Introduction
A colovesical fistula (CVF), a communication between
the colon and bladder, is a known but rare complication of colon
cancer (1–3), and it can occur secondary to other
diseases (4). The prognosis of CVF
is poor, and is often accompanied by uremia, septicemia and even
renal failure (5). If CVF could be
detected in the early stage of the disease, the poor prognosis of
CVF may be changed. However, due to the rarity of CVF, the
non-specificity of the symptoms (6), signs and imaging examination findings
(7), and the poor prognosis, it is
challenging and yet crucial to confirm CVF early. Currently,
considerable debate exists in the literature on the choice of the
initial diagnostic study (6); there
is no single optimal test and the investigations employed vary. We
recommend computed tomography (CT) as the primary imaging
investigation in a suspected CVF. In the present study, the case
database of Yangzhou First People's Hospital (Yangzhou, China) was
reviewed, and out of a total of 39 suspected cases, four cases of
CVF with different grades of disease and different prognoses were
identified for discussion. The present study was approved by the
Ethics Committee of Yangzhou First People's Hospital and written
informed consent for future publication was obtained from all
patients, including the patient who died.
Case report
Case one
A 59-year-old man presented to the Affiliated
Hospital of Yangzhou University (Yangzhou, China) on 30 July 2020
with abdominal pain and distention accompanied by cessation of anal
gas and defecation that had persisted for 3 days. The patient had
recurrent colon cancer and had previously undergone a radical
resection of colon cancer. The patient was afebrile with normal
vital signs. A routine blood test showed a neutrophil level of
87.1×109/l (reference range, 0.04-0.5×109/l).
A routine urine test showed a red blood cell level of 3/high-power
field (HPF) (reference range, 0/HPF). A kidney function test showed
a creatinine level of 130.2 µmol/l (reference range, 50–110
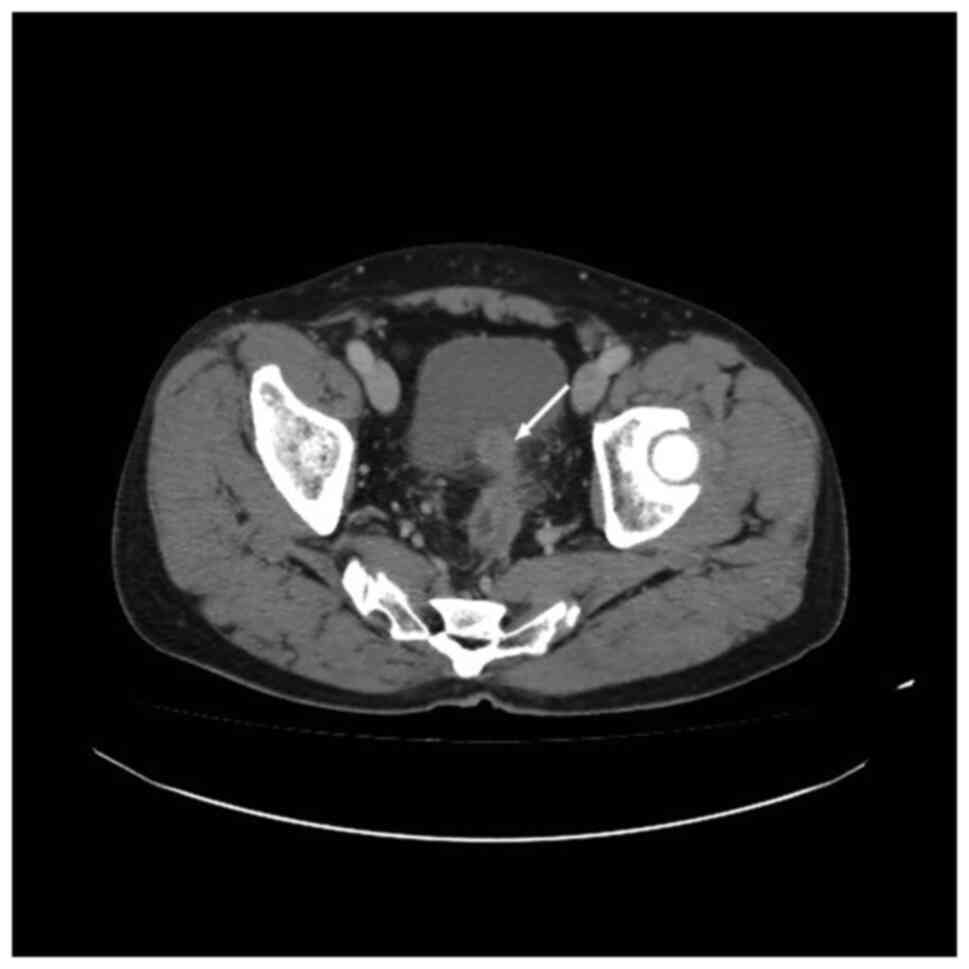
µmol/l). CT revealed recurrence of the colon cancer, with invasion
in the left posterior bladder wall, and gas in the ascending and
sigmoid colon (Fig. 1). The
diagnosis was colon cancer with a CVF. The patient refused surgical
treatment and was treated with 0.5 g levofloxacin, once a day for
10–14 days. The symptom of lower abdominal pain remained 11 months
later.
