Introduction
Thymic epithelial tumors (TETs) are rare thoracic
cancers arising in the mediastinum. They are classified into two
major, but heterogeneous histopathologic groups according to the
most recent WHO histopathologic classification: (a) thymomas (TM)
and (b) thymic carcinomas (TC) (1).
TM are more frequent compared to TC and they are further
categorized into five different types (A, AB, B1, B2 and B3) based
on the relative proportion of the non-neoplastic lymphocytic
component and the resemblance to normal thymus (1). TC are rare and highly aggressive
tumors with most frequent histologic subtype that of squamous cell
carcinoma. Staging of thymic tumors is currently based on the
eighth edition of the American Joint Committee on Cancer/Union for
International Cancer Control tumor node metastasis (TNM) staging
classification (2) which replaced
the previous Masaoka-Koga surgical staging system (3).
The management of TETs requires a multidisciplinary
approach (4,5). Surgery is the cornerstone of the
curative-intent treatment. In the case of locally advanced tumors
with invasion of neighboring structures when an upfront complete
resection is not feasible, chemotherapy could be used to reduce the
tumor burden-potentially allowing subsequent surgery and/or
radiotherapy (4). It should be
noted that stage IV in TETs may still be eligible for
curative-intent multimodal treatment, especially in the case of
pleural invasion or oligometastatic presentation. Metastatic and
recurrent tumors, which are more frequently TC than TM, should be
treated with systemic anticancer therapy. Carboplatin coupled with
paclitaxel is the recommended therapy for TC, while the combination
of cisplatin, doxorubicin, and cyclophosphamide (CAP) is the
preferred regimen for TM (4,5).
Unfortunately, no standard subsequent treatments are established
for platinum-refractory patients.
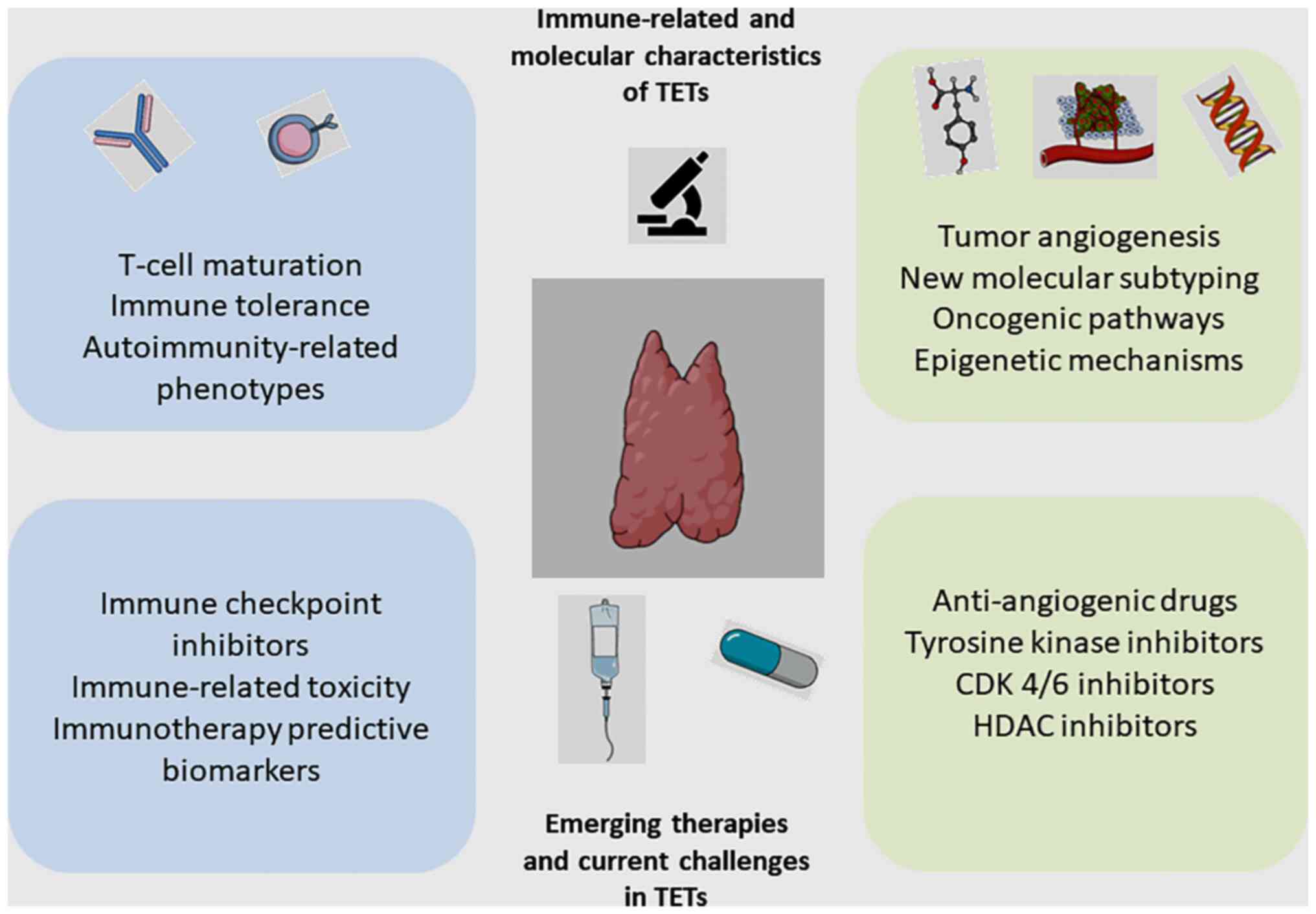
Current research perspective in TETs involves the
genomic characterization of the tumors, the exploration of
oncogenic pathways and the investigation of the tumor
microenvironment, especially regarding its unique tissue-specific
immune component (6,7). Alternative therapeutic options are
emerging, including targeted agents and immune checkpoint
inhibitors (Fig. 1). Many novel
trials are ongoing to implement precision medicine in the
management of TETs. The aim of this review is to summarize current
clinical research on systemic treatments for TETs, focusing on the
fields of immunotherapy and targeted therapies.
Immunotherapy in TETs
Immunobiology of the thymus
Thymus is a primary lymphoid organ with a crucial
role in T cell maturation and the development of immune tolerance.
The structure of the gland consists of an outer capsule, a cortex
and a medulla. Immature T cells (thymocytes) move through the
thymic cortex and corticomedullary junction, undergoing serial
phenotypic modifications, which eventually result in their
maturation through a positive and negative selection process
(8,9). During positive selection, only those
thymocytes that have a T cell receptor (TCR) capable of binding the
Major Histocompatibility Complex (MHC) expressed on thymic
epithelial cells are preserved and enter the thymic medulla, where
a negative selection process takes places. More specifically, the
medulla contains medullary thymic epithelial cells (mTECs)
expressing various tissue-specific self-antigens (TSAs). Those T
cells that interact with TSAs with high affinity undergo apoptosis
(8,9). Expression of TSAs by mTECs is
controlled by the transcription factors auto immune regulator
(AIRE) and forebrain embryonic zinc finger-like protein 2 (Fezf2)
(9,10). Nevertheless, negative selection is
not completely efficient, since some auto reactive T cells might
escape thymic selection and be released into the bloodstream and,
therefore, additional peripheral tolerance mechanisms are critical
to avoid autoimmunity (11,12).
Autoimmunity and thymomas
Approximately 30% of patients with TM present with
autoimmune and paraneoplastic syndromes at the time of diagnosis,
the most common being Myasthenia Gravis (MG) and less frequently
pure red cell aplasia, systemic lupus erythematosus and
hypogammaglobulinaemia (13,14).
In contrast to TM, TC, which is a more aggressive tumor, with local
invasiveness, early nodal dissemination, and a higher metastatic
potential, is not associated with autoimmune disorders, possibly
because of the absence of immature T cells within the tumor
(13).
It has been suggested that the disruption of thymic
architecture and the dysfunctional mTECs in patients with TETs may
result in impaired maturation of thymocytes and release of
autoreactive T cells into the bloodstream (13). Defective expression of transcription
factors AIRE and Fezf2 has also been implicated in impaired
negative selection of autoreactive T cells. In addition,
downregulated expression of MHC class II molecules by thymoma cells
has been implicated in the depletion of central immune tolerance
and predisposition towards autoimmunity (13–18).
Of note, data from The Cancer Genome Atlas analysis
(TCGA) raise the hypothesis that deficient central immunotolerance
and immunosuppression are unlikely to be the sole mechanism of MG
in TM (15). In this study, the
molecular aberrations of 24 TM associated with Myasthenia Gravis
(MG+) were compared to those of 72 TM without Myasthenia Gravis
(MG-). Genes that are characteristically implicated in
immunotolerance mechanisms were not differentially expressed
between MG+ and MG- thymomas. Moreover, MG+ thymomas were not
associated with mutations in any single gene or with any specific
DNA methylation signature or miRNA expression profile. MG+
thymomas, however, overexpress genes coding for mid-sized
neurofilament and ryanodine receptors type III proteins, which
share sequences with major antigens associated with MG, such as the
acetylcholine receptor (AChR) and titin epitopes. Hence, it was
proposed that an additional mechanism of autoimmunity in MG+
Thymomas could rely on molecular mimicry of antigens between tumor
cells and the target organ (15).
