Introduction
Bladder cancer is one of the most common
malignancies worldwide (1). In
total, ~70% of patients with bladder cancer are initially diagnosed
with non-muscle invasive bladder cancer (NMIBC), which is confined
to the muscular layer and submucosa (2,3).
Transurethral resection of bladder tumors (TURBT) is the primary
surgical procedure for NMIBC (4,5), but
>50% of patients experience recurrence within 1 to 2 years.
Therefore, there is an urgent need to find novel treatments to
reduce the rate of postoperative recurrence of NMIBC.
After recurrence of bladder cancer, progression to
MIBC is likely (6), and radical
resection of bladder cancer is needed at a later stage, which is
associated with increased pain and a worse prognosis. Currently,
TURBT combined with adjuvant therapy is considered to be effective
in reducing the incidence of postoperative recurrence (7,8).
Adjuvant therapy drugs, such as mitomycin C (MMC) (9,10),
epirubicin (EPI) (11) and
pirarubicin (THP) (12), have
increased benefits due to their ability to be used in intravesical
instillation. Due to its safety, low number of toxic side effects
and price, THP has been widely used in the clinic. However, it is
mainly used for postoperative adjuvant therapy, and there is still
a lack of relevant studies proving the efficacy of preoperative
intravesical instillation for the prevention of bladder cancer
recurrence.
In recent years, laser en bloc resection with a
980-nm diode laser has been shown to exhibit a notably reduced
incidence of complications and recurrence compared with
conventional TURBT surgery (13).
For diode lasers at a 980-nm wavelength, a new generation of laser
technology, their energy can be absorbed by both water and
hemoglobin. Compared with conventional transurethral electric
resection, due to the tissue vaporization and cutting ability,
coagulation characteristics and controllable penetration depth of
980-nm diode laser, this technique has shown increased efficacy and
safety, and can markedly reduce the amount of bleeding and the risk
of bladder perforation (13,14).
However, the efficacy of the combination of 980-nm diode laser en
bloc resection and preoperative THP intravesical instillation for
the treatment of patients with NMIBC remains unclear. In the
present study, the aim was to investigate the effect of combining
980-nm diode laser en bloc resection with preoperative intravesical
instillation of THP on the rates of postoperative recurrence and
complications of NMIBC.
Materials and methods
Patients
A total of 120 patients who were diagnosed with
NMIBC at the Department of Urology, The Fourth Affiliated Hospital
of Guangxi Medical University (Liuzhou, China) between May 2021 and
July 2022 were retrospectively included in the present study.
Patients with Ta-T1N0M0 (8th American Joint Committee on Cancer TNM
staging system) (15) bladder
tumors that were diagnosed by preoperative magnetic resonance
imaging examination and who underwent surgery were included in the
current study. Exclusion criteria included: i) Patients with
recurrent or muscle-invasive bladder tumors; ii) patients with
other tumors; and iii) patients with distant metastasis. The
patients were treated using either a 980-nm diode laser combined
with preoperative intravesical instillation of THP (LaT), a 980-nm
laser alone (La), TURBT combined with preoperative intravesical
instillation of THP (TUT) or TURBT alone (TU). In the laser surgery
group, the low-power 980-nm diode laser was used to free the tumor
in the submucosa, and then the tumor was completely removed.
Subsequently, the high-power 980-nm diode laser was used to
vaporize the edge and base of the tumor to further ensure negative
margins.
The patients in the LaT and TUT groups received
preoperative intravesical instillation of 30 mg THP/30 ml saline
for 15 min. The patients in the La and TU groups received
preoperative intravesical instillation of 30 ml saline for 15 min.
During the operation, a biopsy was performed at the THP staining
sites (orange staining) in the LaT and TUT groups. For those
patients with ≤3 stained sites, a biopsy was taken within 2 cm of
the tumor to supplement the remaining number. In the La and TU
groups, a biopsy was performed at three random sites within 2 cm of
the tumor. Intravesical instillation chemotherapy with 50 ml
gemcitabine (20 mg/ml) was performed for 1 year after surgery. The
first chemotherapy session started within 24 h after surgery, once
a week for the first 2 months and once a month after 2 months. Each
patient was followed up and underwent cystoscopy every 3
months.
