|
1
|
Kuhn E, Morbini P, Cancellieri A, Damiani
S, Cavazza A and Comin CE: Adenocarcinoma classification: Patterns
and prognosis. Pathologica. 110:5–11. 2018.
|
|
2
|
Herbst RS, Morgensztern D and Boshoff C:
The biology and management of non-small cell lung cancer. Nature.
553:446–454. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hynds RE, Ben Aissa A, Gowers KHC, Watkins
TBK, Bosshard-Carter L, Rowan AJ, Veeriah S, Wilson GA, Quezada SA,
Swanton C, et al: Expansion of airway basal epithelial cells from
primary human non-small cell lung cancer tumors. Int J Cancer.
143:160–166. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ding Y, Zhang L, Guo L, Wu C, Zhou J, Zhou
Y, Ma J, Li X, Ji P, Wang M, et al: Comparative study on the
mutational profile of adenocarcinoma and squamous cell carcinoma
predominant histologic subtypes in Chinese non-small cell lung
cancer patients. Thorac Cancer. 11:103–112. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wang X and Adjei AA: Lung cancer and
metastasis: New opportunities and challenges. Cancer Metastasis
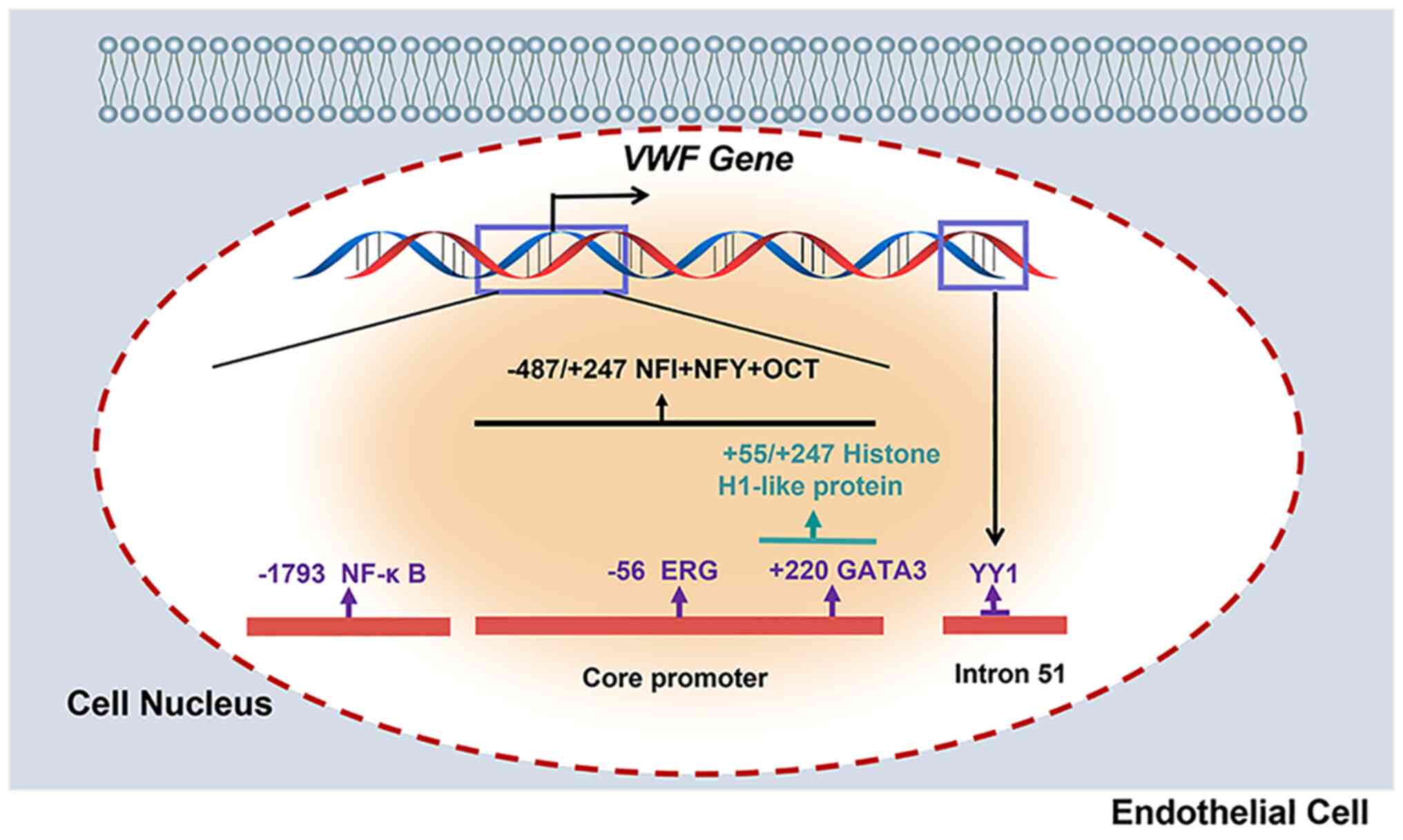
Rev. 34:169–171. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2018. CA Cancer J Clin. 68:7–30. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
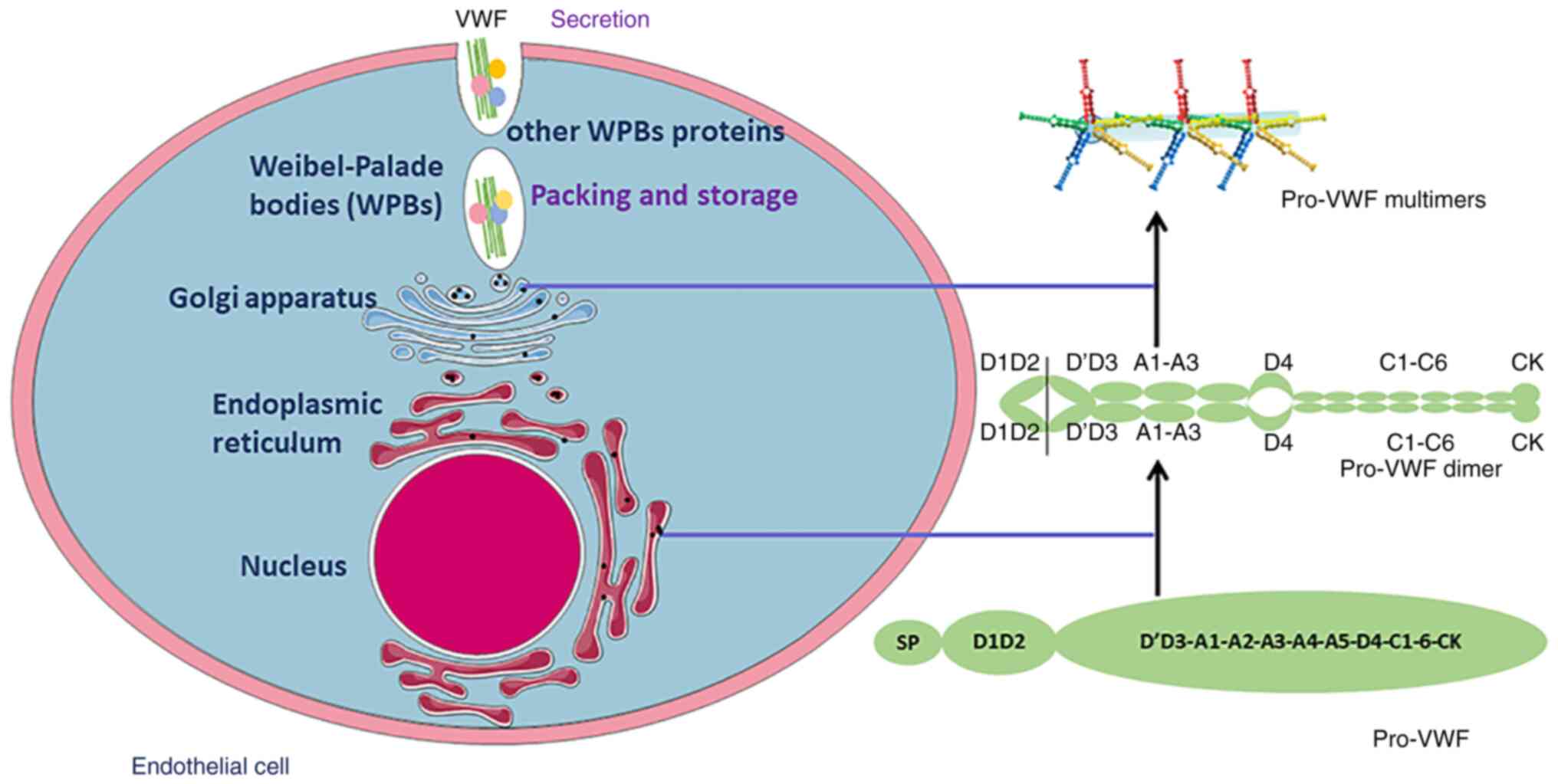
7
|
Liu B and Wei C: Hypoxia induces
overexpression of CCL28 to recruit treg cells to enhance
angiogenesis in lung adenocarcinoma. J Environ Pathol Toxicol
Oncol. 40:65–74. 2021. View Article : Google Scholar
|
|
8
|
Zahn LM: Effects of the tumor
