Introduction
In recent years, the incidence of tumours is
increasing and significant progress has been made in the early
diagnosis and comprehensive treatment of various tumours. However,
the presence of distant metastases from tumours seriously affects
the prognosis of the disease (1).
Bone marrow metastasis (BMM) refers to the metastasis of malignant
tumours originating from nonhematopoietic tissues to the bone
marrow (2). The nonhematopoietic
malignant tumour cells metastasize to the bone marrow via
heterogeneous dissemination or direct invasion to form metastases.
Subsequently, the bone marrow is infiltrated by cancer cells,
resulting in the destruction of the bone marrow structure and the
development of haematopoietic disorders (2). The clinical manifestations of BMMs are
complex and diverse. Various cases are initially treated in the
haematology department for haematological abnormalities, such as
anaemia or thrombocytopenia (3).
Neuroblastoma, Ewing's sarcoma and primitive neuroectodermal
tumours are the most common BMMs noted in paediatric patients
(4). BMMs from adult tumours are
general in breast cancer, prostate cancer, gastrointestinal
tumours, and lung cancer (5).
Certain patients are at a stage where the primary lesion is unknown
and a bone marrow biopsy may reveal BMMs, which may lead to a
definitive diagnosis. The prognosis of metastatic bone marrow
cancer is poor; rapid progression of disease seen in marrow
infiltration of medulloblastoma results in a median interval of 12
months between the detection of bone marrow disease and mortality
in adults (1); therefore, it is
necessary to enhance the awareness of this disease by improving the
early detection and diagnosis, as well as its treatment. This can,
in turn, improve the patients' quality of life and disease
prognosis, and prolong their survival. In the present study, the
clinical features of 52 cases of BMM are summarized and
reported.
Patients and methods
Patient selection
The patient data in the Affiliated Tumour Hospital
of Tianjin Medical University were retrospectively reviewed. A
total of 52 cases of patients with BMM were included with complete
follow-up from September 2010 to October 2021. All patients were
diagnosed based on bone marrow biopsy examination.
Data collection
Patient baseline and clinical data, including age,
sex, laboratory tests (routine blood, liver and kidney function,
lactate dehydrogenase, β2-microglobulin and bone marrow biopsy) and
imaging examination [ultrasound (Philips EPIQ Elite; Philips
Medical Systems B.V.) for superficial lymph nodes, computerized
tomography (CT; Siemens 08098027; Siemens AG) or positron emission
tomography (PET)-CT (GE Discovery PET/CT Elite; Cytiva) for chest,
abdomen and pelvic] were collected. For bone marrow cytology, 6–7
bone marrow smears were performed from bone marrow aspiration under
local anaesthesia and aseptically at the anterior or posterior
superior iliac spine, with Wright's staining at 25°C. Bone marrow
smears were viewed in full with an Olympus BX53 light microscope
(Olympus Corporation) at ×100 magnification and then re-examined at
×1,000 magnification to search for tumour cells. For bone marrow
biopsy a Dako H&E staining instrument (CoverStainer; Dako;
Agilent Technologies, Inc.). The operations were conducted at a
humidity of 20–85% and a temperature 15–30°C. Reagents included
Dako hematoxylin and eosin staining solutions (Dako; Agilent
Technologies, Inc.), 10% neutral formaldehyde, Besso dewaxing
(clearing agent), Beso Sealant, Dako H&E special reagents (Dako
Hematoxylin, Dako Eosin and Dako Bluing Buffer). The bone marrow
specimens were fixed in 10% neutral formaldehyde for at ≥6 h and
washed in water. They were then decalcified, dehydrated and
paraffin-embedded. Thickness of sections was 3 μm. The staining
procedure followed dewaxing and hydration of paraffin sections.
Sections were stained in hematoxylin for 1–3 min, rinsed in water.
and blued for 1–2 min, washed with water then stained with eosin
for 1–3 min, washed with water then dehydrated with 95% ethanol for
2 min followed by anhydrous ethanol twice for 2 min and xylene
twice for 2 min. Then the slides were sealed. The pathology was
observed using an Olympus BX53 light microscope (Olympus
Corporation) and the images captured at a ×200 and ×400×
magnification. The present study was performed following The
Declaration of Helsinki and applicable local regulatory
requirements and laws including Tianjin Medical University Cancer
Institute and Hospital for ethics approval and patient informed
consent (approval no. bc2022043).
Patient treatment
A total of 16 patients were not treated and the
remaining patients underwent the following treatment: i) Combined
chemotherapy, where the chemotherapy regimen was based on the
primary tumour and pathological type, and the range of the
chemotherapy cycles was 2–6; ii) radiotherapy, where radiation was
administered to a limited number of metastatic sites; iii) surgery,
which was performed following 3–5 courses of chemotherapy for
neuroblastoma; chemotherapy was continued following surgery for a
total of ≤12 courses; iv) autologous haematopoietic stem cell
transplantation (ASCT), which was performed for neuroblastoma with
partial remission; an v) support for symptomatic treatment, which
included red cell suspensions or platelet transfusion in patients
with anaemia or thrombocytopenia.
