Introduction
Sinus histiocytosis with massive lymphadenopathy
(SHML), also known as Rosai-Dorfman disease (RDD), is a rare and
benign self-limiting histiocytic disease of unknown etiology
(1). Since the first report of RDD
in 1969, >400 cases have been reported worldwide to date
(2). Patients with RDD have
differing disease durations and varying clinical manifestations.
Although extranodal manifestations of RDD are common, intracranial
RDD is rare, with the literature mostly reporting individual cases
(3). In 1983, Isaacson and Wright
were the first to describe extranodal marginal zone lymphoma of
mucosa-associated lymphoid tissue (MALT lymphoma) in the
gastrointestinal tract (4,5). Despite successive reports of MALT
lymphomas developing in other locations, intracranial MALT
lymphomas are rare, all of which are reported as individual cases
(6). RDD coexisting with MALT
lymphoma is even rarer. The present study reports a rare case of
adult intracranial RDD complicated by MALT lymphoma. To the best of
our knowledge, the case reported in the present study is the first
case of adult intracranial RDD complicated by MALT lymphoma in the
literature.
Case report
A 55-year-old female patient was admitted to The
Second Affiliated Hospital of Jiaxing University (Jiaxing, China)
due to headache for half a month and ptosis of the right eyelid for
4 days. The patient was in good health and had no other medical
