Introduction
Radiotherapy is one of the standard treatment
methods for patients with early laryngeal carcinoma, although laser
therapy and partial laryngectomy can be used for definitive
treatment as well (1–3). The goal of treatment is not only to
cure cancer, but also to keep the vocal cords with acceptable voice
quality, and avoid major treatment-related adverse events (AEs).
These goals can be achieved with definitive radiotherapy in most
patients with early laryngeal carcinoma. Laryngeal carcinoma is
classified in supraglottic, glottic, and subglottic types based on
the location, and glottic carcinomas are the most common type
(70%). Additionally, most glottic carcinomas are diagnosed in its
early stage, accounting for approximately 70% of all cases.
Irradiation for early glottic carcinoma is delivered through small
radiation portals covering the glottic tumor because the lymph node
metastasis in neck is rare. Therefore, AEs are considered mild
after radiotherapy for early glottic carcinoma. Nevertheless,
serious AEs, including hypothyroidism, may occur after definitive
radiotherapy in rare cases of early glottic carcinoma.
Hypothyroidism can be divided into two categories:
clinical and subclinical hypothyroidism. Clinical hypothyroidism is
a condition of a high thyroid-stimulating hormone (TSH) level in
the presence of a free thyroxine (FT4) level lower than the normal
range, whereas subclinical hypothyroidism is a condition of a high
TSH level in the presence of an FT4 level within the normal range.
The fatigue, drowsiness, intolerance of cold, weight gain,
constipation, aural changes, and dry skin are common clinical
symptoms of hypothyroidism (4).
Patients with mild hypothyroidism may have no obvious symptoms, but
severe hypothyroidism may increase the incidence of cardiovascular
disease and risk of death, including heart failure, atrial
fibrillation, and coronary artery disease (5–7).
In our previous study (8), we identified the risk factor for
local failure in T1 glottic carcinoma irradiated at the prescribed
66 Gy. However, this study was insufficient to investigate AEs, and
risk factors for radiation-related hypothyroidism were unclear.
Numerous researchers have examined factors associated with
hypothyroidism in patients with head and neck cancers who receive
whole-neck radiotherapy. Clinical and demographic factors such as
dose-volume parameters (9–11), chemotherapy (12–14),
neck surgery (15,16), sex (12,13,17),
age (12,18), and follow-up duration (19) are considered risk factors for
radiation-induced hypothyroidism. However, no study to date has
examined the risk factors for hypothyroidism specifically after
definitive radiotherapy in patients with early glottic carcinoma.
We therefore conducted a retrospective study to investigate the
risk factors associated with hypothyroidism after definitive
radiotherapy in patients with early glottic carcinoma given that
the knowledge of these factors is important to improve the safety
of radiotherapy in these patients.
Materials and methods
Patients
A total of 109 consecutive patients with T1 or T2,
N0 glottic squamous cell carcinoma were irradiated definitively
without concurrent chemotherapy between June 3, 2009 and December
25, 2020 in the study institution. This retrospective study
included patients who were evaluated for thyroid function and
followed for a minimum of 6 months after radiotherapy. Therefore,
73 of the 109 patients were included in this study. All patients
provided written informed consent, and the study was approved by
the Institutional Review Board of Tokyo Medical University Hospital
(approval no. T2021-0260).
Cancer stage was classified according to the 2016
TNM classification (8th edition, Union for International Cancer
Control). This study cohort included 62 male and 11 female
patients, and the median age of patient was 72 (range, 47–86)
years. The Eastern Cooperative Oncology Group performance status
was 0 in 98% of the patients. The cancer stages were T1N0M0 and
T2N0M0 in 53 and 20 patients, respectively, and no patients had
neck or distant metastases. In the study cohort, 16 patients (22%)
had two primary cancers and 3 patients (4%) had three primary
cancers.
Radiation treatment
Three-dimensional radiotherapy was planned and
performed on patients in the supine position using a shell. As part
of the treatment planning, all patients underwent cervical computed
tomography (CT) imaging with 2.5-mm slice thickness. Treatment
planning was performed using the Eclipse™ treatment planning system
(Varian Medical Systems, Palo Alto, CA). In all patients, the
standard radiotherapy technique with parallel-opposed lateral
fields was used to deliver the photons of a 4-MV X-ray beam for 5
days per week. Irradiation was delivered via local radiation
portals, mostly those sized 5–6×5–6 cm, which covered only the
glottic tumor. The cervical lymph node chain was not included in
the treatment plan. The dose was 66 Gy administered in 33 fractions
over 6.6 weeks in patients with T1 glottic carcinoma and 70 Gy
administered in 35 fractions over 7 weeks in patients with T2
glottic carcinoma. The patient characteristics and radiotherapy
details are summarized in Table
I.
 | Table I.Characteristics of the patients (n=73)
and radiation treatment. |
Table I.