Efficacy and adverse effects
Following 30 days after all types of treatment,
PET-CT was utilized to evaluate the treatment efficacy. According
to the World Health Organization standards (6), the acute and subacute adverse cancer
drug reaction classification was also applied to evaluate the
adverse effects.
Statistical analysis
All data were analysed using SPSS version 18.0
(SPSS, Inc.). The survival curves were constructed using the
Kaplan-Meier method. Overall survival (OS) was defined as the
interval from the diagnosis of BMM to death or the end of
follow-up.
Results
Baseline characteristics
The present study recruited 30 male (58%) and 22
female (42%) patients. The age ranged from 4–85 yearswith the
median being 54 years. Of these, six cases were ≤20 years old, four
were 21–30 years old, six were 31–40 years old, eight were 41–50
years old, 11 were 51–60 years old, nine were 61–70 years old and
eight were 71–80 years old. A total of 17 patients were >60
years of age. The primary cancer types included the following:
Breast, prostate, lung, oesophageal, thyroid, endometrial and
gastric cancers, malignant melanoma, neuroblastoma and embryonal
rhabdomyosarcoma. The pathological types are shown in Table I. According to the TNM staging of
the tumour, stage IV was defined as the presence of BMMs and all
patients were classified as stage IV.
 | Table I.Distribution of primary tumour. |
Table I.
Distribution of primary tumour.
| Primary cancer | Number (%) |
|---|
| Breast | 15 (28.8) |
| Prostate | 9 (17.3) |
| Neuroblastoma | 7 (13.5) |
| Lung | 6 (11.5) |
| Gastric | 5 (9.6) |
| Colorectal | 4 (7.7) |
| Others | 6 (11.5) |
| Total | 52 |
Clinical features of the patients
The main clinical manifestation was moderate anaemia
in 35 patients, whereas six experienced severe anaemia. A total of
13 patients presented with scattered bleeding spots on the skin due
to thrombocytopenia. Anaemia and bleeding symptoms were more severe
as the disease progressed. Other symptoms included bone pain,
emaciation, fatigue and the corresponding symptoms caused by the
primary tumour. The majority of the patients were accompanied by
other site metastasis (33 patients with lymph node metastases, 18
patients with bone metastases, 12 patients with liver metastases,
four patients with pleural metastases, seven patients with
peritoneal metastases and one patient with central metastases). The
clinical features of the 52 patients with BMM are shown in Table II.
 | Table II.The clinical features of the 52 cases
of bone marrow metastasis. |
Table II.
The clinical features of the 52 cases
of bone marrow metastasis.
|
| Cancer type, N
(%) |
|---|
|
|
|
|---|
| Demographic and
clinical features | Breast | Prostate | Neuroblastoma | Lung | Gastric | Colorectal | Others |
|---|
| Sex | - | - | - | - | - | - | - |
| Male | - | 9 (17.3) | 3 (5.8) | 4 (7.7) | 3 (5.8) | 2 (3.8) | 3 (5.8) |
|
Female | 15 (28.8) | - | 4 (7.7) | 2 (3.8) | 2 (3.8) | 2 (3.8) | 3 (5.8) |
| Anemia | 13 (25) | 6 (11.5) | 5 (9.6) | 3 (5.8) | 5 (9.6) | 6 (11.5) | 4 (7.7) |
| Bleeding | 6 (11.5) | 2 (3.8) | 0 | 0 | 3 (5.8) | 2 (3.8) | 0 |
| Emaciation | 7 (13.5) | 3 (5.8) | 0 | 3 (5.8) | 4 (7.7) | 3 (5.8) | 0 |
| Fatigue | 5 (9.6) | 4 (7.7) | 1 (1.9) | 3 (5.8) | 4 (7.7) | 4 (7.7) | 3 (5.8) |
| Lymph node
metastasis | 8 (15.4) | 3 (5.8) | 5 (9.6) | 4 (7.7) | 6 (11.5) | 4 (7.7) | 3 (5.8) |
| Visceral
metastases | 3 (5.8) | 0 | 0 | 3 (5.8) | 4 (7.7) | 2 (3.8) | 0 |
| Soft tissue
metastases | 0 | 0 | 0 | 4 (7.7) | 3 (5.8) | 4 (7.7) | 0 |
| Bone metastases
(bone pain) | 7 (13.5) | 5 (9.6) | 0 | 1 (1.9) | 3 (5.8) | 2 (3.8) | 0 |
Clinical examination
Patients underwent the following clinical
examinations: i) Complete blood count. A total of 42 patients
presented with haemoglobin reduction and the minimum haemoglobin
concentration was 45 g/l. A total of six patients presented with
severe anaemia and accounted for 11.5% of the total sample size.
