Introduction
The duodenum, 25–30 cm in length, is the widest
portion of the small bowel and is divided into four parts (1–3). The
first part of the duodenum consists of the 2.5-cm-long
intraperitoneal segment as a continuation of the pylorus, which is
called the duodenal bulb, and the 2.5-cm-long retroperitoneal
segment, which ends at the superior duodenal flexure (1–3).
Regarding the blood supply to the duodenal bulb, which is the
portion utilized in anastomosing the duodenum and remnant stomach
following distal gastrectomy, Hentati et al (4) reported that all of the arterial
pedicles reached the duodenal bulb on its posterior wall and
thereafter spread along its anterior wall. In brief, the posterior
wall of the duodenal bulb is considered to be the mesenteric side,
in which the gastroduodenal artery (GDA) is the marginal artery and
the superior duodenal arteries branching off from the GDA are the
vasae rectae. In addition, as with the small intestine, it is
assumed that these superior duodenal arteries branching off from
the GDA reach the duodenal bulb on its posterior wall and then
spread along its anterior wall, and they anastomose at its anterior
wall, which is considered the antimesenteric side (5).
Over the past 20 years, totally laparoscopic distal
gastrectomy (TLDG), in which lymph node dissection, transection of
the duodenal bulb and stomach, and anastomosis are carried out
intracorporeally, has been developed (6–11), and
intracorporeal gastroduodenostomy using an endoscopic linear
stapler (ELS) has been performed since 2002 (6).
In intracorporeal linear-stapled gastroduodenostomy
following TLDG, the blood supply of the duodenal wall between the
transecting staple line and the anastomotic staple line needs to be
considered because both transection of the duodenal bulb and the
gastroduodenostomy are performed using an ELS and the duodenal wall
between the staple lines can be ischemic after the anastomosis
(6). Since it needs to be decided
intraoperatively whether this duodenal site is preserved or
removed, the present review discusses the technical differences
among several procedures for intracorporal linear-stapled
gastroduodenostomy following TLDG, classifying them into two groups
based on the intraoperative management of the duodenal wall between
the transecting staple line and anastomotic staple line. The
present review was approved by the Institutional Review Board of
Otori Stomach and Intestines Hospital (Sakai, Japan) and the
Institutional Review Board of Hokusetsu-Miki Hospital (Suita,
Japan) (both approval no. 23000001).
Intracorporeal linear-stapled
gastroduodenostomy with preservation of the duodenal wall between
the transecting staple line and anastomotic staple line
Delta-shaped gastroduodenostomy
(DSG)
Kanaya et al (6,7) first
reported DSG in Billroth I (B-I) reconstruction following TLDG.
Following their reports, several studies have described the
performance of this anastomotic technique (8–20).
When performing the transection of the duodenal bulb and
gastroduodenostomy in DSG, the operator was positioned at the right
side of the patient, with the first assistant at the left side and
the laparoscopist between the legs of the patient. Thus, all of the
linear staples were performed by the first assistant using their
left hand within the surgical field set up by the operator
(6–20). The duodenal bulb was transected in a
posteroanterior direction, that is, from the mesenteric side to the
antimesenteric side (6–20). After the operator had dissected
several cranial supraduodenal vessels and created the space
required for insertion of the ELS fork around the cranial wall of
the duodenal bulb, this wall and the posterior wall of the remnant
stomach were anastomosed by one linear staple so that the duodenal
and gastric walls between the transecting staple lines and
anastomotic staple became as wide as possible (6–20).
Only the ELS entry hole was closed by one or two linear staples,
and thus, the duodenal wall between the transecting staple line and
anastomotic staple line was preserved in DSG (6–20). We
hypothesized that although the blood supply via the remnant cranial
supraduodenal vessels is blocked by the anastomotic linear staple,
the blood supply of this area in the DSG is assumed to be retained
via the caudal supraduodenal vessels because the caudal and cranial
supraduodenal vessels anastomosed at the anterior wall, that is, at
the antimesenteric side (4,5).
Some authors have expressed concern that an
insufficient supply of blood to the duodenal wall between the
transecting staple line and anastomotic staple line in DSG could be
caused by unsuccessful transection of the duodenal bulb in a
posteroanterior direction and the extensive dissection of
supraduodenal vessels (11,17,21–25).
Iwasaki et al (24)
indicated that the twisting of the duodenal bulb at the
posteroanterior transection is technically demanding. In DSG, to
obtain an adequate anastomotic area for the purpose of preventing
anastomotic stenosis, the unsuccessful posteroanterior transection
of the duodenal bulb due to its incomplete twisting may lead to
extensive dissection of the supraduodenal vessels, that is,
dissection of not only the cranial but also the caudal
supraduodenal vessels (24).
Similarly, when the duodenal bulb diameter is relatively short,
extensive dissection of the supraduodenal vessels can be performed
to obtain an adequate anastomotic area (26).