Characteristics of the patients (n=73)
and radiation treatment.
| Variables | Value |
|---|
| Sex, n (%) |
|
| Male | 62 (85) |
|
Female | 11 (15) |
| Median age, years
(range) | 72 (47–86) |
| Performance status,
n |
|
| 0 | 72 |
| 1 | 1 |
| Stage of primary
tumors, n (%) |
|
| T1 | 53 (73) |
| T2 | 20 (27) |
| Total
dose/fractionation, n (%) |
|
| 66 Gy/33
Fr | 60 (82) |
| 70 Gy/35
Fr | 13 (18) |
| Field size, n
(%) |
|
| <6
cm | 36 (50) |
| ≥6
cm | 37 (50) |
Follow-up procedures
Patients were followed up regularly at 2- to 3-month
intervals for the first 2 years after diagnosis and 4- to 6-month
intervals thereafter in patients without clinical symptoms. At each
follow-up visit, the medical history, physical examination,
laryngoscopy, CT scans, and tumor marker assessment were evaluated.
Data on radiotoxicity were retrospectively collected from the
patient files. Hypothyroidism was defined as the presence of a high
TSH level regardless of the FT4 level and was graded as follows
according to the Common Terminology Criteria for Adverse Events v.
4.0: grade 1, asymptomatic hypothyroidism requiring clinical or
diagnostic observation only; grade 2, symptomatic hypothyroidism
requiring medical intervention; grade 3, severely symptomatic
hypothyroidism requiring hospitalization; grade 4, life-threatening
consequences of hypothyroidism requiring urgent intervention; and
grade 5, death.
Assessment of risk factors for
hypothyroidism
Age, sex, Tumor stage (T) stage, and pretreatment
thyroid volume were evaluated as clinical risk factors for
hypothyroidism. Pretreatment thyroid volumes were determined using
CT scans obtained during treatment planning for radiotherapy. Field
size, total prescribed dose, and thyroid receiving dose were
evaluated as dosimetric risk factors for hypothyroidism. Underlying
irradiated thyroid volumes of more than 5, 10, 20, 30, 40, 50, 60,
and 65 Gy (V5Gy, V10Gy, V20Gy, V30Gy, V40Gy, V50Gy, V60Gy, and
V65Gy, respectively) and mean thyroid dose were calculated as
thyroid receiving doses.
Statistical analysis
The time to hypothyroidism onset after definitive
radiotherapy was calculated from the first day of radiotherapy. The
relationship of hypothyroidism with age, sex, T stage, field size,
and total prescribed dose was calculated using Fisher's exact
probability test. The relationship of hypothyroidism with
pretreatment thyroid volume, V5Gy, V10Gy, V20Gy, V30Gy, V40Gy,
V50Gy, V60Gy, V65Gy, and mean thyroid dose were analyzed using the
Mann-Whitney U test. For these factors, the receiving operating
characteristic (ROC) curves were generated to determine the cutoff
values that yielded the optimal sensitivity and specificity.
Univariate logistic regression analyses were performed to evaluate
the data using IBM SPSS Statistics 20.0 (SPSS, Armonk, NY, USA).
Differences with P-values of <0.05 were considered indicating
statistical significance.
Results
Incidence of hypothyroidism
The median follow-up duration was 61 (range, 7–150)
months. Hypothyroidism was present in 15 (21%) of the 73 patients
and were classified as grades 1 and 2 in 12 and 3 patients,
respectively. The median time to hypothyroidism onset after the
start of definitive radiotherapy was 16 (range, 3–77) months.
Hypothyroidism improved in 6 of the 15 patients in a median of 13
(range, 5–24) months.
