Introduction
Hepatocellular carcinoma (HCC) is currently the
sixth most frequently occurring malignant tumor and ranks fourth in
terms of cancer-related mortality (1). Sorafenib, an oral tyrosine kinase
inhibitor, has been associated with increased survival in patients
with HCC (2). However, because
12–32% of patients with HCC have vascular invasion as well as
distant metastases at diagnosis (3), the efficacy of sorafenib in these
patients is limited (4,5). As a result, combination therapy may
be more beneficial. Current therapy options include vascular
interventions, local ablation therapy, external radiation therapy,
targeted drug therapy, immunotherapy and systemic chemotherapy
(6). Hepatic arterial intervention
therapy is widely used for its benefits, which include improved
tumor-targeting ability, reduced effect on surrounding normal
tissues and a lower incidence of serious adverse events (SAEs).
However, using transcatheter arterial chemoembolization (TACE) to
achieve complete embolization in the treatment of giant HCC is
challenging and may increase the incidence of SAEs; additionally,
multiple TACE interventions may cause liver injury and negatively
affect patient prognosis (7).
Hepatic artery infusion chemotherapy (HAIC) with portal vein tumor
thrombosis (PVTT) is recommended as the first-line treatment for
HCC in Japan due to its stability, safety and high conversion rate
(8). Moreover, its efficacy in
large HCC has been shown to be superior to that of TACE in other
studies (9,10).
Although the overall response rate (ORR) of
cisplatin and 5-fluorouracil (5-FU)-based HAIC (PF-HAIC), the most
commonly used HAIC regimen in Japan, can reach 27.6 to 40.5%
(11), it is questionable whether
HAIC is superior to TACE in combination therapy. A previous
meta-analysis showed that HAIC combined with sorafenib was not
effective in prolonging survival compared with sorafenib alone
(12), while a meta-analysis by Li
et al (13) demonstrated
that TACE combined with sorafenib significantly prolonged survival
compared with sorafenib alone, despite a greater number of reported
adverse events (AEs) during treatment. Given that these studies
included patients with advanced HCC, whether high-dose chemotherapy
is more effective than vascular embolization is debatable. Studies
conducted in recent years have shown that the clinical efficacy of
HAIC-oxaliplatin is much improved when used as a combination
therapy. A head-to-head study of 5-FU, leucovorin and oxaliplatin
(FOLFOX)-HAIC vs. TACE also demonstrated a clear advantage of the
former in terms of efficacy and safety (14); however, numerous questions remain
regarding this study (15,16). Therefore, additional randomized
controlled trials (RCTs) are warranted to determine whether the
efficacy of HAIC is influenced by the treatment modality or
therapeutic regimen.
There is a lack of evidence from trials in which
different interventional modalities and various regimens for HAIC
have been directly compared; thus, a network meta-analysis can
assist in the comparison of two or more therapies that have not
been directly compared. In the present study, to aid physicians in
the selection of appropriate interventions and regimens, HCC was
stratified into primary and secondary cancers due to their
different pathogenesis, and only clinical prospective RCTs related
to primary HCC were included to eliminate bias in the analysis. A
network meta-analysis of the included RCTs was performed to assess
the survival and incidence of AEs in patients with unresectable
liver cancer receiving different HAIC regimens or TACE.
Materials and methods
Protocol and registration
The present study followed the PRISMA guidelines
(17) and was preliminarily
registered on PROSPERO (registration no. CRD42021288497). The
systematic review was conducted in accordance with the previously
established protocol outlined in Appendix S1.
Literature retrieval process
Potentially relevant and eligible studies published
before April 2022 were systemically retrieved from electronic
databases including PubMed, Cochrane Library and Embase. The PubMed
database was searched with keywords including ‘unresectable
hepatocellular carcinoma’, ‘unresectable HCC’, ‘HAIC’, ‘hepatic
arterial infusion chemotherapy’, ‘TACE’ and ‘transcatheter arterial
chemoembolization’. The search strategy is detailed in Appendix
S2.
Study inclusion and exclusion
criteria
The study inclusion criteria were as follows: RCTs;
studies that included patients diagnosed with advanced HCC; studies
with complete data on methodology, patients’ characteristics, AEs
and overall survival (OS); and studies comparing ≥2 arms that
consisted of the modalities of interest, including sorafenib alone,
TACE with sorafenib, and HAIC with sorafenib. The study exclusion
criteria were as follows: Letters to the editor, study protocols,
conference abstracts, case reports, non-RCTs, animal studies,
editorials and posters. In addition, only reports in English were
included in the study.
Literature screening
Two reviewers (XLC and HCY) independently evaluated
all titles and abstracts. Additionally, all references cited by
enrolled studies were manually reviewed to identify additional
potentially eligible studies. Articles were further screened in a
stepwise fashion according to their abstract and then full-text
using the aforementioned inclusion and exclusion criteria. Any
disagreements were resolved through consensus and the opinion of a
third reviewer (QGF).
Data extraction and quality
assessment
The first author's name, publication year,
population characteristics, number of patients in each treatment
arm and outcomes including OS, ORR, SAEs, hazard ratios (HRs) and
95% confidence intervals (CIs) were extracted. Moreover,
information about the trial design, interventions and comparators,
statistical analysis, primary and secondary outcomes and quality of
life outcomes were also retrieved.
Risk of bias assessment and data
analyses
De-duplication of retrieved documents was performed
via EndNote X9 (Clarivate). The quality of the included studies was
assessed using the Cochrane risk of bias tool (version 5.1.0; The
Cochrane Institute). Two reviewers (XLC and HCY) evaluated each
study for bias and rated it as follows: Low risk of bias, high risk
of bias or unclear. Unclear was defined as either the lack of
information to determine bias or uncertainty for bias.
The network meta-analysis was conducted in R package
(4.1.2) using the gemtc package (1.0-1). This package uses a
Bayesian Markov chain Monte Carlo sampler to run the model with
50,000 adaptation or ‘burn-in’ samples followed by 100,000 samples
without thinning. Model convergence was established by the visual
inspection of Brook-Gelman Rubin plots. As the analyses used a
contrast-based approach for OS data, the analysis assumed that the
data conformed to the proportional hazards assumption. Certain
survival data were extracted from the survival curves according to
the methods described by Parmar et al (18) and Wang and Zeng (19). Methods were as described in the
Cochrane Handbook for Systematic Reviews of Interventions (20). For Kaplan-Meier data, the
proportional hazards assumption was tested by fitting a Cox
proportional hazards regression model to the time-to-event data and
assessing whether the Schoenfeld residuals from the Cox model were
independent of time. HRs with 95% CIs were calculated to explore
the efficacy of various treatment options on OS, odds ratios (ORs)
with 95% CI were used for ORR, whereas risk ratios (RRs) with 95%
CI were used for SAEs.