conditions. On physical examination, the bilateral pupillary light
reflex was sensitive, the right eyelid was ptosed and eyeball
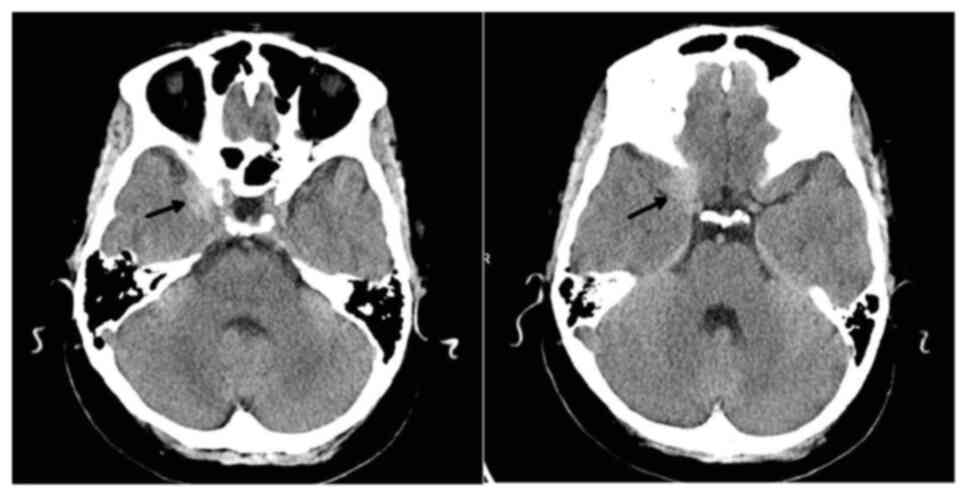
movement was normal. Cranial computed tomography (CT) revealed
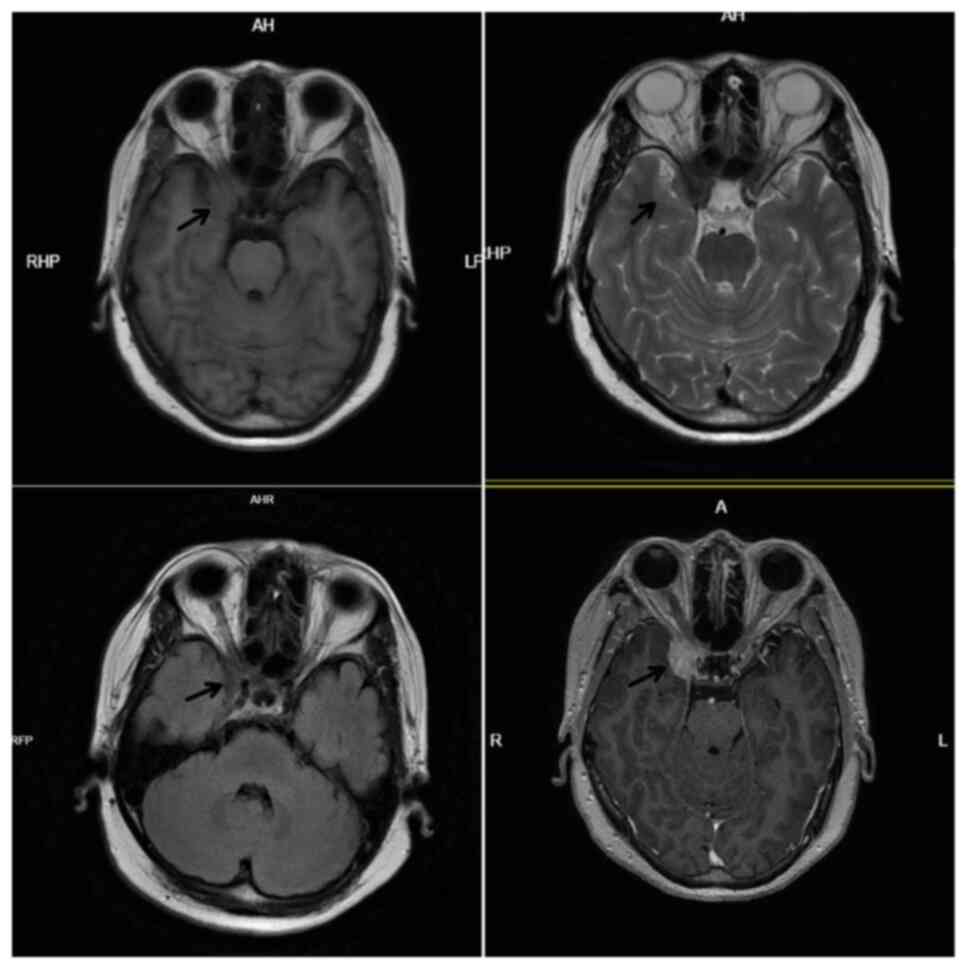
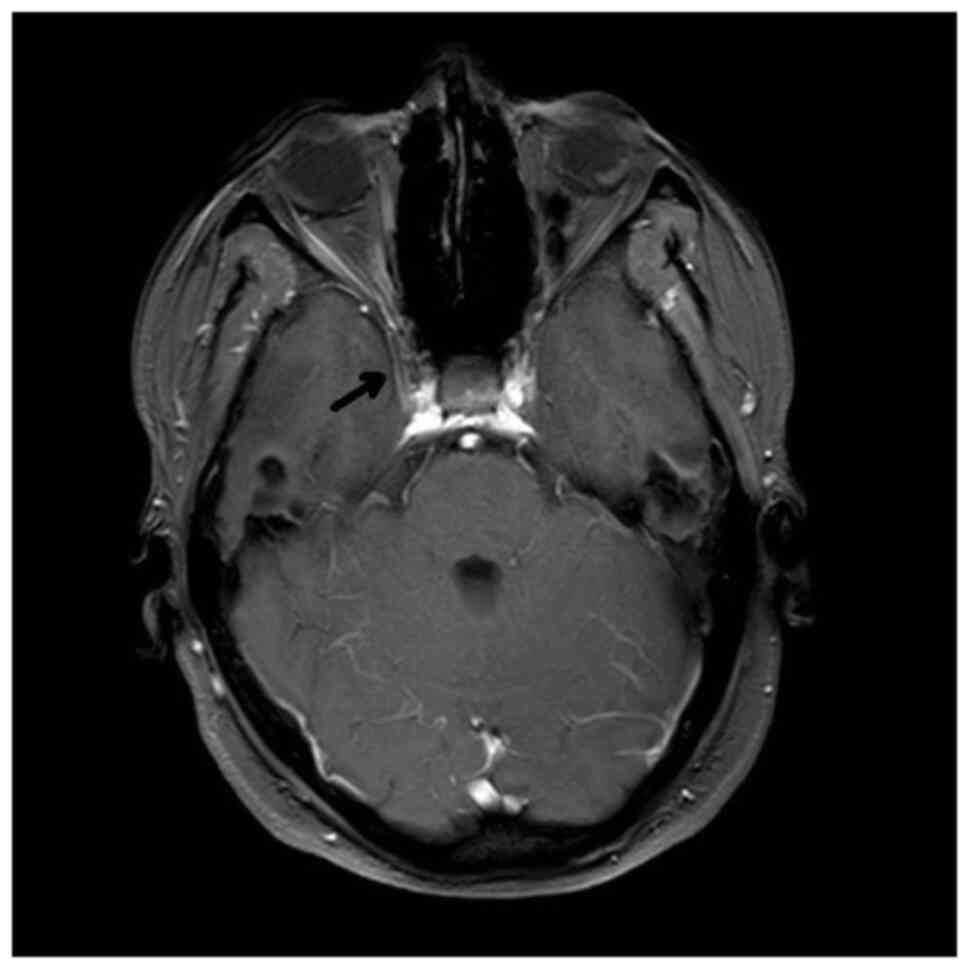
high-density lesions at the right parasellar region (Fig. 1). MRI revealed a right parasellar
lesion, ~30×25 mm, with equal signal on T1, low signal on T2 and
fluid-attenuated inversion recovery (FLAIR) and uniform enhancement
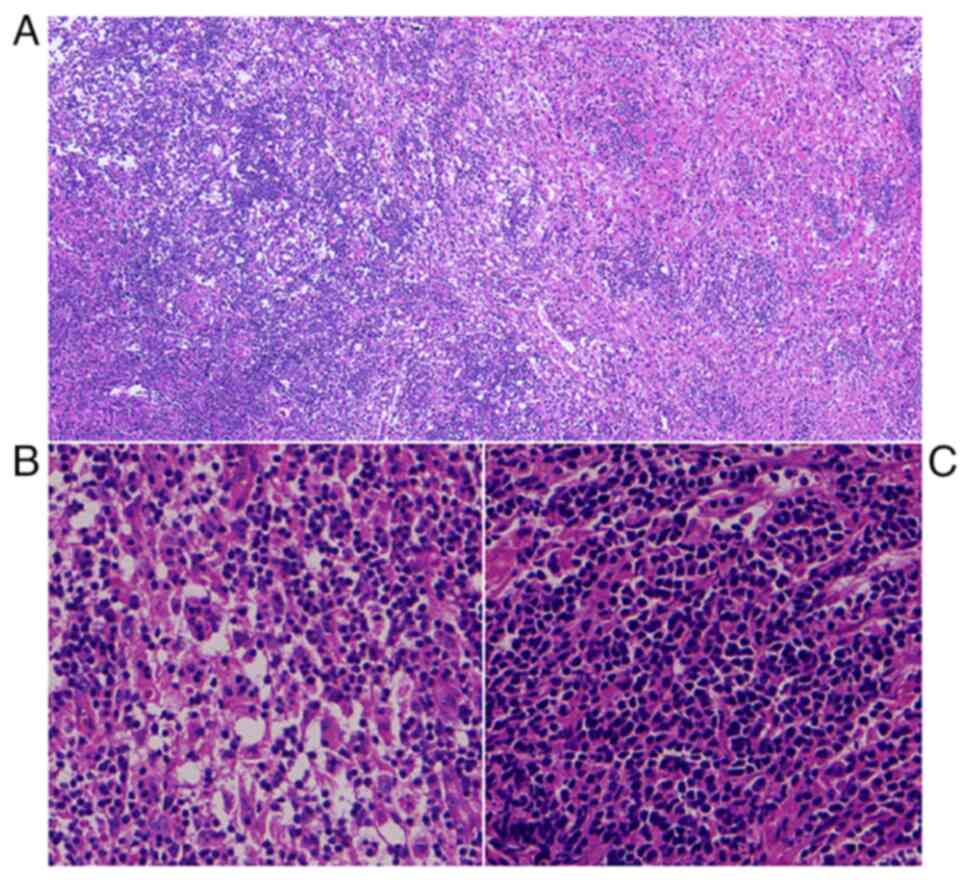
(Fig. 2). Subtotal resection of the
tumor was performed and postoperative pathology revealed a MALT
lymphoma complicated by RDD (Fig.
