|
1
|
Davar D, Dzutsev AK, McCulloch JA,
Rodrigues RR, Chauvin JM, Morrison RM, Deblasio RN, Menna C, Ding
Q, Pagliano O, et al: Fecal microbiota transplant overcomes
resistance to anti-PD-1 therapy in melanoma patients. Science.
371:595–602. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Dzutsev A, Badger JH, Perez-Chanona E, Roy
S, Salcedo R, Smith CK and Trinchieri G: Microbes and cancer. Annu
Rev Immunol. 35:199–228. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Finlay BB, Goldszmid R, Honda K,
Trinchieri G, Wargo J and Zitvogel L: Can we harness the microbiota
to enhance the efficacy of cancer immunotherapy? Nat Rev Immunol.
20:522–528. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Garrett WS: The gut microbiota and colon
cancer. Science. 364:1133–1135. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Grivennikov SI, Greten FR and Karin M:
Immunity, inflammation, and cancer. Cell. 140:883–899. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Iida N, Dzutsev A, Stewart CA, Smith L,
Bouladoux N, Weingarten RA, Molina DA, Salcedo R, Back T, Cramer S,
et al: Commensal bacteria control cancer response to therapy by
modulating the tumor microenvironment. Science. 342:967–970. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Routy B, Le Chatelier E, Derosa L, Duong
CPM, Alou MT, Daillère R, Fluckiger A, Messaoudene M, Rauber C,
