Introduction
The laparoscopic approach for abdominal surgery has
been increasingly applied, becoming the gold standard for numerous
surgical procedures, including appendicectomy (1), sigmoidectomy for diverticular disease
(2), left lateral hepatectomy for
benign lesions (3,4) and bariatric roux-en-y gastrectomy
(5). However, previous studies on
this technique have been variable regarding its surgical
application for malignant conditions. Although this approach is
beneficial in terms of postoperative recovery, early postoperative
quality of life and postoperative complications (6), other issues arise when it comes to
oncologic resections, such as achievement of R0 resection, disease
free survival (DFS) and overall survival (OS), where contradictory
evidence questions the value of laparoscopic surgery (7,8).
Postulated causes include surgeons performing laparoscopic
resections while still in training, along with a lack of tactile
feedback that might lead to increased R1 resections. Other concerns
include the dissemination of cancer cells due to pneumoperitoneum
(9), and in gastric surgery
specifically, the inability to perform adequately extensive
lymphadenectomy, which is crucial for gastric cancer oncological
outcomes (8).
Gastrointestinal stromal tumours (GISTs) are
malignant lesions of the gastrointestinal tract, arising from
interstitial Cajal cells. Positive long-term outcomes in patients
with GISTs rely on the success of surgical resection. Contrary to
gastric adenocarcinoma, extensive lymphadenectomy does not appear
to be considered as important for GISTs (10). This observation, along with the fact
that GISTs are usually well-localized tumours, presents advantages
for laparoscopic resection. Several studies have demonstrated the
safety and efficacy of GIST laparoscopic resection (11). However, almost all of these are
retrospective studies, and although short-term outcomes have been
extensively presented and discussed, long-term oncological outcomes
have not been adequately reported. Current findings have been
incorporated into respective guidelines, with conclusions stating
that basic oncologic principles should be adhered to, including
complete resection and the avoidance of rupture (12,13).
Therefore, laparoscopic surgery may be reserved for smaller tumours
(12), and for tumours of the
anterior wall of the stomach (13).
The present study aimed to examine current evidence
regarding the oncological outcomes of laparoscopic resection in
comparison with open resection performed in patients with GISTs. To
achieve these aims, a systematic review was performed, in which
relevant studies were critically evaluated.
Literature search
Two authors of the current study separately carried
out the literature search, study screening and selection, data
extraction and study evaluation. Disagreements that arose were
settled by a third author. The literature search was conducted
across three independent databases, including PubMed, Library,
Information Science and Technology Abstracts (EBSCO) and the
Library of Congress. Two groups of search terms were used. The
first group included one of the following terms: ‘Minimal’,
‘minimally’, ‘MIS’, ‘laparoscopic’ and ‘laparoscopically’. The
second group included one of the following terms: ‘GIST’, ‘stroma’,
‘stromal’, ‘stromatic’, ‘mesenchymal’ and ‘mesenchymatic’. Search
terms regarding the anatomical area of the stomach were not used in
the present literature search due to the large variability of
relevant descriptors. Manual screening was performed in place of
this. All possible combinations of one term per group were searched
for in the title and/or abstract of studies. The search was limited
to articles published from 2016 onwards to cover the last 5 years
to date. Only those published in English, and only the studies
reporting direct comparisons between laparoscopic resection and
open surgery were included. The exclusion criteria were as follows:
Unavailability of full text, tumour size limitations and secondary
studies, such as reviews and meta-analyses. Upon the initial
literature search and following the removal of duplicates, titles
and abstracts were screened for relevance. Full texts were
retrieved for those that were deemed relevant. References were
screened for relevant articles that were potentially not detected
through the initial literature search, and respective full texts
were additionally retrieved. Finally, full texts were screened and
selected for inclusion in the present study.
Data extraction
Data were extracted using a pre-agreed pro forma
spreadsheet. Data included: First author, year of publication,
studied time period, type of design (prospective vs. retrospective;
cohort vs. subgroup vs. propensity score matching), total number of
patients, number of patients per group (laparoscopic vs. open), sex
(as a percentage of males per group), age (as the median age in
years per group), tumour size (as the median maximum diameter in cm
per group), conversion rate, R0 achievement (as the rate per
group), duration of operation (as the median duration in min per
group), intraoperative blood loss (as median blood loss in ml per
group), length of hospital stay [as median length of stay (LoS) in
days per group], complication rate [as the percentage of patients
that developed grade III or IV complications according to the
Dindo-Clavien classification (14),
per group], duration of follow-up (as the median follow-up in
months per group), recurrence rate (as the percentage per group),
DFS (for studies that reported 100% R0 resection; recorded as
median survival in months per group), 5-year recurrence free
survival (for studies that reported 100% R0 resection; recorded as
percentage per group), mortality (as defined in each study;
recorded as the percentage per group), OS (as the median survival
in months per group) and 5-year survival (as the percentage per
group).
The evaluation of included studies was performed
according to modified MINORS criteria (15). Plain descriptive statistics were
implemented to group studies in quartiles according to overall
grade.