Analysis for the demographic and
clinical factors with hypothyroidism
The relationships of the demographic and clinical
factors with hypothyroidism are summarized in Table II. Briefly, sex and pretreatment
thyroid volume were significantly associated with hypothyroidism
(P=0.007 and <0.001, respectively). The incidence rates of
hypothyroidism were 15 and 55% in male and female patients,
respectively, and the incidence of hypothyroidism was 3.67 times
higher in female patients than in male patients. The median
pretreatment thyroid volumes were 12.3 (range, 4.9-62.8) and 7.0
(4.0-32.5) ml in male and female patients, respectively. The
pretreatment thyroid volume was significantly lower in female
patients than in male patients (P=0.035). The ROC analysis for
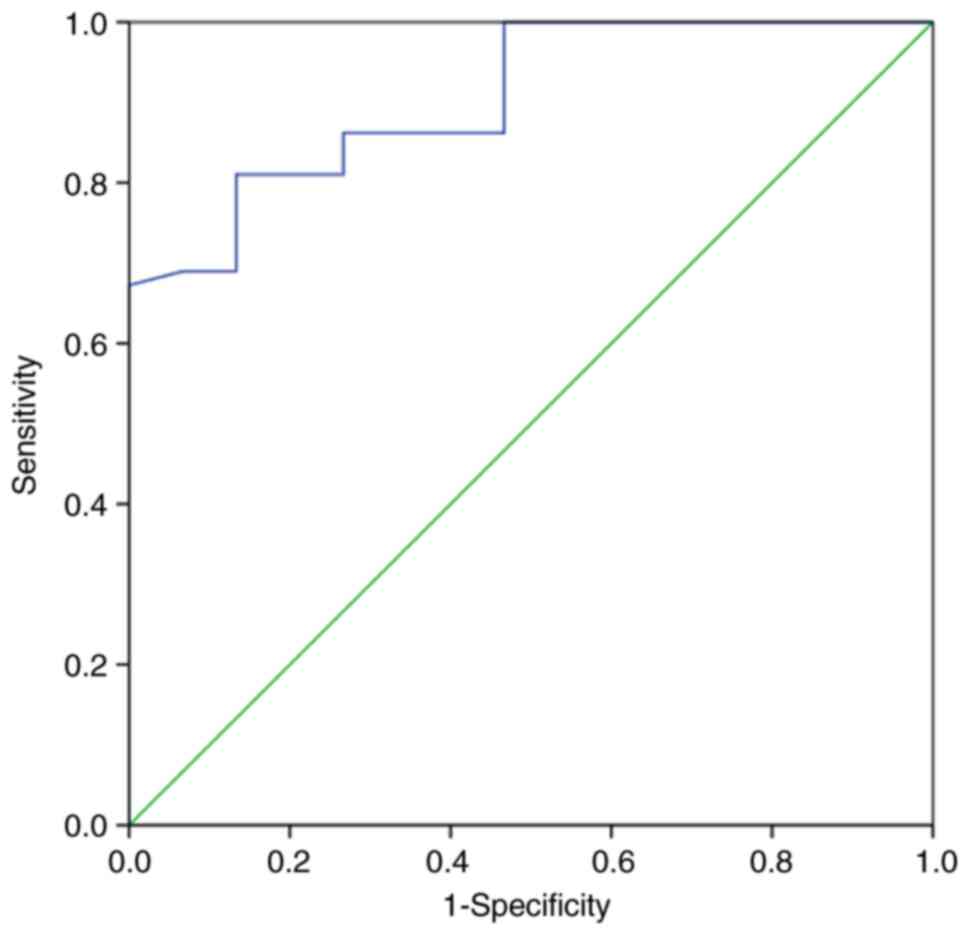
hypothyroidism showed that the area under the ROC curve (AUC) for
pretreatment thyroid volume was 0.905 [95% confidence interval
(CI), 0.833-0.978] (Fig. 1). The
cutoff value of pretreatment thyroid volume was 9.50 ml, with a
sensitivity of 81.0% and a specificity of 86.7%. The incidence
rates of hypothyroidism were 54 and 4.1% for patients with
pretreatment thyroid volumes of <9.50 and ≥9.50 ml,
respectively. The incidence of hypothyroidism was 13.2 times higher
in patients with a pretreatment thyroid volume of <9.50 ml than
in those with a pretreatment thyroid volume of ≥9.50 ml.
 | Table II.Clinical risk factors associated with
hypothyroidism. |
Table II.
Clinical risk factors associated with
hypothyroidism.
| Variables | Without
hypothyroidism (n=58) | With hypothyroidism
(n=15) | P-value |
|---|
| Sex (male vs.
female) | 53 vs. 5 | 9 vs. 6 | 0.007 |
| Age (<75 vs. ≥75
years) | 38 vs. 20 | 7 vs. 8 | 0.149 |
| T stage (T1 vs.
