Introduction
Cervical cancer is the fourth most common type of
cancer in women according to the World Health Organization and a
worldwide analysis from 2018 (1).
Adenocarcinoma in situ (AIS) is considered a precursor of
adenocarcinoma (2). The current
global incidence rate of AIS is 6.6 per 100,000 individuals, with a
mean age of 35–37 years at diagnosis (3). The proportion of cytological smears
that display dysplasia and/or abnormalities varies considerably
between countries, from 0.98 to 15.5% (4,5).
Notably, histological diagnosis of AIS can develop from either
glandular or squamous abnormalities (6).
In Germany, there are guiding rules regarding the
performance of cervical screening for women and cytological
diagnosis is graded according to the Munich classification III
(7) (Table I). This classification system is
quite similar to the Bethesda classification (8) but with some details in subgroup II-e,
which is defined as when abnormal endometrial cells are detected in
the cytology from women >40 years old in the second phase of the
menstrual cycle. In addition, in the Muenchener classification III,
there is a separation of high-grade squamous lesions into IIID2 and
IVa-p, whereas in the Bethesda system, both moderate and high
dysplasia are classified under one grade, high-grade squamous
intraepithelial lesion (Table I)
(8).
 | Table I.Association of Muenchener
classification III with Bethesda classification. |
Table I.
Association of Muenchener
classification III with Bethesda classification.
| Group | Definition | Bethesda
classification |
|---|
| 0 | Not enough
material | Unsatisfactory for
evaluation |
| I | No abnormality | NILM |
| II-a | No abnormality with a
history of abnormal cytological diagnosis | NILM |
| II-p | Squamous cells with
morphological changes but not CIN I | ASC-US |
| II-g | Endocervical glands
with morphological changes e.g., irritation | AGC endocervical
NOS |
| II-e | Endometrial glands in
women >40 years old in second phase of menstrual cycle | Normal endometrial
cells |
| III-p | Atypical squamous
cells: CIN II/III or squamous cell carcinoma are to be
considered | ASC-H |
| III-g | Atypical glandular
cells: AIS/Adenocarcinoma are to be considered | AGC endocervical
favor neoplastic |
| III-e | Abnormal endometrial
glands especially postmenopausal | AGC endometrial |
| III-x | Anormal glands not
endocervical or endometrial | AGC favor
neoplastic |
| IIID1 | Squamous cells with
mild dysplasia (CIN I) | LSIL |
| IIID2 | Squamous cells with
moderate dysplasia (CIN II) | HSIL |
| IVa-p | Squamous cells with
high dysplasia (CIN III) | HSIL |
| IVa-g | Endocervical cells
with high dysplasia (AIS) | AIS |
| IVb-p | Squamous cells with
high dysplasia that may be squamous cell carcinoma | HSIL with features of
invasion |
| IVb-g | Endocervical cells
with high dysplasia (AIS) and may be invasion | AIS with features of
invasion |
| V-p | Squamous cell
carcinoma | Squamous cell
carcinoma |
| V-g | Endocervical
adenocarcinoma | Endocervical
adenocarcinoma |
| V-e | Endometrial
adenocarcinoma | Endometrial
adenocarcinoma |
| V-x | Other type of
malignancy | Other malignant
neoplasms |
In Germany (9),
under the age of 30 years, cervical screening depends mainly on
conventional cytological methods, including either cervical smear
or liquid-based techniques. Between the ages of 30 and 34 years,
cervical screening is performed according to conventional methods,
with the possibility of performing human papillomavirus (HPV)
testing 6 months after conventional cytology in cases with atypical
morphology (II-p, II-g and IIID1). From the age of 35 years,
cervical screening consists of both conventional cytological
methods and HPV testing. Other countries have investigated the
differences between cervical screening methods, and countries such
as Australia and the Netherlands perform cervical screening only
with detection of high-risk HPV (HPV-HR) (10). Currently, different approaches are
used as some researchers depend completely on the detection of HPV
subtypes, focusing on HPV16 and HPV18, as the major causes for the
development of squamous and glandular cervical lesions.
While assessing the literature, no study was
identified that had examined the association between the presence
of II-e or III-e cytology with histological findings in cervical
biopsies. Furthermore, to the best of our knowledge, no previous
study assessed the distribution of lesions, such as those with II-g
and III-g cytology, in different age groups and their association
with HPV subtypes. The present study assessed glandular lesions
(II-g, II-e, III-g, III-e, IVa-g, IVb-g, V-g and V-e) in different
age groups, and determined their association with HPV subtypes and
the histopathological diagnosis of cervical biopsies. The aim of
the present study was to avoid the misdiagnosis of squamous cell
changes and endometrial glandular lesions as endocervical glandular
lesions in the presence of metaplasia or atypia in cervical
screening; therefore, a colposcopy and histopathological diagnosis
of biopsies should follow cytological investigation in highly
suspicious cases. The present study highlighted the importance of
combining cytological screening and HPV genotyping as a predictive
method in cases at risk of developing dysplastic, premalignant and
malignant glandular lesions. The present study also aimed to ensure
that screening by performing cytological examination and HPV
genotyping could detect HPV-negative adenocarcinoma, HPV-negative
gastric-type AIS and non-cervical adenocarcinoma
(metastasis/infiltration). Vaccination against HPV infection should
be further increased to protect women against dangerous
subtypes.
