Introduction
Angiosarcomas usually occur on the scalp and upper
forehead (1), with scalp
angiosarcoma (SA) accounting for ~50% of all angiosarcoma cases
(2). A history of radiation and
chronic lymphoedema are established risk factors for the disease,
while being immunocompromised, and the presence of arteriovenous
fistulae and xeroderma pigmentosum are potential risk factors for
the disease (3). Angiosarcomas that
occur on the scalp and face are more likely to recur, and treatment
of angiosarcomas in these areas is difficult (4). The prognosis for angiosarcoma of the
head and neck is poor, with a reported 5-year survival rate of
11–53% (5). Treatment options for
angiosarcoma include curative-intent surgery, radiotherapy and
chemotherapy (6). Curative-intent
surgery has been reported to contribute to overall survival in
patients with primary angiosarcomas of the scalp and face (5). For angiosarcoma with distant
metastases, cytotoxic chemotherapy is the mainstay of treatment
(6). However, the best treatment
strategy remains uncertain.
The present study reports the case of a patient with
multiple postoperative SA recurrences. On each occasion, the
patient was treated using curative-intent surgery alone; however,
the prognosis was poor.
Case report
Patient
The present study reports the case of an 87-year-old
man hospitalized for the fifth time with SA. The patient had
suffered multiple lacunar infarctions and gout for >3 and >5
years, respectively. The patient had experienced four previous
recurrences of SA and underwent curative-intent surgery four times
(Table I). Each time angiosarcoma
recurred, the patient underwent curative-intent surgery with
negative pathological margins. No radiotherapy or chemotherapy was
administered after the surgeries. The fifth recurrence was in
September 2022, when a dark red mass measuring ~1.5×1.0 cm appeared
on the scalp, which gradually increased in size and became more
numerous; ulcers also developed. The lesion was painful which was
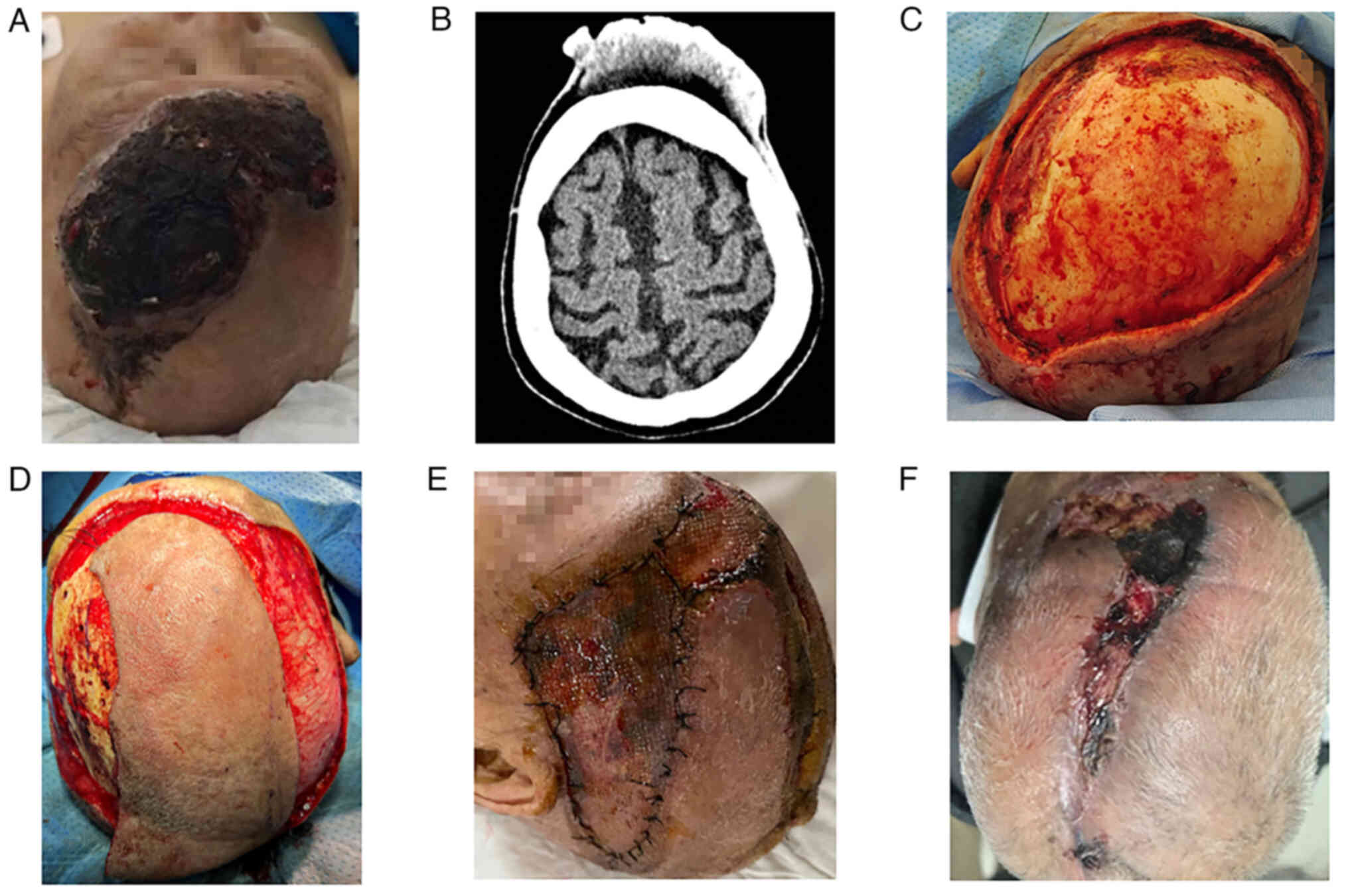
relieved with oral painkillers. On physical examination, an
irregularly shaped mass measuring ~14.0×7.0 cm was identified, with
most of the surface of the mass broken and bleeding (Fig. 1A). Cranial computed tomography
demonstrated an irregular soft tissue mass with uneven density in
the frontal region; no invasive damage to the skull was
demonstrated (Fig. 1B). The
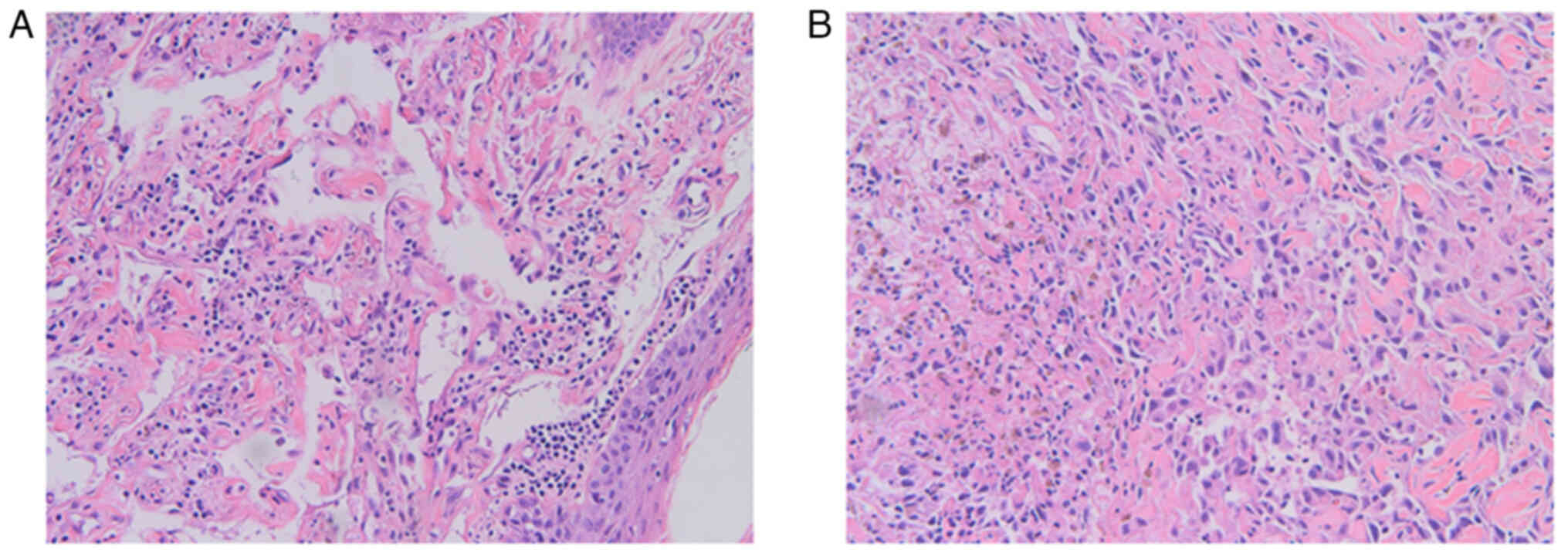
postoperative pathological diagnosis of the fourth recurrence was
angiosarcoma (Fig. 2A).