Results
Screening
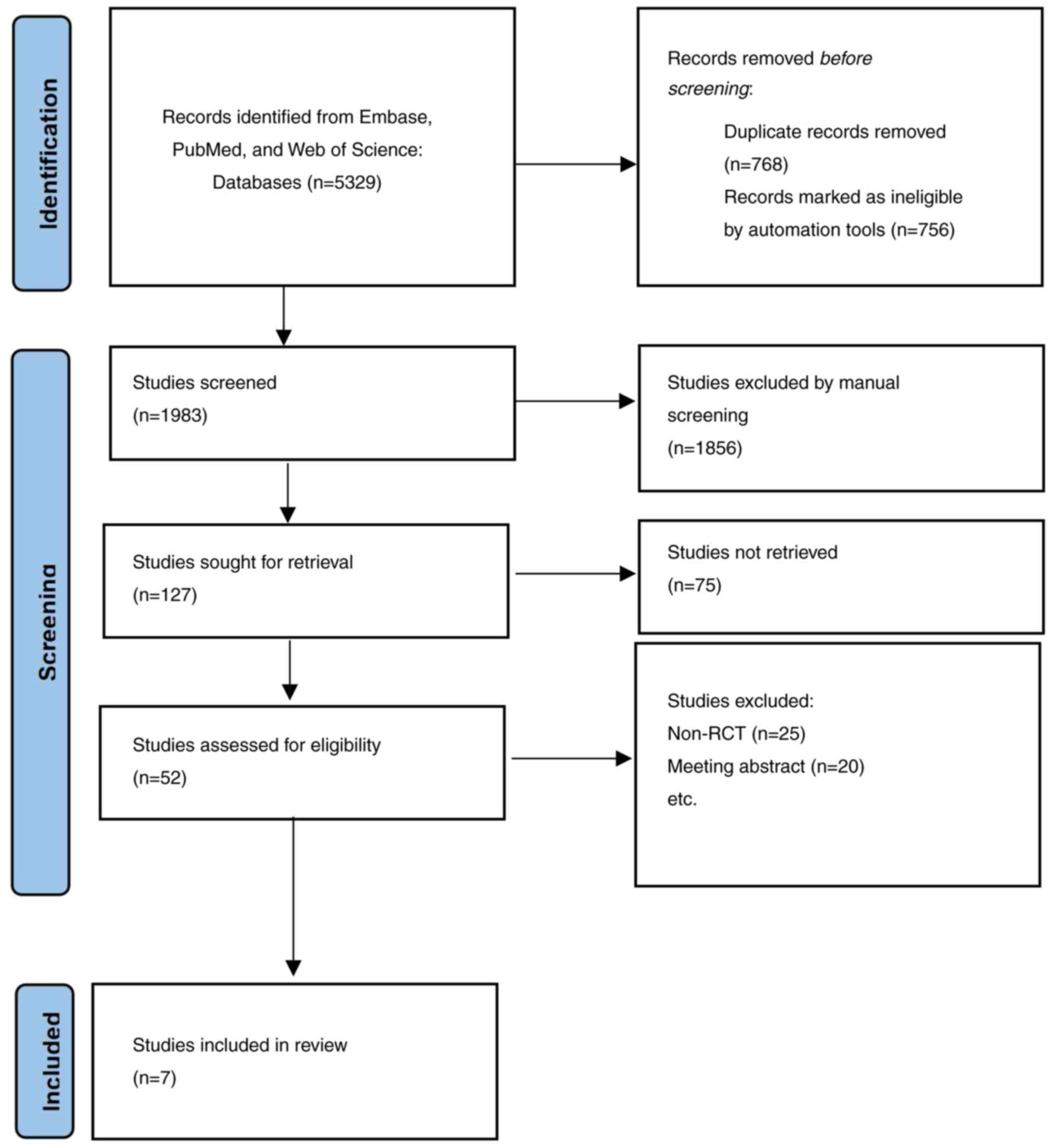
A total of 5,329 articles were retrieved for this
study. EndNote X9 was used to eliminate 3,256 duplicates. A further
1,931 articles were excluded by reading the titles and abstracts.
After reading 52 accessible articles in full, 20 articles related
to trial registration and 25 retrospective studies were excluded.
Eventually, a total of 7 studies (21–27)
involving 1,073 patients were included, as presented in Fig. 1.
Risk of bias assessment
Based on the Cochrane risk of bias tool, the
methodological quality of the included studies was fair, as
demonstrated in Table SI and
Fig. S1. All 7 studies had
adequate outcome measurement, enrolled a representative sample of
patients and had a reasonable length of follow-up.
Characteristics of included
studies
Table I presents
the characteristics of the included studies. The 7 studies included
a total of 1,073 patients (sorafenib alone, n=517; sorafenib plus
HAIC, n=359; sorafenib plus TACE, n=197), of whom 925 were male and
148 were female. The most common etiology of HCC was hepatitis B
virus infection [sorafenib plus HAIC, 49.86% (179/359); sorafenib
alone, 57.25% (296/517); sorafenib plus TACE, 77.66% (153/197)],
followed by hepatitis C virus infection [sorafenib plus HAIC,
26.18% (94/359); sorafenib alone, 22.24% (115/517), sorafenib plus
TACE, 5.0% (10/197)]. Furthermore, 26.74% (96/359) patients treated
with sorafenib plus HAIC, 18.96% (98/517) patients treated with
sorafenib alone and 39.59% (78/197) treated with sorafenib plus
TACE group had extrahepatic metastases. Only the studies by He
et al (22), Zheng et
al (21) and Lee et al
(27) observed a statistically
significant difference in OS between the two groups being compared
in the respective study (HR=0.35, 95% CI: 0.26-0.48; HR=0.28, 95%
CI: 0.15-0.53; and HR=0.59, 95% CI: 0.84-0.48, respectively). Since
Lee et al (27) did not
report the HR values with a 95% CI, the aforementioned data were
extracted from the Kaplan-Meier curve provided in the article. All
7 studies enrolled HCC patients with PVTT, and all included
patients were unsuitable for curative resection or local
ablation.
 | Table I.Characteristics of included
studies. |
Table I.