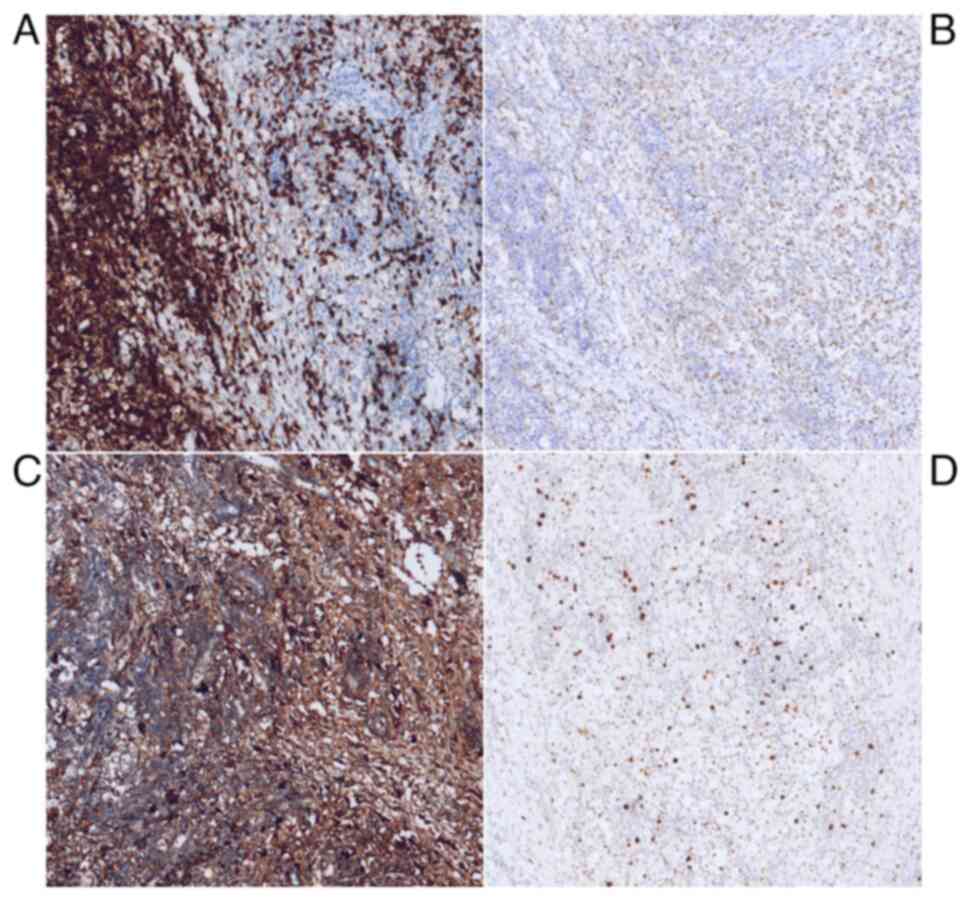
3). Immunohistochemistry (IHC) findings revealed the presence
of the following proteins: i) CD20(+); ii) CD79a(+); iii) S-100(+);
iv) CD68(+); v) κ (partially +); vi) CD3(−); vii) CD5(−);
viii) CD10(−); ix) CD43(−); x) CD21(−); xi) CD23(−); xii)
epithelial membrane antigen(−); xiii) Bcl-6(−); xiv) progesterone
receptor(−); and xv) Ki-67(+, 15%) (Fig. 4). The rearrangements of the
immunoglobulin heavy chain (IGH) gene were positive.
To determine whether the patient had lymphomas in
other locations, a bone marrow puncture was performed. Bone marrow
biopsy revealed good hematopoiesis and no lymphocytosis.
Rearrangements of the BCL-2, BCL-6 and IGH genes were negative.
PET-CT revealed that: i) The surgical site was slightly dense; and
ii) that there were multiple lymph nodes in the right neck with
increased 18F-fluorodeoxyglucose uptake. Lymphoma
infiltration was considered, which was treated using rituximab and
lenalidomide. The patient recovered well and the ptosis of the
right eyelid improved. Magnetic resonance imaging (MRI) examination
6 months after surgery demonstrated that the residual tumor had
disappeared (Fig. 5). After >1
year of follow-up, the patient was generally in good condition and
was going to work as normal.