microenvironment. Science. 355:1386–1388. 2017. View Article : Google Scholar
|
|
9
|
Lugano R, Ramachandran M and Dimberg A:
Tumor angiogenesis: Causes, consequences, challenges and
opportunities. Cell Mol Life Sci. 77:1745–1770. 2020. View Article : Google Scholar
|
|
10
|
Liu F, Wang B, Li L, Dong F, Chen X, Li Y,
Dong X, Wada Y, Kapron CM and Liu J: Low-dose cadmium upregulates
VEGF expression in lung adenocarcinoma cells. Int J Environ Res
Public Health. 12:10508–10521. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liu J, Li Y, Dong F, Li L, Masuda T, Allen
TD and Lobe CG: Trichostatin A suppresses lung adenocarcinoma
development in Grg1 overexpressing transgenic mice. Biochem Biophys
Res Commun. 463:1230–1236. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Frezzetti D, Gallo M, Maiello MR,
D'Alessio A, Esposito C, Chicchinelli N, Normanno N and De Luca A:
VEGF as a potential target in lung cancer. Expert Opin Ther
Targets. 21:959–966. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fuchs CS, Tomasek J, Yong CJ, Dumitru F,
Passalacqua R, Goswami C, Safran H, Dos Santos LV, Aprile G, Ferry
DR, et al: Ramucirumab monotherapy for previously treated advanced
gastric or gastro-oesophageal junction adenocarcinoma (REGARD): an
international, randomised, multicentre, placebo-controlled, phase 3
trial. Lancet. 383:31–39. 2014. View Article : Google Scholar
|
|
14
|
Kurzrock R and Stewart DJ: Exploring the
Benefit/Risk associated with antiangiogenic agents for the
treatment of non-small cell lung cancer patients. Clin Cancer Res.