Immunotherapy-related biomarkers in
TETs
Immune checkpoint inhibitors (ICIs) have changed the
natural history of many types of cancer and have achieved durable
responses in a subset of patients. The identification of predictive
biomarkers to define the patients that are more likely to respond
to checkpoint inhibition is an ongoing challenge (16). The two most well-studied biomarkers,
yet with several limitations, are the programmed cell death
ligand-1 (PD-L1) expression on tumor cells and/or lymphocytes and
the tumor mutational burden (TMB) representing the number of single
nucleotide variants in a tumor genome coding area and putatively
indicating the ‘immunogenicity’ of the tumor (16).
It should be noted that PD-L1 is normally expressed
in the non-neoplastic thymus (17)
and PD-1/PD-L1 interaction negatively regulates the beta-selection
and modulates the positive selection as well. Studies report that
PD-L1 is generally highly expressed in neoplastic epithelial cells
in TETs (18), but correlations
with clinicopathological data and survival remain ambiguous with
controversial results among studies (19–23).
Also, TETs are characterized by a low TMB, which is the lowest
among adult cancers, but it is significantly higher in TC compared
to TM (15).
Immune checkpoint inhibitors in
TETs
After several case reports were published, trials
are now being conducted to assess the efficacy and safety of
PD-1/PD-L1 inhibitors in patients with ΤΕΤs (Table I).
 | Table I.Published trials of immune checkpoint
inhibitors in TETs. |
Table I.
Published trials of immune checkpoint
inhibitors in TETs.
| First author,
year | Phase | Drug | Patients
(TM/TC) | ORR,
TM/TCa | DCR,
TM/TCa | mPFS,
TM/TCa | mOS,
TM/TCa | irAE G3-4,
TM/TCa | Primary
endpoint/Positive or negative trial | (Refs.) |
|---|
| Cho et al,
2019 | II | Pembrolizumab | 33 (7/26) | 29%/19% | 100%/73% | 6.1/6.1 | NR/14.5 | 71.4%/15.4% | ORR/Positive | (26) |
| Giaccone et
al, 2018 | II | Pembrolizumab | 40 (0/40) | -/22.5% | -/75% | -/4.2 | -/24.9 | -/15% | ORR/Positive | (24) |
| Katsuya et
al, 2019 | II | Nivolumab | 15 (0/15) | -/0% | -/73.3% | -/3.8 | -/14.1 | -/13.3% | ORR/Negative | (29) |
| Rajan et al,
2019 | I | Avelumab | 8 (7/1) | 28.5%/0% | 87%/100% | NA | NA | 62.5%/0% | NA | (27) |
Pembrolizumab
The PD-1 inhibitor pembrolizumab was investigated by
Giaccone et al in 40 patients with recurrent TC in a phase
II trial (24). Patients with prior
history of autoimmune disease were ineligible. An overall response
rate (ORR) of 22.5% was observed. Disease control was achieved in
30 (75%) patients with a median duration of response of 3 years.
Median progression-free survival (mPFS) was 4.2 months and median
overall survival (mOS) was 24.9 months. High PD-L1 expression
(>50% of tumor cells), was found in ten patients, six of whom
had a complete response (CR) or partial response (PR). Out of 27
patients with low or negative PD-L1 expression, 85% had progression
of disease (PD) as the best response. IFN-γ signature expression
was correlated with response to pembrolizumab. Targeted exome
sequencing showed that TP53 mutations were associated to
lower expression of PD-L1 and shorter OS, while mutations in
CYLD, another tumor suppressor gene, were associated with
high PD-L1 expression. When four patients were rechallenged with
pembrolizumab, two responses were recorded, one of them two years
after completing therapy. Six patients (15%) developed severe
immune-related adverse events (irAEs), including myocarditis and
polymyositis (24,25).
Another phase II trial evaluated pembrolizumab in 26
patients with recurrent TC and 7 patients with recurrent TM
(26). Patients with active
autoimmune disease were excluded. The ORR was 19.2% in patients
with TC and 28.6% in patients with TM. The median duration of
response was not reached in patients with TM and was 9.7 months in
patients with TC. Median PFS was 6.1 months in both groups. Median
OS was 14.5 months for TC and not reached in patients with TM. High
PD-L1 levels were confirmed as significant predictive biomarker of
response: 35.7% of patients with high PD-L1 expression achieved a
PR, whereas none of the patients with low PD-L1 expression
responded. Patients with TM experienced significantly more grade 3
or 4 irAEs as compared to TC (71% vs. 15%, respectively) including
hepatitis, myocarditis and MG (26).
Avelumab
Rajan et al conducted a phase I trial with
the PD-L1 inhibitor avelumab in 7 patients diagnosed with TM and
one with TC (27). Almost 30% of
the patients had an objective response, while 3 patients had
response after a single dose of avelumab. A particularly higher
rate of irAEs was described compared to other solid tumors treated
with avelumab. The incidence of grade 3 AEs was 38%, with the same
rate for grade 4 AEs: 5 patients developed severe irAEs including
myositis and respiratory muscle insufficiency. Interestingly, all
responders who developed irAEs had previously been treated with
sunitinib, a multikinase inhibitor with an anti-angiogenic effect
and with immunomodulatory properties. Only one of the patients that
did not respond developed an irAE. PD-L1 expression predictive
value was not evaluated due to inadequate number of patients for
analysis.
Further analysis of the trial uncovered that
pretreatment absolute lymphocyte count was higher in responders
compared to non-responders, while percentage of B cells, regulatory
T cells and natural killer cells were lower in responders vs.
non-responders. Intratumoral immune infiltrates were also evaluated
in two patients with TM and showed that the immune pre-treatment
infiltrate mainly composed of immature T cells, shifted towards
predominantly mature CD8+ T cells infiltrate in the responder,
while it kept an immature T cells predominance in the
non-responder. Moreover, pre-therapy peripheral blood mononuclear
cells exhibited higher T-cell receptor diversity in patients who
responded and developed irAEs compared to those who did not
(27).
The same group also demonstrated that pre-existing
anti-acetylcholine receptor (anti-AchR) autoantibodies and B cell
lymphopenia confer risk for developing myositis after treatment
with avelumab even in the absence of autoimmune clinical history
(28). These findings need
additional evaluation because they might represent biomarkers of
pre-existing autoimmunity in patients without a clinical history of
autoimmune disease, at higher risk of irAEs. These markers are
under evaluation in an ongoing trial of avelumab in patients with
advanced TETs (NCT03076554).
Nivolumab
The PRIMER study was a two-stage single arm phase II
trial that investigated the activity of the PD-1 inhibitor
nivolumab in 15 patients with TC (29). No objective responses were observed
in this trial and accrual closed early for futility at the first
stage. The disease control rate (DCR) was 73%, the mPFS was 3.8
months and the mOS was 14.1 months, while the toxicity profile was
manageable (29). Ak and Aydiner
retrospectively tested the efficacy of nivolumab at four TMs, three
TCs, and one mixed histology (30).
Two patients' evaluation of best response was not applicable. Among
the five available patients, the ORR was 66.7%, and the DCR was
100%. The median follow-up time was 16.1 months. The mPFS and mOS
were 6.5 months and 7.4 months, respectively (30).
The NIVOTHYM trial (NCT03134118) is the first
international multicenter phase II trial evaluating the use of
nivolumab with or without ipilimumab in patients with
advanced/relapsed type B3 TM or TC after platinum-based
chemotherapy. The primary endpoint is PFS rate at 6 months. The
results of the nivolumab monotherapy cohort demonstrate a
manageable safety profile and objective activity; however, they are
insufficient to meet the trial primary objective. The second cohort
is currently ongoing to assess the combination of nivolumab plus
ipilimumab and the results are eagerly awaited.
Targeted agents in TETs
Anti-angiogenic agents
Angiogenesis plays a pivotal role in tumor
progression and is regulated by several pro-angiogenic molecules,
such as vascular endothelial growth factor (VEGF), platelet-derived
growth factor (PDGF) and transforming growth factor beta (TGFβ),
which have been found overexpressed in several cohorts of TETs
(31–33). Recently, it has been reported that
the deregulation of the equilibrium between activine A and its
natural inhibitor follistatin is also a pro-angiogenic pathogenic
mechanism in TETs. In patients with TC, high follistatin levels
were observed and correlated with advanced tumor stage, and tumor
microvessel density (34).
