Introduction
According to global cancer statistics, the incidence
of oral cancer is >300,000 cases and it causes 145,400
cancer-associated deaths annually (1). The most widespread malignant tumor of
the mouth is squamous cell carcinoma, which occurs in 80–90% of all
oral cancer cases (2). Currently,
the treatment methods of squamous cell carcinoma include surgery,
chemotherapy, radiation therapy, immunotherapy and targeted
therapy. These treatment methods have their respective applications
and roles in the treatment process. Surgical resection is a key
treatment method for tumors of the oral cavity and oropharynx
(3–5). However, as noted by various studies,
after tumor resection, the presence of residual tumor cells is
frequent, which usually leads to tumor recurrence (6–8). The
aim of the present study was not to discuss the preferences
regarding the selection of surgical methods of oral squamous cell
carcinoma treatment, nor the role of surgical margins, tumor
location, size and depth, and histological differentiation, since
these aspects have already been described by multiple studies in
detail (9–11). The present study focused instead on
controlled drug delivery systems. It was hypothesized that,
following tumor resection, a gel-based targeted drug delivery
system would prevent metastasis formation. For this purpose, a
biocompatible two-layer multicomponent fibrin-based gel (MCPFTG)
was developed. The efficacy of MCPFTG was assessed in a rat model
of squamous cell carcinoma of the tongue constructed using
4-nitroquinoline 1-oxide (4NQO).
Materials and methods
Creation of the multicomponent
gel
A multicomponent gel was created by slightly
modifying a previously published protocol for creating polyethylene
glycol (PEG)-fibrin gel, which was developed by Zhang et al
(12). TBS (40 mg/ml; pH 7.8) and
250 µl PEG were added to 500 µl commercially purchased fibrinogen
(MilliporeSigma). The acquired compound was then placed in a
Falcon® 24-well Companion Plate (Falcon; Corning Life
Sciences) and incubated at 37°C with 5% CO2 and 90%
humidity for 20 min. The compound that was generated through this
method was called pegylated fibrinogen (PGF).
Preparation of cisplatin-loaded
CultiSpher-S (CPtCS) microcarrier
A total of 0.1 g commercially purchased microcarrier
CultiSpher-S (MilliporeSigma) was placed in 5.0 ml cisplatin
solution (KOÇAK Farma), and 3.0 ml 1% sodium citrate was added. The
solution was then placed in a spinner flask, and stirred at 200 × g
for 4 h at room temperature. Subsequently, the solution was
transferred to a 50-ml Falcon test tube (Falcon; Corning Life
Sciences), where 15 ml cisplatin solution was added, and
subsequently centrifuged at a 10,000 × g for 10 min at 40°С. After
removing the supernatant, CPtCS was placed in a freeze dryer (Power
Dry PL 6000 Freeze Dryer; Heto Lab Equipment). At first, the shelf
temperature was set at −32°C, and the vacuum was controlled under
10 Pa. The drying process lasted for 16 h. The shelf was then
heated up to 20°C at a rate of 0.2°C/min and held for 6 h. When the
process was completed, CPtCS was stored under sterile conditions at
room temperature until further use.
Preparation of bone marrow stem cell
(BMSC)-loaded CultiSpher-S microcarrier
BMSCs were acquired as previously described
(13). Briefly, 20 Lewis inbred
laboratory rats of both sexes weighing 200–250 g were used in the
present study. Animals were euthanized with thiopental sodium
(MilliporeSigma) with an intraperitoneal dose of 200 mg/kg. The
lower extremities were amputated after being treated with 70%
ethanol solution. Femurs, which were cleared of muscle tissues,
were resected in the epiphysis and diaphysis areas. A needle was
inserted into the lumen of the bone canal, and a syringe was used
to elute the bone marrow with DMEM (MilliporeSigma). The
mononuclear fraction was isolated by density gradient
centrifugation at 400 × g for 30 min at room temperature using
Ficoll Paque Plus or Ficoll Paque Premium solution (GE Healthcare
Bio-Sciences). After being washed with PBS, the cells were
centrifuged at 200 × g at 24°C for 5 min. Together with 0.1 g
microcarrier CultiSpher-S, the acquired stem cells were placed in
12 of the wells of a Falcon 24-well Companion Plate (Falcon;
Corning Life Sciences), and incubated at 37°C with 5%
CO2 and 90% humidity for 1 h. DMEM, 10% FBS
(MilliporeSigma), 50 U/ml penicillin and 0.05 mg/ml streptomycin
was used as the cell culture medium. An orbital shaker (110 rpm),
onto which a plate was placed, was then introduced into the
incubator. The cells were co-cultured with CultiSpher-S for 7 days.
The culture medium was changed every 3 days. Upon culture,
CultiSpher-S and BMSCs were placed in a freeze drier for
lyophilization, and then stored under sterile conditions at a room
temperature until further use.
For creating an external layer of the gel, 500 µl
fibrinogen, 250 µl PEG, 0.1 g microcarrier CultiSpher-S and 0.5 mg
cisplatin were used. For the creation of the internal layer, 500 µl
fibrinogen, 250 µl PEG, 0.1 g microcarrier CultiSpher-S and
2.5×106 freeze-dried BMSCs were used.
Rat model of squamous cell carcinoma
of the tongue
A total of 60 male specific pathogen-free Lewis
laboratory rats, (age, 8 weeks; weight, ~250 g), were used for
establishing a model of squamous cell carcinoma of the tongue. The
animals were acquired from the vivarium of Tbilisi State Medical
University (Tbilisi, Georgia). The rats were maintained under
controlled conditions at 24±2°C using a 12-h light-dark cycle and
with free access to water and food. The studies were performed in
accordance with the recommendations of the Animal Care and Use
Committee of Tbilisi State Medical University. All animal protocols
were approved by a recognized institutional review board (Tbilisi
State Medical University; approval no. 812).
For establishing a model of squamous cell carcinoma
of the tongue in rats, 4NQO powder (MilliporeSigma) was used, which
was dissolved in the drinking water of the animals to a final
concentration of 0.02 g/l (20 ppm). The water was changed on a
weekly basis (14). Notably, 4NQO
is widely used to study oral carcinogenesis in animals (15,16),
as it can lead to induction of all phases of oral carcinogenesis
(including hyperplasia, dysplasia, acute dysplasia, carcinoma in
situ and squamous cell carcinoma).
Methods of treatment of squamous cell
carcinoma of the tongue in rats
After successful modeling, the 60 rats were divided
into three groups: Group I, 4-NQO untreated controls (n=20); group
II, 4-NQO + surgery (n=20); and group III, 4-NQO + surgery + MCPFTG
(n=20).
At 2 months after the initiation of the animal
model, 85% of each squamous cell carcinoma tumor was removed in the
animals of the second group, and the 0.4-0.6-cm diameter wound was
closed with knotted 7.0 atraumatic sutures (Ethicon, Inc.; Johnson
& Johnson).
