Introduction
Gastric cancer is one of the leading causes of
cancer death and a malignant tumor with a high global incidence
(11.7%) (1). Gastric cancer is also
a common gastrointestinal tumor, and the 5-year survival rate is
very low (<15.0%) (2). In China,
gastric cancer has a rapid annual increase in incidence, and was
responsible for 8.2% of all deaths from cancer in 2018 (3–5).
Clinically, gastrectomy is the main treatment for patients with
non-metastatic gastric cancer, and early surgery can reduce the
incidence of cancer-related mortality and tumor metastasis
(6,7). Although the prognosis of advanced
gastric cancer has been improved by the use of gastrectomy with
adjuvant therapy (radiotherapy, chemotherapy, immunotherapy and
other therapies), the 5-year overall survival rate is still low
(8). In addition, patients with
gastric cancer who undergo gastrectomy frequently experience
postoperative complications (POCs), with a reported range of 20–46%
of cases affected (9). The most
common POCs of patients with gastric cancer who undergo gastrectomy
are gastric hemorrhage, duodenal stump rupture, gastrointestinal
anastomotic fistula and postoperative obstruction (10). Furthermore, POCs may increase the
risk of metal health issues and decrease the quality of life in the
perioperative period (11).
Traditional Chinese medicine (TCM) has antitumor
potential, with the characteristics of access to multiple targets,
a low number of side effects and good therapeutic effects (12). TCM nursing intervention is
frequently used in clinical care, including for postoperative care
for malignant tumor resections and percutaneous coronary
intervention (13). In recent
years, TCM has been shown to be effective in treating patients with
gastric cancer, with its main advantages being that it is a
comprehensive intervention with multiple approaches and multiple
targets for tumor cells (14–16).
Clinically, TCM nursing can prolong the survival time and improve
the quality of life for patients with cancer due to less side
effects (17). Perioperative TCM
nursing intervention can improve an unhealthy mental state and
reduces the occurrence of POCs in patients with gastric cancer
(18). Treatment with TCM regulates
both innate immunity (dendritic cells, myeloid-derived suppressor
cells, natural killer cells and macrophages) and adaptive immunity
(regulatory T and B cells, and CD4/CD8 T lymphocytes) (19). Combining early chemotherapy with TCM
(Zhipu Liujunzi decoction) nursing intervention can improve the
function of the immune system and the quality of life in patients
with gastric cancer after surgery (20). More recently, the understanding of
the targets and mechanisms of TCM involved in the consequent
alterations in tumor parameters has expanded (16,21).
Notably, when used as an adjuvant therapy TCM has been indicated to
extend the median survival time and improve the overall survival
rate of patients with gastric cancer (22). However, further studies and clinical
trials are required in order to assess the efficiency and safety of
TCM in patients with gastric cancer after gastrectomy.
Nursing intervention is an effective approach to aid
patients with gastric cancer who suffer from psychological
disorders during the perioperative period (23). Although postoperative TCM nursing
interventional therapy should be integrated for patients across all
stages of gastric cancer, most nursing intervention has focused on
patients with metastatic disease (24). It has been shown that Jianpi
Yangzheng Xiaozheng decoction can reduce the incidence of adverse
drug reactions and improve the quality of life of patients with
gastric cancer (25). Jianpi
Yangzheng Xiaozheng decoction comprises Dangshen (Campanulaceae),
Baizhu (Composite), Fuling (Polyporaceae), Shengyiren (Composite),
Danggui (Grass family), Shanyao (Dioscoreaceae), Muxiang
(Composite), Baishao (Asclepiadaceae), Chenpi (Rutaceae), Baqia
(Liliaceae), Shijianchuan (Lamiaceae) and Zhigancao (Leguminosae),
which decrease the toxic effects of chemotherapy, regulate immune
function and improve macrophage cell activity in patients with
gastric cancer (26). Jianpi
Yangzheng Xiaozheng decoction considerably improves the quality of
life of patients, relieving pain and prolonging survival time for
patients with advanced-stage gastric cancer in China (25). However, there is limited knowledge
on the potential effects of Jianpi Yangzheng Xiaozheng decoction
nursing intervention on patients with gastric cancer after
gastrectomy.
The present study investigated the ameliorative
effects of TCM (Jianpi Yangzheng Xiaozheng decoction) nursing
intervention on POCs and long-term survival in patients with
gastric cancer after curative resection. The effects of TCM nursing
intervention on postoperative gastrointestinal function,
inflammatory index, physical capacity, quality of life, immune
activity and recurrence were also systematically investigated.
Materials and methods
Patients
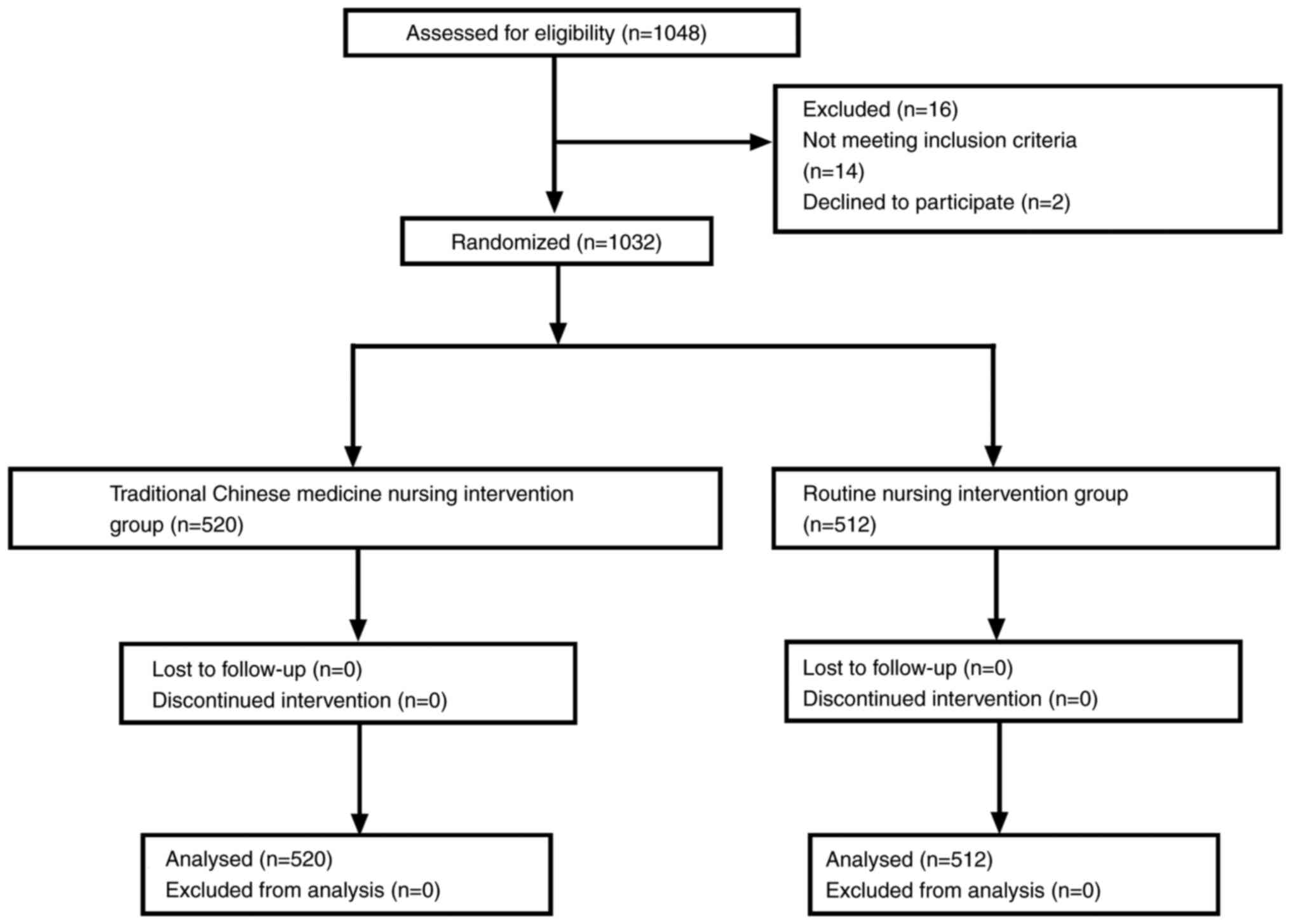
The present study is a prospective, randomized
controlled trial that was performed in The First Hospital of Harbin
(Harbin, China). The study protocol was approved by the Ethics
Committee of The First Hospital of Harbin (approval no.