Roberti MP, et al: Gut microbiome influences efficacy of PD-1-based
immunotherapy against epithelial tumors. Science. 359:91–97. 2018.
View Article : Google Scholar : PubMed/NCBI
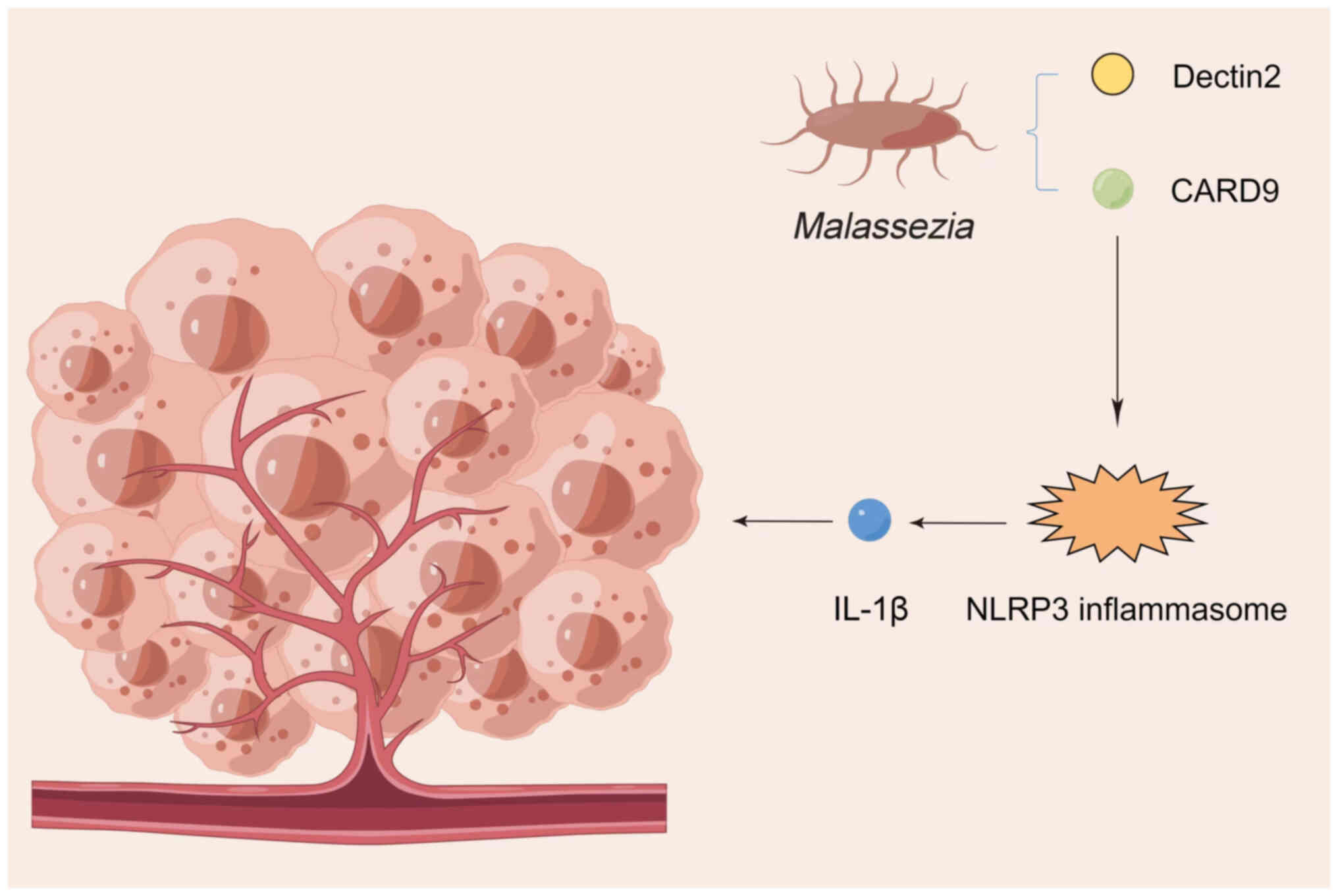
|
|
8
|
Sharma P, Hu-Lieskovan S, Wargo JA and
Ribas A: Primary, adaptive, and acquired resistance to cancer
immunotherapy. Cell. 168:707–723. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
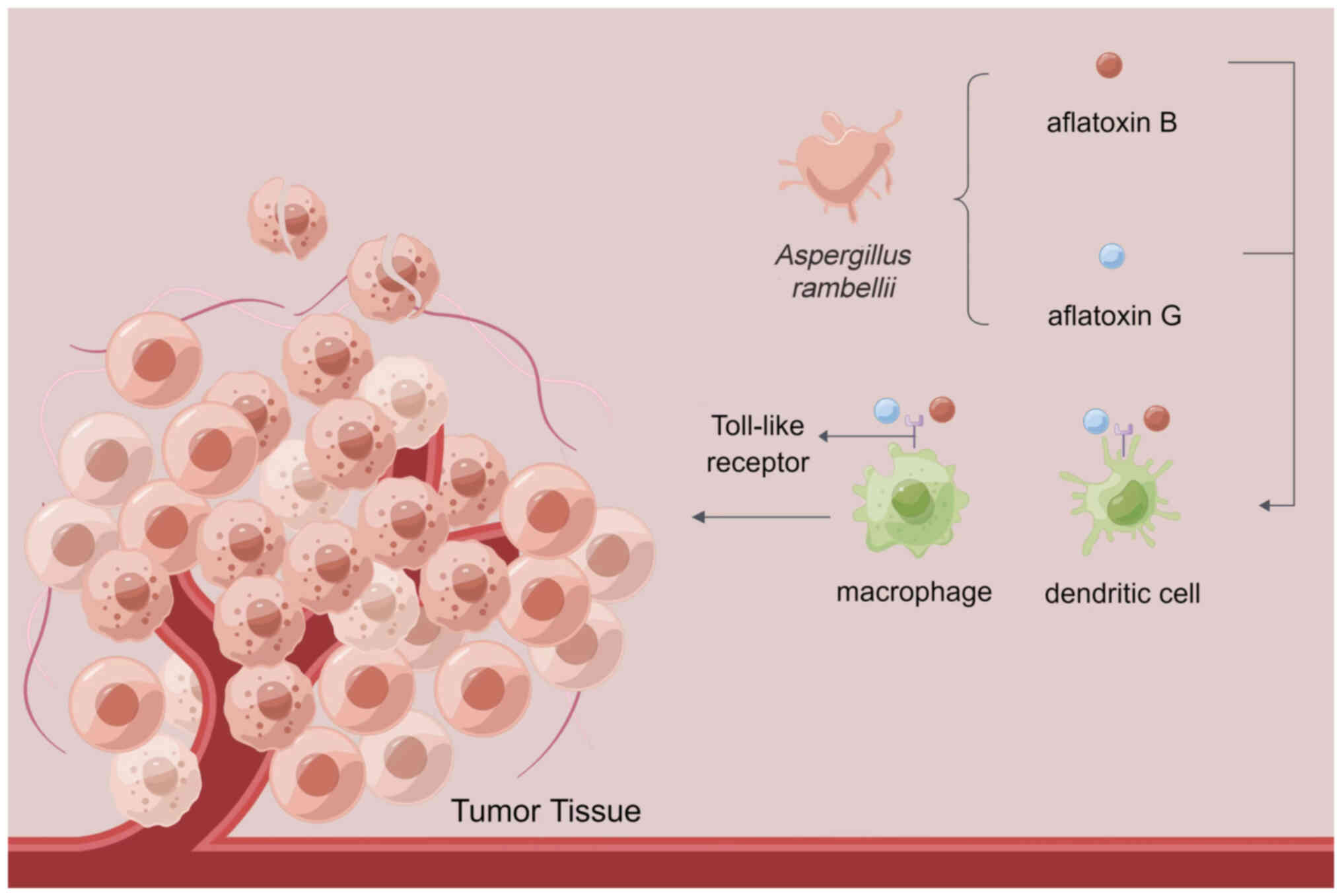
|
Shiao SL, Kershaw KM, Limon JJ, You S,
Yoon J, Ko EY, Guarnerio J, Potdar AA, McGovern DPB, Bose S, et al:
Commensal bacteria and fungi differentially regulate tumor
responses to radiation therapy. Cancer cell. 39:1202–1213.e6. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Spencer CN, McQuade JL, Gopalakrishnan V,
McCulloch JA, Vetizou M, Cogdill AP, Khan MAW, Zhang X, White MG,
Peterson CB, et al: Dietary fiber and probiotics influence the gut
microbiome and melanoma immunotherapy response. Science.
374:1632–1640. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tanoue T, Morita S, Plichta DR, Skelly AN,
Suda W, Sugiura Y, Narushima S, Vlamakis H, Motoo I, Sugita K, et
al: A defined commensal consortium elicits CD8 T cells and
anti-cancer immunity. Nature. 565:600–605. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sokol H, Leducq V, Aschard H, Pham HP,
