Introduction
Epithelioid hemangioendothelioma (EH) is a vascular
endothelial cell neoplasm of low malignancy. In 1982, Weiss and
Enzinger (1) reported a group of
vascular tumors occurring in the surrounding soft tissues that they
termed EH. Since 2002, the World Health Organization (WHO) has
classified EH as a malignant tumor (2,3). EH
occurs in the superficial or deep soft tissues of the limbs, liver,
lungs and bones, among others, and rarely occurs in the orbit
and/or eyelid (4,5). EH can occur at any age, with cases
occurring in patients between 13 and 86 years old, with a median
age of ~50 years. EHE occurs slightly more often in women,
especially in the lungs and liver. The overall 5-year survival rate
for patients with the neoplasm is 73% (2). Since Tsuji et al (6) first reported EH of the eyelid (EHE)
in 2010, four cases have been reported in studies published in
English (6–9). Microscopically, the tumor consists of
proliferating epithelioid and fusiform vascular endothelial cells,
and the atypia of epithelioid and spindle cells is not obvious.
These cells form a mass of primitive blood vessels and the lumina
contain red blood cells. The local cytoplasm of the tumor cells is
obviously vacuolated, and immunohistochemistry shows positive
expression of CD31 and/or CD34. In one case, the tumor cells in the
eyelid were involved with the lacrimal glands (8). Current EHE treatment is based on
extensive tumor resection with a negative margin.
Case report
Patient
In January 2022, A 10-year-old girl was admitted to
the Department of Ophthalmology of the First People's Hospital of
Xiaoshan District (Hangzhou, China) due to a painless red mass in
the left eyelid that had been present for 6 months.
Physical examination
The left upper eyelid mass was ~1.0×0.6×0.3 cm in
size, with a red surface. The patient experienced tenderness and
normal vision. The blood routine, including liver function,
myocardial enzyme profile and coagulation time, was normal. A left
upper eyelid cyst was thus clinically diagnosed. After successful
