Introduction
Mixed epithelial and stromal tumor (MEST) is a rare
neoplasm of the kidney (1–9), with ~100 cases having been described
in the up-to-date literature (1,2,4–5,9,10).
It has been recognized as a renal tumor since its
introduction to the classification by World Health Organization in
2004 (4). MEST is most commonly
diagnosed in women of menopausal age (1–11).
Most of neoplasms were related to women with history of long
estrogen therapy. Due to this information it can be considered that
hormones are a risk factor for this tumor. The clinical
presentation of MEST is similar to typical renal tumor (1,2,4–5,6,8,10–12).
However approximately ¼ of known diagnosed MESTs were asymptomatic.
Current treatment strategy is based on surgical operation. Imaging
studies usually reveal a cystic lesion with soft tissue components
(1–12). Microscopic findings consist of
epithelium with mesenchymal tissue (1–12).
The risk of malignant transformation in a patient with MEST is
highly dependent on the individual characteristics of a tumor, but
in vast majority of patients, the neoplasm was of benign character
and the prognosis is good (1–12).
Case report
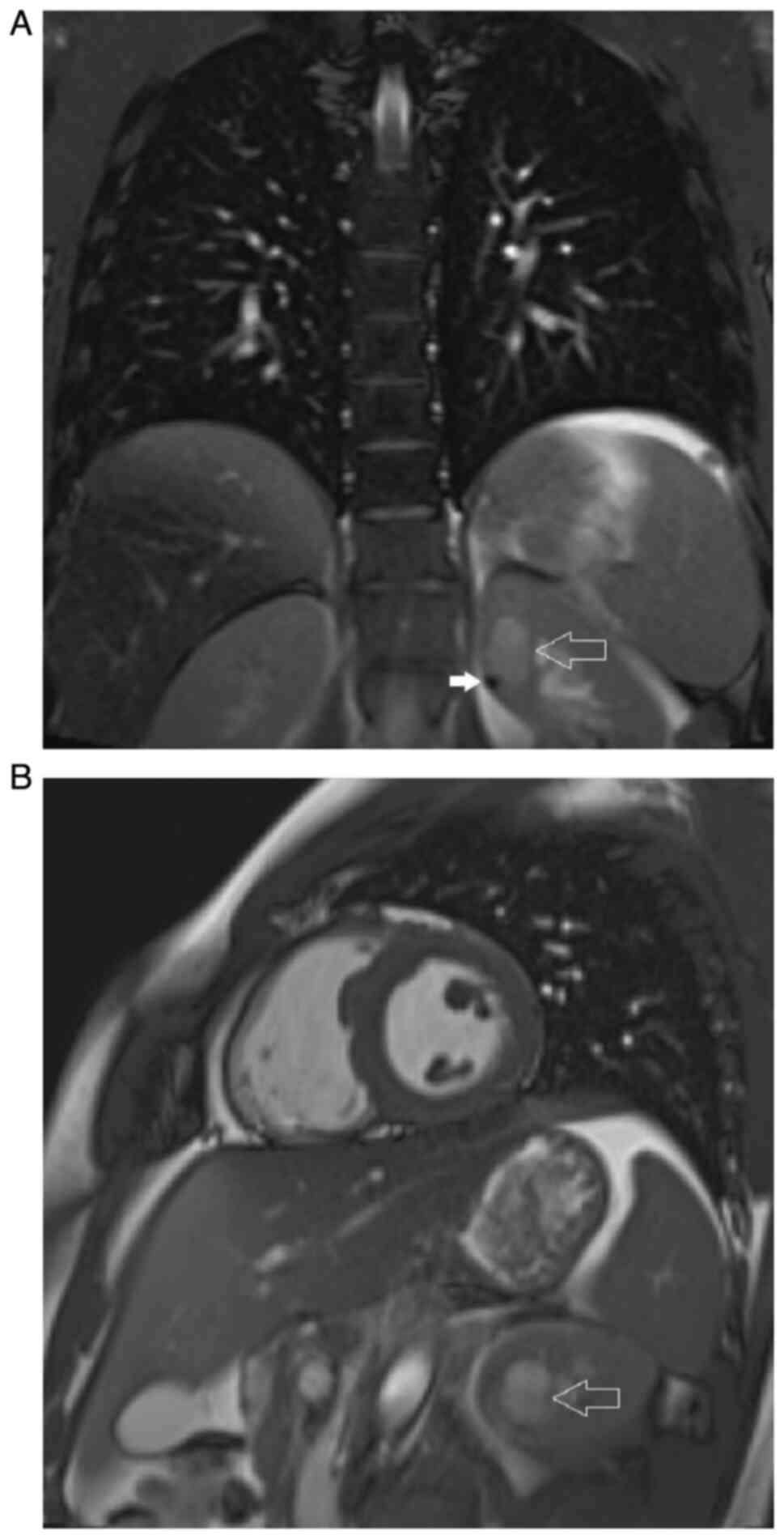
An 18-year-old male patient was incidentally
diagnosed with a lesion of the left kidney on magnetic resonance
(MR) imaging of the heart, performed as part of diagnostic
evaluation for a history of exercise-induced syncope episodes.
Apart from familiar hypertension, treated with lisinopril, the past
