumors in mice. Nat Med. 2:689–692. 1996. View Article : Google Scholar
|
|
53
|
Folkman J and Hochberg M: Self-regulation
of growth in three dimensions. J Exp Med. 138:745–753. 1973.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Turley RS, Fontanella AN, Padussis JC,
Toshimitsu H, Tokuhisa Y, Cho EH, Hanna G, Beasley GM, Augustine
CK, Dewhirst MW and Tyler DS: Bevacizumab-induced alterations in
vascular permeability and drug delivery: A novel approach to
augment regional chemotherapy for in-transit melanoma. Clin Cancer
Res. 18:3328–3339. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Iwasaki J and Nihira S: Anti-angiogenic
therapy against gastrointestinal tract cancers. Jpn J Clin Oncol.
39:543–551. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Falcetta F, Bizzaro F, D'Agostini E, Bani
MR, Giavazzi R and Ubezio P: Modeling cytostatic and cytotoxic
responses to new treatment regimens for ovarian cancer. Cancer Res.
77:6759–6769. 2017. View Article : Google Scholar : PubMed/NCBI
|