Introduction
Glutamine (gln) is the most abundant free amino acid
in the body, held within skeletal muscle cells. Gln is used by the
cell for both bioenergetic and biosynthetic needs. Once taken up by
the cell, the vast majority of gln is converted to glutamate by
mitochondrial glutaminase, an enzyme whose levels are frequently
upregulated in tumors and tumor cell lines (1,2).
Proliferatively active cells require a source of
carbon and nitrogen for the synthesis of macromolecules. Although
most tumor cells utilize aerobic glycolysis and shunt metabolites
away from mitochondrial oxidative phosphorylation, numerous tumor
cells exhibit increased mitochondrial activity. In these cells, gln
uptake is markedly enhanced and far exceeds the metabolic
requirements of the cell (3).
In the case of tumor growth and proliferation, a
single conceptual model of the cancer metabolism program does not
exist. Variability exists across different types of cancer in terms
of glycolytic and glutaminolytic contribution to malignant
proliferation, which allows tumors to utilize different anaplerotic
precursors or metabolic platforms as a means of dynamic adaptation
under stress (4).
Cancer cells exhibit dysregulation of the
proteins/enzymes involved in the key regulatory steps of glucose
transport, glycolysis, tricarboxylic acid (TCA) cycle and
glutaminolysis, governed not only by oncogenes such as c-Myc but
also by hypoxia-inducible factor-1 and loss of function tumor
suppressor p53 (5). The MYC
oncogene, which serves a critical role in numerous types of human
cancer, is considered a master regulator of cell metabolism and
proliferation, reprogramming mitochondrial metabolism towards
sustaining cellular viability and TCA cycle anaplerosis (6).
Numerous in vitro studies provided evidence
that upregulation of the gln pathway provides cancer cells with a
variety of essential products to sustain cell proliferation, such
as ATP and macromolecules, for biosynthesis. Human cancer cell
lines exhibited a 5- to 10-fold faster rate of gln consumption than
non-malignant cells (7). It may be
inferred that available gln predicts a more aggressive tumor
behavior and raises the possibility that nutritional
supplementation with gln may stimulate tumor growth by promoting
angiogenesis, survival and motility of cancer cells through the
activation of NF-κB (8). Several
gln analogs have been studied as potential chemotherapeutic (CT)
agents in preclinical animal studies and in phase I clinical trials
in patients with the rationale to diminish blood gln levels and,
thereby, decrease the availability of gln to the tumor; however,
the results were disappointing, and studies were discontinued due
to side effects (9). On the
contrary, in rat model studies, supplemental oral gln improved host
tolerance through altering glutathione metabolism and protected
normal tissues from CT treatment-related injury (10).
These contradictory results of in vitro and
animal studies clearly indicate that reliable information regarding
the effects of supplemental gln may only be made based on clinical
studies in humans. If gln is not available from exogenous sources,
tumor cells may manipulate the host metabolism to cover their needs
endogenously. Thus, any measures to establish a gln depletion
situation ‘artificially’ cannot stop or even retard tumor growth
(11). Furthermore, the endogenous
use of gln by parasitic cancer cells is associated with impaired
physiological functions of disturbed mucosal integrity and
diminished immune competence (12).
With this hypothesis, within the last two decades,
numerous clinical trials evaluated supplemental oral, enteral, or
parenteral gln tolerance, safety and effects in various cancer
patient groups; dosage, time, and frequency of gln supplementation,
as well as cancer type and stage of disease, varied considerably
(13). In general, oral/enteral
and parenteral gln dipeptide supplementation was safe and
well-tolerated, with tumor growth and tumor protein synthesis being
unaltered and with no adverse effects on the efficacy of antitumor
treatment (14).
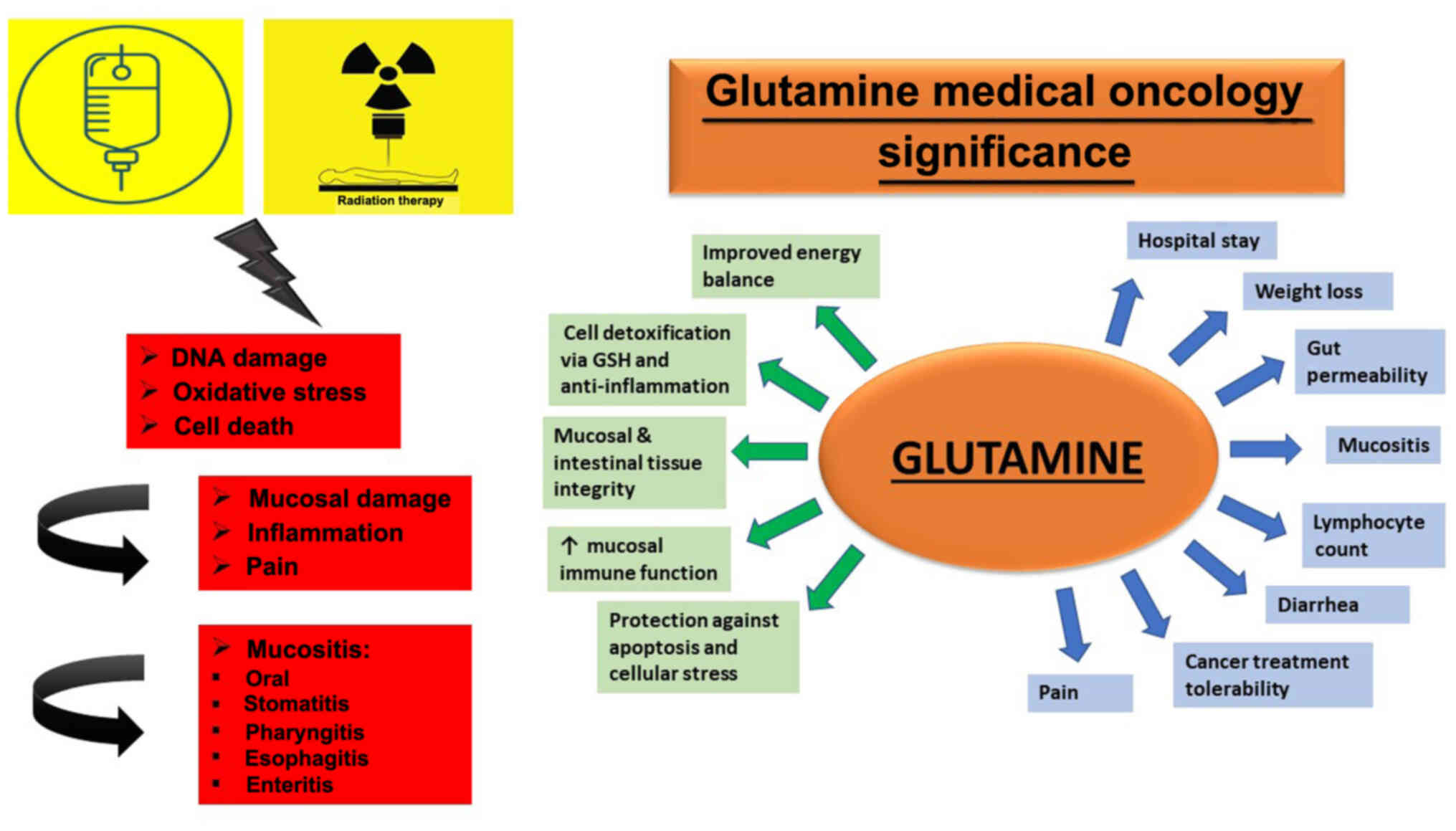
Concerning gln supplementation, >50 clinical
studies for all cancer types (from the MEDLINE Database between
2000 and 2020) have been performed. For patients with thoracic and
upper aerodigestive malignancies (T&UAM), 22 clinical studies
with oral gln supplementation [16 randomized controlled trials
(RCTs), 3 pilot and 3 retrospective studies] evaluated its safety,
tolerance and effect on mucositis/stomatitis, esophagitis, pain,
weight loss and hospital stay. According to most of the available
clinical evidence, gln supplementation may decrease the incidence
and/or severity of standard of care treatment-associated toxicities
in tumors of the lung and esophagus, as well as head & neck
tumors (H&NT) (13,15), while dosimetric modality parameters
impacting this effect remain to be clarified and this effect
remains to be translated into the need for analgesic therapy
(Fig. 1).