23:1137–1148. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Starke RD, Ferraro F, Paschalaki KE,
Dryden NH, McKinnon TA, Sutton RE, Payne EM, Haskard DO, Hughes AD,
Cutler DF, et al: Endothelial von Willebrand factor regulates
angiogenesis. Blood. 117:1071–1080. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Löf A, Müller JP and Brehm MA: A
biophysical view on von Willebrand factor activation. J Cell
Physiol. 233:799–810. 2018. View Article : Google Scholar
|
|
17
|
Kremer Hovinga JA, Coppo P, Lämmle B,
Moake JL, Miyata T and Vanhoorelbeke K: Thrombotic thrombocytopenic
purpura. Nat Rev Dis Primers. 3:170202017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sadler JE: Pathophysiology of thrombotic
thrombocytopenic purpura. Blood. 130:1181–1188. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhou YF, Eng ET, Zhu J, Lu C, Walz T and
Springer TA: Sequence and structure relationships within von
Willebrand factor. Blood. 120:449–458. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chen J, Schroeder JA, Luo X and Shi Q: The
impact of von Willebrand factor on factor VIII memory immune
responses. Blood Adv. 1:1565–1574. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
O'Sullivan JM, Preston RJS, Robson T and
O'Donnell JS: Emerging roles for von willebrand factor in cancer
cell biology. Semin Thromb Hemost. 44:159–166. 2018. View Article : Google Scholar
|
|
22
|
Kawecki C, Lenting PJ and Denis CV: von
Willebrand factor and inflammation. J Thromb Haemost. 15:1285–1294.
