Introduction
Angiosarcoma is a rare and aggressive, vascular
malignancy accounting for nearly 2% of all sarcomas, with an
estimated incidence of 2/10,000,000 worldwide. It typically affects
elderly population aged between 60 and 70 years with a poor
prognosis (1). Angiosarcomas
commonly involve skin, head and neck, and superficial soft tissue.
They can also arise in other well-recognized sites, such as liver,
spleen, breast, heart, and central nervous system. However, areas
previously exposed to irradiation, and bone and lung are rarely
affected (2). Angiosarcomas of the
lung can be divided into primary pulmonary angiosarcoma (PPA) and
metastatic pulmonary angiosarcoma (MPA). MPA is more common than
PPA (90% vs. 10%) (3). To date,
fewer than 30 cases of PPA have been reported, based on searching
PubMed search, especially MEDLINE. This study presents a case of
PPA mimicking diffuse pulmonary hemorrhage or pulmonary infection
from an imaging perspective. The study introduces the clinical
characteristics, diagnosis, and treatment of PPA. The study also
reviews the relevant published studies were also reviewed in this
study.
Case presentation
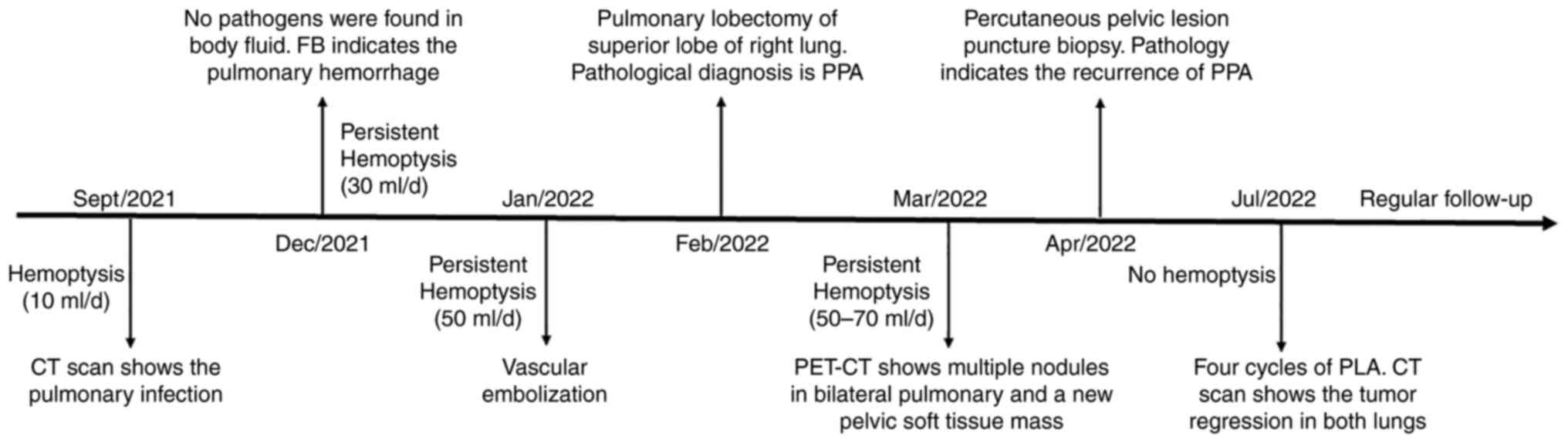
A 78-year-old man with a 3-month history of cough
and persistent hemoptysis was admitted to the hospital on December
31, 2021. He was a lifelong nonsmoker. The physical examination
revealed moist rales in the right lung lobe. Routine laboratory
tests, such as blood parameters, C-reactive protein, serum