Therefore, the present study aimed to evaluate the
potential effect of oral gln to reduce radiation-induced
toxicities, weight loss and pain in patients with T&UAM. In
addition, to define a subgroup of patients who are more likely to
benefit from treatment, association with dosimetric parameters
predictive of these adverse effects, such as the length of the
irradiated esophagus, were determined. The primary endpoints were
the incidence of toxicities of grade 2, weight loss and the need
for analgesic therapy. The secondary endpoint was the correlation
of the length of the irradiated esophagus from radiotherapy (RT)
treatment planning with the use of opioids as analgesics.
Materials and methods
Study subjects
A total of 72 patients with biopsy-confirmed
T&UAM, treated either with sequential or concomitant RT-CT
(62%) or RT alone (38%) and supplemented with oral gln prior to the
initiation of the RT treatment were prospectively recruited from
the Department of Radiation Oncology of Athens Medical Center
(Athens, Greece) between April 2013 and September 2017. Sample size
calculation was not performed a priori since it was restricted by
the sample availability. The mean age of the patients was 65.6±1.2
years (age range, 54–77 years). Most participants were males (n=54,
75%). Table I provides
demographics and clinical characteristics of the patients. The
study was approved by the Ethics Committee of the Hospital
(approval no. 2281/26-04-2013).
 | Table I.Patient characteristics and features
of their disease and treatment. |
Table I.
Patient characteristics and features
of their disease and treatment.
| Variable | Value |
|---|
| Age, years | 65.6±11.2 |
| Sex |
|
|
Male | 54 (75.0) |
|
Female | 18 (25.0) |
| Weight loss after
RT |
|
| No | 30 (42.3) |
|
Yes | 41 (57.7) |
| PS |
|
| 0 | 29 (40.3) |
| 1 | 37 (51.4) |
| 2 | 6 (8.3) |
| Cancer type |
|
| Chest
tumor | 33 (45.8) |
| Head
& neck | 39 (54.2) |
| Grade |
|
| 1 | 7 (11.7) |
| 2 | 24 (40.0) |
| 3 | 29 (48.3) |
| Stage |
|
| I | 11 (15.9) |
| II | 12 (17.4) |
|
III | 37 (53.6) |
| IV | 9 (13.0) |
| Duration of RT,
days | 33.6±13.0 |
| Total dose,
cGY |
5,489.4±1,196.2 |
| Irradiation
fractions | 26.4±7.1 |
| Length of the
radiated | 12.4±3.3 |
| esophagus from
treatment planning, cm | Length of the
radiated esophagus from treatment planning (cm) |
| <12 | 31 (43.7) |
| >12 | 40 (56.3) |
| Prior surgery | 25 (34.7) |
| Prior
chemotherapy | 31 (43.7) |
| Concurrent
chemotherapy | 27 (38.0) |
|
Chemotherapy (before and at
the same time as RT) | 14 (19.7) |
|
Chemotherapy only at the same
time as RT | 13 (18.3) |
| Only RT | 27 (38.0) |
| Subsequent
chemotherapy after RT | 21 (29.6) |
| Smoking |
|
| No | 19 (26.4) |
|
Yes | 43 (59.7) |
| Former
smoker | 10 (13.9) |
| Alcohol
consumption | 28 (41.8) |
| Diabetes | 20 (31.7) |
| Hypertension | 30 (54.5) |
Demographics and clinical
characteristics
Patient characteristics and features of their
disease and treatment are presented in Table I, more than half of the
participants (54.2%) had H&NT, while the remaining (45.8%) had
tumors of the chest, i.e. lung cancer (LC). In addition, 40.0% of
the participants had grade 2 cancer and 53.6% were in stage III.
The mean duration of RT was 33.6±13.0 days and in 56.3% of the
cases, the length of the irradiated esophagus from treatment
planning was >12 cm. A total of 34.7% of the patients had
previous surgery and 43.7% had a CT prior to RT. Furthermore, 19.7%
of the patients had CT prior to and at the same time as RT, while
18.3% had CT only at the same time as RT (concurrent CT-RT). A
total of 57.7% of the participants had lost weight after the RT and
the majority had a performance status (PS) of <2. Diabetes and
hypertension were present in 31.7% and 54.5% of the patients,
respectively.
Patient treatment
All participants were treated either with sequential
or concomitant RT-CT (62%) or RT alone (38%) and received
prophylactic gln powder in doses of 15 g 2 times per day (bid), for
the total duration of RT treatment. The radiation technique was
three-dimensional conformal RT. Prior to RT, patients had a
computerized tomography scan on the region of the body treated
using adequate immobilization. Clinical treatment volumes, planning
treatment volumes and organs at risk were contoured on each slice
(3 mm/5 mm) with isodose distribution on the nasopharynx or
mediastinum, also displaying the length of the irradiated
esophagus. 3D plans were generated on a Masterplan (Nucletron Group
Ltd.) treatment planning system using the collapsed cone algorithm.
Irradiation was then performed using a 6MV Primus (Siemens AG)
linear accelerator with a total dose of 50–70 Gy and 2–2.5
Gy/fraction. Concurrent CT consisted of low-dose weekly cisplatin
in 38% of the patients.
The severity of different acute radiation toxicities
was graded according to the RT Oncology Group/European Organization
for Research and Treatment of Cancer criteria (16). The median follow-up of the acute
radiation toxicities was one month, as for the duration of gln
supplementation. For each patient, the medical history was reviewed
and clinical examination was performed.
Smoking history and alcohol use were marked as risk
factors and diabetes and hypertension as comorbidities, while
stomatitis, esophagitis, dysphagia, pain and mycosis were reported
as acute adverse events of RT.
Medications for pain control were prescribed when
the patient became symptomatic. Antimycotic treatment was given in
clinical fungal infection, while antimycotic prophylactic therapy
was given in patients with a high probability of displaying one
[patients with a high grade of oral mucositis (OM), pain and
dysphagia]. Table II provides the
grading system for pain medications, following the World Health
Organization's pain relief ladder (17).
 | Table II.Grading system for pain
medications. |
Table II.
Grading system for pain
medications.
| Gradea | Drug | Group |
|---|
| 0 | None | No |
| 1 | Simple
analgesics | Simple analgesics
and/or NSAIDs |
| 2 | Simple analgesics
and NSAIDs | Simple analgesics
and/or NSAIDs |
| 3 | Weak narcotics,
i.e., codeine | Opioids |
| 4 | Narcotics,i.e.,
fentanyl patch | Opioids |
Statistical analysis
Quantitative variables are presented as mean values
± standard deviation, while qualitative variables are presented as
frequencies with percentages (%). For comparison of proportions,
Pearson's χ2 and Fisher's exact tests were used.
Student's t-tests were applied for comparison of continuous
variables between the groups. Logistic regression analysis in a
stepwise method (for entry, P=0.05; for removal, P=0.10) was
performed to identify independent factors associated with weight
loss after RT. Adjusted odds ratios (OR) with the corresponding 95%
confidence intervals (95% CI) were calculated from logistic
regression analyses. All reported P-values were two-tailed and
P<0.05 was considered to indicate statistical significance.
Analyses were performed using SPSS statistical software (version
19.0; IBM Corporation).