20150507TFHX1). A total of 1,032 eligible patients with gastric
cancer who underwent gastrectomy were recruited between May 2015
and June 2017. All patients were diagnosed with gastric cancer
using imaging and pathology assessments and met the indications for
radical gastrectomy. The baseline clinicopathological
characteristics, including hypoproteinemia, tumor size, tumor stage
and American Society of Anesthesiologists grade (27) were analyzed and are shown in
Table I. After gastrectomy,
patients voluntarily chose to undergo postoperative treatment and
all patients provided written informed consent. All the patients
were randomly assigned into two groups: The TCM nursing
intervention group (TCM group; n=520) and the routine nursing
intervention group (control group; n=512). Patients were assigned
into these two groups using a block randomization method based on
the disease status of patients with cancer (28). No differences in treatment were
applied between the two groups, with the exception of the Jianpi
Yangzheng decoction. The TCM used in this study was Jianpi
Yangzheng decoction, which is composed of 12 types of Chinese
herbal medicine (15 g Dangshen, 10 g Baizhu, 10 g Fuling, 15 g
Shengyiren, 10 g Danggui, 15 g Shanyao, 10 g Muxiang, 10 g Baishao,
6 g Chenpi, 10 g Baqia, 15 g Shijianchuan and 3 g Zhigancao)
(26). The raw herbs for the Jianpi
Yangzheng decoction were obtained from Heilongjiang Traditional
Chinese Medicine Hospital (Harbin, China). All the herbs were mixed
with 500 ml sterile water and boiled for 30 min, and then the
patients drunk the leachate. One dose of Jianpi Yangzheng decoction
was orally administrated to the TCM group every day after
gastrectomy for at least 6 months. The study flowchart is shown in
Fig. 1. The duration of the
postoperative hospital stay for patients after gastrectomy was
recorded.
 | Table I.Baseline clinicopathological
characters of patients with gastric cancer who underwent a
gastrectomy. |
Table I.
Baseline clinicopathological
characters of patients with gastric cancer who underwent a
gastrectomy.
| Characteristic | Control | TCM | P-value |
|---|
| Total patients, n
(%) | 512 (49.6) | 520 (50.4) |
|
| Sex, n (%) |
|
| 0.84a |
|
Male | 265 (51.8) | 272 (52.3) |
|
|
Female | 247 (48.2) | 248 (47.7) |
|
| Age, years | 57.2±7.3 | 57.8±8.2 | 0.72b |
| BMI,
kg/m2 | 22.4±3.6 | 22.2±3.4 | 0.78b |
| Hypoproteinemia, n
(%) |
|
| 0.72a |
|
Yes | 412 (80.5) | 408 (78.5) |
|
| No | 100 (19.5) | 112 (21.5) |
|
| Tumor size, n
(%) |
|
| 0.80a |
| ≤5
cm | 391 (76.4) | 397 (76.3) |
|
| >5
cm | 121 (23.6) | 123 (23.7) |
|
| TNM tumor stage, n
(%) |
|
| 0.90a |
| I | 138 (27.0) | 142 (27.3) |
|
| II | 313 (61.1) | 320 (61.5) |
|
|
III | 61 (11.9) | 58 (11.2) |
|
| ASA grade, n
(%) |
|
| 0.87a |
| I | 330 (64.5) | 336 (64.6) |
|
| II | 120 (23.4) | 115 (22.1) |
|
|
III | 62 (12.1) | 69 (13.3) |
|
Inclusion criteria and exclusion
criteria
The inclusion criteria for the study were as
follows: i) Patients diagnosed with gastric cancer; ii) patients
aged from 25 to 70 years old; iii) patients with a life expectancy
of at least 6 months; iv) patients underwent a gastrectomy; v)
after gastrectomy, patients provided written informed consent to
participate in the study according to the Good Clinical Practice
criteria (29); and vi) a Karnofsky
Performance Status score of >60 (30). The exclusion criteria were as
follows: i) Patients with other cancer types; ii) pregnant or
lactating women; iii) patients who were unable to swallow TCM; iv)
patients with symptomatic brain metastasis or mental disorders; and
v) patients with severe cardiovascular disease, chronic liver
disease, kidney disease or blood disease.
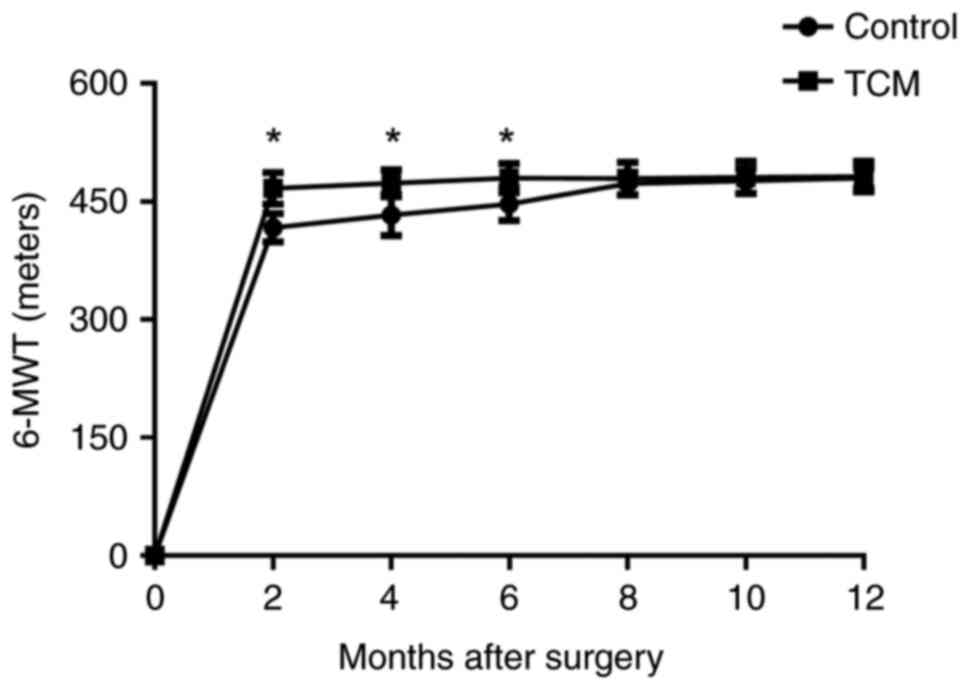
Physical capacity
To assess physical capacity, the 6-min walk test
(6-MWT) (31) was performed every 2
months in the patients of each group. The test was performed in a
50-meter corridor and all patients were instructed to walk as far
as possible in 6 min.
Postoperative pain and POCs
After gastrectomy, the postoperative pain scores of
the patients in the two groups were evaluated every 3 days during
the hospital stay (on days 0, 3, 6, 9, 12 and 15) using the 0–10
Numeric Rating Scale, with 0 representing no pain and 10
representing the worst imaginable pain (32). POCs in the patients with gastric
cancer after surgery were recorded and classified according to the
Clavien-Dindo (C-D) classification grade (33).
Postoperative inflammation
Blood samples were collected from each patient every
3 days (on days 0, 3, 6, 9, 12 and 15) to measure serum
inflammatory cytokine levels. Postoperative inflammation score was
determined by inflammation score, as described previously (34). Postoperative serum levels of
C-reactive protein (CRP) (cat. no. ab260058), IL-1β (cat. no.
ab214025), IL-6 (cat. no. ab178013), IL-8 (cat. no. ab214030),
IL-10 (cat. no. ab185986) and TNF-α (cat. no. ab181421) were
measured using ELISA kits (all Abcam) according to the
manufacturer's instructions. CD3+, CD4+,
CD8+, CD16+, CD19+ and
CD45+ expression levels in peripheral T lymphocytes were
analyzed using a FACS Canto II flow cytometer and FACS Diva
software (BD Biosciences).
Analysis of gastrointestinal function,
abdominal pain and abdominal distention
The clinical outcomes were standard measures of
gastrointestinal function and included the time from the operation
to the first passage of flatus, the time from the operation to the
passage of the first defecation, and the number of patients who
were comfortable with the intake of a semi-fluid diet as measured
every 3 days (on days 0, 3, 6, 9, 12 and 15 days) during the
hospitalization. The abdominal pain of each patient from the two
groups was evaluated using Prince Henry Pain Scale scoring
(35) (0, no pain when coughing; 1,
pain only when coughing; 2, no pain when quiet, but pain with deep
breathing; 3, mild and bearable pain when resting; 4, severe and
unbearable pain). Abdominal distension (36) was evaluated using the following
scale: 0, no sense of abdominal distension; 1, mild distension; 2,
moderate abdominal distention; and 3, severe abdominal
distention.