Immunohistochemically, the tumour cells were positive for CD31,
CD34 and D2-40, with a Ki-67 focal positivity rate of ~30%. The
patient was diagnosed with recurrent SA. Considering the patient's
poor condition, curative-intent surgery was performed in a single
stage (Fig. 1C), followed by
postoperative flap grafting and skin grafting twice, 7 days
(Fig. 1D) and 14 days later. The
wound had healed well 7 days after the second postoperative flap
and skin grafting was performed (Fig.
1E). Postoperative recovery was fair, and the patient was
discharged. The post-operative pathological diagnosis was
angiosarcoma (Fig. 2B).
 | Table I.Times of tumour discovery and
treatment. |
Table I.
Times of tumour discovery and
treatment.
|
| Disease
occurrence |
|---|
|
|
|
|---|
| Action | 1st | 2nd | 3rd | 4th | 5th |
|---|
| Discovery of
tumour | November 2019 | July 2020 | January 2021 | April 2021 | September 2022 |
| Treatment | December 2019 | September 2020 | February 2021 | August 2021 | November 2022 |
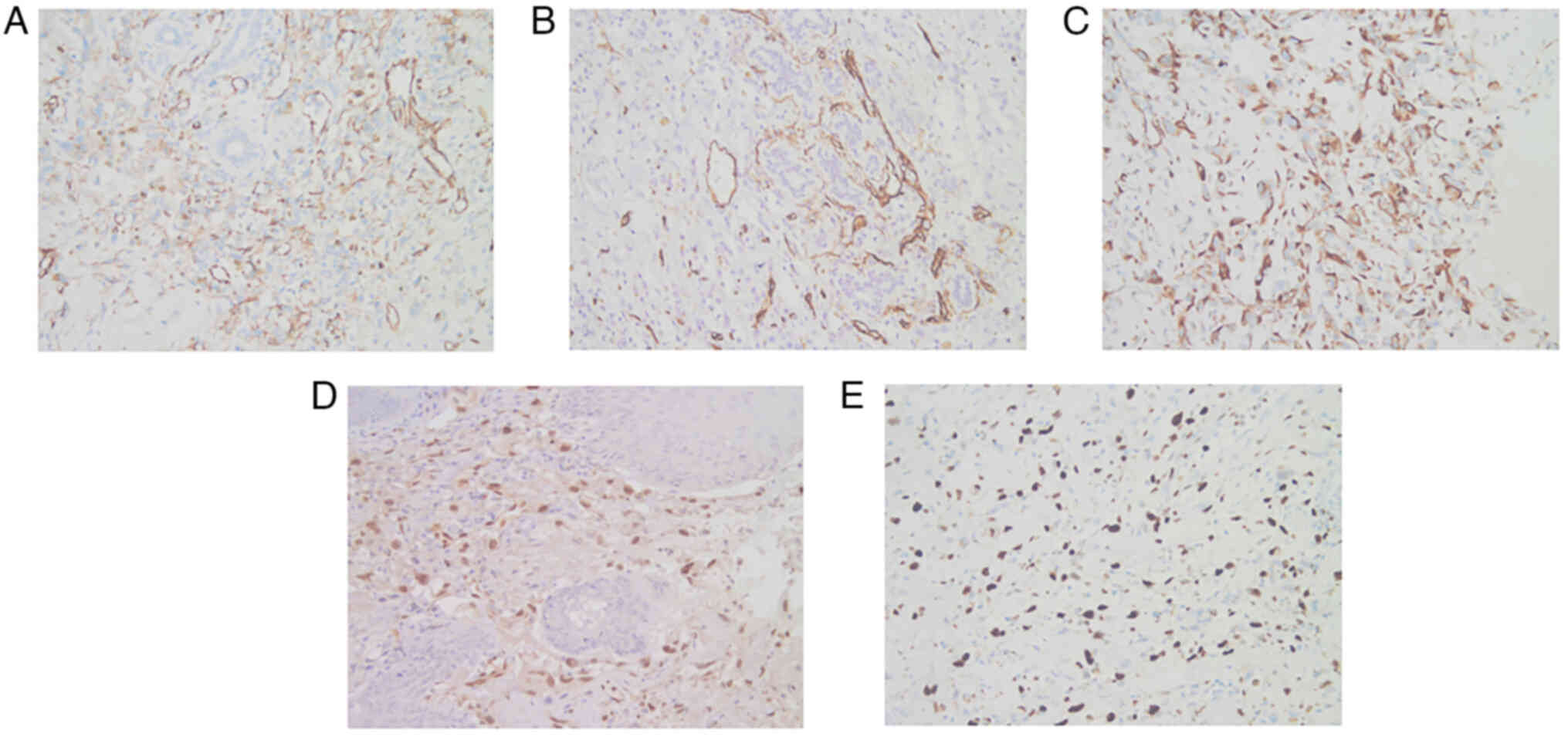
The cells were positive for CD31 (Fig. 3A), CD34 (Fig. 3B), D2-40, Vimentin (Fig. 3C) and ETS-related gene (ERG)
(Fig. 3D), with a Ki-67 (Fig. 3E) focal positivity rate of ~50%, as
observed by light microscopy. Hematoxylin and eosin staining was
also performed.
At 20 days after surgery, some of the tissue at the
edges of the surgical area became necrotic (Fig. 1F) and the necrotic area