Results
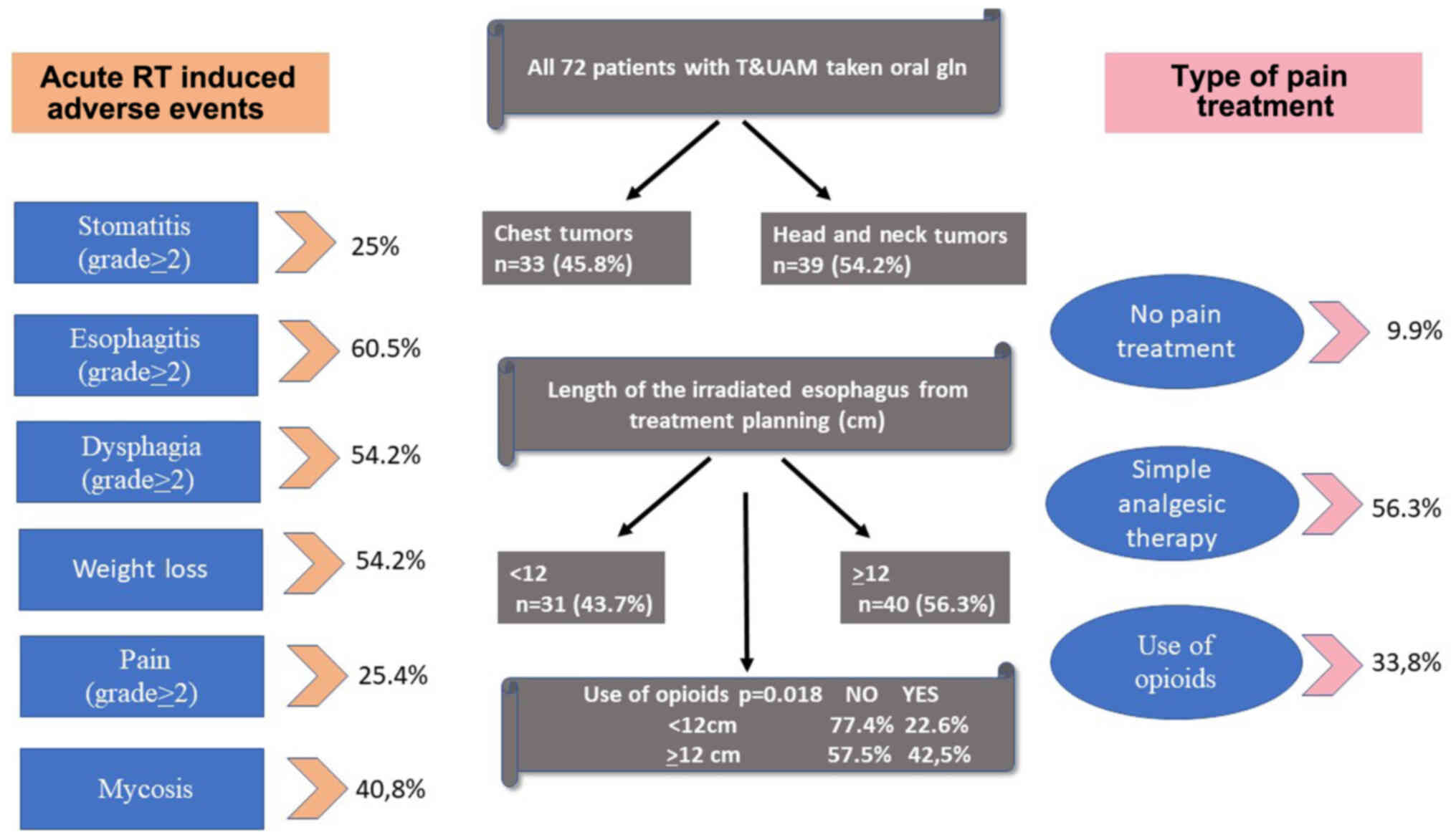
Adverse events and pain treatment
The frequencies of patients with adverse events and
pain treatment are presented in Table III. In 39.7% of the patients,
stomatitis was grade 1 or more and the frequencies for esophagitis,
dysphagia and pain were 88.7, 87.1 and 88.7%, respectively. Mycosis
was present in 40.8% of the patients (all of them manages with
antimycotic treatment) and 89.6% had at least one adverse event.
Opioids were used in 16.9% of the cases and in 16.9% of the cases,
the combination of both simple analgesics and opioids was utilized.
In total, opioids were used in 33.8% of the study population.
 | Table III.Adverse events and pain
treatment. |
Table III.
Adverse events and pain
treatment.
| Item | n (%) |
|---|
| Stomatitis,
grade |
|
| 0 | 41 (60.3) |
| 1 | 10 (14.7) |
| 2 | 9 (13.2) |
| 3 | 8 (11.8) |
| Esophagitis,
grade |
|
| 0 | 8 (11.3) |
| 1 | 20 (28.2) |
| 2 | 28 (39.4) |
| 3 | 15 (21.1) |
| Dysphagia,
grade |
|
| 0 | 9 (12.9) |
| 1 | 23 (32.9) |
| 2 | 33 (47.1) |
| 3 | 5 (7.1) |
| Pain, grade |
|
| 0 | 8 (11.3) |
| 1 | 45 (63.4) |
| 2 | 7 (9.9) |
| 3 | 11 (15.5) |
| Mycosis |
|
| No | 42 (59.2) |
|
Yes | 29 (40.8) |
| At least one
adverse event |
|
| No | 7 (10.4) |
|
Yes | 60 (89.6) |
| Pain treatment |
|
|
None | 7 (9.9) |
| Simple
analgesics | 40 (56.3) |
| Simple
analgesics and opioids | 12 (16.9) |
|
Opioids | 12 (16.9) |
| Antimycotic
treatment |
|
| No | 42 (59.2) |
|
Yes | 29 (40.8) |
| Antimycotic
prophylaxis |
|
| No | 40 (61.5) |
|
Yes | 25 (38.5) |
Association between adverse events and
patient characteristics
The occurrence of stomatitis, esophagitis and
dysphagia in association with demographics and clinical
characteristics are presented in Table IV. Stomatitis grade 2 to 3 was
more frequent in H&NT (P=0.001), in those having previous
surgery (OR: 11.818; 95% CI: 3.207-43.550; P<0.001) and in those
having concurrent CT (OR: 3.125; 95% CI: 1.007-9.699; P=0.044).
Esophagitis (OR: 3.500; 95% CI: 1.185-10.335; P=0.020) and
dysphagia (OR: 3.968; 95% CI: 1.385-11.369; P=0.008) grade 2 to 3
was more frequent in those having concurrent CT-RT (Table SI). In addition, the duration of
RT was indicated to be significantly greater in patients with
esophagitis (P=0.001) and dysphagia (P=0.006) grades 2 to 3.
Furthermore, it was indicated (data not shown) that patients who
consume alcohol had grade 2–3 esophagitis in a significantly
greater percentage compared to the ones who did not consume any
alcohol (78.6 vs. 48.7%; P=0.013). In addition, patients who
consumed alcohol had grade 2–3 dysphagia in a significantly greater
percentage compared to the ones who did not consume any alcohol
(71.4 vs. 42.1%; P=0.018). In addition, grade 2–3 dysphagia was
present in a significantly greater percentage of patients with
diabetes than in those without diabetes (70.0 vs. 38.1%;
P=0.019).
 | Table IV.Occurrence of stomatitis, esophagitis
and dysphagia in association with demographics and clinical
characteristics. |
Table IV.
Occurrence of stomatitis, esophagitis
and dysphagia in association with demographics and clinical
characteristics.