T2) | 42 vs. 16 | 11 vs. 4 | 0.610 |
| Pretreatment thyroid
volume, ml [median (mean ± SD)] | 13.5 (14.7±8.3) | 6.7 (7.4±2.2) | <0.001 |
Analysis for the dosimetric factors
with hypothyroidism
Table III shows
the relationship of hypothyroidism with dosimetric factors in the
study cohort. The univariate analysis revealed that hypothyroidism
was significantly associated with V5Gy (P=0.012), V10Gy (P=0.015),
V20Gy (P=0.020), V30Gy (P=0.024), V40Gy (P=0.028), V50Gy (P=0.028),
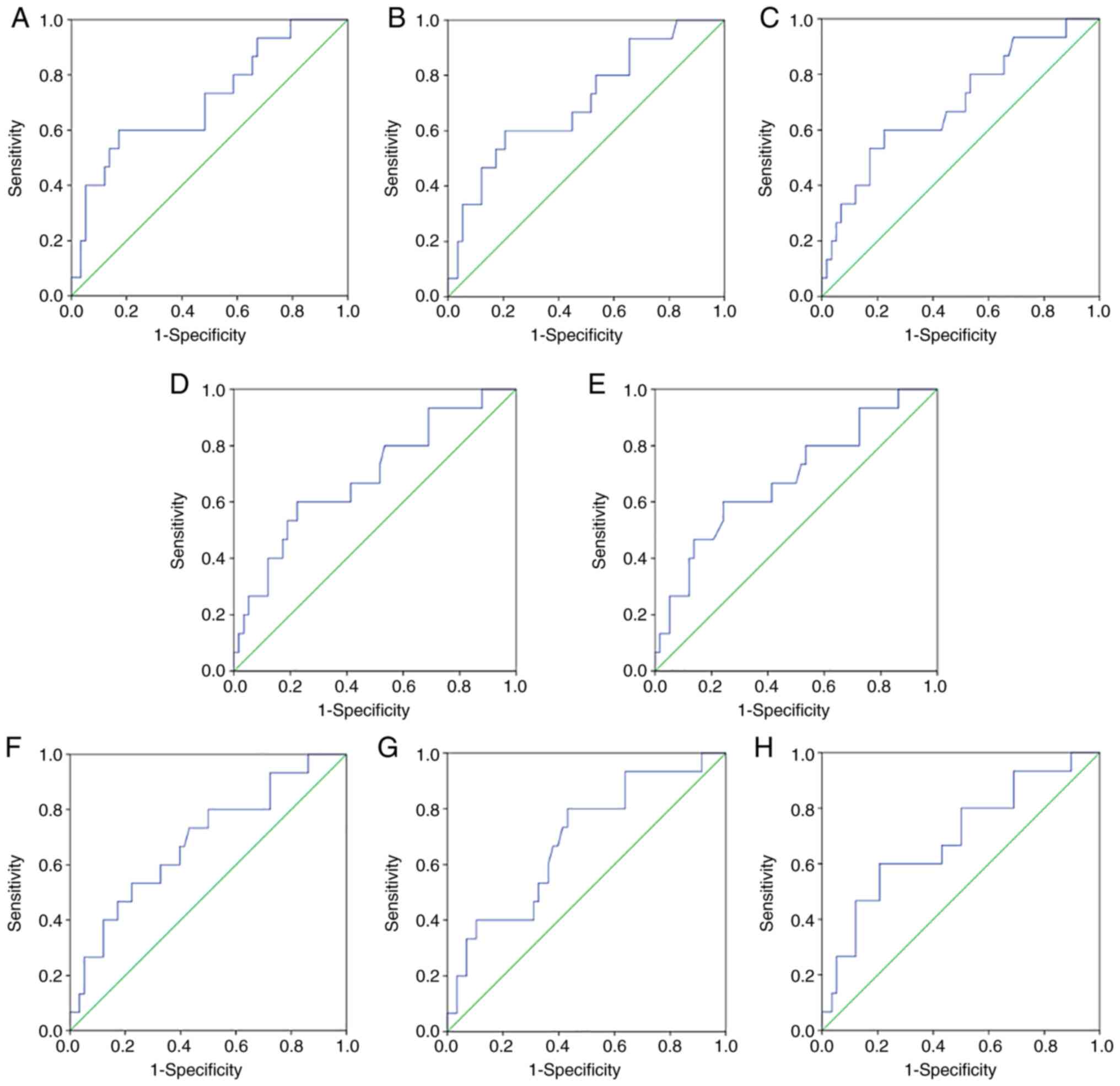
V60Gy (P=0.027), and mean thyroid dose (P=0.023). The ROC analysis
revealed that that the AUCs for V5Gy, V10Gy, V20Gy, V30Gy, V40Gy,
V50Gy, V60Gy, and mean thyroid dose were 0.711 (95% CI,
0.558-0.865), 0.705 (0.554-0.857), 0.695 (0.541-0.850), 0.690
(0.535-0.845), 0.684 (0.528-0.841), 0.684 (0.531-0.838), 0.686
(0.536-0.846), and 0.692 (0.537-0.847), respectively (Fig. 2). V5Gy had the highest AUC value
among all factors related to the thyroid receiving dose. The cutoff
value of V5Gy was 45.6%, with a sensitivity of 73.3% and a
specificity of 51.3%.
