Introduction
Meningioma is a benign spinal cord tumor that arises
from cap cells of the arachnoid membrane or fibroblasts of the dura
mater. Globally, meningiomas account for 10–30% of intraspinal
tumors (1), and 85% of meningiomas
are located in the extramedullary subdural space (2). Atypical meningioma is rarely reported
in the literature; its clinical manifestations are non-specific,
and the imaging findings are similar to other intraspinal
space-occupying lesions. Notably, atypical meningioma is usually
misdiagnosed as schwannoma or metastases, and intraoperative
findings and pathological examination are required to confirm the
diagnosis. The tumor grows slowly and often presents with symptoms
of chronic progressive spinal cord compression, resulting in limb
motor, sensory and reflex disturbances below the level of
compression. Meningiomas show low signal intensity on T1-weighted
images, high signal intensity on T2-weighted images, and high
signal intensity on enhanced images (3). Atypical meningioma with bone
destruction in the cervical spinal canal is even rarer, and only a
small number of relevant reports have been reported (4,5). At
present, surgical resection is the main treatment for atypical
meningiomas, and postoperative adjuvant therapy is mainly
radiotherapy. The present case report describes the clinical data
of a patient with cervical intraspinal atypical meningioma admitted
to the Department of Neurosurgery, Shengli Oilfield Central
Hospital (Dongying, China), with the aim of improving the
understanding of this disease.
Case report
A 50-year-old female patient was admitted to Shengli
Oilfield Central Hospital in June 2023, due to numbness of four
extremities, unstable walking for 3 years, and aggravation of
symptoms for 6 months. A total of 3 years prior, the patient had
numbness in both hands without obvious inducement and did not
receive specific treatment. A total of 6 months prior, the symptoms
of the patient were gradually aggravated, and the patient had
numbness of all four extremities, unstable walking, the sensation
of walking on cotton wool, inflexible fine movements of both hands,
a girdle sensation on the chest and back, self-perceived neck pain
and discomfort, but no vertigo, palpitations, tinnitus or diplopia,
and no radiating pain in both upper limbs. A total of 6 months
prior to admission, the aforementioned symptoms were markedly
aggravated and the patient had fallen due to unstable walking. The
patient therefore visited a local hospital (Dongying People's
Hospital, Dongying, China) for oral methylcobalamin (0.5 mg/time,
tid) drug treatment with poor results, and was later admitted to
Shengli Oilfield Central Hospital for further treatment. The
patient had a history of hypertension for 3 years and was regularly
treated with oral benazepril (10 mg/time, qd) every day with good
blood pressure control. A neurological examination showed the
following: Straightening of physiological curvature of the cervical
vertebrae, no obvious limitation of cervical motion, no obvious
tenderness or percussion pain in the spinous process and
paravertebral region of the cervical vertebrae, cervical
hyperflexion, and hyperextension test (+); hypoesthesia of distal
skin in the shoulder joints of the bilateral upper limbs, normal
sensation in the remaining limbs; muscle strength of the bilateral
upper limbs, grade 4, muscle strength of the lower limbs, grade 5;
hypertonia of four extremities; bilateral biceps reflex (+ + +),
triceps reflex (+ + +), radial membrane reflex (+ +), bilateral
knee tendon-reflex (+ + + +), Achilles tendon reflex (+ + +);
bilateral ankle clonus (+), patellar clonus (−); bilateral Hoffman
sign (+), bilateral Babinski sign (+). The diagnosis on admission
was: i) Cervical spondylotic myelopathy; ii) hypertension. However,
the patient's blood pressure was well controlled with medication
and their blood pressure on admission was 111/72 mmHg.