Literature search results and patient
demographics
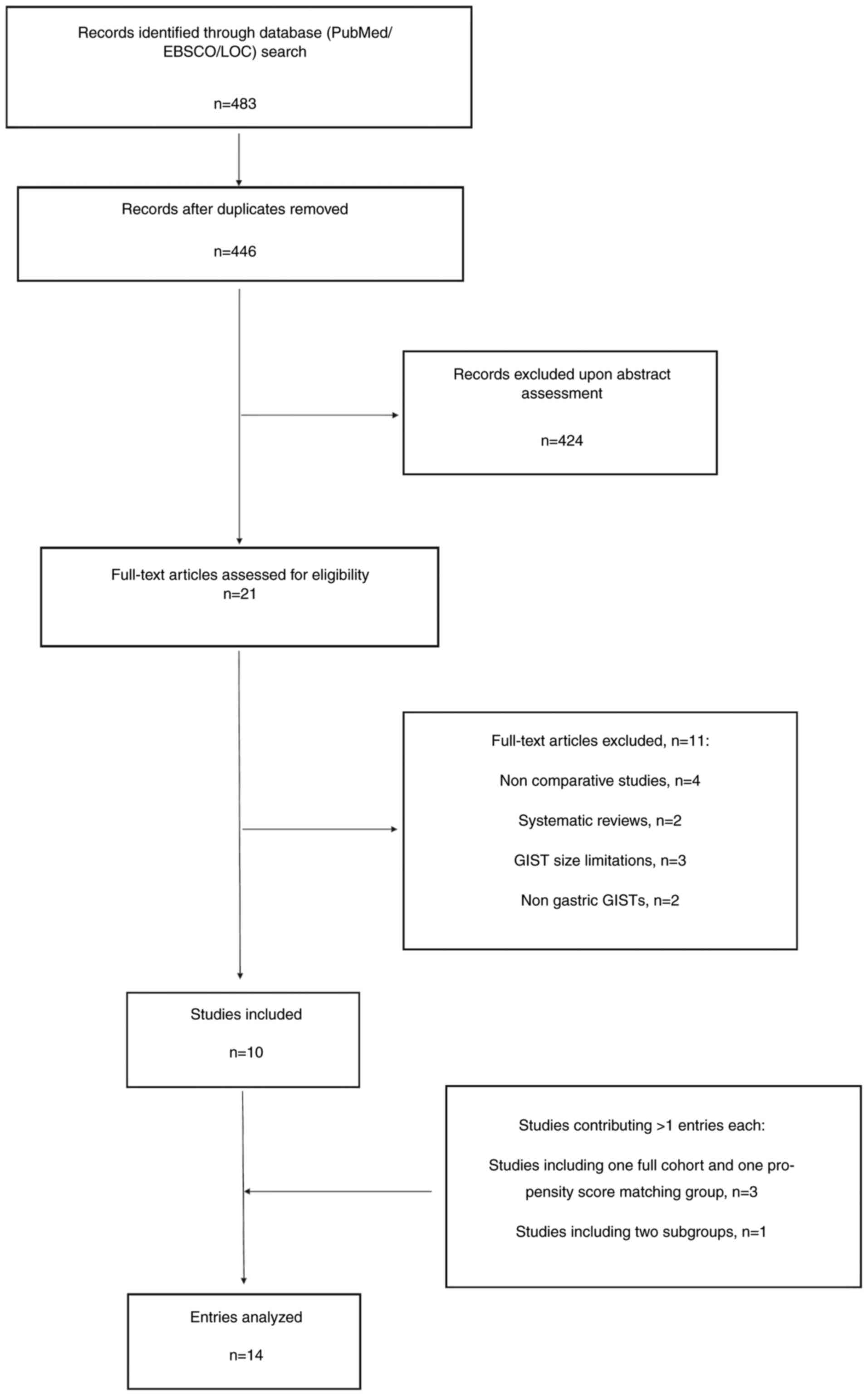
The initial literature search yielded 483 papers, of
which the titles and abstracts of 446 articles were screened for
relevance following the removal of duplicates. A total of 22 full
texts were retrieved, with 10 studies put forward for inclusion
(16–25). A full cohort was provided in three
studies, where propensity score matched analysis was performed,
meaning that these studies yielded two entries each (19,23,24). One
study presented two subgroup analyses, contributing a total of two
entries (20). Consequently, 14
entries were analysed. Fig. 1
presents the flow chart of article selection, providing further
details for the articles that were excluded. As predicted, there
were no randomized studies.
Table I presents the
design characteristics of the included entries, as well as the main
epidemiological parameters. Study sample size ranged from 74 to 426
patients in total. Inclusion of the male sex ranged from 26.05 to
54% for the laparoscopic groups, and from 18.69 to 62% for the open
resection groups. Median age ranged from 55 to 66 years in the
laparoscopic groups and from 57 to 70 years in the open resection
groups. None of the above was reported to be statistically
significant. Conversion rate was not reported in four entries
deriving from two studies (23,24) and
was only 8% in the study performed in the USA (25). Furthermore, the conversion rate was
3.07% in one study (17) and 0% in
the remaining studies.
 | Table I.Included studies, design
characteristics and main epidemiological parameters. |
Table I.