The final pathological diagnosis was sigmoid colon
cancer. According to the American Joint Committee on Cancer
Tumor-Node-Metastasis (AJCC TNM) classification (8), the patient was diagnosed with stage
T4N0M0 disease, indicating intermediate-grade colon cancer.
Case two
An 84-year-old man presented to the Affiliated
Hospital of Yangzhou University in April 2015, with urinary
frequency and urgency that had persisted for 2 days. On
presentation, the patient was afebrile with normal vital signs. A
routine blood test showed a hemoglobin level of 84 g/l (reference
range, 100–160 g/l) and a neutrophil level of 81.1×109/l
(reference range, 0.04-0.5×109/l). A routine urine test
showed a red blood cell level of 2,452.2/HPF (reference range,
0–3/HPF) and a white blood cell level of 15,619.2/HPF (reference
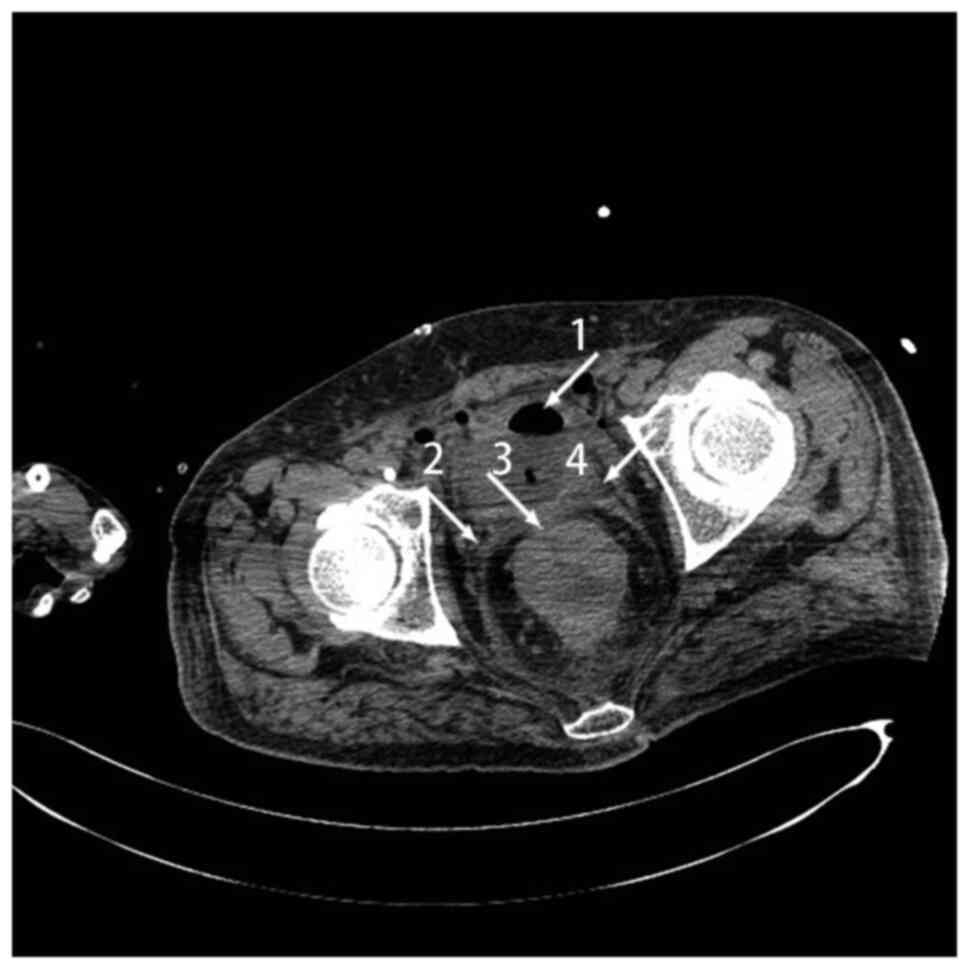
range, 0–5/HPF). CT revealed thickening in the sigmoid colon,
rectum and bladder wall, which was considered to be colon cancer,
and air in the bladder (Fig. 2).
The diagnosis was colon cancer with a CVF. The patient refused
surgical treatment and was treated with levofloxacin 0.5 g once,
once a day, for 10 to 14 days. The subsequent clinical course was
marked by deterioration, and the patient died due to the CVF 2
months later.
