|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global Cancer Statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249. 2021.
|
|
2
|
Siegel RL, Torre LA, Soerjomataram I,
Hayes RB, Bray F, Weber TK and Jemal A: Global patterns and trends
in colorectal cancer incidence in young adults. Gut. 68:2179–2185.
2019.
|
|
3
|
Kim MJ, Jeong SY, Choi SJ, Ryoo SB, Park
JW, Park KJ, Oh JH, Kang SB, Park HC, Heo SC and Park JG: Survival
paradox between stage IIB/C (T4N0) and stage IIIA (T1-2N1) colon
cancer. Ann Surg Oncol. 22:505–512. 2015.
|
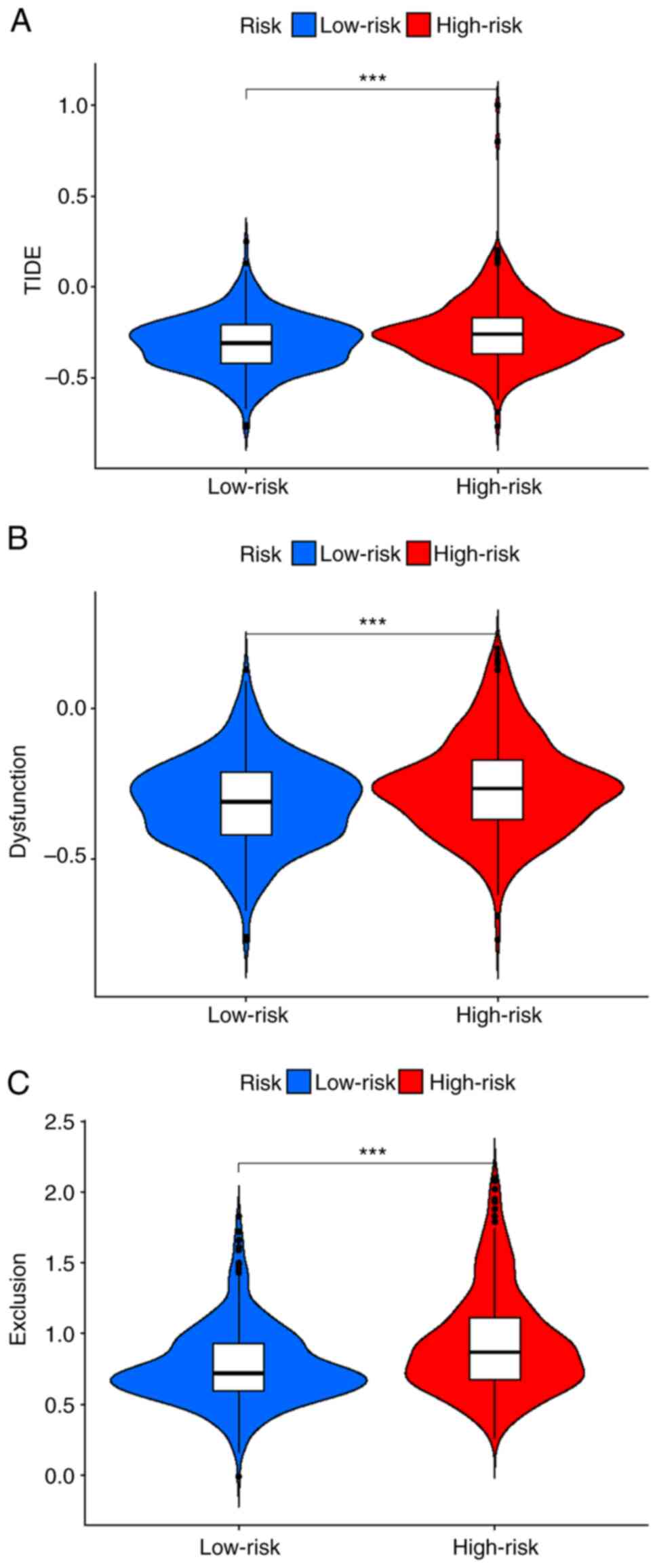
|
4
|
Almatroudi A: The incidence rate of
colorectal cancer in Saudi Arabia: An observational descriptive
epidemiological analysis. Int J Gen Med. 13:977–990. 2020.
|
|
5
|
Gan GL, Liu J, Chen WJ, Ye QQ, Xu Y, Wu HT
and Li W: The diverse roles of the mucin gene cluster located on
chromosome 11p15.5 in colorectal cancer. Front Cell Dev Biol.