Included studies, design
characteristics and main epidemiological parameters.
| Author, year | Span | Design | n | n, lap vs. open | Sex, male %, lap vs.
open | Age, median in years,
lap vs. open | Size, max cm, lap vs.
open | Conversion, % | (Refs.) |
|---|
| Chen et al,
2016 | 2006-2012 | Retrospective | 214 | 133 vs. 81 | 32.70 vs.
18.69 | 59.10 vs.
57.40 | >10.00 vs.
>10.00 | NA | (23) |
|
| 2006-2012 | After PSM | 142 | 71 vs. 71 | 26.05 vs.
26.05 | 57.90 vs.
57.30 | >10.00 vs.
>10.00 | NA |
|
| Hu et al,
2016 | 2009-2014 | Prospective | 181 | 93 vs. 88 | 55.00 vs.
48.00 | 61.10 vs.
63.28 | 5.93 vs. 6.08 | 0.00 | (16) |
| Xu et al,
2017 | 2005-2014 | Retrospective | 88 | 44 vs. 44 | 47.70 vs.
43.20 | 55.10 vs.
57.40 | 7.00 vs. 7.40 | 0.00 | (22) |
| Chi et al,
2017 | 2006-2015 | Retrospective | 126 | 63 vs. 63 | 39.70 vs.
39.70 | 58.50 vs.
58.02 | 6.35 vs. 6.07 | 0.00 | (21) |
| Huang et al,
2017 | 2006-2014 | Retrospective | 214 | 133 vs. 81 | NA | NA | NA | NA | (20) |
|
| 2006-2014 | Favourable | 140 | 90 vs. 50 | 52.22 vs.
52.00 | 58.80 vs.
56.60 | 7.40 vs. 10.30 | 0.00 |
|
|
| 2006-2014 | Unfavourable | 74 | 43 vs. 31 | 53.48 vs.
45.16 | 59.50 vs.
58.70 | 6.80 vs. 8.20 | 0.00 |
|
| Ye et al,
2017 | 2005-2014 | Retrospective | 224 | 102 vs. 122 | 42.15 vs.
43.44 | NA | 14.00 vs.
>10.00 | NA | (24) |
|
| 2005-2014 | After PSM | 160 | 80 vs. 80 | 45.00 vs.
41.25 | NA | 14.00 vs.
>10.00 | NA |
|
| Wakamatsu et
al, 2018 | 2003-2015 | Retrospective | 89 | 65 vs. 24 | 54.00 vs.
62.00 | 66.00 vs.
69.50 | 5.00 vs. 12.60 | 3.07 | (17) |
| Xiong et al,
2020 | 2005-2017 | Retrospective | 426 | 185 vs. 241 | 50.80 vs.
55.20 | 57.38 vs.
56.90 | >10.00 vs.
>10.00 | 0.00 | (19) |
|
| 2005-2017 | After PSM | 256 | 128 vs. 128 | 53.10 vs.
50.00 | 58.23 vs.
57.98 | >10.00 vs.
>10.00 | 0.00 |
|
| Stanek et
al, 2019 | 2002-2017 | Retrospective | 68 | 46 vs. 22 | 28.30 vs.
36.40 | 67.00 vs.
65.00 | 5.50 vs. 7.00 | 0.00 | (18) |
| Mazer et al,
2021 | 2000-2018 | Retrospective | 77 | 53 vs. 24 | NA | NA | 4.00 vs. 7.00 | 8.00 | (25) |
Perioperative data
Table II presents
perioperative data. Five entries did not report data on the
completeness of resection (16,20,24).
Mazer et al (25) reported an
R0 rate of 95.83% in the open resection group (which comprised one
patient). However, R0 rate was 100% in the respective laparoscopic
group as well as in all other studies that reported this outcome.
Median duration varied greatly from 87 to 125 min in the
laparoscopic groups, and from 95 to ~700 min in the open resection
groups. Nine entries reported a shorter median duration of
operation for the laparoscopic approach, all of which were
statistically significant. One entry reported identical median
durations, while three entries reported shorter median operative
times in the open resection group, with only one of these reaching
statistical significance. Four entries did not include data on
intraoperative blood loss. The remaining entries presented
significantly less intraoperative blood loss in the respective
laparoscopic groups. One entry did not report on LoS. The remaining
entries reported significantly shorter hospitalization times in the
respective laparoscopic groups. Median LoS in laparoscopic groups
ranged from 3 to 10 days, while the open resection group ranged
from 6 to 15 days. Four entries did not report on postoperative
complications, and the remaining 10 did not demonstrate statistical
significance.
 | Table II.Perioperative outcomes. |
Table II.
Perioperative outcomes.
| Author, year | R0, %, lap vs.
open | Duration, median
min, lap vs. open | Blood loss, median
mls, lap vs. open | LoS, median days,
lap vs. open | Complications,
III–IV %, lap vs. openb | (Refs.) |
|---|
| Chen et al,
2016 | 100.00 vs.
100.00 | 111.00 vs.
190.00a | 35.00 vs.
297.00a | 8.60 vs.
13.40a | 2.30 vs. 2.50 | (23) |
|
| 100.00 vs.
100.00 | 115.00 vs.
186.00a | 36.00 vs.
290.00a | 8.80 vs.