The majority of them presented with normochromic anaemia. A total
of 27 patients presented with thrombocytopenia. The minimum
platelet count was 5×109/l. The white blood cell count
ranged from 1.27×109/l to 12.74×109/l. The
white blood cell count was lower than normal in eight patients; ii)
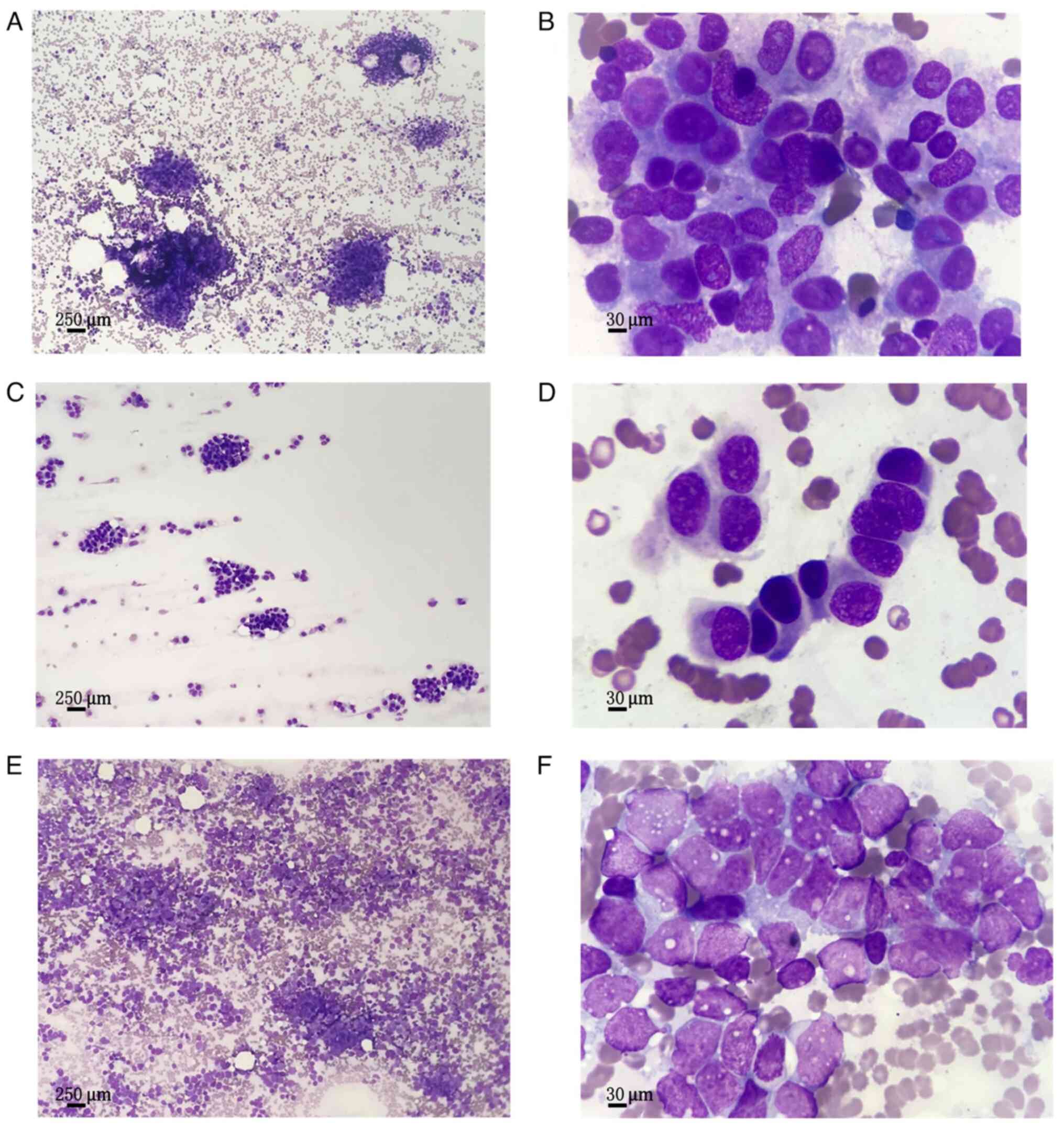
morphological characteristic of the bone marrow. Metastatic cancer
cells were detected in bone marrow smears of all the examined
patients. Scattered or clustered metastatic cancer cells were found
in varying numbers on bone marrow smears, mostly at the head, tail
or margins of the smears and in clusters of several or hundreds of