Data collection
Clinicopathological data were also collected and
evaluated, including sex, age, American Society of
Anesthesiologists (ASA) grade (16), tumor location, maximum tumor
diameter, tumor multiplicity, grade (17), tumor (T) stage (15), operation time, blood loss volume,
perforation, obturator nerve reflex (ONR), days of bladder
irrigation (BI), days of catheter extubation (CE), days of
postoperative hospitalization (PH) and delayed bleeding.
Statistical analysis
All statistical analyses were performed using SPSS
(version 23.0; IBM Corp.). One-way analysis of variance was
performed to analyze the difference in continuous variables among
the four groups, followed by the Bonferroni post hoc test.
Continuous variables are presented as the mean ± SD.
χ2 or Fisher's exact test was employed to
evaluate categorical variables. Univariate and multivariate Cox
regression analyses were applied to identify independent risk
factors. Kaplan-Meier analysis was used to compare the survival
differences among the four groups, with statistical analysis using
the log-rank test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Baseline characteristics of
patients
The clinicopathological characteristics of patients
with NMIBC in the four different groups, namely, the LaT group
(n=32), the La group (n=30), the TUT group (n=29) and the TU group
(n=29), are shown in Table I. There
was no significant difference with regard to sex, age, ASA, tumor
location, tumor diameter, multiplicity of tumor, T stage and grade
among the four groups.
 | Table I.Clinicopathological characteristics of
patients with non-muscle invasive bladder cancer in the LaT (n=32),
La (n=30), TUT (n=29) and TU (n=29) groups. |
Table I.
Clinicopathological characteristics of
patients with non-muscle invasive bladder cancer in the LaT (n=32),
La (n=30), TUT (n=29) and TU (n=29) groups.
| Clinicopathological
characteristics | LaT group | La group | TUT group | TU group | P-value |
|---|
| Sex, n (%) |
|
|
|
| 0.936 |
| Male | 26 (81.3) | 24 (80.0) | 22 (75.9) | 22 (75.9) |
|
|
Female | 6 (18.7) | 6 (20.0) | 7 (24.1) | 7 (24.1) |
|
| Age,
yearsa | 64.7±7.5 | 64.9±5.7 | 65.1±8.1 | 65.2±9.3 | 0.995 |
| ASA, n (%) |
|
|
|
| 0.985 |
| I | 17 (53.1) | 14 (46.7) | 14 (48.3) | 12 (41.4) |
|
| II | 14 (43.8) | 15 (50.0) | 14 (48.3) | 16 (55.2) |
|
|
III | 1 (3.1) | 1 (3.3) | 1 (3.4) | 1 (3.4) |
|
| Tumor location, n
(%) |
|
|
|
| 0.274 |
|
Lateral | 19 (59.4) | 14 (46.7) | 14 (48.3) | 20 (69.0) |
|
|
Others | 13 (40.6) | 16 (53.3) | 15 (51.7) | 9 (31.0) |
|
| Tumor diameter,
cma | 2.6±0.8 | 2.4±0.9 | 2.8±1.0 | 2.3±0.6 | 0.090 |
| Multiplicity of
tumor, n (%) |
|
|
|
| 0.800 |
|
Single | 28 (87.5) | 24 (80.0) | 23 (79.3) | 23 (79.3) |
|
|
Multiple | 4 (12.5) | 6 (20.0) | 6 (20.7) | 6 (20.7) |
|
| T stage, n (%) |
|
|
|
| 0.688 |
| Ta | 24 (75.0) | 19 (63.3) | 20 (69.0) | 18 (62.1) |
|
| T1 | 8 (25.0) | 11 (36.7) | 9 (31.0) | 11 (37.9) |
|
| WHO 2004 grade, n
(%) |
|
|
|
|
|
|
PUNLMP | 17 (53.1) | 10 (33.3) | 9 (31.0) | 6 (20.7) | 0.206 |
|