|
| Stomatitis
(grade) |
| Esophagitis
(grade) |
| Dysphagia
(grade) |
|
|---|
|
|
|
|
|
|
|
|
|---|
| Item | 0/1 | 2/3 | P-value | 0/1 | 2/3 | P-value | 0/1 | 2/3 | P-value |
|---|
| Age, years | 65.8±10.3 | 62.6±13.7 | 0.314a | 65.6±11 | 65.3±11.4 | 0.888a | 65.8±11.0 | 64.7±11.3 | 0.675a |
| Sex |
|
| 0.053b |
|
| 0.615c |
|
| 0.500c |
|
Male | 41 (82.0) | 9 (18.0) |
| 20 (37.7) | 33 (62.3) |
| 25 (48.1) | 27 (51.9) |
|
|
Female | 10 (55.6) | 8 (44.4) |
| 8 (44.4) | 10 (55.6) |
| 7 (38.9) | 11 (61.1) |
|
| PS |
|
| 0.066c |
|
| 0.781c |
|
| 0.281c |
| 0 | 25 (86.2) | 4 (13.8) |
| 12 (41.4) | 17 (58.6) |
| 15 (53.6) | 13 (46.4) |
|
|
1/2 | 26 (66.7) | 13 (33.3) |
| 13 (38.1) | 26 (61.9) |
| 17 (40.5) | 25 (59.5) |
|
| Cancer type |
|
|
<0.001c |
|
| 0.146c |
|
| 0.104c |
| Chest
tumors | 30 (100.0) | 0 (0.0) |
| 16 (48.5) | 17 (51.5) |
| 18 (56.3) | 14 (43.8) |
|
| Head
neck | 21 (55.3) | 17 (44.7) |
| 12 (31.6) | 26 (68.4) |
| 14 (36.8) | 24 (63.2) |
|
| Grade |
|
| 0.211c |
|
| 0.113c |
|
| 0.123c |
|
1/2 | 24 (80.0) | 6 (20.0) |
| 17 (54.8) | 14 (45.2) |
| 19 (61.3) | 12 (38.7) |
|
| 3 | 19 (65.5) | 10 (34.5) |
| 10 (34.5) | 19 (65.5) |
| 12 (41.4) | 17 (58.6) |
|
| Stage |
|
| 0.100c |
|
| 0.888c |
|
| 0.668c |
|
I/II | 19 (86.4) | 3 (13.6) |
| 9 (40.9) | 13 (59.1) |
| 11 (50.0) | 11 (50.0) |
|
|
III/IV | 29 (67.4) | 14 (32.6) |
| 18 (39.1) | 28 (60.9) |
| 20 (44.4) | 25 (55.6) |
|
| Duration of RT,
days | 33.6±12.4 | 32.7±15.7 | 0.804a | 27.1±12.2 | 38±11.8 | 0.001a | 29.3±12.9 | 38±11.6 | 0.006a |
| Total dose,
cGY |
5,414.7±1,128.1 |
5,817.6±1,388.2 | 0.233a |
5,203.9±1,193.8 |
5,675.3±1,174.2 | 0.105a |
5,329.1±1,167.1 | 5,690±1,155.3 | 0.199a |
| Irradiation
fractions | 26.0±7.0 | 28.6±6.8 | 0.188a | 24.9±7.2 | 27.4±6.8 | 0.138a | 25.8±7.2 | 27.4±6.5 | 0.304a |
| Length of the
radiated esophagus from treatment planning, cm | 12±2.8 | 13.4±4.5 | 0.124a | 12.1±3.3 | 12.7±3.3 | 0.453a | 11.9±2.9 | 12.8±3.5 | 0.229a |
| Length of the
radiated esophagus from treatment planning, cm |
|
| 0.325c |
|
| 0.174c |
|
| 0.172c |
|
<12 | 25 (80.6) | 6 (19.4) |
| 15 (48.4) | 16 (51.6) |
| 17 (54.8) | 14 (45.2) |
|
|
>12 | 26 (70.3) | 11 (29.7) |
| 13 (32.5) | 27 (67.5) |
| 15 (38.5) | 24 (61.5) |
|
| Prior surgery |
|
|
<0.001c |
|
| 0.431c |
|
| 0.623c |
| No | 40 (90.9) | 4 (9.1) |
| 17 (36.2) | 30 (63.8) |
| 22 (47.8) | 24 (52.2) |
|
|
Yes | 11 (45.8) | 13 (54.2) |
| 11 (45.8) | 13 (54.2) |
| 10 (41.7) | 14 (58.3) |
|
| Prior
chemotherapy |
|
| 0.255c |
|
| 0.385c |
|
| 0.377c |
| No | 28 (70.0) | 12 (30.0) |
| 14 (35.0) | 26 (65.0) |
| 16 (41.0) | 23 (59.0) |
|
|
Yes | 23 (82.1) | 5 (17.9) |
| 14 (45.2) | 17 (54.8) |
| 16 (51.6) | 15 (48.4) |
|
| Concurrent
chemotherapy |
|
| 0.044c |
|
| 0.020c |
|
| 0.008c |
| No | 35 (83.3) | 7 (16.7) |
| 22 (50.0) | 22 (50.0) |
| 25 (58.1) | 18 (41.9) |
|
|
Yes | 16 (61.5) | 10 (38.5) |
| 6 (22.2) | 21 (77.8) |
| 7 (25.9) | 20 (74.1) |
|
| Only RT |
|
| 0.317c |
|
| 0.239c |
|
| 0.122c |
| No | 29 (70.7) | 12 (29.3) |
| 15 (34.1) | 29 (65.9) |
| 17 (38.6) | 27 (61.4) |
|
|
Yes | 22 (81.5) | 5 (18.5) |
| 13 (48.1) | 14 (51.9) |
| 15 (57.7) | 11 (42.3) |
|
| Subsequent
chemotherapy |
|
| 0.649c |
|
| 0.225c |
|
| 0.059c |
| No | 36 (76.6) | 11 (23.4) |
| 22 (44.0) | 28 (56.0) |
| 26 (53.1) | 23 (46.9) |
|
|
Yes | 15 (71.4) | 6 (28.6) |
| 6 (28.6) | 15 (71.4) |
| 6 (28.6) | 15 (71.4) |
|
Pain and opioid use
Table V presents
the frequencies of patients with pain, mycosis and at least one
adverse event according to demographics and clinical
characteristics. Pain grade 2 to 3 (OR: 5.067; 95% CI:
1.608-15.967; P=0.004) and mycosis (OR: 6.000; 95% CI:
2.096-17.173; P=0.001) were more frequent in those having
concurrent CT-RT. Mycosis was more frequent in cases with PS 1 to 2
(OR: 4.640; 95% CI: 1.569-13.728; P=0.004). Pain grade 2 to 3 (OR:
3.417; 95% CI: 1.108-10.553; P=0.028) and mycosis (OR: 4.667; 95%
CI: 1.568-13.886; P=0.004) were also more frequent in those having
CT after RT, while the proportion of subjects with mycosis was
lower in those treated with RT only (OR: 0.350; 95% CI:
0.123-0.994; P=0.045; Table
SI).
 | Table V.Proportion of patients with pain,
mycosis and at least one adverse event according to demographics
and clinical characteristics. |
Table V.
Proportion of patients with pain,
mycosis and at least one adverse event according to demographics
and clinical characteristics.
|
| Pain (grade) |
| Mycosis |
| At least one
adverse event |
|
|---|
|
|
|
|
|
|
|
|
|---|
| Item | 0-1 | 2-3 | P-value | No | Yes | P-value | No | Yes | P-value |
|---|
| Age, years | 66±11.5 | 63.7±10.3 | 0.462a | 65.6±10.9 | 65.1±11.7 | 0.833a | 66.7±12.1 | 64.6±1.1 | 0.631a |
| Sex |
|
| 0.763b |
|
| 0.142c |
|
| 0.375b |
|
Male | 40 (75.5) | 13 (24.5) |
| 34 (64.2) | 19 (35.8) |
| 4 (8.2) | 45 (91.8) |
|
|
Female | 13 (72.2) | 5 (27.8) |
| 8 (44.4) | 10 (55.6) |
| 3 (16.7) | 15 (83.3) |
|
| PS |
|
| 0.192c |
|
| 0.004c |
|
| 0.440b |
| 0 | 24 (82.8) | 5 (17.2) |
| 23 (79.3) | 6 (20.7) |
| 4 (14.3) | 24 (85.7) |
|
|
1/2 | 29 (69.0) | 13 (31.0) |
| 19 (45.2) | 23 (54.8) |
| 3 (7.7) | 36 (92.3) |
|
| Cancer type |
|
| 0.066c |
|
| 0.230c |
|
| 1.000b |
| Chest
tumor | 28 (84.8) | 5 (15.2) |
| 22 (66.7) | 11 (33.3) |
| 3 (10.3) | 26 (89.7) |
|
| Head
& neck | 25 (65.8) | 13 (34.2) |
| 20 (52.6) | 18 (47.4) |
| 4 (10.5) | 34 (89.5) |
|
| Grade |
|
| 0.111c |
|
| 0.073c |
|
| 0.195b |
|
1/2 | 25 (80.6) | 6 (19.4) |
| 22 (71.0) | 9 (29.0) |
| 5 (16.7) | 25 (83.3) |
|
| 3 | 18 (62.1) | 11 (37.9) |
| 14 (48.3) | 15 (51.7) |
| 1 (3.4) | 28 (96.6) |
|
| Stage |