Discussion
Rosai and Dorfman first reported four cases of SHML
in 1969, whose clinical manifestations are painless cervical
lymphadenopathy with low-grade fever, leukocytosis, weight loss and
elevated erythrocyte sedimentation rate (ESR) (1). Extranodal RDD is also common and may
occur in ~40% of patients (7). It
can be complicated by lymph node involvement, or be an independent
lesion of extranodal origin without lymphadenopathy (8). Common extranodal sites of involvement
include the skin and soft tissues (17%); the nasal cavity and
sinuses (16%); the eyes, orbits and ocular appendages (11%); the
skeletal system (11%); and the salivary glands (7%) (7,9). RDD
of the central nervous system (CNS) is rare and accounts for <5%
of reported RDD (10–12). Overall, ~75% of CNS RDD occur
intracranially, while 25% involve the spine (13). In addition, 70% are unassociated
with lymphadenopathy and are only manifested as solitary lesions
(13). Furthermore, >90% involve
only the meninges (11).
In 1983, Isaacson and Wright (4) reported that the IHC of certain
low-grade B-cell gastrointestinal lymphomas indicated features of
MALT. Subsequently, the authors extended these observations to
include numerous other extranodal low-grade B-cell lymphomas
(5). Paradoxically, the stomach is
the most common site of MALT lymphoma, where the lymphoid tissues
are often absent (14). In recent
years, other sites of MALT lymphoma have been reported, including
the lungs, ocular adnexa, breasts, skin, bladder, kidneys,
prostate, liver, gallbladder and cervix (15). MALT lymphomas can also occur
intracranially, although rarely (15,16).
According to a literature review by Matmati et al (16), 57 cases of dural MALT lymphoma have
been reported in total.
RDD is common among children and adolescents [median
age, 13 (range, 5–65) years] and is characterized by long duration
of the disease [median duration, 6 (range, 3–15) years], with a
slight predominance in males (7,16). By
contrast, intracranial MALT mainly occurs in adults and all
patients reported so far have been between 39 and 62 years old
(15). The majority occur in women,
accounting for 85.7% of cases (17).
The etiology of RDD remains unclear and possible
pathogeneses include infection [varicella-zoster virus, human
herpesvirus 6, Epstein-Barr virus (EBV), cytomegalovirus, HIV,
Brucella and Klebsiella] (18–20),
genetics and immune and inflammatory processes (19–21).
It is known that gastric MALT lymphomas are closely associated with
Helicobacter pylori, while MALT lymphomas in other locations
may not be associated with infectious stimuli (16). Its etiology remains to be
elucidated.
Intracranial RDD and MALT lymphomas are mostly
single intracranial lesions and extracranial lesions are rare
(3,16). The patient in the present report was
complicated by cervical lymph node infiltration in addition to the
intracranial lesions, which is even rarer (16). Intracranial RDD shares similar onset
locations and clinical symptoms with intracranial MALT lymphoma.
Common clinical manifestations include headache, vomiting,
epileptic seizures, limb weakness and cranial nerve deficit
depending on the location and size of the lesions (16,18).
According to a literature report, ESR, C-reactive
protein and D-dimer levels are elevated in numerous patients with
RDD (16). These indicators were
normal for the present patient and the present report did not find
any potential pathogens (including EBV, cytomegalovirus,
Brucella, Salmonella, hepatitis A, B and C viruses, HIV and
tubercle bacillus).
The imaging findings of intracranial RDD are similar
to those of intracranial MALT lymphoma. The majority of the
reported cases are located extra-axially and are closely associated
with the meninges (12,15,16).
There may be varying degrees of cerebral edema and meningeal
enhancement and only a few cases show invasion of the brain
parenchyma (17). It is similar to
meningioma in clinical and radiological aspects, so it is often
misdiagnosed as a meningioma before surgery (12,16,22).
Differential diagnosis includes meningiomas, eosinophilic
granulomas, intracranial solitary fibrous tumors, plasma cell
granulomas and dural metastases (12,23,24).
For the patient in the present case, meningioma was also considered
preoperatively. However, due to the short disease duration and
rapid progression, lymphoma was considered as well. In intracranial
RDD, free radicals generated by macrophage phagocytosis may appear
as hypointense on T2-weighted or FLAIR images of MRI, which may be
a manifestation of intracranial RDD (12,25).
According to literature reports, DWI in MRI of intracranial RDD
reveal restricted diffusion of lesions (11,12,16).