Low | 10 (31.3) | 10 (33.3) | 12 (41.4) | 14 (48.3) |
|
|
High | 5 (15.6) | 10 (33.3) | 8 (27.6) | 9 (31.0) |
|
Perioperative surgical outcomes and
detection of lesions
The perioperative surgical outcomes among the four
different groups are listed in Table
II. No significant differences in operation time or ONR were
observed among the four groups. However, ONR did not occur in the
two 980-nm laser groups but it did occur in the two TURBT groups,
with a single case in the TUT group (3.4%) and two cases in the TU
group (6.9%). There were significant differences among the four
groups in terms of blood loss, perforation, days of BI, CE and PH,
and delayed bleeding (P<0.05). Among the four groups, the blood
loss in the two 980-nm laser groups (LaT group, 8.8±2.6 ml; La
group, 8.8±2.3 ml) was significantly lower than that in the two
TURBT groups (TUT group, 17.1±5.3 ml; TU group, 15.7±6.2 ml;
P<0.001). For perforation, the incidence was similar to ONR, but
statistically significant, with no perforation events occurring in
the two laser groups but four cases in the TUT group (13.8%) and
three cases in the TU group (10.3%). Similarly, the days of BI, CE
and PH were observed to be significantly shorter in the two laser
groups than in the two TURBT groups, and the time was shortened by
~2 days (P<0.001). In addition, there was a significant
difference in delayed bleeding among the four groups, with no
delayed bleeding in the two laser groups but seven cases of delayed
bleeding in the TURBT groups; three in the TUT group (10.3%) and
four in the TU group (13.8%). As illustrated in Table III, the detection rate of
suspicious lesions in the preoperative intravesical instillation of
THP (LaT and TUT) groups was significantly higher than that in the
other two (La and TU) groups without THP (P<0.001).
 | Table II.Comparison of perioperative surgical
outcomes in patients with non-muscle invasive bladder cancer in the
LaT (n=32), La (n=30), TUT (n=29) and TU (n=29) groups. |
Table II.
Comparison of perioperative surgical
outcomes in patients with non-muscle invasive bladder cancer in the
LaT (n=32), La (n=30), TUT (n=29) and TU (n=29) groups.
| Perioperative
surgical outcomes | LaT group | La group | TUT group | TU group | P-value |
|---|
| Operation time,
mina | 45.6±8.2 | 43.8±9.4 | 44.2±8.4 | 47.4±8.5 | 0.377 |
| Blood loss,
mla | 8.8±2.6 | 8.8±2.3 | 17.1±5.3 | 15.7±6.2 | <0.001 |
| Perforation, n
(%) | 0 (0.0) | 0 (0.0) | 4 (13.8) | 3 (10.3) | <0.05 |
| ONR, n (%) | 0 (0.0) | 0 (0.0) | 1 (3.4) | 2 (6.9) | 0.142 |
| Days of
BIa | 1.4±0.5 | 1.6±0.5 | 3.3±1.0 | 3.4±1.2 | <0.001 |
| Days of
CEa | 2.4±0.5 | 2.6±0.5 | 4.3±1.0 | 4.4±1.2 | <0.001 |
| Days of
PHa | 3.7±0.7 | 3.9±0.7 | 5.7±1.0 | 5.7±1.0 | <0.001 |
| Delayed bleeding, n
(%) | 0 (0.0) | 0 (0.0) | 3 (10.3) | 4 (13.8) | <0.05 |
 | Table III.Difference in the detection rate of
suspected lesions by preoperative intravesical instillation of THP
in groups with no irrigation with THP (La and TU) (n=177) and
irrigation with THP (LaT and TUT) (n=183)a. |
Table III.