In the animals of the third group, at 2 months from
the beginning of modeling, 85% of each squamous cell carcinoma
tumor was also removed, and MCPFTG was introduced into the
0.4-0.6-cm diameter wound. Initially, the wound was covered with
PGF gel that contained CPtCS (internal layer). Next, a solution
containing 1.0% calcium chloride and 52 U/ml thrombin
(MilliporeSigma) diluted in saline solution was added to the PGF
gel. While merging, a glutinous mass was formed between these two
components, and it became transparent within 5–6 sec. PGF that was
seeded with CultiSpher-S + BMSCs was placed on top of the internal
layer, while a solution containing 1.0% calcium chloride and 52
U/ml thrombin was used for solidifying the external layer.
All surgical procedures were conducted under general
anesthesia using intraperitoneal injection of pentobarbital sodium
(30 mg/kg).
Postoperative care
Animals were housed in standard laboratory
conditions under normal day and night cycles with provision of
pelleted rodent diet and water ad libitum. During the
postoperative period, the rate of wound healing was determined
using the planimetric method.
On days 30, 40, 60, 90, 120 and 150 after surgery,
the rats were euthanized with a lethal dose (200 mg/kg) of sodium
thiopental solution via intraperitoneal injection. At necropsy,
full thickness skin samples covering the jaw and neck, including
subcutaneous tissue and tissue of the tongue with a tumor were
excised for histopathological studies.
Scanning electron microscopy
Scanning electron microscopy was performed as
previously described (17).
Briefly, the collected wound tissues were immersed in a fixative
solution containing 2.5% glutaraldehyde and 4% paraformaldehyde in
0.1 M of phosphate buffer. After fixation, the samples were
dehydrated in 30, 50, 70, 80 and 90% ethanol (for 10 min each) and
twice in 95% ethanol (20 min each) in succession at room
temperature. The samples were then immersed in a mixture of 95%
ethanol and isoamyl acetate (1:1) for 10 min, and in pure isoamyl
acetate for 15 min. After removing isoamyl acetate, the samples
were dried with a Tousimis Samdri-780 Critical Point Dryer
(Tousimis Research Corporation). Next, the tissues were sputter
coated lightly with gold and imaged on a JEOL JSM-65 10 LW scanning
electron microscope (JEOL, Ltd.).
Energy dispersive spectroscopy
Energy dispersive spectroscopy was used to determine
the quantity of CPtCS in the MCPFTG before and after it was applied
to the wound. For energy dispersive analysis of the results of
scanning electron microscopy, the analytical AztecEnergy-EDS
software (Oxford Instruments, Inc.) and the X-MaxN SDD detector
(Oxford Instruments, Inc.) were used.
Method of determination of wound
healing speed
For an objective assessment of wound healing speed,
and to acknowledge the changes in size of the wound within a
certain period of time, the method of planimetry was used in all
animals. For this purpose, a sheet of cellophane sterilized in an
autoclave was applied to the wound, on which the contours of the
wound were outlined with ink. Next, the cellophane with the
outlined contour was placed on a paper denoting mm, and the area of
the wound was determined by counting the number of mm2
inside the contour. The percentage of daily wound reduction was
determined by using the following formula: [(S - Sn) × 100] / (S ×
t), where S is the wound area during any subsequent measurement, Sn
is the wound area during the current measurement and t is the
number of days between the measurements.
Tumor volume determination, and
histopathological and immunohistochemical analyses
After establishing a rat model of squamous cell
carcinoma of the tongue, the tumor volume was measured during the
autopsy after collection of material for histopathological analysis
at various time points. The tumor volume was calculated according
to the formula: Volume = length × width × height × (π/6).
For histopathological studies, the tongue tumor and
its surrounding tissues were fixed in 10% neutral buffered formalin
for 24 h at room temperature, embedded in paraffin and cut into
5-µm thick slices. After deparaffinization and rehydration, the
tissues were stained with hematoxylin and eosin (Leica Biosystems
Newcastle Ltd.), and Masson's trichrome (Bio-Optica Ltd.), at room
temperature for 35 min according the manufacturers' protocols.
Immunostaining with anti-p63 (incubation time, 20 min; clone 7JUL;
dilution 1:25; cat. no. PA0103; Leica Biosystems Newcastle Ltd.),
anti-Ki67 (incubation time, 20 min; clone MM1; dilution 1:200; cat.
no. PA0118; Leica Biosystems Newcastle Ltd.), anti-cyclin D1
(incubation time, 20 min; clone EP12; dilution 1:50; cat. no.
PA0046; Leica Biosystems Newcastle Ltd.) and anti-E cadherin
(incubation time, 20 min; clone 36B5; dilution 1:25; cat. no.
PA0387; Leica Biosystems Newcastle Ltd.) antibodies was performed
with the manual staining method using the Novolink DAB Polymer
Detection system (incubation time, 20 min; cat no. RE7260-CE; Leica
Biosystems Newcastle Ltd.) according to the manufacturer's
recommendations. Endogenous peroxidase activity was neutralized
using the Peroxidase Block reagent [3–4% (v/v) hydrogen peroxide;
Novolink DAB Polymer Detection system; cat. no. RE7260-CE; Leica
Biosystems Newcastle Ltd]. To reduce non-specific binding of
primary antibody Novocastra Protein Block reagent was used (0.4%
casein in phosphate-buffered saline, with stabilizers, surfactant
and 0.2% Bronidox L as a preservative; Novolink DAB Polymer
Detection system). As the secondary antibody, rabbit anti-mouse IgG
(<10 µg/ml) in 10% (v/v) animal serum in Tris-buffered
saline/0.1% ProClin™ 950 was used (Novolink DAB Polymer Detection
system). All reactions for immunohistochemistry were performed at
room temperature. The samples were next observed under a light
microscope. For image capture, the LAS V4.0 (Leica Microsystems
Ltd.) software was used. Images than was analyzed using ImageJ
v1.51 (National Institutes of Health). Percentage of positive
nuclei were counted using the ImmunoRatio macros plugin for ImageJ.
Intensity of cytoplasmic staining was evaluated by a 4-tier visual
scoring method (0, no staining; 1+, weak; 2+, moderate; and 3+,
strong ).
Statistical analysis
Statistical analysis was performed using GraphPad
Prism 9.0 software (GraphPad Software, Inc.). Tumor growth was
calculated and compared between groups for each time point, and
statistical analysis was assessed with one-way ANOVA followed by
Tukey's post hoc test. All experiments were repeated at least three
times. P<0.05 was considered to indicate a statistically
significant difference.