Sunitinib is an anti-angiogenic multikinase
inhibitor targeting VEGFR, PDGFR and c-KIT. Sunitinib was
administered as 50 mg orally once daily for six-week cycles (4
weeks on/2 weeks off treatment) in a phase II trial in patients
with TETs (35). The study met its
primary endpoint in the TC cohort with an ORR of 26% (DCR was 91%),
while ORR in TM was only 6% leading to early close of the TM cohort
per protocol rule. Also, mPFS was 7.2 and mOS was not reached
within the TC cohort, while mPFS was 8.5 months and mOS was 15.5
months within the TM cohort. Lower baseline levels of circulating
tumor cells and lower or stable levels of circulating endothelial
cells after administration of sunitinib were associated with
improved OS. An upregulation of immune checkpoint receptors was
reported in most patients, which was associated with improved OS.
Overall, toxicity profile was well tolerated, with a rate of
adverse events similar to what is described in other cancers, but
many patients in both cohorts required dose reductions (35).
Further studies have been conducted to evaluate
alternative schedules of sunitinib and/or its administration in
heavily pretreated TETs. A phase II study evaluated sunitinib at a
modified dose of 50 mg once daily using a 2-weeks-on/1-week-off
schedule. However, only 8% of the patients with TC responded
(36). Another phase II trial
conducted in 25 patients with metastatic TC after platinum-based
chemotherapy reported 22% ORR and 70% SD with a PFS of 15.2 months
(37). An ongoing phase II trial
(NCT01621568) is also investigating sunitinib toxicity and efficacy
using a schedule of 3-week cycles (50 mg daily for 2 weeks with 1
week off) in patients with advanced TETs with at least one prior
line of platinum-based chemotherapy. In a real-world retrospective
study of 28 patients from the French RYTHMIC network, 15 patients
received sunitinib as ≥fourth-line treatment, with initial daily
dose of sunitinib of 50 mg in 11 patients, 37.5 mg in 16 patients,
and 25 mg in one patient (38).
Sunitinib-related AEs seem to be tolerable. In the overall
population, ORR was 22% (29% for TM and 20% for TC) and median PFS
was 3.7 months (5.4 months for TM and 3.3 months for TC) (38).
REMORA trial explored the activity of lenvatinib, an
oral multi-kinase inhibitor that targets VEGFR, FGFR, c-KIT, and
other kinases, in 42 patients with TC who progressed after at least
one line of platinum-based chemotherapy and had not previously
received any anti-angiogenic agents (39). The trial met its primary endpoint
with an ORR of 38% and an acceptable toxicity profile. The DCR was
95%, the mPFS was 9.3 months and the mOS was not reached. The most
frequent treatment-related AEs were hypertension, thrombocytopenia,
diarrhea and palmar-plantar erythrodysesthesia syndrome. Serious
AEs were reported in 19% of the patients, including bowel
perforation, left ventricular dysfunction, pneumonitis and
electrocardiogram T wave abnormalities, while there were no deaths
due to AEs (39). Additionally, a
post hoc subgroup analysis by histological type revealed ORRs of
46.7 and 16.7% for squamous cell carcinoma and non-squamous cell
carcinoma, respectively. The clinical activity of lenvatinib with
ORR of 38% is the highest, to date, that has been reported in TETs
that progressed after first-line chemotherapy, and therefore,
lenvatinib is a promising therapeutic option.
Novel, small-molecule tyrosine kinase inhibitors
(TKIs) with anti-angiogenic activity are explored for patients with
TETs. Anlotinib is a new oral, broad spectrum TKI, which can
strongly inhibit VEGFR, PDGFR, FGFR, c-kit. Anlotinib is highly
selective for VEGF receptors VEGFR2 and VEGFR3 (40,41). A
recent case report described the efficacy of anlotinib in a patient
with refractory TC after multiple lines of chemotherapy as well as
anti-angiogenic therapy with another multi-target TKI, apatinib
(42). Apatinib is a highly
selective TKI, which mainly competes with the ATP-binding site of
VEGFR-2. The patient was unable to tolerate the toxicity associated
with apatinib and by the 13th month disease progressed (43). After the first anti-angiogenic TKI
failed, anlotinib was well tolerated, without obvious AEs and the
patient achieved a PFS of over 23 months; therefore, further
clinical investigation of anlotinib is warranted (42). Moreover, lucitanib is an oral,
potent selective inhibitor of VEGFR, PDGFR and fibroblast growth
factor receptor (FGFR), which was evaluated in a phase Ib trial
enrolling 15 patients with TM or TC. Two patients had PR, while 11
patients had SD. PFS was 7.5 months in thymic carcinomas (44). Finally, a phase II trial with TKI
regorafenib, in patients with TETs who progressed after at least
one line of chemotherapy recently reported results with a disease
control rate of 78.9% (45).
Less favorable results have been reported with
bevacizumab, a humanized monoclonal antibody against VEGF, which
was investigated in a phase 2 trial in combination with erlotinib.
The trial enrolled 18 patients with recurrent TM or TC. No
objective responses were observed, SD was observed in 11 patients
(60%), while in 7 patients (40%) PD was the best response (46).
Currently, several phase II trials are ongoing with
anti-angiogenic drugs either as single-agent therapies or in
combination with other types of systemic treatment (chemotherapy or
immunotherapy). A phase II trial assesses the activity of sunitinib
in patients with type B3 TM or TC who have received at least one
prior platinum-based chemotherapy (Style Trial-NCT03449173).
RELEVENT is a phase II trial that will investigate the combination
of ramucirumab, an anti-VEGFR2 monoclonal antibody, with
carboplatin and paclitaxel in the first-line setting for relapsed
or metastatic TETs of any histological type (NCT03921671).
KIT inhibitors
c-KIT (CD117) is a transmembrane receptor with
tyrosine kinase activity encoded by the proto-oncogene KIT.
Overexpression of c-KIT is associated with the development of
gastrointestinal stromal tumors (GIST), melanomas and certain types
of leukemias and lymphomas; however, apart from the above,
activating mutations of KIT are uncommon in most solid
tumors (47). In TETs,
overexpression of c-KIT is quite often in TC (46–80%), but
KIT mutations are rare and are found in less than 10%. On
the other hand, c-KIT overexpression is rare in TM (2–4%) (15,48).
Most KIT-mutated TCs are poorly differentiated squamous cell
carcinomas (48). Petrini et
al evaluated a large cohort of 120 TETs specimens (13 TC and
107 TM) and observed that KIT overexpression was much higher in TC
than TM, there was no association with the stage of the disease,
but KIT overexpression was a negative prognostic marker. In this
study, no KIT mutations were identified by sequencing the
gene from exons 1 to 20 (49).
Although mutations in KIT are rare, when
arising, they might be targetable with TKIs, such as imatinib
mesylate, which is already widely used in chronic myeloid leukemia
and GISTs. A number of studies have been performed to evaluate the
association of specific mutations with sensitivity to imatinib or
other inhibitors.
Girard et al investigated seven samples of TC
and sequenced exons 10 and 14 in addition to the more
frequently-mutated exons 9, 11, 13, and 17 (48). Interestingly, one of the mutations,
H697Y, was in exon 14 and showed higher in vitro sensitivity
to sunitinib than imatinib (48).
Other mutations that have been reported in TC and show differential
sensitivity to TKIs are V560del at exon 11, L576P at exon 11, Y553N
at exon 11, D820E at exon 17, V559G at exon 11, V577-579del at exon
11, and K642E at exon 13 (47).
Mutations at exon 11 confer sensitivity to imatinib. Strobel et
al reported a V560del kit mutation in a patient with metastatic
poorly differentiated epidermoid carcinoma, which was sensitive to
imatinib and achieved a PFS of 6 months (50). Yoh et al identified the L576P
kit mutation in exon 11 of a TC. This mutation was previously
described in GIST to be sensitive to imatinib (51). V559G and Y553N mutations at exon 11
are susceptible to imatinib as well (52,53).
Mutations at exons 13, 14 and 17 seem to be associated with primary
resistance to imatinib. D820E mutation at exon 17 and K642E
mutation at exon 13 confer resistance to imatinib but are sensitive
to sorafenib (54,55). Bisagni et al reported a case
of a TC harboring the mutation D820E at exon 17. The patient was
treated with sorafenib, and the authors reported a partial response
of more than 15 months (54).
Another case with a 577-579del in exon 11 also conferred
sensitivity to sorafenib (56).
Although responses to imatinib have been reported in
those KIT-mutated tumors previously described, no responses
were reported in two phase II trials evaluating the activity of
imatinib in unselected patients or selected only based upon
histologic type (B3 TM or TC), or KIT staining by
immunohistochemistry and not upon genotyping (57,58).
Sorafenib is a multi-target TKI of KIT and other
kinases. As previously described, it demonstrated efficacy in
KIT-mutated tumors (54–56).