local anesthesia, a horizontal incision of ~1 cm was made at the
mass site to separate the fascia and muscularum tissue from the
surface of the mass. A cystic mass ~1.0 cm in diameter was found.
Tobramycin and dexamethasone eye ointment and clonbitone eye drops
were given for symptomatic treatment (twice a day, 2 drops each
time for 3 days).
Macroexamination
There were two pieces of gray and red soft tissue
with a total volume of ~1.1×0.6×0.3 cm. The maximum diameter of
gray-red coloration in the section area was ~0.6 cm, The texture of
the tissue was soft and no obvious capsule was observed.
Microscopic observation
The tissue was fixed with 4% neutral formalin (24 h
at 25°C) and embedded in paraffin, and 4-µm serial sections were
prepared that were subjected to hematoxylin and eosin (H&E)
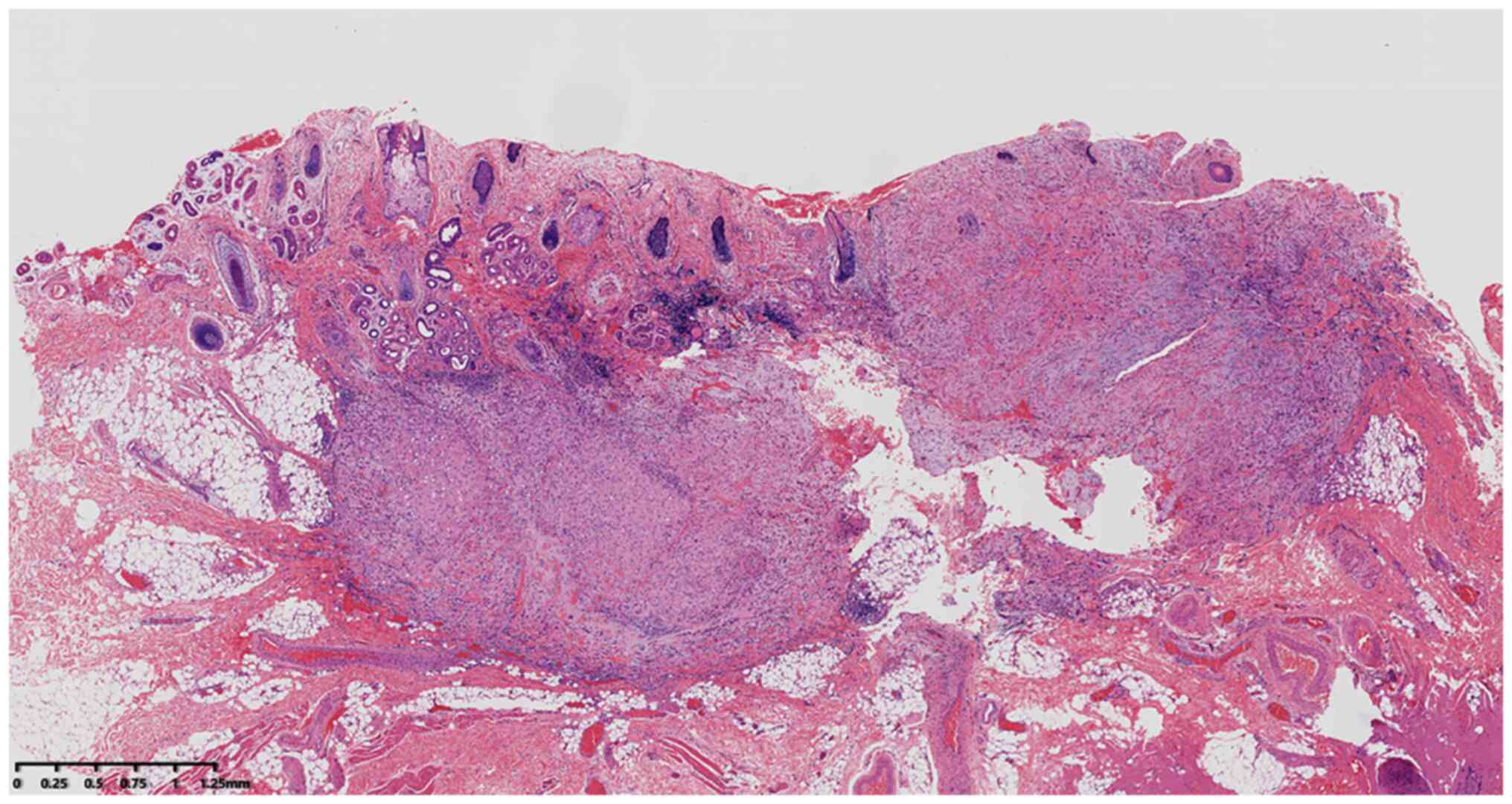
staining (8 h at 25°C). At low magnification (digital slice
scanner; Ningbo Jiangfeng Biological Information Technology, Co.,