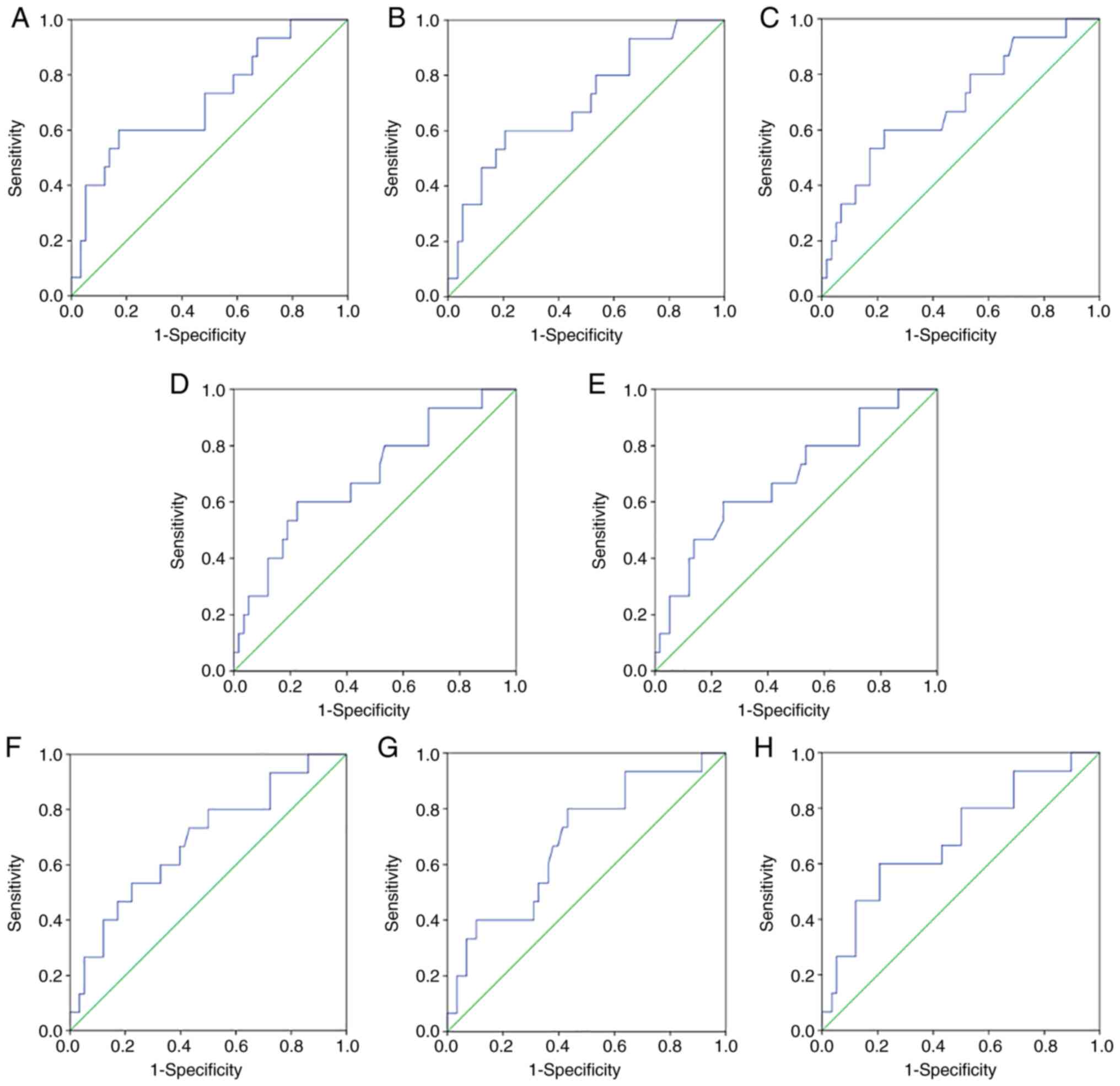 | Figure 2.Receiver operating characteristic
analysis of the thyroid receiving doses associated with the
development of hypothyroidism after radiotherapy for early glottic
carcinoma. The AUCs for V5Gy, V10Gy, V20Gy, V30Gy, V40Gy, V50Gy,
V60Gy and V65Gy are shown. (A) V5Gy, 0.711 (95% CI, 0.558-0.865);
(B) V10Gy, 0.705 (95% CI, 0.554-0.857); (C) V20Gy, 0.695 (95% CI,
0.541-0.850); (D) V30Gy, 0.690 (95% CI, 0.535-0.845); (E) V40Gy,
0.684 (95% CI, 0.528-0.841); (F) V50Gy, 0.684 (95% CI,
0.531-0.838); (G) V60Gy, 0.686 (95% CI, 0.536-0.846); and (H) mean
thyroid dose, 0.692 (95% CI, 0.537-0.847). The AUC value was the
highest for V5Gy. The cutoff value of V5Gy was 44.8%, with a
sensitivity of 73.3% and a specificity of 50.0%. AUC, area under
the receiver operating characteristic curve. Vx Gy, irradiated
underlying thyroid volumes of more than × Gy. |
 | Table III.Association between dosimetric factors
and hypothyroidism. |
Table III.
Association between dosimetric factors
and hypothyroidism.
| Variables | Without
hypothyroidism (n=58) | With hypothyroidism
(n=15) | P-value |
|---|
| Field size (<6 vs.