Materials and methods
Patient samples, age and methods of
investigation
At the Institute for Pathology and Cytology
(Schüttorf, Germany), 210,510 female cytological samples were
analyzed between the beginning of January 2020 and the beginning of
January 2021. A total of 63,710 samples were from women <35
years old and 146,791 samples were from women ≥35 years old. The
samples were processed for both conventional cytological
techniques, and for molecular detection and subtyping of HPV-HR
according to the advice and measurements of BD Biosciences (117,765
samples) using Viper-Test and the PapilloCheck® HPV test
(5,579 samples). The difference of ~87,000 samples resulted either
from women <35 years old without medical reasons to detect the
HPV subtypes because they exhibited normal cytology (grade I,
according to Munich classification) or they were not tested at our
institute or due to samples with few cells.
Study approach
The present study included the cases (n=123,344) for
which both conventional cytology and HPV molecular analysis are
available. According to BD Biosciences, certain HPV-HR subtypes
were studied, namely HPV16, 18, 45, 31, 33, 52, 58, 35, 59, 56, 51,
39, 68, 73, 82, 53, 66, 70, 6, 40, 42, 43, 44/45, 33/58, 56/59/66
and 35/39/68. The present study focused on the HPV vaccination
history of the patients and divided the dataset into the following
age groups: <35, 35–40, 41–50, 51–60 and >60 years. In these
groups, the present study focused on the presence of atypical
glandular lesions, their association with HR-HPV subtypes and the
results of histopathology after colposcopy. The present study also
investigated the presence of atypical, precancerous and cancerous
endometrial glands in cervical cytology to detect the incidence of
occurrence in different age groups and to compare with the presence
of endocervical gland lesions. The grading of cytological diagnoses
was performed according to the Muenchener classification III
(Table I).
Ethics approval
The present study was approved by the Ethics
Committee of the Medical Association, Hannover, Germany (approval
no. Bo/14/2021). Informed consent for inclusion in the present
study was waived as patient records were anonymized and
retrospectively analyzed. The samples were anonymized to ensure
data protection.
Results
Distribution of glandular lesions in
relation to different age groups
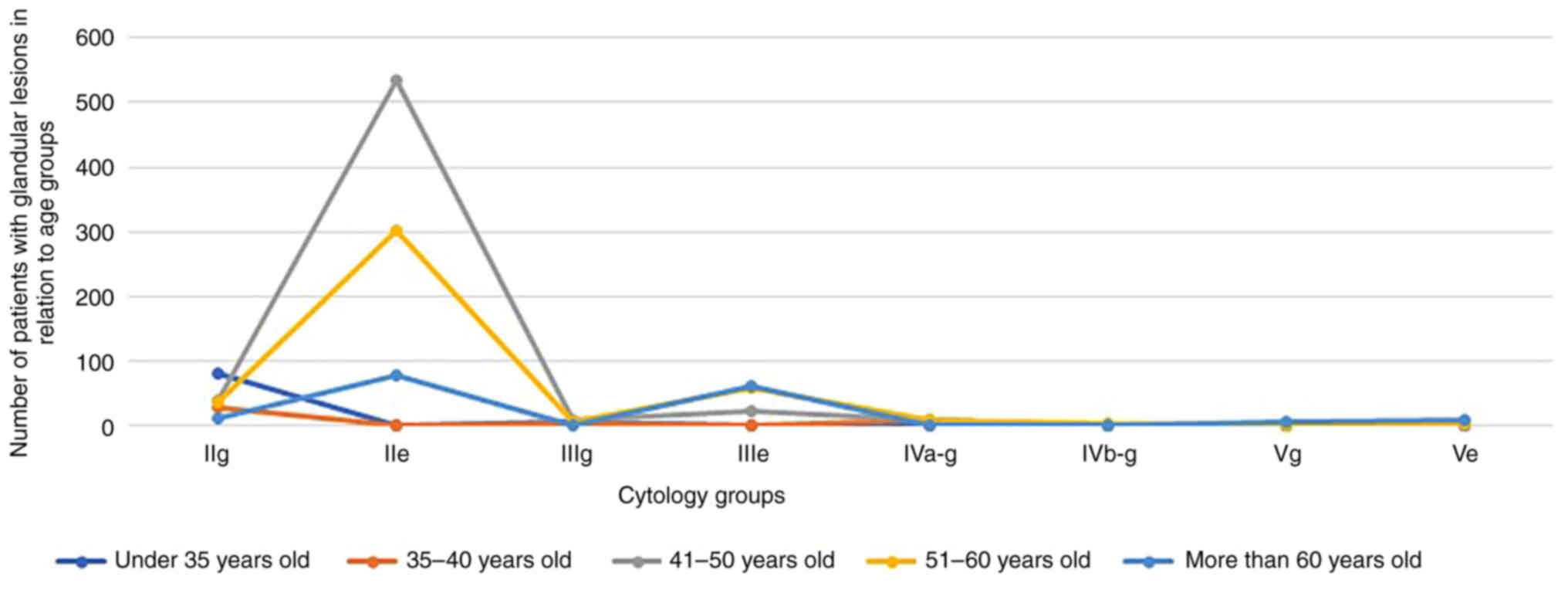
In individuals <35 years old, 0.12% cases had
II-g cytology. Another peak was noticed in the age groups 41–50 and
51–60 years (0.11%). There was a peak in the 41–50-years age group
for II-e (1.5%). There were few cases of III-g cytology in all age
groups, with the maximum detected in the 41–50-years age group
(0.023%). There were more cases of III-e in the 51–60 and
>60-years age groups (0.12%). A peak for IVa-g was observed in
the 41–50-years age group (0.028%). V-g and V-e cytology were
highest in the >60-years age group (0.012 and 0.016%,
respectively) (Table II; Fig. 1).
 | Table II.Distribution of glandular lesions in
relation to different age groups. |
Table II.