Ltd.), the tumor showed nodular and solid patchy growth in the
dermis and subcutaneous adipose tissue (Fig. 1). No skin accessory recidivity was
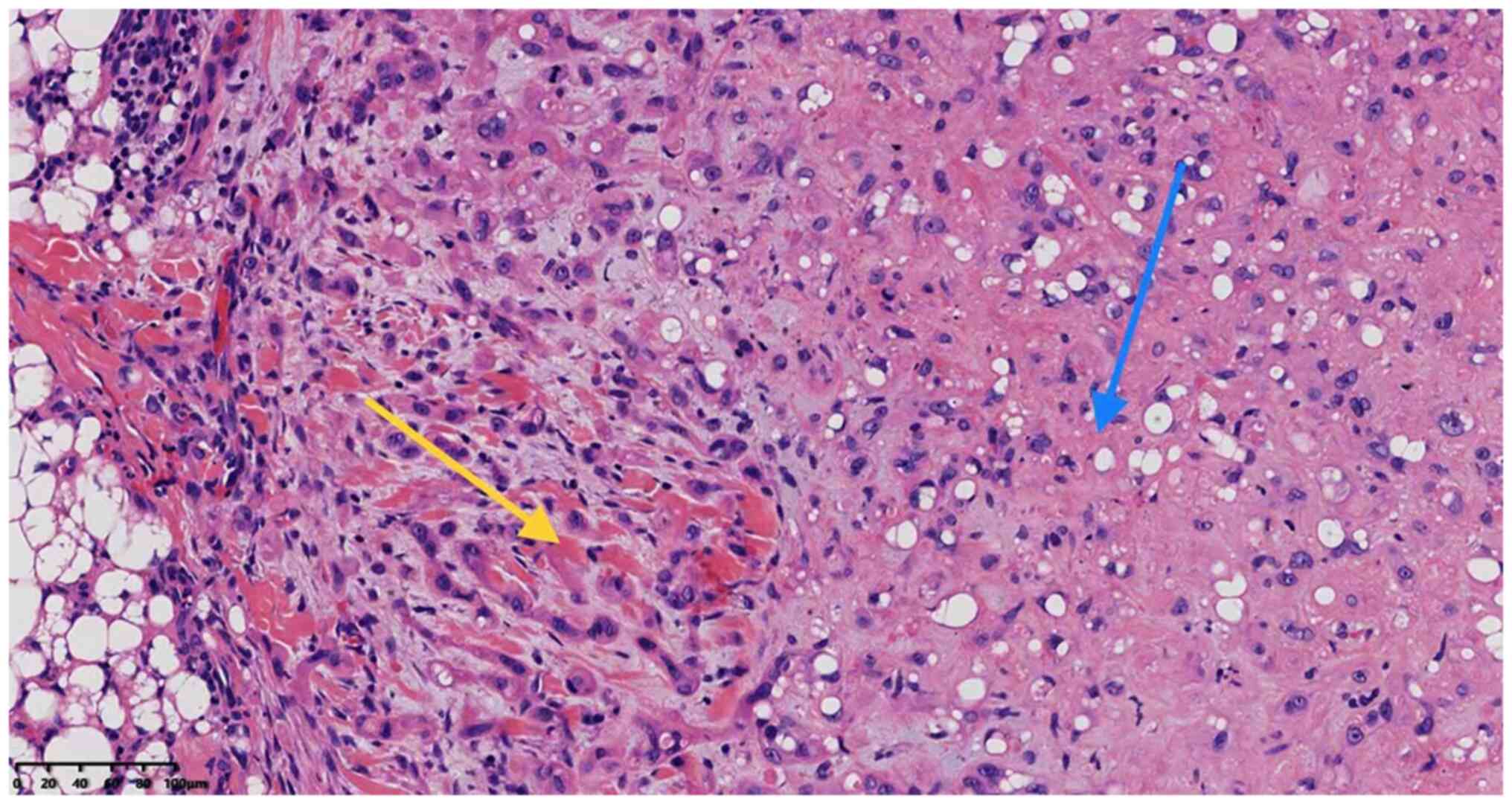
observed. At high magnification, the tumor cells consisted of
epithelioid cells (70%) and spindle cells (30%). The epithelial
cells were distributed in the shape of nests and cords, and the
cells were round and oval, with some ill-defined boundaries,
enlarged nuclei, lightly stained chromatin, partial thick nuclear
membrane, nucleoli, no mitotic signs, no obvious atypia, abundant
eosinophilic cytoplasm and partial nuclear deviated cytoplasm with
signet ring-like or vacuolated changes (Figs. 2 and 3). Red blood cells could be seen in the
lumen where the original blood vessels were formed (Fig. 4). Extensive branching and
antler-like structures were not seen in areas with high vascular
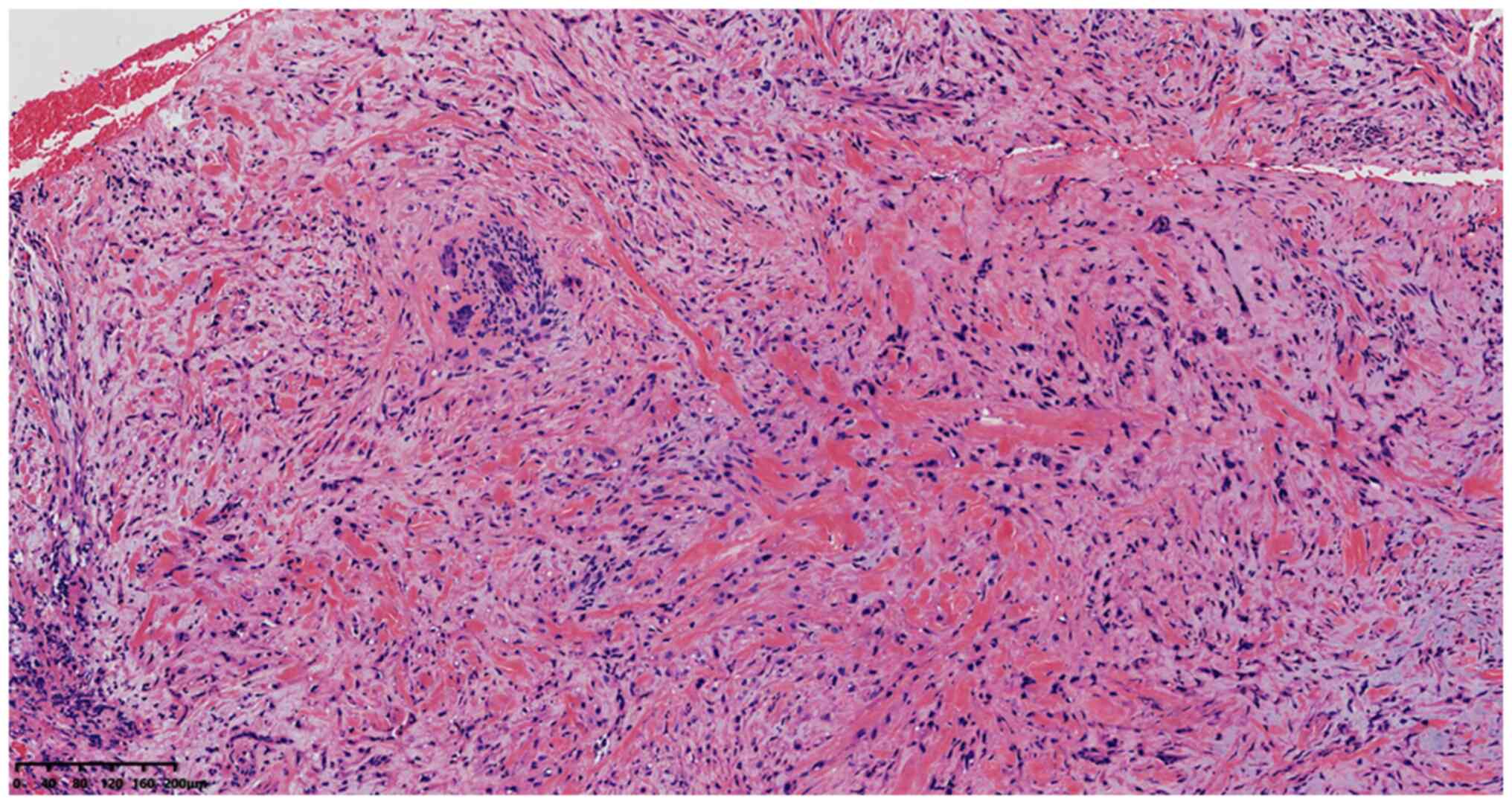
density. Some spindle cells were distributed in a braided shape,
and the cells were long and spindle-like, with no abnormal nuclei,