procalcitonin, and tumor marker, were all normal. Tests were
negative for Mycobacterium tuberculosis. Fungal antigen tests
including G test and GM tests for glucans and galactomannans,
respectively, were also negative. The patient underwent chest
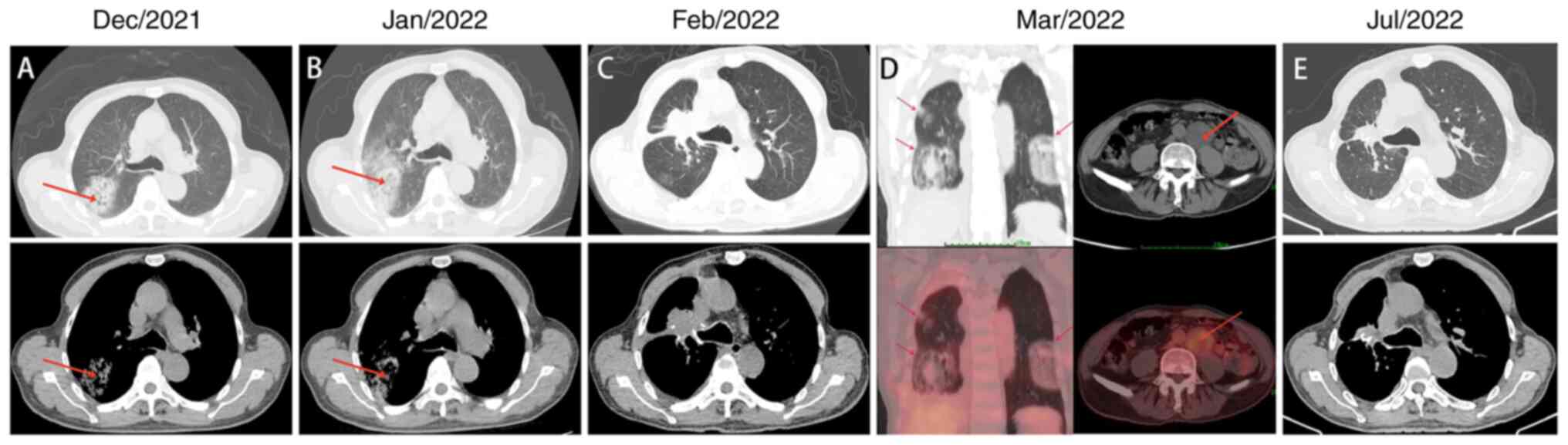
computed tomography (CT) and abdominal CT. Chest CT showed a
hypodense and noncalcified nodule, approximately 5.5×4.8 cm in
size, in the right upper lobe (Fig.
1A). No nodular lesions were found in the abdomen. Fiberoptic
bronchoscopy indicated hemorrhage of the right upper lobe bronchus.
No pathogens were found in the alveolar lavage fluid. The patient's
clinical symptoms did not improve following treatment for pulmonary
infection with moxifloxacin and meropenem for 7 days (Fig. 1B). He received selective bronchial
artery interventional hemostasis with embolization on February 08,
2022. However, the CT scan revealed persistent pulmonary hemorrhage
and enlarged pulmonary lesion (Fig.
1C). Pulmonary lobectomy of superior lobe of right lung and
mediastinal lymph node dissection were performed on February 25,
2022, to establish a definitive diagnosis for prompt clinical
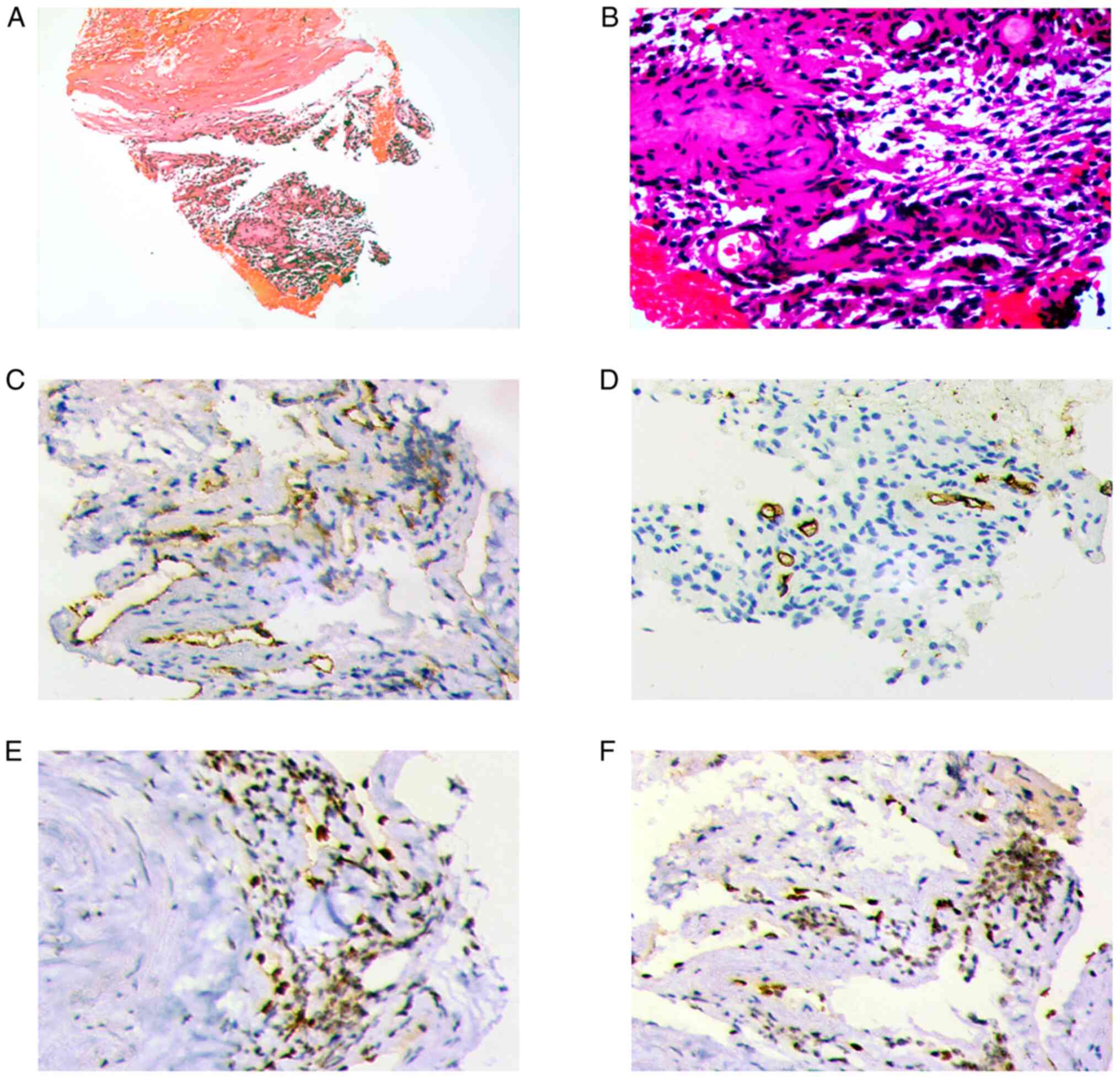
treatment. Hematoxylin and eosin (H&E) staining showed poor
cell differentiation, deeply stained nucleus, and karyokinesis
(Fig. 2A-B). Immunohistochemical
staining revealed weakly positive vascular antigen CD31, negative
CD34, and strongly positive ERG and FLI (Fig. 2C-F). The pathological examination