progressively increased. At 4 months subsequent to this, the
patient died of multiple organ failure.
Tissue analysis
Immunohistochemical staining was performed by the
Department of Pathology using formalin-fixed (0.4% neutral formalin
for 12 h), paraffin-embedded tissues at a 3- to 4-µm thickness.
Antigen retrieval was performed using a stainless steel pan at
~110°C. PBS was used as the washing reagent. Rehydration was
performed in a descending alcohol series diluted with
double-distilled water. Hydrogen peroxide (3%) was used to block
endogenous peroxidase/phosphatase activity. Incubation for was
performed with the following primary antibodies: CD31 (cat. no.
ZM-0044; OriGene Technologies, Inc.; 37°C; 60 min), CD34 (cat. no.
ZM-0046; OriGene Technologies, Inc.; 37°C; 60 min), ERG (cat. no.
ZM-0103; OriGene Technologies, Inc.; 37°C; 60 min), D2-40 (cat. no.
MAB-0567; Fuzhou Maixin Biotech. Co., Ltd.; room temperature; 60
min), Ki-67 (cat. no. 05278384001; Roche Diagnostics; 37°C; 16 min)
and vimentin (cat. no. 05278139001; Roche Diagnostics; 37°C; 16
min) (all ready-to-use). Secondary antibody incubation was
performed using the contents of the PV-8000D (OriGene Technologies,
Inc.) and 05269806001 (Roche Diagnostics) kits at room temperature
for 20 and 10 min, respectively. Hematoxylin staining solution was
applied for 30 sec at room temperature for counterstaining.