medical history of the patient was insignificant. The MR imaging
revealed a 3-cm, well-demarcated, non-protruding, complex cystic
lesion with a soft tissue component adjacent to its wall, located
in the upper pole of the left kidney. The lesion was showing high
signal intensity on T2-weighted imaging but no contrast enhancement
(Fig. 1). The presence of the
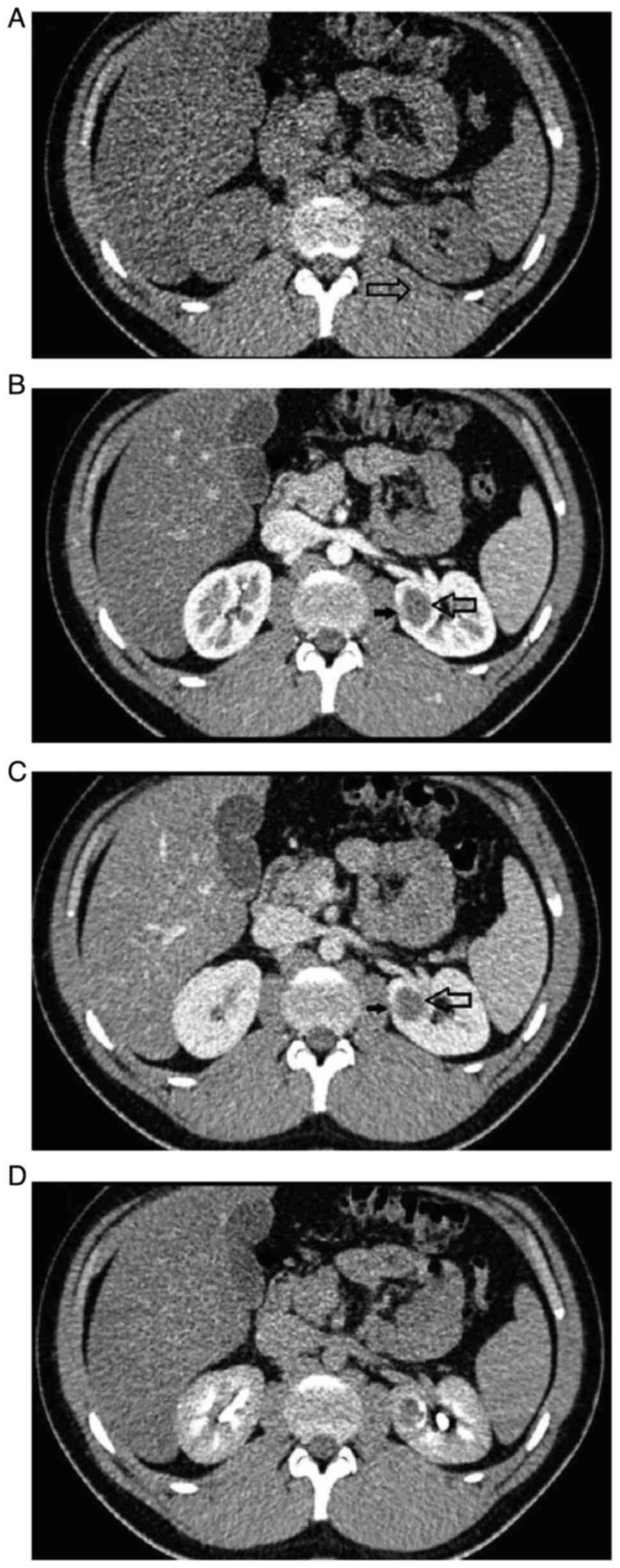
lesion was then confirmed on multiphase abdominal computed
tomography (CT) scan (Fig. 2). The
attenuation of the lesion on native-phase images was 30 Hounsfield
units (HU), with minimal and non-significant contrast enhancement
on subsequent phases, which was interpreted as indicative of cystic
nature of the lesion. However, medially within the cyst a 7-mm