Characteristics of included
studies.
| Author, year | Country | ECOG | Group | Interventional
therapy details | mOS, months | N | Sex (M/F) | Age, years | Tumor size, cm | No. of tumors
(single/multiple) | PVTT | Child-Pugh | BCLC | Data time
frame | (Refs.) |
|---|
| Ikeda, 2016 | Japan | 0-1 | SorCDDP | Cisplatin (65
mg/m2)/4–6 weeks | 10.6 | 65 | 56/9 | 49 (41–55) | 10.1
(7.7-13.2) | 30/95 | 40/25 | 5-6 | NA | June 2011-December
2013 | (25) |
|
|
|
| Sorafenib
alone | 400 mg twice
daily | 8.7 | 41 | 32/9 | 49 (40–56) | 10.1
(8.3-12.1) | 33/89 | 17/24 |
|
|
|
|
| Kudo, 2018 | Japan | 0-1 | Sorafenib +
PF-HAIC | Cisplatin (20
mg/m2) on days 1 and 8 + 5-FU (330 mg/m2) on days 1–5 and 8–12/28
days | 11.8 | 102 | 89/13 | 69 (62–75) | NA | NA | 58/44 | 5-7 | 0/32/70 | November 2010-June
2014 | (24) |
|
|
|
| Sorafenib
alone | 400 mg twice
daily | 11.5 | 103 | 88/15 | 68 (62–75) |
|
| 64/39 |
| 0/27/76 |
|
|
| Kondo, 2019 | Japan | 0-1 | SorCDDP | Cisplatin (65
mg/m2)/4–6 weeks | 15.2 | 35 | 28/7 | 72 (65–79) | NA | NA | 21/14 | 5-7 | 2/14/19 | August
2011-November 2014 | (23) |
|
|
|
| Sorafenib
alone | 400 mg sorafenib
twice daily | 10.0 | 33 | 27/6 | 70.9 (61.8-80) |
|
| 22/11 |
| 2/13/18 |
|
|
| He, 2019 | China | 0-2 | Sorafenib +
FOLFOX-HAIC | Oxaliplatin (85
mg/m2) + leucovorin (400 mg/m2) + 5-FU (400 mg/m2); 5-FU infusion
2,400 mg/m2 for 46 h/3 weeks | 13.4 | 125 | 111/14 | 49 (41–55) | 10.1
(7.7-13.2) | 30/95 | 125/0 | 5-6 | NA | April 2016-October
2017 | (22) |
|
|
|
| Sorafenib
alone | 400 mg twice
daily | 7.1 | 122 | 112/10 | 49 (40–56) | 10.1
(8.3-12.1) | 33/89 | 122/0 |
|
|
|
|
| Zheng, 2022 | China | 0-2 | Sorafenib +
HAIC | Oxaliplatin (35
mg/m2) + 5-FU (600 mg/m2) + leucovorin (200 mg/m2 injected
intravenously)/ 28 days | 16.3 | 32 | 30/2 | 56 (45–67) | 10.6
(6.6-14.6) | 15/17 | 32/0 | 5-7 | NA | June 2017-November
2019 | (21) |
|
|
|
| Sorafenib | 400 mg twice
daily | 6.5 | 32 | 31/1 | 55 (45–65) | 10.7
(6.8-14.6) | 12/20 | 32/0 |
|
|
|
|
| Lee, 2020 | China | 0-2 | Sorafenib +
TACE | Lipiodol + 10–20 mg
Adriamycin/elution beads + Adriamycin/2–3 months | 11.0 | 27 | 23/4 | 60 (53-65.5) | 6.2 (3.5-13.5) | NA | 11/16 | 5-7 | NA | NA | (27) |
|
|
|
| Sorafenib | 200–400 mg twice
daily | 5.0 | 17 | 15/2 | 59 (51–62) | 6.5 (3.4-12.5) |
| 5/12 |
|
|
|
|
| Park, 2018 | South Korea | 0-2 | Sorafenib +
TACE | Doxorubicin or
cisplatin + embolization materials/28 days | 12.8 | 170 | 136/34 | 60.2
(50.6-69.8) | NA | NA | 68/102 | 5-7 | 3/39/128 | January
2013-December 2015 | (26) |
|
|
|
| Sorafenib | 200–400 mg twice
daily | 10.8 | 169 | 147/22 | 61.3
(51.7-70.9) |
|
| 63/106 |
| 0/4/125 |
|
|
Network meta-analysis
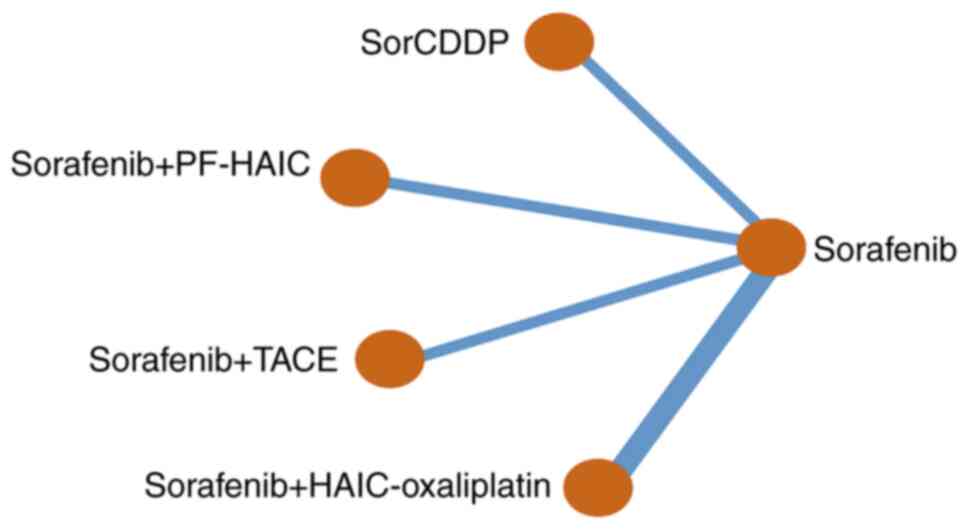
The 7 RCTs identified through the literature reviews
enabled the creation of a seven-node network with two edges, which
included sorafenib alone, sorafenib with cisplatin-HAIC (CDDP)
(SorCDDP), sorafenib with HAIC-oxaliplatin, sorafenib with TACE,
and sorafenib with PF-HAIC. Fig. 2
shows the network meta-analysis (NMA) map of the interventional
therapies in the studies that were directly compared for efficacy
in prolonging survival. According to deviance information criterion
(DIC) and total residual deviance statistics, the I2
value was much higher than 50%, and the random-effects model had a
superior fit to the data than the fixed-effects model, with the
former model having fewer parameters and a lower DIC (28). It was not possible to assess
inconsistency within the network due to the absence of any closed
loops. The proportional hazards assumption was not violated in the
studies with time-to-event data. The Kaplan-Meier curves in all 7
RCTs crossed over; however, violation of the proportional hazards
assumption was not supported by the statistical data.