metastatic cancer cells known as cancer nests (Fig. 1). Because lung cancer and breast
cancer are more prevalent in male and female, respectively, these
two representative tumours were chosen; prostate cancer, which is
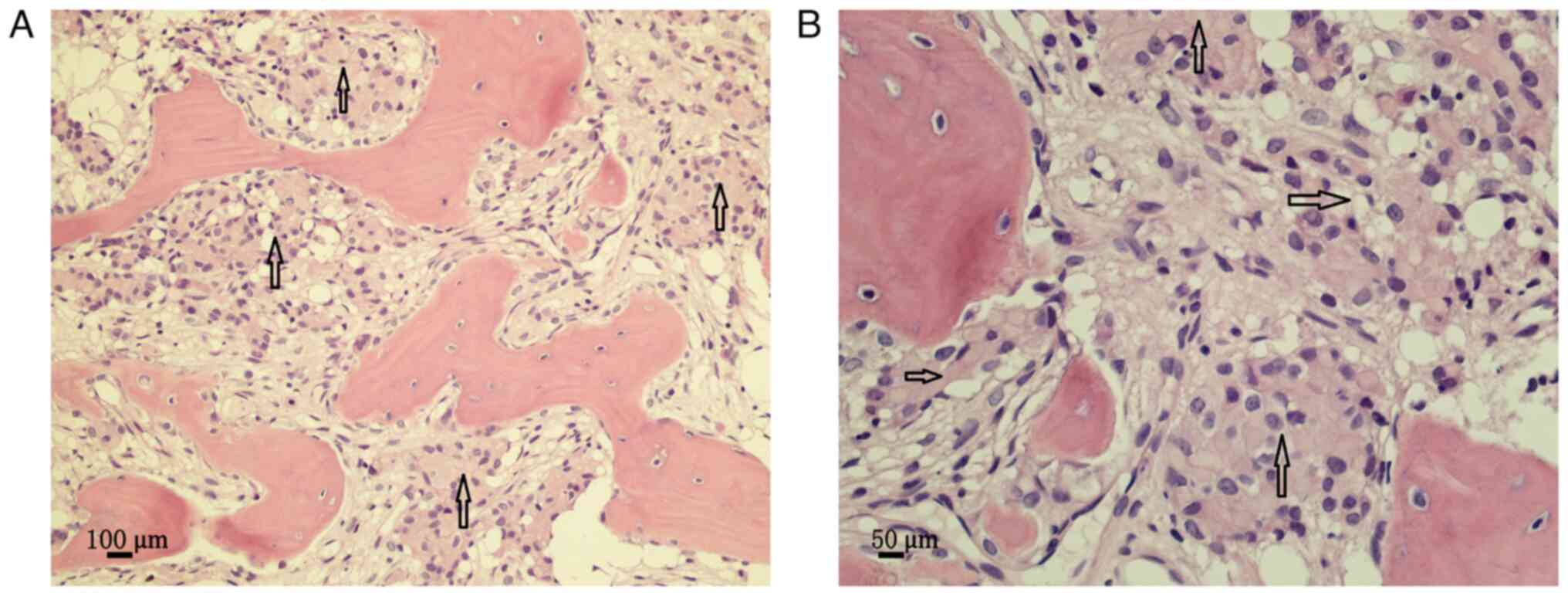
representative of male patients, was also selected; iii) bone
marrow pathology. The cancerous tissues were in the form of nests
or cords, ‘squeezing out’ hematopoietic tissue or space-occupying
hyperplasia. There were hematopoietic cells, such as granulocytes,
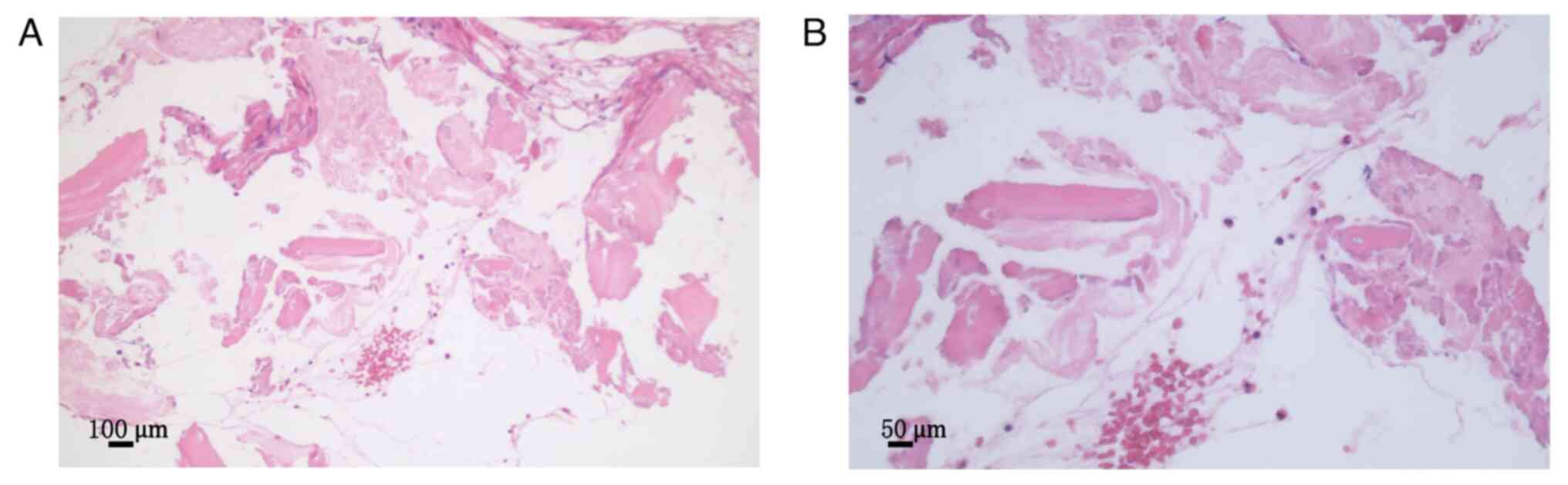
erythrocytes and megakaryocytes, around the cancer nest (Fig. 2). A post-treatment bone marrow
biopsy is shown in Fig. 3, which
indicates a normal bone marrow.