≥6 cm) | 28 vs. 30 | 8 vs. 7 | 0.476 |
| Total prescribed dose
(66 vs. 70 Gy) | 48 vs. 10 | 12 vs. 3 | 0.531 |
| V 5Gy, % [median
(mean ± SD)] | 44.9 (45.2±18.3) | 65.7 (62.0±22.5) | 0.012 |
| V10 Gy, % [median
(mean ± SD)] | 38.6 (38.3±17.3) | 53.5 (54.5±23.1) | 0.015 |
| V20 Gy, % [median
(mean ± SD)] | 32.8 (33.0±16.4) | 47.0 (48.5±23.2) | 0.020 |
| V30 Gy, % [median
(mean ± SD)] | 28.7
(29.4±15.7) | 41.5
(44.2±23.1) | 0.024 |
| V40 Gy, % [median
(mean ± SD)] | 25.3
(26.1±15.1) | 36.0
(40.1±22.9) | 0.028 |
| V50 Gy, % [median
(mean ± SD)] | 19.8
(22.4±14.2) | 31.3
(35.4±22.6) | 0.028 |
| V60 Gy, % [median
(mean ± SD)] | 11.6
(16.1±12.9) | 19.8
(27.2±20.9) | 0.027 |
| V65 Gy, % [median
(mean ± SD)] | 1.8 (7.4±10.6) | 9.2
(11.2±11.9) | 0.304 |
| Mean thyroid dose,
Gy [median (mean ± SD)] | 19.0
(20.3±9.9) | 27.6
(29.2±13.9) | 0.023 |
Discussion
In the present study, hypothyroidism was present in
15 (21%) of the 73 patients with early glottic carcinoma, including
12 and 3 patients with grade 1 and 2 hypothyroidism, respectively.
Our analyses revealed that sex, pretreatment thyroid volume, V5Gy,
V10Gy, V20Gy, V30Gy, V40Gy, V50Gy, V60Gy, and mean thyroid dose
were significantly associated with hypothyroidism. Several studies
reported the risk factors of radiation-induced hypothyroidism in
patients with head and neck cancers (9–23).
The reported incidence of hypothyroidism after definitive
radiotherapy in the neck varies between 23 and 53% (20). In the present study, hypothyroidism
developed in 21% of the patients, in agreement with the previous
studies. Although numerous groups investigated factors related to
radiation-induced hypothyroidism in patients undergoing whole-neck
radiotherapy for head and neck cancers, such as nasopharyngeal,
oral, and hypopharyngeal cancers, to our knowledge this is the
first study examining the risk factors for hypothyroidism after
definitive radiotherapy in patients with early glottic carcinoma,
because small radiation portals are used to cover only the primary
tumor and the cervical lymph node chain is not included in the
treatment plan.
We found that sex and pretreatment thyroid volume
were significantly associated with hypothyroidism in patients with
early glottic carcinoma receiving definitive radiotherapy. Fan
et al (12) found that the
incidence of hypothyroidism was 2.0 times higher in female patients
than in male patients. Rønjom et al (24) found that the median thyroid volume
of female patients was significantly lower than that of male
patients (13.4 vs. 18.4 cm3, P<0.001).
Lertbutsayanukul et al (11) conducted a prospective analysis of
178 patients and reported that a small thyroid volume (<8
cm3) was a risk factor for hypothyroidism based on
univariate analysis, similar to the findings of a study by Zhai
et al (21), who reported
that younger age, female sex, and a smaller thyroid volume were
significantly associated with hypothyroidism. Although the
relationship between sex and thyroid volume remains to be further
elucidated, many studies reveal that female patients are more
likely to develop hypothyroidism (22). In the present study, we also found
that the pretreatment thyroid volume was significantly lower in
female patients than in male patients. We suggest that female
patients may be at higher risk for hypothyroidism because of a
significantly lower thyroid volume compared with male patients.
Our analyses indicated that V5Gy, V10Gy, V20Gy,
V30Gy, V40Gy, V50Gy, V60Gy, and mean thyroid dose were
significantly associated with hypothyroidism after definitive
radiotherapy in patients with early glottic carcinoma. Several
studies elucidated the association between thyroid dose and
hypothyroidism in patients with head and neck cancers who were
treated with radiotherapy. Sachdev et al (23) reported that V50Gy ≥60% was
associated with 6.76 times increased risk of clinical
hypothyroidism compared with V50Gy <60%. In a prospective
analysis of 135 patients by Zhai et al (21), the univariate analysis indicated
that the thyroid mean dose, the minimum dose V30Gy, V35Gy, V40Gy,
V45Gy, and V50Gy of the thyroid gland were associated with
hypothyroidism and that Dmean, V45Gy, and V50Gy were independent
predictors of hypothyroidism after radiotherapy. Altogether, these
studies implicate thyroid receiving dose as a risk factor for
hypothyroidism in patients with head and neck cancers requiring
whole-neck irradiation. In the present study, low dose areas for
thyroid, such as V5 Gy, were factors in hypothyroidism. These
thyroid doses are lower than the doses in the previous studies. We
consider that this is because the large irradiation field such as
whole-neck radiotherapy in the previous studies resulted in almost
100% of the low-dose area for thyroid, such as V5Gy, and therefore
there was no difference in the low-dose area in each patient. In
addition, other thyroid doses that may be factors in hypothyroidism
could be found if analyzed using continuous values or values below
V5Gy. However, this would increase the volume of data, complicate
statistical evaluation, and reduce reliability. Furthermore, V5Gy
is clinically small enough in prescribed doses of 66–70 Gy, and
evaluation of doses lower than this may not be necessary. In this
study, all patients were treated with three-dimensional
radiotherapy. Although it is difficult to reduce the thyroid dose
with treatment using three-dimensional radiotherapy, it may be
possible to reduce the thyroid dose with treatment using Intensity
Modulated Radiation Therapy (IMRT) technique. If the thyroid dose
cannot be reduced, it is important to explain to the patient the
risk of developing hypothyroidism.
