Introduction
Radiation retinopathy is a known visual complication
of radiotherapy administered to orbital or periorbital structures,
with an incidence of proliferative retinopathy reported at 6% at 5
years in a large study of 3,841 eyes treated with plaque
radiotherapy for ocular melanoma (1). Irradiation of nasopharyngeal
carcinomas involve treatment over a large field with high dosage
(2). Though nasopharyngeal
carcinomas are relatively radiosensitive (2), a significant proportion of patients
have a long life-expectancy, and therefore late visual
complications can occur and are a concern to patients, ENT
specialists, ophthalmologists and radiation oncologists. We
describe a succinct case of a patient that developed radiation
retinopathy following treatment for nasopharyngeal carcinoma.
Case report
A 37-year-old male was referred to the ophthalmology
department by his optometrist, with a one-month history of blurred
vision in the left eye. Ten years previously, he had received
radical radiotherapy for a nasopharyngeal carcinoma staged T1N1M0.
There was no recurrence and no other medical history of note.
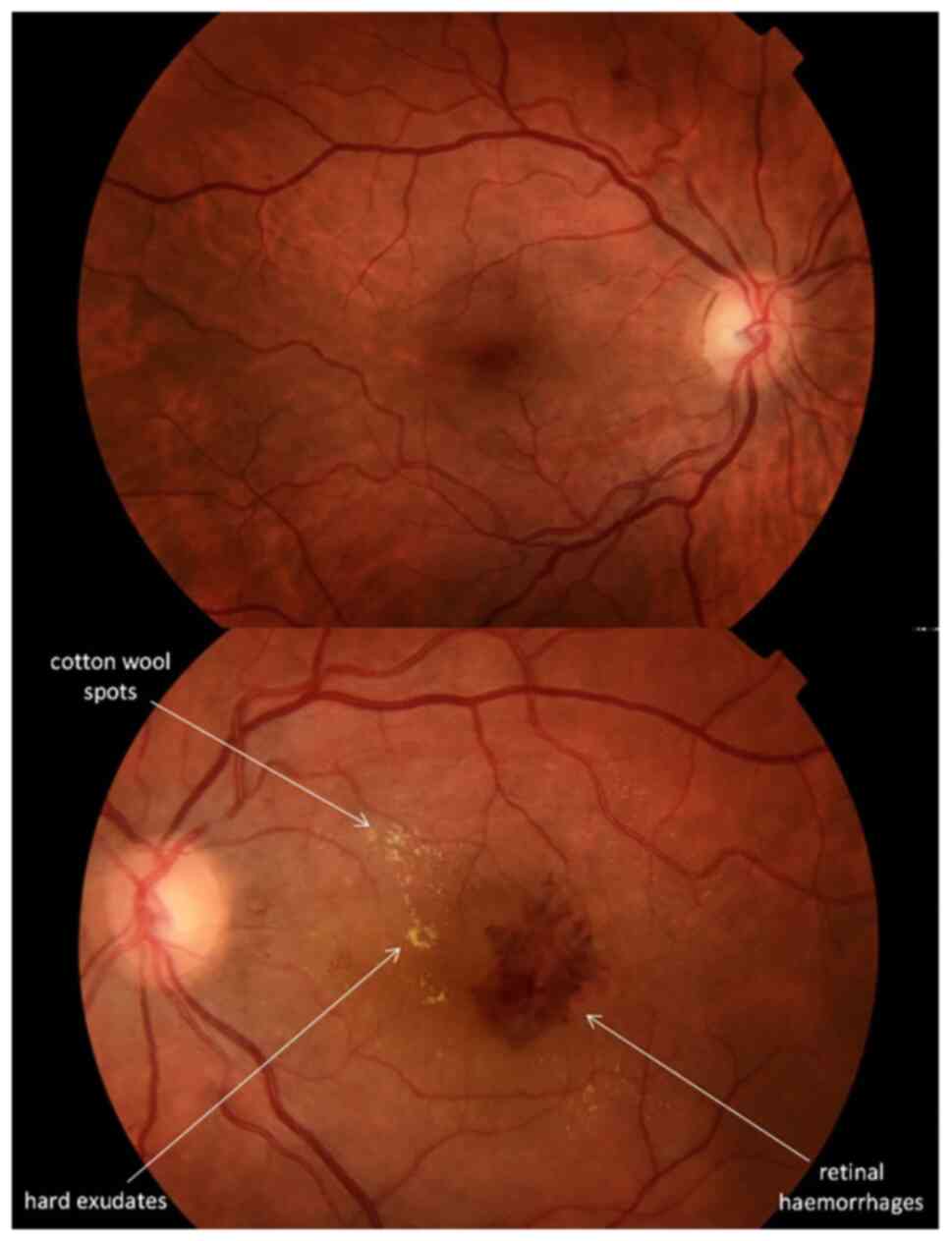
On presentation, his visual acuities were 6/6 right
eye and 6/36 left eye. The eyes on inspection appeared healthy and
the right eye's retinal examination was unremarkable, however the
left retina demonstrated fine intraretinal haemorrhages, cotton
wool spots and hard exudates (Fig.
1).
An optical coherent tomography scan of the left
retina showed macular oedema. Blood pressure and blood tests
including glucose and HbA1c were all normal. A diagnosis of
radiation retinopathy was made and the patient received four doses
of intravitreal Ranibizumab at one-month intervals, even though
evidence for this intervention is limited. The visual acuity of the
left eye improved to 6/18 by the time of the third injection and
has remained at this level for a follow-up period of three
years.