2017. View Article : Google Scholar
|
|
23
|
Wang X, Zhao J, Zhang Y, Xue X, Yin J,
Liao L, Xu C, Hou Y, Yan S and Liu J: Kinetics of plasma von
Willebrand factor in acute myocardial infarction patients: A
meta-analysis. Oncotarget. 8:90371–90379. 2017. View Article : Google Scholar
|
|
24
|
Li Y, Li L, Dong F, Guo L, Hou Y, Hu H,
Yan S, Zhou X, Liao L, Allen TD and Liu JU: Plasma von Willebrand
factor level is transiently elevated in a rat model of acute
myocardial infarction. Exp Ther Med. 10:1743–1749. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Peng X, Wang X, Fan M, Zhao J, Lin L and
Liu J: Plasma levels of von Willebrand factor in type 2 diabetes
patients with and without cardiovascular diseases: A meta-analysis.
Diabetes Metab Res Rev. 36:e31932020. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Fan M, Wang X, Peng X, Feng S, Zhao J,
Liao L, Zhang Y, Hou Y and Liu J: Prognostic value of plasma von
Willebrand factor levels in major adverse cardiovascular events: A
systematic review and meta-analysis. BMC Cardiovasc Disord.
20:722020. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Randi AM, Smith KE and Castaman G: von
Willebrand factor regulation of blood vessel formation. Blood.
132:132–140. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Guo R, Yang J, Liu X, Wu J and Chen Y:
Increased von Willebrand factor over decreased ADAMTS-13 activity
is associated with poor prognosis in patients with advanced
non-small-cell lung cancer. J Clin Lab Anal. 32:e222192018.
View Article : Google Scholar
|
|
29
|
Marfia G, Navone SE, Fanizzi C, Tabano S,
Pesenti C, Abdel Hadi L, Franzini A, Caroli M, Miozzo M, Riboni L,
et al: Prognostic value of preoperative von Willebrand factor
plasma levels in patients with Glioblastoma. Cancer Med.
5:1783–1790. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Obermeier HL, Riedl J, Ay C, Koder S,
Quehenberger P, Bartsch R, Kaider A, Zielinski CC and Pabinger I:
The role of ADAMTS-13 and von Willebrand factor in cancer patients:
Results from the vienna cancer and thrombosis Study. Res Pract
Thromb Haemost. 3:503–514. 2019. View Article : Google Scholar
|
|
31
|
Pépin M, Kleinjan A, Hajage D, Büller HR,
Di Nisio M, Kamphuisen PW, Salomon L, Veyradier A, Stepanian A and
Mahé I: ADAMTS-13 and von Willebrand factor predict venous
thromboembolism in patients with cancer. J Thromb Haemost.
14:306–315. 2016. View Article : Google Scholar
|
|
32
|
Qi Y, Chen W, Liang X, Xu K, Gu X, Wu F,
Fan X, Ren S, Liu J, Zhang J, et al: Novel antibodies against GPIbα
inhibit pulmonary metastasis by affecting vWF-GPIbα interaction. J
Hematol Oncol. 11:1172018. View Article : Google Scholar
|
|
33
|
Jin E, Ghazizadeh M, Fujiwara M, Nagashima
M, Shimizu H, Ohaki Y, Arai S, Gomibuchi M, Takemura T and Kawanami
O: Angiogenesis and phenotypic alteration of alveolar capillary
endothelium in areas of neoplastic cell spread in primary lung
adenocarcinoma. Pathol Int. 51:691–700. 2001. View Article : Google Scholar
|
|
34
|
Xu Y, Pan S, Liu J, Dong F, Cheng Z, Zhang
J, Qi R, Zang Q, Zhang C, Wang X, et al: GATA3-induced vWF
upregulation in the lung adenocarcinoma vasculature. Oncotarget.