Efficacy
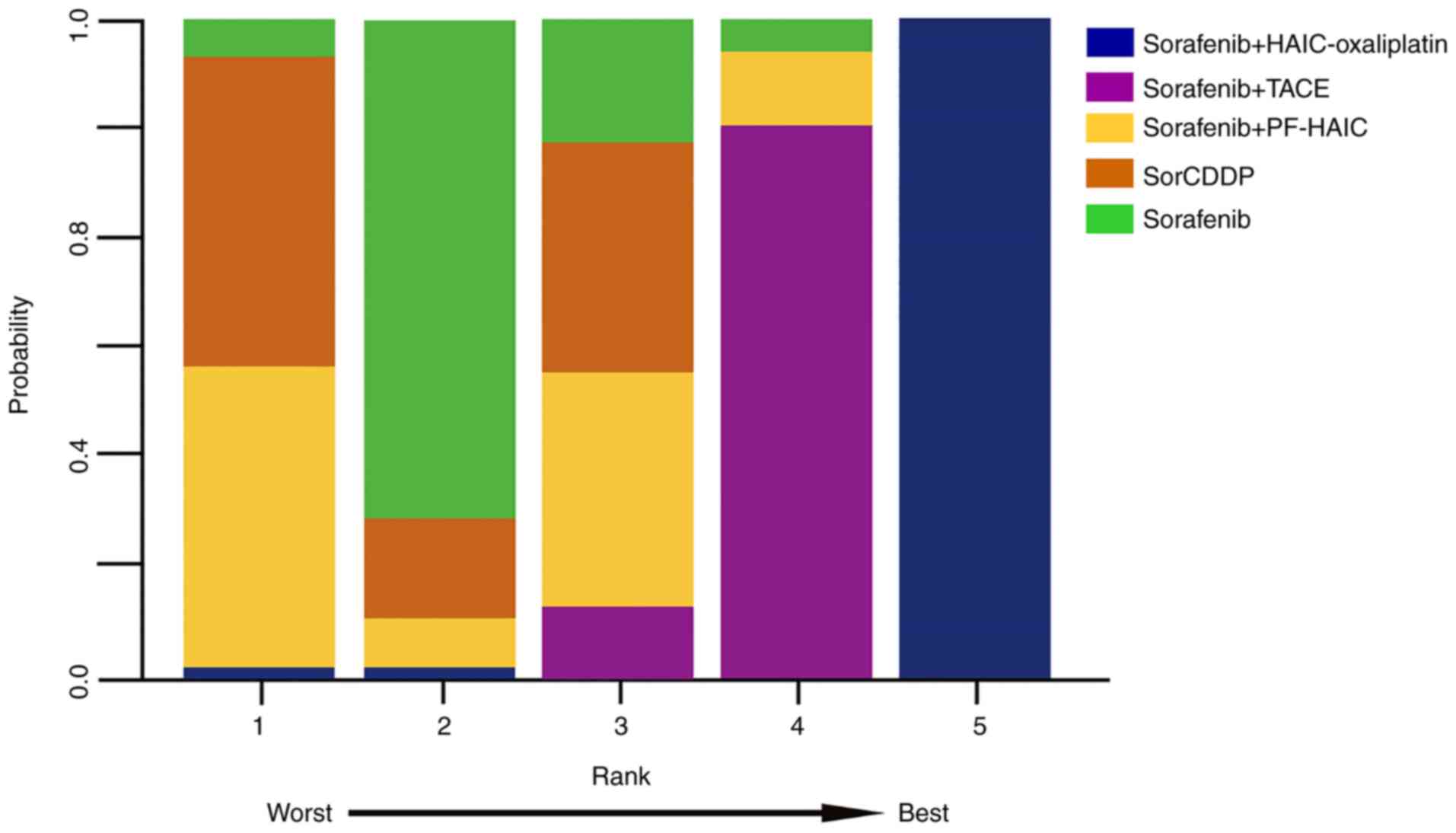
The NMA revealed a significant difference between
the sorafenib plus HAIC-oxaliplatin regimen and other treatment
strategies in terms of OS (HR=0.33, 95% CI: 0.25-0.44). By
contrast, comparisons between sorafenib plus PF-HAIC, SorCDDP and
sorafenib plus TACE identified little difference with mortality HRs
of 1.01 (95% CI: 0.74-1.38), 1.22 (95% CI: 0.88-1.71) and 0.79 (95%
CI: 0.62-1.01), respectively. Fig.
3 depicts the ranking of the treatments with regard to the
likelihood of being the superior treatment. Rank probability plots
revealed that there would be a 99.9% likelihood of sorafenib plus
FOLFOX-HAIC being the most effective treatment, followed by
sorafenib plus TACE at 86.6% and SorCDDP at 75.6%. Furthermore, a
comparison based on mRECIST criteria found that patients treated
with sorafenib plus FOLFOX-HAIC had significantly higher ORR than
those receiving other treatment regimens (OR=22.0, 95% CI:
10.6-25.7).
SAEs
The analysis of SAEs revealed that the risk of liver
injury was higher in the sorafenib plus TACE group compared with
other groups (HR=5.93, 95% CI: 2.70-15.41); there was no
significant difference in the risk of liver injury between patients
receiving sorafenib plus HAIC compared with those receiving
sorafenib alone. Furthermore, no significant differences in the
constitutional symptoms and gastrointestinal reactions were
detected between all the treatment groups. Table II summarizes the results of the
network meta-analyses regarding OS, ORR and SAEs.
 | Table II.Comparisons of efficacy in terms of
OS and severe adverse events in advanced hepatocellular
carcinoma. |
Table II.
Comparisons of efficacy in terms of
OS and severe adverse events in advanced hepatocellular
carcinoma.