Jegou S, Landman C, Cohen D, Liguori G, Bourrier A, Nion-Larmurier
I, et al: Fungal microbiota dysbiosis in IBD. Gut. 66:1039–1048.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Findley K, Oh J, Yang J, Conlan S, Deming
C, Meyer JA, Schoenfeld D, Nomicos E, Park M; NIH Intramural
Sequencing Center Comparative Sequencing Program, ; et al:
Topographic diversity of fungal and bacterial communities in human
skin. Nature. 498:367–370. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hoarau G, Mukherjee PK, Gower-Rousseau C,
Hager C, Chandra J, Retuerto MA, Neut C, Vermeire S, Clemente J,
Colombel JF, et al: Bacteriome and mycobiome interactions
underscore microbial dysbiosis in familial Crohn's disease. mBio.
7:e01250–16. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Leonardi I, Paramsothy S, Doron I, Semon
A, Kaakoush NO, Clemente JC, Faith JJ, Borody TJ, Mitchell HM,
Colombel JF, et al: Fungal trans-kingdom dynamics linked to
responsiveness to fecal microbiota transplantation (FMT) therapy in
ulcerative colitis. Cell Host Microbe. 27:823–829.e3. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Doron I, Mesko M, Li XV, Kusakabe T,
Leonardi I, Shaw DG, Fiers WD, Lin WY, Bialt-DeCelie M, Román E, et
al: Mycobiota-induced IgA antibodies regulate fungal commensalism
in the gut and are dysregulated in Crohn's disease. Nat Microbiol.