Distribution of glandular lesions in
relation to different age groups.
| Age group (number of
patients) | II-g | II-e | III-g | III-e | IVa-g | IVb-g | V-g | V-e |
|---|
| <35 years old
(63,710) | 81 | 0 | 7 | 1 | 2 | 1 | 1 | 0 |
| 35–40 years old
(22,136) | 28 | 0 | 3 | 1 | 9 | 0 | 0 | 0 |
| 41–50 years old
(34,667) | 40 | 534 | 8 | 23 | 10 | 0 | 1 | 0 |
| 51–60 years old
(41,276) | 38 | 302 | 7 | 59 | 8 | 3 | 0 | 4 |
| >60 years old
(48,721) | 11 | 78 | 1 | 61 | 2 | 0 | 6 | 8 |
Vaccine status, HPV status and
histopathological diagnosis in the different age groups
Among individuals <35 years old, 0.03% were
vaccinated (Table III). There
were four cases with IVa-g (two cases), IVb-g (one case) and V-g
(one case), and no endometrial carcinoma (V-e) was detected in this
age group. Among individuals aged 35–40 years old, there was
prominence of II-g (0.126%) (Table
IV). Notably, there was only one vaccinated case in this group
(35–40 years old). In addition, in this age group, the following
HPV-HR subtypes were detected: 16, 18, 45, 56/59/66, 35/39/68 and
52. There was no IVb-g, V-g or V-e cytology detected in this age
group. There were two cases negative for HPV-HR subtypes, and with
histopathological diagnoses of cervical intraepithelial neoplasia
(CIN) II and CIN III. Among individuals aged 41–50 years old, there
was prominence of II-e (1.54%) (Table
V). There was only one vaccinated case (0.0028%) in this group.
In addition, in this age group, there was one case negative for
HPV-HR but that was histopathologically diagnosed with AIS. Among
individuals aged 51–60 years old, there was prominence of II-e
(0.73%) and there was one vaccinated case in this group (Table VI). In addition, in this age
group, the following HPV-HR subtypes were detected: 16, 18, 45, 51,
52, 31, 33/58, 35/39/68 and 56/59/66. A total of 10 cases of
endometrial carcinoma and 19 cases with molecular pathological
detection of HPV-HR (HPV18 and 52) and without histopathological
dysplasia were detected. Among individuals aged >60 years old,
there were more cases of III-e (0.125%) and no vaccinated cases
(Table VII). In addition, in
this age group, the following HPV-HR subtypes were detected: 16,
35/39/68, 33/58, 18, 52 and 56/59/66. Endometrial carcinoma was
detected in 21 cases and endocervical adenocarcinoma in five cases,
and there were single cases of CIN I, CIN III and squamous cell
carcinoma detected.
 | Table III.Vaccination status, HPV status and
histopathological diagnosis in women <35 years old. |
Table III.
Vaccination status, HPV status and
histopathological diagnosis in women <35 years old.
| Variable | II-g | II-e | III-g | III-e | IVa-g | IVb-g | V-g | V-e |
|---|
| Total patients
(n=63,710) | 81a | 0 | 7 | 1 | 2b | 1 | 1 | 0 |
| Vaccinated, n | 20 | 0 | 1 | 0 | 1 | 0 | 0 | 0 |
| Not vaccinated,
n | 60 | 0 | 6 | 1 | 0 | 0 | 0 | 0 |
| HPV status, n (HPV
type) | 70 (n=1) | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Histopathology | 0 | 0 | AIS (n=1), | 0 | WD | Sq.c.ca. | endo.aden. | 0 |
|
|
|
| WD (n=6) |
| (n=2) | (n=1) | (n=1) |
|
 | Table IV.Vaccination status, HPV status and
histopathological diagnosis in women 35–40 years old. |
Table IV.
Vaccination status, HPV status and
histopathological diagnosis in women 35–40 years old.
| Variable | II-g | II-e | III-g | III-e | IVa-g | IVb-g | V-g | V-e |
|---|
| Total patients
(n=22,136) | 28 | 0 | 3 | 1a | 9 | 0 | 0 | 0 |
| Vaccinated, n | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| Not vaccinated,
n | 28 | 0 | 3 | 0 | 8 | 0 | 0 | 0 |
| HPV status | 18 (n=1), 45 (n=2),
56/59/66 (n=1), 35/39/68 (n=1) | 0 | 68 (n=1), 56/59/66
(n=1), 45 (n=1) | 0 | 52 (n=1), 18 (n=1),
18 and 31 (n=1), 16 (n=1) | 0 | 0 | 0 |
| Histopathology | CIN II with HPV18
(n=1) | 0 | CIN II with HPV45
(n=1) | WD (n=1) | AIS with HPV18
(n=1), CIN III with HPV16 (n=1) | 0 | 0 | 0 |
| Histopathology
negative for HPV-HR | 0 | 0 | 0 | 0 | CIN III (n=1), CIN
II (n=1), WD (n=2) | 0 | 0 | 0 |
 | Table V.Vaccination status, HPV status and
histopathological diagnosis in women 41–50 years old. |
Table V.