soft-tissue tumor was revealed adjacent to the cystic wall, showing
a moderate contrast-enhancement, which raised suspicions for
malignant character of the lesion. The patient did not report
hematuria, flank pain nor any other symptoms that could have
indicated a renal tumor.
The patient was scheduled for surgery and a partial
nephrectomy was performed, leading to a complete excision of the
lesion. The perioperative course was uneventful. Gross examination
of the nephrectomy specimen demonstrated 3 cm multicystic tumor of
the renal medulla with 7 mm greyish solid component within the
cyst. The tumor was non-encapsulated. No necrosis was found.
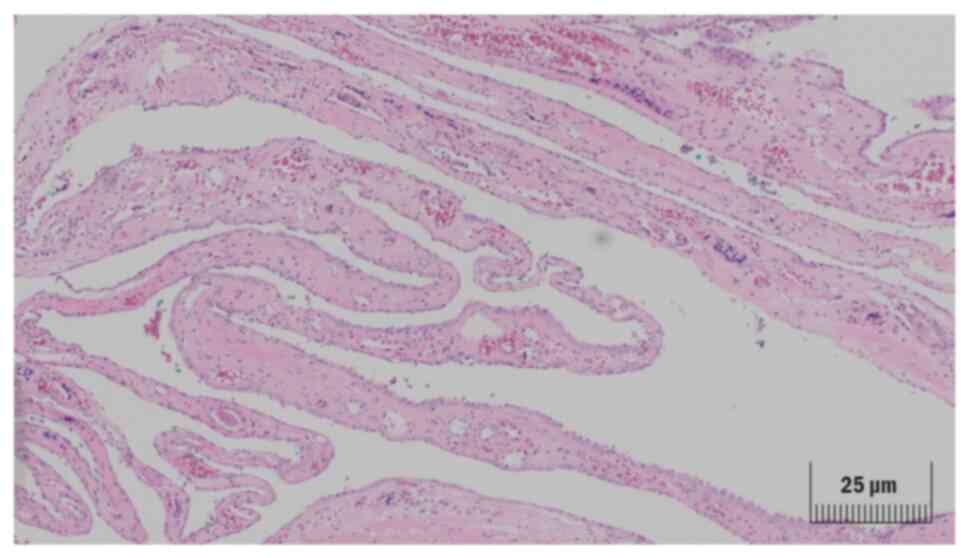
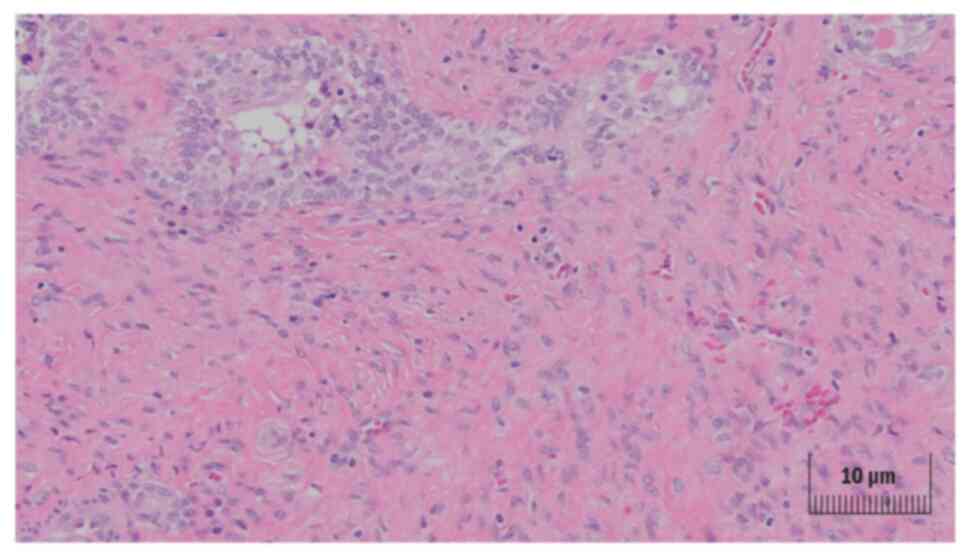
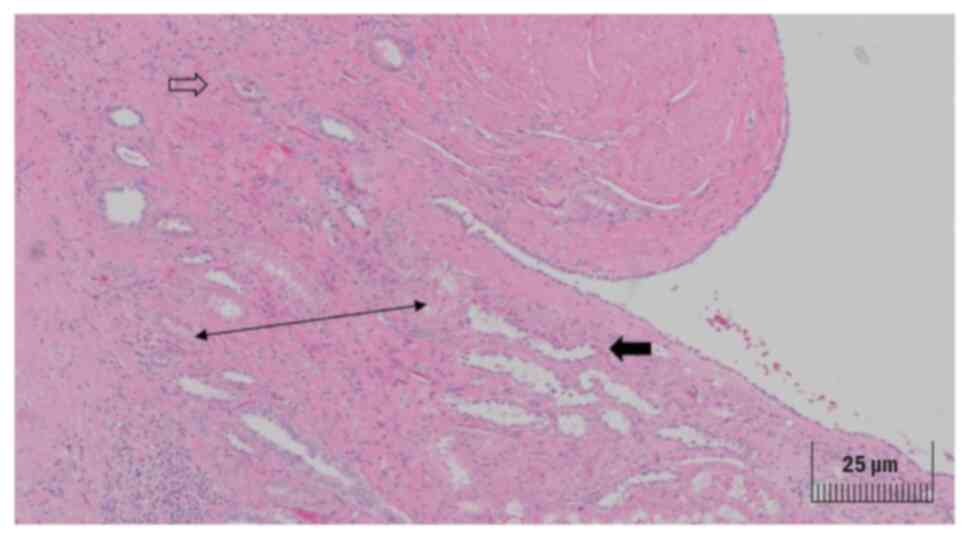