Difference in the detection rate of
suspected lesions by preoperative intravesical instillation of THP
in groups with no irrigation with THP (La and TU) (n=177) and
irrigation with THP (LaT and TUT) (n=183)a.
| Groups | No irrigation with
THP | Irrigation with
THP | P-value |
|---|
| Lesions, n (%) | 6 (3.4) | 24 (13.1) | <0.001 |
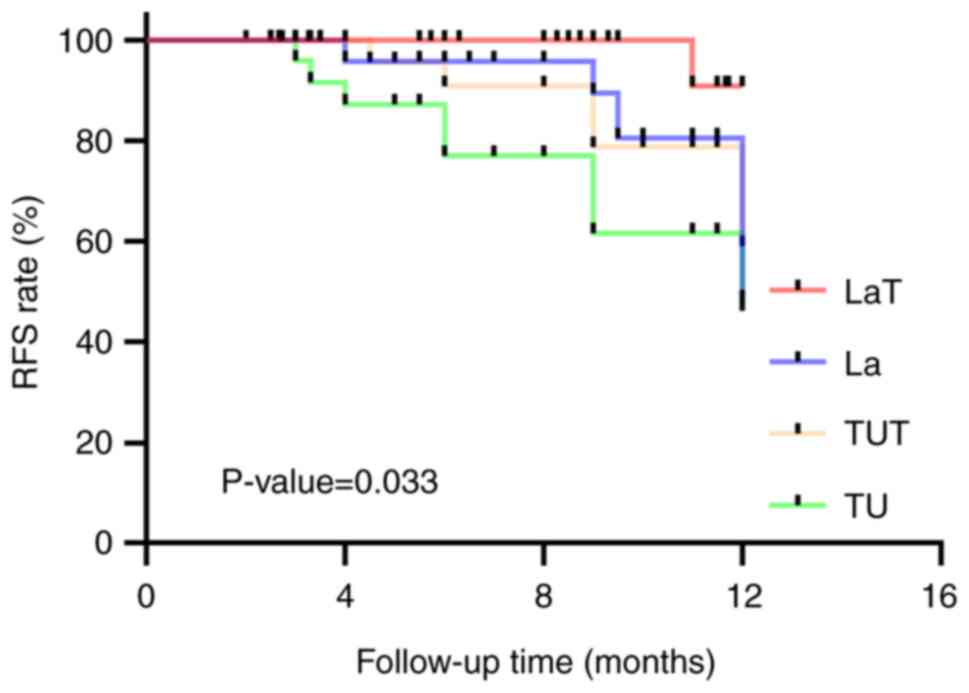
Cox regression analysis and survival
analysis
To further identify independent risk factors for
NMIBC recurrence, both univariate and multivariate Cox regression
analyses were employed. As shown in Table IV, the univariate and multivariate
Cox regression analyses revealed that maximum tumor diameter ≥3 cm,
tumor multiplicity, 980-nm laser surgery and preoperative
intravesical instillation of THP were independent risk factors for
recurrence of NMIBC. Among them, the maximum tumor diameter ≥3 cm
[hazard ratio (HR), 6.155; 95% confidence interval (CI),
1.716-22.083; P<0.01] and tumor multiplicity (HR, 4.819; 95% CI,
1.778-13.059; P<0.01) were adverse risk factors, while 980-nm
laser surgery (HR, 0.266; 95% CI, 0.088-0.803; P<0.05) and
irrigation with THP (HR, 0.195; 95% CI, 0.065-0.584; P<0.01)
were protective risk factors. Moreover, a survival analysis was
conducted to further investigate the effect of combining the 980-nm
laser with preoperative intravesical instillation of THP on the
recurrence-free survival (RFS) rate of patients with NMIBC. The
Kaplan-Meier survival curves are plotted in Fig. 1. The results indicated that the RFS
rate of the LaT group was significantly higher than that of the
other three groups (P=0.033).
 | Table IV.Results of univariate and
multivariate Cox regression analyses. |
Table IV.
Results of univariate and
multivariate Cox regression analyses.