13.30a | 2.80 vs. 1.40 |
|
| Hu et al,
2016 | 100.00 vs.
100.00 | 103.00 vs.
172.00a | 100.00 vs.
144.00a | 7.90 vs.
12.80a | 8.80 vs. 16.50 | (16) |
| Xu et al,
2017 | NA | 90.40 vs.
118.10a | 93.50 vs.
108.10a | 6.00vs.
9.70a | NA | (22) |
| Chi et al,
2017 | 100.00 vs.
100.00 | 87.46 vs.
119.58a | 36.80 vs.
115.50a | 6.10 vs.
8.60a | NA | (21) |
| Huang et al,
2017 | NA | 107.30 vs.
187.00a | 35.20 vs.
263.80a | 8.30 vs.
12.40a | 2.20 vs. 0.00 | (20) |
|
| NA | 119.00 vs.
197.40a | 35.20 vs.
350.60a | 9.50 vs.
14.90a | 2.30 vs. 6.50 |
|
| Ye et al,
2017 | NA | NA | NA | NA | NA | (24) |
|
| NA | 90.83 vs.
118.38a | 91.88 vs.
121.25a | 9.26 vs.
11.73a | NA |
|
| Wakamatsu et
al, 2018 | 100.00 vs.
100.00 | 108.00 vs.
108.00 | 32.50 vs.
100.00a | 3.00 vs.
6.00a | 9.00 vs. 12.00 | (17) |
| Xiong et al,
2020 | 100.00 vs.
100.00 | 121.97 vs.
698.67a | NA | 10.04 vs.
13.75a | 1.62 vs. 1.65 | (19) |
|
| 100.00 vs.
100.00 | 125.53 vs.
102.94a | NA | 10.21 vs.
12.56a | 2.34 vs. 0.00 |
|
| Stanek et
al, 2019 | 100.00 vs.
100.00 | 100.00 vs.
95.00 | 25.00 vs.
175.00a | 3.00 vs.
9.00a | 4.30 vs. 0.00 | (18) |
| Mazer et al,
2021 | 100.00 vs.
95.83 | 117.00 vs.
104.00 | NA | 3.00 vs.
7.00a | 1.88 vs. 8.33 | (25) |
The duration of follow-up was reported in 11
entries, ranging from 32 to 64 months in the laparoscopic groups,
and 25 to 67 months in the open resection groups. No significant
differences were reported in terms of recurrence rate. Only four
entries reported on DFS, two of which did not detect any
significant differences (19,22).
Furthermore, one entry reported a significantly longer DFS in the
laparoscopic group (19), wheras
another entry reported the opposite (24). Similar results were reported in OS,
with two studies reporting insignificant differences (17,19), one
in favour of the laparoscopic approach (19) and one in favour of the open resection
approach (24). Five entries
presented the 5-year recurrence-free survival rate; however, no
statistically significant differences were detected. Similarly, six
entries reported mortality rate, again without any significant
differences. Finally, five studies reported on the 5-year survival
rate, demonstrating no significant difference between the two
groups. The latter ranged from 93.1 to 100% in the laparoscopic
groups, and from 85.9 to 98.75% in the open resection groups.
Table III presents long-term
outcomes in detail.
 | Table III.Follow-up and long-term outcomes. |
Table III.
Follow-up and long-term outcomes.
| Author, year | F-up, median
months, lap vs. open | Recurrence, %, lap
vs. open | DFS, median months,
lap vs. open | 5-year
recurrence-free survival rate, %, lap vs. open | Mortality, %, lap
vs. open | OS, median months,
lap vs. open | 5-year survival
rate, %, lap vs. open | (Refs.) |
|---|
| Chen et al,
2016 | 35.00 vs.
35.00 | 6.80 vs. 13.60 | NA | 82.20 vs.
86.10 | NA | NA | 95.40 vs.
85.90 | (23) |
|
| 36.00 vs.
36.00 | 8.50 vs. 7.00 | NA | 82.50 vs.
91.90 | NA | NA | 93.10 vs.
91.90 |
|
| Hu et al,
2016 | 32.00 vs.
34.20 | 13.18 vs.
21.17 | NA | NA | 4.00 vs. 7.00 | NA | NA | (16) |
| Xu et al,
2017 | NA | 0.00 vs. 4.50 | 98.30 vs.
98.10 | NA | 2.30 vs. 4.50 | NA | 100.00 vs.
95.00 | (22) |
| Chi et al,
2017 | 64.00 vs.
67.00 | 9.52 vs. 15.87 | NA | 92.10 vs.
88.90 | 6.35 vs. 7.94 | NA | NA | (21) |
| Huang et al,
2017 | 40.00 vs.
40.00 | NA | NA | NA | NA | NA | NA | (20) |
|
| 40.00 vs.
40.00 | NA | NA | NA | NA | NA | NA |
|
| Ye et al,
2017 | NA | NA | NA | NA | NA | NA | NA | (24) |
|
| 35.30 vs.
40.99 | 3.75 vs. 5.00 | 97.04 vs.
111.61a | 97.50 vs.
96.25 | 1.25 vs. 2.50 | 99.65 vs.
115.26a | 98.75 vs.
