|
1
|
Jayaraman MV, Mayo-Smith WW, Movson JS,
Dupuy DE and Wallach MT: CT of the duodenum: An overlooked segment
gets its due. Radiographics. 21:S147–S160. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Reghunath A, Kabilan K and Mittal MK:
Exploring the neglected segment of the intestine: The duodenum and
its pathologies. Pol J Radiol. 85:e230–e244. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Terra C, Ramos-Andrade D, Sá-Marques I,
Brito J, Caseiro-Alves F and Curvo-Semedo L: Duodenal imaging on
the spotlight: From A to Z. Insights Imaging. 12:942021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hentati N, Fournier HD, Papon X, Aube C,
Vialle R and Mercier P: Arterial supply of the duodenal bulb: An
anatomoclinical study. Surg Radiol Anat. 21:159–164. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
von Trotha KT, Butz N, Grommes J,
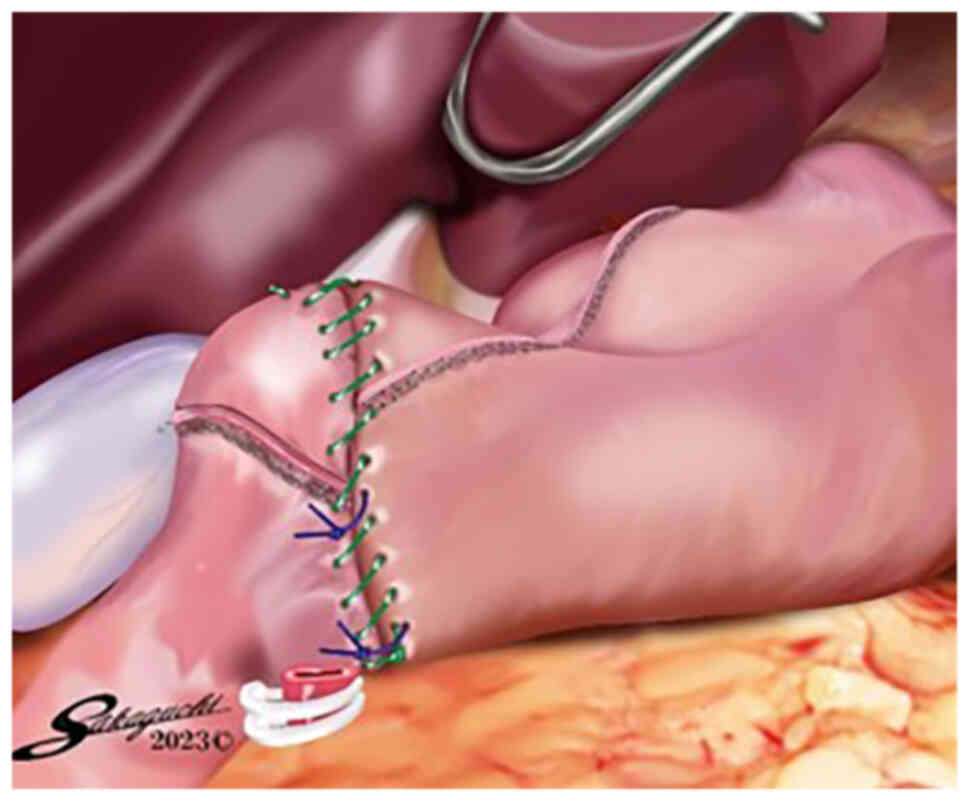
Binnebösel M, Charalambakis N, Mühlenbruch G, Schumpelick V, Klinge
U, Neumann UP, Prescher A and Krones CJ: Vascular anatomy of the
small intestine-a comparative anatomic study on humans and pigs.
Int J Colorectal Dis. 30:683–690. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kanaya S, Gomi T, Momoi H, Tamaki N, Isobe
H, Katayama T, Wada Y and Ohtoshi M: Delta-shaped anastomosis in
totally laparoscopic Billroth I gastrectomy: New technique of
intraabdominal gastroduodenostomy. J Am Coll Surg. 195:284–287.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kanaya S, Kawamura Y, Kawada H, Iwasaki H,
Gomi T, Satoh S and Uyama I: The delta-shaped anastomosis in
laparoscopic distal gastrectomy: Analysis of the initial 100
consecutive procedures of intracorporeal gastroduodenostomy.