It also showed antitumor activity in patients with refractory TCs,
irrespective of the presence of KIT mutations (59–61). A
case series of 5 patients with metastatic pre-treated TC reported
DCR of 80% (PR in 2 patients, SD in 2 patients), and PD in 1
patient (20%) (59). The mPFS and
mOS were 6.4 and 21.2 months, respectively. Of note, the tumor of
only one of the two responding patients harbored a KIT
mutation (D820E at exon 17).
Schirosi et al proposed an interesting and
practical therapeutic algorithm based on the type of KIT
mutations in order to choose the most effective TKI. It seems that
clinical activity of imatinib in TC significantly depends on the
presence and type of c-KIT mutation. On the other hand, sorafenib
and sunitinib seem to be less selective than imatinib and can be
effectively used in TC harboring imatinib-resistant c-KIT mutations
(i.e. in exons 13, 14 and 17) or in wild-type TC due to their
anti-angiogenic activity. Those data are based on small number of
patients and further trials should be designed including
genetically well-characterized populations (62).
PI3K/mTOR inhibitors
Mutations at different levels of the
phosphatidylinositol-3 kinase (PI3K)/AKT/mammalian target of
rapamycin (mTOR) pathway have been observed in both TM and TC and
despite their rarity if taken singularly, when taken together, they
are found in more than 5% of TETs according to the TCGA PanCancer
Atlas (15,63,64).
Therefore, it has been suggested that compounds targeting proteins
of the pathway, such as mTOR or PI3K might have clinical efficacy
in TETs (63–65).
Everolimus, an oral mTOR inhibitor, was evaluated in
a phase II trial, enrolling 32 patients with TM and 19 patients
with TC after at least one previous platinum-based chemotherapy
(66). The study met its primary
endpoint with a DCR of 88% with one patient with TC achieving a CR
and the majority of patients presenting with SD (76% SD, 10% PR, 2%
CR). Further evaluation by histologic type showed that DCR was 94%
in TM (including 3 PRs) and 78% in TC (including 1 CR and 2 PRs).
The mPFS was 16.6 and 5.6 months for TM and TC respectively, and
the mOS was not reached for TM and was 14.7 months for TC. Toxicity
was an important issue since 14 patients developed severe AEs and 3
patients with TM died of drug-related pneumonitis.
An additional immunohistochemical analysis in the
samples of 27 patients of the aforementioned trial revealed two
prognostic biomarkers (positive expression of proteins IGF1-R and
p4E-BP1) but no predictive biomarker for response to everolimus was
identified (66). A study of
next-generation sequencing on tumor samples from a small cohort of
15 pretreated patients with TET who received everolimus did not
identify any predictive biomarkers either (67). Mutations in genes including TP53,
KEAP1 and CDKN2A were observed in 27% of patients,
without association with time to treatment failure (TTF) (67). Recently, in a study suggesting a
molecular classification of TETs using genomic information,
targeted agents were evaluated and in vitro resistance was
noted for everolimus in tumors of TH4 subtype (68). Taking into consideration the limited
antitumor activity, mainly in the form of stabilization of disease
rather than antitumor activity, and the toxicity profile,
everolimus should not be considered as a standard treatment for
patients with TETs.
PI3K inhibitors have been evaluated in preclinical
studies and showed potential efficacy in TETs. In vitro
exposure to the PI3K inhibitor pictilisib inhibited cell viability
and proliferation. However, a phase II study of buparlisib, another
PI3K inhibitor, in relapsed or refractory TMs was closed early
because of high rate of Grade 3–4 AEs (50%) and low efficacy (ORR
of 7.1%) (NCT02220855) (69).
Insulin-like growth factor receptor
(IGFR-1) inhibitors
Zucali et al performed an immunohistochemical
investigation of the insulin-like growth factor 1 receptor (IGF-1R)
in 132 TETs and concluded that higher expression levels of IGF-1R
were significantly correlated with more aggressive histology and
more advanced stage of disease (64). Expression of IGF-1R is common in all
histological subtypes of TETs (70).
The clinical efficacy of cixutumumab, a fully human
monoclonal antibody binding the IGF-1R, was tested in a phase II
study with 49 pre-treated patients with advanced TM and TC
(71). In the TM cohort, only five
out of 37 patients presented a PR, while 28 had SD. In the TC
cohort, none of the 12 patients responded to treatment and only
five had SD. The accrual in the TC cohort closed early due to poor
efficacy. Regarding the toxicity profile, 31% of patients developed
severe AEs, and 2 patients died. The most common grade 3–4 AEs were
hyperglycemia and increased serum lipases. Also, 24% of patients
with TM developed autoimmune disorders during treatment, the most
common being pure red-cell aplasia. In this trial, a significant
increase in IFN-γ expressing CD4+ T cells in blood samples of
patients after treatment, especially among responders, was reported
(71). High toxicity and
insufficient efficacy as monotherapy halted the development of
IGF-1R inhibitors in most solid tumors, and although some activity
was reported in TM, further investigation is unlikely.
Epidermal growth factor receptor
(EGFR) inhibitors
Epidermal growth factor receptor (EGFR) upregulation
is detected and successfully targeted in many solid tumors. While
EGFR overexpression is common in TM and TC and is associated with
poor PFS and OS, EGFR mutations are rare (48,51,72).
Even though clinical activity of anti-EGFR targeted
therapy, such as cetuximab, has been reported in case reports
(73,74), two phase II trials reported poor
efficacy (46,75): in a phase II study of gefitinib
including 26 patients with advanced TM or TC, there was only one
patient with PR as best response. DNA sequencing revealed no
mutations in EGFR exons 18–21 (75). In another phase II trial, 18
patients with advanced TETs were enrolled to determine the effects
of combined treatment with erlotinib plus bevacizumab, but no
objective responses were observed (46). Recently, Zu et al presented a
patient with advanced TC who harbored an EGFR exon 19
deletion and was treated with icotinib. Eventually, the patient had
a complete response for almost 40 months (76).
Cyclin-dependent kinases
inhibitors
Aberrations of cyclin-dependent kinases (CDKs), the
enzymes that strictly control the transition of the cell cycle
machinery, are frequent in solid tumors, leading to abnormal cell
proliferation (77). Inhibition of
CDKs is actively investigated across numerous solid tumors
(78). In the case of TC, deletion
of CDKN2A gene, encoding for CDK2, and loss of p16
expression, an inhibitor of the cell cycle, have been described and
correlated with unfavorable prognosis (79).
Milciclib, an oral CDK inhibitor, was tested in two
phase II trials. The CDKO-125A-006 trial enrolled 72 pre-treated
with only one line of chemotherapy patients with B3 TM (27,8%) or
TC (72,2%). The CDKO-125A-007 trial included 30 patients with B3 TM
(56.7%) or TC (43.3%) who had already received multiple lines of
chemotherapy. ORR was less than 5% in both trials, but DCR was 75.9
and 83.3%. The mPFS and mOS were 6.83 and 24.18 months for the
first study, while mPFS was 9.76 months, and OS was not reached for
the second trial (80).
Recently, the results of a phase II trial of
palbociclib, another CDK4-6 inhibitor, have been reported
(NCT03219554). The population of the study was 48 patients with
advanced TETs who had been treated with one or more lines of
cytotoxic chemotherapy. After a medial follow-up of 14.5 months,
the PFS at 6 months was 60% and the mPFS was 11.0 months. Six of 48
patients (12.5%) achieved PR. The mOS was 26.4 months. The toxicity
profile was overall tolerable (81).
Somatostatin analogues
Somatostatin Receptors (SSTRs) are expressed in
TETs, thus the activity of octreotide, a somatostatin analog, with
and without prednisone has been evaluated by three phase II trials
(82–84). The primary endpoint was the ORR in
each study, and was 37, 31.6, and 88%, respectively. Notably, no
responses were reported in TCs. According to these results,
somatostatin analogues may represent an option in
octreoscan-positive TM.
Histone deacetylase (HDAC)
inhibitors
Interestingly, a comprehensive analysis of
cancer-related genetic alterations among TETs reported frequent
somatic mutations in epigenetic regulatory genes in TC (85). Histone deacetylase (HDAC) are
enzymes that regulate gene expression by altering the chromatin
accessibility state and they represent the most investigated target
of epigenetic therapy.
Belinostat, a HDAC inhibitor, was evaluated alone or
in combination with chemotherapy, in 67 patients with TETs in two
phase II trials (86,87). In the first study, the activity of
belinostat was tested in 41 pretreated patients with advanced TETs
(25 TM and 16 TC). The best response was PR for two (5%) patients
(both with TM), SD for 25 (61%) patients and PD for 13 patients.
The mPFS was 5.8 months (86).