Results
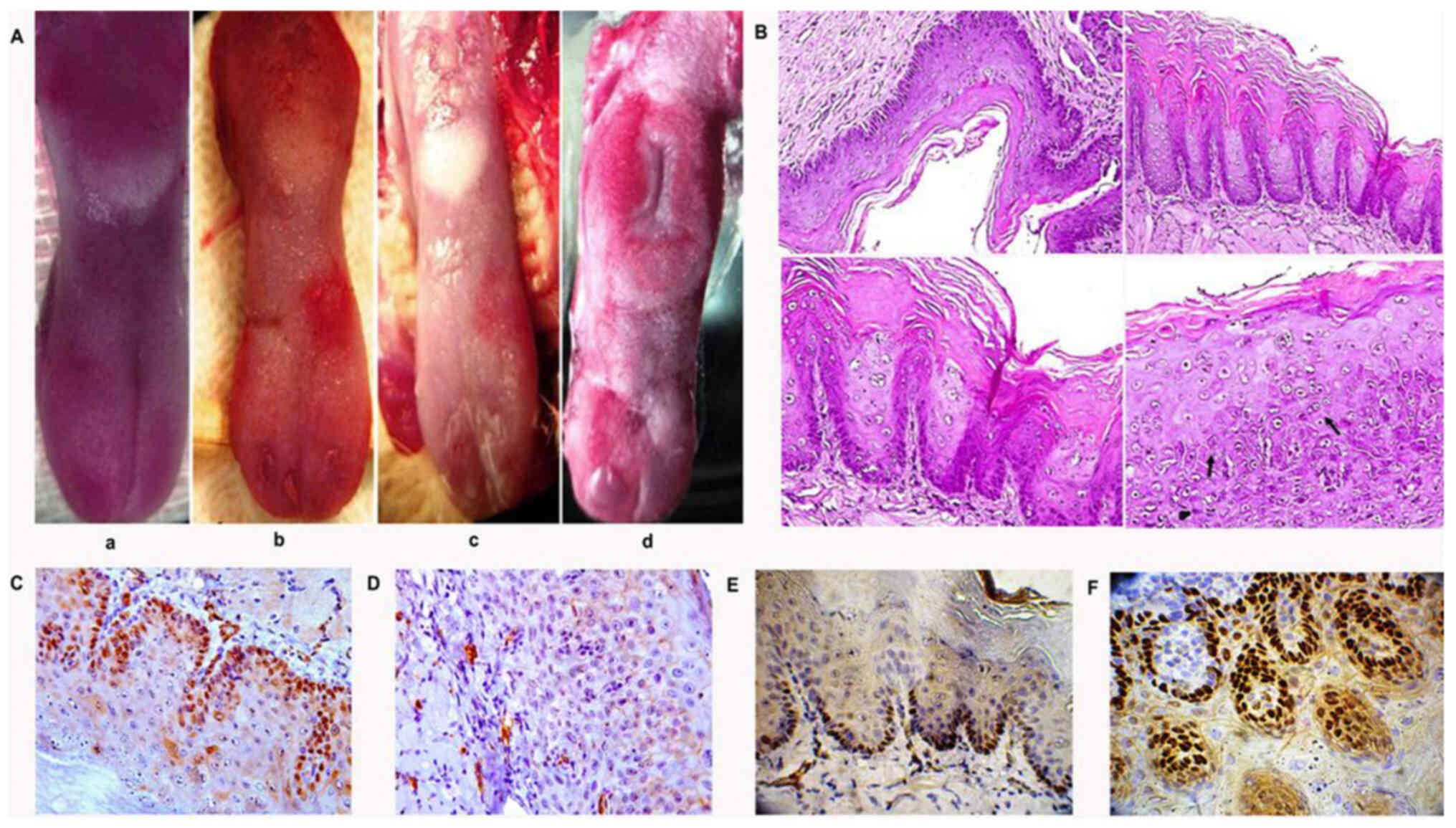
At 2 months after the creation of a model of
squamous cell carcinoma in 60 rats on the surface of the tongue, a
well-defined carcinoma in situ was visible, the presence of which
was confirmed by histopathological and immunohistochemical methods.
(Fig. 1).
Loss of epithelial cell polarity, nuclear
polymorphism and hyperchromatism were evident in the tissue of the
tongue. Abnormal keratinization (dyskeratosis) of individual cells,
cytological disorganization and abnormal mitosis without mucous
membrane invasion were also observed. Inflammatory cells were
detected in the connective tissue. Dysplasia, as well as
hyperplasia and carcinoma in situ, were identified at
different time points in all groups of animals. High expression of
cyclin D1 and low expression of E-cadherin were revealed by
immunohistochemistry. At a later period, 3.5–4 months after
initiation of the model, a well differentiated squamous cell
carcinoma with signs of keratin formation was observed.
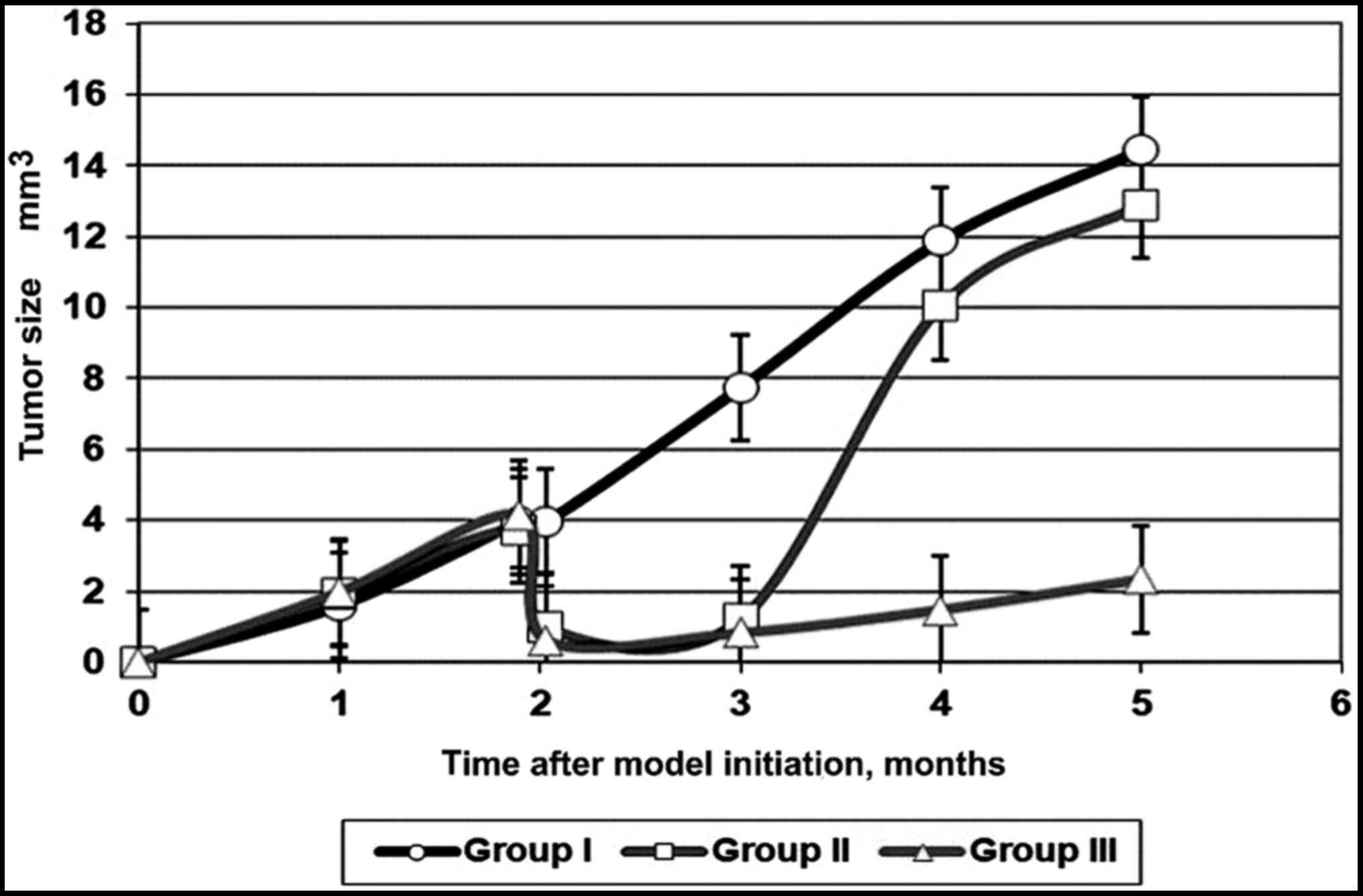
Over the entire 5-month period, the size of the
tumors (Fig. 2) in the animals of
groups I and II were significantly different [mean difference, 0.7;
95% confidence interval (CI), 0.1558-1.244; P=0.0097]. The
difference between the size of the tumors in the animals of groups
II and III was also significant (mean difference, 11.34; 95% CI,
10.80-11.88; P<0.0001). The difference between the size of the
tumors in the animals of groups I and III was also significant
(mean difference, 12.04; 95% CI, 11.50-12.58; P<0.0001).