8:5142020.
|
|
6
|
Sasidharan Nair V, Saleh R, Taha RZ, Toor
SM, Murshed K, Ahmed AA, Kurer MA, Abu Nada M, Al Ejeh F and Elkord
E: Differential gene expression of tumor-infiltrating CD4+ T cells
in advanced versus early stage colorectal cancer and identification
of a gene signature of poor prognosis. Oncoimmunology.
9:18251782020.
|
|
7
|
Ihnát P, Vávra P and Zonča P: Treatment
strategies for colorectal carcinoma with synchronous liver
metastases: Which way to go. World J Gastroenterol. 21:7014–7021.
2015.
|
|
8
|
Mármol I, Sánchez-de-Diego C, Pradilla
Dieste A, Cerrada E and Rodriguez Yoldi MJ: Colorectal carcinoma: A
general overview and future perspectives in colorectal cancer. Int
J Mol Sci. 18:1972017.
|
|
9
|
Ciardiello D, Vitiello PP, Cardone C,
Martini G, Troiani T, Martinelli E and Ciardiello F: Immunotherapy
of colorectal cancer: Challenges for therapeutic efficacy. Cancer
Treat Rev. 76:22–32. 2019.
|
|
10
|
Cunningham D, Atkin W, Lenz HJ, Lynch HT,
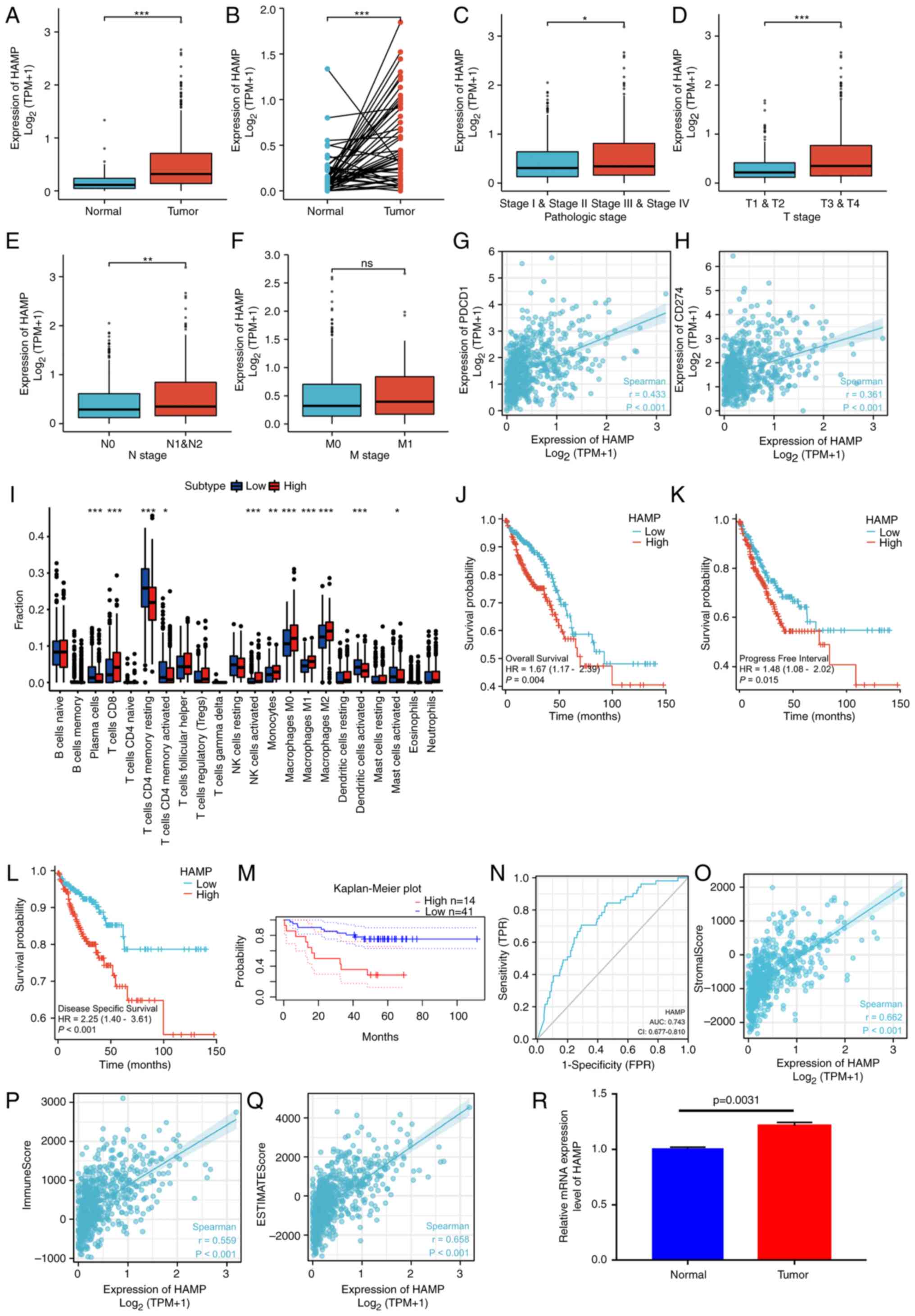
Minsky B, Nordlinger B and Starling N: Colorectal cancer. Lancet.