Another phase I/II trial of belinostat, alone and in combination
with CAP chemotherapy in the first-line of metastatic or recurrent
TETs included 26 patients (12 TM and 14 TCs) and demonstrated an
ORR of 64% in patients with TM and 21% in patients with TC
(87). Of note, belinostat showed
immunomodulatory activity, leading to reduction in Tregs and
exhausted CD8 (+) T cell populations in blood samples of patients,
which was associated with efficacy endpoints. Such immunomodulatory
properties of belinostat should be further examined in combination
with immunotherapy (87). Clinical
efficacy in these trials was modest, but additional investigation
is needed.
Exportin-1 (XPO-1) inhibitors
The inactivation of tumor suppressor proteins (TSPs)
is a common pathogenic mechanism of oncogenesis. Exportin-1 (XPO1)
is the main nuclear export receptor for many TSPs involved in
apoptotic signaling and cell-cycle regulation. Inhibition of XPO1
has been proposed as a novel therapeutic strategy. A preclinical
study in models of TETs revealed that XPO1 hyperactivation led to
nuclear exclusion and inactivation of TSPs, whereas its inhibition
could restore TSPs nuclear accumulation and activity (88).
Antitumor activity of selinexor, a selective XPO1
inhibitor, has been reported in 4 patients with TETs in a phase I
trial. One patient presented a PR, and three patients presented SD
(89). Two ongoing phase II trials
are evaluating the activity of selinexor in advanced TETs
(NCT03193437, NCT03466827) but the first one of them was early
terminated due to slow accrual. Table
II summarizes selected clinical trials of targeted agents in
TETs.
 | Table II.Selected published clinical trials of
targeted agents in TETs. |
Table II.
Selected published clinical trials of
targeted agents in TETs.
| First author,
year | Phase | Drug | Patients
(TM/TC) | ORR,
TM/TCa | DCR,
TM/TCa | mPFS,
TM/TCa | mOS,
TM/TCa | Primary
endpoint/Positive or negative trial | (Refs.) |
|---|
| Palmieri et
al, 2002 | II | Octreotide,
prednisone | 16 (10/6) | 37% | 75% | 14 | 15 | ORR/Positive | (83) |
| Loehrer et
al, 2004 | II | Octreotide +/-
prednisone | 38 (32/6) | 37.5%/0% | 67.1% | 8.8/4.5 | NR/23.4 | ORR/Positive (TM)
and negative (TC) | (84) |
| Kirzinger et
al, 2016 | II | Octreotide LAR,
prednisone | 17 (15/2) | 88% | NA | NA | NA | ORR/Positive | (82) |
| Giaccone et
al, 2009 | II | Imatinib | 7 (2/5) | 0% | 100%/0% | 2 | 4 | ORR/Negative | (57) |
| Palmieri et
al, 2012 | II | Imatinib | 15 (12/3) | 0% | 8.3%/0% | 3 | NR | ORR/Negative | (58) |
| Thomas et
al, 2015 | II | Sunitinib | 40 (16/24) | 6%/26% | 81%/91% | 8.5/7.2 | 15.1/NR | ORR/Negative (TM)
and positive (TC) | (35) |
| Kim et al,
2018 | II | Sunitinib | 25 (0/25) | 22% | 92% | 15.2 | NA | ORR/Positive | (37) |
| Sato et al,
2020 | II | Lenvatinib | 42 (0/42) | 38% | 95% | 9.3 | NR | ORR/Positive | (39) |
| Bedano et
al, 2008 | II | Erlotinib,
Bevacizimab | 18 (11/7) | 0% | 60% | NA | NA | ORR/Negative | (46) |
| Kurup et al,
2005 | II | Gefitinib | 26 (19/7) | 3.8% | 58% | NA | NA | ORR/Negative | (75) |
| Zucali et
al, 2018 | II | Everolimus | 51 (32/19) | 11.8% | 94%/78% | 16.6/5.6 | NR/14.7 | ORR/Positive | (66) |
| Abu Zaid et
al, 2022 | II | Buparlisib | 14 (14/0) | 7.1% | 50% | 11.1 | NA | ORR/Negative | (69) |
| Rajan et al,
2014 | II | Cixutumumab | 49 (37/12) | 14%/0% | 89%/42% | 9.9/1.7 | 25.7/8.4 | ORR/Positive (TM)
and negative (TC) | (71) |
| Giaccone et
al, 2011 | II | Belinostat | 41 (25/16) | 8%/0% | 25% | 5.2 | NR/12.4 | ORR/Negative | (86) |
| Thomas et
al, 2014 | I/II | Belinostat,
chemotherapy | 26 (12/14) | 64%/21% | 100%/93% | NR/7.2 | NR/21.4 | ORR/Negative | (87) |
| Besse et al,
2018 | II | Milciclib | 72 (20/52) | 3.7% | 75.9% | 6.8 | 24.1 | 3-month
PFS/Positive | (80) |
| Besse et al,
2018 | II | Milciclib | 30 (17/13) | 4.2% | 83.3% | 9.8 | NR | 3-month
PFS/Positive | (80) |
| Ahn et al,
2021 | II | Palbociclib | 48 (25/23) | 12.5% | NA | 11 | 26.4 | 6-month
PFS/Positive | (81) |
| Abdul Razak et
al, 2016 | I | Selinexor | 4 (4/0) | 25% | 100% | NA | NA | NA | (89) |
Discussion
TETs are rare malignancies with limited therapeutic
options. Recent research advances in TETs involve their
comprehensive genomic characterization, including the TCGA project,
and the exploration of their immune microenvironment; however, the
relative importance of their pathogenic mechanisms remains elusive.
Cytotoxic chemotherapy is the recommended approach for first-line
therapy. Our literature review revealed that clinical investigation
is active, mainly for subsequent lines of treatment, mainly
involving immunotherapeutic or targeted agents.
ICIs have shown clinical activity in relapsed and
refractory TETs. Second-line pembrolizumab has shown encouraging
efficacy results with high response rates in TC (24,25).
Responders also seem to have sustained clinical benefit with long
term follow-up. Toxicity is a significant issue when treating TETs
with ICIs, given the susceptibility of those patients to
autoimmunity. ICIs should be avoided in patients with preexisting
autoimmune disorders until risk mitigation strategies are
established. Biomarkers for identification of individuals at risk
for irAEs are under investigation. Treatment with ICIs is
preferable to be administered in the context of a clinical
trial.
Anti-angiogenic TKIs have been tested in phase II
trials with lenvatinib reporting efficacy for TC with a remarkable
ORR. Sunitinib has also showed high response rate and could
constitute a promising alternative. Though cross-trial comparison,
which should be done with caution and with its limitations, it has
been assumed that lenvatinib achieved a higher response rate as
compared to other compounds, with a better toxicity profile
(35,37,38).
This could be due to differences in pharmacodynamics features, with
lenvatinib being a more potent inhibitor of several tyrosine kinase
receptors including VEGFR2.
Since preclinical and clinical data suggest that the
combination of immunotherapy with anti-angiogenic therapy may have
a synergistic antitumor effect in other solid tumors, this
combination is being evaluated in TETs. Two phase II trials are
assessing the combination of pembrolizumab with sunitinib or
Lenvatinib in patients with TC (NCT03463460, NCT04710628). Another
phase I/II study will evaluate the combination of the oral
VEGFR/PDGFR TKI vorolanib with nivolumab in patients with thoracic
malignancies, including TC (NCT03583086).
Recent research has led to the identification of
specific molecular alterations associated with TETs, some of them
being relatively rare among other neoplasms-e.g. the
mutations in GFT2I gene- and some of them being targetable,
such as the overexpression of the tyrosine kinase receptors c-KIT,
EGFR, IGFR (15,47). Nevertheless, the clinical activity
of the relevant targeted agents is modest. Such results could
indicate the unknown implicated mechanisms and the need to
elucidate the oncogenic potential of each independent alteration.
In addition, several molecular alterations are not currently
targetable, highlighting the need for novel drug development. It
should also be noted that TETs are heterogeneous tumors with
distinctive pathogenic mechanisms and a unified management approach
is quite challenging. However, the rarity of the cases hinders the
accumulation of evidence for different subtypes of TETs.
The identification of predictive markers to define
patients who could have a maximum benefit of a specific treatment
is a priority. TETs are rare tumors and thus, a clever strategy
might be the inclusion of patients in basket trials of targeted
agents being investigated across different malignancies with
similar molecular characteristics. SPECTA-lung (NCT02214134) is a
pan-European program with the objective to screen patients with
thoracic tumors (lung cancer, malignant pleural mesothelioma, TM or
TC) to collect the molecular characteristics of the neoplasms and
offer access to targeted clinical trials.