Modified DSG (mDSG) with the operator
positioned between the legs of the patient
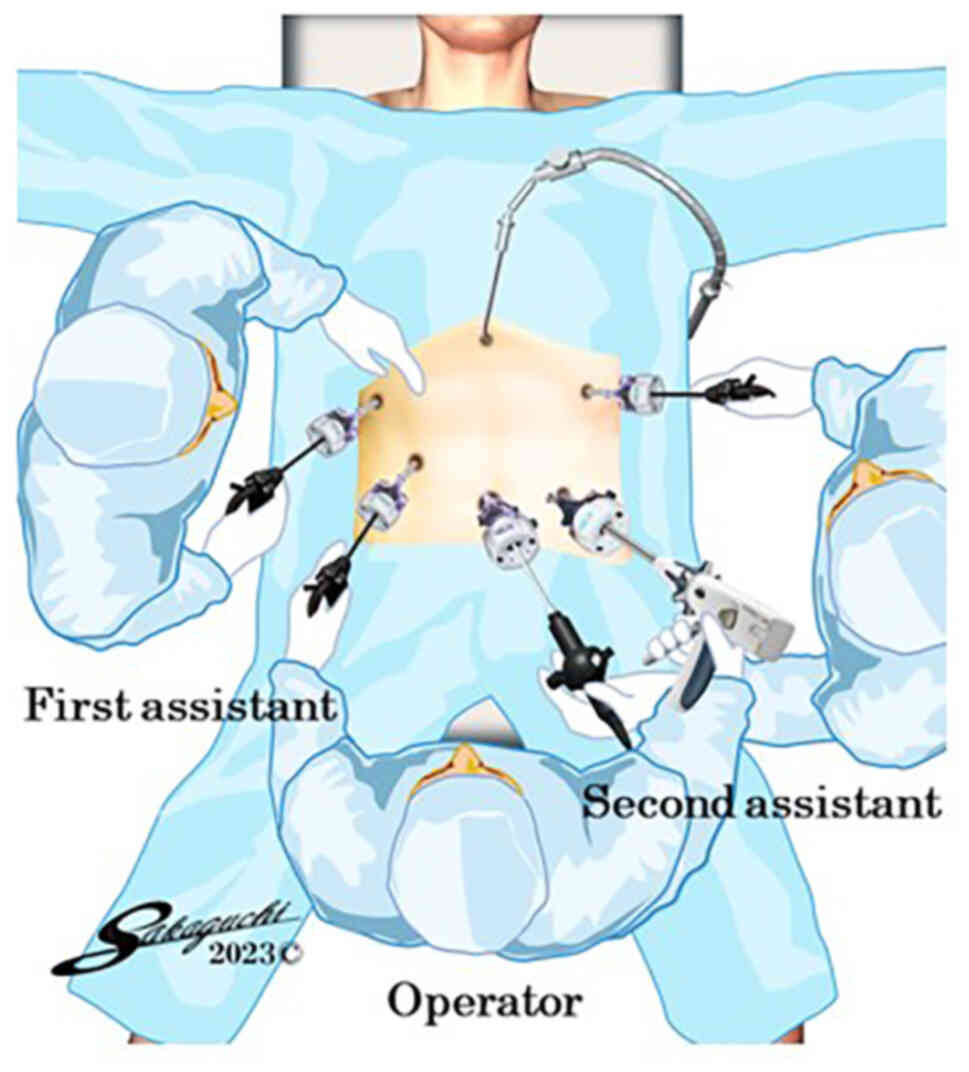
Our previous study in 2020 described an mDSG
technique with the operator positioned between the legs of the
patient (26). In this technique,
the operator was positioned between the legs of the patient, with
the first assistant manipulating a laparoscope at the left side of
the patient and the second assistant at the right side, when
performing transection of the duodenal bulb and gastroduodenostomy
in this procedure (Fig. 1).
Therefore, within the surgical field set up by the two assistants,
all of the linear staples were performed by the operator using
their right hand with the assistance of their left hand. The
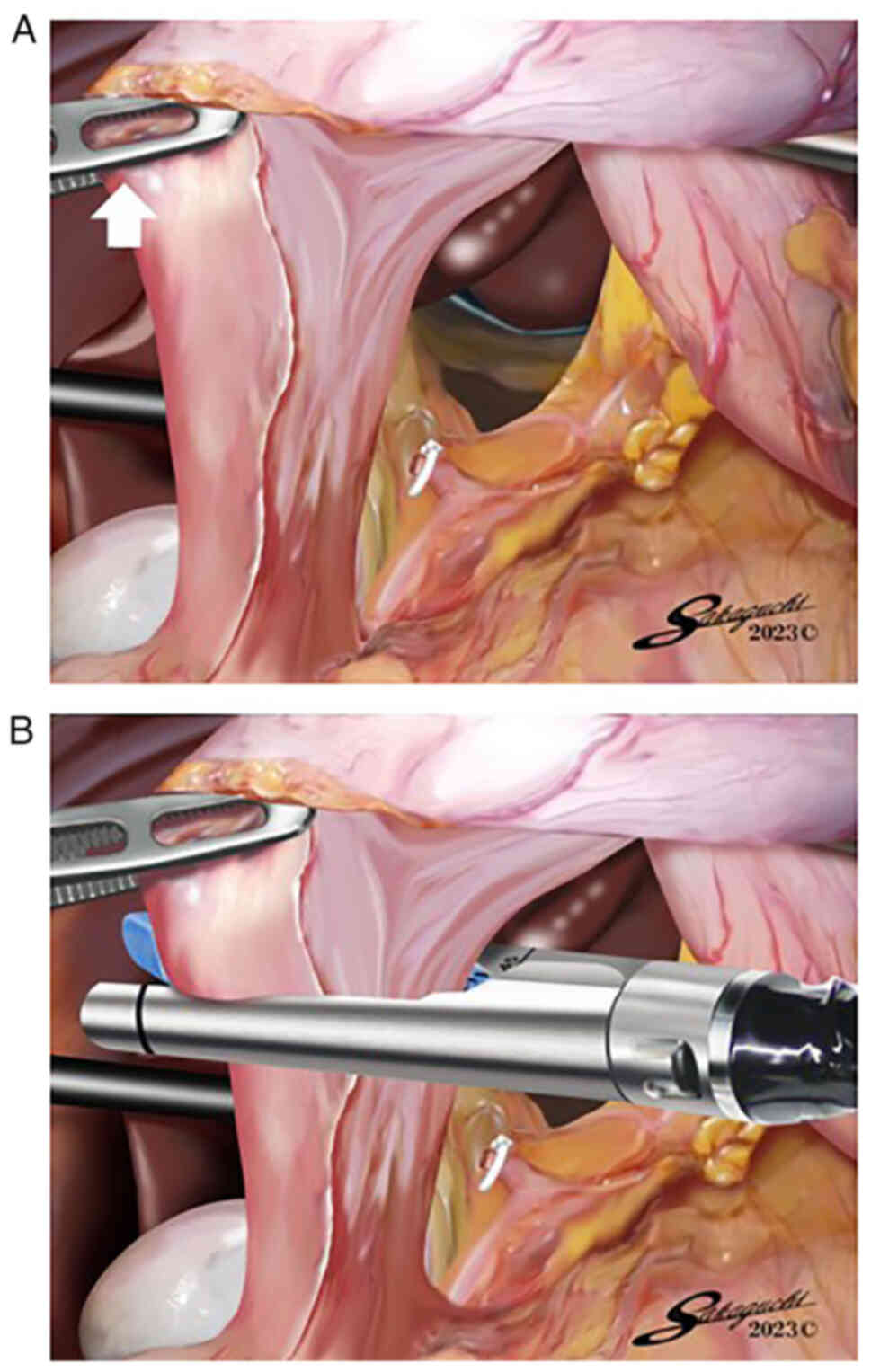
operator retracted the pyloric ring externally with the left hand,