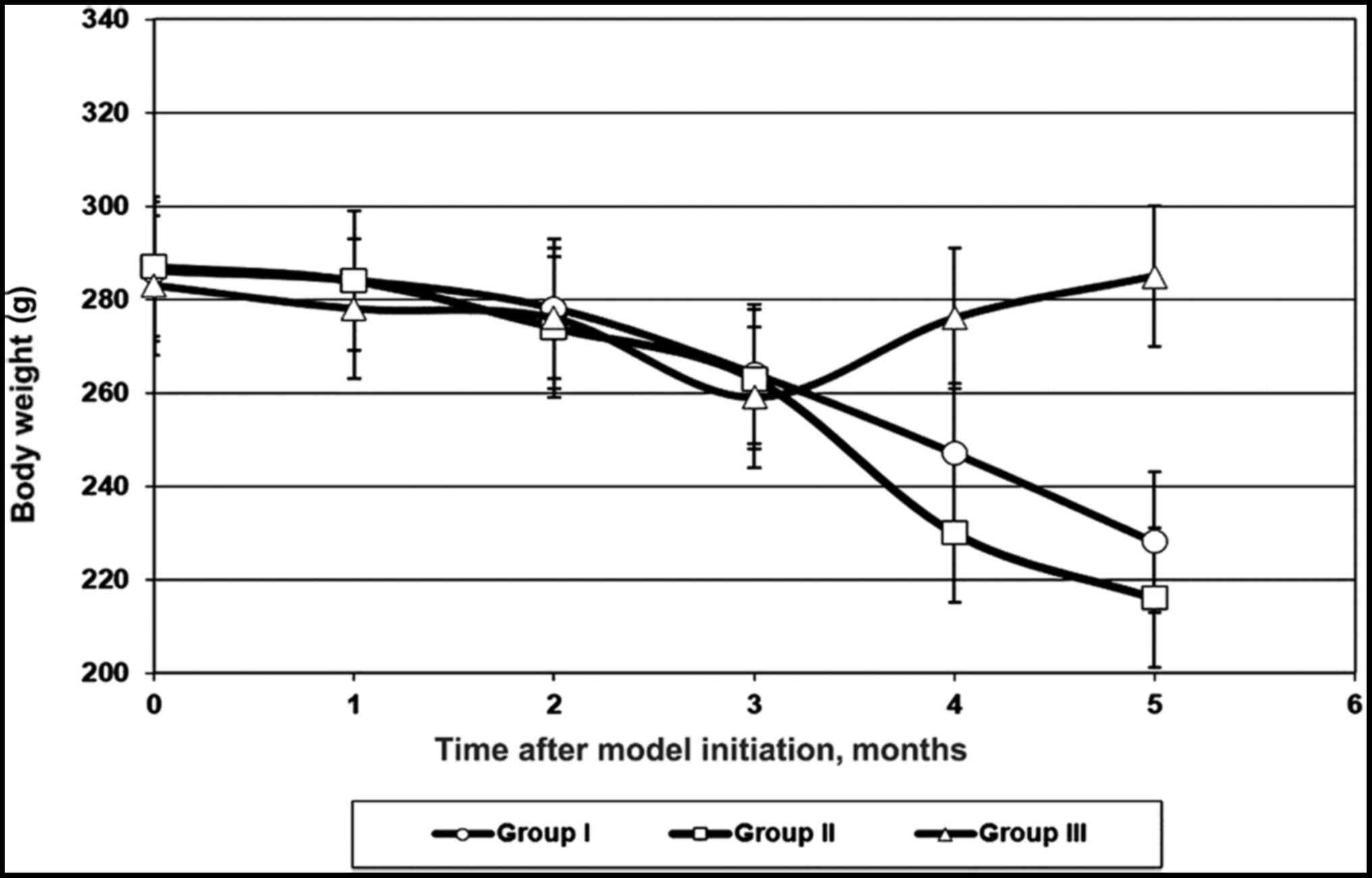
Compared with that of the first group, the rate of
tumor growth after surgery was slightly suppressed for 24 days in
the animals of the second group. However, after 30–35 days, the
tumor began to progress rapidly. It should be noted that in animals
of the first and second groups, a decrease in body weight was
observed (Fig. 3).