8:110517–110529. 2017. View Article : Google Scholar
|
|
35
|
Morishita C, Jin E, Kikuchi M, Egawa S,
Fujiwara M, Ohaki Y, Ghazizadeh M, Takemura T and Kawanami O:
Angiogenic switching in the alveolar capillaries in primary lung
adenocarcinoma and squamous cell carcinoma. J Nippon Med Sch.
74:344–354. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
He Y, Liu R, Yang M, Bi W, Zhou L, Zhang
S, Jin J, Liang X and Zhang P: Identification of VWF as a novel
biomarker in lung adenocarcinoma by comprehensive analysis. Front
Oncol. 11:6396002021. View Article : Google Scholar
|
|
37
|
Liu J, Yuan L, Molema G, Regan E, Janes L,
Beeler D, Spokes KC, Okada Y, Minami T, Oettgen P and Aird WC:
Vascular bed-specific regulation of the von Willebrand factor
promoter in the heart and skeletal muscle. Blood. 117:342–351.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Liu J, Kanki Y, Okada Y, Jin E, Yano K,
Shih SC, Minami T and Aird WC: A +220 GATA motif mediates basal but
not endotoxin-repressible expression of the von Willebrand factor
promoter in Hprt-targeted transgenic mice. J Thromb Haemost.
7:1384–1392. 2010. View Article : Google Scholar
|
|
39
|
Yuan L, Sacharidou A, Stratman AN, Le Bras
A, Zwiers PJ, Spokes K, Bhasin M, Shih SC, Nagy JA, Molema G, et
al: RhoJ is an endothelial cell-restricted Rho GTPase that mediates
vascular morphogenesis and is regulated by the transcription factor
ERG. Blood. 118:1145–1153. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Liu F, Liu Q, Yuan F, Guo S and Liu J, Sun
Z, Gao P, Wang Y, Yan S and Liu J: Erg mediates downregulation of
claudin-5 in the brain endothelium of a murine experimental model
of cerebral malaria. FEBS Lett. 593:2585–2595. 2019. View Article : Google Scholar
|
|
41
|
Wang X, Dong F, Wang F, Yan S, Chen X,
Tozawa H, Ushijima T, Kapron CM, Wada Y and Liu J: Low dose cadmium
upregulates the expression of von Willebrand factor in endothelial
cells. Toxicol Lett. 290:46–54. 2018. View Article : Google Scholar
|
|
42
|
Stockschlaeder M, Schneppenheim R and
Budde U: Update on von Willebrand factor multimers: Focus on
high-molecular-weight multimers and their role in hemostasis. Blood
Coagul Fibrinolysis. 25:206–216. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Kleinschmidt AM, Nassiri M, Stitt MS,
Wasserloos K, Watkins SC, Pitt BR and Jahroudi N: Sequences in
intron 51 of the von Willebrand factor gene target promoter
activation to a subset of lung endothelial cells in transgenic
mice. J Biol Chem. 283:2741–2750. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Nassiri M, Liu J, Kulak S, Uwiera RR, Aird
WC, Ballermann BJ and Jahroudi N: Repressors NFI and NFY
participate in organ-specific regulation of von Willebrand factor
promoter activity in transgenic mice. Arterioscler Thromb Vasc
Biol. 30:1423–1429. 2010. View Article : Google Scholar
|
|
45
|
Harvey PJ, Keightley AM, Lam YM, Cameron C
and Lillicrap D: A single nucleotide polymorphism at
nucleotide-1793 in the von Willebrand factor (VWF) regulatory
region is associated with plasma VWF: Ag levels. Br J Haematol.