|
| Univariate | Multivariate |
|---|
|
|
|
|
|---|
| Variable | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Sex | 1.679 | 0.487-5.781 | 0.412 |
|
|
|
| Age, years | 1.034 | 0.972-1.100 | 0.283 |
|
|
|
| ASA | 1.334 | 0.565-3.147 | 0.511 |
|
|
|
| Lateral | 1.778 | 0.713-4.429 | 0.217 |
|
|
|
| Diameter, >3
cm | 6.140 | 2.032-18.554 | <0.01 | 6.155 | 1.716-22.083 | <0.01 |
| Multiplicity | 5.134 | 2.073-12.715 | <0.001 | 4.819 | 1.778-13.059 | <0.01 |
| Operation time | 1.017 | 0.960-1.078 | 0.558 |
|
|
|
| Blood loss, ml | 1.023 | 0.955-1.097 | 0.515 |
|
|
|
| Grade | 1.822 | 1.030-3.224 | <0.05 | 1.180 | 0.558-2.494 | 0.665 |
| T stage | 2.656 | 1.077-6.552 | <0.05 | 1.652 | 0.560-4.872 | 0.363 |
| 980-nm laser | 0.364 | 0.138-0.959 | <0.05 | 0.266 | 0.088-0.803 | <0.05 |
| Irrigation with
THP | 0.394 | 0.149-1.036 | 0.059 | 0.195 | 0.065-0.584 | <0.01 |
Discussion
To date, traditional TURBT is the standard surgical
treatment for NMIBC, but it has some intraoperative complications,
including bleeding, bladder perforation and ONR (18), which are closely associated with the
surgical experience and skill of surgeons. Meanwhile, due to the
segmented resection method of TURBT surgery, tumor cells may be
shed during the operation to some extent, thereby increasing the
risks of recurrence and metastasis (19,20).
To reduce the occurrence of these complications, surgeons have
conducted additional research on new approaches. In 1978, Staehler
et al (21) first explored
the use of laser surgery for bladder neoplasms. Studies have shown
that compared with TURBT surgery, laser procedures such as holmium
(22–24), 2-µm (25–27),
1.9-µm Vela (28) and
potassium-titanyl-phosphate (29,30)
lasers used to treat NMIBC can not only reduce the incidence of
complications, but can also reduce the postoperative recurrence
rate when used with en bloc resection. However, studies on en bloc
resection of NMIBC with a 980-nm diode laser have rarely been
reported (13,31).
In the present study, the intraoperative and
postoperative characteristics, and the recurrence status of
patients with NMIBC were retrospectively compared in the LaT, La,
TUT and TU groups. It was shown that 980-nm diode laser en bloc
resection was more effective at reducing intraoperative blood loss
than TURBT surgery. Furthermore, intraoperative perforation and ONR
did not occur in the two 980-nm diode laser surgery groups, while
four cases of perforation and a single case of ONR occurred in the
TUT group, and three cases of perforation and two cases of ONR
occurred in the TU group. Due to its improved hemostatic effect,
the number of days of PI, CE and PH was significantly decreased
compared with that in the TURBT group. In addition, no delayed
bleeding was observed in the two 980-nm laser groups. According to
the aforementioned results, compared with TURBT surgery, the 980-nm
diode laser has similar advantages to other lasers (27,28,32–34),
and the treatment of NMIBC with a 980-nm diode laser can not only
decrease the incidence of intraoperative and postoperative
complications, but can also accelerate postoperative recovery. More
importantly, the laser groups had a lower 1-year recurrence rate,
which significantly improved RFS time in the patients with
NMIBC.
To prevent recurrence in patients with NMIBC,
transurethral resection is usually followed by adjuvant therapy.
Postoperative intravesical instillation of chemotherapeutic agents,
such as MMC, EPI and THP, can effectively improve prognosis and
prolong RFS time in patients with NMIBC (7). On the one hand, it has been reported
that THP can be rapidly absorbed by tumor cells, and enter the
nucleus to inhibit DNA synthesis (35). A meta-analysis study showed that
intravesical instillation of THP significantly reduced the risk of
tumor recurrence and was superior to MMC and EPI (8). On the other hand, according to the
characteristics of the THP solution, preoperative intravesical
instillation of THP can stain tumors orange, which may be conducive
to the detection of small lesions and reduce the risk of missed
detection. However, the effect of preoperative intravesical
instillation of THP on postoperative recurrence in patients with
NMIBC remains unclear. Considering the advantages of both the
980-nm diode laser and the intravesical instillation of THP
solution, the combined effect of preoperative intravesical
instillation of THP and the 980-nm diode laser was investigated on
the postoperative recurrence of NMIBC in the present study.