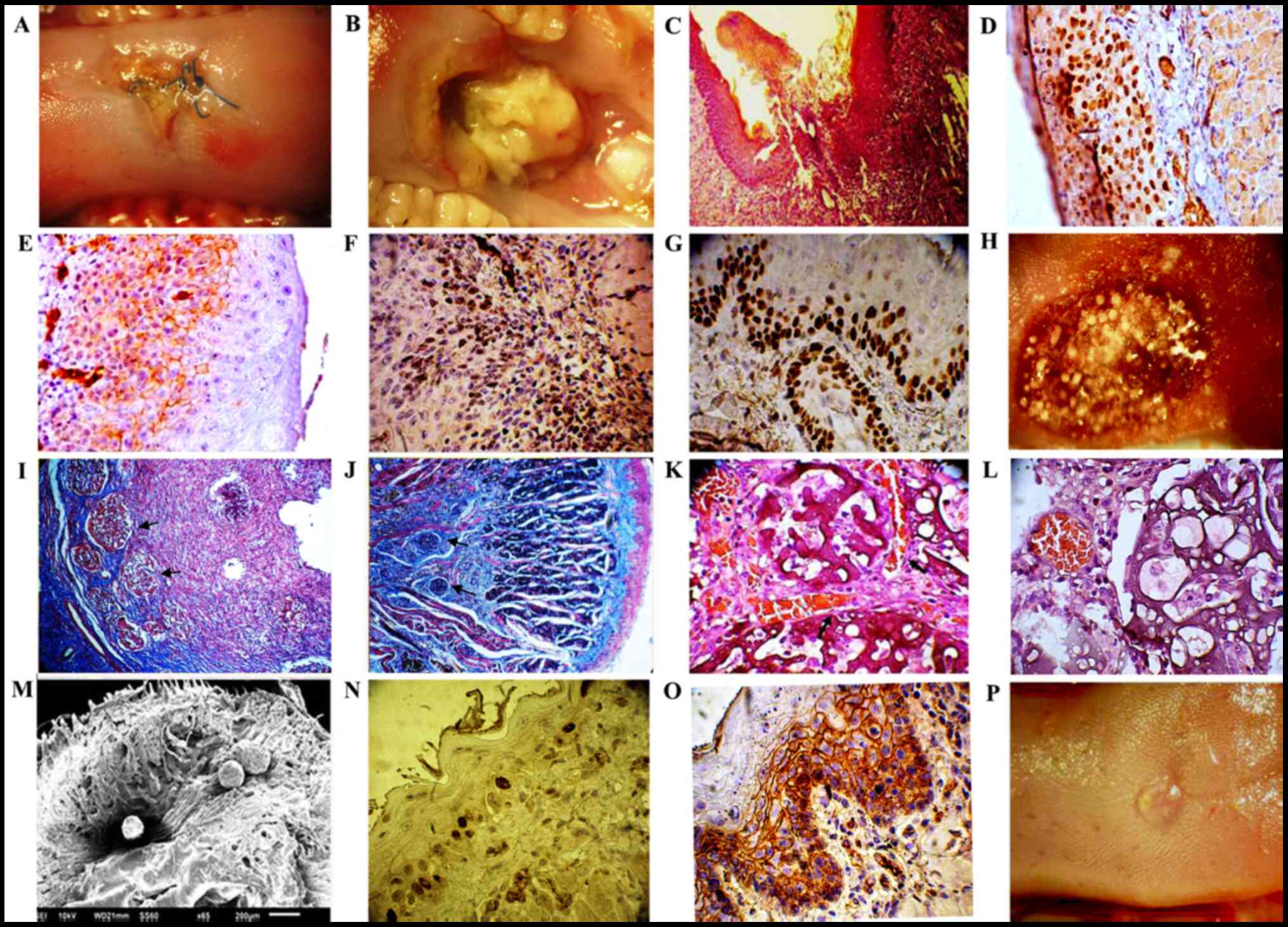
Histological examination of animals of the second
group identified 14 (70%) cases of highly differentiated squamous
cell carcinoma of the tongue. In the rest of the animals of this
group, epithelial dysplasia with varying degrees of atypia was
observed at different time points. Immunohistochemical analysis
revealed high expression of cyclin D1 and low expression of
E-cadherin. High expression of Ki-67 and p63 was also observed
(Fig. 4A-G).
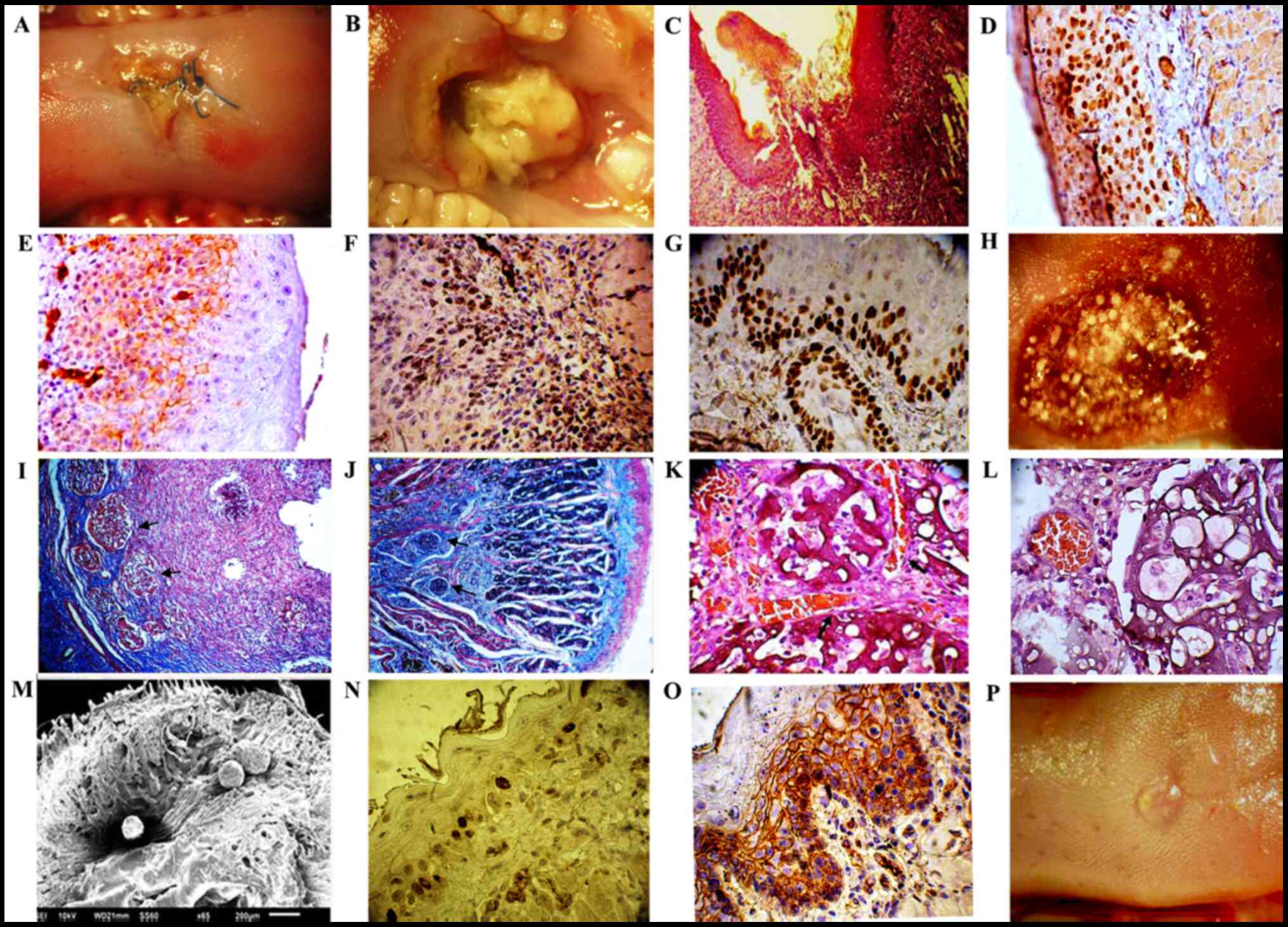 | Figure 4.Process of wound healing after 85%
resection of tongue squamous cell carcinoma and treatment with
MCPFTG. (A-G) Group II, 4-NQO + surgery: (A) Non-healing wound of
the tongue after 85% resection of squamous cell carcinoma
(observation period, 20 days). (B) Tumor progression (observation
period, 25–30 days). (C) Non-healing wound of the tongue.