Postoperative metal status
Postoperative mental status was evaluated in
patients every 2 months post-surgery by clinicians for a total of
12 months. Quality of life after surgery was evaluated using the
36-Item Short Form Health Survey (SF-36) questionnaire (37). Scores in the SF-36 range from 0 to
100 (0 representing the worst and 100 the best). The Beck
Depression Inventory (38) was used
to assess the depression level in the patients after surgery. The
Beck Depression Inventory includes 21 clinical symptoms of
depression and the scores range from 5 to 63 (5–9, normal; 10–18,
mild-to-moderate depression; 19–29, moderate-to-severe depression;
30–63, severe depression). Anxiety in patients with gastric cancer
after surgery was determined by the State-Trait Anxiety Inventory
(STAI) (39). The STAI includes
separate measures of state- and trait-anxiety, which are scored as
a minimum of 20 to a maximum of 80 (20–29, without anxiety; 20–30,
the presence of anxiety; 31–49, an intermediate level of anxiety;
50–80, a high degree of anxiety).
Postoperative survival, recurrence and
follow-up
Patients were followed up every 3 months during the
60-month follow up period. The overall survival time of the
patients with gastric cancer after surgery was recorded from the
date of surgery to death or the last follow-up. Recurrence time was
defined as the time from surgery to recurrence or the last
follow-up.
Safety of TCM
The safety of the TCM used in this study was
assessed using National Cancer Institute Common Terminology
Criteria for Adverse Events, version 4.0 (40).
Statistical analysis
Data are expressed as the mean ± standard deviation
or n (%). Data were analyzed using SPSS version 21.0 (SPSS Inc.;
IBM Corp.). Unpaired Student's t-test was used to compare the data
between two groups. Qualitative data were calculated using the
χ2 test or Fisher's test. Overall survival and
recurrence were analyzed using Kaplan-Meier analysis. P<0.05 was
considered to indicate a statistically significant difference.
Results
Characteristic of patients with
gastric cancer
A total of 1,032 patients with gastric cancer who
underwent a gastrectomy were recruited to the present study.
Patients with a mean age of 57.5 years (range, 53.2–62.8 years)
were assigned into two groups: The TCM group (n=520) and the
control group (n=512). There were 560 male and 472 female patients
with gastric cancer. The surgical outcomes of the patients are
shown in Table I. All patients
received the same anesthetic drugs during the operation and
underwent a gastrectomy. There were no significant differences
between the two groups (all P>0.05). The study follow-up time
was 60 months.
Effects of TCM nursing intervention on
hospital stay, postoperative pain and frequency of postoperative
symptoms
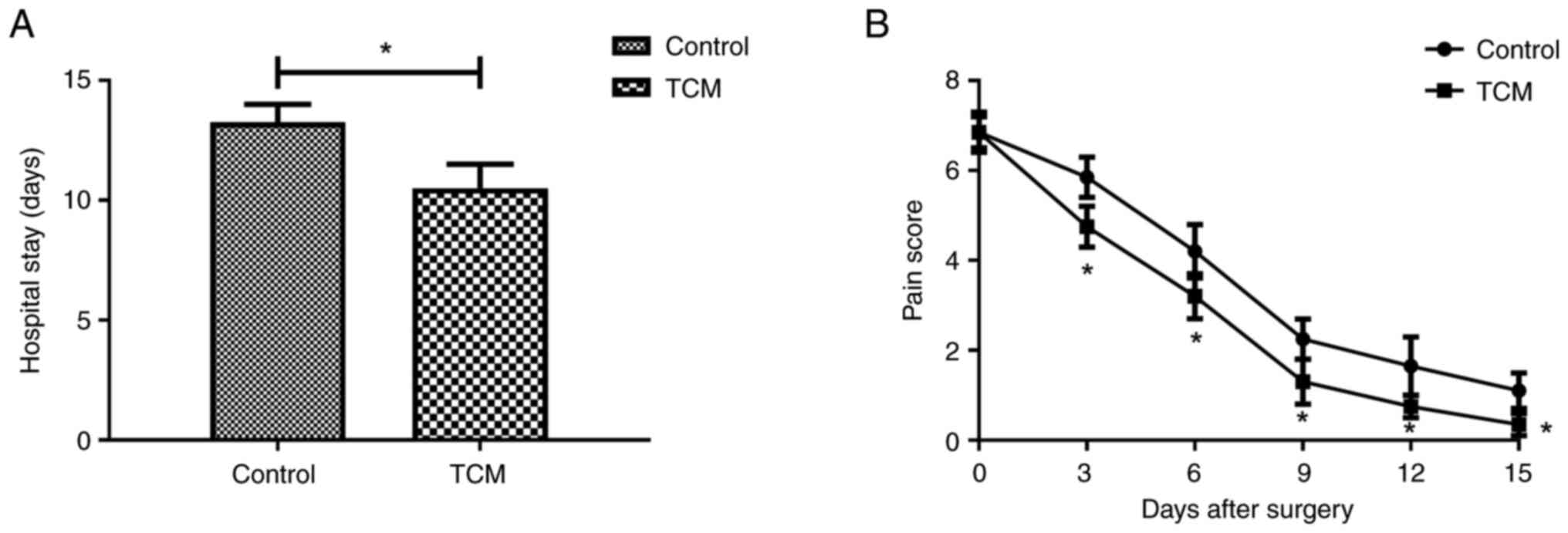
To verify the efficacy of TCM nursing intervention,
hospital stay, postoperative pain and frequency of postoperative
symptoms in patients were evaluated between the two groups.
Patients in the TCM nursing intervention group had a shorter
hospital stay and lower postoperative pain scores compared with
those in the control group (both P<0.05; Fig. 2). It was observed that TCM nursing
intervention decreased the use rate of opioids compared with the
control group (P<0.05; Table
II). Compared with the control, TCM nursing intervention
significantly decreased the frequency of postoperative dizziness,
vomiting, nausea, distention, diarrhea and comfort of intake of a
semi-fluid diet during the hospital stay (all P<0.05; Table II).
 | Table II.Effect of TCM nursing intervention on
hospital stay, postoperative pain and frequency of postoperative
symptoms. |
Table II.
Effect of TCM nursing intervention on
hospital stay, postoperative pain and frequency of postoperative
symptoms.
| Events | Control | TCM | P-value |
|---|
| Hospital stay,
days | 12.5±3.5 | 10.5±2.5 | 0.046a |
| Postoperative pain
score | 6.4±1.8 | 5.3±1.3 | 0.040a |
| Use rate of
opioids, % | 63.6±7.5 | 45.2±6.8 | 0.025a |
| Postoperative
symptoms, n (%) |
|
|
|
|
Dizziness | 42 (8.2) | 25 (4.8) | 0.032b |
|
Vomiting | 25 (4.9) | 16 (3.1) | 0.044b |
|
Nausea | 30 (5.9) | 18 (3.5) | 0.040b |
|
Distention | 36 (7.0) | 22 (4.2) | 0.018b |
|
Diarrhea | 41 (8.0) | 30 (5.8) | 0.032b |
| Comfort
of intake of a semi-fluid diet | 417 (81.4) | 476 (91.5) | 0.012b |
| C-D grade, n
(%) |
|
|
|
| I | 368 (71.9) | 403 (77.5) | 0.032b |
| II | 42 (8.2) | 67 (12.9) | 0.035b |
|
III | 25 (4.9) | 14 (2.7) | 0.041b |
| IV | 23 (4.5) | 12 (2.3) | 0.020b |
| V | 19 (3.7) | 9 (1.7) | 0.044b |
| VI | 15 (2.9) | 7 (1.3) | 0.041b |
|
VII | 10 (2.0) | 5 (1.0) | 0.028b |
|
VIII | 10 (2.0) | 3 (0.6) | 0.013b |
Effects of TCM nursing intervention on
postoperative gastrointestinal dysfunction
Postoperative gastrointestinal dysfunction can cause
the accumulation of secretions and gas, which will result in
postoperative symptoms of gastrointestinal discomfort after
gastrectomy (41). Thus, the
differences in postoperative gastrointestinal dysfunction were
compared between the two groups of patients with gastric cancer who
underwent gastrectomy (Table
III). The data revealed that TCM nursing intervention
significantly decreased the time to first postoperative flatus and
defecation, and the fasting time (all P<0.05). Postoperative
patients in the TCM group were more comfortable with the intake of
a semi-fluid diet than patients in the control group at 15 days
post-surgery. Compared with the control, TCM nursing intervention
significantly decreased the occurrence of abdominal pain and
abdominal distension in the patients after gastrectomy (all
P<0.05; Table III).
 | Table III.Effect of TCM nursing intervention on
postoperative gastrointestinal dysfunction in gastric cancer
patients after surgery. |
Table III.