|
| 0.284c |
|
| 0.107c |
|
| 0.220b |
|
I/II | 18 (81.8) | 4 (18.2) |
| 16 (72.7) | 6 (27.3) |
| 4 (18.2) | 18 (81.8) |
|
|
III/IV | 32 (69.6) | 14 (30.4) |
| 24 (52.2) | 22 (47.8) |
| 3 (7.1) | 39 (92.9) |
|
| Duration of RT,
days | 32.6±14.0 | 36.2±9.4 | 0.330a | 31.3±13.7 | 37±11.3 | 0.084a | 33.6±4.7 | 33.7±13.8 | 0.974a |
| Total dose,
cGY |
5,384.9±1,219.1 |
5,797.2±1,100.5 | 0.209a |
5,340.0±1,192.4 |
5,705.9±1,188.7 | 0.207a |
5,214.3±1,120.2 |
5,592.5±1,176.6 | 0.422a |
| Irradiation
fractions | 25.7±7.4 | 28.6±5.8 | 0.142a | 25.5±7.4 | 27.7±6.5 | 0.204a | 26.3±5.5 | 27±6.9 | 0.802a |
| Length of the
radiated esophagus from treatment planning, cm | 12.2±3.0 | 13.1±4.0 | 0.297a | 12.1±3.0 | 12.9±3.6 | 0.304a | 11.3±2.6 | 12.5±3.4 | 0.380a |
| Length of the
radiated esophagus from treatment planning, cm |
|
| 0.637c |
|
| 0.195c |
|
| 0.236b |
|
<12 | 24 (77.4) | 7 (22.6) |
| 21 (67.7) | 10 (32.3) |
| 5 (16.1) | 26 (83.9) |
|
|
>12 | 29 (72.5) | 11 (27.5) |
| 21 (52.5) | 19 (47.5) |
| 2 (5.6) | 34 (94.4) |
|
| Prior surgery |
|
| 0.598c |
|
| 0.541c |
|
| 1.000b |
| No | 36 (76.6) | 11 (23.4) |
| 29 (61.7) | 18 (38.3) |
| 5 (11.6) | 38 (88.4) |
|
|
Yes | 17 (70.8) | 7 (29.2) |
| 13 (54.2) | 11 (45.8) |
| 2 (8.3) | 22 (91.7) |
|
| Prior
chemotherapy |
|
| 0.637c |
|
| 0.747c |
|
| 0.690b |
| No | 29 (72.5) | 11 (27.5) |
| 23 (57.5) | 17 (42.5) |
| 5 (12.8) | 34 (87.2) |
|
|
Yes | 24 (77.4) | 7 (22.6) |
| 19 (61.3) | 12 (38.7) |
| 2 (7.1) | 26 (92.9) |
|
| Concurrent
chemotherapy |
|
| 0.004c |
|
| 0.001c |
|
| 1.000b |
| No | 38 (86.4) | 6 (13.6) |
| 33 (75.0) | 11 (25.0) |
| 4 (9.8) | 37 (90.2) |
|
|
Yes | 15 (55.6) | 12 (44.4) |
| 9 (33.3) | 18 (66.7) |
| 3 (11.5) | 23 (88.5) |
|
| Only RT |
|
| 0.110c |
|
| 0.045c |
|
| 0.417b |
| No | 30 (68.2) | 14 (31.8) |
| 22 (50.0) | 22 (50.0) |
| 3 (7.3) | 38 (92.7) |
|
|
Yes | 23 (85.2) | 4 (14.8) |
| 20 (74.1) | 7 (25.9) |
| 4 (15.4) | 22 (84.6) |
|
| Subsequent
chemotherapy |
|
| 0.028c |
|
| 0.004c |
|
| 0.419b |
| No | 41 (82.0) | 9 (18.0) |
| 35 (70.0) | 15 (30.0) |
| 6 (13.0) | 40 (87.0) |
|
|
Yes | 12 (57.1) | 9 (42.9) |
| 7 (33.3) | 14 (66.7) |
| 1 (4.8) | 20 (95.2) |
|
A total of 40 patients (56.3%) received only simple
analgesics for pain treatment, while opioid therapy with or without
analgesics was taken by 24 patients (33.8%). A total of 7 patients
(9.9%) did not report any pain and received no pain treatment
(Table III). The mean length of
the irradiated esophagus from treatment planning (P=0.024) and
duration of RT (P=0.023) were significantly greater in those to
whom opioids were administered (Table
VI). The use of opioids was more frequent in cases where the
length of the irradiated esophagus from treatment planning was
>12 cm (P=0.018; Table VI).
Contrarily, the use of opioids was less frequent in patients with
stomatitis grade 0–1 (OR: 6.667; 95% CI: 2.012-22.085; P=0.001) and
in patients with pain grade 0–1 (OR: 4.835; 95% CI: 1.553-15.052;
P=0.005; Table VII).
 | Table VI.Use of opioids according to
demographics and clinical characteristics. |
Table VI.
Use of opioids according to
demographics and clinical characteristics.
|
| Opioids |
|
|---|
|
|
|
|
|---|
| Item | No | Yes | P-value |
|---|
| Age, years | 64.9±10.6 | 66.3±12.4 | 0.621a |
| Sex |
|
| 0.532b |
|
Male | 34 (64.2) | 19 (35.8) |
|
|
Female | 13 (72.2) | 5 (27.8) |
|
| PS |
|
| 0.153b |
| 0 | 22 (75.9) | 7 (24.1) |
|
|
1/2 | 25 (59.5) | 17 (40.5) |
|
| Cancer type |
|
| 0.278b |
| Chest
tumor | 24 (72.7) | 9 (27.3) |
|
| Head
& neck | 23 (60.5) | 15 (39.5) |
|
| Grade |
|
| 0.951b |
|
1/2 | 19 (61.3) | 12 (38.7) |
|
| 3 | 18 (62.1) | 11 (37.9) |
|
| Stage |
|
| 0.134b |
|
I/II | 17 (77.3) | 5 (22.7) |
|
|
III/IV | 27 (58.7) | 19 (41.3) |
|
| Duration of RT,
days | 36.2±12.3 | 28.6±13.1 | 0.023a |
| Total dose,
cGY |
5,511.1±1,123.4 |
5,447.1±1,351.9 | 0.833a |
| Irradiation
fractions | 26.6±6.8 | 26.2±7.8 | 0.847a |
| Length of the
radiated esophagus from treatment planning, cm | 11.8±2.9 | 13.6±3.6 | 0.024a |
| Length of the
radiated esophagus from treatmentxmer planning (cm) |
|
| 0.018b |
|
<12 | 24 (77.4) | 7 (22.6) |
|
|
>12 | 23 (57.5) | 17 (42.5) |
|
| Prior surgery |
|
| 0.317b |
| No | 33 (70.2) | 14 (29.8) |
|
|
Yes | 14 (58.3) | 10 (41.7) |
|
| Prior
chemotherapy |
|
| 0.442b |
| No | 28 (70) | 12 (30) |
|
|
Yes | 19 (61.3) | 12 (38.7) |
|
| Concurrent
chemotherapy |
|
| 0.652b |
| No | 30 (68.2) | 14 (31.8) |
|
|
Yes | 17 (63) | 10 (37) |
|
| Only RT |
|
| 0.272b |
| No | 27 (61.4) | 17 (38.6) |
|
|
Yes | 20 (74.1) | 7 (25.9) |
|
| Subsequent
chemotherapy |
|
| 0.957b |
| No | 33 (66) | 17 (34) |
|
|
Yes | 14 (66.7) | 7 (33.3) |
|
 | Table VII.Use of opioids according to the
presence of adverse events. |
Table VII.
Use of opioids according to the
presence of adverse events.
|
| Opioids |
|
|---|
|
|
|
|
|---|
| Item | No | Yes | P-value |
|---|
| Stomatitis,
grade |
|
| 0.001a |
|
0/1 | 40 (87.0) | 11 (50.0) |
|
|
2/3 | 6 (13.0) | 11 (50.0) |
|
| Esophagitis,
grade |
|
| 0.075a |
|
0/1 | 22 (46.8) | 6 (25.0) |
|
|
2/3 | 25 (53.2) | 18 (75.0) |
|
| Dysphagia,
grade |
|
| 0.623a |
|
0/1 | 22 (47.8) | 10 (41.7) |
|
|
2/3 | 24 (52.2) | 14 (58.3) |
|
| Pain, grade |
|
| 0.005a |
|
0/1 | 40 (85.1) | 13 (54.2) |
|
|
2/3 | 7 (14.9) | 11 (45.8) |
|
| Mycosis |
|
| 0.103a |
| No | 31 (66.0) | 11 (45.8) |
|
|
Yes | 16 (34.0) | 13 (54.2) |
|
| At least one
adverse event |
|
| 0.412b |
| No | 6 (13.3) | 1 (4.5) |
|
|
Yes | 39 (86.7) | 21 (95.5) |
|
Weight loss
The percentages of patients who lost weight after RT
are presented in Table VIII.