| A, OS [HR (95%
CI)] |
|---|
|
|---|
| Author, year | Treatment
group | Sorafenib +
HAIC-oxaliplatin | Sorafenib +
TACE | Sorafenib +
PF-HAIC | SorCDDP | (Refs.) |
|---|
| Zheng, 2022; He,
2019 | Sorafenib +
HAIC-oxaliplatin | - | - | - | - | (21,22) |
| Park, 2018; Lee,
2020 | Sorafenib +
TACE | 0.42
(0.29-0.62) | - | - | - | (26,27) |
| Kudo, 2018 | Sorafenib +
PF-HAIC | 0.33
(0.22-0.50) | 0.78
(0.52-1.17) | - | - | (24) |
| Kondo, 2018; Ikeda,
2016 | SorCDDP | 0.27
(0.18-0.42) | 0.64
(0.42-0.97) | 0.83
(0.52-1.30) | - | (23,25) |
| All of the
above | Sorafenib
(Control) | 0.33
(0.25-0.44) | 0.79
(0.62-1.01) | 1.01
(0.74-1.38) | 1.22
(0.88-1.71) | (21–27) |
|
| B, Overall
response rate [OR (95% CI)] |
|
| Author,
year | Treatment
group | Sorafenib +
HAIC-oxaliplatin | Sorafenib +
TACE | Sorafenib +
PF-HAIC | SorCDDP | (Refs.) |
|
| Zheng, 2022; He,
2019 | Sorafenib +
HAIC-oxaliplatin | - | - | - | - | (21,22) |
| Park, 2018; Lee,
2020 | Sorafenib +
TACE | 9.26
(3.03-29.26) | - | - | - | (26,27) |
| Kudo, 2018 | Sorafenib +
PF-HAIC | 8.16
(3.01-23.79) | 0.88
(0.32-2.54) | - | - | (24) |
| Kondo, 2018; Ikeda,
2016 | SorCDDP | 7.73
(2.05-27.81) | 0.83
(0.22-2.96) | 0.95
(0.27-3.03) | - | (23,25) |
| All of the
above | Sorafenib
(Control) | 22.18
(10.69-52.56) | 2.4
(1.10-5.58) | 2.72
(1.43-5.36) | 2.88
(1.12-8.58) | (21–27) |
|
| C, Liver injury
[OR (95% CI)] |
|
| Author,
year | Treatment
group | Sorafenib +
HAIC-oxaliplatin | Sorafenib +
TACE | Sorafenib +
PF-HAIC | SorCDDP | (Refs.) |
|
| Zheng, 2022; He,
2019 | Sorafenib +
HAIC-oxaliplatin | - | - | - | - | (21,22) |
| Park, 2018; Lee,
2020 | Sorafenib +
TACE | 0.22
(0.07-0.68) | - | - | - | (26,27) |
| Kudo, 2018 | Sorafenib +
PF-HAIC | 1.34
(0.49-3.81) | 5.98
(2.07-19.30) | - | - | (24) |
| Kondo, 2018; Ikeda,
2016 | SorCDDP | 1.35
(0.51-3.62) | 6.02
(2.17,18.53) | 1.01
(0.39-2.55) | - | (23,25) |
| All of the
above | Sorafenib
(Control) | 1.34
(0.64-2.90) | 5.93
(2.70-15.41) | 1.00
(0.49-2.00) | 0.99
(0.54-1.86) | (21–27) |
|
| D,
Constitutional symptoms [OR (95% CI)] |
|
| Author,
year | Treatment
group | Sorafenib +
HAIC-oxaliplatin | Sorafenib +
TACE | Sorafenib +
PF-HAIC | SorCDDP | (Refs.) |
|
| Zheng, 2022; He,
2019 | Sorafenib +
HAIC-oxaliplatin | - | - | - | - | (21,22) |
| Park, 2018; Lee,
2020 | Sorafenib +
TACE | 1.47
(0.35-6.59) | - | - | - | (26,27) |
| Kudo, 2018 | Sorafenib +
PF-HAIC | 1.39
(0.33-6.23) | 0.94
(0.25-3.65) | - | - | (24) |
| Kondo, 2018; Ikeda,
2016 | SorCDDP | 0.53
(0.06-3.41) | 0.36
(0.04-2.07) | 0.38
(0.04-2.15) | - | (23,25) |
| All of the
above | Sorafenib
(Control) | 1.81
(0.63-5.92) | 1.24
(0.48-3.28) | 1.31
(0.52-3.40) | 3.36
(0.83-25.50) | (21–27) |
|
| E,
Gastrointestinal reactions [OR (95% CI)] |
|
| Author,
year | Treatment
group | Sorafenib +
HAIC-oxaliplatin | Sorafenib +
TACE | Sorafenib +
PF-HAIC | SorCDDP | (Refs.) |
|
| Zheng, 2022; He,
2019 | Sorafenib +
HAIC-oxaliplatin | - | - | - | - | (21,22) |
| Park, 2018; Lee,
2020 | Sorafenib +
TACE | 0.72
(0.22-2.35) | - | - | - | (26,27) |
| Kudo, 2018 | Sorafenib +
PF-HAIC | 2.05
(0.59-8.51) | 2.86
(0.63,14.83) | - | - | (24) |
| Kondo, 2018; Ikeda,
2016 | SorCDDP | 0.57
(0.07-3.35) | 0.78
(0.08-5.63) | 0.27
(0.03-2.05) | - | (23,25) |
| All of the
above | Sorafenib
(Control) | 0.9
(0.49-1.63) | 1.24
(0.45-3.53) | 0.44
(0.12-1.30) | 1.57
(0.30-12.06) | (21–27) |
Discussion
Due to the lack of clinical RCTs in which different
treatments of HCC are directly compared, the present meta-analysis
used 7 RCT studies to indirectly evaluate the efficacy and safety
of CDDP, PF-HAIC, HAIC-oxaliplatin and TACE as interventional
modalities when combined with sorafenib.
The study findings revealed that combining CDDP,
PF-HAIC and TACE with sorafenib did not significantly differ from
sorafenib alone in terms of OS, indicating that inappropriate
treatment modalities and regimens are not beneficial to HCC patient
survival. However, the prognosis of patients receiving
HAIC-oxaliplatin plus sorafenib was found to be significantly
improved when compared with other treatment modalities. The
survival benefit may be explained in part by the superior efficacy
of oxaliplatin in HCC treatment. Compared with cisplatin,
oxaliplatin has significantly improved pharmacokinetic,
biochemical, cytotoxic and immunological properties (29). Oxaliplatin is an inhibitor of
ribosomal RNA synthesis, which induces ribosome biogenesis stress
during the active translation of RNA interference. Thus,
oxaliplatin exerts its cytotoxic effects by inhibiting protein
synthesis rather than via a DNA damage response (30). In addition, oxaliplatin induces
antitumor immune responses to anthracyclines via the stimulation of
pro-apoptotic cell calreticulin exposure, leading to immunogenic
tumor cell death (31). Notably,
sorafenib normalizes HCC vasculature and increases drug transport
by interacting with platinum transporter proteins to increase the
local enrichment of the oxaliplatin concentration in tumors
(32). As a result, a multidrug
combination based on oxaliplatin may be superior to cisplatin
alone. The present findings indirectly support a previous study
suggesting that HAIC-oxaliplatin plus sorafenib has greater
efficacy than TACE for large HCC (≥7 cm) (14). It is hypothesized that this may be
because the prolonged and continuous infusion of chemotherapeutic
agents through the target artery increases the local drug
concentration and tumor uptake compared with systemic intravenous
chemotherapy (33). In addition,
there may be a synergistic antitumor effect between sorafenib,
oxaliplatin and 5-FU. Sorafenib has several targets, including
Raf-1, vascular endothelial growth factor (VEGF) receptor 1–3 and
platelet-derived growth factor receptor-β; the inhibition of Raf-1
can induce apoptosis and counteract the resistance of tumor cells
to FOLFOX (34,35). It has been shown that 5-FU, in
particular, increases tumor sensitivity to oxaliplatin by
increasing multidrug resistance-associated protein 2 mRNA
expression, and its synergistic efficacy with oxaliplatin mediates
the expression of drug transporter proteins (22). TACE plus sorafenib is more
effective than traditional HAIC, which is likely due to the tumor
microenvironment created by TACE treatment-induced ischemia and
hypoxia, which causes the upregulation of local inflammatory
factors, including insulin-like growth factor-2 and VEGF (36). Moreover, sorafenib inhibits
tyrosine kinases of the VEGF signaling pathway, inhibiting tumor
angiogenesis and weakening the proliferation ability of tumor cells
(37). The combination of
sorafenib with TACE can improve patient survival, since sorafenib
promotes the deposition of the drug-eluting TACE component lipiodol
in HCC vessels, where it exhibits a tumor necrotizing effect
(38). TACE induces ischemia and
hypoxia in tumor tissues by the targeted embolization of arteries
during treatment; however, this effect requires hepatic vein
patency to ensure normal tissue metabolism, and since ischemic and
hypoxic conditions may favor the resistance of tumor cells to
therapeutic agents (39),
promoting angiogenesis and the migration of certain cytokines, for
example IL-8, this may lead to tumor metastasis (40). HAIC, by contrast, is continuously
administered throughout the treatment process, and tumor cells are
killed via a cytotoxic response, without any dependence of normal
tissue metabolism on the hepatic vein and the resistance and
metastasis induced by inflammatory factors. Therefore, HAIC may be
a more effective and safer intervention for HCC than TACE.