Meningiomas typically show increased choline levels, and alanine is
also present in some meningiomas (26). RDD has a higher choline peak
(26). The low intensity of MRI T2
and limited diffusion of MRI DWI are also imaging features of
intracranial MALT lymphoma that can help distinguish between MALT
lymphoma and typical meningiomas (16,27).
Diagnosis of intracranial RDD and MALT lymphoma
mainly depends on pathological examination (28,29).
In addition to typical cytological findings, the positive
expression of S-100 and CD68 on IHC staining are also the main
basis for differentiating RDD from other diseases (15,21).
Meanwhile, MALT lymphomas express B-cell-associated antigens (such
as CD20), but do not express CD5, CD10 or CD23 (16,30).
The patient in the present report was diagnosed as intracranial RDD
complicated by MALT lymphoma based on typical pathological
manifestations and IHC findings.
Occasionally, RDD can be complicated by other
conditions, including malignant diseases (such as lymphoma and
leukemia) and benign diseases (such as rheumatoid arthritis and
Sjögren's syndrome). There have been reports of RDD complicated by
lymphoma in the literature, which are extremely rare and are
individual cases (21). Literature
reviews have indicated that, as of 2018, <30 cases of RDD
complicated with lymphomas have been revealed, mainly occurring
with Hodgkin's lymphoma (31,32).
Reports of RDD complicated by MALT lymphoma are even rarer, with
only four cases identified through literature retrieval (21,32–34).
RDD can appear before or after lymphoma diagnosis and these two
pathological processes mostly involve different anatomical sites
(33,34). However, in a minority of patients,
RDD and lymphoma are found concurrently in the same specimens
(2,35,36).
Regarding the treatment of RDD and MALT lymphoma,
there is currently no standard therapeutic regimen due to the
rarity of the disease. For the majority of patients with RDD,
follow-up observation can be performed (37). As for patients with progressive,
symptomatic or refractory RDD, such treatments as radiotherapy,
chemotherapy and surgery are available (37,38).
Some researchers consider MALT lymphomas to be biologically inert
and thus can be followed closely after surgical resection, with or
without chemotherapy, or with delayed radiotherapy (16). The management of intracranial RDD is
similar to that of MALT lymphoma. Surgical resection is an
effective therapy, while other treatments include chemotherapy and
radiotherapy (12,15). The tumor in the present report was
not completely resected and PET-CT revealed lymphoma infiltration
in the neck. Considering that RDD and MALT lymphoma are sensitive
to chemotherapy, postoperative chemotherapy was used, which
achieved good efficacy.
Prognosis of RDD is associated with the number of
involved lymph nodes and/or the number of extranodal sites
(39). Overall, the prognosis is
good (39). RDD with poor outcome
is often accompanied by malignancy or immune disease (40). Intracranial MALT lymphoma is almost
always localized, which rarely presents with systemic involvement
and has a mean progression-free survival >29 months (16). The patient in the present report
underwent subtotal surgical resection supplemented with
chemotherapy. After >1 year of follow-up, the patient had no
symptoms and was going to work as normal.
In conclusion, both intracranial RDD and
intracranial MALT lymphoma are rare and occur primarily in the
meninges, with imaging manifestations resembling meningiomas. The
primary treatment is surgery, which can be supplemented by
chemotherapy and radiotherapy and the outcome is good.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
are available from the corresponding author on reasonable
request.
Authors' contributions
GW, HS and WC were responsible for designing and
conceiving the study. YL and YW acquired the data. YL and YW
analyzed and interpretated the data. GW, HS and WC drafted or
revised the manuscript for intellectual content. GW and HS confirm
the authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The Ethics Committee of the Second Affiliated
Hospital of Jiaxing University approved the study protocol
(approval no. jxey-20180021).
Patient consent for publication
The patient provided written informed consent for
publication of the article (including imaging results).
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Rosai J and Dorfman RF: Sinus
histiocytosis with massive lymphadenopathy. A newly recognized
benign clinicopathological entity. Arch Pathol. 87:63–70.
1969.PubMed/NCBI
|
|
2
|
Garg KK and Singh H: Sinus histiocytosis
with massive lymphadenopathy (rosai-dorfman disease) and anaplastic
large cell lymphoma. Eur J Case Rep Intern Med.