Vaccination status, HPV status and
histopathological diagnosis in women 41–50 years old.
| Variable | II-g | II-e | III-g | III-e | IVa-g | V-g |
|---|
| Total patients
(n=34,667) | 40 | 534 | 8 | 23 | 10 | 1 |
| Vaccinated, n | 0 | 0 | 0 | 0 | 1 | 0 |
| Not vaccinated,
n | 40 | 534 | 8 | 23 | 9 | 1 |
| HPV status | 56/59/66 (n=1) | 16 (n=3), 18 (n=2),
31 (n=5), 52,56/59/66 (n=1), 51 (n=1), 33/58 (n=1), 56/59/66 (n=2),
35/39/68 (n=3) | 18 (n=2), 52 (n=1),
31 and 52 (n=1) | 16 (n=1) | 16 (n=2), 18 (n=3),
52 and 33/58 (n=2), 16 and 31 (n=1), 35/39/68 (n=1) | 0 |
| Histopathology | WH (n=1) | WH (n=17) | endo.ca with HPV18
(n=1), WD with HPV18 (n=1), CIN II with HPV52 (n=1), CIN III with
HPV31 and 52 (n=1), AIS with HPV-HR− (n=1) | Sq.c.ca with HPV16
(n=1), WD with HPV-HR− (n=22) | sq.c.ca with HPV16
(n=1), endo.ca. with HPV16 (n=1), CIN III with HPV18 (n=1), AIS
with HPV18 (n=1), AIS with HPV16 and 31 (n=1), CIN III with HPV52
and 33/58 (n=1), CIN III with HPV35/39/68 (n=1) | endo.ca. |
 | Table VI.Vaccination status, HPV status and
histopathological diagnosis in women 51–60 years old. |
Table VI.
Vaccination status, HPV status and
histopathological diagnosis in women 51–60 years old.
| Variable | II-g | II-e | III-g | III-e | IVa-g | IVb-g | V-e |
|---|
| Total patients
(n=41,276) | 38 | 302 | 7 | 59 | 8 | 3 | 4 |
| Vaccinated, n | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Not vaccinated,
n | 38 | 301 | 7 | 59 | 8 | 3 | 4 |
| HPV status | 16 (n=1), 52 (n=1),
35/39/68 (n=1), 56/59/66 (n=1), 16 and 56/59/66 (n=1) | 35/39/68 (n=2),
56/59/66 (n=2), 45 (n=1), 18 (n=3), 51 (n=1), 31 (n=1) | 45, 33/58
(n=2) | 0 | 18 (n=4), 16 (n=1),
52 (n=1) | 18 (n=2), 16
(n=1) | 16 (n=1) |
| Histopathology | WH with HPV 16, 52,
35/39/68, 56/59/66 and 16 and 56/59/66 (n=5) | WH with HPV18
(n=3), 31 (n=1), 45 (n=1), 51 (n=1), 35/39/68 (n=2) and 56/59/66
(n=2). | Sq.c.ca with HPV45
(n=1), WH with HPV33/58 (n=1), CIN I with HPV-HR− (n=2),
WD with HPV-HR− (n=1) CIN II with HPV-HR−
(n=1) | WD (n=27), end.ca.
(n=1), endomet.ca. (n=7) | AIS with HPV18 | endo.ca with
HPV18 | sq.c.ca with |
|
|
|
|
|
| (n=1), CIN II with
HPV18 (n=1), WD with HPV18 (n=1), AIS with HPV16 (n=1), WD with
HPV52 (n=1) | (n=1), endomet.ca
with HPV16 (n=1), WD with HPV16 (n=1) | HPV16 (n=1),
endomet.ca. with HPV-HR− (n=2) WD (n=1) |
 | Table VII.Vaccination status, HPV status and
histopathological diagnosis in women >60 years old. |
Table VII.
Vaccination status, HPV status and
histopathological diagnosis in women >60 years old.
| Variable | II-g | II-e | III-g | III-e | IVa-g | V-g | V-e |
|---|
| Total patients
(n=48,721) | 11 | 78 | 1 | 61 | 2 | 6 | 8 |
| Vaccinated, n | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Not vaccinated,
n | 11 | 78 | 1 | 61 | 2 | 6 | 8 |
| HPV status | 16 (n=1) | 16 (n=1), 35/39/68
(n=) | 0 | 16 (n=1) | 33/58 (n=1) | 18 (n=1),
52,56/59/66 (n=1) | 35/39/68 (n=1) |
| Histopathology | WH with HPV16
(n=1) | endomet.ca with HPV
16 and 35//39/68 (n=2). | WH with
HPV-HR−(n=1) | endomet.ca. with