confirmed the diagnosis as PPA. The patient received no adjuvant
treatment after the surgery due to his old age and poor Eastern
Cooperative Oncology Group (ECOG) performance status.
Unfortunately, hemoptysis persisted after the surgical procedures,
and was exacerbated on March 18, 2022. Positron emission
tomography-CT (PET-CT) was performed on March 28, 2022. The PET
scan showed metabolically active bilateral pulmonary nodules
(standardized uptake value, SUVmax, 3.1) and a new pelvic soft
tissue mass beside the left common iliac artery (SUVmax, 3.4),
suggesting PPA recurrence and metastases (Fig. 1D). The patient underwent
percutaneous needle biopsy of pelvic lesion on April 1, 2022, which
revealed a pathological diagnosis of PPA. Considering the rapid
disease progression and poor ECOG performance of the patient,
pegylated liposomal doxorubicin (PLA) was selected as the adjuvant
treatment. The patient's symptoms of hemoptysis were significantly
relieved after two cycles of chemotherapy (PLA 40 mg/m2,
d1, at an interval of 3 weeks). After the completion of four cycles
of chemotherapy, the hemoptysis did not relapse anymore, and the
lesions in both lungs obviously diminished (Fig. 1E). Further, the pelvic lesion also
contracted (Fig. S1). The patient
refused further treatment and was followed up regularly. Currently,
the patient exhibits no evidence of disease recurrence after 6
months of follow-up. The detailed diagnosis and treatment
procedures are shown in Fig. 3.