375:1030–1047. 2010.
|
|
11
|
de Weger VA, Turksma AW, Voorham QJ, Euler
Z, Bril H, van den Eertwegh AJ, Bloemena E, Pinedo HM, Vermorken
JB, van Tinteren H, et al: Clinical effects of adjuvant active
specific immunotherapy differ between patients with
microsatellite-stable and microsatellite-instable colon cancer.
Clin Cancer Res. 18:882–889. 2012.
|
|
12
|
Le DT, Uram JN, Wang H, Bartlett BR,
Kemberling H, Eyring AD, Skora AD, Luber BS, Azad NS, Laheru D, et
al: PD-1 blockade in tumors with mismatch-repair deficiency. N Engl
J Med. 372:2509–2520. 2015.
|
|
13
|
Benson AB, Venook AP, Al-Hawary MM, Azad
N, Chen YJ, Ciombor KK, Cohen S, Cooper HS, Deming D,
Garrido-Laguna I, et al: Rectal cancer, version 2.2022, NCCN
clinical practice guidelines in oncology. J Natl Compr Canc Netw.
20:1139–1167. 2022.
|
|
14
|
Koncina E, Haan S, Rauh S and Letellier E:
Prognostic and predictive molecular biomarkers for colorectal
cancer: Updates and challenges. Cancers (Basel). 12:3192020.
|
|
15
|
Vacante M, Borzì AM, Basile F and Biondi
A: Biomarkers in colorectal cancer: Current clinical utility and
future perspectives. World J Clin Cases. 6:869–881. 2018.
|
|
16
|
Amado RG, Wolf M, Peeters M, Van Cutsem E,
Siena S, Freeman DJ, Juan T, Sikorski R, Suggs S, Radinsky R, et
al: Wild-type KRAS is required for panitumumab efficacy in patients
with metastatic colorectal cancer. J Clin Oncol. 26:1626–1634.
2008.
|
|
17
|
Bokemeyer C, Bondarenko I, Makhson A,
Hartmann JT, Aparicio J, de Braud F, Donea S, Ludwig H, Schuch G,
Stroh C, et al: Fluorouracil, leucovorin, and oxaliplatin with and
without cetuximab in the first-line treatment of metastatic
colorectal cancer. J Clin Oncol. 27:663–671. 2009.
|
|
18
|
Douillard J, Oliner KS, Siena S, Tabernero
J, Burkes R, Barugel M, Humblet Y, Bodoky G, Cunningham D, Jassem
J, et al: Panitumumab-FOLFOX4 treatment and RAS mutations in
colorectal cancer. N Engl J Med. 369:1023–1034. 2013.
|
|
19
|
Karapetis CS, Khambata-Ford S, Jonker DJ,
O'Callaghan CJ, Tu D, Tebbutt NC, Simes RJ, Chalchal H, Shapiro JD,
Robitaille S, et al: K-ras mutations and benefit from cetuximab in
advanced colorectal cancer. N Engl J Med. 359:1757–1765. 2008.
|
|
20
|
Sorich MJ, Wiese MD, Rowland A,
Kichenadasse G, McKinnon RA and Karapetis CS: Extended RAS
mutations and anti-EGFR monoclonal antibody survival benefit in
metastatic colorectal cancer: A meta-analysis of randomized,
controlled trials. Ann Oncol. 26:13–21. 2015.
|
|
21
|
Van Cutsem E, Köhne CH, Láng I, Folprecht
G, Nowacki MP, Cascinu S, Shchepotin I, Maurel J, Cunningham D,
Tejpar S, et al: Cetuximab plus irinotecan, fluorouracil, and
leucovorin as first-line treatment for metastatic colorectal
cancer: Updated analysis of overall survival according to tumor
KRAS and BRAF mutation status. J Clin Oncol. 29:2011–2019.