According to the AJCC TNM classification, the
patient was diagnosed with stage T4N0M0 disease, indicating
low-grade colon cancer.
Case three
A 45-year-old man presented to the Affiliated
Hospital of Yangzhou University in June 2020 with fecaluria that
had persisted for 1 month. The patient had a background of colon
cancer. On presentation, the patient was afebrile with normal vital
signs. A routine blood test showed a hemoglobin level of
57×1012 g/l (reference range, 100–160×1012
g/l), neutrophils of 9.81×109 g/l (reference range,
0.04-0.5×109 g/l). A routine urine test showed a red
blood cell level of 3/HPF (reference range, 0–3/HPF). A liver
function test showed a creatinine level of 380 µmol/l (reference
range, 50–110 µmol/l) and urea nitrogen level of 42.65 mmol/l
(reference range, 2.86-7.14 mmol/l). Cystoscopy showed cloudy urine
and fecal scraps in the bladder. Enteroscopy revealed multiple
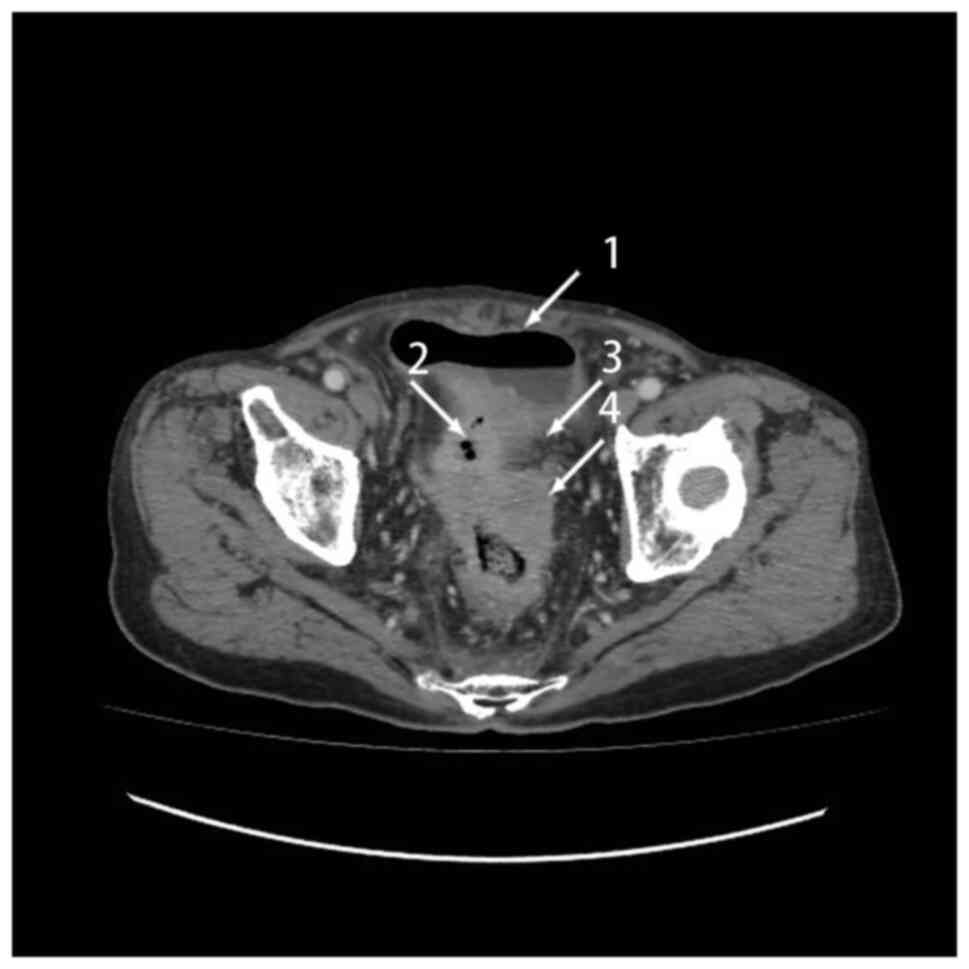
tumors 10 cm above the anus. CT showed uneven thickening, with
enhancement in the distal regions of the sigmoid colon and proximal
regions of the rectum wall, which was colon cancer and a fistula
(Fig. 3). The diagnosis was colon
cancer with a CVF. The patient was treated with 0.5 g levofloxacin,
once a day for 10–14 days. Due to the patient's good physical
condition and lack of obvious manifestations of inflammation or
intestinal obstruction, the patient underwent a palliative
sigmoidectomy, proximal colostomy, partial small intestine
resection and partial cystectomy, and was lost to follow-up
subsequent to a period of 5 months.