Gastric Cancer. 14:365–371. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kim JJ, Song KY, Chin HM, Kim W, Jeon HM,
Park CH and Park SM: Totally laparoscopic gastrectomy with various
types of intracorporeal anastomosis using laparoscopic linear
staplers: Preliminary experience. Surg Endosc. 22:436–442. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Song KY, Park CH, Kang HC, Kim JJ, Park
SM, Jun KH, Chin HM and Hur H: Is totally laparoscopic gastrectomy
less invasive than laparoscopy-assisted gastrectomy?: Prospective,
multicenter study. J Gastrointest Surg. 12:1015–1021. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ikeda O, Sakaguchi Y, Aoki Y, Harimoto N,
Taomoto J, Masuda T, Ohga T, Adachi E, Toh Y, Okamura T and Baba
Hz: Advantages of totally laparoscopic distal gastrectomy over
laparoscopically assisted distal gastrectomy for gastric cancer.
Surg Endosc. 23:2374–2379. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kim MG, Kawada H and Kim BS, Kim TH, Kim
KC, Yook JH and Kim BS: A totally laparoscopic distal gastrectomy
with gastroduodenostomy (TLDG) for improvement of the early
surgical outcomes in high BMI patients. Surg Endosc. 25:1076–1082.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kinoshita T, Shibasaki H, Oshiro T,
Ooshiro M, Okazumi S and Katoh R: Comparison of
laparoscopy-assisted and total laparoscopic Billroth-I gastrectomy
for gastric cancer: A report of short-term outcomes. Surg Endosc.
25:1395–1401. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Noshiro H, Iwasaki H, Miyasaka Y,
Kobayashi K, Masatsugu T, Akashi M and Ikeda O: An additional
suture secures against pitfalls in delta-shaped gastroduodenostomy
after laparoscopic distal gastrectomy. Gastric Cancer. 14:385–389.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kim MG, Kim KC and Kim BS, Kim TH, Kim HS,
Yook JH and Kim BS: A totally laparoscopic distal gastrectomy can
be an effective way of performing laparoscopic gastrectomy in obese
patients (body mass index≥30). World J Surg. 35:1327–1332. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kim DG, Choi YY, An JY, Kwon IG, Cho I,
Kim YM, Bae JM, Song MG and Noh SH: Comparing the short-term
outcomes of totally intracorporeal gastroduodenostomy with
extracorporeal gastroduodenostomy after laparoscopic distal
gastrectomy for gastric cancer: A single surgeon's experience and a
rapid systematic review with meta-analysis. Surg Endosc.
27:3153–3161. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Okabe H, Obama K, Tsunoda S, Tanaka E and
Sakai Y: Advantage of completely laparoscopic gastrectomy with
linear stapled reconstruction: A long-term follow-up study. Ann
Surg. 259:109–116. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kitagami H, Morimoto M, Nozawa M, Nakamura
K, Tanimura S, Murakawa K, Murakami Y, Kikuchi K, Ushigome H, Sato
L, et al: Evaluation of the delta-shaped anastomosis in
laparoscopic distal gastrectomy: Midterm results of a comparison
with Roux-en-Y anastomosis. Surg Endosc. 28:2137–2144. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lee HH, Song KY, Lee JS, Park SM and Kim
JJ: Delta-shaped anastomosis, a good substitute for conventional
Billroth I technique with comparable long-term functional outcome
in totally laparoscopic distal gastrectomy. Surg Endosc.
29:2545–2552. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jeong O, Jung MR, Park YK and Ryu SY:
Safety and feasibility during the initial learning process of
intracorporeal Billroth I (delta-shaped) anastomosis for
laparoscopic distal gastrectomy. Surg Endosc. 29:1522–1529. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Man-I M, Suda K, Kikuchi K, Tanaka T,
Furuta S, Nakauchi M, Ishikawa K, Ishida Y and Uyama I: Totally
intracorporeal delta-shaped B-I anastomosis following laparoscopic
distal gastrectomy using the Tri-Staple™ reloads on the manual
Ultra handle: A prospective cohort study with historical controls.
Surg Endosc. 29:3304–3312. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ikeda T, Kawano H, Hisamatsu Y, Ando K,
Saeki H, Oki E, Ohga T, Kakeji Y, Tsujitani S, Kohnoe S and Maehara
Y: Progression from laparoscopic-assisted to totally laparoscopic
distal gastrectomy: Comparison of circular stapler (i-DST) and
linear stapler (BBT) for intracorporeal anastomosis. Surg Endosc.