Patient treatment outcome
A total of 13 patients underwent chemotherapy
treatment and the median course of chemotherapy was four (2–6).
Following chemotherapy, the following clinical information was
collected: Five patients achieved complete remission (CR), 11
patients presented with partial remission, 15 patients experienced
stable disease (SD) and 21 patients developed progressive disease.
The total effective rate was 30%. Anaemia symptoms were improved in
31 patients following chemotherapy, 15 of whom demonstrated normal
haemoglobin levels. Thrombocytopenia was elevated in 25 patients
compared with the pre-chemotherapy group and platelet levels were
normal in 13 patients.
Survival outcome
A total of 52 patients were followed up until
January 2022 and no patient was lost during the follow-up. The
median follow-up period was 10 months (2–18 months). At the end of
the follow-up period, six cases were diagnosed as CR, of whom four
were neuroblastomas and the remaining were breast and prostate
cancers. A total of six patients were in partial remission, of whom
four were prostate and two breast cancer cases. A total of five
patients achieved SD, of whom two and three patients presented
prostate and breast cancer, respectively. A total of 35 patients
did not survive due to disease progression, including 18 patients
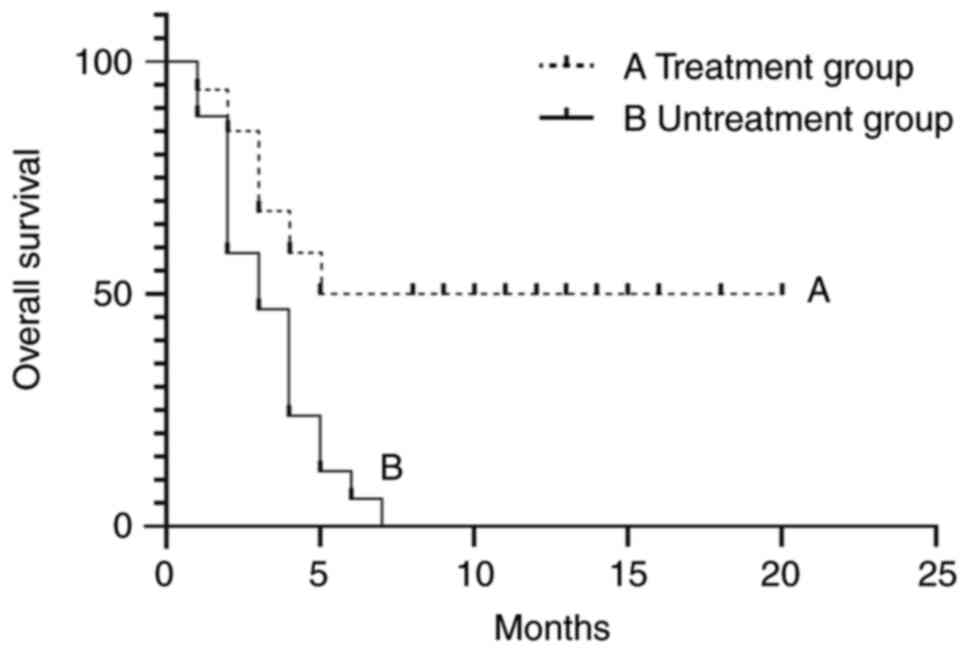
who were not treated. The median OS of patients treated with
antitumor therapy was significantly higher than that of untreated
patients (11.5 vs. 3.3 months P<0.01; Fig. 4).
Adverse effects related to
treatment
During therapy, IV-grade myelosuppression occurred
in 28 patients. Following treatment with recombinant human
granulocyte colony-stimulating factor, the leucocyte levels
returned to normal. Adverse reactions of the digestive system, such
as nausea and vomiting, occurred in 36 patients. Serve pneumonia
was observed in eight cases, which was alleviated after the
combination of imipenem and fluconazole treatment.