while the first assistant elevated the posterior wall of the
stomach ventrally and the second assistant elevated the liver
cranially (Fig. 2A), and the
operator transected the duodenal bulb with the right hand using one
ELS in a posteroanterior direction, that is, from the mesenteric
side to the antimesenteric side (Fig.
2B). The posterior wall of the duodenal bulb is considered to
be the mesenteric side, in which the GDA is the marginal artery and
the superior duodenal arteries branching off from the GDA are the
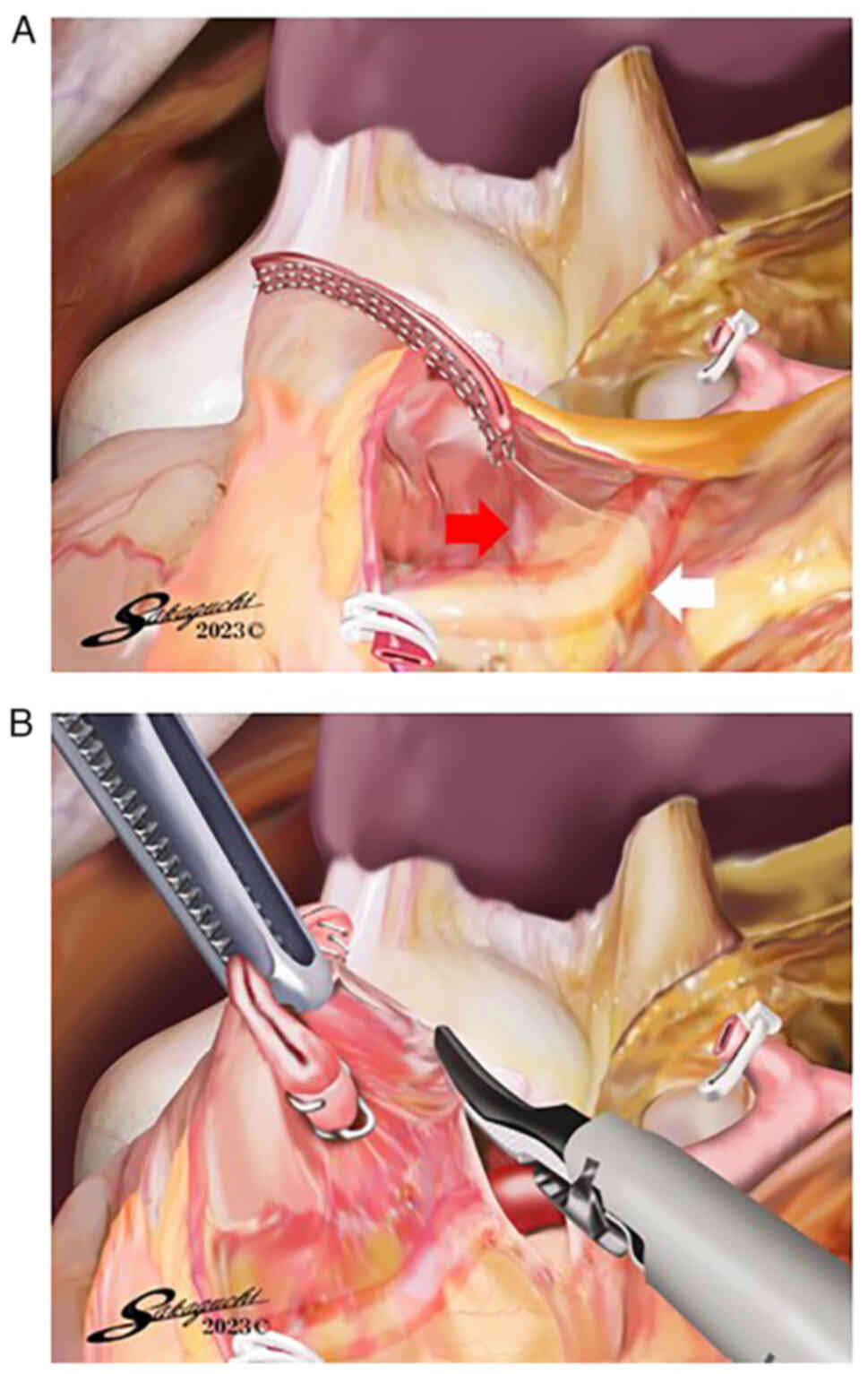
vasae rectae (Fig. 3A) (4). After the operator dissected several
cranial supraduodenal vessels branching off the GDA and created the
space required for insertion of the ELS fork around the cranial
wall of the duodenal bulb (Fig.