Microscopically, appearance of the cystic component of the tumor
resembled an adult cystic nephroma (Fig. 3). The cystic septa were covered
with monolayer of benign flat and cuboidal epithelial cells. The
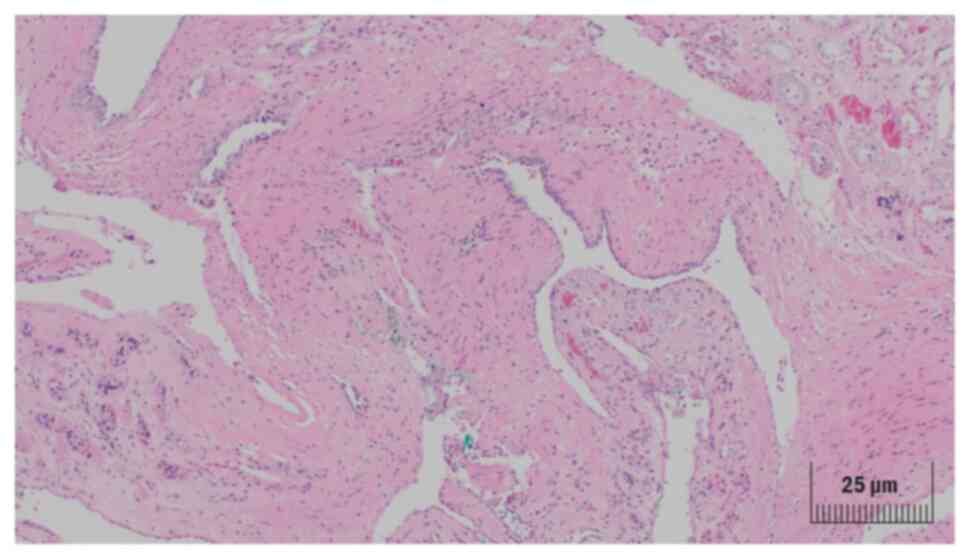
histology of the solid component was typical for MEST with
epithelial component consisted of branched glandular structures.
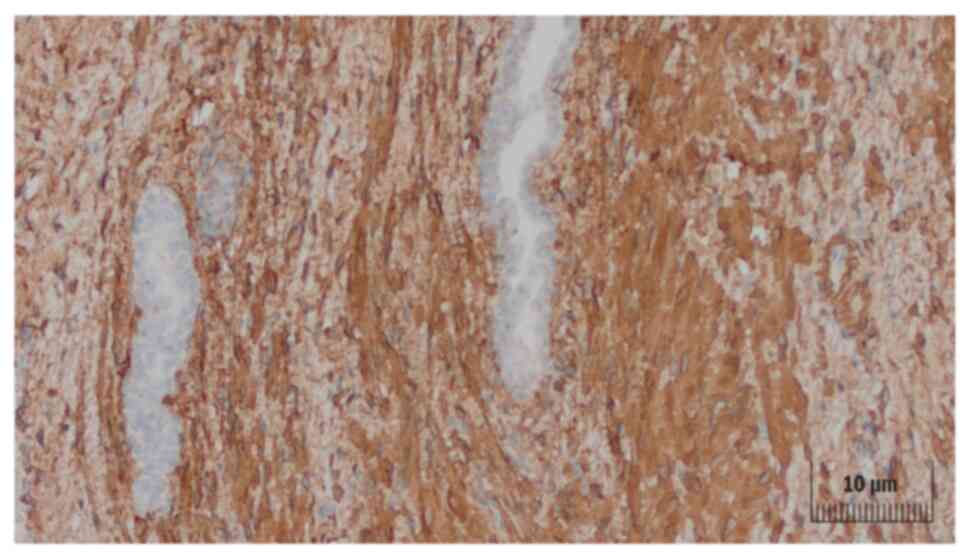
The stromal component contained elongated spindle-shaped smooth
muscle-like cells with vesicular nuclei surrounded by hypocellular
highly collagenized matrix with flattened vessels (Fig. 4). Apart from these findings, the
solid tumor contained scattered small tubular structures lined with
transitional cells with amphiphilic or clear cytoplasm.