In the present study, the proportion of suspicious
lesions detected in the two THP groups, LaT and TUT, was
significantly higher than that in the random sampling groups, La
and TU, suggesting that preoperative intravesical instillation of
THP was beneficial for detecting suspicious and unobtrusive
lesions. Furthermore, Cox regression analysis showed that both the
preoperative intravesical instillation of THP and 980-nm diode
laser surgery were protective factors for the recurrence of NMIBC,
which significantly reduced the risk of tumor recurrence. In
addition, the survival analysis showed that among the four groups,
the LaT group exhibited a significantly higher 1-year RFS rate for
patients with NMIBC compared with that in the other three groups,
followed by the La, TUT and TU groups. The results indicated that
preoperative THP intravesical instillation or en bloc resection
with a 980-nm diode laser could effectively prolong RFS time in
patients with NMIBC and reduce the postoperative recurrence
rate.
However, there are some limitations to the current
study. The study is retrospective rather than a double-blind
prospective randomized controlled study, which may have led to
selection bias to some extent. Additionally, the small sample size
of this study may also have led to the deviation of results. In the
future, a randomized controlled study will be performed to draw
more rigorous conclusions.
In summary, compared with TURBT surgery alone,
980-nm diode laser en bloc resection combined with preoperative
intravesical instillation of THP not only assists in reducing the
incidence of intraoperative and postoperative complications, but
also accelerates postoperative recovery in patients and reduces the
risk of recurrence of NMIBC.
Acknowledgements
Not applicable.
Funding
The present study was funded by the Guangxi Zhuang Autonomous
Region Health and Family Planning Commission (grant no.
Z20210478).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZT prepared the manuscript and performed the
statistical analysis. JP performed the data analysis. SW and FZ
contributed to the data acquisition, analysis and interpretation.
MW presented the concept of the study and designed the study. ZT
and PJ confirm the authenticity of all the raw data. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
The Fourth Affiliated Hospital of Guangxi Medical University
(Liuzhou, China) (approval no. KY2021053) and written informed
consent was obtained from all patients.
Patient consent for publication
Written informed consent was obtained from the
patients to publish this paper.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
NMIBC
|
non-muscle invasive bladder cancer
|
|
TURBT
|
transurethral resection of bladder
tumors
|
|
THP
|
pirarubicin
|
|
LaT
|
laser with THP
|
|
La
|
laser alone
|
|
TUT
|
TURBT with THP
|
|
TU
|
TURBT alone
|
|
RFS
|
recurrence-free survival
|
|
MMC
|
mitomycin C
|
|
EPI
|
epirubicin
|
|
ASA
|
American Society of
Anesthesiologists
|
|
ONR
|
obturator nerve reflex
|
|
BI
|
bladder irrigation
|
|
CE
|
catheter extubation
|
|
PH
|
postoperative hospitalization
|
References
|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kirkali Z, Chan T, Manoharan M, Algaba F,
Busch C, Cheng L, Kiemeney L, Kriegmair M, Montironi R, Murphy WM,
et al: Bladder cancer: Epidemiology, staging and grading, and
diagnosis. Urology. 66:4–34. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kamat AM, Hahn NM, Efstathiou JA, Lerner
SP, Malmström PU, Choi W, Guo CC, Lotan Y and Kassouf W: Bladder
cancer. Lancet. 388:2796–2810. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Babjuk M, Bohle A, Burger M, Tobisawa Y,
Yoneyama T, Yamamoto H, Imai A, Ito H, Yoneyama T, Hashimoto Y, et
al: EAU Guidelines on Non-Muscle-invasive Urothelial Carcinoma of
the Bladder: Update 2016. Eur Urol. 71:447–461. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nishiyama H: Asia Consensus Statement on
NCCN Clinical Practice Guideline for bladder cancer. Jpn J Clin
Oncol. 48:3–6. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sylvester RJ: Natural history, recurrence,
and progression in superficial bladder cancer.