hyperchromatic nuclei and no mitosis (Fig. 5). Areas of epithelioid and spindle
cells transitioned with each other (Fig. 6). The interstitial area had myxoid
degeneration (Fig. 7) and was
collagenous. There was no eosinophil infiltration, no necrosis, no
vascular and nerve recidivization, and the incision margin was
positive.
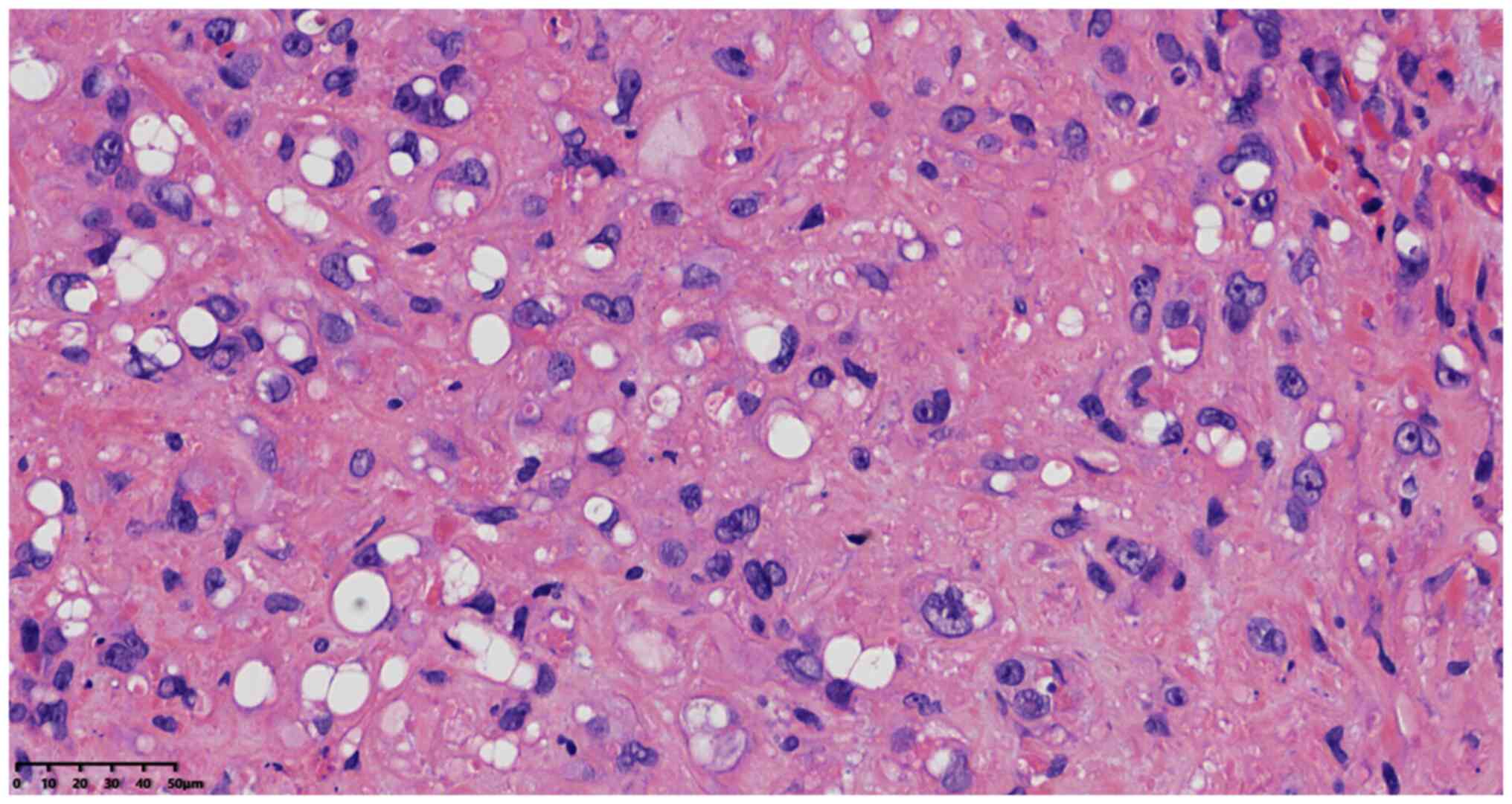
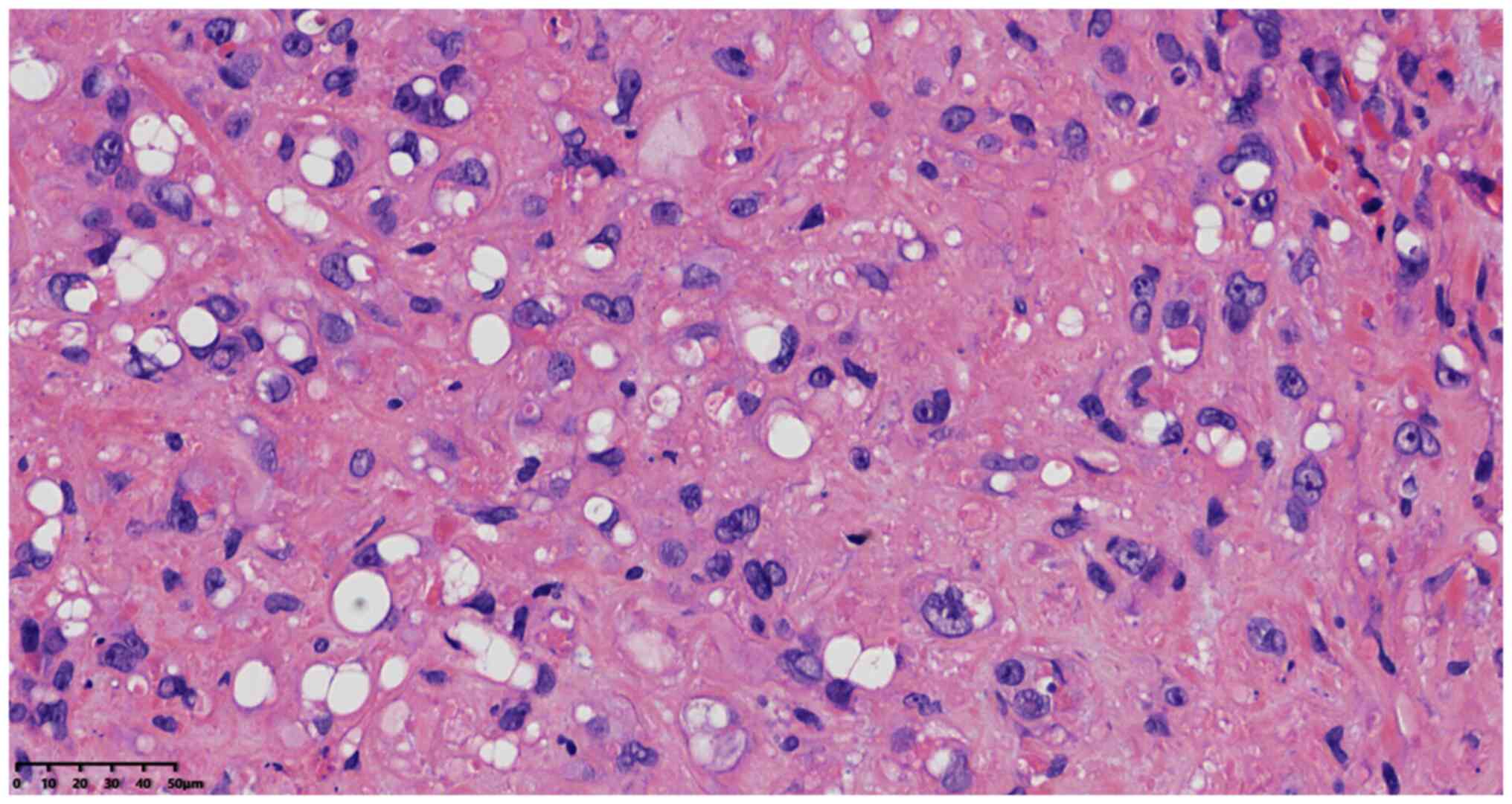 | Figure 3.Cells were round and oval, with some
indistinct boundaries, enlarged nuclei, lightly stained chromatin,
a thick nuclear membrane, nucleoli, no mitosis, no obvious atypia,
abundant eosinophilic cytoplasm and partial nuclear deviated
cytoplasm with signet ring-like or vacuolization changes
(magnification, ×400; scale bar, 50 µm; H&E staining). |
Immunohistochemical staining with the EnVision
Systems method using antibodies from Beijing Zhongshan Jinqiao
Biotechnology Co., Ltd., and Fuzhou Maixin Biotechnology
Development Co., Ltd., was performed at 37°C for 40 min for all