The tumor was formed of infiltrating extra-muscular
fibrous adipose tissue. A total of eight metastatic tumors were
indicated in the peri-intestinal lymph node. The final pathological
diagnosis was of sigmoid colon cancer. According to the AJCC TNM
classification, the patient was diagnosed with stage T4N3M0
disease, indicating low-grade colon cancer.
Case four
A 55-year-old man presented to the Affiliated
Hospital of Yangzhou University in December 2020 with urinary
frequency, urgency and pain that had persisted for 4 months. The
patient had a background of sigmoid cancer. On presentation, the
patient was afebrile with normal vital signs. A routine blood test
showed a neutrophil level of 87.1×109 g/l (reference
range, 0.04-0.5 ×109 g/l), a hemoglobin level of
84×1012 g/l (reference range, 120–160 g/l). A routine
urine test showed a red blood cell level of 3/HPF (reference range,
0–3/HPF) and a white blood cell level of 139.8/HPF (reference
range, 0–5/HPF). The urine culture found Escherichia coli,
and the fecal occult blood test was positive. CT showed sigmoid
cancer with invasion and a fistula in the bladder wall. Cystoscopy
revealed hyperemia, edema and thickening in the bladder wall.
Colonoscopy confirmed colon cancer (Fig. 4). The patient was treated with 0.5 g
levofloxacin, once a day for 10–14 days. Due to the patient's good
physical condition and a lack of obvious manifestations of
inflammation or intestinal obstruction, a laparoscopic palliative
sigmoidectomy and a partial cystectomy were performed. The
diagnosis was colon cancer with a CVF. The patient remained
asymptomatic after 10 months.
The tumor measured 4.5×3.5×2.5 cm in size and the
final pathological diagnosis was sigmoid colon cancer. According to
the AJCC TNM classification, the patient was diagnosed with stage
T4N0M0 disease, indicating low-grade colon cancer.
Discussion
A CVF is a communication between the colon and
bladder that is caused by colon cancer, and it has a poor
prognosis. The clinicopathological characteristics of CVF in the
four cases presented in the current study are summarized in
Table I. However, CVF is extremely
rarely reported worldwide. As CVF as an abbreviation has many
ambiguities, an electronic search of PubMed (https://pubmed.ncbi.nlm.nih.gov) was performed using
the key words ‘colovesical fistula’, and reviewing the previous
literature, only 17 cases were found. The characteristics of each
case are shown in Table II
(1–3,9–19). The
leading cause of CVF is diverticulitis, accounting for 72–75% of
cases, followed by colon cancer at 16% (3). Due to the differences in anatomy, the
probability of a CVF in women is lower (20). Colon cancer invasion can lead to
bladder wall ulceration and necrosis, and even CVF (21,22).
 | Table I.Clinicopathological characteristics of
four cases of colovesical fistula. |
Table I.
Clinicopathological characteristics of
four cases of colovesical fistula.
| Case no. | Age, years | Sex | Etiology | Presenting
symptoms | Site of causative
lesion | Air in bladder | Bladder and/or bowel
wall thickening | Fistulous tract
visualized | Invasion in the
bladder wall | Extravesival mass
that often contained air | Cytoscopy | Colonscopy | Clinical stage | Treatment | Prognosis |
|---|
| 1 | 59 | Male | Colon cancer | Abdominal pain and
distention accompanied by cessation of anal gas and defecation | Sigmoid colon | N | N | N | Y | Y | Not performed | Not performed | T4N0M0 | Refused
surgery | Abdominal pain
remained |
| 2 | 84 | Male | Colon cancer | Urinary frequency
and urgency | Sigmoid colon | Y | Y | N | N | N | Not performed | Not performed | T4N0M0 | Refused
surgery | Died of CVF |
| 3 | 45 | Male | Colon cancer | Fecal urine | Sigmoid colon | N | Y | N | N | N | Cloudy urine and
fecal scraps in the bladder | Multiple tumors 10
cm above the anus | T4N3M0 | Underwent
surgery | Lost to
follow-up |
| 4 | 55 | Male | Sigmoid cancer | Urinary frequency,
urgency and pain | Sigmoid colon | N | N | Y | Y | N | Hyperemia, edema
and thickening of the bladder wall | Colon cancer | T4N0M0 | Underwent
surgery | Asymptomatic |
 | Table II.Reported cases of colon cancer with
vesical fistula. |
Table II.