2011.
|
|
22
|
Maughan TS, Adams RA, Smith CG, Meade AM,
Seymour MT, Wilson RH, Idziaszczyk S, Harris R, Fisher D, Kenny SL,
et al: Addition of cetuximab to oxaliplatin-based first-line
combination chemotherapy for treatment of advanced colorectal
cancer: Results of the randomised phase 3 MRC COIN trial. Lancet.
377:2103–2114. 2011.
|
|
23
|
Le DT, Kim TW, Van Cutsem E, Geva R, Jäger
D, Hara H, Burge M, O'Neil B, Kavan P, Yoshino T, et al: Phase II
open-label study of pembrolizumab in treatment-refractory,
microsatellite instability-high/mismatch repair-deficient
metastatic colorectal cancer: KEYNOTE-164. J Clin Oncol. 38:11–19.
2020.
|
|
24
|
Fu J, Li K, Zhang W, Wan C, Zhang J, Jiang
P and Liu XS: Large-scale public data reuse to model immunotherapy
response and resistance. Genome Med. 12:212020.
|
|
25
|
Jiang P, Gu S, Pan D, Fu J, Sahu A, Hu X,
Li Z, Traugh N, Bu X, Li B, et al: Signatures of T cell dysfunction
and exclusion predict cancer immunotherapy response. Nat Med.
24:1550–1558. 2018.
|
|
26
|
Love MI, Huber W and Anders S: Moderated
estimation of fold change and dispersion for RNA-seq data with
DESeq2. Genome Biol. 15:5502014.
|
|
27
|
Wang X, Duanmu J, Fu X, Li T and Jiang Q:
Analyzing and validating the prognostic value and mechanism of
colon cancer immune microenvironment. J Transl Med. 18:3242020.
|
|
28
|
Li L, Zhang W, Qiu J, Zhang W, Lu M, Wang
J, Jin Y and Xi Q: Stem cell-associated signatures help to predict
diagnosis and prognosis in ovarian serous cystadenocarcinoma. Stem
Cells Int. 2023:45005612023.
|
|
29
|
Hänzelmann S, Castelo R and Guinney J:
GSVA: Gene set variation analysis for microarray and RNA-Seq data.
BMC Bioinformatics. 14:72013.
|
|
30
|
Ritchie ME, Phipson B, Wu D, Hu Y, Law CW,
Shi W and Smyth GK: Limma powers differential expression analyses
for RNA-sequencing and microarray studies. Nucleic Acids Res.
43:e472015.
|
|
31
|
Finotello F, Mayer C, Plattner C,
Laschober G, Rieder D, Hackl H, Krogsdam A, Loncova Z, Posch W,
Wilflingseder D, et al: Molecular and pharmacological modulators of
the tumor immune contexture revealed by deconvolution of RNA-seq
data. Genome Med. 11:342019.
|
|
32
|
Yoshihara K, Shahmoradgoli M, Martínez E,
Vegesna R, Kim H, Torres-Garcia W, Treviño V, Shen H, Laird PW,
Levine DA, et al: Inferring tumour purity and stromal and immune
cell admixture from expression data. Nat Commun. 4:26122013.
|
|
33
|
Newman AM, Liu CL, Green MR, Gentles AJ,
Feng W, Xu Y, Hoang CD, Diehn M and Alizadeh AA: Robust enumeration
of cell subsets from tissue expression profiles. Nat Methods.