Effect of TCM nursing intervention on
postoperative gastrointestinal dysfunction in gastric cancer
patients after surgery.
| Events | Control | TCM | P-value |
|---|
| Time to first
postoperative flatus, days | 3.2±0.8 | 1.5±0.4 | 0.033a |
| Time to first
postoperative defecation, days | 4.0±1.6 | 2.1±0.8 | 0.028a |
| Fasting time,
days | 3.6±1.0 | 1.4±0.6 | 0.022a |
| Comfortable with
semi-fluid diet, n (%) | 432 (84.4) | 481 (92.5) | 0.010b |
| Duration of
postoperative stay, days | 9.7±3.8 | 6.2±2.4 | 0.029a |
| Postoperative
abdominal pain grade, n (%) |
|
|
|
| 1 | 186 (36.3) | 205 (39.4) | 0.045b |
| 2 | 245 (47.9) | 285 (54.8) | 0.042b |
| 3 | 53 (10.4) | 18 (3.5) | 0.010b |
| 4 | 28 (5.5) | 12 (2.3) | 0.027b |
| Postoperative
abdominal distension grade, n (%) |
|
|
|
| 0 | 95 (18.6) | 162 (31.2) | 0.008b |
| 1 | 121 (23.6) | 146 (28.1) | 0.041b |
| 2 | 168 (32.8) | 124 (23.8) | 0.024b |
| 3 | 128 (25.0) | 88 (16.9) | 0.026b |
Effects of TCM nursing intervention on
postoperative inflammation index in gastric cancer patients
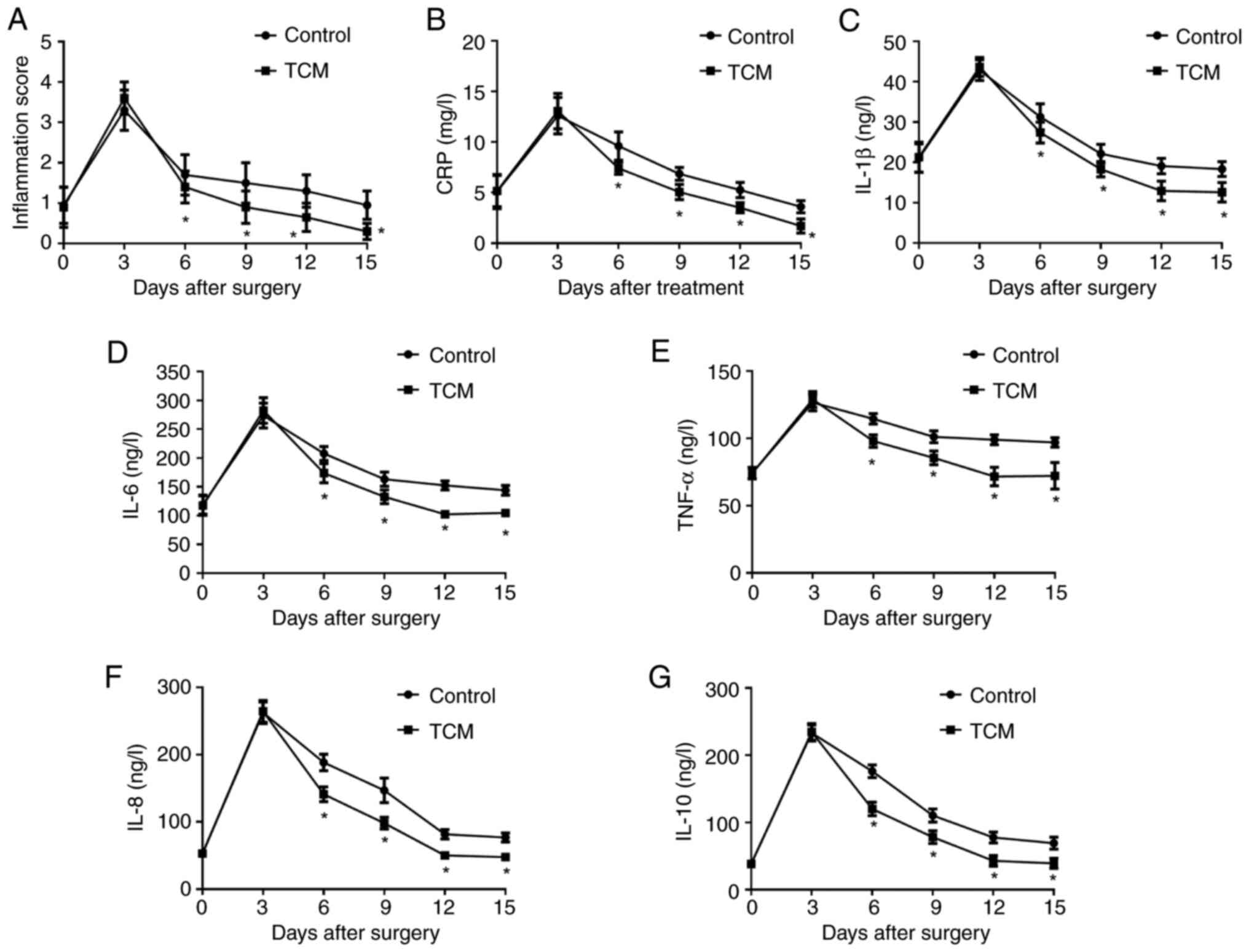
The effects of TCM nursing intervention on
postoperative inflammation index were analyzed in the patients with
gastric cancer who underwent gastrectomy. As shown in Fig. 3A, the patients in the TCM group
exhibited lower inflammation scores than those in the control group
at 6 days post-surgery. TCM nursing intervention also decreased the
inflammatory cytokines levels of CRP, IL-1β, IL-6, TNF-α, IL-8 and
IL-10 after gastrectomy compared with the control group during the
hospital stay (Fig. 3B-G).
Effects of TCM nursing intervention on
POCs in patients with gastric cancer who underwent gastrectomy
POCs in each patient with gastric cancer were
recorded, classified according to the C-D classification grade and
compared between the two groups. The characteristics of the
patients in each C-D grade in the propensity score-matched cohorts
are shown in Table IV. Grade I
complications were present in 403 (77.5%) and 368 (71.9%) patients
in the TCM and control groups, respectively. Grade II complications
were recorded in 67 (13.1%) and 42 (8.1%) patients in the TCM and
control groups, respectively. It was also demonstrated that 14
(2.7%) and 25 (4.9%) patients experienced grade III complications
in the TCM and control groups, respectively, while patients with
grade IV–VIII complications accounted for 36 (6.9%) and 77 (15.0%)
patients at 12 months after surgery in the TCM and control groups,
respectively.
 | Table IV.Effect of TCM nursing intervention on
postoperative complications in patients with gastric cancer who
underwent surgery. |
Table IV.