HPV-HR− (n=15), WH with HPV16 (n=1), endo.ca. with
HPV-HR− (n=3) | CIN III with
HPV33/58 (n=1), CIN I with HPV-HR− (n=1) | endo.ca. with HPV
52 und 56/59/66 (n=1), endomet.ca. with HPV-HR− (n=2),
Sq.c.ca with HPV18 (n=1) | endomet.ca. with
HPV-HR− (n=2), endo. Ca. with HPV35/39/68 (n=1) WD with
HPV-HR− (n=2), WH with HPV-HR− (n=3) |
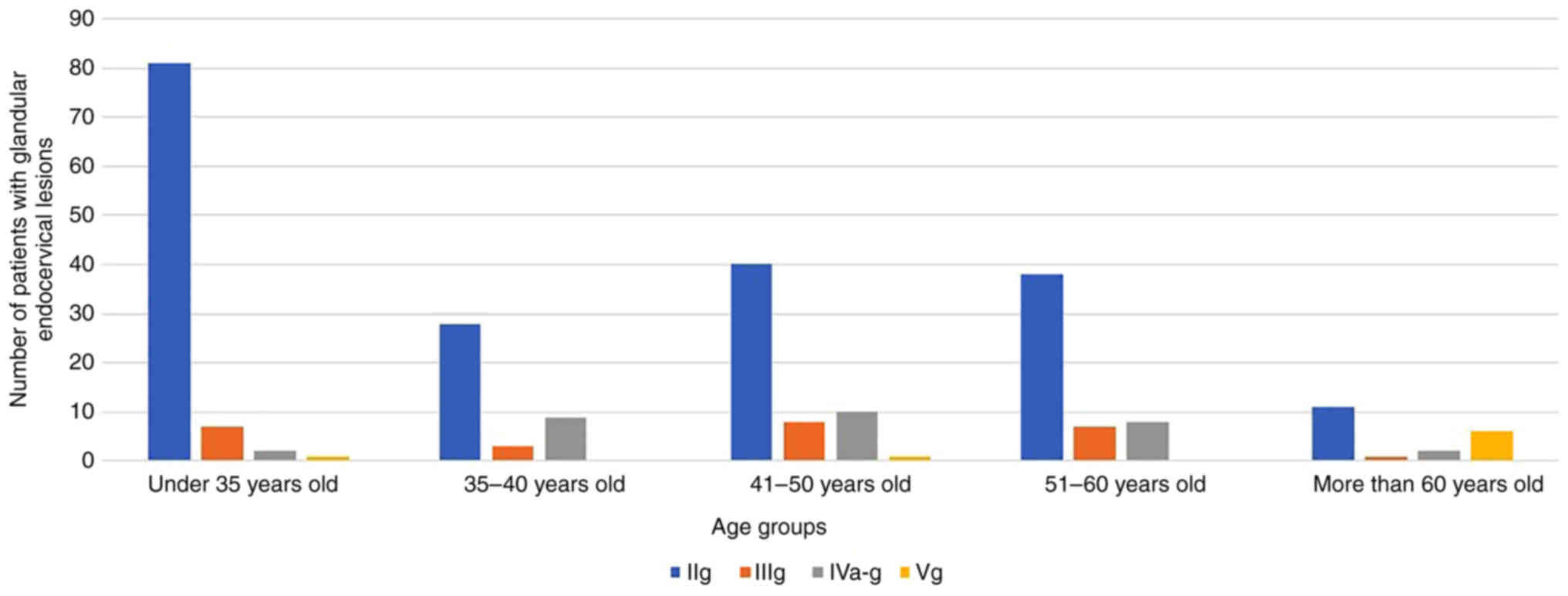
Association between glandular lesions
of endocervical glands and the different age groups
The prevalence of III-g cytology (15 cases) was high
in the 41–60-years age group (0.02%), whereas the prevalence of
IVa-g cytology was high in all age groups (0.04% in the 35–40-years
age group; 0.028% in the 41–60-years age group). Furthermore, V-g
cytology was detected in the <35-years (one case), 41–50-years
(one case) and >60 years (six cases) age groups, which may
indicate that there is no direct relationship between precursor
non-invasive lesions of endocervical glands and invasive
endocervical glandular lesions in almost all age groups (Table VIII; Fig. 2). Furthermore, different HPV-HR
subtypes were detected in all investigated age groups which may be
due to sexual activity, as HPV is mainly transmitted sexually. In
individuals >60 years old, only the following HPV subtypes were
detected: 16, 33/58, 18, 52 and 56/59/66, which may indicate the
persistence of these subtypes throughout life and the hazardousness
of these subtypes, due to the higher incidence of invasive cervical
carcinoma in older age groups (Table
IX).
 | Table VIII.Association between glandular lesions
of endocervical glands and age. |
Table VIII.
Association between glandular lesions
of endocervical glands and age.
| Age group | II-g | III-g | IVa-g | V-g |
|---|
| <35 years
old | 81 | 7 | 2 | 1 |
| 35–40 years
old | 28 | 3 | 9 | 0 |
| 41–50 years
old | 40 | 8 | 10 | 1 |
| 51–60 years
old | 38 | 7 | 8 | 0 |
| >60 years
old | 11 | 1 | 2 | 6 |
 | Table IX.Association between glandular lesions
and HPV status in the different age groups. |
Table IX.
Association between glandular lesions
and HPV status in the different age groups.
|
| Number of patients
(HPV type) |
|---|
|
|
|
|---|
| Cytology | <35 years
old | 35–40 years
old | 41–50 years
old | 51–60 years
old | >60 years
old |
|---|
| II-g | 1 (70) | 1 (18), 2 (45), 1 (56/59/66), 1
(35/39/68) | 1 (56/59/66) | 1 (16), 1 (52), 1 (35/39/68), 1 (56/59/66),
1 (16,56/59/66) | 1 (16) |
| III-g | 0 | 1 (68), 1
(56/59/66), 1 (45) | 2 (18), 1 (52), 1(31 and 52) | 1 (45), 1
(33/58) | 0 |
| IVa-g | 0 | 1 (52), 2 (18), 1 (16) | 3 (18), 1 (16), 2 (33/58,52), 1 (16,31), 1 (35) | 4 (18), 1 (16), 1 (52) | 1 (33/58) |
| V-g | 0 | 0 | 0 | 0 | 1 (18), 1 (52,56/59/66) |
There was an association identified between HPV16,
HPV18 and HPV45 with CIN III, AIS, endocervical adenocarcinoma and
squamous cell carcinoma. In addition, other HPV-HR subtypes, such
as HPV 33/58 (>40 years old), as well as 52 (>35 years old),
56/59/66 (>35 years old) were associated with the occurrence of
CIN II and CIN III in the different age groups (Table IV, Table V, Table VI).