Hematoxylin and eosin staining; magnification, ×200 (observation
period, 15 days). (D) High expression of cyclin D1; magnification,
×400 (observation period, 30 days). (E) Low expression of
E-cadherin; magnification, ×400 (observation period, 30 days). (F)
High expression of Ki-67; magnification, ×400 (observation period,
30 days). (G) High expression of p63; magnification ×400
(observation period, 30 days). (H-P) Group III, 4-NQO + surgery +
MCPFTG: (H) After 85% resection of squamous cell carcinoma, the
wound of the tongue was covered with MCPFTG. (I) Wound bed with
incorporated microcarriers (CultiSpher-S; black arrows). Masson's
trichrome staining; magnification, ×200 (observation period, 2
days). (J) Section of re-epithelialized wound bed with incorporated
microcarriers. Residual CultiSpher-S were detected in the wound
(black arrows). Masson's trichrome; magnification, ×200
(observation period, 45 days). (K and L) Presence of connective
tissue and neo-angiogenesis around the CultiSpher-S (black arrows).
Hematoxylin and eosin staining; magnification, ×400 (observation
period, 20 days). (M) Scanning electron microscopy. CultiSpher-S
was placed in the wound. (N) Low expression of cyclin D1;
magnification, ×400 (observation period, 3 months). (O) High
expression of E-cadherin; magnification, ×400 (observation period,
3 months). (P) Re-epithelialization of the wound after removal of
the tumor and use of MCPFTG; observation period, 20–25 days. |
In the present study, the humane endpoints for the
size of the carcinoma of the tongue were set in the range of 12–14
mm3. Macroscopic examination of the liver, lungs and
kidneys revealed no metastasis. Wound healing analysis showed that
the majority of animals in the second group had non-healing tongue
wounds within 3 months after tumor removal.
In most animals of the third group, the wounds
healed within 20–25 days after tumor removal and MCPFTG
application. Suppression of the tumor growth throughout 150 days
without tumor recurrence was evident in the all animals treated
with MCPFTG. Macroscopic examination of the liver, lungs and
kidneys revealed no metastasis.
The results of the research showed that MCPFTG had
formed a three-dimensional structure that filled the entire wound,
and the surface area of contact of cisplatin with the remaining
tumor cells was increased. Immunohistochemical analysis revealed
low and moderate expression of cyclin D1, as well as high
expression of E-cadherin throughout the whole observation period
(Fig. 4H-P).
Discussion
Fibrinogen/thrombin gel has long been widely used in
surgical practice; it is also used as a wound dressing for the
closure of wounds (18).
Fibrinogen/thrombin gel are important in tissue engineering
(19). However, it has been
reported that fibrinogen affects tumor growth and metastasis in
vivo (20,21). Additionally, three-dimensional
fibrin gel promotes the selection and growth of tumorigenic cells
(22). A previous study reported
that in situ condensation of an anticancer drug into fibrin
gel enables effective inhibition of tumor cell growth (23). The efficacy of the clinical
application of human fibrinogen-thrombin patch
(TachoSil®) in upper gastrointestinal cancer surgery has
been demonstrated in another study (24). Currently, the bioresorbable polymer
carriers of fibrinogen-based micro- and nanostructures are
effectively used for creating targeted drug delivery systems.
Fibrinogen has successfully been used as a 5-fluoroaracil carrier
for cancer drug delivery applications (25). It has also been reported that
fibrin glue enhances antitumor performance in models of
subcutaneous and abdominal metastasis of murine colorectal cancer
(26).
The present study aimed to develop a gel that, over
a period of time, could release anticancer drugs locally to prevent
recurrence and concomitantly accelerate wound healing.
The local drug delivery system based on MCPFTG that
was developed in the present study has demonstrated efficacy in
treating squamous cell carcinoma of the tongue in rats.
Importantly, in 80% of the animals that were treated with MCPFTG,
suppression of tumor growth was notable for 150 days without tumor
recurrence. Additionally, in the majority of animals, at 45–50 days
from tumor resection and introduction of MCPFTG into the wound,
complete epithelialization of the wound was observed.
Scanning electron microscopy demonstrated that CPtCS
was placed in the MCPFTG without being damaged, and was evenly
distributed both on the surface and within the gel. The platinum
cisplatin nanoparticles with a size of 10.7-11.2 nm had a
cylindrical shape. Micro Energy-dispersive X-ray spectroscopy
analysis showed that MCPFTG contained 29.1 µg platinum
nanoparticles. After placement in the wound, the quantity of
platinum nanoparticles did not change for 5 months, and
consequently they exhibited a long-term effect on residual tumor
cells.
Overall, the current study showed that MCPFTG
exerted an inhibitory effect on the growth of tongue squamous cell
carcinoma. MCPFTG reduced the toxicity of cisplatin, and improved
its antitumor activity by inhibiting the migration, invasion and
proliferation of squamous cell carcinoma in rats.
CultiSpher-S microcarrier can function as a tissue
scaffold and be beneficial as a temporary matrix for wound healing.
A previous study reported similar results (27); however, in the current study, the
freeze-dried BMSCs that were attached to the microcarrier
significantly accelerated the re-epithelialization of the wound.
Since CultiSpher-S microcarrier promotes in vitro cell
attachment and migration, it was hypothesized that CultiSpher-S
microcarrier can become an in vivo trap for residual tumor
cells after it has been removed. The porous structure of the
microcarrier allows the attachment and migration of tumor cells
both on the surface and the inner structure of the microcarrier,
and the cisplatin-loaded microcarrier is expected to destroy tumor
cells.
We hypothesized that the internal layer of MCPFTG
that directly contacted the surface of the wound could release
cisplatin locally over a certain period of time, and destroy any
residual tumor cells. The external layer of MCPFTG consisted of
Cultispher-S microcarrier and freeze-dried BMSCs. Cultispher-S
filled the residual wound cavities creating a 3-dimensional
structure, and freeze-dried paracrine factors of BMSCs enhanced the
wound regeneration process. Additionally, the possibility of using
freeze-dried BMSCs for the treatment of non-healing wounds has been
discussed in detail in our previous studies articles. The first
study used a radiation wound model in rats. It was found that
freeze-dried BMSCs retained their unique paracrine factors and
improved clinical healing and re-epithelialization of non-healing
wounds (28). Stem cell therapy
for the treatment of non-healing chronic wounds has demonstrated
positive therapeutic potential in a number of preclinical and
clinical studies (29,30). Cells are known to be potential
sources of paracrine factors, and, as previously indicated, these
paracrine bioactive factors are associated with the therapeutic
effects of stem cells in chronic wound treatment (31). As previously reported, mesenchymal
stem cell (MSC)-conditioned media contains keratinocyte growth
factor, epidermal growth factor, VEGF-α, insulin-like growth factor
1, stromal cell-derived factor 1, erythropoietin, and macrophage
inflammatory proteins 1α and 1β (28). MSCs may accelerate the
wound-healing process via a paracrine mechanism (32,33).
MSCs are also able to secrete paracrine angiogenesis-enhancing
factors such as granulocyte colony-stimulating factor, VEGF,
hepatocyte growth factor, interleukin 6, monocyte chemotactic
protein-1 and TGFβ1 (34,35). However, there are no conclusive
answers with regard to the mechanism by which MSCs exert positive
effects (31).