Significantly greater were weight loss percentages in patients with
H&NT (OR: 2.6; 95% CI: 0.987-6.846; P=0.051), in those who had
concurrent CT (OR: 4.2; 95% CI: 1.420-12.419; P=0.007) and in those
who had CT after the RT (OR: 3.2; 95% CI: 1.016-10.076; P=0.041).
In addition, the duration of RT (P=0.001), total dose in cGY
(P<0.001), irradiation fractions (P<0.001) and length of the
irradiated esophagus from treatment planning (P=0.009) were
significantly greater in patients with weight loss. When multiple
logistic regression analysis was applied with weight loss as the
dependent variable, a significant association with the total dose
of RT and concurrent CT-RT was observed and larger doses of RT
resulted in a higher likelihood of weight loss (OR: 1.08; 95% CI:
1.02-1.14; P=0.007). In addition, patients with concurrent CT-RT
had a higher weight loss likelihood (OR: 3.21; 95% CI: 1.03-10.0;
P=0.044).
 | Table VIII.Weight loss after RT according to
demographics and clinical characteristics. |
Table VIII.
Weight loss after RT according to
demographics and clinical characteristics.
|
| Weight loss after
RT |
|
|---|
|
|
|
|
|---|
| Item | No | Yes | P-value |
|---|
| Age, years | 66.2±11.6 | 64.8±10.9 | 0.613a |
| Sex |
|
| 0.441b |
|
Male | 21 (39.6) | 32 (60.4) |
|
|
Female | 9 (50.0) | 9 (50.0) |
|
| PS |
|
| 0.393b |
| 0 | 14 (48.3) | 15 (51.7) |
|
|
1/2 | 16 (38.1) | 26 (61.9) |
|
| Cancer type |
|
| 0.051b |
| Chest
tumor | 18 (54.5) | 15 (45.5) |
|
| Head
& neck | 12 (31.6) | 26 (68.4) |
|
| Grade |
|
| 0.058b |
|
1/2 | 16 (51.6) | 15 (48.4) |
|
| 3 | 8 (27.6) | 21 (72.4) |
|
| Stage |
|
| 0.697b |
|
I/II | 8 (36.4) | 14 (63.6) |
|
|
III/IV | 19 (41.3) | 27 (58.7) |
|
| Duration of RT,
days | 27.6±13.3 | 37.7±11.3 | 0.001a |
| Total dose,
cGY |
4,919.7±1,324.7 | 5,906.3±900.0 |
<0.001a |
| Irradiation
fractions | 23.0±7.8 | 28.9±5.3 |
<0.001a |
| Length of the
radiated esophagus from treatment planning, cm | 11.3±2.3 | 13.3±3.6 | 0.009a |
| Length of the
radiated esophagus from treatment planning, cm |
|
| 0.059b |
|
<12 | 17 (54.8) | 14 (45.2) |
|
|
>12 | 13 (32.5) | 27 (67.5) |
|
| Prior surgery |
|
| 0.663b |
| No | 19 (40.4) | 28 (59.6) |
|
|
Yes | 11 (45.8) | 13 (54.2) |
|
| Prior
chemotherapy |
|
| 0.160b |
| No | 14 (35.0) | 26 (65.0) |
|
|
Yes | 16 (51.6) | 15 (48.4) |
|
| Concurrent
chemotherapy |
|
| 0.007b |
| No | 24 (54.5) | 20 (45.5) |
|
|
Yes | 6 (22.2) | 21 (77.8) |
|
| Only RT |
|
| 0.431b |
| No | 17 (38.6) | 27 (61.4) |
|
|
Yes | 13 (48.1) | 14 (51.9) |
|
| Subsequent
chemotherapy |
|
| 0.041b |
| No | 25 (50.0) | 25 (50.0) |
|
|
Yes | 5 (23.8) | 16 (76.2) |
|
Discussion
Glutamine is the most abundant amino acid in the
body. A tumor may act as a gln trap by depleting host gln stores
and resulting in cachexia. This fact led to the development of one
of the first successful metabolic therapies, L-asparaginase, for
the treatment of acute lymphoblastic leukemia (ALL) 30 years ago.
L-asparaginase is able to deplete plasma asparagine and gln, while
ALL cells, which require large amounts of gln, are affected by this
treatment (18). However,
L-asparaginase has only been proven to be effective in ALL and
certain natural killer/T-cell lymphomas, with no effect in acute
myeloid leukemia, non-Hodgkin's lymphoma and solid tumors (19). Recent studies eventually provided
evidence that explained this lack of antitumor effect of gln
deprivation, by suggesting that various tumor types may reside in
an environment where gln is profoundly limited and they adapted to
this by pursuing strategies in order to sustain their growth and
survival (20–22). In most glutamine-deprived cell
lines, induction of de novo biosynthesis of gln or
acquisition of gln through catabolism of extracellular and
intracellular proteins has been indicated to provide a source of
missing gln for cells (23).
The variation of nutrient acquisition in amino
acid-replete and amino acid-starved settings varies among different
cancer types. For instance, the response of human breast carcinoma
cells to gln deprivation was observed to exert the same effects as
lactate accumulation in tumors: Increased NF-κB activity and
subsequent stimulation of IL-8/C-X-C motif chemokine ligand 8
expression, which, in turn, promotes angiogenesis (24). In a recent study, gln
supplementation in a rat model blocked melanoma tumor growth by
suppressing epigenetically activated oncogenic pathways (25). These contradictory results from
in vitro, animal and clinical studies clearly indicate that
reliable information about the effects of supplemental gln may only
be obtained based on in vivo studies for each cancer type
separately (26). Particularly for
solid tumors, supplementation of gln was indicated to decrease
tumor growth through stimulation of the immune system and
protection of mucosal integrity (27).
Treatment for H&NT primarily involves three
modalities: Surgery, RT and CT, administered alone or in
combination. RT alone is the most common treatment for certain
types of H&NT, such as cancer of the nasopharynx, larynx and
oropharynx (28). The therapeutic
strategies employed for resectable stage III non-small cell LC
(NSCLC) include surgical resection with adjuvant CT and sequential
RT, preoperative CT with adjuvant RT, preoperative CT and RT. In
most patients with stage III NSCLC, the tumors are unresectable and
are treated with CT and RT therapy, frequently referred to as
combined modality therapy or concurrent CT-RT. For stage IV NSCLC,
treatment is based on systematic CT + palliative RT (29). In the present study, patients were
treated with sequential or concurrent CT-RT (38%) or RT alone (38%)
classified as stage III in the majority of subjects (53.6%).
According to the literature, gln doses of up to 40
g/day via total parenteral nutrition and up to 30 g/day taken
orally in divided doses were determined to be a safe and effective
treatment for mucositis and stomatitis (7). All study patients received oral gln
supplementation (15 g bid) and no gln intolerance or toxicity was
reported.
In H&NT patients on RT, oral gln was applied as
a ‘swish and swallow’ therapy with the purpose to increase
enterocyte contact and decrease the severity and duration of
stomatitis. This rationale implies that not only the dose, but also
effective penetration and local mucosal cell uptake of glutamine
are probably important (13). In
the published studies, different gln supplementation regimens were
implemented, from the first round of conventional CT and/or RT
until two weeks post-therapy, with positive results indicating
either a shorter duration or reduced severity of OM (30–39).
For patients with chest tumors and LC, as far as
esophagitis is concerned, the same beneficial results were
indicated in most studies (40–44).
First, a pilot study by Algara et al (40) assessed the usefulness of oral gln
to prevent RT-CT-induced esophagitis, along with a dosimetric
parameter of V50 predictive of esophagitis and its duration. The
randomized trials that followed (41,42)
evaluated the efficacy of oral gln in the prevention of acute
RT-induced esophagitis (ARIE) and weight loss in patients with LC.
In a study by Topkan et al (41), V55, the mean volume of the lung
receiving 55 Gy, was the only dosimetric parameter correlated with
the severity of ARIE in gln-free patients and it was concluded that
gln may be beneficial in the prevention of ARIE and weight loss in
patients with LC undergoing thoracic irradiation.