ScientificWorldJournal. 6:2617–2625. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sylvester RJ, Oosterlinck W, Holmang S,
Sydes MR, Birtle A, Gudjonsson S, De Nunzio C, Okamura K, Kaasinen
E, Solsona E, et al: Systematic review and individual patient data
meta-analysis of randomized trials comparing a single immediate
instillation of chemotherapy after transurethral resection with
transurethral resection alone in patients with stage pTa-pT1
urothelial carcinoma of the bladder: Which patients benefit from
the instillation? Eur Urol. 69:231–244. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kang M, Jeong CW, Kwak C, Kim HH and Ku
JH: Single, immediate postoperative instillation of chemotherapy in
non-muscle invasive bladder cancer: A systematic review and network
meta-analysis of randomized clinical trials using different drugs.
Oncotarget. 7:45479–45488. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Solsona E, Iborra I, Ricos JV, Monros JL,
Casanova J and Dumont R: Effectiveness of a single immediate
mitomycin C instillation in patients with low risk superficial
bladder cancer: Short and long-term followup. J Urol.
161:1120–1123. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tolley DA, Parmar MK, Grigor KM, Lallemand
G, Benyon LL, Fellows J, Freedman LS, Grigor KM, Hall RR, Hargreave
TB, et al: The effect of intravesical mitomycin C on recurrence of
newly diagnosed superficial bladder cancer: A further report with 7
years of follow up. J Urol. 155:1233–1238. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Oosterlinck W, Kurth KH, Schroder F,
Bultinck J, Hammond B and Sylvester R: A prospective European
Organization for Research and Treatment of Cancer Genitourinary
Group randomized trial comparing transurethral resection followed
by a single intravesical instillation of epirubicin or water in
single stage Ta, T1 papillary carcinoma of the bladder. J Urol.
149:749–752. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Okamura K, Ono Y, Kinukawa T, Matsuura O,
Yamada S, Ando T, Fukatsu T, Ohno Y and Ohshima S; Nagoya
University Urological Oncology Group, : Randomized study of single
early instillation of (2'R)-4′-O-tetrahydropyranyl-doxorubicin for
a single superficial bladder carcinoma. Cancer. 94:2363–2368. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mao T, Zhang H, Cui J, Zhao Z, Jiao D and
Zhang W: The 980 nm diode laser treatment for non-muscle-invasive
bladder tumor with en bloc technique: Single-center experience.
World J Surg Oncol. 20:3242022. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wendt-Nordahl G, Huckele S, Honeck P,
Alken P, Knoll T, Michel MS and Häcker A: 980-nm Diode laser: A
novel laser technology for vaporization of the prostate. Eur Urol.
52:1723–1728. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Magers MJ, Lopez-Beltran A, Montironi R,
Williamson SR, Kaimakliotis HZ and Cheng L: Staging of bladder
cancer. Histopathology. 74:112–134. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
De Cassai A, Boscolo A, Tonetti T, Ban I
and Ori C: Assignment of ASA-physical status relates to
anesthesiologists' experience: A survey-based national-study.
Korean J Anesthesiol. 72:53–59. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Varma M, Delahunt B and van der Kwast T:
Grading Noninvasive Bladder Cancer: World Health Organisation 1973
or 2004 May Be the Wrong Question. Eur Urol. 76:413–415. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Xu J, Wang C, Ouyang J, Sun J and Hu C:
Efficacy and Safety of transurethral laser surgery versus
transurethral resection for Non-Muscle-invasive bladder cancer: A
Meta-Analysis and systematic review. Urol Int. 104:810–823. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Engilbertsson H, Aaltonen KE, Bjornsson S,
Kristmundsson T, Patschan O, Rydén L and Gudjonsson S:
Transurethral bladder tumor resection can cause seeding of cancer
cells into the bloodstream. J Urol. 193:53–57. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Liang H, Yang T, Wu K, He D and Fan J: En
bloc resection improves the identification of muscularis mucosae in
non-muscle invasive bladder cancer. World J Urol. 37:2677–2682.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Staehler G, Schmiedt E and Hofstetter A:
Destruction of bladder neoplasms by means of transurethral
neodym-YAG-laser coagulation. Helv Chir Acta. 45:307–311. 1978.(In
German). PubMed/NCBI
|
|
22
|
D'Souza N and Verma A: Holmium laser
transurethral resection of bladder tumor: Our experience. Urol Ann.