98.75 |
|
| Wakamatsu, et
al, 2018 | 32.60 vs.
24.70 | 0.00 vs. 8.33 | NA | NA | 3.07 vs. 8.33 |
Non-significant | NA | (17) |
| Xiong et al,
2020 | 43.00 vs.
43.00 | NA |
lap>opena | NA | NA |
Lap>opena | NA | (19) |
|
| 43.00 vs.
43.00 | NA |
non-significant | 93.90 vs.
81.70 | NA |
Non-significant | 95.90 vs.
89.70 |
|
| Stanek et
al, 2019 | 57.00 vs.
57.00 | 0.00 vs. 22.72 | NA | NA | 13.63 vs. 2.17 | NA | NA | (18) |
| Mazer et al,
2021 | NA | NA | NA | NA | NA | NA | NA | (25) |
Objective evaluation
All 10 studies were evaluated and scored according
to the modified MINORS criteria, which produces an overall score
from 0 to 18. The lowest score awarded to a study was 5, and the
highest awarded study score was 15. When the full scoring spectrum
was divided in quartiles, the first quartile included one study
(25). The remaining three quartiles
included three studies each. Three studies would be included in the
top quartile with scores 14 (21),
15 (22) and 15 (24), respectively. Table IV presents this evaluation in
further detail. Regarding controversial findings on perioperative
data, all three top-quartile studies had reported statistical
significance in favour of the laparoscopic approach. The study that
had reported significantly improved findings in the open resection
group received a grade of 12 and was thus included in the next
quartile. Regarding discrepancies in long-term outcomes, two of the
top quartile studies had detected no statistically significant
differences, while the third study of the top quartile, which
conducted a propensity score matched analysis, reported
significantly improved DFS and OS in the open resection group
(24). Furthermore, the study that
reported significantly improved DFS and OS for the laparoscopic
group was allocated a score of 12 and had the largest sample size
(426 patients) (19). However, in
the same study, when propensity score matching was implemented,
statistical significance was lost. In terms of scoring, a lack of
reporting on the number of patients lost to follow up was a
consistent reason for lost points; none of the included studies
mentioned a relevant number. The second most common reason for lost
points was study design, since only one study was prospective.
 | Table IV.Evaluation of included studies
according to MINORS criteria. |
Table IV.
Evaluation of included studies
according to MINORS criteria.
| Author, year | Study aim | Consecutive
patients | Data collection
methodology | Reported
endpoints | Outcome evaluation
bias | Equivalent
groups | Statistical
methods | Follow-up
period | Patients lost to
follow-up | Total | (Refs.) |
|---|
| Chen et al,
2016 | 1 | 0 | 1 | 2 | 2 | 2 | 2 | 2 | 0 | 12 | (23) |
| Hu et al,
2016 | 2 | 1 | 2 | 1 | 0 | 0 | 2 | 1 | 0 | 9 | (16) |
| Xu et al,
2017 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 0 | 15 | (22) |
| Chi et al,
2017 | 2 | 2 | 1 | 2 | 1 | 2 | 2 | 2 | 0 | 14 | (21) |
| Huang et al,
2017 | 2 | 0 | 1 | 2 | 1 | 0 | 2 | 2 | 1 | 11 | (20) |
| Ye et al,
2017 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 0 | 15 | (24) |
| Wakamatsu et
al, 2018 | 2 | 0 | 1 | 2 | 0 | 0 | 2 | 1 | 0 | 8 | (17) |
| Xiong et al,
2020 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | 0 | 12 | (19) |
| Stanek et
al, 2019 | 2 | 0 | 1 | 2 | 0 | 0 | 2 | 1 | 0 | 8 | (18) |
| Mazer et al,
2021 | 0 | 0 | 1 | 2 | 0 | 0 | 2 | 0 | 0 | 5 | (25) |
Historical and current topics
Since the first publication of laparoscopic GIST
resection (26), ~30 years have
passed, during which a marked number of studies have been
published. However, questions remain regarding other indications
for surgery. The early focus of research was the feasibility and
safety of laparoscopic GIST resection. Although studies of cohorts
within the previous decade demonstrated encouraging results, the
evidence for feasibility and safety was sparse, with specific
tumour features, such as size and location, appearing to mitigate
reported advantages (27). This was
attributed to performance bias, as surgeons were still learning how
to conduct this procedure. A large multicentre study by Piessen
et al (28) in 2015 provided
a sound confirmation regarding the feasibility and safety of
laparoscopic GIST resection, even for tumours that were >8 cm.
Another unaddressed issue that required reliable clarification was
whether laparoscopic resection demonstrated oncological inferiority
compared with open resection. Recent studies have reported
minimally invasive resections of malignant lesions, where
disadvantages were identified over the open resection approach
(29). Laparoscopic surgery
performed on patients with gastric cancer, where a number of
technical parameters influence long-term outcomes, has been
received with scepticism. The IMIGASTRIC study was designed to
investigate the oncological outcomes of minimally invasive
resections in gastric cancer, based on a multicentre, prospective
registry (30). Studies over the
past decade have consistently reported on long-term and oncological
outcomes following laparoscopic GIST resection in recognition of
the clinical importance of this approach.