Discussion
The current retrospective study based on 210,510
cases included not only dysplastic, premalignant and malignant
endocervical glandular lesions, but also reactive changes of
endocervical glands. In addition, endometrial reactive changes were
included, as well as premalignant and malignant changes of the
endometrium. This was not only to monitor the endometrial changes
in the cases assessed, but also as a control group for endocervical
gland changes, to avoid misinterpretation and overinterpretation,
which have been noticed in previous works as reported by Schnatz
et al (11) and Risse et
al (12) that have described
the dysplastic changes in the endocervical epithelium and atypical
glandular lesions. The present study also included the vaccination
status of individuals against HPV, as until now, to the best of our
knowledge, the importance of vaccination has not been well
understood. Because of the importance of vaccination to protect
women from HPV infection, the study also included the status of
HPV-HR infection. The present study aimed to provide an overview of
the most common HPV subtypes, which were found in the examined age
groups. Finally, histological diagnosis was included in the present
study as a gold standard to compare with and also to control the
cytological findings.
Schnatz et al (11), DeSimone et al (13) and Marques et al (14) previously reported an II-g incidence
(Atypical glandular cells not otherwise specified in Bethesda
classification) of 0.1-2.1% in investigated women. In the present
study, the II-g prevalence ranged from 0.09% (51–60-years age
group) to 0.12% (>35-years age group). A cohort study from
Sweden reported that women with II-g in cervical screening had a
higher risk of cervical carcinoma incidence, particularly
adenocarcinoma, compared with women with high-grade squamous
lesions (15). In the present
study, cytologically, the highest incidence of II-g was in women
<35 years old (0.12%), whereas the highest incidence of V-g
(invasive adenocarcinoma of endocervical epithelium) was in women
>60 years old (0.012%). The highest incidence of cytological
dysplastic changes (III-g) was 0.016% in the 51–60-years age group,
whereas the lowest incidence of III-g was 0.002% in women >60
years old, which may indicate that the dysplastic changes have
reduced with age, whereas the incidence of invasive cervical
adenocarcinoma has increased with age, which may explain the
finding of the previous study (15). The incidence of premalignant
changes (IVa-g), which is equivalent to AIS, was lowest in women
<35 years old (0.003%) but was higher in women in the
35–40-years (0.04%) and 41–50-years (0.02%) age groups.
Furthermore, IVa-g was again lower in women in the 51–60-years
(0.019%) and >60-years (0.004%) age groups, which may suggest
that there are numerous factors that lead to invasive cervical
lesions in the older age groups.
The present study also assessed the vaccination
status of individuals against HPV and HPV-infection status. The
vaccination status against HPV infection was low in all age groups:
<35 years, 0.034%; 35–40 years, 0.004%; 41–50 years, 0.002%;
51–60 years, 0.002%; and >60 years, 0%. The HPV infection status
was lowest in women <35 years old (0.001%; one case out of
63,710 cases), whereas it was higher in the 35–40 and 41–50-years
age groups (0.06 and 0.09% respectively; common subtypes: HPV16,
18, 31, 45, 51, 52, 68,56/59/66, 35/39/68 and 33/58), and
relatively lower in the 51–60-years age group (0.05%) than younger
age groups (<50 years old) and even lower in the >60-years
age group (0.016%), with common HPV-subtypes including HPV 16, 18,
31, 45, 51, 52, 33/58, 35/39/68 and 56/59/66, which may point to
the highest incidence of HPV in ages (<50 years old) associated
with higher sexual activity. The similarity of HPV subtypes between
the younger and older age groups may indicate persistence of some
subtypes of HPV and may indicate the relative risk of developing
cervical cancer in older ages; this partially agrees with the key
findings of Graue et al (6). This previous study stated that there
is a high risk of cervical adenocarcinoma following atypical
glandular changes. The present study may add to this key message
that atypical glandular changes could be associated with HPV
subtypes. Pirog et al (16)
and Holl et al (17)
reported that most cases of cervical adenocarcinoma are related to
persistent infection with oncogenic HPV-HR subtypes. The present
study identified other HPV subtypes than Ronnett et al
(18) and Pirog et al
(16), who documented only HPV16,
18 and 45, and reported that these glandular lesions with HPV
association were common in younger patients <40 years old.