8:439–443. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kramer MW, Rassweiler JJ, Klein J, Martov
A, Baykov N, Lusuardi L, Janetschek G, Hurle R, Wolters M, Abbas M,
et al: En bloc resection of urothelium carcinoma of the bladder
(EBRUC): A European multicenter study to compare safety, efficacy,
and outcome of laser and electrical en bloc transurethral resection
of bladder tumor. World J Urol. 33:1937–1943. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Xishuang S, Deyong Y, Xiangyu C, Tao J,
Quanlin L, Hongwei G, Jibin Y, Dongjun W, Zhongzhou H, Jianbo W, et
al: Comparing the safety and efficiency of conventional monopolar,
plasmakinetic, and holmium laser transurethral resection of primary
non-muscle invasive bladder cancer. J Endourol. 24:69–73. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Chen X, Liao J, Chen L, Qiu S, Mo C, Mao
X, Yang Y, Zhou S and Chen J: En bloc transurethral resection with
2-micron continuous-wave laser for primary non-muscle-invasive
bladder cancer: A randomized controlled trial. World J Urol.
33:989–995. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Liu H, Wu J, Xue S, Zhang Q, Ruan Y, Sun X
and Xia S: Comparison of the safety and efficacy of conventional
monopolar and 2-micron laser transurethral resection in the
management of multiple nonmuscle-invasive bladder cancer. J Int Med
Res. 41:984–992. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhong C, Guo S, Tang Y and Xia S: Clinical
observation on 2 micron laser for non-muscle-invasive bladder tumor
treatment: Single-center experience. World J Urol. 28:157–161.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Xu H, Ma J, Chen Z, Yang J, Yuan H, Wang
T, Liu J, Yang W and Ye Z: Safety and efficacy of en bloc
transurethral resection With 1.9 microm vela laser for treatment of
Non-Muscle-invasive bladder cancer. Urology. 113:246–250. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Cheng B, Qiu X, Li H and Yang G: The
safety and efficacy of front-firing green-light laser endoscopic en
bloc photoselective vapo-enucleation of non-muscle-invasive bladder
cancer. Ther Clin Risk Manag. 13:983–988. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Yang D, Xue B, Zang Y, Liu X, Zhu J, Zhou
Y and Shan Y: Efficacy and safety of potassium-titanyl-phosphate
laser vaporization for clinically non-muscle invasive bladder
cancer. Urol J. 11:1258–1263. 2014.PubMed/NCBI
|
|
31
|
Tao W, Sun C, Yao Q, Fu K, Shan Y, Zhang
Y, Xue B and Yang D: The clinical study of en bloc transurethral
resection with 980 nm laser for treatment of primary non-muscle
invasive bladder cancer. J Xray Sci Technol. 28:563–571.
2020.PubMed/NCBI
|
|
32
|
Chen J, Zhao Y, Wang S, Jin X, Sun P,
Zhang L and Wang M: Green-light laser en bloc resection for primary
non-muscle-invasive bladder tumor versus transurethral
electroresection: A prospective, nonrandomized two-center trial
with 36-month follow-up. Lasers Surg Med. 48:859–865. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Migliari R, Buffardi A and Ghabin H:
Thulium laser endoscopic en bloc Enucleation of Nonmuscle-Invasive
bladder cancer. J Endourol. 29:1258–1262. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Xu Y, Guan W, Chen W, Xie C, Ouyang Y, Wu
Y and Liu C: Comparing the treatment outcomes of
potassium-titanyl-phosphate laser vaporization and transurethral
electroresection for primary nonmuscle-invasive bladder cancer: A
prospective, randomized study. Lasers Surg Med. 47:306–311. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kunimoto S, Miura K, Takahashi Y, Takeuchi
T and Umezawa H: Rapid uptake by cultured tumor cells and
intracellular behavior of 4′-O-tetrahydropyranyladriamycin. J
Antibiot (Tokyo). 36:312–317. 1983. View Article : Google Scholar : PubMed/NCBI
|