Nevertheless, more studies are required to clarify and demonstrate
whether this efficacy is due to interventional modalities or the
regimen used. Based on the current findings, we hypothesize that
HAIC-oxaliplatin currently is a superior interventional combination
therapy for HCC. However, whether this efficacy advantage is due to
the type of treatment or the drug combination remains unclear and
requires validation in high-quality head-to-head studies.
A comparison of the various SAEs in the present
meta-analysis revealed that patients treated with TACE plus
sorafenib had an elevated risk of liver injury. This could be
because TACE and its associated metabolites stimulate the
expression of pro-apoptotic genes and the activation of multiple
death signaling pathways, thereby promoting apoptosis and inducing
an inflammatory response that accelerates the progression of
drug-induced liver injury. Moreover, embolic agents are able to
enter small arteries and capillaries in non-cancerous areas,
causing ischemia and hypoxia in normal tissues and exacerbating
oxidative stress and liver injury (41). Furthermore, patients with HCC who
have intrahepatic metastases typically have a history of hepatitis
and cirrhosis, and their liver function is already compromised
(42). According to previous
research, liver injury frequently occurs in colorectal
cancer-related chemotherapy using the FOLFOX regimen, most likely
due to the toxicity of oxaliplatin metabolites, which affects the
permeability of the hepatic sinusoidal cells and raises the
pressure in the hepatic venous sinusoids, resulting in liver injury
and sinusoidal portal hypertension (43,44).
However, the present study indicates that HAIC-oxaliplatin plus
sorafenib is significantly safer than TACE when combined with
sorafenib. Regarding constitutional symptoms and gastrointestinal
events, we hypothesize that patients with HCC who are treated with
HAIC-oxaliplatin are at a higher risk of SAEs because they have a
heavier tumor burden. Notably, the incidence of overall SAEs
suggests that HAIC-oxaliplatin may be more appropriate than TACE
and other HAIC therapies in the combination treatment of patients
with a heavier tumor burden.
The combination of interventional therapy and oral
drugs has markedly improved the survival of patients with advanced
HCC. The REFLECT trial established the first-line status of
lenvatinib (45), and Ding et
al (46) demonstrated its
superior efficacy compared with sorafenib in HCC combination
therapy. Regorafenib and cabozantinib, which are the second-line
drugs for advanced HCC, were also approved following the RESORCE
and CELESTIAL trials (47,48), With the development of drug-eluting
beads and the advancement of super-selective TACE (2,49),
further studies are recommended to investigate the efficacy of
these new oral drugs in combination with interventional modalities
for advanced HCC.
There are several limitations to the present study.
Firstly, only 7 RCTs met the inclusion criteria of the
meta-analysis, and the potential bias of the studies could impact
the results. Furthermore, because the pathogenesis and prevalence
of hepatitis vary greatly across different regions and populations,
the fact that the population in this study comprises only Asian
patients may limit the generalizability of the study findings.
In conclusion, the present study indicates that in
patients with advanced primary HCC, HAIC-oxaliplatin significantly
improves patient survival when combined with sorafenib compared
with other regimens or interventional modalities. Although there
may be significant bias in assessing outcome indicators due to
patient enrollment differences, the results suggest that the
HAIC-oxaliplatin plus sorafenib combination should be more widely
used. However, the study of HAIC dosing regimens for advanced HCC
and exploration of combination treatment options in the future
studies is recommended.
Supplementary Material
Supporting Data
Supporting Data
Acknowledgements
Not applicable.
Funding
This work is supported by the Gansu Traditional Chinese Medicine
Research Project (grant no. GZKP-2020-28) and the Lanzhou City
Chengguan District Science and Technology Plan Project (grant no.
2020-2-11-4).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
XLC and HCY conceived and designed the research.
XLC, HCY and QGF performed data acquisition, data analysis and
manuscript preparation. QY, WKJ, SZR and WCZ assisted with data
acquisition, data analysis and statistical analysis. WCZ and SZR
confirm the authenticity of all the raw data. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
ORR
|
overall response rate
|
|
5-FU
|
5-fluorouracil
|
|
FOLFOX, 5-FU
|
leucovorin and oxaliplatin
|
|
HAIC
|
hepatic artery infusion
chemotherapy
|
|
TACE
|
transcatheter arterial
chemoembolization
|
|
HCC
|
hepatocellular carcinoma
|
|
PF
|
cisplatin and 5-FU
|
|
RCT
|
randomized controlled trial
|
|
CDDP
|
cisplatin-HAIC
|
|
SorCDDP
|
sorafenib with CDDP
|
|
PVTT
|
portal vein tumor thrombosis
|
|
DIC
|
deviance information criterion
|
|
AEs
|
adverse events
|
|
SAEs
|
serious AEs
|
|
VEGF
|
vascular endothelial growth factor
|
References
|
1
|
Siegel RL, Miller KD, Fuchs HE and Jemal
A: Cancer statistics, 2022. CA Cancer J Clin. 72:7–33. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Xu S, Bie ZX, Li YM, Li B, Kong FL, Peng
JZ and Li XG: Drug-eluting bead bronchial arterial
chemoembolization with and without microwave ablation for the
treatment of advanced and standard treatment-refractory/ineligible
non-small cell lung cancer: A comparative study. Front Oncol.
12:8518302022. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wong KM, King GG and Harris WP: The
treatment landscape of advanced hepatocellular carcinoma. Curr
Oncol Rep. 24:917–927. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ni JY, Liu SS, Sun HL, Wang WD, Zhong ZL,
Hou SN, Chen YT and Xu LF: Transcatheter hepatic arterial infusion
chemotherapy vs sorafenib in the treatment of patients with
hepatocellular carcinoma of Barcelona Clinic Liver Cancer stage C:
A meta-analysis of Asian population. Onco Targets Ther.