In the absence of randomized controlled trials,
conclusions need to be drawn based on the findings of
single-centre, retrospective studies. Hence, the present study
aimed to conduct an objective and critical review of current
evidence. Over the past 5 years, 10 studies were identified that
reported a comparison between laparoscopic and open GIST resection
without focusing on tumour size. The current results confirmed that
the laparoscopic approach was feasible and safe. The reported
conversion rate was 0 in most studies and in the three that
reported a higher rate, this value never exceeded 10% (17,25).
This is encouraging considering the reported average conversion
rate of 10.1% for laparoscopic gastrectomy (31) and 14% for major colorectal surgery
(32). It is also important to
highlight that the aforementioned studies reporting a conversion
rate of >0 were those that had the smallest sample size and the
lowest MINORS score. In terms of postoperative complications, the
majority of studies and especially those with higher MINORS scores,
reported a Dindo-Clavien III–IV complication rate of ~2% which is
well below the respective rate in major colorectal and gastric
surgery (31,32). Data on procedure duration,
intra-operative blood loss and length of stay were almost
consistently in favour of the laparoscopic approach. As most
surgeons that perform these types of procedures are now well into
the plateau phase of their practical training, operation duration
is ~2 h on average, blood loss does not exceed 100 ml and length of
hospital stay does not exceed 10 days on average, which on most
occasions was 2–3 days shorter than respective open resection
groups.
With regards to the more topical questions of
long-term outcomes, it should be stated that only one study
followed-up patients for >5 years (21). Regarding the outcomes of 5-year
survival and 5-year recurrence free survival, only this single
study provided reliable results (21). Unfortunately, this study reported
only on 5-year recurrence free survival, which was 92.1% for the
laparoscopic group and 88.9% for the open resection group, with a
sample size of 126 patients. This difference was statistically
insignificant. It can be argued that 5-year survival should be
fairly high, given that patients have effective treatment options
even after recurrence. In fact, the studies that did examine 5-year
survival reported rates of 93–100% for the laparoscopic group and
86–99% for the open resection group; however, this difference was
not statistically significantly different. Two of these studies had
a sample size of >200 patients and MINORS scores of 12 (19,23).
Only one study reported DFS and OS in detail (24). With a propensity score derived from
160 patients, this study presented a median DFS of 97 months and a
median OS of ~100 months. However, the respective numbers for the
open resection group were 112 and 115 months, respectively, making
the DFS significantly higher than that of laparoscopic group. This
is the only study that reported a significantly improved long-term
outcome for the open resection group. In a study by Xiong et
al (19) comprising 426
patients, significantly improved DFS and OS was reported for the
laparoscopic group. However, these results should be considered
with scepticism, as firstly no exact numbers were reported and
secondly, when propensity score matching was implemented on the
same cohort, this statistical significance was removed. This may
mean that bias existed, and consequently results from propensity
score matched analyses should be considered more reliable in this
setting.
Conclusions and limitations
Overall, there was an even distribution of studies
across the MINORS scoring system. The most common reason for missed
points was reporting loss to follow-up. This is a consistent issue
with retrospective studies; however, it is also an index of good
practice, from a clinical and research point of view. Particularly
when examining long-term outcomes, it is important to implement an
adequately long follow-up period as well as to limit or at least
report the number of patients that were lost to follow-up. A
minimum follow-up of 5 years and a loss to follow-up of <5% are
the ideal targets. Another consistent issue with the studies
assessed in the current review was design and data collection. It
is inevitable that retrospective studies will suffer from various
types of bias. Moreover, in the context of follow-up and subsequent
treatments, there was also an inconsistency regarding the
management of metastatic disease, which certainly affects overall
outcomes. Specifically, although the general consensus is that
patients with metastatic disease should be treated with systematic
chemotherapy, it is argued that for patients with oligometastatic
disease and a good response to systematic treatment, metastasectomy
might be of benefit (33).
Accordingly, such a stratification needs to be resolved in future
studies. All the above methodological concerns can be limited by
designing a prospective study with pre-agreed perioperative
protocols and data collection pro formas. Propensity score matching
is also a method that can compensate for certain types of bias, as
explained above. Therefore, an ideal assessment would be performed
as a randomized controlled study; however, the rarity of these
lesions would certainly involve a multicentre design.
Several other questions were posed in the literature
but were not examined in the present study, either because they
were outside its scope or because there were not enough data. One
key point is tumour size. Although studies have confirmed the
safety of laparoscopic resections of tumours >5 cm, which was
initially considered a cut-off, larger lesions are now being
treated in this manner, despite there being an unknown oncological
impact. Of the examined studies, two included tumours >10 cm
(19,23). The results of these studies were
comparable to those of studies including smaller tumours; however,
a stratification based on size is lacking in the literature and
would yield interesting results. Moreover, surgical technique
varied among studies. In certain articles, a combined endoscopic
and laparoscopic approach was implemented (20). Authors argue that this approach
improved the localization of tumours and improved perioperative
outcomes. However, the examined comparison was between
endoscopic/laparoscopic resection vs. open resection. The design
that would answer the question of whether endoscopy significantly
improves outcomes would involve a comparison between
endoscopic/laparoscopic resection vs. laparoscopic resection alone.