Effect of TCM nursing intervention on
postoperative complications in patients with gastric cancer who
underwent surgery.
| Clavien-Dindo
grade | Control, n (%) | TCM, n (%) | P-value |
|---|
| I | 368 (71.9) | 403 (77.5) | 0.031 |
| II | 42 (8.2) | 67 (12.9) | 0.036 |
| III | 25 (4.9) | 14 (2.7) | 0.041 |
| IV | 23 (4.5) | 12 (2.3) | 0.020 |
| V | 19 (3.7) | 9 (1.7) | 0.044 |
| VI | 15 (2.9) | 7 (1.3) | 0.040 |
| VII | 10 (2.0) | 5 (1.0) | 0.030 |
| VIII | 10 (2.0) | 3 (0.6) | 0.015 |
Effect of TCM nursing intervention on
physical capacity and metal status
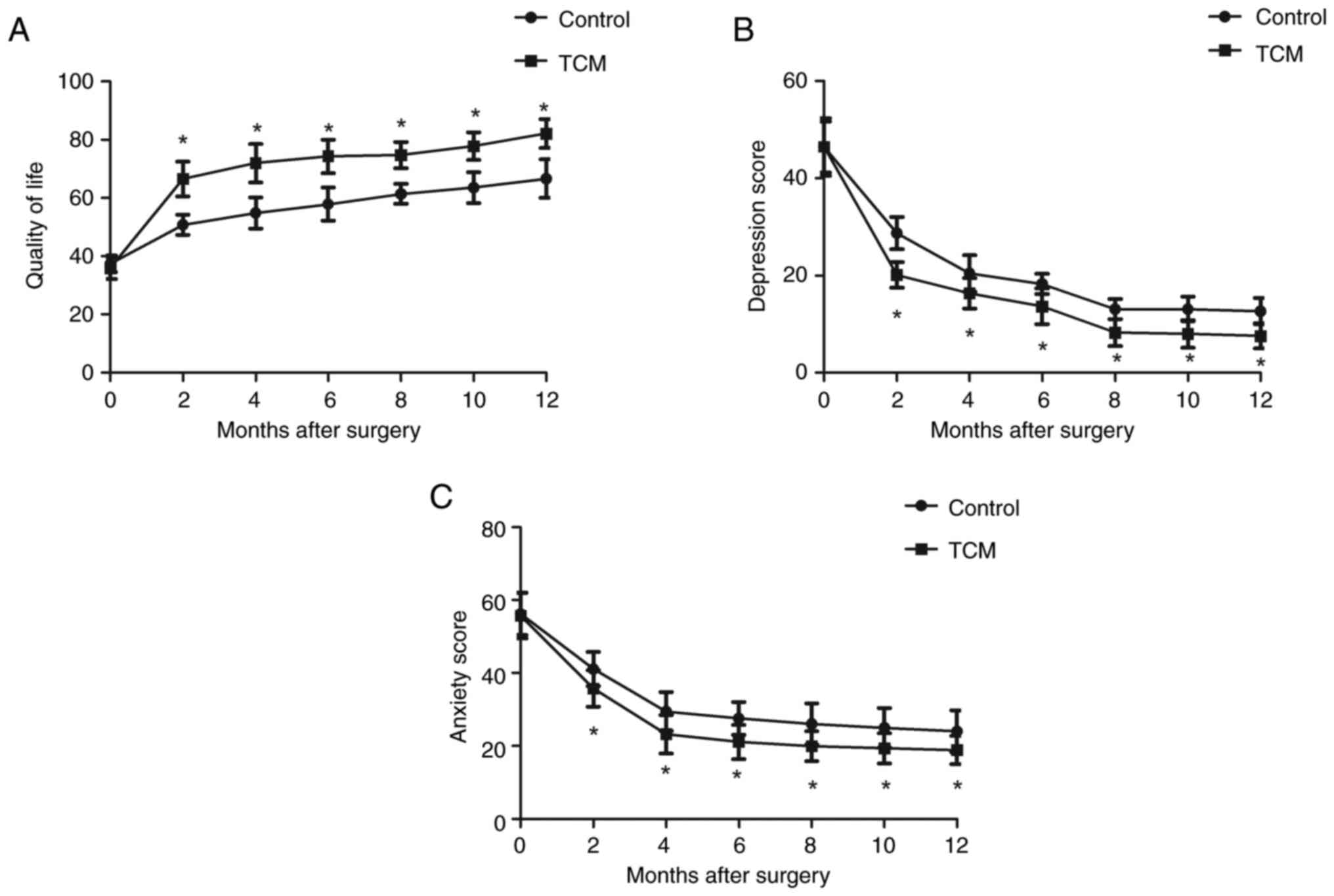
Physical capacity and metal status were evaluated at
the time of hospitalization and discharge for the two groups of
patients with gastric cancer who underwent gastrectomy. The results
data showed that TCM nursing intervention significantly improved
clinician-rated measures of depression and anxiety during
hospitalization compared with the control (all P<0.05). The
quality of life of the patients after gastrectomy also increased in
the TCM nursing intervention group when compared with that of the
control group (all P<0.05). After 12-month discharge, the
patients in the TCM group experienced less depression and anxiety,
and a higher quality of life than those in the control group (all
P<0.05) (Fig. 4). TCM nursing
intervention also improved the postoperative physical capacity, as
determined by 6-MWT (Table V). TCM
nursing intervention increased the physical capacity of gastric
cancer patients at 2, 4 and 6 months compared with the control
(Fig. 5). After 6 months of
follow-up, no significant difference in postoperative physical
capacity was observed between the two groups.
 | Table V.Effect of TCM nursing intervention on
postoperative physical capacity in patients with gastric cancer who
underwent surgery. |
Table V.
Effect of TCM nursing intervention on
postoperative physical capacity in patients with gastric cancer who
underwent surgery.
| Day | Control group | TCM group | P-value |
|---|
| 3 | 252.2±86.4 | 276.0±93.5 | 0.041 |
| 6 | 275.1±59.7 | 302.4±68.4 | 0.038 |
| 9 | 328.4±64.2 | 395.8±60.0 | 0.034 |
| 12 | 388.0±69.4 | 442.2±57.2 | 0.024 |
| 15 | 401.2±77.5 | 486.5±63.0 | 0.016 |
Effects of TCM nursing intervention on
postoperative immune activity
It is now known that altered immune cell expression
may be responsible for the low survival and poor prognosis in
patients with gastric cancer after surgery (42). Thus, the immune function in patients
with gastric cancer who underwent gastrectomy was compared between
the two treatment groups in the present study. As shown in Table VI, CD3+,
CD4+, CD8+, CD16+,
CD19+ and CD45+ expression levels were
recorded in peripheral T lymphocytes, and were higher in patients
in the TCM group compared with those in the control group (all
P<0.05). Compared with that in the control group, a significant
increase in the concentration of natural killer cells and T cells
was observed in patients in the TCM group (both P<0.05)
(Table VI).
 | Table VI.Effect of TCM nursing intervention on
survival and recurrence in patients with gastric cancer who
underwent surgery. |
Table VI.
Effect of TCM nursing intervention on
survival and recurrence in patients with gastric cancer who
underwent surgery.
| Immune cells | Control | TCM | P-value |
|---|
|
CD3+ | 35.68±10.10 | 50.35±12.62 | 0.024 |
|
CD4+ | 24.12±8.63 | 40.24±14.46 | 0.031 |
|
CD8+ | 14.88±6.74 | 24.60±9.80 | 0.015 |
|
CD16+ | 18.41±7.65 | 25.55±10.22 | 0.039 |
|
CD19+ | 16.25±6.02 | 24.32±9.40 | 0.041 |
|
CD45+ | 20.07±6.89 | 27.06±9.44 | 0.018 |
| NK cells | 8.58±4.16 | 12.66±6.07 | 0.044 |
| T cells | 6.66±3.45 | 11.04±6.88 | 0.030 |
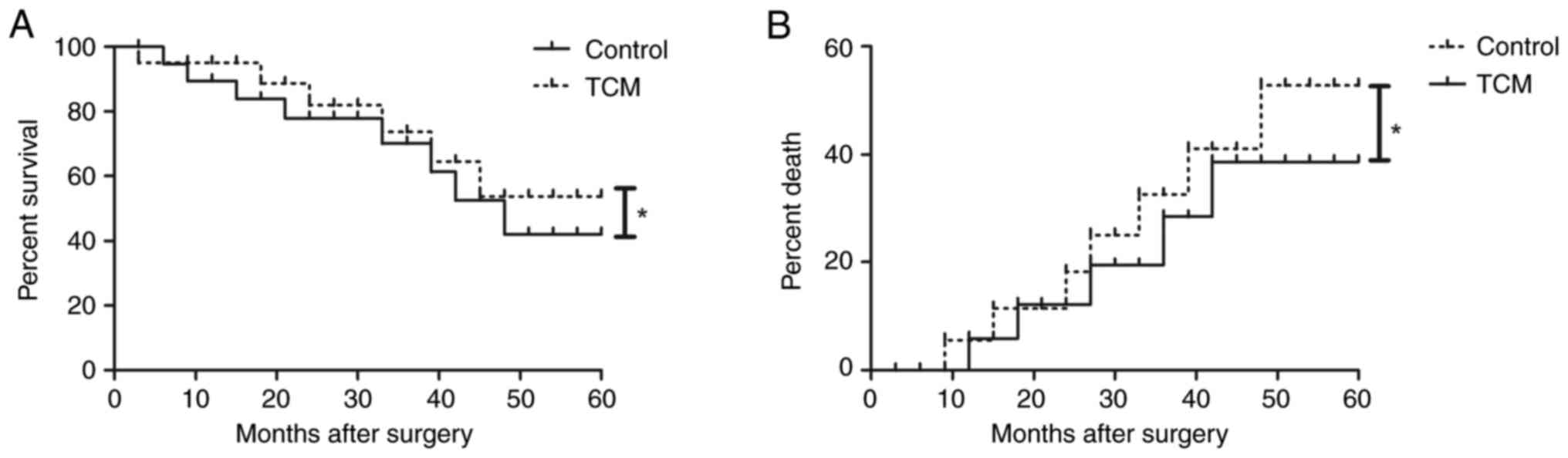
Effects of TCM nursing intervention on
survival and recurrence
The survival and recurrence times in the patients
with gastric cancer were recorded and compared between the two
groups. The data revealed that TCM nursing intervention prolonged
the survival after gastrectomy compared with the control during the
60-month follow-up period (Fig.