HE staining was performed by the Department of
Pathology using formalin-fixed (0.4% neutral formalin for 12 h),
paraffin-embedded tissues at a 3- to 4-µm thickness. Samples were
heated to 80°C for 10 min. The waxes were dissolved by placing the
paraffin sections in a deparaffinising agent (xylene for 3 min,
three times). An appropriate dewatering solution (in a descending
alcohol series diluted with double-distilled water) was used for
deparaffinisation. Hematoxylin staining was performed for 5 min.
The sections were acid-washed in acidic alcohol to remove excess
hematoxylin dye (1% hydrochloric alcohol for 13 sec and 95% ethanol
CH3CH2OH for 30 sec). Eosin staining was
performed for 1 min.
Discussion
SA is rare, accounting for <1% of soft tissue
sarcomas (7) and its prognosis is
poor. The prognostic factors for SA are related to tumour diameter,
infiltration depth, margin status, recurrence and metastasis
(8).
The most reliable treatment strategy for SA is
surgery (9–13) and patients can undergo surgical
excision which can improve their survival (7). Curative-intent surgery is associated
with increased overall survival in patients with primary cutaneous
angiosarcomas of the scalp and face (5). Reports in the literature state that
the 1- and 5-year survival rates for patients who did not undergo
definitive surgery were 68.0 and 18.0%, respectively, compared with
78.2 and 34.1% for those who underwent surgery; however, there
remains a risk of local tumour recurrence after surgical resection
(11,14–16).
The combination of radiotherapy and chemotherapy can deliver better
results than any single regimen (17).
In addition to surgery, radiotherapy and
chemotherapy can improve a patient's condition. Radiotherapy serves
a significant role in controlling tumour growth, reducing
exudation, and preventing rupture. Radiotherapy can also improve
the efficacy of treatment for patients with SA (18). Two patients have been reported to
have been cured by radiotherapy alone (19,20).
Patel and Speer (19) reported that
a patient received radiotherapy as a single modality treatment that
resulted in complete remission of an angiosarcoma of the face.
Gkalpakiotis et al (20)
reported that an elderly patient was cured of angiosarcoma by
undergoing radiotherapy and had no recurrence in the long term.
Sorrentino et al (21)
reported that postoperative radiotherapy improved the prognosis of
patients with SA. Ohguri et al (22) reported that radiotherapy combined
with recombinant interleukin 2 is a highly effective and efficient
method for treating SA. However, recurrence and distant metastases
may still occur after radiotherapy (23). Cheng et al (24) reported the case of a 77-year-old
patient who developed recurrence and distant metastases after
receiving postoperative adjuvant radiotherapy. The patient later
received intravenous paclitaxel, which markedly improved their
condition (24). Chemotherapy has
been recommended for patients who are ineligible for surgical
tumour removal or those who experience recurrence or distant
metastases after treatment (11,25).
Paclitaxel, an effective agent for angiosarcoma treatment, may
prolong survival by reducing the rate of distant failure after
radiotherapy (26). Penel et
al (27) and Fujisawa et
al (28) performed a phase II
clinical trial and retrospective study, respectively, and reported
that the prognosis of paclitaxel combined with radiotherapy was
better than that of conventional surgery combined with
radiotherapy, and paclitaxel combined with radiotherapy was better
than radiotherapy alone. Therefore, radiation therapy combined with
chemotherapy is now recommended for the curative treatment of
patients who can or cannot undergo surgery (29). However, postoperative patients
should be monitored for bone marrow suppression as one of the
possible side effects of chemotherapy (30). Moreover, appropriate indications for
adjuvant chemotherapy should be further elucidated to reduce
potential toxicity issues and issues with tolerance to taxane-based
regimens (6).
In addition to radiotherapy and chemotherapy,
targeted therapy can also be used to treat angiosarcoma. Ji et
al (6) reported the case of
advanced angiosarcoma successfully treated with apatinib, an oral
tyrosine kinase inhibitor targeting the intracellular domain of
vascular endothelial growth factor receptor-2. This suggested that
apatinib had fewer toxic effects than traditional cytotoxic
chemotherapy, making it a potential alternative for angiosarcoma
treatment, particularly in elderly patients (6).