According to the results of the present study, the
adverse event of stomatitis grade 2 to 3 was significantly
associated with the cancer type; it was observed more frequently in
patients with H&NT (P=0.001), and with modality treatment;
previous surgery (P<0.001) and concurrent CT (P=0.044).
Concerning the adverse events of esophagitis and dysphagia, both
were significantly associated with concurrent CT-RT (P=0.020 and
P=0.008, respectively).
Published data so far regarding gln supplementation
focused on depicting the decrease in the incidence and/or severity
of standard of care treatment-associated toxicities in tumors of
the lung and esophagus, as well as H&NT (13,15).
For the first time, to the best of our knowledge, the present study
determined a dosimetric parameter, such as the irradiated esophagus
length from treatment planning, to be correlated with analgesic
therapy and weight loss. In patients who used opioids, the mean
length of the irradiated esophagus from treatment planning
(P=0.024) and duration of RT (P=0.023) were significantly greater.
In addition, the use of opioids was more frequent in cases where
the length of the irradiated esophagus from treatment planning was
>12 cm (P=0.018). For weight loss after RT, there was also
significant association with duration of RT (P=0.001), total dose
cGY (P<0.001), irradiation fractions (P<0.001) and length of
irradiated esophagus from treatment planning (P=0.009) and
concurrent or subsequent CT (P=0.007 and P=0.041, respectively).
The key findings and features of the present study are summarized
in Fig. 2.
The present study was not without limitations. For
example, all patients received the same dose of oral gln, and no
comparison to a control group (taking no gln), was made. Thus,
further case-control studies with larger sample sizes are required
to validate the results presented here.
In conclusion, the use of oral gln supplementation
may have an important role in reducing acute radiation toxicities,
weight loss and the need for analgesics in patients with T&UAM,
mainly if the treatment plan includes CT and RT. Most of the
clinical trials evaluating the use of oral gln in chest and H&N
tumors had positive results regarding its protective effect on the
mucositis, esophagitis and weight loss level (30–44).
The favorable efficacy and low toxicity of oral gln observed in
clinical trials provide a strong rationale for large RCTs in
patients with cancer receiving RT and/or CT (45,46).
Recent meta-analyses specifically focusing on OM in such groups of
patients concluded that gln reduces the severity of OM and the
incidence of severe OM (grade 3 and 4) (47,48).
In addition, gln reduced the incidence of opioid analgesic use,
feeding tube use, hospitalization and treatment interruption caused
by OM (46).
The present study revealed dosimetric parameters,
including the total RT dose, the irradiated esophagus length, the
concurrent CT regimen and the radiation techniques applied, which
influenced the incidence and severity of RT toxicities. Further
RCTs will help comprehensively analyze precise dosimetric
parameters from RT treatment planning, and indicate the group of
patients most likely to benefit from gln supplementation. In
addition, RCTs will help identify the appropriate individualized
dose and duration of treatment for gln supplementation according to
the specific cancer type and the applied therapeutic modality in
order to optimize its protective effect, to reduce the severity and
duration of RT toxicities, relieving the degree of mucosal
pain.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LV and NS contributed to the conception and design
of the study. ND supervised the study. ND and LV confirm the
authenticity of all the raw data. AP was involved in the patients'
clinical history and data acquisition and wrote the manuscript. LV
was involved in the patient recruitment process and in the
collection of the subjects' medical files and their evaluation. AP
and MP analyzed the data. ND, AC, DAS, GL and SK reviewed and
edited the manuscript, and contributed to the interpretation of the
data. All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Athens Medical Center (Athens, Greece; approval no.
2281/26-04-2013) and written informed consent was provided by all
participants prior to the study start.
Patient consent for publication
Not applicable.
Competing interests
DAS is the Editor-in-Chief for the journal, but had
no personal involvement in the reviewing process, or any influence
in terms of adjudicating on the final decision, for this article.
The other authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
gln
|
glutamine
|
|
RT
|
radiotherapy
|
|
CT
|
chemotherapy
|
|
H&NT
|
head and neck tumors
|
|
T&UAM
|
thoracic and upper aerodigestive
malignancies
|
|
TCA
|
tricarboxylic acid
|
|
RCT
|
randomized controlled trial
|
|
LC
|
lung cancer
|
|
ALL
|
acute lymphoblastic leukemia
|
|
ARIE
|
acute RT-induced esophagitis
|
|
NSCLC
|
non-small cell LC
|
|
OM
|
oral mucositis
|
References
|
1
|
DeBerardinis RJ and Cheng T: Q's next: The
diverse functions of glutamine in metabolism, cell biology and
cancer. Oncogene. 29:313–324. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Levine AJ and Puzio-Kuter AM: The control
of the metabolic switch in cancers by oncogenes and tumor
suppressor genes. Science. 330:1340–1344. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Barger JF and Plas DR: Balancing
biosynthesis and bioenergetics: Metabolic programs in oncogenesis.
Endocr Relat Cancer. 17:R287–R304. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cantor JR and Sabatini DM: Cancer cell
metabolism: One hallmark, many faces. Cancer Discov. 2:881–898.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Liu W, Le A, Hancock C, Lane AN, Dang CV,
Fan TW-M and Phang JM: Reprogramming of proline and glutamine
metabolism contributes to the proliferative and metabolic responses
regulated by oncogenic transcription factor c-MYC. Proc Natl Acad
Sci USA. 109:8983–8988. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chen JQ and Russo J: Dysregulation of
glucose transport, glycolysis, TCA cycle and glutaminolysis by
oncogenes and tumor suppressors in cancer cells. Biochim Biophys
Acta. 1826:370–384. 2012.PubMed/NCBI
|
|
7
|
Kuhn KS, Muscaritoli M, Wischmeyer P and
Stehle P: Glutamine as indispensable nutrient in oncology:
Experimental and clinical evidence. Eur J Nutr. 49:197–210. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Polet F and Feron O: Endothelial cell
metabolism and tumour angiogenesis: Glucose and glutamine as
essential fuels and lactate as the driving force. J Intern Med.
273:156–165. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ahluwalia GS, Grem JL, Hao Z and Cooney
DA: Metabolism and action of amino acid analog anti-cancer agents.
Pharmacol Ther. 46:243–271. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rubio IT, Cao Y, Hutchins LF, Westbrook KC
and Klimberg VS: Effect of glutamine on methotrexate efficacy and
toxicity. Ann Surg. 227:772–778; discussion 778–780. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cluntun AA, Lukey MJ, Cerione RA and
Locasale JW: Glutamine Metabolism in Cancer: Understanding the
Heterogeneity. Trends Cancer. 3:169–180. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Choi YK and Park KG: Targeting Glutamine
Metabolism for Cancer Treatment. Biomol Ther (Seoul). 26:19–28.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Anderson PM and Lalla RV: Glutamine for
Amelioration of Radiation and Chemotherapy Associated Mucositis
during Cancer Therapy. Nutrients. 12:16752020. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Savarese DM, Savy G, Vahdat L, Wischmeyer
PE and Corey B: Prevention of chemotherapy and radiation toxicity
with glutamine. Cancer Treat Rev. 29:501–513. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Papanikolopoulou A, Syrigos KN and
Drakoulis N: The role of glutamine supplementation in thoracic and
upper aerodigestive malignancies. Nutr Cancer. 67:231–237. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cox JD, Stetz J and Pajak TF: Toxicity
criteria of the Radiation Therapy Oncology Group (RTOG) and the
European Organization for Research and Treatment of Cancer (EORTC).
Int J Radiat Oncol Biol Phys. 31:1341–1346. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Subramaniam AV, Salem Yehya AH and Oon CE:
Molecular Basis of Cancer Pain Management: An Updated Review.
Medicina (Kaunas). 55:5842019. View Article : Google Scholar
|
|
18
|
van den Berg H: Asparaginase revisited.
Leuk Lymphoma. 52:168–178. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jaffe N, Traggis D, Das L, Moloney WC,
Hann HW, Kim BS and Nair R: L-asparaginase in the treatment of
neoplastic diseases in children. Cancer Res. 31:942–949.