In the present study, there were fewer female than
male. All studies should be conducted according to the Sex and
Gender Equity in Research (SAGER) guidelines (25). However, the incidence of laryngeal
carcinoma is 5 times higher in male than in female (26), and is overwhelmingly more common in
male, which inevitably results in fewer female. In addition, it is
impossible to adjust for the sex ratio due to the nature of the
retrospective study. Importantly, this is the first study to
identify that thyroid receiving dose was associated with
hypothyroidism even in patients with early glottic carcinoma after
definitive radiotherapy, which is delivered using small portals
covering only the primary tumor.
A limitation of the present study is the potential
selection bias regarding predictive factors, which cannot be ruled
out because of the retrospective study design. In addition, due to
the nature of the retrospective study, it is possible that some
patients may not have regular follow-up. Future prospective studies
are warranted to confirm the main study findings.
In conclusion, sex, pretreatment thyroid volume,
V5Gy, V10Gy, V20Gy, V30Gy, V40Gy, V50Gy, V60Gy, and mean thyroid
dose were significantly associated with hypothyroidism after
definitive radiotherapy in patients with early glottic carcinoma.
These findings indicate that caution should be exercised regarding
hypothyroidism, which can develop even in patients with early
glottic carcinoma who receive definitive radiotherapy through small
portals covering only the primary tumor. Particularly, the
receiving dose to the thyroid gland should be reduced in female
patients and in those with small thyroid volumes who are at higher
risk of hypothyroidism.
Acknowledgements
The authors would like to thank radiological
technologist Mr. Hideaki Chiba (Department of Radiology, Tokyo
Medical University Hospital, Tokyo, Japan) and Dr Yu Tajima
(Department of Radiology, Tokyo Medical University Hospital, Tokyo,
Japan) for their statistical analysis assistance.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MO, TI, TS and DY conceived the study, and wrote and
revised the manuscript. RM, YO, SS and TK reviewed, collected and
analyzed the data. KT and KS designed the study and acquired the
data. All authors contributed to the writing of the manuscript. MO
and TI confirmed the authenticity of all the raw data, and
participated in writing and editing. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
The study was approved by Tokyo Medical University,
Institutional Review Board (approval no. T2021-0260; Tokyo, Japan).
All patients provided written informed consent to participate.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mendenhall WM, Werning JW, Hinerman RW,
Amdur RJ and Villaret DB: Management of T1-T2 glottic carcinomas.
Cancer. 100:1786–1792. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Beitler JJ and Johnson JT: Transoral laser
excision for early glottic cancer. Int J Radiat Oncol Biol Phys.
56:1063–1066. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Back G and Sood S: The management of early
laryngeal cancer: Options for patients and therapists. Curr Opin
Otolaryngol Head Neck Surg. 13:85–91. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Carlé A, Pedersen IB, Knudsen N, Perrild
H, Ovesen L and Laurberg P: Gender differences in symptoms of
hypothyroidism: A population-based DanThyr study. Clin Endocrinol
(Oxf). 83:717–725. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Floriani C, Gencer B, Collet TH and
Rodondi N: Subclinical thyroid dysfunction and cardiovascular
diseases: 2016 Update. Eur Heart J. 39:503–507. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Biondi B, Cappola AR and Cooper DS:
Subclinical hypothyroidism: A review. JAMA. 322:153–160. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rodondi N, den Elzen WP, Bauer DC, Cappola
AR, Razvi S, Walsh JP, Asvold BO, Iervasi G, Imaizumi M, Collet TH,
et al: Subclinical hypothyroidism and the risk of coronary heart
disease and mortality. JAMA. 304:1365–1374. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Okubo M, Itonaga T, Saito T, Shiraishi S,
Mikami R, Sakurada A, Sugahara S, Park J, Tokuuye K and Saito K:
Predictive factors for local control of early glottic squamous cell
carcinomas after definitive radiotherapy. Mol Clin Oncol.