Eosinophilic secretions were seen inside the tubules (Fig. 5). Some of the tubules were
protruding among the papillary ducts (Fig. 6). The cells of both epithelial and
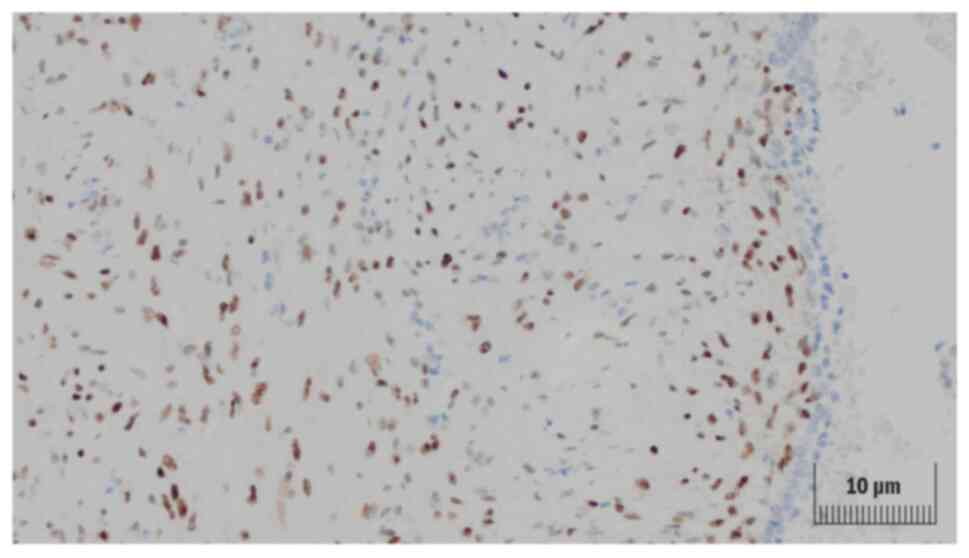
stromal components did not show atypia or mitoses. The stromal
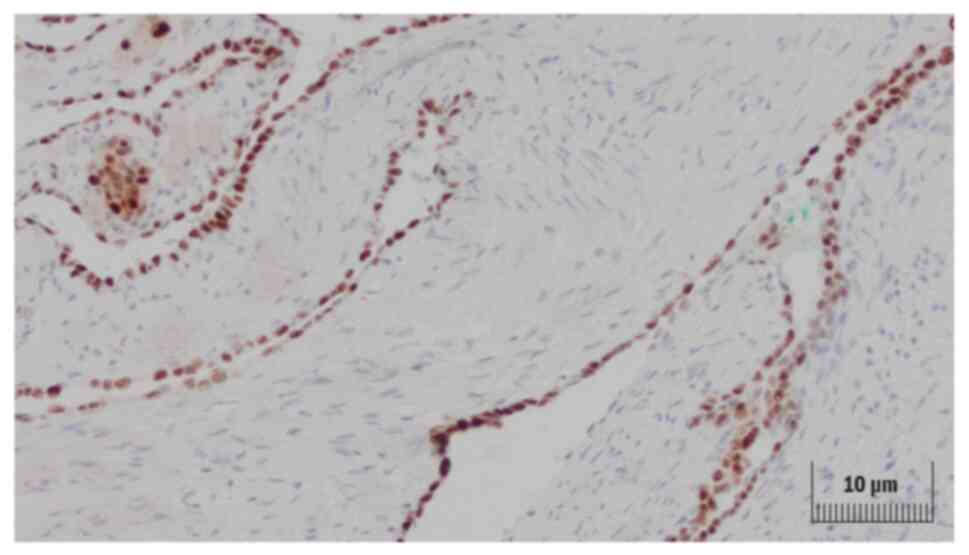
cells were, immunohistochemically, positive for ER [Dako, catalog
number IR084 RTU, 30′Ab, room temperature] (Fig. 7), PgR [Dako IR068 RTU, 30′Ab, room
temperature], SMA [Dako IR611 RTU, 30′Ab, room temperature]
(Fig. 8) and caldesmon. The
epithelial component was positive for GATA-3 [Ventana L50-823,
30′Ab, room temperature] and PAX-8 [Cell Marque MRQ-50, 30′Ab, room
temperature] (Fig. 9).
Immunostains for inhibin [Dako IR058 RTU, 30′Ab, room temperature],
calretinin [Dako IR627 RTU, 30′Ab, room temperature] and CD-10
[Dako IR648 RTU, 30′Ab, room temperature] were negative. Until now,
no disease recurrence nor progression has been observed in the
patient during the one-year follow-up.