12:453–457. 2015.
|
|
34
|
Wu T, Hu E, Xu S, Chen M, Guo P, Dai Z,
Feng T, Zhou L, Tang W, Zhan L, et al: clusterProfiler 4.0: A
universal enrichment tool for interpreting omics data. Innovation
(Camb). 2:1001412021.
|
|
35
|
Yu G, Wang LG, Han Y and He QY:
clusterProfiler: An R package for comparing biological themes among
gene clusters. OMICS. 16:284–287. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Subramanian A, Tamayo P, Mootha VK,
Mukherjee S, Ebert BL, Gillette MA, Paulovich A, Pomeroy SL, Golub
TR, Lander ES and Mesirov JP: Gene set enrichment analysis: A
knowledge-based approach for interpreting genome-wide expression
profiles. Proc Natl Acad Sci USA. 102:15545–15550. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Chin CH, Chen SH, Wu HH, Ho CW, Ko MT and
Lin CY: cytoHubba: Identifying hub objects and sub-networks from
complex interactome. BMC Syst Biol. 8 (Suppl 4):S112014. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) Method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Liu J, Lichtenberg T, Hoadley KA, Poisson
LM, Lazar AJ, Cherniack AD, Kovatich AJ, Benz CC, Levine DA, Lee
AV, et al: An integrated TCGA pan-cancer clinical data resource to
drive high-quality survival outcome analytics. Cell.
173:400–416.e11. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Tang YL, Li DD, Duan JY, Sheng LM and Wang
X: Resistance to targeted therapy in metastatic colorectal cancer:
Current status and new developments. World J Gastroenterol.
29:926–948. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Seliger B: Basis of PD1/PD-L1 Therapies. J
Clin Med. 8:21682019. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Pitt JM, Vétizou M, Daillère R, Roberti
MP, Yamazaki T, Routy B, Lepage P, Boneca IG, Chamaillard M,
Kroemer G and Zitvogel L: Resistance mechanisms to
immune-checkpoint blockade in cancer: Tumor-intrinsic and
-extrinsic factors. Immunity. 44:1255–1269. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Sun C, Mezzadra R and Schumacher TN:
Regulation and function of the PD-L1 checkpoint. Immunity.
48:434–452. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Chen DS and Mellman I: Elements of cancer
immunity and the cancer-immune set point. Nature. 541:321–330.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Horn L, Spigel DR, Vokes EE, Holgado E,
Ready N, Steins M, Poddubskaya E, Borghaei H, Felip E, Paz-Ares L,
et al: Nivolumab versus docetaxel in previously treated patients
with advanced non-small-cell lung cancer: Two-Year outcomes from
two randomized, open-label, phase III trials (CheckMate 017 and
CheckMate 057). J Clin Oncol. 35:3924–3933. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Topalian SL, Sznol M, McDermott DF, Kluger
HM, Carvajal RD, Sharfman WH, Brahmer JR, Lawrence DP, Atkins MB,
Powderly JD, et al: Survival, durable tumor remission, and
long-term safety in patients with advanced melanoma receiving
nivolumab. J Clin Oncol. 32:1020–1030. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Reck M, Rodríguez-Abreu D, Robinson AG,
Hui R, Csőszi T, Fülöp A, Gottfried M, Peled N, Tafreshi A, Cuffe
S, et al: Pembrolizumab versus chemotherapy for PD-L1-Positive
non-small-cell lung cancer. N Engl J Med. 375:1823–1833. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Ferris RL, Blumenschein G Jr, Fayette J,
Guigay J, Colevas AD, Licitra L, Harrington K, Kasper S, Vokes EE,
Even C, et al: Nivolumab for recurrent squamous-cell carcinoma of
the head and neck. N Engl J Med. 375:1856–1867. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Danaher P, Warren S, Lu R, Samayoa J,
Sullivan A, Pekker I, Wallden B, Marincola FM and Cesano A:
Pan-cancer adaptive immune resistance as defined by the Tumor
Inflammation Signature (TIS): Results from The Cancer Genome Atlas
(TCGA). J Immunother Cancer. 6:632018. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Koebel CM, Vermi W, Swann JB, Zerafa N,
Rodig SJ, Old LJ, Smyth MJ and Schreiber RD: Adaptive immunity
maintains occult cancer in an equilibrium state. Nature.