Our second previously published study concerned the
reconstruction of defects within the mandible using autogenous bone
and decellularized bovine bone grafts with freeze-dried BMSC
paracrine factors. The study consisted of one man and three women
(age range, 38–55 years) who underwent surgery for a primary tumor
of the mandible between January 2008 and December 2015 in the
Cancer Research Center of Tbilisi (Tbilisi, Georgia) (36). Initial clinical investigations
revealed that a biologically active bone graft seeded with
freeze-dried BMSC paracrine factors could be applied for
reconstructing large mandibular bone defects after tumor resection.
The biologically active bone graft contained type III collagen,
glycoproteins and a number of different growth factors, including
basic fibroblast growth factor, epidermal growth factor, VEGF,
keratinocyte growth factor, TGFα and β, PDGF, nerve growth factor
and hepatocyte growth factor.
It has been reported that MSCs are able to migrate
towards the tumor regardless of the type of tumor. This process of
migration is mediated via a paracrine signaling loop between tumor
microenvironment chemoattractants and corresponding receptor
expression in MSCs (37). There
are several reports demonstrating successful treatment of various
types of tumor by using MSCs as carriers for anticancer drug
delivery (38–42). As aforementioned, freeze-dried
BMSCs are able to retain >80% of paracrine factors, including
VEGF-1, epidermal growth factor, insulin-like growth factor 1,
hepatocyte growth factor, monocyte chemoattractant protein-1,
angiopoietin-1, stromal cell-derived factor-1, erythropoietin and
keratinocyte growth factor (28).
It could be suggested that freeze-dried BMSC paracrine factors can
attract residual tumor cells and enable their attachment to the
surface of the CultiSpher-S microcarrier. However, this hypothesis
requires further research for verification.
The mechanism by which MCPFTG suppresses the growth
of tumor cells remains unclear. Further studies are required to
understand the mechanism of tumor growth suppression mediated by
MCPFTG. A limitation of the present study is associated with the
use of paracrine factors of bone marrow stem cells, which require
more detailed study into their role in tumor treatment.
We are currently conducting western blotting studies
on the expression of several related proteins and hope that these
results will be reflected in future publications.
In conclusion, the MCPFTG-based local drug delivery
system has been shown to be effective in suppressing tumor growth
and preventing recurrence. In the present study, MCPFTG reduced the
toxicity of cisplatin and improved its antitumor activity. In
addition, freeze-dried BMSC paracrine factors presented in the
MCPFTG enhanced the wound healing processes after tumor removal.
Thus, the present study suggests novel opportunities for the
development of a multifunctional drug delivery system for the
treatment of squamous cell carcinoma.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
The authors confirm contribution to the paper as
follows: MZK and TP performed experimental studies, data analysis
and participated in the preparation of the manuscript. NK was
responsible for the study concept. KM and ZV processed experimental
data and performed data interpretation for the study. MJ and KG
performed histological and immunohistochemical studies, and the
statistical analysis. LK and DC processed experimental data and
confirm the authenticity of all the raw data. ZK conceived and
planned the experiments, performed the analysis and the prepared of
the manuscript. All authors read and approved the final version of
the manuscript.
Ethics approval and consent to
participate
The housing and handling of the rats followed
guidelines established by the Animal Care and Use Committee of
Tbilisi State Medical University (Tbilisi, Georgia). Animals were
monitored daily for infection and other illnesses by trained animal
technicians. All individuals who handled rats were registered to
protocols at Tbilisi State Medical University. All animal protocols
were approved by the Institutional Review Board of Tbilisi State
Medical University (approval no. 812).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
4NQO
|
4-nitroquinoline 1-oxide
|
|
PEG
|
polyethylene glycol
|
|
PGF
|
pegylated fibrinogen
|
|
CPtCS
|
cisplatin-loaded CultiSpher-S
|
|
BMSC
|
bone marrow stem cell
|
References
|
1
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Johnson NW, Jayasekara P and Amarasinghe
AA: Squamous cell carcinoma and precursor lesions of the oral
cavity: Epidemiology and aetiology. Periodontol 2000. 57:19–37.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mahvi DA, Liu R, Grinstaff MW, Colson YL
and Raut CP: Local Cancer Recurrence: The Realities, Challenges,
and Opportunities for New Therapies. CA Cancer J Clin. 68:488–505.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Oliver RJ, Clarkson JE, Conway DI, Glenny
A, Macluskey M, Pavitt S, Sloan P and Worthington HV; CSROC Expert
Panel, : Interventions for the treatment of oral and oropharyngeal
cancers: Surgical treatment. Cochrane Database Syst Rev.
4:CD0062052007.PubMed/NCBI
|
|
5
|
Bulsara VM, Worthington HV, Glenny AM,
Clarkson JE, Conway DI and Macluskey M: Interventions for the
treatment of oral and oropharyngeal cancers: Surgical treatment.
Cochrane Database Syst Rev. 12:CD0062052018.PubMed/NCBI
|
|
6
|
Sun LM, Leung SW, Su CY and Wang CJ: The
relapse patterns and outcome of postoperative recurrent tongue
cancer. J Oral Maxillofac Surg. 55:827–831. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kishi N, Imai Y, Kanayama N, Hirata T,
Kawaguchi Y, Konishi K, Nishiyama K and Teshima T: Recurrence
Patterns of Postoperative Radiation Therapy for Patients with Head
and Neck Squamous Cell Carcinoma. Int J Radiat Oncol Biol Phys.
96:E389–E390. 2016. View Article : Google Scholar
|
|
8
|
Liao CT, Chang JT, Wang HM, Ng SH, Hsueh
C, Lee LY, Lin CH, Chen IH, Huang SF, Cheng AJ, et al: Salvage
therapy in relapsed squamous cell carcinoma of the oral cavity: How
and when? Cancer. 112:94–103. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rowe DE, Carroll RJ and Day CL Jr:
Prognostic factors for local recurrence, metastasis, and survival
rates in squamous cell carcinoma of the skin, ear, and lip.
Implications for treatment modality selection. J Am Acad Dermatol.
26:976–990. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Larsen SR, Johansen J, Sørensen JA and
Krogdahl A: The prognostic significance of histological features in
oral squamous cell carcinoma. J Oral Pathol Med. 38:657–662. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Woolgar JA and Triantafyllou A: A
histopathological appraisal of surgical margins in oral and
oropharyngeal cancer resection specimens. Oral Oncol. 41:1034–1043.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhang G, Wang X, Wang Z, Zhang J and Suggs
L: A PEGylated fibrin patch for mesenchymal stem cell delivery.
Tissue Eng. 12:9–19. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kakabadze Z, Kipshidze N, Mardaleishvili
K, Chutkerashvili G, Chelishvili I, Harders A, Loladze G,
Shatirishvili G, Kipshidze N, Chakhunashvili D, et al: Phase 1
Trial of Autologous Bone Marrow Stem Cell Transplantation in
Patients with Spinal Cord Injury. Stem Cells Int. 2016:67682742016.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sagheer SH, Whitaker-Menezes D, Han JYS,
Curry JM, Martinez-Outschoorn U and Philp NJ: 4NQO induced
carcinogenesis: A mouse model for oral squamous cell carcinoma.
Methods Cell Biol. 163:93–111. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hawkins BL, Heniford BW, Ackermann DM,
Leonberger M, Martinez SA and Hendler FJ: 4NQO carcinogenesis: A
mouse model of oral cavity squamous cell carcinoma. Head Neck.