Discussion
Radiation retinopathy occurs after exposure to
radiation (external beam, plaque brachytherapy or stereotactic
radiosurgery) administered around the orbital region (3). This occurs in 7% of cases that
receive radiation to the globe, orbit, sinuses or nasopharynx
(1). Retinopathy usually occurs
after 6 months to 3 years after treatment, which is thought to be
the turnover time for endothelial cells of the retinal vasculature
(4), although cases have been
reported after 15 years of exposure (1). Radiation retinopathy is often dose,
daily fraction size and fraction interval dependent, with the usual
threshold dose for retinal damage at 30–35 Gy (1). Higher total radiation dose and fewer
fractions was associated with increased risk of developing
retinopathy (5,6).
Clinical features include retinal microvascular
changes including endothelial cell loss, capillary occlusion,
telangiectasia and microaneurysms. Other retinal findings are
oedema, exudates, cotton wool spots, haemorrhages, papillopathy
(inflammation of the head of the optic nerve), radiation-induced
optic neuropathy and proliferative retinopathy. Affected patients
may also develop other ophthalmic features including cataract and
keratopathy (3).
Differential diagnoses to consider are diabetic
retinopathy, retinal vein occlusion, ocular ischaemic syndrome and
hypertensive retinopathy. Radiation retinopathy is mainly
distinguished from its differentials due to a) a history of
identified exposure to ionising radiation b) clinical examination
shows irregular dilation of the capillary bed at the posterior pole
of the fundus, rather than significant venous or arterial
irregularities which may signify vein occlusion or hypertensive
retinopathy c) presence of macular oedema, which would occur with
radiation or diabetic retinopathy, but not in uncomplicated
hypertensive retinopathy d) normal blood pressure and diabetic
blood tests. In summary, a vascular work up, a history of exposure
together with retinal findings would need to be considered when
considering the differential diagnoses.
Treatment aim is to reduce retinal oedema and
prevent new vessel formation. Treatment options include the use of
laser photocoagulation, intravitreal corticosteroids and
anti-vascular endothelial growth factor (anti-VEGF) agents, such as
Bevacizumab and Ranibizumab (7–10).
Prognosis depends on the severity of involvement.
Poor prognostic factors include papillopathy and proliferative
retinopathy, which may result in vitreous haemorrhage and
tractional retinal detachment (8–11).
This case highlights the importance of recognising
the effects that radiation administered to structures near the eye
can have on vision. Even though there was no recurrence, and the
patient was discharged from ENT and oncology, the latency of this
case demonstrates the need for routine eye tests in patients who
have undergone radiotherapy near the orbit. Prompt recognition and
referral to ophthalmologists is necessary for all suspected cases
to best manage visual loss.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analysed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AK and ST were involved in designing the study and
in the acquisition of the data. AK, MT and ST analysed and
interpreted the data. AK wrote the initial draft and MT edited the
draft and subsequent versions. AK, MT and ST critically analysed
the content. AK and ST confirm the authenticity of all the raw
data. AK, MT and ST agree to be accountable for all aspects of the
work in ensuring that questions related to the accuracy or
integrity of any part of the work are appropriately investigated
and resolved. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for inclusion of the images for publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bianciotto C, Shields CL, Pirondini C,
Mashayekhi A, Furuta M and Shields JA: Proliferative Radiation
retinopathy after plaque radiotherapy for uveal melanoma.
Ophthalmology. 117:1005–1012. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rosenblatt E, Brook OR, Erlich N, Miller
B, Joachims HZ and Kuten A: Late visual and auditory toxicity of
radiotherapy for nasopharyngeal carcinoma. Tumori. 89:68–74. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Amoaku WM and Archer DB: Fluorescein
angiographic features, natural course and treatment of radiation
retinopathy. Eye (Lond). 4((Pt 5)): 657–667. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Archer DB and Gardiner TA: Ionizing
radiation and the retina. Curr Opin Ophthalmol. 5:59–65. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Parsons JT, Bova FJ, Fitzgerald CR,
Mendenhall WM and Million RR: Radiation retinopathy after
external-beam irradiation: Analysis of time-dose factors. Int J
Radiat Oncol Biol Phys. 30:765–773. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Monroe AT, Bhandare N, Morris CG and
Mendenhall WM: Preventing radiation retinopathy with
hyperfractionation. Int J Radiat Oncol Biol Phys. 61:856–864. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Abramson DH, Beaverson KL, Chang ST,
Dunkel IJ and McCormick B: Outcome following initial external beam
radiotherapy in patients with Reese-Ellsworth Group Vb
retinoblastoma. Arch Ophthalmol. 122:1316–1323. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Finger PT and Kurli M: Laser
photocoagulation for radiation retinopathy after ophthalmic plaque
radiation therapy. Br J Ophthalmol. 89:730–738. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Giuliari GP, Sadaka A, Hinkle DM and
Simpson ER: Current treatments for radiation retinopathy. Acta
Oncol. 50:6–13. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Reichstein D: Current treatments and
preventive strategies for radiation retinopathy. Curr Opin
Ophthalmol. 26:157–166. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yanoff M and Duker J: Ophthalmology. 3rd
Edition. Mosby Inc., Elsevier; Maryland Heights, MO: 2008
|