Discussion
Angiosarcoma of the lung is a rare malignancy
derived from the vascular endothelium with extremely low incidence.
MPA is far more common than PPA and is usually the result of
metastatic cutaneous and cardiac angiosarcomas, or secondary
tumors. Generally, PPA is detected promptly, as most patients
present with persistent hemoptysis, chest pain, cough, fatigue and
weight loss. However, 20% of cases are asymptomatic and are
detected incidentally or during autopsy (4).
Angiosarcoma of the lung can occur at any age. The
reported median age of onset is 45 years, with no sex differences
(4). PPA may be triggered by risk
factors, such as Lucite-ball Plombage, expose to Thorotrast,
polyvinyl chloride, and chronic empyema (5). The common CT presentation may be a
solitary mass with variable degrees of consolidation or multifocal
lesions. Occasionally, it may present as ground-glass opacity,
which usually manifests as diffuse pulmonary hemorrhage or
pulmonary infection, similar to the case scenario presented in this
study. Since PPA tends to spread to different parts of the body by
the time of presentation, PET-CT is highly suggestive because of
its sensitivity to metastatic disease (6). However, neither CT nor PET-CT can
differentiate PPA from other pulmonary malignant neoplasms.
The definitive diagnosis of PPA must be based on
histopathological and immunohistochemical findings. Endothelial
cell markers, such as CD31, CD34, FLI-1, factor VIII, and
epithelial markers (EMA and cytokeratin), are considered to be
specific for the diagnosis. A recent study indicated that aldehyde
dehydrogenase may be also an important clinical marker for PPA
(7).
To date, no standard regimen exists, especially for
PPA, because of the limited number of cases. Typically, the
treatment options depend on the stage of the disease. Surgery is
the mainstay of treatment for local confined diseases. Vascular
embolization can be performed before surgery, especially in
patients with large tumor size and severe hemorrhage symptoms.
Local ablative treatment may also be an alternative for patients
with small tumor size (<3 cm), or patients with surgical
contraindications (8). Adjuvant
radiotherapy and aminolevulinic acid-photodynamic therapy are
complementary treatments after the surgery due to the
radiosensitivity of the tumor (9,10). In
view of the risk of metastasis, anthracycline-based chemotherapy is
also recommended (2). Chemotherapy
is the primary treatment for advanced-stage disease. The commonly
used treatment regimen is doxorubicin with or without ifosfamide.
The combination of gemcitabine and docetaxel is also highly
efficacious as few patients achieve a complete radiographic
response (6). However, in most
cases, chemotherapy is exclusively used as a palliative treatment
for angiosarcoma in the absence of substantial response (5). Another promising strategy is the use
of vascular-targeted drugs. Studies indicated that antiangiogenic
molecules, such as bevacizumab and sorafenib, are clinically
effective in the control of angiosarcomas (2). Other potential treatments for
angiosarcoma are still under investigation clinically.
Vascular-disrupting compounds (ASA404) and immune modulators
(interleukin-2, interferon-α) might prolong progression-free
survival; however, further investigations are needed (11,12).
Emerging data also suggest that immune checkpoint inhibitors can be
used to treat a subtype of angiosarcoma (13). PPA is an extremely rare sarcoma,
less than 30 cases have been described in the English literature to
date, and most studies are case reports. Therefore, it is difficult
for us to determine which treatment is most suitable for
patients.
The prognosis of angiosarcoma is extremely grave,
the reported 5-year survival ranging from 16 to 56% (14). Most patients die within one year of
diagnosis regardless of the treatment mode.