Conclusions
TETs are rare malignancies with scarce therapeutic
options regarding their systemic treatment. Both immunotherapy and
targeted therapy are currently under investigation, but the
unraveling of the specific subset of patients that may benefit with
each approach requires even more thorough understanding of the
complex immune-related mechanisms and comprehensive molecular
characterization of the tumors as well as pertinent clinical
trials' design for rare disease entities.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
AD performed the literature review and wrote the
original manuscript, GG, IT, EP, ED and NS wrote the revised
manuscript and prepared the figure. EK interpreted the data,
critically revised the manuscript and supervised the work. Data
authentication is not applicable. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
TET
|
thymic epithelial tumors
|
|
irAE
|
immune-related adverse events
|
|
EGFR
|
epidermal growth factor receptor
|
|
IGFR
|
insulin-like growth factor
receptor
|
|
PI3K
|
phosphatidylinositol-3 kinase
|
|
mTOR
|
mammalian target of rapamycin
|
|
CDK
|
cyclin dependent kinase
|
|
HDAC
|
histone deacetylase
|
References
|
1
|
Marx A, Chan JKC, Chalabreysse L, Dacic S,
Detterbeck F, French CA, Hornick JL, Inagaki H, Jain D, Lazar AJ,
et al: The 2021 WHO classification of tumors of the thymus and
mediastinum: What is new in thymic epithelial, germ cell, and
mesenchymal tumors? J Thorac Oncol. 17:200–213. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Detterbeck FC, Stratton K, Giroux D,
Asamura H, Crowley J, Falkson C, Filosso PL, Frazier AA, Giaccone
G, Huang J, et al: The IASLC/ITMIG thymic epithelial tumors staging
project: Proposal for an evidence-based stage classification system
for the forthcoming (8th) edition of the TNM classification of
malignant tumors. J Thorac Oncol. 9 (9 Suppl 2):S65–S72. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Detterbeck FC, Nicholson AG, Kondo K, Van
Schil P and Moran C: The Masaoka-Koga stage classification for
thymic malignancies: Clarification and definition of terms. J
Thorac Oncol. 6 (7 Suppl 3):S1710–S1716. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Girard N, Ruffini E, Marx A, Faivre-Finn C
and Peters S; ESMO Guidelines Committee, : Thymic epithelial
tumours: ESMO clinical practice guidelines for diagnosis, treatment
and follow-up. Ann Oncol. 26 (Suppl 5):v40–v55. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ettinger DS, Wood DE, Aisner DL, Akerley
W, Bauman JR, Bharat A, Bruno DS, Chang JY, Chirieac LR, D'Amico
TA, et al: NCCN guidelines insights: Non-small cell lung cancer,
version 2.2021. J Natl Compr Canc Netw. 19:254–266. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Conforti F, Pala L, Giaccone G and De Pas
T: Thymic epithelial tumors: From biology to treatment. Cancer
Treat Rev. 86:1020142020. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Masaoutis C, Palamaris K, Kokkali S,
Levidou G and Theocharis S: Unraveling the immune microenvironment
of thymic epithelial tumors: Implications for autoimmunity and
treatment. Int J Mol Sci. 23:78642022. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kondo K, Ohigashi I and Takahama Y: Thymus
machinery for T-cell selection. Int Immunol. 31:119–125. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Takaba H and Takayanagi H: The mechanisms
of T cell selection in the thymus. Trends Immunol. 38:805–816.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Anderson MS and Su MA: AIRE expands: New
roles in immune tolerance and beyond. Nat Rev Immunol. 16:247–258.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Iberg CA, Jones A and Hawiger D: Dendritic
cells as inducers of peripheral tolerance. Trends Immunol.
38:793–804. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Owen DL, Sjaastad LE and Farrar MA:
Regulatory T cell development in the thymus. J Immunol.
203:2031–2041. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Weksler B and Lu B: Alterations of the
immune system in thymic malignancies. J Thorac Oncol. 9 (9 Suppl
2):S137–S142. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Boucher M, Dansin E, Kerjouan M, Mazieres
J, Pichon E, Thillays F, Massard G, Quantin X, Youssef O, Westeel
V, et al: OA 03.01 prevalence of autoimmune diseases in thymic
epithelial tumors (TET) insights from RYTHMIC. J Thorac Oncol. 12
(Suppl 2):S1748–S1749. 2017. View Article : Google Scholar
|
|
15
|
Radovich M, Pickering CR, Felau I, Ha G,
Zhang H, Jo H, Hoadley KA, Anur P, Zhang J, McLellan M, et al: The
integrated genomic landscape of thymic epithelial tumors. Cancer
Cell. 33:244–258.e10. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tateo V, Manuzzi L, De Giglio A, Parisi C,
Lamberti G, Campana D and Pantaleo MA: Immunobiology of thymic
epithelial tumors: Implications for immunotherapy with immune
checkpoint inhibitors. Int J Mol Sci. 21:90562020. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Marchevsky AM and Walts AE: PD-L1, PD-1,
CD4, and CD8 expression in neoplastic and nonneoplastic thymus. Hum
Pathol. 60:16–23. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Weissferdt A, Fujimoto J, Kalhor N,
Rodriguez J, Bassett R, Wistuba II and Moran CA: Expression of PD-1
and PD-L1 in thymic epithelial neoplasms. Mod Pathol. 30:826–833.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Owen D, Chu B, Lehman AM, Annamalai L,
Yearley JH, Shilo K and Otterson GA: Expression patterns,
prognostic value, and intratumoral heterogeneity of PD-L1 and PD-1
in thymoma and thymic carcinoma. J Thorac Oncol. 13:1204–1212.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yokoyama S, Miyoshi H, Nishi T, Hashiguchi
T, Mitsuoka M, Takamori S, Akagi Y, Kakuma T and Ohshima K:
Clinicopathologic and prognostic implications of programmed death
ligand 1 expression in thymoma. Ann Thorac Surg. 101:1361–1369.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Padda SK, Riess JW, Schwartz EJ, Tian L,
Kohrt HE, Neal JW, West RB and Wakelee HA: Diffuse high intensity
PD-L1 staining in thymic epithelial tumors. J Thorac Oncol.
10:500–508. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yokoyama S, Miyoshi H, Nakashima K,
Shimono J, Hashiguchi T, Mitsuoka M, Takamori S, Akagi Y and
Ohshima K: Prognostic value of programmed death ligand 1 and
programmed death 1 expression in thymic carcinoma. Clin Cancer Res.
22:4727–4734. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Arbour KC, Naidoo J, Steele KE, Ni A,
Moreira AL, Rekhtman N, Robbins PB, Karakunnel J, Rimner A, Huang
J, et al: Expression of PD-L1 and other immunotherapeutic targets
in thymic epithelial tumors. PLoS One. 12:e01826652017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Giaccone G, Kim C, Thompson J, McGuire C,
Kallakury B, Chahine JJ, Manning M, Mogg R, Blumenschein WM, Tan
MT, et al: Pembrolizumab in patients with thymic carcinoma: A
single-arm, single-centre, phase 2 study. Lancet Oncol. 19:347–355.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Giaccone G and Kim C: Durable response in
patients with thymic carcinoma treated with pembrolizumab after
prolonged follow-up. J Thorac Oncol. 16:483–485. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Cho J, Kim HS, Ku BM, Choi YL, Cristescu
R, Han J, Sun JM, Lee SH, Ahn JS, Park K and Ahn MJ: Pembrolizumab
for patients with refractory or relapsed thymic epithelial tumor:
An open-label phase II trial. J Clin Oncol. 37:2162–2170. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Rajan A, Heery CR, Thomas A, Mammen AL,
Perry S, O'Sullivan Coyne G, Guha U, Berman A, Szabo E, Madan RA,
et al: Efficacy and tolerability of anti-programmed death-ligand 1
(PD-L1) antibody (Avelumab) treatment in advanced thymoma. J
Immunother Cancer. 7:2692019. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Mammen AL, Rajan A, Pak K, Lehky T,
Casciola-Rosen L, Donahue RN, Lepone LM, Zekeridou A, Pittock SJ,
Hassan R, et al: Pre-existing antiacetylcholine receptor
autoantibodies and B cell lymphopaenia are associated with the
development of myositis in patients with thymoma treated with
avelumab, an immune checkpoint inhibitor targeting programmed
death-ligand 1. Ann Rheum Dis. 78:150–152. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Katsuya Y, Horinouchi H, Seto T, Umemura
S, Hosomi Y, Satouchi M, Nishio M, Kozuki T, Hida T, Sukigara T, et
al: Single-arm, multicentre, phase II trial of nivolumab for
unresectable or recurrent thymic carcinoma: PRIMER study. Eur J
Cancer. 113:78–86. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ak N and Aydiner A: Nivolumab treatment
for metastatic thymic epithelial tumors. J Oncol Pharm Pract.