3B), the operator performed linear stapling of the cranial wall
of the duodenal bulb and the posterior wall of the remnant stomach
as follows: i) Insertion of the cartridge of one 45-mm ELS into the
remnant stomach entirely with the right hand, while the first
assistant pulled the staple line of the remnant stomach externally;
ii) insertion of the fork of the ELS into the duodenal bulb as far
as possible with the right hand, while pulling the staple line of
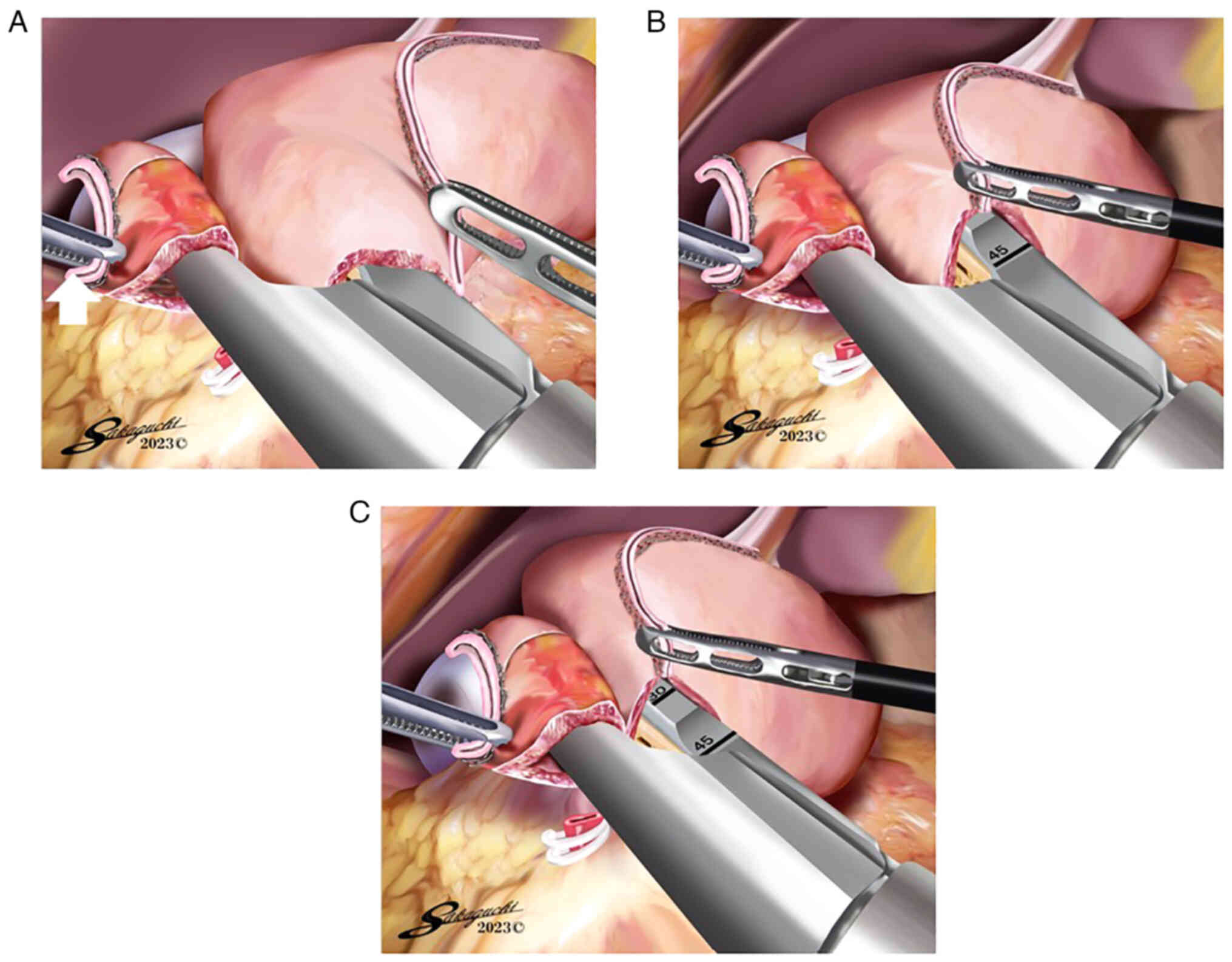
the duodenum externally with the left hand (Fig. 4A); and iii) after the operator and
first assistant changed the position of the duodenal bulb and
remnant stomach without creating a gap (Fig. 4B), the operator fired the ELS with
the right hand so that the duodenal and gastric walls between the
transecting staple line and anastomotic staple line became as wide
as possible (Fig. 4C).