Reported cases of colon cancer with
vesical fistula.
| First author/s,
year | Country | Age, years | Sex | Chief
complaint | Tumor location | CT description | Ureteroscopy or
cystoscopy/biopsy result | (Refs.) |
|---|
| Oda et al,
1984 | Japan | 50 | Male | Hematuria,
constipation, lower abdominal discomfort, fecaluria | Sigmoid colon | Deformity and a
tumor mass in the bladder | A fistula in the
posterior bladder wall, a mass at 35 cm from the anal margin | (15) |
| Kao et al,
1997 | China | 73 | Male | Terminal gross
hematuria, fecaluria, diarrhea and painful urination | Sigmoid colon | CT not
performed | Colon
adenocarcinoma | (14) |
| Repici et
al, 2000 | Italy | 76 | Female | Large bowel
obstruction, severe anemia, fecaluria and pneumaturia | Sigmoid colon | A neoplastic mass
infiltrating the entire pelvic cavity | A mass 7 to 8 cm
from the anal margin; colon adenocarcinoma | (13) |
| Godbole and
Loughridge, 2003 | UK | 75 | Female | Painless
hematuria | Sigmoid colon | A fistula between
the ileum and bladder | A globular swelling
at the fundus of the bladder | (12) |
| Yabuki et
al, 2004 | Japan | 76 | Male | Pain in urination,
abdominal pain during defecation and fever | Sigmoid colon | CT not
performed | A fistula in the
bladder dome | (11) |
| Medlicott et
al, 2007 | Canada | 69 | Male | Recurrent urinary
tract infections with pneumaturia | Right colon | Diverticulosis coli
complicated by a CVF | Colon
adenocarcinoma | (33) |
| Patel et al,
2009 | USA | 43 | Female | Weight loss,
nausea, vomiting, stool incontinence and tenesmus | Sigmoid colon | A sigmoid colon
mass lesion invading the bladder | A sigmoid mass with
ulceration, a fistula between the mass and the urinary bladder;
colon adenocarcinoma | (34) |
| Ahmad et al,
2010 | UK | 62 | Male | Recurrent urinary
tract infections and fecaluria | Sigmoid colon | Progression of
sigmoid cancer | Examinations not
performed | (17) |
| Pineda and Maxwell,
2012 | USA | 82 | Female | Left lower
abdominal pain, pneumaturia and particulate in the urine | Sigmoid colon | Sigmoid colonic
thickening and air in the bladder | Small cell
carcinoma | (35) |
| Kim et al,
2015 | Korea | 70 | Male | Asymptomatic | Sigmoid colon | Thickening of the
sigmoid colon and a fistula of the colon and bladder | Examinations not
performed | (19) |
| Nakazawa et
al, 2015 | Japan | 84 | Male | Hematuria,
fecaluria, pneumaturia and micturitional pain | Sigmoid colon | CVF | Colon
adenocarcinoma | (10) |
| Kachaamy et
al, 2016 | USA | 56 | Male | Vomiting and
fecaluria | Terminal ileum | A rectal mass
invading the terminal ileum and bladder, and air in the
bladder | Fistula with distal
obstruction | (16) |
| Li et al,
2017 | China | 54 | Male | Urinary frequency,
urge incontinence, urodynia, dysuria, hematuria and
hypogastralgia | 20 cm from the anal
margin | Thickening in the
bladder wall and a mass on the left anterior bladder wall | A mass in the
sigmoid colon; tumor in sigmoid colon | (1) |
| Yang et al,
2018 | Korea | 71 | Male | Weight loss with
diarrhea | Sigmoid colon | Irregular
thickening in the sigmoid colon | A mass in the
sigmoid colon; colon adenocarcinoma | (3) |
| Skierucha et
al, 2018 | Poland | 81 | Female | Diarrhea | 10 cm from the anal
verge | A heterogeneous
conglomerate of structures in the bladder | A mass and leakage
in the sigmoid colon | (2) |
| Ashrafi and Sotelo,
2019 | USA | 72 | Female | Passing gas in the
urine | Sigmoid colon | A mass extending
from the sigmoid colon to the bladder | Diverticulosis in
the sigmoid colon; gas in bladder | (18) |
| Pineda and Maxwell,
2012 | USA | 63 | Male | Burning and the
passage of flatus with urination | Sigmoid colon | Diverticula, and
bladder and sigmoid wall thickening | Irregularity of the
dome of the bladder; colon adenocarcinoma | (35) |
The chief complaints caused by a fistula are
pneumaturia and fecaluria, and these non-specific symptoms can
delay the diagnosis. Considering the risk of uremia, septicemia and
renal failure, a patient with advanced colon cancer presenting with
urinary tract symptoms should be considered for CVF and imaging
examinations should be performed (5). In the four presented cases, CT,
cystoscopy, colonoscopy and biopsy were performed to detect the
fistulae. Clinically, CT is the first method selected to examine
patients with CVF due to its non-invasiveness and high sensitivity.