27:1710–1715. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lattanzio R, La Sorda R, Facciolo F,
Sioletic S, Lauriola L, Martucci R, Gallo E, Palmieri G, Evoli A,
Alessandrini G, et al: Thymic epithelial tumors express vascular
endothelial growth factors and their receptors as potential targets
of antiangiogenic therapy: A tissue micro array-based multicenter
study. Lung Cancer. 85:191–196. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Cimpean AM, Raica M, Encica S, Cornea R
and Bocan V: Immunohistochemical expression of vascular endothelial
growth factor A (VEGF), and its receptors (VEGFR1, 2) in normal and
pathologic conditions of the human thymus. Ann Anat. 190:238–245.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Cimpean AM, Ceausu R, Encică S, Gaje PN,
Ribatti D and Raica M: Platelet-derived growth factor and
platelet-derived growth factor receptor-α expression in the normal
human thymus and thymoma. Int J Exp Pathol. 92:340–344. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Janik S, Bekos C, Hacker P, Raunegger T,
Schiefer AI, Müllauer L, Veraar C, Dome B, Klepetko W, Ankersmit HJ
and Moser B: Follistatin impacts tumor angiogenesis and outcome in
thymic epithelial tumors. Sci Rep. 9:173592019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Thomas A, Rajan A, Berman A, Tomita Y,
Brzezniak C, Lee MJ, Lee S, Ling A, Spittler AJ, Carter CA, et al:
Sunitinib in patients with chemotherapy-refractory thymoma and
thymic carcinoma: An open-label phase 2 trial. Lancet Oncol.
16:177–186. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Rajan A, Kim C, Guha U, Szabo E, Berman A,
Sciuto L, Spittler AJ, Trepel J, Steinberg S, Harris P, et al:
OA18.02 evaluation of a modified dosing regimen (2-weeks
on/1-week off) of sunitinib as part of a phase II trial in thymic
carcinoma. J Thorac Oncol. 12 (Suppl):S313–S314. 2017. View Article : Google Scholar
|
|
37
|
Kim SH, Kim YJ, Ock C, Kim M, Keam B, Kim
TM, Kim D, Heo DS and Lee JS: OA11.05 phase II study of sunitinib
in patients with thymic carcinoma previously treated with
platinum-based chemotherapy (KOSMIC trial). J Thorac Oncol. 13
(Suppl):S346–S347. 2018. View Article : Google Scholar
|
|
38
|
Remon J, Girard N, Mazieres J, Dansin E,
Pichon E, Greillier L, Dubos C, Lindsay CR and Besse B: Sunitinib
in patients with advanced thymic malignancies: Cohort from the
French RYTHMIC network. Lung Cancer. 97:99–104. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Sato J, Satouchi M, Itoh S, Okuma Y, Niho
S, Mizugaki H, Murakami H, Fujisaka Y, Kozuki T, Nakamura K, et al:
Lenvatinib in patients with advanced or metastatic thymic carcinoma
(REMORA): A multicentre, phase 2 trial. Lancet Oncol. 21:843–850.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Xie C, Wan X, Quan H, Zheng M, Fu L, Li Y
and Lou L: Preclinical characterization of anlotinib, a highly
potent and selective vascular endothelial growth factor receptor-2
inhibitor. Cancer Sci. 109:1207–1219. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Lin B, Song X, Yang D, Bai D, Yao Y and Lu
N: Anlotinib inhibits angiogenesis via suppressing the activation
of VEGFR2, PDGFRβ and FGFR1. Gene. 654:77–86. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Zuo R, Zhang C, Lin L, Meng Z, Wang Y, Su
Y, Abudurazik M, Du Y and Chen P: Durable efficacy of anlotinib in
a patient with advanced thymic squamous cell carcinoma after
multiline chemotherapy and apatinib: A case report and literature
review. Thorac Cancer. 11:3383–3387. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Yudong S, Zhaoting M, Xinyue W, Li L,
Xiaoyan X, Ran Z, Jinliang C and Peng C: EGFR exon 20 insertion
mutation in advanced thymic squamous cell carcinoma: Response to
apatinib and clinical outcomes. Thorac Cancer. 9:885–891. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Besse B, Girard N, Gazzah A, Hierro C,
Tabernero J, Debraud F, Camboni G, Dubois F, Leger C, Legrand F, et
al: Clinical activity of lucitanib in advanced thymic epithelial
tumours. J Thorac Oncol. 10:S3532015.
|
|
45
|
Perrino M, De Pas T, Bozzarelli S,
Giordano L, De Vincenzo F, Conforti F, Digiacomo N, Cordua N,
D'Antonio F, Borea F, et al: Resound trial: A phase 2 study of
regorafenib in patients with thymoma (type B2-B3) and thymic
carcinoma previously treated with chemotherapy. Cancer.
128:719–726. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Bedano PM, Perkins S, Burns M, Kessler K,
Nelson R, Schneider BP, Risley L, Dropcho S and Loehrer PJ: A phase
II trial of erlotinib plus bevacizumab in patients with recurrent
thymoma or thymic carcinoma. J Clin Oncol. 26 (15
Suppl):S190872008. View Article : Google Scholar
|
|
47
|
Tateo V, Manuzzi L, Parisi C, De Giglio A,
Campana D, Pantaleo MA and Lamberti G: An overview on molecular
characterization of thymic tumors: Old and new targets for clinical
advances. Pharmaceuticals (Basel). 14:3162021. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Girard N, Shen R, Guo T, Zakowski MF,
Heguy A, Riely GJ, Huang J, Lau C, Lash AE, Ladanyi M, et al:
Comprehensive genomic analysis reveals clinically relevant
molecular distinctions between thymic carcinomas and thymomas. Clin
Cancer Res. 15:6790–6799. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Petrini I, Zucali PA, Lee HS, Pineda MA,
Meltzer PS, Walter-Rodriguez B, Roncalli M, Santoro A, Wang Y and
Giaccone G: Expression and mutational status of c-kit in thymic
epithelial tumors. J Thorac Oncol. 5:1447–1453. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Ströbel P, Hartmann M, Jakob A, Mikesch K,
Brink I, Dirnhofer S and Marx A: Thymic carcinoma with
overexpression of mutated KIT and the response to imatinib. N Engl
J Med. 350:2625–2626. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Yoh K, Nishiwaki Y, Ishii G, Goto K,
Kubota K, Ohmatsu H, Niho S, Nagai K and Saijo N: Mutational status
of EGFR and KIT in thymoma and thymic carcinoma. Lung Cancer.
62:316–320. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Hirai F, Edagawa M, Shimamatsu S, Toyozawa
R, Toyokawa G, Nosaki K, Yamaguchi M, Seto T, Twakenoyama M and
Ichinose Y: c-kit mutation-positive advanced thymic carcinoma
successfully treated as a mediastinal gastrointestinal stromal
tumor: A case report. Mol Clin Oncol. 4:527–529. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Buti S, Donini M, Sergio P, Garagnani L,
Schirosi L, Passalacqua R and Rossi G: Impressive response with
imatinib in a heavily pretreated patient with metastatic c-KIT
mutated thymic carcinoma. J Clin Oncol. 29:e803–e805. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Bisagni G, Rossi G, Cavazza A, Sartori G,
Gardini G and Boni C: Long lasting response to the multikinase
inhibitor bay 43–9006 (sorafenib) in a heavily pretreated
metastatic thymic carcinoma. J Thorac Oncol. 4:773–775. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Catania C, Conforti F, Spitaleri G,
Barberis M, Preda L, Noberasco C, Lazzari C, Toffalorio F, de
Marinis F, Manzotti M and De Pas TM: Antitumor activity of
sorafenib and imatinib in a patient with thymic carcinoma harboring
c-KIT exon 13 missense mutation K642E. Onco Targets Ther.
7:697–702. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Dişel U, Oztuzcu S, Beşen AA, Karadeniz C,
Köse F, Sümbül AT, Sezer A, Nursal GN, Abalı H and Ozyılkan O:
Promising efficacy of sorafenib in a relapsed thymic carcinoma with
C-KIT exon 11 deletion mutation. Lung Cancer. 71:109–112. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Giaccone G, Rajan A, Ruijter R, Smit E,
van Groeningen C and Hogendoorn PC: Imatinib mesylate in patients
with WHO B3 thymomas and thymic carcinomas. J Thorac Oncol.
4:1270–1273. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Palmieri G, Marino M, Buonerba C, Federico
P, Conti S, Milella M, Petillo L, Evoli A, Lalle M, Ceribelli A, et
al: Imatinib mesylate in thymic epithelial malignancies. Cancer
Chemother Pharmacol. 69:309–315. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Pagano M, Sierra NM, Panebianco M, Rossi
G, Gnoni R, Bisagni G and Boni C: Sorafenib efficacy in thymic
carcinomas seems not to require c-KIT or PDGFR-alpha mutations.