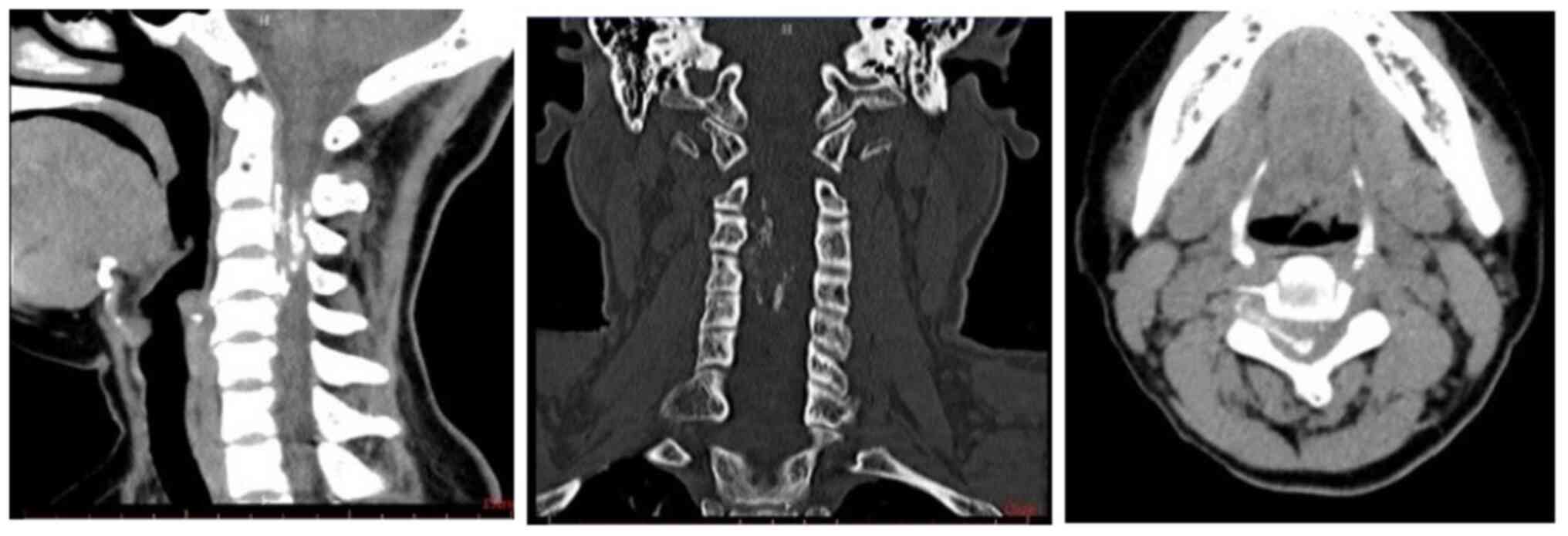
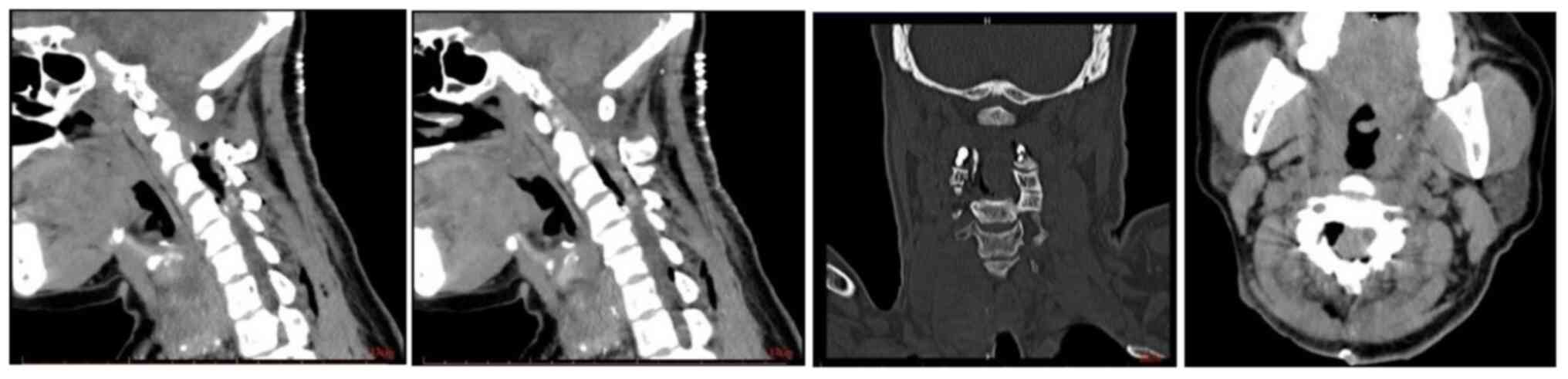
The day after admission, a cervical spine CT showed
a mixed density lesion in the spinal canal and spinal stenosis at
the posterior edge of the cervical 3–4 pyramid (Fig. 1). A total of 3 days after admission,
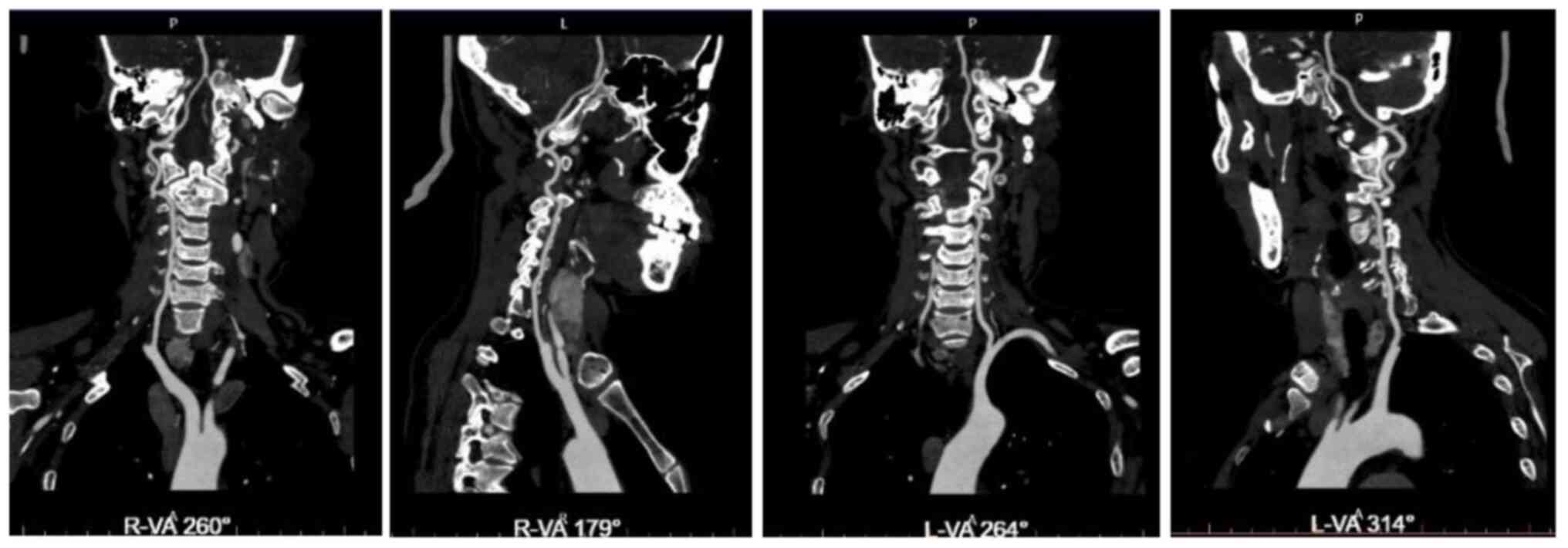
head and neck CT angiography showed no significant abnormalities
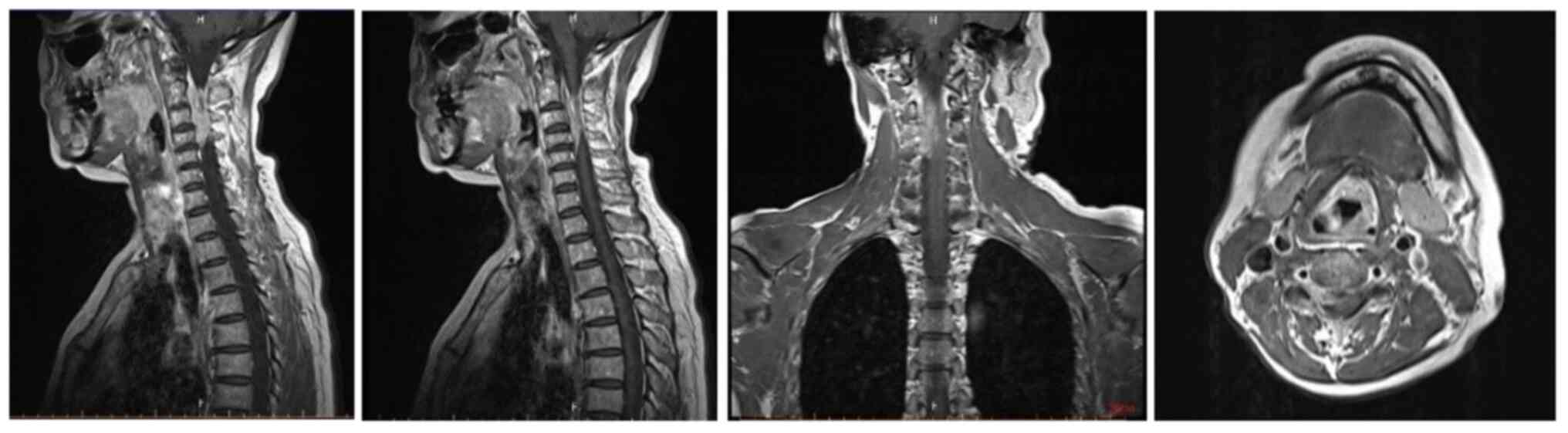
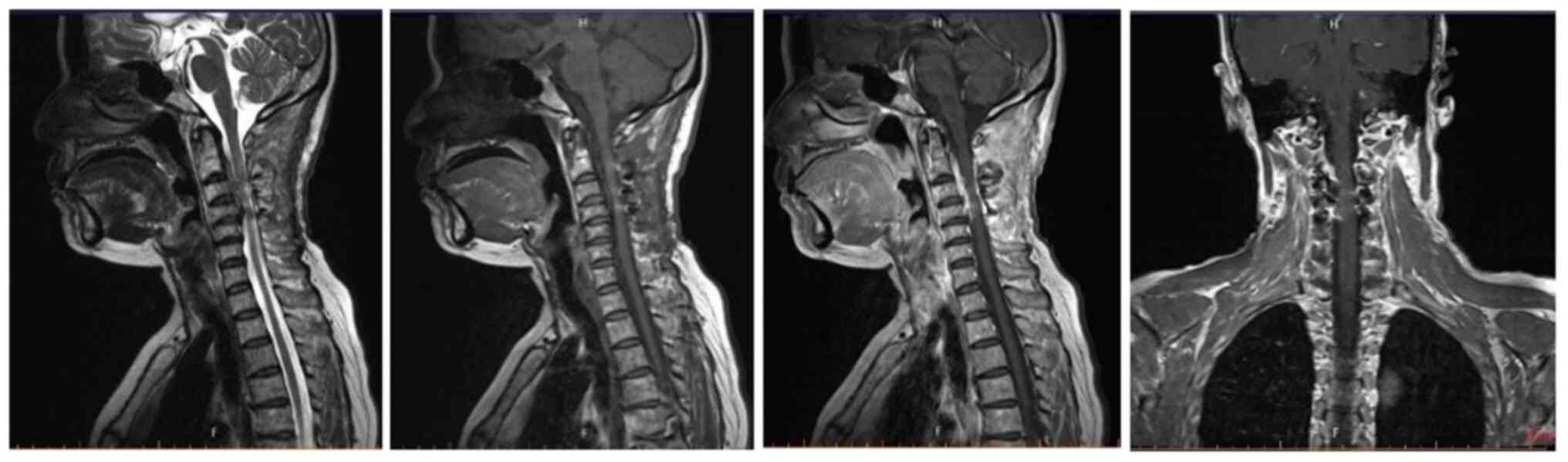