Discussion
The clinical manifestations of BMM are complex and
diverse due to the presence of different primary cancers; however,
a series of symptoms are caused by cancer cell infiltration into
the bone marrow, such as anaemia, thrombocytopenia, and fatigue
(3). Haematological changes are
often the earliest or main clinical manifestation of bone marrow
metastatic carcinoma (3). Anaemia
or thrombocytopenia result from a reduction in normal
haematopoiesis and a decrease in haematopoietic cells due to the
secretion of inhibitory cytokines by metastatic cancer cells or the
inhibition of the release of haematopoietic stimulating factors by
bone marrow stromal cells through cell-to-cell contact (7). When extramedullary tumour cells
metastasize to the bone marrow, the normal haematopoietic system is
inhibited and disrupted by the proliferation of cancer cells
(8). In the present study, 41
patients presented with anaemia and 27 with thrombocytopenia.
Therefore, anaemia or thrombocytopenia were the most common and
dominant clinical manifestations of BMM.
When patients are found to present with unexplained
blood abnormalities, the possibility of BMMs from malignant tumours
must be considered. Of the 52 patients, seven were diagnosed with
malignant tumours due to haematological abnormalities found at the
time of examination; metastatic cancer cells were found through
bone marrow aspiration and subsequently, the primary focus further
confirmed the diagnosis of malignancy. An additional 45 patients
for different primary malignancies with BMM presented due to
haematological abnormalities. When an abnormal hemogram occurs in a
patient with malignant tumours, the possibility of the patient
experiencing BMMs must be considered to facilitate earlier
detection and treatment. Bone marrow smear and bone marrow biopsy
are the gold standard for the diagnosis of BMMs (9). However, it is not possible to identify
tumour cells in a single bone marrow aspiration, since BMMs are
multifocal and myelofibrosis occurs which increases the difficulty
of obtaining the bone marrow (10).
Multi-site bone marrow aspiration should be performed if necessary.
In 52 patients, BMMs were confirmed through immunohistochemical
analysis through bone marrow biopsy, which is important in the
diagnosis of metastatic cancer of the bone marrow.
BMM occurs in breast, prostate, lung and gastric
cancers, and in neuroblastoma; the incidence of BMM from breast
cancer is significantly higher than that of other tumours (3). In the present study, a total of 15
patients exhibited breast cancer, accounting for 29%. Kopp et
al (11) demonstrated that a
high proportion of bone marrow metastases from breast cancer was
associated with a predisposition to bone metastases from breast
cancer. In the current study, 29 and 17% of patients presenting
with breast or prostate cancer, respectively, developed bone
metastases. When patients develop bone metastases, they may present
with pathological fractures, hypercalcemia, bone pain and spinal
cord compression. Bone metastasis is a complex multistep process in
which disseminated tumour cells extravasate, enter the bone marrow
compartment and occupy one of two specialized microenvironments or
niches which consist of perivascular and endothelial cells of the
sinusoids in the bone marrow and the endosteal niche. This step is
followed by a period of dormancy in which the disseminated tumour
cells adapt, survive and reside in the bone for a long period,
possibly years or even decades (12,13).
Therefore, when bone metastases occur, patients are not necessarily
accompanied by BMMs. The third step is the reactivation of cancer
cells that have acquired the ability to escape from dormancy,
followed by their outgrowth to form micrometastasis, eventually
leading to the development of overt bone metastasis (14). In the present study, bone metastases
occurred mainly in patients with breast and prostate cancers. The
mechanism of BMM development may be based on the ability of the
tumour cells to overexpress chemokine receptor (CXCR) 4 and induce
tumour cell invasion and homing to the bone marrow via the
chemokine C-X-C motif ligand (CXCL)12/CXCR4 signalling pathway
(15). Over the last few years, the
potential pathogenetic role of bone marrow adipocytes (BMAds) and
their molecular basis have been intensively investigated in marrow
neoplastic diseases, such as haematological malignancies and cancer
metastasis. Therefore, it has been shown that BMAdscan modulate the
migration and aggressiveness of neoplastic cells (16). Dello Spedale Venti et al
(17) reported the possibility of
BMAds being associated with tumour BMM.
Metastatic bone marrow cancer is a systemic,
incurable disease with a poor prognosis which indicates that the
patient is at an advanced stage. The median survival time of bone
marrow metastatic carcinoma was 1.5–3 months (18). The reasons for the poor treatment
outcomes were as follows: i) Patients who had received chemotherapy
several times could have developed resistance to the tumour and
patients with BMMs had poor bone marrow tolerance; therefore
chemotherapeutic drugs which caused lower myelosuppression and
required appropriate reductions in their dose were required to be
selected as a treatment; ii) patients with poor body condition
(with anaemia and thrombocytopenia) were prone to systemic
infections, bleeding and other complications; iii) patients with an
unknown primary focus could not be effectively treated with an
antitumor therapy. It was previously proposed that metastatic
cancer of the bone marrow could exhibit a poor prognosis and that
the toxic side effects of antitumor therapy could reduce patient
survival (19). A previous study
indicated that the application of antitumor therapy could improve
disease prognosis (20). The
anaemia and thrombocytopenia of patients with BMMs could not be
fundamentally altered by blood transfusion. A recent study showed
that antitumor therapy could significantly improve symptoms, such
as anaemia and control disease progression (21). In the present study, anaemia and
thrombocytopenia were improved in 30 patients following antitumor
treatment. There were only six patients who remained in CR at the
end of follow-up, of whom four exhibited paediatric neuroblastoma
following chemotherapy (or combined radiotherapy), surgery and
autologous hematopoietic stem cell transplantation; the remaining
two were cases of breast and prostate cancers, respectively. For
paediatric neuroblastoma, ASCT could delay disease progression and
prolong the child's survival time when surgery was unsatisfactory
and the malignant cells could not be eliminated through
radiotherapy and chemotherapy (22). The long-term survival rate for
patients with paediatric neuroblastoma who developed BMMs was poor
(23). According to research data
from the last decade, the 3-year OR rate of the single ASCT group
was 74.1% (24). Consequently,
paediatric neuroblastoma with BMMs should be treated aggressively.