Discussion
MEST is a rare neoplasm of the kidney (1–9). Up
to date, ~100 of cases have been described in the literature
(1,2,4–5,8,10).
The majority of diagnosed tumors occurred in women at menopausal
age (1–11) and only a few cases have been
described in men (1,2,4–5,7–8),
with a female-to-male ratio of 10 to 1 (1,2,4,8,11,12).
The age of diagnosis varied from 17 to 78 in cases described in the
literature, most commonly being ~50 (1,2,4,6,7,12),
with a single pediatric case having been reported (7). MEST appears to be more common in
women with a history of prolonged estrogen replacement therapy, as
well as in men treated with some forms of hormonal therapy,
reflecting a possible role of sex hormones in the etiology and
development of these tumors.
The clinical presentation of MEST may include flank
pain, hematuria, urinary tract infections and a palpable abdominal
mass, which comprise for typical symptoms of a renal tumor
(1,2,4,5,6,8,10–12).
However, approximately a quarter of patient diagnosed with MEST
were asymptomatic with the tumor being incidentally diagnosed on
abdominal imaging (1,2,4,5,8,10–12).
The vast majority of MESTs are benign lesions,
showing no local recurrence nor distant metastases. The risk of
malignant transformation in a patient with MEST is highly dependent
on the individual characteristics of a tumor. A few cases of
malignant transformation have been described in the literature,
affecting both epithelium or stromal tumor (1–8,10–12),
including transformation into sarcoma, rhabdomyosarcoma,
chondrosarcoma or papillary renal cell carcinoma. Thus, the
differential diagnosis of MEST should include the above
malignancies (1–7,11,12).
MESTs of the kidney present as unilateral and
solitary lesions. Usually the tumor is well-demarcated, with the
size of 3 to 24 cm having been reported in the literature (1–4,6–7,12).
It can develop both in the renal cortex and in the medulla
(1,2,4). CT
scan commonly reveals cystic lesions, described as III or IV in the
Bosniak classification, with solid components demonstrating
contrast enhancement on the delayed phase (1,2,4,5,8,12).
MR imaging usually shows complex cysts with cystic components of
low and high signal intensity on T1 and T2-weighted imaging,
respectively, and solid components of high and low signal intensity
on T1 and T2-weighted imaging, respectively (9). Tissue sections show a tumor with
cystic and solid components (1–12).
While the cystic component is more prominent in adult nephroma, the
composition of MEST is mainly stromal. The microscopic appearance
of both epithelial and stromal compounds of MEST is highly
variable. The spindle-shaped stromal cells may have hyperchromatic
nuclei with scant cytoplasm, or vesicular nuclei with abundant
cytoplasm, may present as cells with elongated nuclei or
barrel-shaped cells with abundant cytoplasm. The stromal component
may vary in terms of cellularity, which is higher if adjacent to
cystic components, but may also be lower and accompanied by
collagenized or myxoid patterns. The regions with high cellularity
may be organized in bundles that appear similar to smooth-muscle
fibers, occasionally resembling ovarian stroma (1–5,7,8,11–12).
The epithelial component may comprise of small glands or branching
tubular structures with flat, cuboid or hobnail cells lining
(1–3,11).
Approximately 90% of spindle-shaped stromal cells
demonstrate positive immunohistochemistry staining for smooth
muscle actine, desmin, ER and PR. Positive staining for CD-10,
CD-34 and WT1 occurs in ~50% of cases. The epithelial component
stains positive for epithelial markers: PAX8 and GATA3. MEST tumor
cells are immune-negative for inhibin, SF1, HMB45 and catepsine
(1–3,7,8,10–12).
In conclusion, MEST of the kidney is a rare
neoplasm. It is most commonly diagnosed in women at menopausal age.