The present study included histopathological
diagnosis as the gold standard and to compare with and control the
cytological findings. In women <35 years, there were seven cases
with III-g, one of which was confirmed as having AIS by biopsy. In
the same age group, there was one case of V-g which was not
associated with HPV infection. In the 35–40-years age group, there
were 28 cases with II-g, one of which was diagnosed with CIN II
with HPV18; three cases with III-g, one of which was diagnosed with
CIN II with HPV45; nine cases with IVa-g, one of which was
diagnosed with AIS with HPV18, another one was diagnosed with CIN
III with HPV16, and two cases were diagnosed as CIN II and CIN III
without HPV infection. These findings indicated that HPV infection
may be an associated infection in some cases, but that it may not
have initiated aetiology in several other cases, which was
consistent with Schiffmann M and de Sanjose (19). In the 41–50-years age group, there
were eight cases with III-g, one of which was diagnosed with CIN II
with HPV52, one with CIN III with HPV31 and 52, one with
endocervical adenocarcinoma with HPV18 and one with AIS without HPV
infection; 10 cases with IVa-g, one of which was diagnosed with CIN
III with HPV18, one with AIS with HPV18, one with AIS with HPV16
and 31, one with CIN III with HPV52 and 33/58, one with CIN III
with HPV35/39/68, one with endocervical adenocarcinoma with HPV16
and one with squamous cell carcinoma with HPV16; and one case with
V-g, which was diagnosed with invasive carcinoma without HPV
infection. These findings provided further evidence of the
association of HPV infection with the lesions, but not necessarily
the initial aetiology. Notably, different HPV subtypes were
associated with the same histological lesions and the same HPV
subtype were associated with different invasive subtypes of
carcinoma. In the 51–60-years age group, there were seven cases
with III-g, one case was diagnosed was squamous cell carcinoma with
HPV45, and two cases with CIN I and CIN II without HPV infection;
eight cases with IVa-g, one case was diagnosed with CIN II with
HPV18, one with AIS with HPV18 and one with AIS with HPV16; and
three cases with IVb-g (equivalent to in situ lesion
suspicious of already present invasive carcinoma in Bethesda
classification), one of which was diagnosed with endocervical
adenocarcinoma with HPV18. In the >60-years age group, there
were two cases with IVa-g, which were diagnosed with CIN I with
HPV33/58 and CIN III without HPV infection; six cases with V-g, two
of which were diagnosed with endocervical adenocarcinoma with
HPV18, 52 and 56/59/66, and one with squamous cell carcinoma
without HPV infection, and another two cases were diagnosed with
endometrial carcinoma without HPV infection. These findings differ
from those of Clifford and Franceschi (20); this previous study stated that
endocervical neoplasia was commonly associated (50–75%) with HPV18
and the remainder of lesions were associated with HPV16 and 45,
whereas these findings agree with the previous study by Abbas et
al (21).
To detect the prevalence of endometrial lesions in
cervical screening and to determine the actual role of HPV
infection in developing cervical lesions, the present study also
included the other cytological groups, II-e, III-e and V-e. In
individuals <35 years old, there were no cases of II-e or V-e;
and there was one case (0.0015%) of III-e, without
histopathological diagnosis or HPV infection. In the 35–40-years
age group, there were no cases of II-e or V-e; and there was one
case (0.004%) of III-e, without HPV infection and diagnosed without
dysplasia. In the 41–50-years age group, there were 534 (1.54%)
cases of II-e without histopathological diagnosis, with HPV
infection in 17 cases (16, 18, 31, 52, 56/59/66, 51, 33/58 and
35/39/68); 23 cases (0.066%) of III-e, one of which was diagnosed
with squamous cell carcinoma and HPV16, and 22 without dysplasia;
and no cases of V-e. In the 51–60-years age group, there were 302
(0.73%) cases of II-e, 10 cases of which had HPV infection
(35/39/68, 56/59/66, 31, 45, 18 and 51) without histopathological
biopsy; 59 cases (0.14%) of III-e, all of them without HPV
infection, one of which was diagnosed as endocervical
adenocarcinoma and seven with endometrial carcinoma; and four cases
(0.009%) of V-e, only one of which had HPV16 and was diagnosed with
squamous cell carcinoma, two of which were diagnosed with
endometrial carcinoma and one without dysplasia. In the
>60-years age group, there were 78 cases (0.16%) of II-e, two of
which were diagnosed with endometrial carcinoma and two with HPV16
and 35/39/68, but without histopathological biopsy; 61 cases
(0.125%) of III-e, one of which had HPV16 and was without
dysplasia, 15 were diagnosed with endometrial carcinoma and without
HPV-infection, and three were diagnosed with endocervical
adenocarcinoma without HPV infection; and eight cases (0.0164%) of
V-e, one of which had HPV35/39/68 and without dysplasia, and two
were diagnosed with endometrial carcinoma. These findings indicated
that there may be no relationship between HPV infection and
endometrial lesions, but that endocervical lesions may be
misdiagnosed under endometrial lesions as previously reported by
Schnatz et al (11).
Notably, endocervical carcinoma can occur without HPV infection and
HPV infection does not mean that there should necessarily be
cervical epithelial changes.
In conclusion, endocervical glandular dysplastic
changes usually occur in younger individuals aged between 35 and 60
years old, and may or may not be associated with HPV infection.
Furthermore, endocervical adenocarcinoma can occur at any age in
individuals with or without HPV infection. Squamous cell changes
and endometrial lesions can be misdiagnosed as endocervical lesions
in cervical screening; therefore, a histopathological investigation
should follow in highly suspicious cases. The association of
cytological screening and HPV genotyping is a predictive method in
cases of risk for developing dysplastic, premalignant and malignant
glandular lesions. The combination of both cytological examination
and HPV genotyping is also important to detect HPV-negative
adenocarcinoma, AIS from gastral type with negativity for HPV and
non-cervical adenocarcinoma (metastasis/infiltration). Vaccination
against HPV infection should be performed to protect women against
dangerous subtypes. One of the limitations of the present study is
the lack of follow-up data for these cases; however, we aim to
rectify this in future.
Acknowledgements
Many thanks to Mrs. Petra Abbas for
proofreading.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analysed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MA developed the idea of the work and study design,
interpreted the results, drafted the manuscript and provided final
approval. OB collected data and interpreted the results. JDJ
interpreted the results and was involved in analysis of figures. MA
and OB confirm the authenticity of all the raw data. All authors
have read and approved the final manuscript.