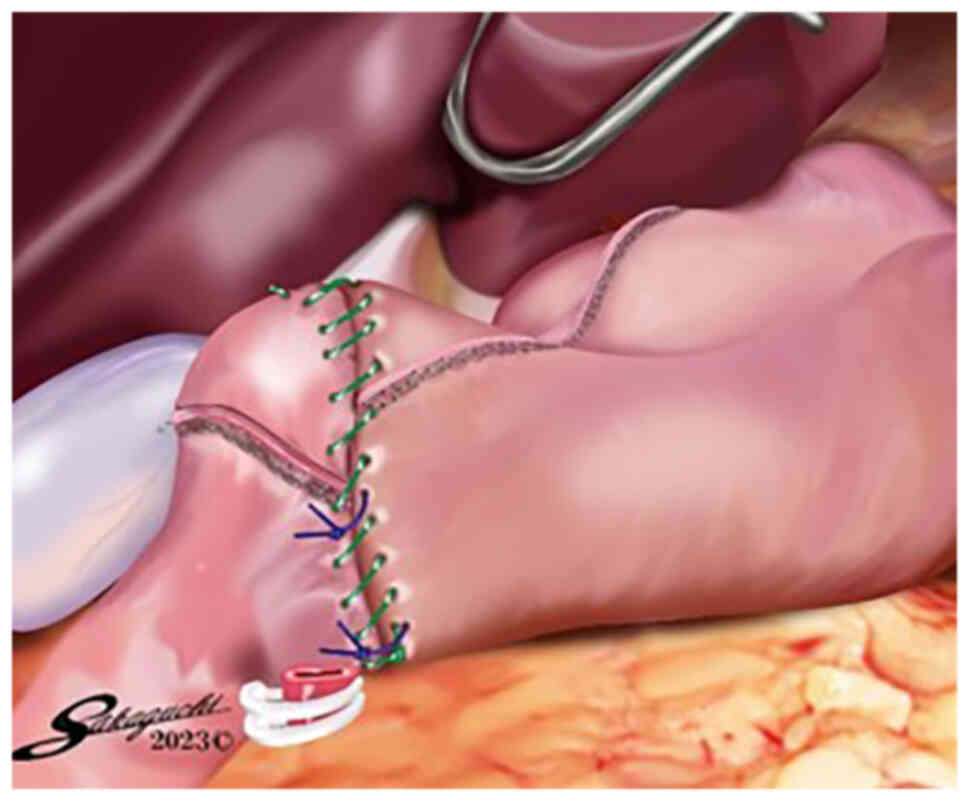
Subsequently, to ensure that the anastomotic area was as wide as
possible, the operator closed the ELS entry hole using a
single-layer full-thickness hand suturing technique with knotted
sutures and a knotless barbed suture. Finally, the mDSG in TLDG was
completed (Fig. 5).
In our previously reported patient series (35
cases), there was no occurrence of postoperative anastomotic
leakage, and the blood supply of the preserved duodenal wall
between the transecting staple line and anastomotic staple line was
considered to be retained (26).
The factors behind this result were hypothesized to be: i) Within
the surgical field set up by the two assistants, the operator was
able to transect the duodenal bulb in a posteroanterior direction
with more certainty by manipulating the ELS with the right hand
with the assistance of the left hand; and ii) no additional
dissection of the supraduodenal vessels was carried out even if the
duodenal bulb diameter was relatively short and an adequate staple
length between the cranial wall of the duodenal bulb and the
posterior wall of the remnant stomach was not obtained.
Overlap gastroduodenostomy (OG)
Several studies have reported OG in B-I
reconstruction following TLDG (25,27–31).
The duodenal bulb was transected from the greater curvature side to
the lesser curvature side (25,27,29–31),
or from the posterior side to the anterior side (28). Before the gastroduodenostomy, no
dissection of the supraduodenal vessels aimed at creating the space
required for insertion of the ELS fork around the duodenum was
performed (25,27–31).
The anterosuperior side or anterior wall of the first part of the
duodenum and the greater curvature side or posterior wall of the
remnant stomach were anastomosed by one linear staple so that the
anastomotic staple line was perpendicular to the transecting staple
line in the duodenum (25,27–31).
Only the ELS entry hole was closed using one linear staple
(25,27–29,31) or
hand suturing (30), and thus, the
duodenal wall between the transecting staple line and anastomotic
staple line was preserved in OG. We hypothesized that in OG, the
blood supply of this area is considered to be retained because the
blood supply of this area via the supraduodenal vessels branching
from the GDA is not blocked by the anastomotic linear staple due to
the anastomotic staple line being perpendicular to the transecting
staple line (4,5). However, there is a concern that an
adequate anastomotic area might not be obtained if the length of
the first part of the duodenum is relatively short (1–3).
Intracorporeal linear-stapled
gastroduodenostomy with removal of the duodenal wall between the
transecting staple line and anastomotic staple line
Intracorporeal triangular anastomotic
technique (INTACT)
Omori et al (22) and Yanagimoto et al (23) reported the INTACT as one type of
intracorporeal linear-stapled gastroduodenostomy. The duodenal bulb
was transected from the greater curvature side to the lesser
curvature side (22,23). Before the gastroduodenostomy, as in
OG, no dissection of the supraduodenal vessels aimed at creating
the space required for insertion of the ELS fork around the
duodenum was performed (22,23).
The posterior walls of the duodenum and the remnant stomach were
anastomosed by one linear stapling so that the anastomotic staple
line was parallel to the transecting staple line in the duodenum
and the end of the transecting staple line in the remnant stomach
(22,23). Removal of the areas between these
staple lines and closure of the ELS entry hole were performed
simultaneously with one or two linear staples (22,23).
As a result, a physiological triangular end-to-end anastomosis with
no need for twisting was completed (22,23).