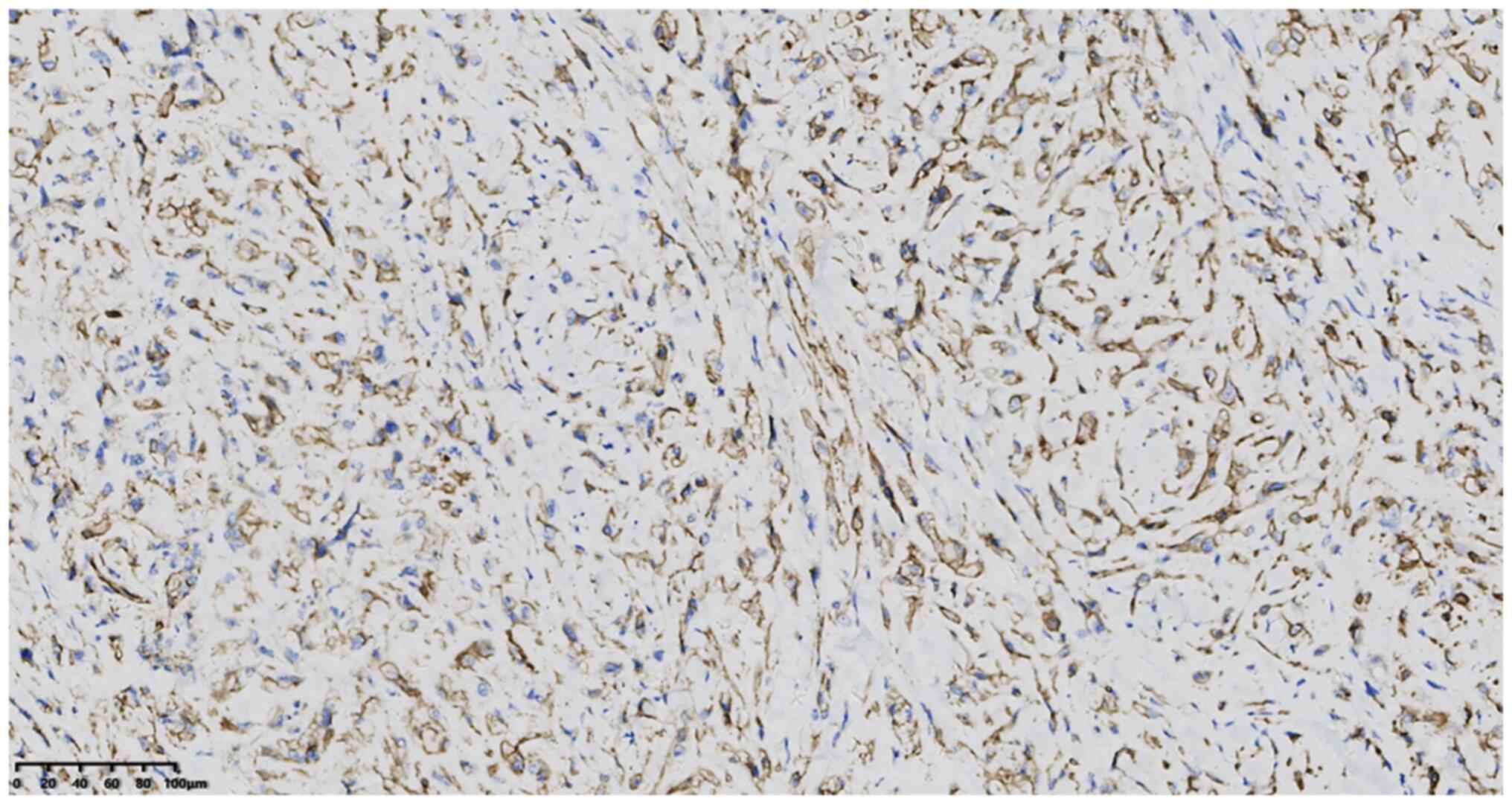
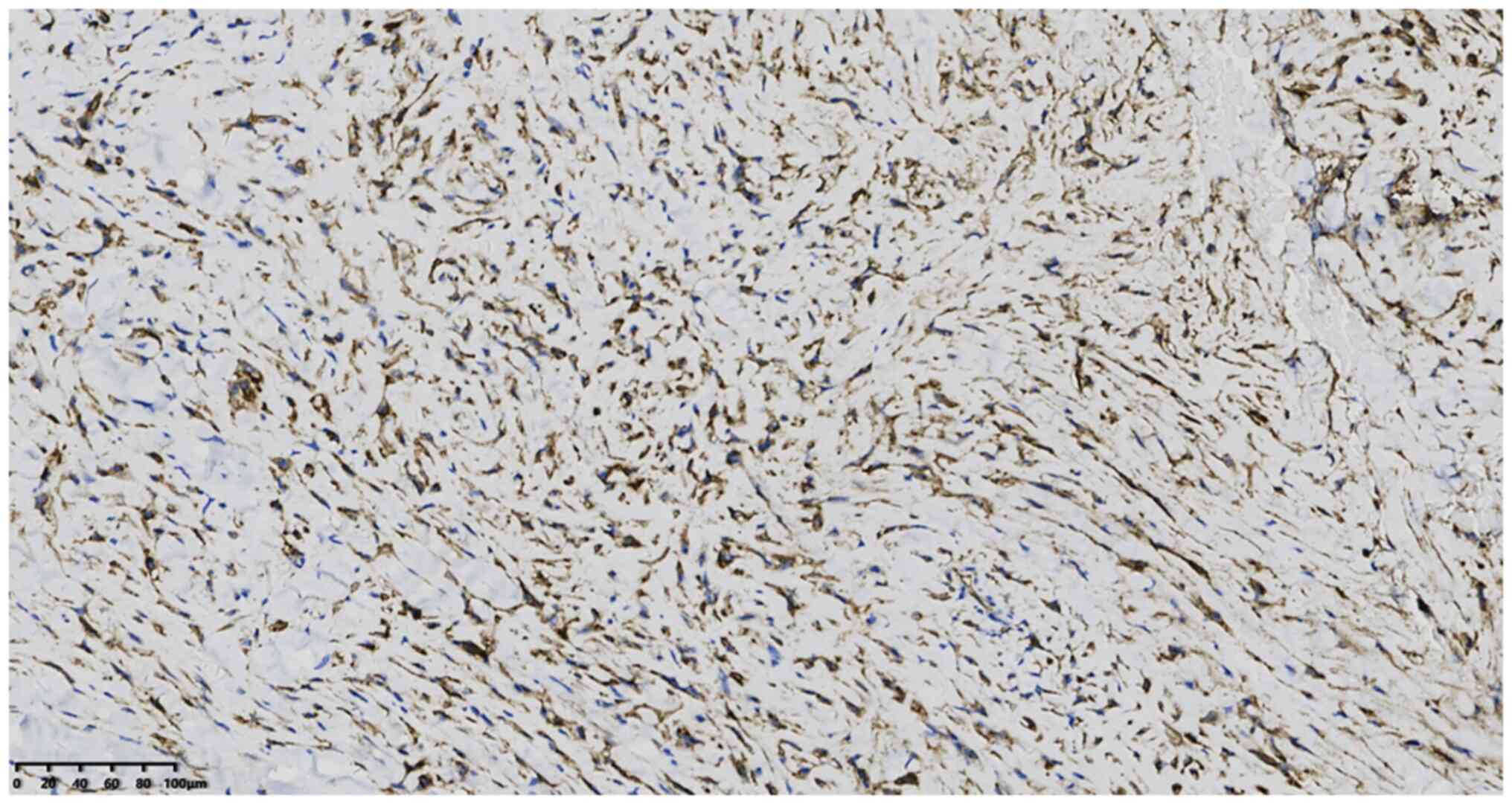
primary antibodies, with the following results: Positivity for CD34
(working liquid; cat. no. 2005270034b) (Fig. 8) and CD31 (working liquid; cat. no.
2104140720b) (Fig. 9), partial
positivity for smooth muscle actin (working liquid; cat. no.
21010809), weak positivity for cytokeratin (working liquid; cat.
no. 21061509), a negative result for Desmin (working liquid; cat.
no. 21011686), epithelial membrane antibody (working liquid; cat.
no 21020730), 34βE12 (working liquid; cat. no. 2109090052c4), p53
(working liquid; cat. no. 20082125) and S-100 protein (working
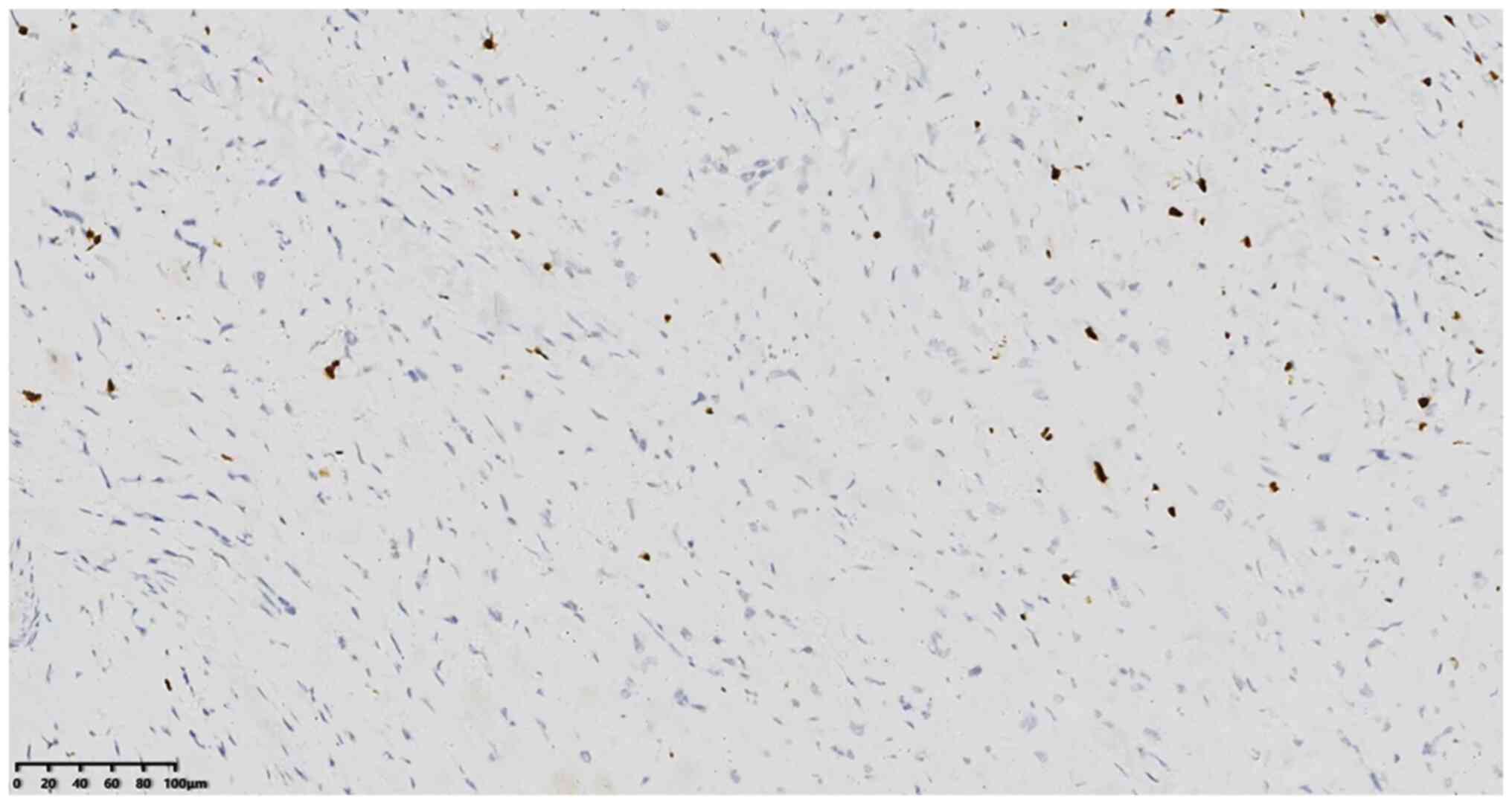
liquid; cat. no. 2012240585C8), and a positive result (3%) for the
Ki-67 proliferative index (1:200; cat. no. 21030436) (Fig. 10). DAB staining solution (polymer
method; KIT-0014) was used at 25°C for 20 min, and results were
assessed using a digital slice scanner (Ningbo Jiangfeng Biological
Information Technology Co., Ltd.).