6:1493–1504. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lewis JD, Chen EZ, Baldassano RN, Otley
AR, Griffiths AM, Lee D, Bittinger K, Bailey A, Friedman ES,
Hoffmann C, et al: Inflammation, antibiotics, and diet as
environmental stressors of the gut microbiome in pediatric Crohn's
disease. Cell Host Microbe. 18:489–500. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Liguori G, Lamas B, Richard ML, Brandi G,
da Costa G, Hoffmann TW, Di Simone MP, Calabrese C, Poggioli G,
Langella P, et al: Fungal dysbiosis in mucosa-associated microbiota
of Crohn's disease patients. J Crohns Colitis. 10:296–305. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tipton L, Müller CL, Kurtz ZD, Huang L,
Kleerup E, Morris A, Bonneau R and Ghedin E: Fungi stabilize
connectivity in the lung and skin microbial ecosystems. Microbiome.
6:122018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhai B, Ola M, Rolling T, Tosini NL,
Joshowitz S, Littmann ER, Amoretti LA, Fontana E, Wright RJ,
Miranda E, et al: High-resolution mycobiota analysis reveals
dynamic intestinal translocation preceding invasive candidiasis.
Nat Med. 26:59–64. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zuo T, Wong SH, Cheung CP, Lam K, Lui R,
Cheung K, Zhang F, Tang W, Ching JYL, Wu JCY, et al: Gut fungal
dysbiosis correlates with reduced efficacy of fecal microbiota
transplantation in Clostridium difficile infection. Nat Commun.
9:36632018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Qin J, Li R, Raes J, Arumugam M, Burgdorf
KS, Manichanh C, Nielsen T, Pons N, Levenez F, Yamada T, et al: A
human gut microbial gene catalogue established by metagenomic
sequencing. Nature. 464:59–65. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Brown GD, Denning DW, Gow NA, Levitz SM,
Netea MG and White TC: Hidden killers: Human fungal infections. Sci
Transl Med. 4:165rv132012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Helmink BA, Khan MAW, Hermann A,
Gopalakrishnan V and Wargo JA: The microbiome, cancer, and cancer
therapy. Nat Med. 25:377–388. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Vogtmann E and Goedert JJ: Epidemiologic
studies of the human microbiome and cancer. Br J Cancer.
114:237–242. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Polk DB and Peek RM Jr: Helicobacter
pylori: Gastric cancer and beyond. Nat Rev Cancer. 10:403–414.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sepich-Poore GD, Zitvogel L, Straussman R,
Hasty J, Wargo JA and Knight R: The microbiome and human cancer.
Science. 371:eabc45522021. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Poore GD, Kopylova E, Zhu Q, Carpenter C,
Fraraccio S, Wandro S, Kosciolek T, Janssen S, Metcalf J, Song SJ,
et al: Microbiome analyses of blood and tissues suggest cancer
diagnostic approach. Nature. 579:567–574. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Dohlman AB, Arguijo Mendoza D, Ding S, Gao
M, Dressman H, Iliev ID, Lipkin SM and Shen X: The cancer
microbiome atlas: A pan-cancer comparative analysis to distinguish
tissue-resident microbiota from contaminants. Cell Host Microbe.
29:281–298.e5. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Nejman D, Livyatan I, Fuks G, Gavert N,
Zwang Y, Geller LT, Rotter-Maskowitz A, Weiser R, Mallel G, Gigi E,
et al: The human tumor microbiome is composed of tumor
type-specific intracellular bacteria. Science. 368:973–980. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Aykut B, Pushalkar S, Chen R, Li Q,
Abengozar R, Kim JI, Shadaloey SA, Wu D, Preiss P, Verma N, et al:
The fungal mycobiome promotes pancreatic oncogenesis via activation
of MBL. Nature. 574:264–267. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Elaskandrany M, Patel R, Patel M, Miller
G, Saxena D and Saxena A: Fungi, host immune response, and
tumorigenesis. Am J Physiol Gastrointest Liver Physiol.
321:G213–G222. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Iliev ID and Leonardi I: Fungal dysbiosis:
Immunity and interactions at mucosal barriers. Nat Rev Immunol.
17:635–646. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Narunsky-Haziza L, Sepich-Poore GD,
Livyatan I, Asraf O, Martino C, Nejman D, Gavert N, Stajich JE,
Amit G, González A, et al: Pan-cancer analyses reveal
cancer-type-specific fungal ecologies and bacteriome interactions.