11:7883–7894. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Moriguchi M, Aramaki T, Nishiofuku H, Sato
R, Asakura K, Yamaguchi K, Tanaka T, Endo M and Itoh Y: Sorafenib
versus hepatic arterial infusion chemotherapy as initial treatment
for hepatocellular carcinoma with advanced portal vein tumor
thrombosis. Liver Cancer. 6:275–286. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Benson AB, D'Angelica MI, Abbott DE, Anaya
DA, Anders R, Are C, Bachini M, Borad M, Brown D, Burgoyne A, et
al: Hepatobiliary cancers, version 2.2021, NCCN clinical practice
guidelines in oncology. J Natl Compr Canc Netw. 19:541–565. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lyu N, Wang X, Li JB, Lai JF, Chen QF, Li
SL, Deng HJ, He M, Mu LW and Zhao M: Arterial chemotherapy of
oxaliplatin plus fluorouracil versus sorafenib in advanced
hepatocellular carcinoma: A biomolecular exploratory, randomized,
phase III trial (FOHAIC-1). J Clin Oncol. 40:468–480. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kudo M, Matsui O, Izumi N, Iijima H,
Kadoya M, Imai Y, Okusaka T, Miyayama S, Tsuchiya K, Ueshima K, et
al: JSH consensus-based clinical practice guidelines for the
management of hepatocellular carcinoma: 2014 update by the liver
cancer study Group of Japan. Liver Cancer. 3:458–468. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cai Z, He C, Zhao C and Lin X: Survival
comparisons of hepatic arterial infusion chemotherapy with mFOLFOX
and transarterial chemoembolization in patients with unresectable
intrahepatic cholangiocarcinoma. Front Oncol. 11:6111182021.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tsai WL, Lai KH, Liang HL, Hsu PI, Chan
HH, Chen WC, Yu HC, Tsay FW, Wang HM, Tsai HC and Cheng JS: Hepatic
arterial infusion chemotherapy for patients with huge unresectable
hepatocellular carcinoma. PLoS One. 9:e927842014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Song DS, Song MJ, Bae SH, Chung WJ, Jang
JY, Kim YS, Lee SH, Park JY, Yim HJ, Cho SB, et al: A comparative
study between sorafenib and hepatic arterial infusion chemotherapy
for advanced hepatocellular carcinoma with portal vein tumor
thrombosis. J Gastroenterol. 50:445–454. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Regmi P, Hu HJ, Lv TR, Paudyal A, Sah RB,
Ma WJ, Jin YW and Li FY: Efficacy and safety of sorafenib plus
hepatic arterial infusion chemotherapy for advanced hepatocellular
carcinoma. Surg Oncol. 39:1016632021. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li D, Pang Y, Xu L and Xu X: Efficacy and
safety of sorafenib combined with TACE in the treatment of advanced
hepatocellular carcinoma: A meta-analysis. J BUON. 26:1355–1364.
2021.PubMed/NCBI
|
|
14
|
Li QJ, He MK, Chen HW, Fang WQ, Zhou YM,
Xu L, Wei W, Zhang YJ, Guo Y, Guo RP, et al: Hepatic arterial
infusion of oxaliplatin, fluorouracil, and leucovorin versus
transarterial chemoembolization for large hepatocellular carcinoma:
A randomized phase III trial. J Clin Oncol. 40:150–160. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cai YS and Wu H: Is FOLFOX-HAIC superior
to transarterial chemoembolization in treating large hepatocellular
carcinoma? Hepatobiliary Surg Nutr. 11:164–165. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Mei J, Yu H, Qin L and Jia Z: FOLFOX-HAIC
for unresectable large hepatocellular carcinoma: The effectiveness
has yet to be determined. J Clin Oncol. 40:18412022. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Panagopoulos A, Solou K, Tatani I,
Triantafyllopoulos IK, Lakoumentas J, Kouzelis A, Athanasiou V and
Kokkalis ZT: What is the optimal surgical treatment for Neer type
IIB (IIC) distal clavicle fractures? A systematic review and
meta-analysis. J Orthop Surg Res. 17:2152022. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Parmar MK, Torri V and Stewart L:
Extracting summary statistics to perform meta-analyses of the
published literature for survival endpoints. Stat Med.
17:2815–2834. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wang Y and Zeng T: Response to: Practical
methods for incorporating summary time-to-event data into
meta-analysis. Trials. 14:3912013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Cumpston M, Li T, Page MJ, Chandler J,
Welch VA, Higgins JP and Thomas J: Updated guidance for trusted
systematic reviews: A new edition of the Cochrane handbook for
systematic reviews of interventions. Cochrane Database Syst Rev.
10:ED0001422019.PubMed/NCBI
|
|
21
|
Zheng K, Zhu X, Fu S, Cao G, Li QW, Xu L,
Chen H, Wu D, Yang R, Wang K, et al: Sorafenib plus hepatic
arterial infusion chemotherapy versus sorafenib for hepatocellular
carcinoma with major portal vein tumor thrombosis: A randomized
trial. Radiology. 303:455–464. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
He M, Li Q, Zou R, Shen J, Fang W, Tan G,
Zhou Y, Wu X, Xu L, Wei W, et al: Sorafenib plus hepatic arterial
infusion of oxaliplatin, fluorouracil, and leucovorin vs sorafenib
alone for hepatocellular carcinoma with portal vein invasion: A
randomized clinical trial. JAMA Oncol. 5:953–960. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kondo M, Morimoto M, Kobayashi S, Ohkawa
S, Hidaka H, Nakazawa T, Aikata H, Hatanaka T, Takizawa D,
Matsunaga K, et al: Randomized, phase II trial of sequential
hepatic arterial infusion chemotherapy and sorafenib versus
sorafenib alone as initial therapy for advanced hepatocellular
carcinoma: SCOOP-2 trial. BMC Cancer. 19:9542019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kudo M, Ueshima K, Yokosuka O, Ogasawara
S, Obi S, Izumi N, Aikata H, Nagano H, Hatano E, Sasaki Y, et al:
Sorafenib plus low-dose cisplatin and fluorouracil hepatic arterial
infusion chemotherapy versus sorafenib alone in patients with
advanced hepatocellular carcinoma (SILIUS): A randomised, open
label, phase 3 trial. Lancet Gastroenterol Hepatol. 3:424–432.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ikeda M, Shimizu S, Sato T, Morimoto M,
Kojima Y, Inaba Y, Hagihara A, Kudo M, Nakamori S, Kaneko S, et al:
Sorafenib plus hepatic arterial infusion chemotherapy with
cisplatin versus sorafenib for advanced hepatocellular carcinoma:
Randomized phase II trial. Ann Oncol. 27:2090–2096. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Park JW, Kim YJ, Kim DY, Bae SH, Paik SW,
Lee YJ, Kim HY, Lee HC, Han SY, Cheong JY, et al: Sorafenib with or
without concurrent transarterial chemoembolization in patients with
advanced hepatocellular carcinoma: The phase III STAH trial. J
Hepatol. 70:684–691. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Lee WC, Hung HC, Lee JC, Wang YC, Cheng
CH, Wu TH, Lee CF, Wu TJ, Chou HS and Chan KM: Treatment strategy
of adding transcatheter arterial chemoembolization to sorafenib for
advanced stage hepatocellular carcinoma. Cancer Rep (Hoboken).