109:349–353. 2000. View Article : Google Scholar
|
|
46
|
Lenting PJ, Christophe OD and Denis CV:
von Willebrand factor biosynthesis, secretion, and clearance:
Connecting the far ends. Blood. 125:2019–2028. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Zeng J, Shu Z, Liang Q, Zhang J, Wu W,
Wang X and Zhou A: Structural basis of Von Willebrand Factor
multimerization and tubular storage. Blood. 5–Feb;2022.doi:
10.1182/blood.2021014729. View Article : Google Scholar
|
|
48
|
van den Biggelaar M, Bierings R, Storm G,
Voorberg J and Mertens K: Requirements for cellular co-trafficking
of factor VIII and von Willebrand factor to Weibel-Palade bodies. J
Thromb Haemost. 5:2235–2242. 2007. View Article : Google Scholar
|
|
49
|
Lopes da Silva M and Cutler DF: von
Willebrand factor multimerization and the polarity of secretory
pathways in endothelial cells. Blood. 128:277–285. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Randi AM and Laffan MA: Von Willebrand
factor and angiogenesis: Basic and applied issues. J Thromb
Haemost. 15:13–20. 2017. View Article : Google Scholar
|
|
51
|
Brooks PC, Montgomery AM, Rosenfeld M,
Reisfeld RA, Hu T, Klier G and Cheresh DA: Integrin alpha v beta 3
antagonists promote tumor regression by inducing apoptosis of
angiogenic blood vessels. Cell. 79:1157–1164. 1994. View Article : Google Scholar
|
|
52
|
Sartori A, Portioli E, Battistini L,
Calorini L, Pupi A, Vacondio F, Arosio D, Bianchini F and Zanardi
F: Synthesis of Novel c(AmpRGD)-sunitinib dual conjugates as
molecular tools targeting the αvβ3
Integrin/VEGFR2 couple and impairing tumor-associated angiogenesis.
J Med Chem. 60:248–262. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Somanath PR, Malinin NL and Byzova TV:
Cooperation between integrin alphavbeta3 and VEGFR2 in
angiogenesis. Angiogenesis. 12:177–1185. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Lagrange J, Worou ME, Michel JB, Raoul A,
Didelot M, Muczynski V, Legendre P, Plénat F, Gauchotte G,
Lourenco-Rodrigues MD, et al: The VWF/LRP4/αVβ3-axis represents a
novel pathway regulating proliferation of human vascular smooth
muscle cells. Cardiovasc Res. 118:622–637. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Patsenker E, Popov Y, Stickel F, Schneider
V, Ledermann M, Sägesser H, Niedobitek G, Goodman SL and Schuppan
D: Pharmacological inhibition of integrin alphavbeta3 aggravates
experimental liver fibrosis and suppresses hepatic angiogenesis.
Hepatology. 50:1501–1511. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Cossutta M, Darche M, Carpentier G, Houppe
C, Ponzo M, Raineri F, Vallée B, Gilles ME, Villain D, Picard E, et
al: Weibel-Palade bodies orchestrate pericytes during angiogenesis.
Arterioscler Thromb Vasc Biol. 39:1843–1858. 2019. View Article : Google Scholar
|
|
57
|
Barton WA, Tzvetkova-Robev D, Miranda EP,
Kolev MV, Rajashankar KR, Himanen JP and Nikolov DB: Crystal
structures of the Tie2 receptor ectodomain and the
angiopoietin-2-Tie2 complex. Nat Struct Mol Biol. 13:524–532. 2006.
View Article : Google Scholar
|
|
58
|
Xu H, Cao Y, Yang X, Cai P, Kang L, Zhu X,
Luo H, Lu L, Wei L, Bai X, et al: ADAMTS13 controls vascular
remodeling by modifying VWF reactivity during stroke recovery.
Blood. 130:11–22. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Scholz A, Plate KH and Reiss Y:
Angiopoietin-2: A multifaceted cytokine that functions in both
angiogenesis and inflammation. Ann N Y Acad Sci. 1347:45–51. 2015.