Cell. 185:3789–3806.e17. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Li X and Saxena D: The tumor mycobiome: A
paradigm shift in cancer pathogenesis. Cell. 185:3648–3651. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhong M, Xiong Y, Zhao J, Gao Z, Ma J, Wu
Z, Song Y and Hong X: Candida albicans disorder is
associated with gastric carcinogenesis. Theranostics. 11:4945–4956.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Coker OO: Non-bacteria microbiome (virus,
fungi, and archaea) in gastrointestinal cancer. J Gastroenterol
Hepatol. 37:256–262. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Coker OO, Nakatsu G, Dai RZ, Wu WKK, Wong
SH, Ng SC, Chan FKL, Sung JJY and Yu J: Enteric fungal microbiota
dysbiosis and ecological alterations in colorectal cancer. Gut.
68:654–662. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Dohlman AB, Klug J, Mesko M, Gao IH,
Lipkin SM, Shen X and Iliev ID: A pan-cancer mycobiome analysis
reveals fungal involvement in gastrointestinal and lung tumors.
Cell. 185:3807–3822.e12. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Seelbinder B, Chen J, Brunke S,
Vazquez-Uribe R, Santhaman R, Meyer AC, de Oliveira Lino FS, Chan
KF, Loos D, Imamovic L, et al: Antibiotics create a shift from
mutualism to competition in human gut communities with a
longer-lasting impact on fungi than bacteria. Microbiome.
8:1332020. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Viscoli C, Castagnola E and Machetti M:
Antifungal treatment in patients with cancer. J Intern Med Suppl.
740:89–94. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Alam A, Levanduski E, Denz P,
Villavicencio HS, Bhatta M, Alhorebi L, Zhang Y, Gomez EC, Morreale
B, Senchanthisai S, et al: Fungal mycobiome drives IL-33 secretion
and type 2 immunity in pancreatic cancer. Cancer Cell.
40:153–167.e11. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Qiu X, Zhang F, Yang X, Wu N, Jiang W, Li
X, Li X and Liu Y: Changes in the composition of intestinal fungi
and their role in mice with dextran sulfate sodium-induced colitis.
Sci Rep. 5:104162015. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Malik A, Sharma D, Malireddi RKS, Guy CS,
Chang TC, Olsen SR, Neale G, Vogel P and Kanneganti TD: SYK-CARD9
signaling axis promotes gut fungi-mediated inflammasome activation
to restrict colitis and colon cancer. Immunity. 49:515–530.e5.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Medzhitov R: Origin and physiological
roles of inflammation. Nature. 454:428–435. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Bannenberg GL, Chiang N, Ariel A, Arita M,
Tjonahen E, Gotlinger KH, Hong S and Serhan CN: Molecular circuits
of resolution: Formation and actions of resolvins and protectins. J
Immunol. 174:4345–4355. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Gordon S: Phagocytosis: An immunobiologic
process. Immunity. 44:463–475. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Bishehsari F, Engen PA, Preite NZ, Tuncil
YE, Naqib A, Shaikh M, Rossi M, Wilber S, Green SJ, Hamaker BR, et
al: Dietary fiber treatment corrects the composition of gut
microbiota, promotes SCFA production, and suppresses colon
carcinogenesis. Genes (Basel). 9:1022018. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Singh N, Baby D, Rajguru JP, Patil PB,
Thakkannavar SS and Pujari VB: Inflammation and cancer. Ann Afr
Med. 18:121–126. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2020. CA Cancer J Clin. 70:7–30. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Naylor MS, Stamp GW, Foulkes WD, Eccles D
and Balkwill FR: Tumor necrosis factor and its receptors in human
ovarian cancer. Potential role in disease progression. J Clin
Invest. 91:2194–2206. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Haghnegahdar H, Du J, Wang D, Strieter RM,
Burdick MD, Nanney LB, Cardwell N, Luan J, Shattuck-Brandt R and
Richmond A: The tumorigenic and angiogenic effects of MGSA/GRO
proteins in melanoma. J Leukoc Biol. 67:53–62. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Thun MJ, Namboodiri MM, Calle EE, Flanders
WD and Heath CW Jr: Aspirin use and risk of fatal cancer. Cancer
Res. 53:1322–1327. 1993.PubMed/NCBI
|
|
54
|
Yang Q, Ouyang J, Pi D, Feng L and Yang J:
Malassezia in inflammatory bowel disease: Accomplice of
evoking tumorigenesis. Front Immunol. 13:8464692022. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Wolf AJ, Limon JJ, Nguyen C, Prince A,
Castro A and Underhill DM: Malassezia spp. induce
inflammatory cytokines and activate NLRP3 inflammasomes in
phagocytes. J Leukoc Biol. 109:161–172. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Zhang YJ, Han Y, Sun YZ, Jiang HH, Liu M,
Qi RQ and Gao XH: Extracellular vesicles derived from
Malassezia furfur stimulate IL-6 production in keratinocytes
as demonstrated in in vitro and in vivo models. J Dermatol Sci.