4:e12942021.PubMed/NCBI
|
|
28
|
Barili F, Parolari A, Kappetein PA and
Freemantle N: Statistical primer: Heterogeneity, random- or
fixed-effects model analyses? Interact Cardiovasc Thorac Surg.
27:317–321. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Theile D, Grebhardt S, Haefeli WE and
Weiss J: Involvement of drug transporters in the synergistic action
of FOLFOX combination chemotherapy. Biochem Pharmacol.
78:1366–1373. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Bruno PM, Liu Y, Park GY, Murai J, Koch
CE, Eisen TJ, Pritchard JR, Pommier Y, Lippard SJ and Hemann MT: A
subset of platinum-containing chemotherapeutic agents kills cells
by inducing ribosome biogenesis stress. Nat Med. 23:461–471. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Tesniere A, Schlemmer F, Boige V, Kepp O,
Martins I, Ghiringhelli F, Aymeric L, Michaud M, Apetoh L, Barault
L, et al: Immunogenic death of colon cancer cells treated with
oxaliplatin. Oncogene. 29:482–491. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
He MK, Le Y, Li QJ, Yu ZS, Li SH, Wei W,
Guo RP and Shi M: Hepatic artery infusion chemotherapy using
mFOLFOX versus transarterial chemoembolization for massive
unresectable hepatocellular carcinoma: A prospective non-randomized
study. Chin J Cancer. 36:832017. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Lewandowski RJ, Geschwind JF, Liapi E and
Salem R: Transcatheter intraarterial therapies: Rationale and
overview. Radiology. 259:641–657. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ma SQ, Cao BR, Zhang H, Luo LP, Ren Y, Hu
T and Chen CM: The lack of Raf-1 kinase feedback regulation
enhances antiapoptosis in cancer cells. Oncogene. 36:2014–2022.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Mizukoshi E, Yamashita T, Arai K,
Terashima T, Kitahara M, Nakagawa H, Iida N, Fushimi K and Kaneko
S: Myeloid-derived suppressor cells correlate with patient outcomes
in hepatic arterial infusion chemotherapy for hepatocellular
carcinoma. Cancer Immunol Immunother. 65:715–725. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Pratama MY, Pascut D, Massi MN and
Tiribelli C: The role of microRNA in the resistance to treatment of
hepatocellular carcinoma. Ann Transl Med. 7:5772019. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Chao Y, Chung YH, Han G, Yoon JH, Yang J,
Wang J, Shao GL, Kim BI and Lee TY: The combination of
transcatheter arterial chemoembolization and sorafenib is well
tolerated and effective in Asian patients with hepatocellular
carcinoma: Final results of the START trial. Int J Cancer.
136:1458–1467. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Zheng L, Guo CY, Chen CS, Xiao JC, Hu HT,
Cheng HT, Zong DW, Jiang L and Li HL: Sorafenib improves lipiodol
deposition in transarterial chemoembolization of Chinese patients
with hepatocellular carcinoma: A long-term, retrospective study.
Oncotarget. 8:97613–97622. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
He X, Guo X, Zhang H, Kong X, Yang F and
Zheng C: Mechanism of action and efficacy of LY2109761, a TGF-β
receptor inhibitor, targeting tumor microenvironment in liver
cancer after TACE. Oncotarget. 9:1130–1142. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Lin W, Wang H, Zhong M, Yu S, Zhao S,
Liang S, Du J, Cheng B, Gu W and Ling C: Effect and molecular
mechanisms of jiedu recipe on hypoxia-induced angiogenesis after
transcatheter arterial chemoembolization in hepatocellular
carcinoma. Evid Based Complement Alternat Med.
2021:65293762021.PubMed/NCBI
|
|
41
|
Yang P, Zhou W, Li C, Zhang M, Jiang Y,
Jiang R, Ba H, Li C, Wang J, Yin B, et al: Kupffer-cell-expressed
transmembrane TNF-α is a major contributor to lipopolysaccharide
and D-galactosamine-induced liver injury. Cell Tissue Res.
363:371–383. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Chen LX, Zou SJ, Li D, Zhou JY, Cheng ZT,
Zhao J, Zhu YL, Kuang D and Zhu XH: Prostate-specific membrane
antigen expression in hepatocellular carcinoma, cholangiocarcinoma,
and liver cirrhosis. World J Gastroenterol. 26:7664–7678. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Bloom S, Kemp W and Lubel J: Portal
hypertension: Pathophysiology, diagnosis and management. Internal
Med J. 45:16–26. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Fuentes-Lacouture MC, Barrera-Garavito EC,
Gomez A and Mantilla W: Non-cirrhotic portal hypertension in a
patient with colonic carcinoma treated with oxaliplatin. J Med
Cases. 12:99–101. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Kudo M, Finn RS, Qin S, Han KH, Ikeda K,
Piscaglia F, Baron A, Park JW, Han G, Jassem J, et al: Lenvatinib
versus sorafenib in first-line treatment of patients with
unresectable hepatocellular carcinoma: A randomised phase 3
non-inferiority trial. Lancet. 391:1163–1173. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Ding X, Sun W, Li W, Shen Y, Guo X, Teng
Y, Liu X, Zheng L, Li W and Chen J: Transarterial chemoembolization
plus lenvatinib versus transarterial chemoembolization plus
sorafenib as first-line treatment for hepatocellular carcinoma with
portal vein tumor thrombus: A prospective randomized study. Cancer.
127:3782–3793. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Bruix J, Qin S, Merle P, Granito A, Huang
YH, Bodoky G, Pracht M, Yokosuka O, Rosmorduc O, Breder V, et al:
Regorafenib for patients with hepatocellular carcinoma who
progressed on sorafenib treatment (RESORCE): A randomised,
double-blind, placebo-controlled, phase 3 trial. Lancet. 389:56–66.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Abou-Alfa GK, Meyer T, Cheng AL,
El-Khoueiry AB, Rimassa L, Ryoo BY, Cicin I, Merle P, Chen Y, Park
JW, et al: Cabozantinib in patients with advanced and progressing
hepatocellular carcinoma. N Engl J Med. 379:54–63. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Miyayama S, Yamashiro M, Ikeda R,
Matsumoto J, Takeuchi K, Sakuragawa N, Ueda T, Sanada T, Notsumata
K and Terada T: Efficacy of superselective conventional
transarterial chemoembolization using guidance software for
hepatocellular carcinoma within three lesions smaller than 3 cm.
Cancers (Basel). 13:63702021. View Article : Google Scholar : PubMed/NCBI
|