View Article : Google Scholar
|
|
60
|
Siveen KS, Prabhu K, Krishnankutty R,
Kuttikrishnan S, Tsakou M, Alali FQ, Dermime S, Mohammad RM and
Uddin S: Vascular endothelial growth factor (VEGF) signaling in
tumour vascularization: Potential and challenges. Curr Vasc
Pharmacol. 15:339–351. 2017. View Article : Google Scholar
|
|
61
|
Saint-Lu N, Oortwijn BD, Pegon JN, Odouard
S, Christophe OD, de Groot PG, Denis CV and Lenting PJ:
Identification of galectin-1 and galectin-3 as novel partners for
von Willebrand factor. Arterioscler Thromb Vasc Biol. 32:894–901.
2012. View Article : Google Scholar
|
|
62
|
Tamura K, Hashimoto K, Suzuki K, Yoshie M,
Kutsukake M and Sakurai T: Insulin-like growth factor binding
protein-7 (IGFBP7) blocks vascular endothelial cell growth factor
(VEGF)-induced angiogenesis in human vascular endothelial cells.
Eur J Pharmacol. 610:61–67. 2009. View Article : Google Scholar
|
|
63
|
Pace A, Mandoj C, Antenucci A, Villani V,
Sperduti I, Casini B, Carosi M, Fabi A, Vidiri A, Koudriavtseva T
and Conti L: A predictive value of von Willebrand factor for early
response to Bevacizumab therapy in recurrent glioma. J Neurooncol.
138:527–535. 2018. View Article : Google Scholar
|
|
64
|
Ishihara J, Ishihara A, Starke RD,
Peghaire CR, Smith KE, McKinnon TAJ, Tabata Y, Sasaki K, White MJV,
Fukunaga K, et al: The heparin binding domain of von Willebrand
factor binds to growth factors and promotes angiogenesis in wound
healing. Blood. 133:2559–2569. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Bauer AT, Suckau J, Frank K, Desch A,
Goertz L, Wagner AH, Hecker M, Goerge T, Umansky L, Beckhove P, et
al: von Willebrand factor fibers promote cancer-associated platelet
aggregation in malignant melanoma of mice and humans. Blood.
125:3153–3163. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Lancellotti S, Sacco M, Basso M and De
Cristofaro R: Mechanochemistry of von Willebrand factor. Biomol
Concepts. 10:194–208. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Kappler S, Ronan-Bentle S and Graham A:
Thrombotic microangiopathies (TTP, HUS, HELLP). Hematol Oncol Clin
North Am. 31:1081–1103. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Takaya H, Uemura M, Fujimura Y, Matsumoto
M, Matsuyama T, Kato S, Morioka C, Ishizashi H, Hori Y, Fujimoto M,
et al: ADAMTS13 activity may predict the cumulative survival of
patients with liver cirrhosis in comparison with the
Child-Turcotte-Pugh score and the Model for End-stage liver disease
score. Hepatol Res. 42:459–472. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Claus RA, Bockmeyer CL, Budde U, Kentouche
K, Sossdorf M, Hilberg T, Schneppenheim R, Reinhart K, Bauer M,
Brunkhorst FM and Lösche W: Variations in the ratio between von
Willebrand factor and its cleaving protease during systemic
inflammation and association with severity and prognosis of organ
failure. Thromb Haemost. 101:239–247. 2009. View Article : Google Scholar
|
|
70
|
Yang R, Zhou Y, Du C and Wu Y:
Bioinformatics analysis of differentially expressed genes in tumor
and paracancerous tissues of patients with lung adenocarcinoma. J
Thorac Dis. 12:7355–7364. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Federici AB: The use of desmopressin in
von Willebrand disease: The experience of the first 30 years
(1977–2007). Haemophilia. 14 (Suppl 1):S5–S14. 2008. View Article : Google Scholar
|
|
72
|
Gill JC, Castaman G, Windyga J, Kouides P,
Ragni M, Leebeek FW, Obermann-Slupetzky O, Chapman M, Fritsch S,
Pavlova BG, et al: Hemostatic efficacy, safety, and
pharmacokinetics of a recombinant von Willebrand factor in severe
von Willebrand disease. Blood. 126:2038–2046. 2015. View Article : Google Scholar : PubMed/NCBI
|