4:0006052017.PubMed/NCBI
|
|
3
|
Natarajan S, Post KD, Strauchen J and
Morgello S: Primary intracerebral rosai-dorfman disease: A case
report. J Neurooncol. 47:73–77. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Isaacson P and Wright DH: Malignant
lymphoma of mucosa-associated lymphoid tissue. A distinctive type
of B-cell lymphoma. Cancer. 52:1410–1416. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Isaacson P and Wright DH: Extranodal
malignant lymphoma arising from mucosa-associated lymphoid tissue.
Cancer. 53:2515–2524. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tian S, Pan T, Gao B, Li W, Liu J, Zou K
and Miao Y: Case report: Primary intracranial mucosa-associated
lymphoid tissue lymphoma presenting as two primary tumors involving
the cavernous sinus and extra-axial dura, respectively. Front
Oncol. 12:9270862023. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fukushima T, Yachi K, Ogino A, Ohta T,
Watanabe T, Yoshino A and Katayama Y: Isolated intracranial
Rosai-Dorfman disease without dural attachment-case report. Neurol
Med Chir (Tokyo). 51:136–140. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rodriguez-Galindo C, Helton KJ, Sánchez
ND, Rieman M, Jeng M and Wang W: Extranodal Rosai-Dorfman disease
in children. J Pediatr Hematol Oncol. 26:19–24. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dalia S, Sagatys E, Sokol L and Kubal T:
Rosai-Dorfman disease: Tumor biology, clinical features, pathology,
and treatment. Cancer Control. 21:322–327. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wu M, Anderson AE and Kahn LB: A report of
intracranial Rosai-Dorfman disease with literature review. Ann
Diagn Pathol. 5:96–102. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kattner KA, Stroink AR, Roth TC and Lee
JM: Rosai-Dorfman disease mimicking parasagittal meningioma: Case
presentation and review of literature. Surg Neurol. 53:452–457;
discussion 457. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Anoop TM, John J, Nair SG and Mathew BS:
Intracranial Rosai Dorfman disease. J Neurosci Rural Pract.
5:195–196. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hollowell JP, Wolfla CE, Shah NC, Mark LP
and Whittaker MH: Rosai-Dorman disease causing cervical myelopathy.
Spine (Phila Pa 1976). 25:1453–1456. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Isaacson PG: Gastrointestinal lymphoma.
Hum Pathol. 25:1020–1029. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sanjeevi A, Krishnan J, Bailey PR and
Catlett J: Extranodal marginal zone B-cell lymphoma of malt type
involving the cavernous sinus. Leuk Lymphoma. 42:1133–1137. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Matmati K, Matmati N, Hannun YA, Rumboldt
Z, Patel S, Lazarchick J, Stuart R and Giglio P: Dural MALT
lymphoma with disseminated disease. Hematol Rep. 2:e102010.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Park I, Huh J, Kim JH, Lee SW, Ryu MH and
Kang YK: Primary central nervous system marginal zone B-cell
lymphoma of the Basal Ganglia mimicking low-grade glioma: A case
report and review of the literature. Clin Lymphoma Myeloma.
8:305–308. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Arakaki N, Gallo G, Majluf R, Diez B,
Arias E, Riudavets MA and Sevlever G: Extranodal rosai-dorfman
disease presenting as a solitary mass with human herpesvirus 6
detection in a pediatric patient. Pediatr Dev Pathol. 15:324–328.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Henter JI, Tondini C and Pritchard J:
Histiocyte disorders. Crit Rev Oncol Hematol. 50:157–174. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Levine PH, Jahan N, Murari P, Manak M and
Jaffe ES: Detection of human herpesvirus 6 in tissues involved by
sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman
disease). J Infect Dis. 166:291–295. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Pang CS, Grier DD and Beaty MW:
Concomitant occurrence of sinus histiocytosis with massive
lymphadenopathy and nodal marginal zone lymphoma. Arch Pathol Lab
Med. 135:390–393. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Pavlou G, Pal D, Bucur S, Chakrabarty A
and van Hille PT: Intracranial non-Hodgkin's MALT lymphoma
mimicking a large convexity meningioma. Acta Neurochir (Wien).