These two important aspects should be reported in an objective and
detailed manner in future studies to acquire more evidence.
Since this was a systematic review of non-randomized
studies, a quantitative conclusion cannot be drawn. The
heterogeneity of study design, the frequent shortcomings of
reported studies and the inconsistencies in reporting relevant
outcomes, limit the clinical implementation of the present result.
However, the present review confirmed the perioperative advantages
of GIST laparoscopic resection, which was a consistent finding
among most included studies. Moreover, the current study identified
discrepancies in regard to oncological outcomes and attempted to
grade the reliability of relevant studies, concluding that one
study that questioned the oncological safety of laparoscopic
resection may be considered more reliable than those that supported
opposite findings. Finally, the current study emphasized the most
important shortcomings of current literature, including follow-up
and study design, and provided suggestions for the improvement of
further studies to produce more credible evidence.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
CI and NN conceived the present study. PML and DD
designed this study. The literature search was carried out by CI
and CT. Disagreements were resolved by PML. The manuscript was
drafted by CI and NM. Manuscript revisions and modifications were
carried out by ES and PK. Final changes were made by EP and NN. All
authors have read and approved the final manuscript. Data
authentication is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Biondi A, Di Stefano C, Ferrara F, Bellia
A, Vacante M and Piazza L: Laparoscopic versus open appendectomy: A
retrospective cohort study assessing outcomes and
cost-effectiveness. World J Emerg Surg. 11:442016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Russ AJ, Obma KL, Rajamanickam V, Wan Y,
Heise CP, Foley EF, Harms B and Kennedy GD: Laparoscopy improves
short-term outcomes after surgery for diverticular disease.
Gastroenterology. 138:2267–2274, 2274.e1. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dokmak S, Raut V, Aussilhou B, Ftériche
FS, Farges O, Sauvanet A and Belghiti J: Laparoscopic left lateral
resection is the gold standard for benign liver lesions: A
case-control study. HPB (Oxford). 16:183–187. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Liu Z, Ding H, Xiong X and Huang Y:
Laparoscopic left lateral hepatic sectionectomy was expected to be
the standard for the treatment of left hepatic lobe lesions: A
meta-analysis. Medicine (Baltimore). 97:e98352018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Powell MS and Fernandez AZ Jr: Surgical
treatment for morbid obesity: The laparoscopic Roux-en-Y gastric
bypass. Surg Clin North Am. 911203–1224. (viii)2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lianos GD, Rausei S, Ruspi L, Galli F,
Mangano A, Roukos DH, Dionigi G and Boni L: Laparoscopic
gastrectomy for gastric cancer: Current evidences. Int J Surg.
12:1369–1373. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Colon Cancer Laparoscopic or Open
Resection Study Group, ; Buunen M, Veldkamp R, Hop WC, Kuhry E,
Jeekel J, Haglind E, Påhlman L, Cuesta MA, Msika S, et al: Survival
after laparoscopic surgery versus open surgery for colon cancer:
Long-term outcome of a randomised clinical trial. Lancet Oncol.
10:44–52. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yu J, Huang C, Sun Y, Su X, Cao H, Hu J,
Wang K, Suo J, Tao K, He X, et al: Effect of laparoscopic vs. open
distal gastrectomy on 3-year disease-free survival in patients with
locally advanced gastric cancer: The CLASS-01 randomized clinical
trial. JAMA. 321:1983–1992. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mathis KL and Nelson H: Controversies in
laparoscopy for colon and rectal cancer. Surg Oncol Clin N Am.
23:35–47. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
DeMatteo RP, Lewis JJ, Leung D, Mudan SS,
Woodruff JM and Brennan MF: Two hundred gastrointestinal stromal
tumors: Recurrence patterns and prognostic factors for survival.
Ann Surg. 231:51–58. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ronellenfitsch U and Hohenberger P:
Surgery for gastrointestinal stromal tumors: State of the art of
laparoscopic resection and surgery for M1 tumors. Visc Med.
34:367–374. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Casali PG, Abecassis N, Aro HT, Bauer S,
Biagini R, Bielack S, Bonvalot S, Boukovinas I, Bovee JVMG,
Brodowicz T, et al: Gastrointestinal stromal tumours: ESMO-EURACAN
clinical practice guidelines for diagnosis, treatment and
follow-up. Ann Oncol. 29 (Suppl 4):iv68–iv78. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
von Mehren M, Randall RL, Benjamin RS,
Boles S, Bui MM, Ganjoo KN, George S, Gonzalez RJ, Heslin MJ, Kane
JM, et al: Soft tissue sarcoma, version 2.2018, NCCN clinical
practice guidelines in oncology. J Natl Compr Canc Netw.
16:536–563. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Dindo D, Demartines N and Clavien PA:
Classification of surgical complications: A new proposal with
evaluation in a cohort of 6336 patients and results of a survey.