Pathological diagnosis
The tumor recurred 3 months after the operation, as
the first incision margin was positive. The patient underwent an
extended tumor resection 3 months after this first recurrence. This
time, the pathological analysis showed EH with a negative margin.
The patient is still being followed up after the second
operation.
Discussion
EH is a kind of vascular endothelial cell tumor with
a low degree of malignancy that was first reported by Weiss and
Enzinger (1) in 1982. Since 2002,
the WHO has classified EH as a malignancy (2,3). EH
occurs in superficial or deep soft tissues such as those of the
extremities, liver, lungs and bone, and rarely in the orbit and/or
eyelids (4,5). Since Tsuji et al (6) first reported EHE in 2010, to the best
of our knowledge, only 4 cases have been reported worldwide
(6–9). Combined with the present case, these
5 cases were analyzed in the present literature review.
The age range of EHE, from the literature review
cases reported in Table I, is
between 10 and 55 years old, the mean age is 29.8 years old and the
male to female ratio is 1:4. EHE occurs in a 4:1 ratio of upper and
lower eyelids. Clinical manifestations included a mass on the
eyelid, painless swelling or mild pain, potentially accompanied by
eyelid ptosis. Some of the EHEs had a red or pink raised
appearance, and one patient had lost eyelashes (6). Palpation showed small nodules or
irregular masses with poor mobility. Some cases were clinically
diagnosed as hemangioma, chalazion or cysts. Computed tomography
and magnetic resonance imaging showed multiple eyelid tumors
extending into the orbit without bone tissue involvement in one
case (9). In some patients, other
general examinations such as blood routine, liver and kidney
function tests, chest radiography and abdominal ultrasound showed
no abnormalities.
 | Table I.Clinicopathological data of five
patients with eyelid epithelioid hemangioendothelioma. |
Table I.
Clinicopathological data of five
patients with eyelid epithelioid hemangioendothelioma.
| First author,
year | Sex | Patient age,
years | Location of
tumor | Maximum tumor
diameter, cm | Treatment |
Recurrence/metastasis | Follow-up time,
months | (Refs.) |
|---|
| Tsuji et al,
2010 | F | 34 | Upper left | 0.6 | Tumorectomy | No | 14 | (6) |
| Al-Faky et al,
2011 | F | 27 | Lower right | 0.5 | Local resection | No | 24 | (7) |
| Kiratli et al,
2013 | F | 22 | Upper left | Not published | Lumpectomy | No | 44 | (8) |
| Ennouhi et al,
2018 | M | 55 | Upper right | Not published | Complete resection
was performed after the second recurrence | Yes | 60 | (9) |
| Present study | F | 10 | Upper left | 0.6 | Tumorectomy | Yes | 3 | - |
Pathological examination showed that none of the
tissues from the five cases had a capsule, and the sections were
pink, reddish, grayish brown, and soft or hard in texture and
bleeding. Microscopic histological examination was similar to EH in
other soft-tissue sites. The tumor was composed of hyperplasia of
epithelial-like and fusiform vascular endothelial cells, and myxoid
stroma was seen in two cases (including the present case) (6). Epithelioid cells are round, oval or
polygonal whereas spindle cells contain little cytoplasm and some
nuclei are hyperchromatic without atypia. These cells form a mass
of primitive blood vessels containing one or more red blood cells
in the lumen. In one case, tumor cells in the eyelid were involved
with the lacrimal glands, and erythrocytes could be seen in the
cavity of local cells, with obvious vacuolation of the cytoplasm
and occasional mitosis, without atypia, extensive branching or
antler-type vessels (8). When
comparing the immunohistochemical results, CD31 was positive in 80%
of the cases, CD34 was positive in all cases, EMA was positive in
one case, factor VIII was focal positive in 1/2 of the cases and
the Ki-67 proliferative index was <10%. A molecular genetics
study showed that EH had a specific chromosomal translocation of
t(1;3)(p36.3;q25) and produced a WWTR1-CAM TAI fusion gene
(10), whereas additional studies
observed that a small portion of EH cases possessed
t(x;11)(pl1;q22), which produced a YAP1-TFE3 gene translocation
(11,12). This translocation can be detected
by fluorescence in situ hybridization examination or reverse
transcription-polymerase chain reaction, as well as
immunohistochemistry with CAMTA1 and TFE3 markers (12–14).
In the present case, the tumor was composed of epithelioid and
spindle cells, with primitive blood vessels and signet ring-like or
vacuolated structures. Immunohistochemical studies showed that the
tumor cells diffusely stained positive for CD34 and CD31, p53 was
negative and the Ki-67 labeling index was 3%. The pathological
diagnosis was consistent with EHE.
EHE should be distinguished from the following
tumors: i) Epithelioid hemangiosarcoma: The tumor is often
characterized by irregular vascular lumens, invasive or destructive
growth of neoplastic vessels, obvious cell atypia, large and
vacuolated nuclei with obvious nucleoli, and distinguishable
mitotic images. ii) Epithelioid sarcoma: Mainly occurs in distal
extremities, it is polynodular under the microscope, with obvious
necrosis or hyaloid degeneration in the tumor center, obvious
epithelioid cell atypia, distinguishable mitotic images, no obvious
primitive blood vessels, and cytoplasmic ring-like or vacuolated
structures. iii) Poorly differentiated adenocarcinoma: When EH
tumor occurs in the pleura, bones and other sites, it is easy to
misdiagnose as cancer when the cells are signet ring-like, but the
epithelial marker is positive, the vasogenic marker is negative and
the primary site can be distinguished. iv) Epithelioid hemangioma:
A benign vascular tumor with epithelioid endothelium, also known as
vascular lymphoid tissue hyperplasia accompanied by eosinophilia.