450:903–907. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Dunn GP, Bruce AT, Ikeda H, Old LJ and
Schreiber RD: Cancer immunoediting: From immunosurveillance to
tumor escape. Nat Immunol. 3:991–998. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Pagès F, Berger A, Camus M, Sanchez-Cabo
F, Costes A, Molidor R, Mlecnik B, Kirilovsky A, Nilsson M, Damotte
D, et al: Effector memory T cells, early metastasis, and survival
in colorectal cancer. N Engl J Med. 353:2654–2666. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Zhang N and Bevan MJ: CD8(+) T cells: Foot
soldiers of the immune system. Immunity. 35:161–168. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Alspach E, Lussier DM and Schreiber RD:
Interferon γ and its important roles in promoting and inhibiting
spontaneous and therapeutic cancer immunity. Cold Spring Harb
Perspect Biol. 11:a0284802019. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Liu Y, Zhou N, Zhou L, Wang J, Zhou Y,
Zhang T, Fang Y, Deng J, Gao Y, Liang X, et al: IL-2 regulates
tumor-reactive CD8+ T cell exhaustion by activating the aryl
hydrocarbon receptor. Nat Immunol. 22:358–369. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Zhang J, Endres S and Kobold S: Enhancing
tumor T cell infiltration to enable cancer immunotherapy.
Immunotherapy. 11:201–213. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Franklin RA, Liao W, Sarkar A, Kim MV,
Bivona MR, Liu K, Pamer EG and Li MO: The cellular and molecular
origin of tumor-associated macrophages. Science. 344:921–925. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Wu D, Liu X, Mu J, Yang J, Wu F and Zhou
H: Therapeutic approaches targeting proteins in tumor-associated
macrophages and their applications in cancers. Biomolecules.
12:3922022. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Dahlin AM, Henriksson ML, Van Guelpen B,
Stenling R, Oberg A, Rutegård J and Palmqvist R: Colorectal cancer
prognosis depends on T-cell infiltration and molecular
characteristics of the tumor. Mod Pathol. 24:671–682. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Badoual C, Hans S, Merillon N, Van Ryswick
C, Ravel P, Benhamouda N, Levionnois E, Nizard M, Si-Mohamed A,
Besnier N, et al: PD-1-expressing tumor-infiltrating T cells are a
favorable prognostic biomarker in HPV-associated head and neck
cancer. Cancer Res. 73:128–138. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Vassilakopoulou M, Avgeris M, Velcheti V,
Kotoula V, Rampias T, Chatzopoulos K, Perisanidis C, Kontos CK,
Giotakis AI, Scorilas A, et al: Evaluation of PD-L1 expression and
associated tumor-infiltrating lymphocytes in laryngeal squamous
cell carcinoma. Clin Cancer Res. 22:704–713. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Wang J, Wang S, Song X, Zeng W, Wang S,
Chen F and Ding H: The prognostic value of systemic and local
inflammation in patients with laryngeal squamous cell carcinoma.
Onco Targets Ther. 9:7177–7185. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Forssell J, Oberg A, Henriksson ML,
Stenling R, Jung A and Palmqvist R: High macrophage infiltration
along the tumor front correlates with improved survival in colon
cancer. Clin Cancer Res. 13:1472–1479. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Jung M, Mertens C, Tomat E and Brüne B:
Iron as a central player and promising target in cancer
progression. Int J Mol Sci. 20:2732019. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Torti SV and Torti FM: Iron and cancer:
More ore to be mined. Nat Rev Cancer. 13:342–355. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Wang Y, Yu L, Ding J and Chen Y: Iron
metabolism in cancer. Int J Mol Sci. 20:952018. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Jiang Z, Lim SO, Yan M, Hsu JL, Yao J, Wei
Y, Chang SS, Yamaguchi H, Lee HH, Ke B, et al: TYRO3 induces
anti-PD-1/PD-L1 therapy resistance by limiting innate immunity and
tumoral ferroptosis. J Clin Invest. 131:e1394342021. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Sharma P, Hu-Lieskovan S, Wargo JA and
Ribas A: Primary, adaptive, and acquired resistance to cancer
immunotherapy. Cell. 168:707–723. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Jacolot S, Le Gac G, Scotet V, Quere I,
Mura C and Ferec C: HAMPas a modifier gene that increases the
phenotypic expression of the HFEpC282Y homozygous genotype. Blood.
103:2835–2840. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Casu C, Nemeth E and Rivella S: Hepcidin
agonists as therapeutic tools. Blood. 131:1790–1794. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Armitage AE, Eddowes LA, Gileadi U, Cole
S, Spottiswoode N, Selvakumar TA, Ho LP, Townsend AR and Drakesmith
H: Hepcidin regulation by innate immune and infectious stimuli.