CT could provide information about the complexity of the fistula
(23) and the surrounding
anatomical structures (24), which
could help the next treatment plan (5). An early, small bladder fistula caused
by colon cancer is not easy to diagnose, as compared with that of
Crohn's disease or an intestinal diverticulum, the bladder fistula
caused by colon cancer is usually smaller, mainly manifesting as
inflammatory changes, and it is difficult to obtain an accurate
biopsy. In colon cancer cases, it is difficult for feces to enter
the bladder through the small fistula, so the fecal and urinary
symptoms are not obvious, but this can become a source of bacterial
cystitis, which is difficult to cure. Therefore, CT is a suitable
primary choice for patients with a suspected CVF. Air in the
bladder, uneven thickening in the sigmoid colon and rectal wall
(1–3,25,26), a
fistula in the bladder or colon wall (1), invasion in the bladder wall, and gas
in the ascending and sigmoid colon are common findings on CT scans,
which may indicate the diagnosis of a CVF. Due to inflammatory
signs, it is not always possible to perform a cystoscopy or biopsy
(7), and a cystoscopy cannot always
find the fistula directly. Likewise, due to intestinal obstruction,
a colonoscopy is not always available (7). In particular, an endoscopy is not
suitable for patients who require urgent surgery. According to a
previous study, the poppy seed test, which involves swallowing
poppy seeds and detecting their presence in the urine, is
recommended, as it is highly sensitive (100%), non-invasive and
easy to perform (27). While the
poppy seed test is indeed sensitive, it cannot provide much more
information about etiology or location, and this test should be
treated as a screening test only. Although magnetic resonance
imaging is not used as a routine test, a number of previous studies
have recommended it, due to its intrinsic soft-tissue resolution
(6,28–31).
The present four cases, which underwent different
therapies, including conservative treatment and surgery, were in
stark contrast to each other. The cases of conservative treatment
refused surgery and were prescribed antibiotics on a long-term
low-dose basis. The cases of surgery underwent a palliative
sigmoidectomy, proximal colostomy, partial small intestine
resection and partial cystectomy, and a laparoscopic palliative
sigmoidectomy and partial cystectomy, respectively. The patients
who underwent surgery had better outcomes and quality of life
compared with the patients who underwent conservative treatment. To
the best of our knowledge, surgery is a favorable prognostic factor
for CVF. According to a previous study, conservative treatment is
usually reserved for patients who are unsuitable for major surgery,
for patients with multiple complications and comorbidities, or for
patients too old to tolerate general anesthesia (5). The present study is consistent with
this in that the patient in case 2 accepted conservative treatment.
Due to the potential risk of uremia and septicemia, surgery is
often necessary, although some cases can heal with conservative
management. Moreover, staged repairs may be reserved for patients
with advanced malignancy, and could be performed as palliative
surgery to manage complications from CVF (5,23).
When CVF is confirmed, one-stage radical surgery is
recommended for patients without intestinal obstruction. According
to a previous study, the outcome of staged surgery is not better
than that of one-stage surgery (23). Palliative surgery, such as a partial
colon resection and simple division of the fistula, leads to a
greater probability of recurrence (26). In patients with a shorter expected
life span, a colostomy often leads to discomfort and even death,
especially in cases requiring urgent surgery (13). Laparoscopic surgery has been widely
accepted to treat malignancy, due to its shorter hospital stay,
better resulting postoperative quality of life and fewer
complications (32). Some studies
have recommended stent implantation surgery to help close the
fistula; however, since this is not a common treatment for vesical
fistulas, this hypothesis requires additional study (17,28).
Among the four cases in the present study, the prognosis of the
patients who received surgery was better, while the prognosis of
the patients who refused surgery was associated with the clinical
staging of the primary disease. Moreover, the patient in case one
had difficulty in alleviating the symptoms and experienced a poor
quality of life, as the fistula could not heal itself without
surgery.
The major strength of the present study is the
relatively large number of patients with CVF. However, the study
has several limitations. First, the available imaging
investigations in the Affiliated Hospital of Yangzhou University
are less. Second, since treatment with laparoscopic surgery is
rarely performed, valuable recommendations could not be provided
for specific surgical approaches. Additional studies with a greater
number of imaging investigation methods is needed to confirm any
suggestions. Larger studies with longer follow-up times are also
needed to conclude specific surgical methods.
In conclusion, CVF is a rare complication of colon
cancer. The four CVF cases with a mix of favorable and poor
prognoses are examples of the disease spectrum and act as a
reminder that certain imaging evidence, including invasion and
fistula in the bladder wall, gas in the colon and bladder, and
uneven thickening in the colon and rectal wall, may indicate a CVF
and point to the need for surgery.
Acknowledgements
The authors would like to thank Dr Hailiang Liang
(Department of General Surgery, Affiliated Hospital of Yangzhou
University, Yangzhou University, Yangzhou, China) for their
valuable discussions with regard to the study.