16:424–432. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
El-Rouby DH: Histological and
immunohistochemical evaluation of the chemopreventive role of
lycopene in tongue carcinogenesis induced by
4-nitroquinoline-1-oxide. Arch Oral Biol. 56:664–671. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kakabadze Z, Kakabadze A, Chakhunashvili
D, Karalashvili L, Berishvili E, Sharma Y and Gupta S:
Decellularized human placenta supports hepatic tissue and allows
rescue in acute liver failure. Hepatology. 67:1956–1969. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Rothwell SW, Sawyer E, Dorsey J, Flournoy
WS, Settle T, Simpson D, Cadd G, Janmey P, White C and Szabo KA:
Wound healing and the immune response in swine treated with a
hemostatic bandage composed of salmon thrombin and fibrinogen. J
Mater Sci Mater Med. 20:2155–2166. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ahmed TA, Dare EV and Hincke M: Fibrin: A
versatile scaffold for tissue engineering applications. Tissue Eng
Part B Rev. 14:199–215. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Costantini V and Zacharski LR: The role of
fibrin in tumor metastasis. Cancer Metastasis Rev. 11:283–290.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Staton CA, Brown NJ and Lewis CE: The role
of fibrinogen and related fragments in tumour angiogenesis and
metastasis. Expert Opin Biol Ther. 3:1105–1120. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Liu J, Tan Y, Zhang H, Zhang Y, Xu P, Chen
J, Poh YC, Tang K, Wang N and Huang B: Soft fibrin gels promote
selection and growth of tumorigenic cells. Nat Mater. 11:734–741.
2012. View
Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kuwahara M, Fujita H, Kataoka Y, Nakajima
Y, Yamada M and Sugimoto N: In situ condensation of an anti-cancer
drug into fibrin gel enabling effective inhibition of tumor cell
growth. Chem Commun (Camb). 55:11679–11682. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Marano L and Di Martino N: Efficacy of
Human Fibrinogen-Thrombin Patch (TachoSil) Clinical Application in
Upper Gastrointestinal Cancer Surgery. J Invest Surg. 29:352–358.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Rejinold NS, Muthunarayanan M, Chennazhi
KP, Nair SV and Jayakumar R: 5-fluorouracil loaded fibrinogen
nanoparticles for cancer drug delivery applications. Int J Biol
Macromol. 48:98–105. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hu Y, Yu T, Liu X, He Y, Deng L, Guo J,
Hua Y, Luo T and Gao X: Improved anti-tumor efficacy via
combination of oxaliplatin and fibrin glue in colorectal cancer.
Oncotarget. 9:2515–2526. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Lönnqvist S, Rakar J, Briheim K and Kratz
G: Biodegradable Gelatin Microcarriers Facilitate
Re-Epithelialization of Human Cutaneous Wounds - An In Vitro Study
in Human Skin. PLoS One. 10:e01280932015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kakabadze Z, Chakhunashvili D,
Gogilashvili K, Ediberidze K, Chakhunashvili K, Kalandarishvili K
and Karalashvili L: Bone Marrow Stem Cell and Decellularized Human
Amniotic Membrane for the Treatment of Nonhealing Wound After
Radiation Therapy. Exp Clin Transplant. 17 (Suppl 1):92–98. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Marfia G, Navone SE, Di Vito C, Ughi N,
Tabano S, Miozzo M, Tremolada C, Bolla G, Crotti C, Ingegnoli F, et
al: Mesenchymal stem cells: Potential for therapy and treatment of
chronic non-healing skin wounds. Organogenesis. 11:183–206. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Asanuma H, Meldrum DR and Meldrum KK:
Therapeutic applications of mesenchymal stem cells to repair kidney
injury. J Urol. 184:26–33. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Burdon TJ, Paul A, Noiseux N, Prakash S
and Shum-Tim D: Bone marrow stem cell derived paracrine factors for
regenerative medicine: Current perspectives and therapeutic
potential. Bone Marrow Res. 2011:2073262011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chen L, Tredget EE, Wu PY and Wu Y:
Paracrine factors of mesenchymal stem cells recruit macrophages and
endothelial lineage cells and enhance wound healing. PLoS One.
3:e18862008. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Walter MN, Wright KT, Fuller HR, MacNeil S
and Johnson WE: Mesenchymal stem cell-conditioned medium
accelerates skin wound healing: An in vitro study of fibroblast and
keratinocyte scratch assays. Exp Cell Res. 316:1271–1281. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kwon HM, Hur SM, Park KY, Kim CK, Kim YM,
Kim HS, Shin HC, Won MH, Ha KS, Kwon YG, et al: Multiple paracrine
factors secreted by mesenchymal stem cells contribute to
angiogenesis. Vascul Pharmacol. 63:19–28. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Baraniak PR and McDevitt TC: Stem cell
paracrine actions and tissue regeneration. Regen Med. 5:121–143.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Kakabadze A, Mardaleishvili K, Loladze G,
Karalashvili L, Chutkerashvili G, Chakhunashvili D and Kakabadze Z:
Reconstruction of mandibular defects with autogenous bone and
decellularized bovine bone grafts with freeze-dried bone marrow
stem cell paracrine factors. Oncol Lett. 13:1811–1818. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Chan JK and Lam PY: Human mesenchymal stem
cells and their paracrine factors for the treatment of brain
tumors. Cancer Gene Ther. 20:539–543. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Sasportas LS, Kasmieh R, Wakimoto H,
Hingtgen S, van de Water JA, Mohapatra G, Figueiredo JL, Martuza
RL, Weissleder R and Shah K: Assessment of therapeutic efficacy and
fate of engineered human mesenchymal stem cells for cancer therapy.
Proc Natl Acad Sci USA. 106:4822–4827. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Dwyer RM, Ryan J, Havelin RJ, Morris JC,
Miller BW, Liu Z, Flavin R, O'Flatharta C, Foley MJ, Barrett HH, et
al: Mesenchymal Stem Cell-mediated delivery of the sodium iodide
symporter supports radionuclide imaging and treatment of breast
cancer. Stem Cells. 29:1149–1157. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Li GC, Ye QH, Xue YH, Sun HJ, Zhou HJ, Ren
N, Jia HL, Shi J, Wu JC, Dai C, et al: Human mesenchymal stem cells
inhibit metastasis of a hepatocellular carcinoma model using the
MHCC97-H cell line. Cancer Sci. 101:2546–2553. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Zischek C, Niess H, Ischenko I, Conrad C,
Huss R, Jauch KW, Nelson PJ and Bruns C: Targeting tumor stroma
using engineered mesenchymal stem cells reduces the growth of
pancreatic carcinoma. Ann Surg. 250:747–753. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Khakoo AY, Pati S, Anderson SA, Reid W,
Elshal MF, Rovira II, Nguyen AT, Malide D, Combs CA, Hall G, et al:
Human mesenchymal stem cells exert potent antitumorigenic effects
in a model of Kaposi's sarcoma. J Exp Med. 203:1235–1247. 2006.
View Article : Google Scholar : PubMed/NCBI
|