It is a neoplasm of benign character and good prognosis, although
local recurrences and malignant transformations have been reported
in the literature. As the up-to-date evidence in regard to the
prognosis and survival of patients with MEST of the kidney is
insufficient, reporting new cases could help in developing
guidelines on the diagnosis and treatment of patients with this
condition.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
PK wrote the manuscript, obtained data, and made
substantial contributions to conception and design of the
manuscript. TK, TD, HK, BA and JK performed the operation (TK was
the first surgeon who performed the operation), receiving cancer
tissues that could be used as material for study, performing
acquisition of data. TK carried out microscopic examination of the
tissue obtaining data and made substantial contributions to the
interpretation of data. PK and KS confirm the authenticity of all
the raw data. KS carried out the histopathology examination. JP
carried out radiology studies, such as CT, and wrote a description
for radiology images, interpreting the data. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The patient provided written informed consent for
participation in the study.
Patient consent for publication
The patient provided written informed consent for
the publication of any data and/or accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Adsay NV, Eble JN, Srigley JR, Jones EC
and Grignon DJ: Mixed epithelial and stromal tumor of the kidney.
Am J Surg Pathol. 24:958–970. 2000. View Article : Google Scholar
|
|
2
|
Montironi R, Mazzucchelli R, Lopez-Beltran
A, Martignoni G, Cheng L, Montorsi F and Scarpelli M: Cystic
nephroma and mixed epithelial and stromal tumour of the kidney:
Opposite ends of the spectrum of the same entity? Eur Urol.
54:1237–1246. 2008. View Article : Google Scholar
|
|
3
|
Michal M and Syrucek M: Benign mixed
epithelial and stromal tumor of the kidney. Pathol Res Pract.
194:445–448. 1998. View Article : Google Scholar
|
|
4
|
Ozkanli S, Zerk PE, Zemher E, Culpan M,
Zenginkinet T and Aydin A: Mixed epithelial and stromal tumor of
the kidney: A rare case report. J Med Cases. 5:362–365. 2014.
View Article : Google Scholar
|
|
5
|
Chu LC, Hruban RH, Horton KM and Fishman
EK: Mixed epithelial and stromal tumor of the kidney:
Radiologic-pathologic correlation. Radiographics. 30:1541–1551.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rao HD, Sriram S, Srinivas BH, Challa S,
Reddy RCh and Murthy P: Mixed epithelial stromal tumor of the
kidney. Indian J Urol. 27:284–287. 2011. View Article : Google Scholar
|
|
7
|
Picken MM, Bova D, Pins MR and Quek ML:
Mixed epithelial and stromal tumor of the kidney with extension
into inferior vena cava: Case report and discussion of adult
biphasic cystic renal lesions and the significance of vascular
involvement. Case Rep Pathol. 2018:82342952018.
|
|
8
|
Ye J, Xu Q, Zheng J, Wang SA, Wu YW, Cai
JH and Yuan H: Imaging of mixed epithelial and stromal tumor of the
kidney: A case report and review of the literature. World J Clin
Cases. 7:2580–2586. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tian JL and Cui BP: Mixed epithelial and
stromal tumor of the kidney on 18F-FDG PET/CT in a 21-year-old
female. Saudi Med J. 40:499–502. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Thyavihally YB, Tongaonkar HB and Desai
SB: Benign mixed epithelial stromal tumor of the renal pelvis with
exophytic growth: Case report. Int Semin Surg Oncol. 2:182005.
View Article : Google Scholar
|
|
11
|
Zou L, Zhang X and Xiang H: Malignant
mixed epithelial and stromal tumor of the kidney: The second male
case and review of literature. Int J Clin Exp Pathol. 7:2658–2663.
2014.
|
|
12
|
Minoda R, Takagi T, Toda N, Itagaki H,
Kondo T, Ishida H, Nagashima Y and Tanabe K: Bilateral and multiple
mixed epithelial and stromal tumors of the kidney: A case report.
Mol Clin Oncol. 7:1005–1007. 2017.
|