In the INTACT, the extent of ischemia of the
duodenal wall is considered to be clearly identifiable during the
anastomosis because the blood supply of the duodenal posterior wall
between the transecting staple line and anastomotic staple line via
the supraduodenal vessels branching from the GDA is blocked by the
anastomotic linear stapling due to these staple lines being
parallel to each other (22,23).
However, because it is reported that the area of the triangular
end-to-end colocolostomy is considered to be prescribed by the
colon diameter (32), there is a
concern that, in the INTACT, an adequate anastomotic area might not
be obtained if the duodenal bulb diameter is relatively short
(1–3).
Book-binding technique (BBT)
Several studies have reported the BBT in B-I
reconstruction following TLDG (21,33–36),
whereby the duodenal bulb was transected from the greater curvature
side to the lesser curvature side. Similar to the INTACT, but
without dissection of the supraduodenal vessels branching off from
the GDA before the gastroduodenostomy, linear stapling of the
posterior walls of the duodenum and the remnant stomach was
performed so that the anastomotic staple line was parallel to the
transecting staple line in the duodenum and the end of the
transecting staple line in the remnant stomach (21,33–36).
The ischemic areas between these staple lines were removed using an
energy device, and thereafter, the relatively large hole made in
the anterior side was closed by two linear staples (21,33) or
hand suturing (34–36). As a result, a physiological
triangular end-to-end anastomosis with no need for twisting was
completed (21,33–36).
In the BBT, the operator can remove the ischemic
duodenal posterior wall between the transecting staple line and
anastomotic staple line using the energy device (21,33–36).
However, because it has been reported that the area of the
triangular end-to-end colocolostomy is considered to be prescribed
by the colon diameter (32), there
is a concern that, in the BBT, an adequate anastomotic area might
not be obtained if the duodenal bulb diameter is relatively short
(1–3).
Augmented rectangle technique
(ART)
Fukunaga et al (37) first reported the ART in B-I
reconstruction following TLDG in 2018. As in some of the other
techniques, the duodenal bulb was transected from the greater
curvature side to the lesser curvature side. Before the
gastroduodenostomy, dissection of several supraduodenal vessels
along the lesser curvature side of the duodenum was performed
aiming to create the space required for insertion of the ELS fork.
After the lesser curvature side of the duodenum was retracted
externally, the posterior walls of the first part of the duodenum
and the remnant stomach were anastomosed using one 60-mm ELS so
that the staple length was 60 mm and the anastomotic staple line
was parallel to the end of the transecting staple line in the
remnant stomach. After closure of the ELS entry hole using one
30-mm ELS, the areas between the transecting staple lines and
anastomotic staple line were removed using one 60-mm ELS. As a
result, a physiological rectangular end-to-end anastomosis with the
absence of twisting was completed.
In the ART, the range of duodenal wall ischemia is
considered to be clearly identifiable during the anastomosis
because the blood supply of the duodenal posterior wall between the
transecting staple line and anastomotic staple via the
supraduodenal vessels branching from the GDA is blocked by the
anastomotic linear-staple due to the duodenal bulb being transected
from the greater curvature side to the lesser curvature side and
the anastomotic staple line being positioned in the duodenal
posterior wall (37). Furthermore,
in this procedure, it is presumed that an adequate anastomotic area
is likely to be steadily obtained since the 60-mm staple length is
consistently retained (37).
Conclusion
The present review discusses several intracorporeal
linear-stapled gastroduodenostomy procedures in which not only
transection of the duodenal bulb but also gastroduodenostomy is
performed with an ELS, classifying them into two groups on the
basis of the intraoperative management of the duodenal wall between
the transecting staple line and anastomotic staple line. When this
site is preserved, the blood supply of the duodenal wall needs to
be retained with certainty. On the other hand, when this site is
removed, the ischemic portion of the duodenal wall needs to be
identified and removed. Furthermore, in both groups, an adequate
anastomotic area needs to be secured. In conclusion, surgeons need
to be familiar with the anatomical features of the duodenal bulb,
including its blood perfusion and shape, when carrying out this
characteristic type of gastroduodenostomy.
Acknowledgements
The authors would like to acknowledge Mr. Shigeyuki
Sakaguchi (Clark Kent Co., Ltd., Uda, Nara, Japan) for generating
Fig. 1, Fig. 2, Fig.
3, Fig. 4, Fig. 5 and providing them with kind
permission to reproduce these images.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
TT, EN and MH contributed to conception and design
of the present review. TT and EN performed the literature review
and drafted the initial manuscript. EN and MH revised the
manuscript. Data authentication is not applicable. All authors have
read and approved the final manuscript.