27:325–332. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Omori T, Masuzawa T, Akamatsu H and
Nishida T: A simple and safe method for Billroth I reconstruction
in single-incision laparoscopic gastrectomy using a novel
intracorporeal triangular anastomotic technique. J Gastrointest
Surg. 18:613–616. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yanagimoto Y, Omori T, Fujiwara Y, Demura
K, Jeong-Ho M, Shinno N, Yamamoto K, Sugimura K, Miyata H, Ushigome
H, et al: Comparison of the intracorporeal triangular and
delta-shaped anastomotic techniques in totally laparoscopic distal
gastrectomy for gastric cancer: An analysis with propensity score
matching. Surg Endosc. 34:2445–2453. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Iwasaki K, Cho H, Ogawa R, Ishida H, Oguri
Y, Maezawa Y, Tsuchida K, Nagakawa Y, Katsumata K and Tsuchida A:
Comparison of intracorporeal trapezoidal-shaped gastroduodenostomy
and delta-shaped anastomosis after laparoscopic distal gastrectomy
for gastric cancer: A single-center retrospective study. Surg
Laparosc Endosc Percutan Tech. 32:292–298. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Chen G, Li W, Yu W, Cen D, Wang X, Luo P,
Yan J, Chen G, Zhu Y and Zhu L: Application of overlap
gastroduodenostomy in Billroth i anastomosis after totally
laparoscopic distal gastrectomy for gastric cancer. Can J
Gastroenterol Hepatol. 2022:90949342022. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Tokuhara T, Nakata E, Tenjo T, Kawai I,
Kondo K and Hatabe S: Modified delta-shaped gastroduodenostomy
consisting of linear stapling and single-layer suturing with the
operator positioned between the patient's legs: A technique
preventing intraoperative duodenal injury and postoperative
anastomotic stenosis. PLoS One. 15:e02301132020. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Song HM, Lee SL, Hur H, Cho YK and Han SU:
Linear-shaped gastroduodenostomy in totally laparoscopic distal
gastrectomy. J Gastric Cancer. 10:69–74. 2010. View Article : Google Scholar
|
|
28
|
Jang CE and Lee S: Modified intracorporeal
gastroduodenostomy in totally laparoscopic distal gastrectomy for
gastric cancer: Early experience. Ann Surg Treat Res. 89:306–312.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Byun C, Cui LH, Son SY, Hur H, Cho YK and
Han SU: Linear-shaped gastroduodenostomy (LSGD): Safe and feasible
technique of intracorporeal Billroth I anastomosis. Surg Endosc.
30:4505–4514. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Watanabe Y, Watanabe M, Suehara N, Saimura
M, Mizuuchi Y, Nishihara K, Iwashita T and Nakano T: Billroth-I
reconstruction using an overlap method in totally laparoscopic
distal gastrectomy: Propensity score matched cohort study of short-
and long-term outcomes compared with Roux-en-Y reconstruction. Surg
Endosc. 33:3990–4002. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Wang B, Son SY, Shin HJ, Hur H and Han SU:
The learning curve of linear-shaped gastroduodenostomy associated
with totally laparoscopic distal gastrectomy. J Gastrointest Surg.
24:1770–1777. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kosuge M, Eto K, Hashizume R, Takeda M,
Tomori K, Neki K, Mitsumori N and Yanaga K: Which is the safer
anastomotic method for colon surgery? -Ten-year results. In Vivo.
31:683–687. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Oki E, Tsuda Y, Saeki H, Ando K, Imamura
Y, Nakashima Y, Ohgaki K, Morita M, Ikeda T and Maehara Y:
Book-binding technique for Billroth I anastomosis during totally
laparoscopic distal gastrectomy. J Am Coll Surg. 219:e69–e73. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kim JS, Park EY, Park DJ and Kim GY:
Modified book binding technique (MBBT) for intracorporeal
gastroduodenostomy in totally laparoscopic distal gastrectomy:
Initial experience. J Gastric Cancer. 19:355–364. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kikuchi S, Kuroda S, Nishizaki M, Kuwada
K, Takata N, Kakiuchi Y, Yano S, Noma K, Kagawa S and Fujiwara T:
Intracorporeal semi-hand-sewn Billroth I reconstruction in total
laparoscopic distal gastrectomy. Asian J Endosc Surg. 14:640–643.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Waki Y, Masayoshi O, Sato K and Yagi S:
Modification of book-binding technique during totally laparoscopic
distal gastrectomy with Billroth I reconstruction. J Minim Access
Surg. 18:625–628. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Fukunaga T, Ishibashi Y, Oka S, Kanda S,
Yube Y, Kohira Y, Matsuo Y, Mori O, Mikami S, Enomoto T and Otsubo
T: Augmented rectangle technique for Billroth I anastomosis in
totally laparoscopic distal gastrectomy for gastric cancer. Surg
Endosc. 32:4011–4016. 2018. View Article : Google Scholar : PubMed/NCBI
|