6A). Furthermore, the mortality rate of gastric cancer was also
decreased in the patients in the TCM nursing intervention group
(Fig. 6B). During the 5-year
follow-up period, 65 (12.7%) patients in the control group died and
142 (27.7%) patients experienced recurrence or tumor metastasis,
while only 30 (5.8%) patients died in the TCM nursing intervention
group, and 88 (16.9%) patients experienced recurrence or tumor
metastasis (Table VII).
 | Table VII.Effect of TCM nursing intervention on
survival and recurrence in patients with gastric cancer who
underwent surgery. |
Table VII.
Effect of TCM nursing intervention on
survival and recurrence in patients with gastric cancer who
underwent surgery.
| Parameter | Control group, n
(%) | TCM group, n
(%) | P-value |
|---|
| Death | 65 (12.7) | 30 (5.8) | 0.022 |
| Recurrence | 142 (27.7) | 88 (16.9) | 0.011 |
Cancer treatment-related adverse
events of TCM nursing intervention in patients with gastric cancer
who underwent gastrectomy
The treatment-related adverse events were recorded
after gastrectomy in the TCM nursing intervention group. Most of
the TCM treatment-related adverse events were grade 1 or 2
according to National Cancer Institute Common Terminology Criteria
(Table VIII). The cancer
treatment-related adverse events of TCM included vomiting,
pruritus, gastrointestinal reaction, increased alanine transaminase
(ALT)/aspartate transaminase (AST) levels, fatigue, hypertension
and diarrhea. No toxin-induced death was observed in any patient in
the TCM nursing intervention group. Of the 55 patients affected, 20
(3.8%) had grade 3 diarrhea, 12 (2.3%) had grade 3 hypertension and
33 (6.3%) had a gastrointestinal reaction, and these patients were
forced to reduce the dose of TCM.
 | Table VIII.Cancer treatment-related adverse
events of traditional Chinese medicine nursing intervention in
patients with gastric cancer who underwent surgery. |
Table VIII.
Cancer treatment-related adverse
events of traditional Chinese medicine nursing intervention in
patients with gastric cancer who underwent surgery.
| Treatment-related
adverse events | Patients, n
(%) |
|---|
| Vomiting | 34 (6.5) |
| Pruritus | 48 (9.2) |
| Gastrointestinal
reaction | 33 (6.3) |
| ALT/AST
increased | 42 (8.1) |
| Fatigue | 28 (5.4) |
| Hypertension
grade |
|
| 1 | 24 (4.6) |
| 2 | 20 (3.8) |
| 3 | 12 (2.3) |
| Diarrhea grade |
|
| 1 | 32 (6.2) |
| 2 | 30 (5.8) |
| 3 | 20 (3.8) |
Discussion
In general, gastric cancer is the malignant tumor of
the digestive tract with the highest incidence, prevalence and
mortality rates (43). An
increasing number of young individuals are being affected by the
condition due to changes in lifestyle and dietary structure in
China (44). Despite the treatment
strategies that have been applied in patients with gastric cancer,
the overall survival rate and prognosis are still poor (45). Clinically, TCM has been proven
effective in treating gastric cancer, acting as a comprehensive
interventional method that has multiple approaches and targets
(14). In addition, TCM nursing
intervention can markedly decrease POCs, improve the quality of
sleep, relieve postoperative pain, and improve the mental status
and quality of life of patients who have received gastric cancer
surgery (46). The present study
investigated the effects of TCM nursing intervention on POCs,
survival and recurrence rate in patients with gastric cancer who
underwent gastrectomy. Outcomes showed that TCM nursing
intervention significantly improved depression and anxiety,
suggesting that postoperative mental state in individuals with
gastric cancer may be improved by TMC nursing intervention, with a
basis of routine nursing. Results in the current study also pointed
out that TCM nursing intervention was extremely effective in
decreasing POCs, inflammation and numbers of deaths, and improving
the postoperative gastrointestinal dysfunction, physical capacity,
quality of life and survival of patients with gastric cancer after
gastrectomy.
Most gastric cancer patients need to undergo a
gastrectomy, and postoperatively, patients frequently experience
gastrointestinal dysfunction, POCs, inflammation and a decreased
quality of life (47). A number of
studies have indicated that parameters based solely on preoperative
factors are able to identify the patients who are at the greatest
risk of a POC. Appropriate postoperative care can then contribute
to the improvement of the POC and gastrointestinal dysfunction
(48,49). TCM formulae and chemical components
isolated from some Chinese herbal medicines have been used to treat
gastric cancer, and TCM has been proven effective in treating
gastric cancer patients by inhibiting tumor growth (16). In the current study, it was observed
that TCM nursing intervention shortened the time until first
postoperative flatus, the regression time for epigastric distension
symptoms, the time until first defecation and the recovery time
until comfortable with semi-solid food for patients with gastric
cancer, suggesting that the addition of TCM nursing intervention
could improve the gastrointestinal dysfunction after gastrectomy
compared with routine nursing. In addition, in another study,
perioperative TCM nursing for patients with gastric cancer
alleviated acute inflammation and improved the quality of life of
103 patients with gastric cancer (18). Consistent with this, the results in
the present study demonstrated that TCM nursing intervention not
only improved the quality of life and inflammation index, but also
helped the mental status and postoperative physical capacity in the
1,032 patients with gastric cancer who underwent a gastrectomy.
Different to other studies, TCM nursing intervention could
effectively improve postoperative pain and the frequency of
postoperative symptoms. Furthermore, another previous study found
that enhanced recovery after gastrectomy could decrease
inflammation perioperatively, improve nutrition postoperatively and
decrease hospitalization time in patients with gastric carcinoma
(50). In the present study,
perioperative inflammation and inflammatory cytokines levels of
CRP, IL-1β, IL-6, TNF-α, IL-8 and IL-10 in the patients with
gastric cancer were significantly lower in the patients in the TCM
group compared with those in the patients in the control group
during hospitalization.
TCM combined with chemotherapy may extend the
overall survival time and increase the survival rate and quality of
life of patients with stage IV non-surgical gastric cancer
(51). In addition, TCM plays an
important role in decreasing inflammation and prolonging survival
time in subjects with gastric cancer (52). TCM also has an important potential
value for improving the prognosis of patients with advanced gastric
cancer (53). The present study
evaluated the efficacy of TCM nursing intervention for improving
the postoperative POCs of patients after gastrectomy, and also
investigated its effect on postoperative survival and prognosis. In
a study on oral cancer, the clinical efficacy of TCM anticancer
decoctions plus basic chemotherapy and nursing interventions as
postoperative treatment was notable, with significant improvements
in patient immunity and decreased tumor marker levels (54). Consistent with this, the results of
the present study showed that immune activity, quality of life and
the 5-year cumulative survival rate of patients in the TCM nursing
intervention group were significantly higher than those in the
control group. In addition, the recurrence rate for patients in the
TCM nursing intervention group was significantly lower than that in
the control group. Most patients with gastric cancer who undergo
surgery develop recurrence and metastasis (55). In China, almost all patients want to
choose aggressive treatment (56),
and the present results identified that TCM nursing intervention
was effective when compared with the control. Notably, the results
showed that a limited number of patients in the TCM nursing
intervention group experienced a low number of cancer
treatment-related adverse events, such as vomiting, pruritus,
gastrointestinal reaction, increased ALT/AST levels, fatigue,
hypertension and diarrhea. However, the long-term efficacy of TCM
on immune activity, quality of life and 5-year cumulative survival
rate in patients with gastric cancer were not analyzed in this
study.