93:168–175. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Berti M and Vindigni A: Replication
stress: Getting back on track. Nat Struct Mol Biol. 23:103–109.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Kawanishi S, Ohnishi S, Ma N, Hiraku Y and
Murata M: Crosstalk between DNA damage and inflammation in the
multiple steps of carcinogenesis. Int J Mol Sci. 18:18082017.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Lin Y, Wang G, Yu J and Sung JJY:
Artificial intelligence and metagenomics in intestinal diseases. J
Gastroenterol Hepatol. 36:841–847. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Wong SH and Yu J: Gut microbiota in
colorectal cancer: Mechanisms of action and clinical applications.
Nat Rev Gastroenterol Hepatol. 16:690–704. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Perrone G and Gallo A: Aspergillus
species and their associated mycotoxins. Methods Mol Biol.
1542:33–49. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Dai Z, Coker OO, Nakatsu G, Wu WKK, Zhao
L, Chen Z, Chan FKL, Kristiansen K, Sung JJY, Wong SH and Yu J:
Multi-cohort analysis of colorectal cancer metagenome identified
altered bacteria across populations and universal bacterial
markers. Microbiome. 6:702018. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Lin Y, Lau HC, Liu Y, Kang X, Wang Y, Ting
NL, Kwong TN, Han J, Liu W, Liu C, et al: Altered mycobiota
signatures and enriched pathogenic Aspergillus rambellii are
associated with colorectal cancer based on multicohort fecal
metagenomic analyses. Gastroenterology. 163:908–921. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Luan C, Xie L, Yang X, Miao H, Lv N, Zhang
R, Xiao X, Hu Y, Liu Y, Wu N, et al: Dysbiosis of fungal microbiota
in the intestinal mucosa of patients with colorectal adenomas. Sci
Rep. 5:79802015. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Gao R, Kong C, Li H, Huang L, Qu X, Qin N
and Qin H: Dysbiosis signature of mycobiota in colon polyp and
colorectal cancer. Eur J Clin Microbiol Infect Dis. 36:2457–2468.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Richard ML, Liguori G, Lamas B, Brandi G,
da Costa G, Hoffmann TW, Pierluigi Di Simone M, Calabrese C,
Poggioli G, et al: Mucosa-associated microbiota dysbiosis in
colitis associated cancer. Gut Microbes. 9:131–142. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Cary JW, Ehrlich KC, Beltz SB,
Harris-Coward P and Klich MA: Characterization of the
Aspergillus ochraceoroseus aflatoxin/sterigmatocystin
biosynthetic gene cluster. Mycologia. 101:352–362. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Frisvad JC, Skouboe P and Samson RA:
Taxonomic comparison of three different groups of aflatoxin
producers and a new efficient producer of aflatoxin B1,
sterigmatocystin and 3-O-methylsterigmatocystin, Aspergillus
rambellii sp. nov. Syst Appl Microbiol. 28:442–453. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Navale V, Vamkudoth KR, Ajmera S and Dhuri
V: Aspergillus derived mycotoxins in food and the
environment: Prevalence, detection, and toxicity. Toxicol Rep.
8:1008–1030. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Uka V, Cary JW, Lebar MD, Puel O, De
Saeger S and Diana Di Mavungu J: Chemical repertoire and
biosynthetic machinery of the Aspergillus flavus secondary
metabolome: A review. Compr Rev Food Sci Food Saf. 19:2797–2842.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
McCullough AK and Lloyd RS: Mechanisms
underlying aflatoxin-associated mutagenesis-implications in
carcinogenesis. DNA Repair (Amst). 77:76–86. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Bianco G, Russo R, Marzocco S, Velotto S,
Autore G and Severino L: Modulation of macrophage activity by
aflatoxins B1 and B2 and their metabolites aflatoxins M1 and M2.