148:791–793; discussion 793. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Jamali E, Sharifi G, Ghafouri-Fard S,
Bidari Zerehpoosh F, Yazdanpanahi M and Taheri M: Intracranial
Rosai Dorfman disease presented with multiple huge intraventricular
masses: A case report. Front Surg. 9:7668402022. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Gubian A, Ganau M, Cebula H, Todeschi J,
Scibilia A, Noel G, Spatola G, Chaussemy D, Nannavecchia B,
Gallinaro P, et al: Intracranial solitary fibrous tumors: A
heterogeneous entity with an uncertain clinical behavior. World
Neurosurg. 126:e48–e56. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zhu H, Qiu LH, Dou YF, Wu JS, Zhong P,
Jiang CC, Xu R and Wang XQ: Imaging characteristics of
Rosai-Dorfman disease in the central nervous system. Eur J Radiol.
81:1265–1272. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Yue Q, Isobe T, Shibata Y, Anno I,
Kawamura H, Yamamoto Y, Takano S and Matsumura A: New observations
concerning the interpretation of magnetic resonance spectroscopy of
meningioma. Eur Radiol. 18:2901–2911. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sebastián C, Vela AC, Figueroa R, Marín MÁ
and Alfaro J: Primary intracranial mucosa-associated lymphoid
tissue lymphoma. A report of two cases and literature review.
Neuroradiol J. 27:425–430. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhao YR, Hu RH, Wu R and Xu JK: Primary
mucosa-associated lymphoid tissue lymphoma in the midbrain: A case
report. World J Clin Cases. 9:6566–6574. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Jurić G, Jakić-Razumović J, Rotim K and
Zarković K: Extranodal sinus histiocytosis (Rosai-Dorfman disease)
of the brain parenchyma. Acta Neurochir (Wien). 145:145–149;
discussion 149. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ferguson SD, Musleh W, Gurbuxani S,
Shafizadeh SF and Lesniak MS: Intracranial mucosa-associated
lymphoid tissue (MALT) lymphoma. J Clin Neurosci. 17:666–669. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Edelman A, Patterson B, Donovan K, Malone
J and Callen J: Rosai-Dorfman disease with a concurrent mantle cell
lymphoma. JAAD Case Rep. 5:40–43. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Gorodetskiy VR, Klapper W, Probatova NA,
Vasilyev VI and Rozhnova EV: Simultaneous occurrence of
rosai-dorfman disease and nodal marginal zone lymphoma in a patient
with Sjögren's Syndrome. Case Rep Hematol.
2018:79308232018.PubMed/NCBI
|
|
33
|
Machan S, Medina C, Rodríguez-Pinilla SM,
Suárez-Peñaranda JM, Castro Y, Molés P, Requena C, Saus C, Requena
L and Santonja C: Primary cutaneous marginal IgG4 lymphoma and
Rosai-Dorfman's disease coexisting in several lesions of the same
patient. Am J Dermatopathol. 37:413–418. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Akria L, Sonkin V, Braester A, Cohen HI,
Suriu C and Polliack A: Rare coexistence of Rosai-Dorfman disease
and nodal marginal zone lymphoma complicated by severe
life-threatening autoimmune hemolytic anemia. Leuk Lymphoma.
54:1553–1556. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Falk S, Stutte HJ and Frizzera G:
Hodgkin's disease and sinus histiocytosis with massive
lymphadenopathy-like changes. Histopathology. 19:221–224. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Lu D, Estalilla OC, Manning JT Jr and
Medeiros LJ: Sinus histiocytosis with massive lymphadenopathy and
malignant lymphoma involving the same lymph node: A report of four
cases and review of the literature. Mod Pathol. 13:414–419. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Pulsoni A, Anghel G, Falcucci P, Matera R,
Pescarmona E, Ribersani M, Villivà N and Mandelli F: Treatment of
sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman
disease): Report of a case and literature review. Am J Hematol.
69:67–71. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Adeleye AO, Amir G, Fraifeld S, Shoshan Y,
Umansky F and Spektor S: Diagnosis and management of Rosai-Dorfman
disease involving the central nervous system. Neurol Res.
32:572–578. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Montgomery EA, Meis JM and Frizzera G:
Rosai-Dorfman disease of soft tissue. Am J Surg Pathol. 16:122–129.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Foucar E, Rosai J and Dorfman R: Sinus
histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease):
Review of the entity. Semin Diagn Pathol. 7:19–73. 1990.PubMed/NCBI
|