In conclusion, TCM nursing intervention has an
important value for improving the postoperative gastrointestinal
dysfunction, metal status, POCs, inflammation, immune activity,
survival, and prognosis of patients with gastric cancer who undergo
gastrectomy. In addition, TCM nursing intervention could be
effective, safe and well tolerated for patients with gastric cancer
who undergo gastrectomy, which suggests its potential clinical
application and deserves further research.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LF and YH conceived and designed the study. YL, XL
and DL performed data analysis. RW analyzed the data, and wrote and
revised the manuscript. All authors have read and approved the
manuscript. LF and RW confirm the authenticity of all the raw
data.
Ethics approval and consent to
participate
This study was approved by the Ethics Review
Committee of The First Hospital of Harbin (Harbin, China; approval
no. 20150507TFHX1). Written informed consent was obtained from all
subjects.
Patient consent for publication
Written informed consent was obtained from all
patients, and all patients agreed to publication of their data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Prabhu A, Mishra D, Brandl A and Yonemura
Y: Gastric cancer with peritoneal metastasis-A comprehensive review
of current intraperitoneal treatment modalities. Front Oncol.
12:8646472022. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Aoyama T, Yoshikawa T, Ida S, Cho H,
Sakamaki K, Ito Y, Fujitani K, Takiguchi N, Kawashima Y, Nishikawa
K, et al: Effects of perioperative eicosapentaenoic acid-enriched
oral nutritional supplement on the long-term oncological outcomes
after total gastrectomy for gastric cancer. Oncol Lett. 23:1512022.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhang B, Zhao ZQ and Zhang W: A nomogram
to predict the survival of gastric cancer patients who underwent
radical gastrectomy in west China. Asian J Surg. 45:2928–2929.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pang HY, Zhao LY, Wang H, Chen XL, Liu K,
Zhang WH, Yang K, Chen XZ and Hu JK: Impact of type of
postoperative complications on long-term survival of gastric cancer
patients: Results From A High-Volume Institution in China. Front
Oncol. 11:5873092021. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yoon HH: Ramucirumab plus paclitaxel for
gastric cancer in China. Lancet Gastroenterol Hepatol. 6:975–976.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kimura A, Morinaga N, Wada W, Ogata K,
Okuyama T, Kato H, Sohda M, Shirabe K and Saeki H: Patient with
gastric cancer who underwent distal gastrectomy after treatment of
COVID-19 infection diagnosed by preoperative PCR screening. Surg
Case Rep. 8:122022. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chen YY, Feng Y, Mao QS, Ma P, Liu JZ, Lu
W, Liu YF, Chen X, Hu YL and Xue WJ: Diagnostic and prognostic
value of the peripheral natural killer cell levels in gastric
cancer. Exp Ther Med. 20:3816–3822. 2020.PubMed/NCBI
|
|
8
|
Bacalbasa N, Diaconu C, Socea B,
Gherghiceanu F, Savu C, Dimitriu M, Balescu I and Cordos I:
Neoadjuvant intraperitoneal chemotherapy for advanced stage gastric
cancer (review). Exp Ther Med. 22:13142021. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Merboth F, Garcia S, V Renesse J, Distler
M, Welsch T, Weitz J and Stange DE: Comparative analysis of
postoperative complications after cytoreductive surgery and HIPEC
in gastric cancer. Oncol Res Treat. 45:45–53. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li R, Leng AM, Liu T, Zhou YW, Zeng JX,
Liu XM, Hu TZ, Jiang XX, Zhang LF and Xu CX: Weekday of surgery
affects postoperative complications and long-term survival of
Chinese gastric cancer patients after curative gastrectomy. Biomed
Res Int. 2017:50905342017.PubMed/NCBI
|
|
11
|
Xie D, Shen J, Liu L, Cao B, Wang Y, Qin
J, Wu J, Yan Q, Hu Y, Yang C, et al: Complete mesogastric excision
for locally advanced gastric cancer: Short-term outcomes of a
randomized clinical trial. Cell Rep Med. 2:1002172021. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang K, Chen Q, Shao Y, Yin S, Liu C, Liu
Y, Wang R, Wang T, Qiu Y and Yu H: Anticancer activities of TCM and
their active components against tumor metastasis. Biomed
Pharmacother. 133:1110442021. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Liu Q, Qi B, Zhang L, Zhang M and Xiao L:
Effect of continuous nursing intervention on psychological state
and medication compliance of patients with acute myocardial
infarction after PCI. Panminerva Med. Sep 18–2020.(Epub ahead of
print). View Article : Google Scholar
|
|
14
|
Xu W, Li B, Xu M, Yang T and Hao X:
Traditional Chinese medicine for precancerous lesions of gastric
cancer: A review. Biomed Pharmacother. 146:1125422022. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gu Z, Ling J, Cong J and Li D: A review of
therapeutic effects and the pharmacological molecular mechanisms of
Chinese medicine weifuchun in treating precancerous gastric
conditions. Integr Cancer Ther. 19:15347354209532152020. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Li Z, Zhang G, Cao N, Xu J, Dong J, Li J,
Zhu X, Xu Y, Han C, Wang R, et al: Effects of traditional Chinese
medicine collaborative model (TCMCM) combined with adjuvant
chemotherapy on IIIb and IIIc gastric cancer: A protocol for a
randomized controlled trial. Trials. 23:682022. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wu J, Wang J, Su Q, Ding W, Li T, Yu J and
Cao B: Traditional Chinese medicine Astragalus polysaccharide
enhanced antitumor effects of the angiogenesis inhibitor apatinib
in pancreatic cancer cells on proliferation, invasiveness, and
apoptosis. Onco Targets Ther. 11:2685–2698. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhang Y, Wang X and Yang H: Effect of
traditional Chinese medicine nursing on postoperative patients with
gastric cancer and its impact on quality of life. Am J Transl Res.
13:5589–5595. 2021.PubMed/NCBI
|
|
19
|
Wang Y, Zhang Q, Chen Y, Liang CL, Liu H,
Qiu F and Dai Z: Antitumor effects of immunity-enhancing
traditional Chinese medicine. Biomed Pharmacother. 121:1095702020.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wang M, Wang S, Su Q and Ma T: Effect of
combining early chemotherapy with zhipu liujunzi decoction under
the concept of strengthening and consolidating body resistance for
gastric cancer patients and nursing strategy. Contrast Media Mol
Imaging. 2021:21359242021. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Khan M and Shamim S: Anisi stellati
fructus, a significant traditional Chinese medicine (TCM) herb and
its bioactivity against gastric cancer. Evid Based Complement
Alternat Med. 2022:40714892022. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Cheng M, Hu J, Zhao Y, Jiang J, Qi R, Chen
S, Li Y, Zheng H, Liu R, Guo Q, et al: Efficacy and safety of
astragalus-containing traditional Chinese medicine combined with
platinum-based chemotherapy in advanced gastric cancer: A
systematic review and meta-analysis. Front Oncol. 11:6321682021.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
He XL and Cao ZM: Effect of high-quality
nursing intervention on the psychological disorder in patients with
gastric cancer during perioperative period: A protocol of
systematic review and meta-analysis. Medicine (Baltimore).
99:e203812020. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Shih WT, Yang PR, Shen YC, Yang YH and Wu
CY: Traditional Chinese medicine enhances survival in patients with
gastric cancer after surgery and adjuvant chemotherapy in Taiwan: A
nationwide matched cohort study. Evid Based Complement Alternat
Med. 2021:75846312021. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hou C, Chu HJ, Dai XJ, Wu YQ, He ZF, Yu
YW, Lu QY, Liu YQ and Zhang XC: Metabolomic study on the
therapeutic effect of the Jianpi Yangzheng Xiaozheng decoction on
gastric cancer treated with chemotherapy based on GC-TOFMS
analysis. Evid Based Complement Alternat Med. 2021:88329962021.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wu J, Zhang XX, Zou X, Wang M, Wang HX,
Wang YH, Li CY, Zhao LG, Chen M, Pei LX, et al: The effect of
Jianpi Yangzheng Xiaozheng decoction and its components on gastric
cancer. J Ethnopharmacol. 235:56–64. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Adeyemi OJ, Meltzer-Bruhn A, Esper G,
DiMaggio C, Grudzen C, Chodosh J and Konda S: Crosswalk between
charlson comorbidity index and the American society of
anesthesiologists physical status score for geriatric trauma
assessment. Healthcare (Basel). 11:11372023. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lim CY and In J: Randomization in clinical
studies. Korean J Anesthesiol. 72:221–232. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Camilleri ET, Gustafson MP, Dudakovic A,
Riester SM, Garces CG, Paradise CR, Takai H, Karperien M, Cool S,
Sampen HJ, et al: Identification and validation of multiple cell
surface markers of clinical-grade adipose-derived mesenchymal
stromal cells as novel release criteria for good manufacturing
practice-compliant production. Stem Cell Res Ther. 7:1072016.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Milad S, Ehsan J, Seyed Farzad M, Mohsen
R, Ahmad B, Shahram M, Niayesh M and Alireza K: Effects of dimethyl
fumarate on the karnofsky performance status and serum S100β level
in newly glioblastoma patients: A randomized, phase-II, placebo,
triple blinded, controlled trial: Effect of DMF on the serum S100β
level and KPS score of GBM patients. Galen Med J. 10:1–10.