12:541–550. 2020.PubMed/NCBI
|
|
9
|
Sommat K, Ong WS, Hussain A, Soong YL, Tan
T, Wee J and Fong KW: Thyroid V40 predicts primary hypothyroidism
after intensity modulated radiation therapy for nasopharyngeal
carcinoma. Int J Radiat Oncol Biol Phys. 98:574–580. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lee V, Chan SY, Choi CW, Kwong D, Lam KO,
Tong CC, Sze CK, Ng S, Leung TW and Lee A: Dosimetric predictors of
hypothyroidism after radical intensity-modulated radiation therapy
for non-metastatic nasopharyngeal carcinoma. Clin Oncol (R Coll
Radiol). 28:e52–e60. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lertbutsayanukul C, Kitpanit S, Prayongrat
A, Kannarunimit D, Netsawang B and Chakkabat C: Validation of
previously reported predictors for radiation-induced hypothyroidism
in nasopharyngeal cancer patients treated with intensity-modulated
radiation therapy, a post hoc analysis from a phase III randomized
trial. J Radiat Res. 59:446–455. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fan CY, Lin CS, Chao HL, Huang WY, Su YF,
Lin KT, Tsai IJ and Kao CH: Risk of hypothyroidism among patients
with nasopharyngeal carcinoma treated with radiation therapy: A
population-based cohort study. Radiother Oncol. 123:394–400. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Luo R, Li M, Yang Z, Zhan Y, Huang B, Lu
J, Xu Z and Lin Z: Nomogram for radiation-induced hypothyroidism
prediction in nasopharyngeal carcinoma after treatment. Br J
Radiol. 90:201606862017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sunwoo JB, Herscher LL, Kroog GS, Thomas
GR, Ondrey FG, Duffey DC, Solomon BI, Boss C, Albert PS, McCullugh
L, et al: Concurrent paclitaxel and radiation in the treatment of
locally advanced head and neck cancer. J Clin Oncol. 19:800–811.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tell R, Lundell G, Nilsson B, Sjödin H,
Lewin F and Lewensohn R: Long-term incidence of hypothyroidism
after radiotherapy in patients with head-and-neck cancer. Int J
Radiat Oncol Biol Phys. 60:395–400. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tell R, Sjödin H, Lundell G, Lewin F and
Lewensohn R: Hypothyroidism after external radiotherapy for head
and neck cancer. Int J Radiat Oncol Biol Phys. 39:303–308. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ling S, Bhatt AD, Brown NV, Nguyen P,
Sipos JA, Chakravarti A and Rong Y: Correlative study of dose to
thyroid and incidence of subsequent dysfunction after head and neck
radiation. Head Neck. 39:548–554. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Diaz R, Jaboin JJ, Morales-Paliza M,
Koehler E, Phillips JG, Stinson S, Gilbert J, Chung CH, Murphy BA,
Yarbrough WG, et al: Hypothyroidism as a consequence of
intensity-modulated radiotherapy with concurrent taxane-based
chemotherapy for locally advanced head-and-neck cancer. Int J
Radiat Oncol Biol Phys. 77:468–476. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Grande C: Hypothyroidism following
radiotherapy for head and neck cancer: Multivariate analysis of
risk factors. Radiother Oncol. 25:31–36. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Boomsma MJ, Bijl HP and Langendijk JA:
Radiation-induced hypothyroidism in head and neck cancer patients:
A systematic review. Radiother Oncol. 99:1–5. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhai RP, Kong FF, Du CR, Hu CS and Ying
HM: Radiation-induced hypothyroidism after IMRT for nasopharyngeal
carcinoma: Clinical and dosimetric predictors in a prospective
cohort study. Oral Oncol. 68:44–49. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Vogelius IR, Bentzen SM, Maraldo MV,
Petersen PM and Specht L: Risk factors for radiation-induced
hypothyroidism: A literature-based meta-analysis. Cancer.
117:5250–5260. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sachdev S, Refaat T, Bacchus ID,
Sathiaseelan V and Mittal BB: Thyroid V50 highly predictive of
hypothyroidism in head-and-neck cancer patients treated with
intensity-modulated radiotherapy (IMRT). Am J Clin Oncol.
40:413–417. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Rønjom MF, Brink C, Bentzen SM, Hegedüs L,
Overgaard J and Johansen J: Hypothyroidism after primary
radiotherapy for head and neck squamous cell carcinoma: Normal
tissue complication probability modeling with latent time
correction. Radiother Oncol. 109:317–322. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Heidari S, Babor TF, De Castro P, Tort S
and Curno M: Sex and gender equity in research: Rationale for the
SAGER guidelines and recommended use. Res Integr Peer Rev. 1:22016.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Steuer CE, El-Deiry M, Parks JR, Higgins
KA and Saba NF: An update on larynx cancer. CA Cancer J Clin.
67:31–50. 2017. View Article : Google Scholar : PubMed/NCBI
|