Ethics approval and consent to
participate
The present review was approved by the Institutional
Review Board of Otori Stomach and Intestines Hospital (Sakai,
Japan) and the Institutional Review Board of Hokusetsu-Miki
Hospital (Suita, Japan) (both approval no. 23000001). No specific
patients are mentioned in the present review.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
ART
|
augmented rectangle technique
|
|
BBT
|
book-binding technique
|
|
B-I
|
Billroth I
|
|
DSG
|
delta-shaped gastroduodenostomy
|
|
ELS
|
endoscopic linear stapler
|
|
GDA
|
gastroduodenal artery
|
|
INTACT
|
intracorporeal triangular anastomotic
technique
|
|
mDSG
|
modified DSG
|
|
OG
|
overlap gastroduodenostomy
|
|
TLDG
|
totally laparoscopic distal
gastrectomy
|
References
|
1
|
Jayaraman MV, Mayo-Smith WW, Movson JS,
Dupuy DE and Wallach MT: CT of the duodenum: An overlooked segment
gets its due. Radiographics. 21:S147–S160. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Reghunath A, Kabilan K and Mittal MK:
Exploring the neglected segment of the intestine: The duodenum and
its pathologies. Pol J Radiol. 85:e230–e244. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Terra C, Ramos-Andrade D, Sá-Marques I,
Brito J, Caseiro-Alves F and Curvo-Semedo L: Duodenal imaging on
the spotlight: From A to Z. Insights Imaging. 12:942021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hentati N, Fournier HD, Papon X, Aube C,
Vialle R and Mercier P: Arterial supply of the duodenal bulb: An
anatomoclinical study. Surg Radiol Anat. 21:159–164. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
von Trotha KT, Butz N, Grommes J,
Binnebösel M, Charalambakis N, Mühlenbruch G, Schumpelick V, Klinge
U, Neumann UP, Prescher A and Krones CJ: Vascular anatomy of the
small intestine-a comparative anatomic study on humans and pigs.
Int J Colorectal Dis. 30:683–690. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kanaya S, Gomi T, Momoi H, Tamaki N, Isobe
H, Katayama T, Wada Y and Ohtoshi M: Delta-shaped anastomosis in
totally laparoscopic Billroth I gastrectomy: New technique of
intraabdominal gastroduodenostomy. J Am Coll Surg. 195:284–287.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kanaya S, Kawamura Y, Kawada H, Iwasaki H,
Gomi T, Satoh S and Uyama I: The delta-shaped anastomosis in
laparoscopic distal gastrectomy: Analysis of the initial 100
consecutive procedures of intracorporeal gastroduodenostomy.
Gastric Cancer. 14:365–371. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kim JJ, Song KY, Chin HM, Kim W, Jeon HM,
Park CH and Park SM: Totally laparoscopic gastrectomy with various
types of intracorporeal anastomosis using laparoscopic linear
staplers: Preliminary experience. Surg Endosc. 22:436–442. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Song KY, Park CH, Kang HC, Kim JJ, Park
SM, Jun KH, Chin HM and Hur H: Is totally laparoscopic gastrectomy
less invasive than laparoscopy-assisted gastrectomy?: Prospective,
multicenter study. J Gastrointest Surg. 12:1015–1021. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ikeda O, Sakaguchi Y, Aoki Y, Harimoto N,
Taomoto J, Masuda T, Ohga T, Adachi E, Toh Y, Okamura T and Baba
Hz: Advantages of totally laparoscopic distal gastrectomy over
laparoscopically assisted distal gastrectomy for gastric cancer.
Surg Endosc. 23:2374–2379. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kim MG, Kawada H and Kim BS, Kim TH, Kim
KC, Yook JH and Kim BS: A totally laparoscopic distal gastrectomy
with gastroduodenostomy (TLDG) for improvement of the early
surgical outcomes in high BMI patients. Surg Endosc. 25:1076–1082.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kinoshita T, Shibasaki H, Oshiro T,
Ooshiro M, Okazumi S and Katoh R: Comparison of
laparoscopy-assisted and total laparoscopic Billroth-I gastrectomy
for gastric cancer: A report of short-term outcomes. Surg Endosc.
25:1395–1401. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Noshiro H, Iwasaki H, Miyasaka Y,
Kobayashi K, Masatsugu T, Akashi M and Ikeda O: An additional
suture secures against pitfalls in delta-shaped gastroduodenostomy
after laparoscopic distal gastrectomy. Gastric Cancer. 14:385–389.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kim MG, Kim KC and Kim BS, Kim TH, Kim HS,
Yook JH and Kim BS: A totally laparoscopic distal gastrectomy can
be an effective way of performing laparoscopic gastrectomy in obese
patients (body mass index≥30). World J Surg. 35:1327–1332. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kim DG, Choi YY, An JY, Kwon IG, Cho I,
Kim YM, Bae JM, Song MG and Noh SH: Comparing the short-term
outcomes of totally intracorporeal gastroduodenostomy with
extracorporeal gastroduodenostomy after laparoscopic distal
gastrectomy for gastric cancer: A single surgeon's experience and a
rapid systematic review with meta-analysis. Surg Endosc.
27:3153–3161. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Okabe H, Obama K, Tsunoda S, Tanaka E and
Sakai Y: Advantage of completely laparoscopic gastrectomy with
linear stapled reconstruction: A long-term follow-up study. Ann
Surg. 259:109–116. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kitagami H, Morimoto M, Nozawa M, Nakamura
K, Tanimura S, Murakawa K, Murakami Y, Kikuchi K, Ushigome H, Sato
L, et al: Evaluation of the delta-shaped anastomosis in
laparoscopic distal gastrectomy: Midterm results of a comparison
with Roux-en-Y anastomosis. Surg Endosc. 28:2137–2144. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lee HH, Song KY, Lee JS, Park SM and Kim
JJ: Delta-shaped anastomosis, a good substitute for conventional
Billroth I technique with comparable long-term functional outcome
in totally laparoscopic distal gastrectomy. Surg Endosc.
29:2545–2552. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jeong O, Jung MR, Park YK and Ryu SY:
Safety and feasibility during the initial learning process of
intracorporeal Billroth I (delta-shaped) anastomosis for
laparoscopic distal gastrectomy. Surg Endosc. 29:1522–1529. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Man-I M, Suda K, Kikuchi K, Tanaka T,
Furuta S, Nakauchi M, Ishikawa K, Ishida Y and Uyama I: Totally
intracorporeal delta-shaped B-I anastomosis following laparoscopic
distal gastrectomy using the Tri-Staple™ reloads on the manual
Ultra handle: A prospective cohort study with historical controls.