Funding
This study was supported by the National Natural Science
Foundation of China (grant no. 82002675), the Jiangsu Natural
Science Research of Colleges and Universities-General Project
(grant no. 20KJB320014), the Jiangsu Science and Technology
Program-Youth Fund Project (grant no. BK2020938), the Yangzhou Key
Research and Development-Social Development Project (grant no.
YZ2020110), the Yangzhou Soft Science Research Program (grant no.
YZ2020258), the Jiangsu Postdoctoral Research Funding Program
(grant no. 2020Z268) and the Yangzhou University High-level Talent
Research Start-up Fund (grant no. 2019LYF).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
CD, XP, LW, ZZ, YH, XM, XW, YL, FX and LQ
contributed to the acquisition, analysis and interpretation of the
patient data presented in this case report. CD, XP, YL and FX
drafted the manuscript. All authors made critical revisions. All
authors read and approved the final manuscript. CD, XP, YL and FX
confirm the authenticity of all the raw data.
Ethics approval and consent to
participate
The ethical approval and documentation for a case
report was approved by the Ethical Committee of the Affiliated
Hospital of Yangzhou University (Yangzhou, China; approval no.
2020-YKL03-G042).
Patient consent for publication
All patients provided written informed consent for
the publication of this study. Informed consent for future
publication was obtained before the patient in case two died.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Li S, Chen Z, Zhang Q, Huang C, Wang Z and
Du S: Four cases of enterovesical fistula and the importance of CT
in the diagnosis. BJR Case Rep. 3:201501242017.PubMed/NCBI
|
|
2
|
Skierucha M, Barud W, Baraniak J and
Krupski W: Colovesical fistula as the initial manifestation of
advanced colon cancer: A case report and review of literature.
World J Clin Cases. 6:538–541. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yang DM, Kim HC, Kim SW, Lim SJ and Kim
JS: Sonographic diagnosis of a colovesical fistula due to sigmoid
colon cancer. J Med Ultrasound. 26:160–162. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Velayos B, Del Olmo L, Merino L, Valsero M
and González JM: Non-visible colovesical fistula located by
cystoscopy and successfully managed with the novel
Padlock(®) device for endoscopic closure. Int J
Colorectal Dis. 33:827–829. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Solkar MH, Forshaw MJ, Sankararajah D,
Stewart M and Parker MC: Colovesical fistula-is a surgical approach
always justified? Colorectal Dis. 7:467–471. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tang YZ, Booth TC, Swallow D, Shahabuddin
K, Thomas M, Hanbury D, Chang S and King C: Imaging features of
colovesical fistulae on MRI. Br J Radiol. 85:1371–1375. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
de la Fuente Hernández N, Sánchez CM,
Solerdelcoll MS, Casanovas PH, Rodríguez JB, Sopena JMG and Soler
ET: Colovesical FIstula: Applicability of the laparoscopic approach
and results according to etiology. Cir Esp (Engl Ed). 98:336–341.
2020.(In English, Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Olawaiye AB, Baker TP, Washington MK and
Mutch DG: The new (Version 9) American joint committee on cancer
tumor, node, metastasis staging for cervical cancer. CA Cancer J
Clin. 71:287–298. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Danjoux CE and Catton GE: Delayed
complications in colo-rectal carcinoma treated by combination
radiotherapy and 5-fluorouracil-Eastern Cooperative Oncology Group
(E.C.O.G.) pilot study. Int J Radiat Oncol Biol Phys. 5:311–315.
1979. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nakazawa S, Uemura M, Miyagawa Y,
Tsujimura A and Nonomura N: Urethral fistula and scrotal abscess
associated with colovesical fistula due to the sigmoid colon
cancer. Hinyokika Kiyo. 61:375–378. 2015.(In Japanese). PubMed/NCBI
|
|
11
|
Yabuki D, Sawada Y, Takeuchi Y, Masuda E,
Satoh D, Kuroda K, Tajima M, Sawamura Y, Matsushima M and Shibuya
K: Sigmoid colovesical fistula associated with cancer of the
sigmoid colon. Arch Esp Urol. 57:557–559. 2004.(In Spanish).