2022.PubMed/NCBI
|
|
31
|
Fell B, Hanekom S and Heine M: A modified
six-minute walk test (6MWT) for low-resource settings-a
cross-sectional study. Heart Lung. 52:117–122. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Farrar JT, Polomano RC, Berlin JA and
Strom BL: A comparison of change in the 0–10 numeric rating scale
to a pain relief scale and global medication performance scale in a
short-term clinical trial of breakthrough pain intensity.
Anesthesiology. 112:1464–1472. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Katayama H, Kurokawa Y, Nakamura K, Ito H,
Kanemitsu Y, Masuda N, Tsubosa Y, Satoh T, Yokomizo A, Fukuda H and
Sasako M: Extended Clavien-Dindo classification of surgical
complications: Japan clinical oncology group postoperative
complications criteria. Surg Today. 46:668–685. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Shoka M, Kanda M, Ito S, Mochizuki Y,
Teramoto H, Ishigure K, Murai T, Asada T, Ishiyama A, Matsushita H,
et al: Systemic inflammation score as a predictor of pneumonia
after radical resection of gastric cancer: Analysis of a
multi-institutional dataset. Dig Surg. 37:401–410. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Zubrzycki M, Liebold A, Skrabal C, Reinelt
H, Ziegler M, Perdas E and Zubrzycka M: Assessment and
pathophysiology of pain in cardiac surgery. J Pain Res.
11:1599–1611. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Cutrone M and Van Gysel D: Transient
abdominal telangiectasia of the newborn: Four new cases with
abdominal distension. Pediatr Dermatol. May 31–2023.(Epub ahead of
print). View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Suzuki M, Ishikawa T, Sakuma A, Abe S, Abe
H, Koyama F, Nakano T, Ueki A, Noguchi H, Hasegawa E, et al:
Evaluation of the health-related quality of life using the 36-item
short form health survey in patients with chronic hepatitis C
receiving pegylated interferon/ribavirin/telaprevir triple
treatment. Exp Ther Med. 12:3353–3358. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Kim HJ, Jeon YJ, Kim HC, Jin IH and Jung
SJ: Application of a joint latent space item response model to
clustering stressful life events and the beck depression
inventory-II: results from Korean epidemiological survey data.
Epidemiol Health. 44:e20220932022. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Gustafson LW, Gabel P, Hammer A, Lauridsen
HH, Petersen LK, Andersen B, Bor P and Larsen MB: Validity and
reliability of state-trait anxiety inventory in Danish women aged
45 years and older with abnormal cervical screening results. BMC
Med Res Methodol. 20:892020. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Cirillo M, Venturini M, Ciccarelli L,
Coati F, Bortolami O and Verlato G: Clinician versus nurse symptom
reporting using the national cancer institute-common terminology
criteria for adverse events during chemotherapy: Results of a
comparison based on patient's self-reported questionnaire. Ann
Oncol. 20:1929–1935. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Hosaka M, Arai I, Ishiura Y, Ito T, Seki
Y, Naito T, Masuzawa Y, Nakayama T and Motoo Y: Efficacy of
daikenchuto, a traditional Japanese Kampo medicine, for
postoperative intestinal dysfunction in patients with
gastrointestinal cancers: Meta-analysis. Int J Clin Oncol.
24:1385–1396. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Zhaojun X, Xiaobin C, Juan A, Jiaqi Y,
Shuyun J, Tao L, Baojia C, Cheng W and Xiaoming M: Correlation
analysis between preoperative systemic immune inflammation index
and prognosis of patients after radical gastric cancer surgery:
Based on propensity score matching method. World J Surg Oncol.
20:12022. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Xia JY and Aadam AA: Advances in screening
and detection of gastric cancer. J Surg Oncol. 125:1104–1109. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Lu Y, Xiao F, Wang Y, Wang Z, Liu D and
Hong F: Prevalence of Helicobacter pylori in non-cardia gastric
cancer in China: A systematic review and meta-analysis. Front
Oncol. 12:8503892022. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Kaslow SR, Ma Z, Hani L, Prendergast K,
Vitiello G, Lee AY, Berman RS, Goldberg JD and Correa-Gallego C:
Adherence to guidelines at the patient- and hospital-levels is
associated with improved overall survival in patients with gastric
cancer. J Surg Oncol. 126:479–489. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Hu J, Wang LL and Li Y: Effects of
high-quality nursing intervention on negative emotions,
postoperative complications and gastrointestinal function in
patients with gastric cancer surgery. Am J Transl Res.
14:1652–1662. 2022.PubMed/NCBI
|
|
47
|
Wang G and Jiang X: Effect of
PRECEDE-PROCEED-model-based health education on the life quality
and 5-HTT gene expression of patients with gastric cancer after
surgery. Cell Mol Biol (Noisy-le-grand). 67:242–248. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Lee JY, Jang Y, Kim S and Hyung WJ:
Uncertainty and unmet care needs before and after surgery in
patients with gastric cancer: A survey study. Nurs Health Sci.
22:427–435. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Kanda M: Preoperative predictors of
postoperative complications after gastric cancer resection. Surg
Today. 50:3–11. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Wang WK, Tu CY, Shao CX, Chen W, Zhou QY,
Zhu JD and Xu HT: Impact of enhanced recovery after surgery on
postoperative rehabilitation, inflammation, and immunity in gastric
carcinoma patients: A randomized clinical trial. Braz J Med Biol
Res. 52:e82652019. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Liu X, Xiu LJ, Jiao JP, Zhao J, Zhao Y, Lu
Y, Shi J, Li YJ, Ye M, Gu YF, et al: Traditional Chinese medicine
integrated with chemotherapy for stage IV non-surgical gastric
cancer: A retrospective clinical analysis. J Integr Med.
15:469–475. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Pan X, Tao H, Nie M, Liu Y, Huang P, Liu
S, Sun W, Wu J, Ma T, Dai A, et al: A clinical study of traditional
Chinese medicine prolonging the survival of advanced gastric cancer
patients by regulating the immunosuppressive cell population: A
study protocol for a multicenter, randomized controlled trail.
Medicine (Baltimore). 99:e197572020. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Xu Y, Zhao AG, Li ZY, Zhao G, Cai Y, Zhu
XH, Cao ND, Yang JK, Zheng J, Gu Y, et al: Survival benefit of
traditional Chinese herbal medicine (a herbal formula for
invigorating spleen) for patients with advanced gastric cancer.
Integr Cancer Ther. 12:414–422. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Jiang D, Xiao F, Liu L, Meng Z and Zhang
C: Effects of traditional Chinese medicine anticancer decoction
combined with basic chemotherapy and nursing intervention on oral
cancer patients after surgery and its effect on tumor markers and
immune function. Biomed Res Int. 2022:63413812022. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Jiao J, Li H, Shang L, Ren H, Ye C, Zhang
R, Xiao K, Dong K, Liu J and Li L: Impact of preceding noncurative
endoscopic submucosal dissection on patients with early gastric
cancer who undergo subsequent surgery: A meta-analysis. Expert Rev
Gastroenterol Hepatol. 16:373–382. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Qing XU, Yang W, Zhongyu LI, Jiaxing Y,
Yingpan Z, Ping W and Yandong W: Therapeutic mechanisms of
integrated traditional Chinese and conventional medicine underlying
its treatment of precancerous lesions of gastric cancer. J Tradit
Chin Med. 42:1023–1028. 2022.PubMed/NCBI
|