Demir et al (25) reported
that patients with breast cancer and BMM who accepted antitumor
therapy survived longer than those who did not (17.3 vs. 0.93
months, respectively). Antiandrogen therapy was also shown to be
effective in treating BMMs from prostate cancer (26). In the present study, by the end of
the follow-up period, six patients were in partial remission, of
whom four were cases with prostate cancer and two with breast
cancer. The prognosis of breast and prostate cancers was slightly
improved compared with that of other tumours. The median OS for
untreated patients was only 3.3 months, while it was 11.5 months
for treated patients. Antitumor therapy could improve OS in
patients with BMM. For patients with BMM, it is important to
actively evaluate the patient's condition and select the
appropriate treatment plan for improving the disease prognosis.
In conclusion, although the prognosis for metastatic
bone marrow cancer is poor, its treatment can improve patient
survival. With the development of genetic testing technology,
targeted drugs may offer novel opportunities for patients with
metastatic bone marrow cancer in the future.
Acknowledgement
Not applicable.
Funding
This study was supported by Funded by Tianjin Medical Discipline
(Specialty) Construction Project (approval no. TJYXZDXK-009A) and
by Tianjin Medical University Cancer Institute and Hospital ‘The
14th Five-Year’ Summit Subject Support Plan (approval no.
7-2-12-1;YF Wang)
Availability of data and materials
The datasets used or analysed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HY performed the clinical trial study and drafted
the manuscript. TY and WX performed the clinical data collection.
ZC performed the statistical analysis. FH conceived the study and
participated in its design, and helped to draft the manuscript. HY
and FH confirm the authenticity of all the raw data. All authors
read and approved the final version of the manuscript.
Ethics approval and consent to
participate
The article was a retrospective study and had been
approved by the Medical Ethics Committee of Tianjin Cancer
Institute and Hospital (approval no. bc2022043).
Patient consent for publication
Written informed consent was obtained from the
patients for publication of this case report and any accompanying
images. A copy of the written consent is available from the
Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Clifton BA, Neill JS and Anderson MD:
Treatment of Shh medulloblastoma with extraneural metastasis to the
bone marrow. Current problems in cancer: Case Reports.
4:1001042021. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Shinden Y, Sugimachi K, Tanaka F,
Fujiyoshi K, Kijima Y, Natsugoe S and Mimori K: Clinicopathological
characteristics of disseminated carcinomatosis of the bone marrow
in breast cancer patients. Mol Clin Oncol. 8:93–98. 2018.PubMed/NCBI
|
|
3
|
La Gioia A, Fiorini F and La Gioia N: Bone
marrow involvement by metastatic invasive lobular breast cancer.
Int J Lab Hematol. 44:40–41. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fan HJ, Huang C, Su Y, Wang XD, Zhou YC,
Duan C, Zhao W, Zhao Q, Jin M and Ma XL: Clinical characteristics
and prognosis of high-risk neuroblastoma with bone marrow
metastasis in children. Zhonghua Er Ke Za Zhi. 57:863–869. 2019.(In
Chinese). PubMed/NCBI
|
|
5
|
Rani HS, Hui M, Manasa P, Uppin SG, Uppin
MS, Paul TR and Sadashivudu G: Bone marrow metastasis of solid
tumors: A study of 174 cases over 2 decades from a single
institution in India. Indian J Hematol Blood Transfus. 38:8–14.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Edwards IR and Aronson JK: Adverse drug
reactions: Definitions, diagnosis, and management. Lancet.
356:1225–1229. 2000. View Article : Google Scholar
|
|
7
|
Rana NA, Mahmood A, Robert HM, Zahir S,
Asghar MB and Riaz S: Laboratory evaluation and pathological
features of bone marrow metastasis in non-haematological
malignancies. J Coll Physicians Surg Pak. 32:1367–1369. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hofbauer LC, Bozec A, Rauner M, Jakob F,
Perner S and Pantel K: Novel approaches to target the
microenvironment of bone metastasis. Nat Rev Clin Oncol.