PubMed/NCBI
|
|
12
|
Godbole HC and Loughridge WG:
Entero-cutaneous-vesical fistula: An unusual presentation. Ulster
Med J. 72:1172003.PubMed/NCBI
|
|
13
|
Repici A, Reggio D, Saracco G, Marchesa P,
De Angelis C, Barletti C, Musso A, Falco M and Rizzetto M:
Self-expanding covered esophageal ultraflex stent for palliation of
malignant colorectal anastomotic obstruction complicated by
multiple fistulas. Gastrointest Endosc. 51:346–348. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kao PF, Tzen KY, Chang PL, Chang-Chien CR,
Tsai MF and You DL: Diuretic renography findings in enterovesical
fistula. Br J Radiol. 70:421–423. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Oda Y, Hamami G, Umezu K, Sugimoto M,
Yasumuro C, Fujii A, Kamidono S and Ishigami J: Vesicocolic fistula
formed by ‘collision’ tumor between transitional cell carcinoma of
urinary bladder and adenocarcinoma of the sigmoid colon. Hinyokika
Kiyo. 30:55–58. 1984.PubMed/NCBI
|
|
16
|
Kachaamy T, Weber J, Weitz D, Vashi P and
Kundranda M: Successful endoscopic management of a malignant
ileovesicular fistula. Gastrointest Endosc. 84:536–537. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ahmad M, Nice C and Katory M: Covered
metallic stents for the palliation of colovesical fistula. Ann R
Coll Surg Engl. 92:W43–W45. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ashrafi AN and Sotelo R: Colovesical
fistula. N Engl J Med. 380:e512019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kim SH, Song BI and Won KS: Colon
visualization on (99m)Tc-HDP whole-body bone scan due to sigmoid
colon cancer-related enterovesical fistula. Clin Nucl Med.
40:68–69. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Aurello P, Cicchini C, D'Angelo F,
Ramacciato G and Giuliani A: Localization of a colovesical fistula
using a retrograde guide-wire: Report of a case. Surg Today.
34:799–801. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Krausz M, Manny J, Aviad I and Charuzi I:
Vesicocolic fistula due to ‘collision’ between adenocarcinoma of
the colon and transitional cell carcinoma of the urinary bladder.
Cancer. 38:335–340. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hughes ES: Vesicocolic fistula. Dis Colon
Rectum. 3:103–112. 1960. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Garcea G, Majid I, Sutton CD, Pattenden CJ
and Thomas WM: Diagnosis and management of colovesical fistulae;
six-year experience of 90 consecutive cases. Colorectal Dis.
8:347–352. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Goldman SM, Fishman EK, Gatewood OM, Jones
B and Siegelman SS: CT in the diagnosis of enterovesical fistulae.
AJR Am J Roentgenol. 144:1229–1233. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Nguyen TC, Jaffe AM, Gray D, Cain J and
Brown T: Colovesical fistula as an uncommon presentation of
metastatic lung cancer. Cureus. 10:e27672018.PubMed/NCBI
|
|
26
|
Di Buono G, Bonventre G, Buscemi S,
Randisi B, Romano G and Agrusa A: The colovescical fistula in
diverticular disease: Laparoscopic approach in two different cases.
Int J Surg Case Rep. 77S:S112–S115. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kwon EO, Armenakas NA, Scharf SC,
Panagopoulos G and Fracchia JA: The poppy seed test for colovesical
fistula: Big bang little bucks! J Urol. 179:1425–1427. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Golabek T, Szymanska A, Szopinski T,
Bukowczan J, Furmanek M, Powroznik J and Chlosta P: Enterovesical
fistulae: Aetiology, imaging, and management. Gastroenterol Res
Pract. 2013:6179672013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Schmidt S, Chevallier P, Bessoud B, Meuwly
JY, Felley C, Meuli R, Schnyder P and Denys A: Diagnostic
performance of MRI for detection of intestinal fistulas in patients
with complicated inflammatory bowel conditions. Eur Radiol.
17:2957–2963. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Melchior S, Cudovic D, Jones J, Thomas C,
Gillitzer R and Thüroff J: Diagnosis and surgical management of
colovesical fistulas due to sigmoid diverticulitis. J Urol.
182:978–982. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ravichandran S, Ahmed HU, Matanhelia SS
and Dobson M: Is there a role for magnetic resonance imaging in
diagnosing colovesical fistulas? Urology. 72:832–837. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Coco C, Rizzo G, Manno A, Mattana C and
Verbo A: Surgical treatment of small bowel neoplasms. Eur Rev Med
Pharmacol Sci. 14:327–333. 2010.PubMed/NCBI
|
|
33
|
Medlicott SA, Brown HA, Roland B, Beck PL,
Auer I and Mansoor A: Multiple lymphomatous diverticulosis and
comorbid chronic lymphocytic leukemia: Novel manifestations of
ileocolic mantle cell lymphoma. Int J Surg Pathol. 15:408–413.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Patel DH, Dang S, Bentley FR, Julka RN,
Olden KW and Aduli F: Carcinosarcoma of the colon: A rare cause of
colovesical fistula. Am Surg. 75:335–337. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Pineda D and Maxwell PJ IV: Small cell
lung cancer metastasizing to the colon in a colovesicular fistula
in the setting of diverticulitis. Am Surg. 78:E280–E281. 2012.
View Article : Google Scholar
|