1971.PubMed/NCBI
|
|
20
|
Jia ZY, Shen TY, Jiang W and Qin HL:
Identification of molecular mechanisms of glutamine in pancreatic
cancer. Oncol Lett. 14:6395–6402. 2017.PubMed/NCBI
|
|
21
|
Stanciu AE, Zamfir-Chiru-Anton A, Stanciu
MM, Stoian AP, Jinga V, Nitipir C, Bucur A, Pituru TS, Arsene AL,
Dragoi CM, et al: Clinical significance of serum melatonin in
predicting the severity of oral squamous cell carcinoma. Oncol
Lett. 19:1537–1543. 2020.PubMed/NCBI
|
|
22
|
Olaru OT, Venables L, VAN DE Venter M,
Nitulescu GM, Margina D, Spandidos DA and Tsatsakis AM: Anticancer
potential of selected Fallopia Adans species. Oncol Lett.
10:1323–1332. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Pavlova NN, Hui S, Ghergurovich JM, Fan J,
Intlekofer AM, White RM, Rabinowitz JD, Thompson CB and Zhang J: As
Extracellular Glutamine Levels Decline, Asparagine Becomes an
Essential Amino Acid. Cell Metab. 27:428–438.e5. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bobrovnikova-Marjon EV, Marjon PL, Barbash
O, Vander Jagt DL and Abcouwer SF: Expression of angiogenic factors
vascular endothelial growth factor and interleukin-8/CXCL8 is
highly responsive to ambient glutamine availability: Role of
nuclear factor-kappaB and activating protein-1. Cancer Res.
64:4858–4869. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ishak Gabra MB, Yang Y, Li H, Senapati P,
Hanse EA, Lowman XH, Tran TQ, Zhang L, Doan LT, Xu X, et al:
Dietary glutamine supplementation suppresses
epigenetically-activated oncogenic pathways to inhibit melanoma
tumour growth. Nat Commun. 11:33262020. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhang J, Pavlova NN and Thompson CB:
Cancer cell metabolism: The essential role of the nonessential
amino acid, glutamine. EMBO J. 36:1302–1315. 2017. View Article : Google Scholar
|
|
27
|
García-de-Lorenzo A, Zarazaga A,
García-Luna PP, Gonzalez-Huix F, López-Martínez J, Miján A, Quecedo
L, Casimiro C, Usán L and del Llano J: Clinical evidence for
enteral nutritional support with glutamine: A systematic review.
Nutrition. 19:805–811. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Marur S and Forastiere AA: Head and Neck
Squamous Cell Carcinoma: Update on Epidemiology, Diagnosis, and
Treatment. Mayo Clin Proc. 91:386–396. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Bayman NA, Blackhall F, Jain P, Lee L,
Thatcher N and Faivre-Finn C: Management of unresectable stage III
non-small-cell lung cancer with combined-modality therapy: A review
of the current literature and recommendations for treatment. Clin
Lung Cancer. 9:92–101. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Huang EY, Leung SW, Wang CJ, Chen HC, Sun
LM, Fang FM, Yeh SA, Hsu HC and Hsiung CY: Oral glutamine to
alleviate radiation-induced oral mucositis: A pilot randomized
trial. Int J Radiat Oncol Biol Phys. 46:535–539. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Sarumathy S, Ismail AM and Palasimany A:
Efficacy and safety of oral glutamine in radiation induced oral
mucositis in patients with Head and Neck cancer. Asian J Pharm Clin
Res. 5:138–140. 2012.
|
|
32
|
Zygogianni A, Kyrgias G, Kouvaris J,
Pistevou-Gombaki K, Capezzali G, Zefkili S, Kokkakis J,
Georgakopoulos J, Kelekis K and Kouloulias V: Impact of acute
radiation induced toxicity of glutamine administration in several
hypofractionated irradiation schedules for head and neck carcinoma.
Head Neck Oncol. 4:86–92. 2012.
|
|
33
|
Chattopadhyay S, Saha A, Azam M, Mukherjee
A and Sur PK: Role of oral glutamine in alleviation and prevention
of radiation-induced oral mucositis: A prospective randomized
study. South Asian J Cancer. 3:8–12. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Tsujimoto T, Yamamoto Y, Wasa M, Takenaka
Y, Nakahara S, Takagi T, Tsugane M, Hayashi N, Maeda K, Inohara H,
et al: L-glutamine decreases the severity of mucositis induced by
chemoradiotherapy in patients with locally advanced head and neck
cancer: A double-blind, randomized, placebo-controlled trial. Oncol
Rep. 33:33–39. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Pattanayak L, Panda N, Dash MK, Mohanty S
and Samantaray S: Management of Chemoradiation-Induced Mucositis in
Head and Neck Cancers With Oral Glutamine. J Glob Oncol. 2:200–206.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Lopez-Vaquero D, Gutierrez-Bayard L,
Rodriguez-Ruiz JA, Saldaña-Valderas M and Infante-Cossio P:
Double-blind randomized study of oral glutamine on the management
of radio/chemotherapy-induced mucositis and dermatitis in head and
neck cancer. Mol Clin Oncol. 6:931–936. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Pachón Ibáñez J, Pereira Cunill JL, Osorio
Gómez GF, Irles Rocamora JA, Serrano Aguayo P, Quintana Ángel B,
Fuentes Pradera J, Chaves Conde M, Ortiz Gordillo MJ and García
Luna PP: Prevention of oral mucositis secondary to antineoplastic
treatments in head and neck cancer by supplementation with oral
glutamine. Nutr Hosp. 35:428–433. 2018.PubMed/NCBI
|
|
38
|
Huang CJ, Huang MY, Fang PT, Chen F, Wang
YT, Chen CH, Yuan SS, Huang CM, Luo KH, Chuang HY, et al:
Randomized double-blind, placebo-controlled trial evaluating oral
glutamine on radiation-induced oral mucositis and dermatitis in
head and neck cancer patients. Am J Clin Nutr. 109:606–614. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Pathak S, Soni TP, Sharma LM, Patni N and
Gupta AK: A Randomized Controlled Trial to Evaluate the Role and
Efficacy of Oral Glutamine in the Treatment of
Chemo-radiotherapy-induced Oral Mucositis and Dysphagia in Patients
with Oropharynx and Larynx Carcinoma. Cureus.
11:e48552019.PubMed/NCBI
|
|
40
|
Algara M, Rodríguez N, Viñals P, Lacruz M,
Foro P, Reig A, Quera J, Lozano J, Fernández-Velilla E, Membrive I,
et al: Prevention of radiochemotherapy-induced esophagitis with
glutamine: Results of a pilot study. Int J Radiat Oncol Biol Phys.
69:342–349. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Topkan E, Yavuz MN, Onal C and Yavuz AA:
Prevention of acute radiation-induced esophagitis with glutamine in
non-small cell lung cancer patients treated with radiotherapy:
Evaluation of clinical and dosimetric parameters. Lung Cancer.
63:393–399. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Topkan E, Parlak C, Topuk S and Pehlivan
B: Influence of oral glutamine supplementation on survival outcomes
of patients treated with concurrent chemoradiotherapy for locally
advanced non-small cell lung cancer. BMC Cancer. 12:502–512. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Gul K, Muge A, Taner A and Sehri E: Oral
glutamine supplementation reduces radiotherapy- induced esophagitis
in lung cancer patients. Asian Pac J Cancer Prev. 16:53–58. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Chang SC, Lai YC, Hung JC and Chang CY:
Oral glutamine supplements reduce concurrent
chemoradiotherapy-induced esophagitis in patients with advanced
non-small cell lung cancer. Medicine (Baltimore). 98:e144632019.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Sayles C, Hickerson SC, Bhat RR, Hall J,
Garey KW and Trivedi MV: Oral Glutamine in Preventing
Treatment-Related Mucositis in Adult Patients With Cancer: A
Systematic Review. Nutr Clin Pract. 31:171–179. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Leung HW and Chan AL: Glutamine in
Alleviation of Radiation-Induced Severe Oral Mucositis: A
Meta-Analysis. Nutr Cancer. 68:734–742. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Tang G, Huang W, Zhang L and Wei Z: Role
of Glutamine in the Management of Oral Mucositis in Patients with
Cancer: A Meta-Analysis of Randomized Controlled Trials. Nutr
Cancer. 19:1–14. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Peng TR, Lin HH, Yang LJ and Wu TW:
Correction to: Effectiveness of glutamine in the management of oral
mucositis in cancer patients: a meta-analysis of randomized
controlled trials. Support Care Cancer. 29:48932021. View Article : Google Scholar : PubMed/NCBI
|