18:488–505. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hong YM, Yoon KT, Cho M, Kang DH, Kim HW,
Choi CW, Park SB, Heo J, Woo HY, Lim W and Islam SMB: Bone marrow
metastasis presenting as bicytopenia originating from
hepatocellular carcinoma. Clin Mol Hepatol. 22:267–271. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shi XB, Deng WX and Jin FX: Bone marrow
metastatic neuroendocrine carcinoma with unknown primary site: A
case report and review of the literature. World J Clin Cases.
10:11074–11081. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kopp HG, Krauss K, Fehm T, Staebler A,
Zahm J, Vogel W, Kanz L and Mayer F: Symptomatic bone marrow
involvement in breast cancer-clinical presentation, treatment, and
prognosis: A single institution review of 22 cases. Anticancer Res.
31:4025–4030. 2011.PubMed/NCBI
|
|
12
|
Pan H, Gray R, Braybrooke J, Davies C,
Taylor C, McGale P, Peto R, Pritchard KI, Bergh J, Dowsett M, et
al: 20-year risks of breast-cancer recurrence after stopping
endocrine therapy at 5 years. N Engl J Med. 377:1836–1846. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Park SH, Keller ET and Shiozawa Y: Bone
marrow microenvironment as a regulator and therapeutic target for
prostate cancer bone metastasis. Calcif Tissue Int. 102:152–162.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ripp J, Diab O, Woodroof J and Sun W:
Colorectal adenocarcinoma presenting with isolated metastasis to
the cortical bone and bone marrow: A case report and review of the
literature. Clin Colorectal Cancer. 20:e150–e154. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Jafari A, Fairfield H, Andersen TL and
Reagan MR: Myeloma-bone marrow adipocyte axis in tumour survival
and treatment response. Br J Cancer. 125:775–777. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fairfield H, Dudakovic A, Khatib CM,
Farrell M, Costa S, Falank C, Hinge M, Murphy CS, DeMambro V,
Pettitt JA, et al: Myeloma-modified adipocytes exhibit metabolic
dysfunction and a senescence-associated secretory phenotype. Cancer
Res. 81:634–527. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Dello Spedale Venti M, Palmisano B,
Donsanten S, Farinacci G, Adotti F, Coletta I, Serafini M, Corsi A
and Riminucci M: Morphological and immunophenotypical changes of
human bone marrow adipocytes in marrow metastasis and
myelofibrosis. Front Endocrinol (Lausanne). 13:8823792022.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
DA Silva A, Levy C, Allouache D, Hrab I,
Morel A, Faveyrial A, Gunzer K, Johnson A, Segura C, Licaj I, et
al: Efficacy and safety of weekly paclitaxel in breast cancer with
symptomatic bone marrow infiltration. Anticancer Res. 40:2955–2960.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Braun S, Vogl FD, Janni W, Marth C,
Schlimok G and Pantel K: Evaluation of bone marrow in breast cancer
patients: Prediction of clinical outcome and response to therapy.
Breast. 12:397–404. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Buschhaus JM, Humphries BA, Eckley SS,
Robison TH, Cutter AC, Rajendran S, Haley HR, Bevoor AS, Luker KE
and Luker GD: Targeting disseminated estrogen-receptor-positive
breast cancer cells in bone marrow. Oncogene. 39:5529–5662. 2020.
View Article : Google Scholar
|
|
21
|
Arya L, Sundriyal D, Bhandari R,
Srivastava R and Sehrawat A: Bone marrow metastases from solid
organ cancer in adults. Indian J Surg Oncol. 12:545–548. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Mora J: Autologous stem-cell
transplantation for high-risk neuroblastoma: Historical and
critical review. Cancers (Basel). 14:25722022. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Moreno L, Guo D, Irwin MS, Berthold F,
Hogarty M, Kamijo T, Morgenstern D, Pasqualini C, Ash S, Potschger
U, et al: A nomogram of clinical and biologic factors to predict
survival in children newly diagnosed with high-risk neuroblastoma:
An international neuroblastoma risk group project. Pediatr Blood
Cancer. 68:e287942021. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Park JR, Kreissman SG, London WB, Naranjo
A, Cohn SL, Hogarty MD, Tenney SC, Haas-Kogan D, Shaw PJ, Kraveka
JM, et al: Effect of tandem autologous stem cell transplant vs
singletransplant on event-free survival in patients with high-risk
neuroblastoma: A randomized clinical trial. JAMA. 322:746–755.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Demir L, Akyol M, Bener S, Payzin KB,
Erten C, Somali I, Can A, Dirican A, Bayoglu V, Kucukzeybek Y, et
al: Prognostic evaluation of breast cancer patients with evident
bone marrow metastasis. Breast J. 20:279–287. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hiroshige T and Eguchi Y: Prostate cancer
with disseminated carcinomatosis of the bone marrow: Two case
reports. Mol Clin Oncol. 7:233–236. 2017.PubMed/NCBI
|