Toxicon. 59:644–650. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Mohammadi A, Mehrzad J, Mahmoudi M and
Schneider M: Environmentally relevant level of aflatoxin B1
dysregulates human dendritic cells through signaling on key
toll-like receptors. Int J Toxicol. 33:175–186. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Soler AP, Miller RD, Laughlin KV, Carp NZ,
Klurfeld DM and Mullin JM: Increased tight junctional permeability
is associated with the development of colon cancer. Carcinogenesis.
20:1425–1431. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Martin TA and Jiang WG: Loss of tight
junction barrier function and its role in cancer metastasis.
Biochim Biophys Acta. 1788:872–891. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Liu NN, Jiao N, Tan JC, Wang Z, Wu D, Wang
AJ, Chen J, Tao L, Zhou C, Fang W, et al: Multi-kingdom microbiota
analyses identify bacterial-fungal interactions and biomarkers of
colorectal cancer across cohorts. Nat Microbiol. 7:238–250. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Gmeiner WH, Hellmann GM and Shen P:
Tissue-dependent and -independent gene expression changes in
metastatic colon cancer. Oncol Rep. 19:245–251. 2008.PubMed/NCBI
|
|
79
|
Tjalsma H, Boleij A, Marchesi JR and
Dutilh BE: A bacterial driver-passenger model for colorectal
cancer: Beyond the usual suspects. Nat Rev Microbiol. 10:575–582.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Wirbel J, Pyl PT, Kartal E, Zych K,
Kashani A, Milanese A, Fleck JS, Voigt AY, Palleja A, Ponnudurai R,
et al: Meta-analysis of fecal metagenomes reveals global microbial
signatures that are specific for colorectal cancer. Nat Med.
25:679–689. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Thomas AM, Manghi P, Asnicar F, Pasolli E,
Armanini F, Zolfo M, Beghini F, Manara S, Karcher N, Pozzi C, et
al: Metagenomic analysis of colorectal cancer datasets identifies
cross-cohort microbial diagnostic signatures and a link with
choline degradation. Nat Med. 25:667–678. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Zhu F, Willette-Brown J, Song NY, Lomada
D, Song Y, Xue L, Gray Z, Zhao Z, Davis SR, Sun Z, et al:
Autoreactive T cells and chronic fungal infection drive esophageal
carcinogenesis. Cell Host Microbe. 21:478–493.e7. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Azad MAK, Sarker M, Li T and Yin J:
Probiotic species in the modulation of gut microbiota: An overview.
Biomed Res Int. 2018:94786302018. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Mozaffari Namin B, Daryani NE, Mirshafiey
A, Yazdi MKS and Dallal MMS: Effect of probiotics on the expression
of Barrett's oesophagus biomarkers. J Med Microbiol. 64:348–354.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Rosania R, Minenna MF, Giorgio F,
Facciorusso A, De Francesco V, Hassan C, Panella C and Ierardi E:
Probiotic multistrain treatment may eradicate Helicobacter
pylori from the stomach of dyspeptics: A placebo-controlled
pilot study. Inflamm Allergy Drug Targets. 11:244–249. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Zhu R, Chen K, Zheng YY, Zhang HW, Wang
JS, Xia YJ, Dai WQ, Wang F, Shen M, Cheng P, et al: Meta-analysis
of the efficacy of probiotics in Helicobacter pylori
eradication therapy. World J Gastroenterol. 20:18013–18021. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Kumar V, Yadav AN, Verma P, Sangwan P,
Saxena A, Kumar K and Singh B: β-Propeller phytases: Diversity,
catalytic attributes, current developments and potential
biotechnological applications. Int J Biol Macromol. 98:595–609.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Lipke PN and Ovalle R: Cell wall
architecture in yeast: New structure and new challenges. J
Bacteriol. 180:3735–3740. 1998. View Article : Google Scholar : PubMed/NCBI
|