In the present case, given the patient's age and
poor condition, radiotherapy or chemotherapy was not performed
after each surgery. It was hypothesised however, that such patients
should receive a combination of radiotherapy and chemotherapy after
surgery whenever possible, which may improve their prognosis.
However, this view has certain limitations and should be assessed
by further studies with larger sample sizes which consider the
risks that radiotherapy may pose to patients.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Author's contributions
LM and SL researched the literature, studied the
clinical cases and revised the manuscript. DL researched the
clinical case, participated in the treatment of the patient and
wrote the first draft of the manuscript. ZS researched the clinical
case and participated in the treatment of the patient. All authors
reviewed and edited the manuscript, and read approved the final
manuscript. LM and ZS confirm the authenticity of all the raw
data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Consent for publication was obtained from the
patient's legal guardians as the patient had passed away at the
time of writing.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Nakamura Y, Nakamura Y, Hori E, Furuta J,
Kawachi Y and Otsuka F: Complete long-term response of angiosarcoma
of the scalp with cervical lymph node metastases treated with a
combination of weekly and monthly docetaxel. Br J Dermatol.
163:1357–1358. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Almogy G, Lieberman S, Gips M, Pappo O,
Edden Y, Jurim O, Simon Slasky B, Uzieli B and Eid A: Clinical
outcomes of surgical resections for primary liver sarcoma in
adults: Results from a single centre. Eur J Surg Oncol. 30:421–427.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sturm EC, Marasco IS and Katz SC:
Multidisciplinary management of Angiosarcoma-A review. J Surg Res.
257:213–220. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Maddox JC and Evans HL: Angiosarcoma of
skin and soft tissue: A study of forty-four cases. Cancer.
48:1907–1921. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Oashi K, Namikawa K, Tsutsumida A,
Takahashi A, Itami J, Igaki H, Inaba K and Yamazaki N: Surgery with
curative intent is associated with prolonged survival in patients
with cutaneous angiosarcoma of the scalp and face-a retrospective
study of 38 untreated cases in the Japanese population. Eur J Surg
Oncol. 44:823–829. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ji G, Hong L and Yang P: Successful
treatment of angiosarcoma of the scalp with apatinib: A case
report. Onco Targets Ther. 9:4989–4992. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cassidy RJ, Switchenko JM, Yushak ML,
Madden N, Khan MK, Monson DK, Beitler JJ, Landry JC, Godette KD,
Gillespie TW and Patel KR: The importance of surgery in scalp
angiosarcomas. Surg Oncol. 27:A3–A8. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Morgan MB, Swann M, Somach S, Eng W and
Smoller B: Cutaneous angiosarcoma: A case series with prognostic
correlation. J Am Acad Dermatol. 50:867–874. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Young RJ, Brown NJ, Reed MW, Hughes D and
Woll PJ: Angiosarcoma. Lancet Oncol. 11:983–991. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mendenhall WM, Mendenhall CM, Werning JW,
Reith JD and Mendenhall NP: Cutaneous angiosarcoma. Am J Clin
Oncol. 29:524–528. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Patel SH, Hayden RE, Hinni ML, Wong WW,
Foote RL, Milani S, Wu Q, Ko SJ and Halyard MY: Angiosarcoma of the
scalp and face: The Mayo Clinic experience. JAMA Otolaryngol Head
Neck Surg. 141:335–340. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pawlik TM, Paulino AF, McGinn CJ, Baker
LH, Cohen DS, Morris JS, Rees R and Sondak VK: Cutaneous
angiosarcoma of the scalp: A multidisciplinary approach. Cancer.
98:1716–1726. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
NCCN Clinical Practice Guidelines in
Oncology, . Soft tissue sarcoma version 2. 2017.https://www.nccn.org/professionals/physician_gls/PDF/sarcoma.pdfDecember
5–2017
|
|
14
|
Köhler HF, Neves RI, Brechtbühl ER, Mattos
Granja NV, Ikeda MK and Kowalski LP: Cutaneous angiosarcoma of the
head and neck: Report of 23 cases from a single institution.