Anticancer Res. 34:5105–5110. 2014.PubMed/NCBI
|
|
60
|
Neuhaus T and Luyken J: Long lasting
efficacy of sorafenib in a heavily pretreated patient with thymic
carcinoma. Target Oncol. 7:247–251. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Li XF, Chen Q, Huang WX and Ye YB:
Response to sorafenib in cisplatin-resistant thymic carcinoma: A
case report. Med Oncol. 26:157–160. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Schirosi L, Nannini N, Nicoli D, Cavazza
A, Valli R, Buti S, Garagnani L, Sartori G, Calabrese F, Marchetti
A, et al: Activating c-KIT mutations in a subset of thymic
carcinoma and response to different c-KIT inhibitors. Ann Oncol.
23:2409–2414. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Alberobello AT, Wang Y, Beerkens FJ,
Conforti F, McCutcheon JN, Rao G, Raffeld M, Liu J, Rahhal R, Zhang
YW and Giaccone G: PI3K as a potential therapeutic target in thymic
epithelial tumors. J Thorac Oncol. 11:1345–1356. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Zucali PA, Petrini I, Lorenzi E, Merino M,
Cao L, Di Tommaso L, Lee HS, Incarbone M, Walter BA, Simonelli M,
et al: Insulin-like growth factor-1 receptor and phosphorylated
AKT-serine 473 expression in 132 resected thymomas and thymic
carcinomas. Cancer. 116:4686–4695. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Maury JM, Merveilleux du Vignaux C, Drevet
G, Zarza V, Chalabreysse L, Maisse C, Gineys B, Dolmazon C, Tronc
F, Girard N and Leroux C: Activation of the mTOR/Akt pathway in
thymic epithelial cells derived from thymomas. PLoS One.
14:e01976552019. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Zucali PA, De Pas T, Palmieri G, Favaretto
A, Chella A, Tiseo M, Caruso M, Simonelli M, Perrino M, De Vincenzo
F, et al: Phase II study of everolimus in patients with thymoma and
thymic carcinoma previously treated with cisplatin-based
chemotherapy. J Clin Oncol. 36:342–349. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Hellyer JA, Ouseph MM, Padda SK and
Wakelee HA: Everolimus in the treatment of metastatic thymic
epithelial tumors. Lung Cancer. 149:97–102. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Padda SK, Gökmen-Polar Y, Hellyer JA,
Badve SS, Singh NK, Vasista SM, Basu K, Kumar A and Wakelee HA:
Genomic clustering analysis identifies molecular subtypes of thymic
epithelial tumors independent of World Health Organization
histologic type. Oncotarget. 12:1178–1186. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Abu Zaid MI, Radovich M, Althouse S, Liu
H, Spittler AJ, Solzak J, Badve S and Loehrer PJ Sr: A phase II
study of buparlisib in relapsed or refractory thymomas. Front
Oncol. 12:8913832022. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Girard N, Teruya-Feldstein J, Payabyab EC,
Riely GJ, Rusch VW, Kris MG and Zakowski MF: Insulin-like growth
factor-1 receptor expression in thymic malignancies. J Thorac
Oncol. 5:1439–1446. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Rajan A, Carter CA, Berman A, Cao L, Kelly
RJ, Thomas A, Khozin S, Chavez AL, Bergagnini I, Scepura B, et al:
Cixutumumab for patients with recurrent or refractory advanced
thymic epithelial tumours: A multicentre, open-label, phase 2
trial. Lancet Oncol. 15:191–200. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Sakane T, Murase T, Okuda K, Saida K,
Masaki A, Yamada T, Saito Y, Nakanishi R and Inagaki H: A mutation
analysis of the EGFR pathway genes, RAS, EGFR, PIK3CA, AKT1 and
BRAF, and TP53 gene in thymic carcinoma and thymoma type A/B3.
Histopathology. 75:755–766. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Farina G, Garassino MC, Gambacorta M, La
Verde N, Gherardi G and Scanni A: Response of thymoma to cetuximab.
Lancet Oncol. 8:449–450. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Palmieri G, Marino M, Salvatore M,
Budillon A, Meo G, Caraglia M and Montella L: Cetuximab is an
active treatment of metastatic and chemorefractory thymoma. Front
Biosci. 12:757–761. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
75
|
Kurup A, Burns M, Dropcho S, Pao W and
Loehrer PJ: Phase II study of gefitinib treatment in advanced
thymic malignancies. J Clin Oncol. 23 (16 Suppl):S70682005.
View Article : Google Scholar
|
|
76
|
Zu Y, Luo Y, Li C, Zhao J, He T, Shi X and
Li X: Complete remission following icotinib administration in an
advanced ectopic thymic carcinoma patient harbouring the EGFR exon
19 deletion. J Gene Med. 23:e33402021. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Gomatou G, Trontzas I, Ioannou S, Drizou
M, Syrigos N and Kotteas E: Mechanisms of resistance to
cyclin-dependent kinase 4/6 inhibitors. Mol Biol Rep. 48:915–925.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Panagiotou E, Gomatou G, Trontzas IP,
Syrigos N and Kotteas E: Cyclin-dependent kinase (CDK) inhibitors
in solid tumors: A review of clinical trials. Clin Transl Oncol.
24:161–192. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Aesif SW, Aubry MC, Yi ES, Kloft-Nelson
SM, Jenkins SM, Spears GM, Greipp PT, Sukov WR and Roden AC: Loss
of p16INK4A expression and homozygous CDKN2A deletion
are associated with worse outcome and younger age in thymic
carcinomas. J Thorac Oncol. 12:860–871. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Besse B, Garassino MC, Rajan A, Novello S,
Mazieres J, Weiss GJ, Kocs DM, Barnett JM, Davite C, Crivori P and
Giaccone G: Efficacy of milciclib (PHA-848125AC), a pan-cyclin
d-dependent kinase inhibitor, in two phase II studies with thymic
carcinoma (TC) and B3 thymoma (B3T) patients. J Clin Oncol. 36 (15
Suppl):S85192018. View Article : Google Scholar
|
|
81
|
Ahn MJ, Jung HA, Kim M, Kim JH, Choi YH,
Cho J, Park JH, Park KU, Park S, Sun JM, et al: A phase II study of
palbociclib for recurrent or refractory advanced thymic epithelial
tumor (KCSG LU17-21). J Clin Oncol. 39 (15 Suppl):S85762021.
View Article : Google Scholar
|
|
82
|
Kirzinger L, Boy S, Marienhagen J,
Schuierer G, Neu R, Ried M, Hofmann HS, Wiebe K, Ströbel P, May C,
et al: Octreotide LAR and prednisone as neoadjuvant treatment in
patients with primary or locally recurrent unresectable thymic
tumors: A phase II study. PLoS One. 11:e01682152016. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Palmieri G, Montella L, Martignetti A,
Muto P, Di Vizio D, De Chiara A and Lastoria S: Somatostatin
analogs and prednisone in advanced refractory thymic tumors.
Cancer. 94:1414–1420. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Loehrer PJ Sr, Wang W, Johnson DH, Aisner
SC and Ettinger DS; Eastern Cooperative Oncology Group Phase II
Trial, : Octreotide alone or with prednisone in patients with
advanced thymoma and thymic carcinoma: An eastern cooperative
oncology group phase II trial. J Clin Oncol. 22:293–299. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Wang Y, Thomas A, Lau C, Rajan A, Zhu Y,
Killian JK, Petrini I, Pham T, Morrow B, Zhong X, et al: Mutations
of epigenetic regulatory genes are common in thymic carcinomas. Sci
Rep. 4:73362014. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Giaccone G, Rajan A, Berman A, Kelly RJ,
Szabo E, Lopez-Chavez A, Trepel J, Lee MJ, Cao L, Espinoza-Delgado
I, et al: Phase II study of belinostat in patients with recurrent
or refractory advanced thymic epithelial tumors. J Clin Oncol.
29:2052–2059. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Thomas A, Rajan A, Szabo E, Tomita Y,
Carter CA, Scepura B, Lopez-Chavez A, Lee MJ, Redon CE, Frosch A,
et al: A phase I/II trial of belinostat in combination with
cisplatin, doxorubicin, and cyclophosphamide in thymic epithelial
tumors: A clinical and translational study. Clin Cancer Res.
20:5392–5402. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Conforti F, Zhang X, Rao G, De Pas T,
Yonemori Y, Rodriguez JA, McCutcheon JN, Rahhal R, Alberobello AT,
Wang Y, et al: Therapeutic effects of XPO1 inhibition in thymic
epithelial tumors. Cancer Res. 77:5614–5627. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Abdul Razak AR, Mau-Soerensen M, Gabrail
NY, Gerecitano JF, Shields AF, Unger TJ, Saint-Martin JR, Carlson
R, Landesman Y, McCauley D, et al: First-in-class, first-in-human
phase I study of selinexor, a selective inhibitor of nuclear
export, in patients with advanced solid tumors. J Clin Oncol.
34:4142–4150. 2016. View Article : Google Scholar : PubMed/NCBI
|