Ethics approval and consent to
participate
The approval was granted by the Ethics Committee of
the Medical Association (Hannover, Germany). Informed consent for
inclusion in the study was waived, as patient records were
anonymized and retrospectively analysed. The samples were
anonymized to ensure data protection.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Arbyn M, Weiderpass E, Bruni L, de Sanjosé
S, Saraiya M, Ferlay J and Bray F: Estimates of incidence and
mortality of cervical cancer in 2018: A worldwide analysis. Lancet
Glob Health. 8:e191–e203. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sopracordevole F, Clemente N, Alessandrini
L, Di Giuseppe J, Cigolot F, Buttignol M, Ciavattini A and
Canzonieri V: Detection of occult endocervical glandular dysplasia
in cervical conization specimens for squamous lesions. Pathol Res
Pract. 213:210–216. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Teoh D, Musa F, Salani R, Huh W and
Jimenez E: Diagnosis and management of adenocarcinoma in situ: A
society of gynecologic oncology evidence-based review and
recommendations. Obstet Gynecol. 135:869–878. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Engineer AD and Misra JS: The role of
routine outpatient cytological screening for early detection of
carcinoma of the cervix in India. Diagn Cytopathol. 3:30–34. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ranabhat SK, Shrestha R and Tiwari M:
Analysis of abnormal epithelial lesions in cervical Pap smears in
Mid-Western Nepal. J Pathol Nepal. 1:30–33. 2011. View Article : Google Scholar
|
|
6
|
Graue R, Lönnberg S, Skare GB, Saether SMM
and Bjørge T: Atypical glandular lesions of the cervix and risk of
cervical cancer. Acta Obstet Gynecol Scand. 99:582–590. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Marquardt K, Schenk U and Griesser H:
Muenchen classification for gynaecological cytological diagnoses.
Verband deutscher cytologisch tätiger Assistenten e.V., Langen.
2014.(In German).
|
|
8
|
Griesser H, Marquardt K, Jordan B, Kühn W,
Neis K, Neumann HH, Bollmann R, Pöschel B, Steiner PM and Schenck
U: Münchner nomenklatur III. Frauenarzt. 11:2–7. 2013.
|
|
9
|
Deutsche Krebsgesellschaft, Deutsche
Krebshilfe, AWMF, . S3-Leitlinie Prävention des Zervixkarzinoms.
Langversion 1.0-Dezember 2017. AWMF-Registernummer 015/027OL.
https://www.awmf.org/uploads/tx_szleitlinien/015-027OLl_Praevention_Zervixkarzinom_2018-01.pdf9–January.
2019
|
|
10
|
Hillemanns P: Krebsfrüherkennung:
Zervixkarzinom-doppelter paradigmenwechsel. Dtsch Arztebl.
113:A282–A285. 2016.
|
|
11
|
Schnatz PF, Guile M, O'Sullivan DM and
Sorosky JI: Clinical significance of atypical glandular cells on
cervical cytology. Obstet Gynecol. 107:701–708. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Risse EK, Ouwerkerk-Noordam E and Boon ME:
Endometrial cells in liquid-based cervical cytology: A diagnostic
pitfall solved by preparing cytohistology from the residual thin
layer sample. Acta Cytol. 55:327–333. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
DeSimone CP, Day ME, Tovar MM, Dietrich CS
III, Eastham ML and Modesitt SC: Rate of pathology from atypical
glandular cell Pap tests classified by the Bethesda 2001
nomenclature. Obstet Gynecol. 107:1285–1291. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Marques JP, Costa LB, Pinto AP, Lima AF,
Duarte ME, Barbosa AP and Medeiros PL: Atypical glandular cells and
cervical cancer: Systematic review. Rev Assoc Med Bras (1992).
57:234–238. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang J, Andrae B, Sundström K, Ström P,
Ploner A, Elfström KM, Arnheim-Dahlström L, Dillner J and Sparén P:
Risk of invasive cervical cancer after atypical glandular cells in
cervical screening: Nationwide cohort study. BMJ. 352:i2762016.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Pirog EC, Lloveras B, Molijn A, Tous S,
Guimerà N, Alejo M, Clavero O, Klaustermeier J, Jenkins D, Quint
WG, et al: HPV prevalence and genotypes in different histological
subtypes of cervical adenocarcinoma, a worldwide analysis of 760
cases. Mod Pathol. 27:1559–1567. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Holl K, Nowakowski AM, Powell N,
McCluggage WG, Pirog EC, Collas De Souza S, Tjalma WA, Rosenlund M,
Fiander A, Castro Sánchez M, et al: Human papillomavirus prevalence
and type-distribution in cervical glandular neoplasias: Results
from a European multinational epidemiological study. Int J Cancer.
137:2858–2868. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ronnett BM, Manos MM, Ransley JE,
Fetterman BJ, Kinney WK, Hurley LB, Ngai JS, Kurman RJ and Sherman
ME: Atypical glandular cells of undetermined significance (AGUS):
Cytopathologic features, histopathologic results, and human
papillomavirus DNA detection. Hum Pathol. 30:816–825. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Schiffmann M and de Sanjose S: False
positive cervical HPV screening test results. Papillomavirus Res.
7:184–187. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Clifford G and Franceschi S: Members of
the human papillomavirus type 18 family (alpha-7 species) share a
common association with adenocarcinoma of the cervix. Int J Cancer.
122:1684–1685. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Abbas M, de Jonge J and Bettendorf O:
HPV-genotyping versus conventional cervical cytology as a screening
method to detect dysplastic cervical epithelial changes. Sci Rep.
12:178282022. View Article : Google Scholar : PubMed/NCBI
|