Endothelial cells are distributed on the lumen surface, and
intra-lumen and paravascular surfaces. The tumor may be solid and
patchy and is distinguished by interstitial eosinophilia. v) Eyelid
sebaceous gland cyst: Clinical palpation of this disease diagnoses
a cystic sensory benign lesion and B-mode ultrasound can be used to
find the cyst. Pathological examination of the cysts reveals that
they contain oil, the cyst wall consists of squamous epithelium
and, occasionally, the skin appendage can be seen. vi) Eyelid stye:
Eyelid gland infection caused by eyelid swelling with diffuse pain.
Some indurations caused by infection are palpable and some are not.
Eyelid styes are generally eliminated with anti-inflammatory
medication.
EH treatment is based on an extensive tumor
resection to ensure a negative margin. Chemotherapy and
radiotherapy are also recommended, but the efficacy of radiotherapy
and chemotherapy is not optimal (15). The overall 5-year survival rate for
EH is 73%. It occurs in soft tissues, with a local recurrence rate
of 10–15%, a metastasis rate of 20–30%, mainly to the regional
lymph nodes, lungs and liver, and a mortality rate of 10–20%
(2). In the literature review,
three cases of EHE underwent surgical resection and no recurrence
or metastasis was observed at the 14–44 month follow-up periods
(6–8). Ennouhi et al (9) reported a case of recurrence due to a
positive surgical margin twice, but no recurrence or metastasis was
found in the 60 months of follow-up after the third surgical
resection.
In conclusion, EHE is a rare low-grade malignant
tumor, and its diagnosis needs to be confirmed by pathology and
immunohistochemistry. We believe that a negative margin should be
ensured after the pathological diagnosis of EHE is confirmed in the
surgically resected specimens. If the margin is positive, the
resection should be expanded in time to prevent recurrence. Since
EHE is rare, its clinical, pathological and therapeutic outcomes
need to be further explored.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LC and BH drafted the manuscript and conceived the
study. HL and FH were responsible for the collection and analysis
of case data and literature. BH, JY and HL revised the manuscript
and interpreted the data. BH and HL confirm the authenticity of all
the raw data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The mother of the patient provided written informed
consent for the case study to be published.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Weiss SW and Enzinger FM: Epithelioid
hemangioendothelioma: A vascular tumor often mistaken for a
carcinoma. Cancer. 50:970–981. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wang J and Zhu X: Pathology of soft tissue
tumor [M]. 2nd Ed. Beijing: People's Medical Publishing House; pp.
809–819. 2017, (In Chinese).
|
|
3
|
Fletcher CD, Unni KK and Mertens F: WHO
classification of tumours. Pathology and genetics of tumours of
soft tissue and bone. IARC Press; Lyon: 2002
|
|
4
|
Zaragoza-Herrera A, Morales-Baños DR,
Velasco-Ramos P, Garrido-Sánchez GA, López-Hernández CM and
Borbolla-Pertierra AM: Case report: Orbital epithelioid
haemangioendothelioma. Arch Soc Esp Oftalmol. 92:pp184–188. 2016.
View Article : Google Scholar
|
|
5
|
Su F, Ma R, Zhang N, Li YY, Hei Y, Xu X
and Yang XJ: A case report of orbital epithelioid
hemangioendothelioma. Zhonghua Yan Ke Za Zhi. 57:696–699. 2021.(In
Chinese).
|
|
6
|
Tsuji H, Kanda H, Kashiwagi H and Mimura
T: Primary epithelioid haemangioendothelioma of the eyelid. Br J
Ophthalmol. 94:261–262. 2010. View Article : Google Scholar
|
|
7
|
Al-Faky YH, Al Malki S and Raddaoui E:
Hemangioendothelioma of the eyelid can mimic chalazion. Oman J
Ophthalmol. 4:142–143. 2011. View Article : Google Scholar
|
|
8
|
Kiratli H, Tarlan B and Ruacan S:
Epitheloid hemangioendothelioma of the palpebral lobe of the
lacrimal gland. Orbit. 32:120–123. 2013. View Article : Google Scholar
|
|
9
|
Ennouhi MA, Guerrouani A and Moussaoui A:
Epithelioid hemangioendothelioma, an uncommon tumor of the eyelid:
A case report. J Stomatol Oral Maxillofac Surg. 119:40–43. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Errani C, Zhang L, Sung YS, Hajdu M,
Singer S, Maki RG, Healey JH and Antonescu CR: A novel
WWTR1-CAM-TAl gene fusion is a consistent abnormality in
epithelioid hemangioendothelioma of different anatomic sites. Genes
Chromosomes Cancer. 50:644–653. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Doyle LA, Fletcher CD and Hornick JL:
Nuclear expression of CAMTA1 distinguishes epithelioid
hemangioendothelioma from histologic mimics. Am J Surg Pathol.
40:94–102. 2016. View Article : Google Scholar
|
|
12
|
Puls F, Niblett A, Clarke J, Kindblom LG
and McCulloch T: YAPI-TFE3 epithelioid hemangioendothelioma: A case
without vasoformation and a new transcript varian. Virchows Arch.
466:473–478. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Antonescu CR, Le Loarer F, Mosquera JM,
Sboner A, Zhang L, Chen CL, Chen HW, Pathan N, Krausz T, Dickson
BC, et al: Novel YAPI-TFE3 fusion defines a distinct subset of
epithelioid hemangioendothelioma. Genes Chromosomes Cancer.
52:775–784. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shibuya R, Matsuyama A, Shiba E, Harada H,
Yabuki K and Hisaoka M: CAMTA1 is a useful immunohistochemical
marker for diagnosing epithelioid haemangioendothelioma.
Histopathology. 67:827–835. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lasselin-Boyard P, Olivier Boulet P,
Grados F, Sevestre H and Goëb V: Premier casde vertébroplastie pour
un hémangioendothéliome épithéliolde. Rev Rhum. 82:137–138. 2015.
View Article : Google Scholar
|