Surg Endosc. 29:3304–3312. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ikeda T, Kawano H, Hisamatsu Y, Ando K,
Saeki H, Oki E, Ohga T, Kakeji Y, Tsujitani S, Kohnoe S and Maehara
Y: Progression from laparoscopic-assisted to totally laparoscopic
distal gastrectomy: Comparison of circular stapler (i-DST) and
linear stapler (BBT) for intracorporeal anastomosis. Surg Endosc.
27:325–332. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Omori T, Masuzawa T, Akamatsu H and
Nishida T: A simple and safe method for Billroth I reconstruction
in single-incision laparoscopic gastrectomy using a novel
intracorporeal triangular anastomotic technique. J Gastrointest
Surg. 18:613–616. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yanagimoto Y, Omori T, Fujiwara Y, Demura
K, Jeong-Ho M, Shinno N, Yamamoto K, Sugimura K, Miyata H, Ushigome
H, et al: Comparison of the intracorporeal triangular and
delta-shaped anastomotic techniques in totally laparoscopic distal
gastrectomy for gastric cancer: An analysis with propensity score
matching. Surg Endosc. 34:2445–2453. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Iwasaki K, Cho H, Ogawa R, Ishida H, Oguri
Y, Maezawa Y, Tsuchida K, Nagakawa Y, Katsumata K and Tsuchida A:
Comparison of intracorporeal trapezoidal-shaped gastroduodenostomy
and delta-shaped anastomosis after laparoscopic distal gastrectomy
for gastric cancer: A single-center retrospective study. Surg
Laparosc Endosc Percutan Tech. 32:292–298. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Chen G, Li W, Yu W, Cen D, Wang X, Luo P,
Yan J, Chen G, Zhu Y and Zhu L: Application of overlap
gastroduodenostomy in Billroth i anastomosis after totally
laparoscopic distal gastrectomy for gastric cancer. Can J
Gastroenterol Hepatol. 2022:90949342022. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Tokuhara T, Nakata E, Tenjo T, Kawai I,
Kondo K and Hatabe S: Modified delta-shaped gastroduodenostomy
consisting of linear stapling and single-layer suturing with the
operator positioned between the patient's legs: A technique
preventing intraoperative duodenal injury and postoperative
anastomotic stenosis. PLoS One. 15:e02301132020. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Song HM, Lee SL, Hur H, Cho YK and Han SU:
Linear-shaped gastroduodenostomy in totally laparoscopic distal
gastrectomy. J Gastric Cancer. 10:69–74. 2010. View Article : Google Scholar
|
|
28
|
Jang CE and Lee S: Modified intracorporeal
gastroduodenostomy in totally laparoscopic distal gastrectomy for
gastric cancer: Early experience. Ann Surg Treat Res. 89:306–312.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Byun C, Cui LH, Son SY, Hur H, Cho YK and
Han SU: Linear-shaped gastroduodenostomy (LSGD): Safe and feasible
technique of intracorporeal Billroth I anastomosis. Surg Endosc.
30:4505–4514. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Watanabe Y, Watanabe M, Suehara N, Saimura
M, Mizuuchi Y, Nishihara K, Iwashita T and Nakano T: Billroth-I
reconstruction using an overlap method in totally laparoscopic
distal gastrectomy: Propensity score matched cohort study of short-
and long-term outcomes compared with Roux-en-Y reconstruction. Surg
Endosc. 33:3990–4002. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Wang B, Son SY, Shin HJ, Hur H and Han SU:
The learning curve of linear-shaped gastroduodenostomy associated
with totally laparoscopic distal gastrectomy. J Gastrointest Surg.
24:1770–1777. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kosuge M, Eto K, Hashizume R, Takeda M,
Tomori K, Neki K, Mitsumori N and Yanaga K: Which is the safer
anastomotic method for colon surgery? -Ten-year results. In Vivo.
31:683–687. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Oki E, Tsuda Y, Saeki H, Ando K, Imamura
Y, Nakashima Y, Ohgaki K, Morita M, Ikeda T and Maehara Y:
Book-binding technique for Billroth I anastomosis during totally
laparoscopic distal gastrectomy. J Am Coll Surg. 219:e69–e73. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kim JS, Park EY, Park DJ and Kim GY:
Modified book binding technique (MBBT) for intracorporeal
gastroduodenostomy in totally laparoscopic distal gastrectomy:
Initial experience. J Gastric Cancer. 19:355–364. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kikuchi S, Kuroda S, Nishizaki M, Kuwada
K, Takata N, Kakiuchi Y, Yano S, Noma K, Kagawa S and Fujiwara T:
Intracorporeal semi-hand-sewn Billroth I reconstruction in total
laparoscopic distal gastrectomy. Asian J Endosc Surg. 14:640–643.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Waki Y, Masayoshi O, Sato K and Yagi S:
Modification of book-binding technique during totally laparoscopic
distal gastrectomy with Billroth I reconstruction. J Minim Access
Surg. 18:625–628. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Fukunaga T, Ishibashi Y, Oka S, Kanda S,
Yube Y, Kohira Y, Matsuo Y, Mori O, Mikami S, Enomoto T and Otsubo
T: Augmented rectangle technique for Billroth I anastomosis in
totally laparoscopic distal gastrectomy for gastric cancer. Surg
Endosc. 32:4011–4016. 2018. View Article : Google Scholar : PubMed/NCBI
|