Blood. 118:4129–4139. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Bessman NJ, Mathieu JRR, Renassia C, Zhou
L, Fung TC, Fernandez KC, Austin C, Moeller JB, Zumerle S, Louis S,
et al: Dendritic cell-derived hepcidin sequesters iron from the
microbiota to promote mucosal healing. Science. 368:186–189. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Vyoral D and Petrák J: Hepcidin: A direct
link between iron metabolism and immunity. Int J Biochem Cell Biol.
37:1768–1773. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Mleczko-Sanecka K, Roche F, da Silva AR,
Call D, D'Alessio F, Ragab A, Lapinski PE, Ummanni R, Korf U, Oakes
C, et al: Unbiased RNAi screen for hepcidin regulators links
hepcidin suppression to proliferative Ras/RAF and
nutrient-dependent mTOR signaling. Blood. 123:1574–1585. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Ren F, Yang Y, Wu K, Zhao T, Shi Y, Song M
and Li J: The effects of dandelion polysaccharides on iron
metabolism by regulating hepcidin via JAK/STAT signaling pathway.
Oxid Med Cell Longev. 2021:71847602021. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Saad HKM, Abd Rahman AA, Ab Ghani AS, Taib
WRW, Ismail I, Johan MF, Al-Wajeeh AS and Al-Jamal HAN: Activation
of STAT and SMAD signaling induces hepcidin re-expression as a
therapeutic target for β-Thalassemia patients. Biomedicines.
10:1892022. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Joachim JH and Mehta KJ: Hepcidin in
hepatocellular carcinoma. Br J Cancer. 127:185–192. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Kessler SM, Barghash A, Laggai S, Helms V
and Kiemer AK: Hepatic hepcidin expression is decreased in
cirrhosis and HCC. J Hepatol. 62:977–979. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Maegdefrau U, Arndt S, Kivorski G,
Hellerbrand C and Bosserhoff A: Downregulation of hemojuvelin
prevents inhibitory effects of bone morphogenetic proteins on iron
metabolism in hepatocellular carcinoma. Lab Invest. 91:1615–1623.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Scimeca M and Bonanno E: New highlight in
breast cancer development: The key role of hepcidin and iron
metabolism. Ann Transl Med. 6 (Suppl 1):S562018. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Tesfay L, Clausen KA, Kim JW, Hegde P,
Wang X, Miller LD, Deng Z, Blanchette N, Arvedson T, Miranti CK, et
al: Hepcidin regulation in prostate and its disruption in prostate
cancer. Cancer Res. 75:2254–2263. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Zhao B, Li R, Cheng G, Li Z, Zhang Z, Li
J, Zhang G, Bi C, Hu C, Yang L, et al: Role of hepcidin and iron
metabolism in the onset of prostate cancer. Oncol Lett.
15:9953–9958. 2018.PubMed/NCBI
|
|
83
|
Chen Q, Wang L, Ma Y, Wu X, Jin L and Yu
F: Increased hepcidin expression in non-small cell lung cancer
tissue and serum is associated with clinical stage. Thorac Cancer.
5:14–24. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Phipps O, Brookes MJ and Al-Hassi HO: Iron
deficiency, immunology, and colorectal cancer. Nutr Rev. 79:88–97.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Colorectal cancer cells ectopically
express hepcidin to sequester iron. Cancer Discov. 11:OF22021.
View Article : Google Scholar
|
|
86
|
Schwartz AJ, Goyert JW, Solanki S, Kerk
SA, Chen B, Castillo C, Hsu PP, Do BT, Singhal R, Dame MK, et al:
Hepcidin sequesters iron to sustain nucleotide metabolism and
mitochondrial function in colorectal cancer epithelial cells. Nat
Metab. 3:969–982. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Sornjai W, Nguyen Van Long F, Pion N,
Pasquer A, Saurin JC, Marcel V, Diaz JJ, Mertani HC and Smith DR:
Iron and hepcidin mediate human colorectal cancer cell growth. Chem
Biol Interact. 319:1090212020. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Xiang-Tao P: Expression of hepcidin and
neogenin in colorectal cancer. Open Med (Wars). 12:184–188. 2017.
View Article : Google Scholar : PubMed/NCBI
|