In conclusion, we report a rare case of PPA
misdiagnosed as diffuse pulmonary hemorrhage. The patient
experienced intrapulmonary metastases and pelvic metastasis one
month after surgery. Partial remission was achieved after 4 cycles
of liposomal doxorubicin. The patient is doing well after 6 months
of follow-up. Our experience with this case suggests that
definitive diagnosis and timely treatment are essential for the
successful management of this disease.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
This study was supported by the Innovative Research Program of
Xiangyang No. 1 People's Hospital (grant no. XYY2021Q02), the
Platform Special Fund for Scientific Research of Xiangyang No. 1
People's Hospital (grant no. XYY2022P05) and the Key Projects of
Xiangyang Science and Technology Bureau (grant no. 2021YL26).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
DZ conceptualized the study. YL, HY and CW acquired
and analyzed the data, and wrote reviewed and edited the
manuscript. YL, HY and CW confirm the authenticity of all the raw
data. DZ acquired funding. All authors have read and approved the
final version of the manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics and Scientific
Committee of Hubei University of Medicine (approval no.
XYY2021002).
Patient consent for publication
Informed consent was obtained from the patients and
their families for the publication of this data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cioffi A, Reichert S, Antonescu CR and
Maki RG: Angiosarcomas and other sarcomas of endothelial origin.
Hematol Oncol Clin North Am. 27:975–988. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Young RJ, Brown NJ, Reed MW, Hughes D and
Woll PJ: Angiosarcoma. Lancet Oncol. 11:983–991. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Pandit SA, Fiedler PN and Westcott JL:
Primary angiosarcoma of the lung. Ann Diagn Pathol. 9:302–304.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Adem C, Aubry MC, Tazelaar HD and Myers
JL: Metastatic angiosarcoma masquerading as diffuse pulmonary
hemorrhage: Clinicopathologic analysis of 7 new patients. Arch
Pathol Lab Med. 125:1562–1565. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chen YB, Guo LC, Yang L, Feng W, Zhang XQ,
Ling CH, Ji C and Huang JA: Angiosarcoma of the lung: 2 cases
report and literature reviewed. Lung Cancer. 70:352–356. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wilson R, Glaros S, Brown RK, Michael C
and Reisman D: Complete radiographic response of primary pulmonary
angiosarcomas following gemcitabine and taxotere. Lung Cancer.
61:131–136. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Aramini B, Masciale V, Bianchi D,
Manfredini B, Banchelli F, D'Amico R, Bertolini F, Dominici M,
Morandi U and Maiorana A: ALDH Expression in Angiosarcoma of the
Lung: A Potential Marker of Aggressiveness? Front Med (Lausanne).
7:5441582020. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Falk AT, Moureau-Zabotto L, Ouali M, Penel
N, Italiano A, Bay JO, Olivier T, Sunyach MP, Boudou-Roquette P,
Salas S, et al: Effect on survival of local ablative treatment of
metastases from sarcomas: A study of the French sarcoma group. Clin
Oncol (R Coll Radiol). 27:48–55. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gao Y, Wang WS, Wang HL, Liu J and Lu YG:
Treatment of Epithelioid angiosarcoma with Topical ALA-PDT in the
course of surgery. Photodiagnosis Photodyn Ther. 19:153–155. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sasaki R, Soejima T, Kishi K, Imajo Y,
Hirota S, Kamikonya N, Murakami M, Kawabe T, Ejima Y, Matsumoto A
and Sugimura K: Angiosarcoma treated with radiotherapy: Impact of
tumor type and size on outcome. Int J Radiat Oncol Biol Phys.
52:1032–1040. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gebhardt C, Ziegler B, Stadler S, Goerdt S
and Utikal J: Complete remission of treatment-refractory advanced
angiosarcoma of the scalp by protracted intralesional interleukin-2
therapy. Br J Dermatol. 172:1156–1158. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Young RJ, Woll PJ, Staton CA, Reed MW and
Brown NJ: Vascular-targeted agents for the treatment of
angiosarcoma. Cancer Chemother Pharmacol. 73:259–270. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Rosenbaum E, Antonescu CR, Smith S, Bradic
M, Kashani D, Richards AL, Donoghue M, Kelly CM, Nacev B, Chan JE,
et al: Clinical, genomic, and transcriptomic correlates of response
to immune checkpoint blockade-based therapy in a cohort of patients
with angiosarcoma treated at a single center. J Immunother Cancer.
10:e0041492022. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sturm EC, Marasco IS and Katz SC:
Multidisciplinary management of angiosarcoma-A review. J Surg Res.
257:213–220. 2021. View Article : Google Scholar : PubMed/NCBI
|