Ann Surg. 240:205–213. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lykoudis PM, O'Reilly D, Nastos K and
Fusai G: Systematic review of surgical management of synchronous
colorectal liver metastases. Br J Surg. 101:605–612. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hu J, Or BH, Hu K and Wang ML: Comparison
of the post-operative outcomes and survival of laparoscopic versus
open resections for gastric gastrointestinal stromal tumors: A
multi-center prospective cohort study. Int J Surg. 33:65–71. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wakamatsu K, Lo Menzo E, Szomstein S, Seto
Y, Chalikonda S and Rosenthal RJ: Feasibility of laparoscopic
resection of gastrointestinal stromal tumor of the stomach. J
Laparoendosc Adv Surg Tech A. 28:569–573. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Stanek M, Pisarska M, Budzyńska D, Rzepa
A, Pędziwiatr M, Major P and Budzyński A: Gastric gastrointestinal
stromal tumors: Clinical features and short- and long-term outcomes
of laparoscopic resection. Wideochir Inne Tech Maloinwazyjne.
14:176–181. 2019.PubMed/NCBI
|
|
19
|
Xiong Z, Wan W, Zeng X, Liu W, Wang T,
Zhang R, Li C, Yang W, Zhang P and Tao K: Laparoscopic versus open
surgery for gastric gastrointestinal stromal tumors: A propensity
score matching analysis. J Gastrointest Surg. 24:1785–1794. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Huang JL, Zheng ZH, Wei HB, Chen TF, Liu
JP, Huang Y, Wei B and Fang JF: Endoscopy-assisted laparoscopic
resections for gastric gastrointestinal stromal tumors: A
retrospective study. J Laparoendosc Adv Surg Tech A. 27:110–114.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chi JL, Xu M, Zhang MR, Li Y and Zhou ZG:
Laparoscopic versus open resection for gastric gastrointestinal
stromal tumors (GISTs): A size-location-matched case-control study.
World J Surg. 41:2345–2352. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Xu C, Chen T, Hu Y, Balde AI, Liu H, Yu J,
Zhen L and Li G: Retrospective study of laparoscopic versus open
gastric resection for gastric gastrointestinal stromal tumors based
on the propensity score matching method. Surg Endosc. 31:374–381.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chen QF, Huang CM, Lin M, Lin JX, Lu J,
Zheng CH, Li P, Xie JW, Wang JB, Chen QY, et al: Short- and
long-term outcomes of laparoscopic versus open resection for
gastric gastrointestinal stromal tumors: A propensity
score-matching analysis. Medicine (Baltimore). 95:e31352016.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ye X, Kang WM, Yu JC, Ma ZQ and Xue ZG:
Comparison of short- and long-term outcomes of laparoscopic vs.
open resection for gastric gastrointestinal stromal tumors. World J
Gastroenterol. 23:4595–4603. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mazer L, Worth P and Visser B: Minimally
invasive options for gastrointestinal stromal tumors of the
stomach. Surg Endosc. 35:1324–1330. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lukaszczyk JJ and Preletz RJ Jr:
Laparoscopic resection of benign stromal tumor of the stomach. J
Laparoendosc Surg. 2:331–334. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Goh BK, Goh YC, Eng AK, Chan WH, Chow PK,
Chung YF, Ong HS and Wong WK: Outcome after laparoscopic versus
open wedge resection for suspected gastric gastrointestinal stromal
tumors: A matched-pair case-control study. Eur J Surg Oncol.
41:905–910. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Piessen G, Lefèvre JH, Cabau M, Duhamel A,
Behal H, Perniceni T, Mabrut JY, Regimbeau JM, Bonvalot S, Tiberio
GA, et al: Laparoscopic versus open surgery for gastric
gastrointestinal stromal tumors: What is the impact on
postoperative outcome and oncologic results? Ann Surg. 262:831–839,
829-840. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chen X, Zhao N, Ye P, Chen J, Nan X, Zhao
H, Zhou K, Zhang Y, Xue J, Zhou H, et al: Comparison of
laparoscopic and open radical hysterectomy in cervical cancer
patients with tumor size ≤2 cm. Int J Gynecol Cancer. 30:564–571.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Desiderio J, Jiang ZW, Nguyen NT, Zhang S,
Reim D, Alimoglu O, Azagra JS, Yu PW, Coburn NG, Qi F, et al:
Robotic, laparoscopic and open surgery for gastric cancer compared
on surgical, clinical and oncological outcomes: A
multi-institutional chart review. A study protocol of the
international study group on minimally invasive surgery for GASTRIc
cancer-IMIGASTRIC. BMJ Open. 5:e0081982015. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Yue F and Geng X: Impact of conversion
during laparoscopic gastrectomy on outcomes of patients with
gastric cancer. J BUON. 22:926–931. 2017.PubMed/NCBI
|
|
32
|
2017 and 2015 European Society of
Coloproctology (ESCP) collaborating groups, . The impact of
conversion on the risk of major complication following laparoscopic
colonic surgery: An international, multicentre prospective audit.
Colorectal Dis. 20 (Suppl 6):S69–S89. 2018. View Article : Google Scholar
|
|
33
|
Kikuchi H, Hiramatsu Y, Kamiya K, Morita
Y, Sakaguchi T, Konno H and Takeuchi H: Surgery for metastatic
gastrointestinal stromal tumor: To whom and how to? Transl
Gastroenterol Hepatol. 3:142018. View Article : Google Scholar : PubMed/NCBI
|