Otolaryngol Head Neck Surg. 139:519–524. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Buschmann A, Lehnhardt M, Toman N, Preiler
P, Salakdeh MS and Muehlberger T: Surgical treatment of
angiosarcoma of the scalp: Less is more. Ann Plast Surg.
61:399–403. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Guadagnolo BA, Zagars GK, Araujo D, Ravi
V, Shellenberger TD and Sturgis EM: Outcomes after definitive
treatment for cutaneous angiosarcoma of the face and scalp. Head
Neck. 33:661–667. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hwang K, Kim MY and Lee SH:
Recommendations for therapeutic decisions of angiosarcoma of the
scalp and face. J Craniofac Surg. 26:e253–e256. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hata M: Radiation Therapy for angiosarcoma
of the scalp: Total scalp irradiation and local irradiation.
Anticancer Res. 38:1247–1253. 2018.PubMed/NCBI
|
|
19
|
Patel VB and Speer TW: Successful
treatment of an angiosarcoma of the nose with radiation therapy.
Case Rep Oncol. 5:570–575. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gkalpakiotis S, Arenberger P, Vohradnikova
O and Arenbergerova M: Successful radiotherapy of facial
angiosarcoma. Int J Dermatol. 47:1190–1192. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sorrentino R, Vitiello R and Castelli ML:
Angiosarcoma of the larynx. Case report and review of the
literature. Acta Otorhinolaryngol Ital. 23:191–193. 2003.PubMed/NCBI
|
|
22
|
Ohguri T, Imada H, Nomoto S, Yahara K,
Hisaoka M, Hashimoto H, Tokura Y, Nakamura K, Shioyama Y, Honda H,
et al: Angiosarcoma of the scalp treated with curative radiotherapy
plus recombinant interleukin-2 immunotherapy. Int J Radiat Oncol
Biol Phys. 61:1446–1453. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mendenhall WM, Mendenhall CM, Werning JW,
Reith JD and Mendenhall NP: Cutaneous angiosarcoma. Cancer.
44:524–528. 2006.
|
|
24
|
Cheng YS, Chen TM, Tsai WC and Huang TW:
Pulmonary metastatic angiosarcoma from scalp with fatal
complication: A case report. Int J Surg Case Rep. 34:36–39. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Bhatti Z, Bhatti R, Brangman S, Whiting K
and Dhamoon A: Extensive cutaneous scalp angiosarcoma. Case Rep
Dermatol Med. 2018:84098202018.PubMed/NCBI
|
|
26
|
Donghi D, Dummer R and Cozzio A: Complete
remission in a patient with multifocal metastatic cutaneous
angiosarcoma with a combination of paclitaxel and sorafenib. Br J
Dermatol. 162:697–699. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Penel N, Bui BN, Bay JO, Cupissol D,
Ray-Coquard I, Piperno-Neumann S, Kerbrat P, Fournier C, Taieb S,
Jimenez M, et al: Phase II trial of weekly paclitaxel for
unresectable angiosarcoma: The ANGIOTAX Study. J Clin Oncol.
26:5269–5274. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Fujisawa Y, Ito M, Mori K, Okada S,
Nakamura Y, Kawachi Y and Otsuka F: Intra-arterial
mitoxantrone/paclitaxel in angiosarcoma of the lower limb
associated with chronic lymphedema (Stewart-Treves syndrome) in a
patient with cervical cancer. Eur J Dermatol. 21:119–120. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lee KT, Moon J, Jeong HS, Lim HS and Lim
SY: Benefits of the multidisciplinary approach after curative
surgery for the treatment of scalp angiosarcoma. Ann Plast Surg.
86:39–45. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Yang P, Zhu Q and Jiang F: Combination
therapy for scalp angiosarcoma using bevacizumab and chemotherapy:
A case report and review of literature. Chin J Cancer Res.
25:358–361. 2013.PubMed/NCBI
|