(Fig. 2); on the same day, cervical
spine enhanced magnetic resonance imaging (MRI) showed a
space-occupying lesion in the spinal canal at the C2-4 level
(Fig. 3). A total of 11 days after
admission, cervical intraspinal tumor resection was performed under
general anesthesia, during which the posterior arch of the atlas,
C2-C4 spinous process and lamina were exposed, and the bilateral
laminae of C2-C4 were grooved with a burr to completely remove the
lamina including the C2-C4 spinous process. The lesion broke
through the dura mater and grew into the right C3-C4 intervertebral
foramen, and the base of the tumor was located in the dura mater,
which was firm in consistency, calcified, poorly circumscribed and
rich in blood supply. A piecemeal resection of the tumor was
performed, the boundary of the lesion on the surface of the spinal
cord was carefully separated, part of the C3-C4 facet was abraded,
the intervertebral foramen was explored, and the intraforaminal
lesion was subtotally removed. Finally, the patient underwent
fixation and reduction surgery for the C2-C4 lamina. Postoperative
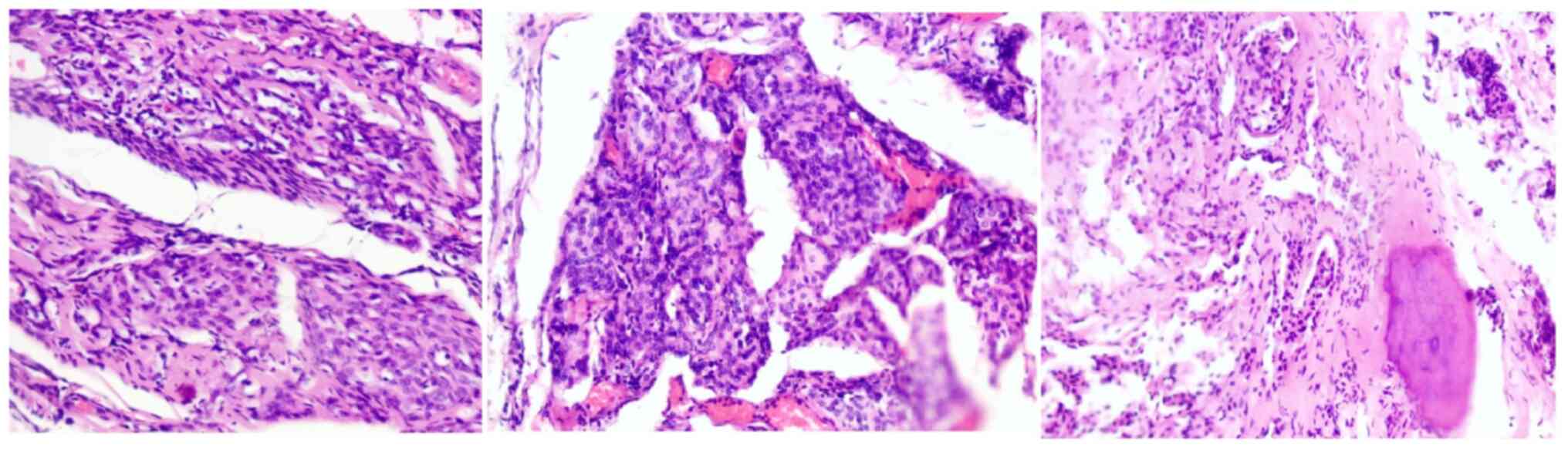
pathology showed cervical spinal meningioma with local hot spot
mitotic figures of ~3/mm, morphology consistent with atypical
meningioma (World Health Organization grade II) (6), accompanied by bone tissue invasion,
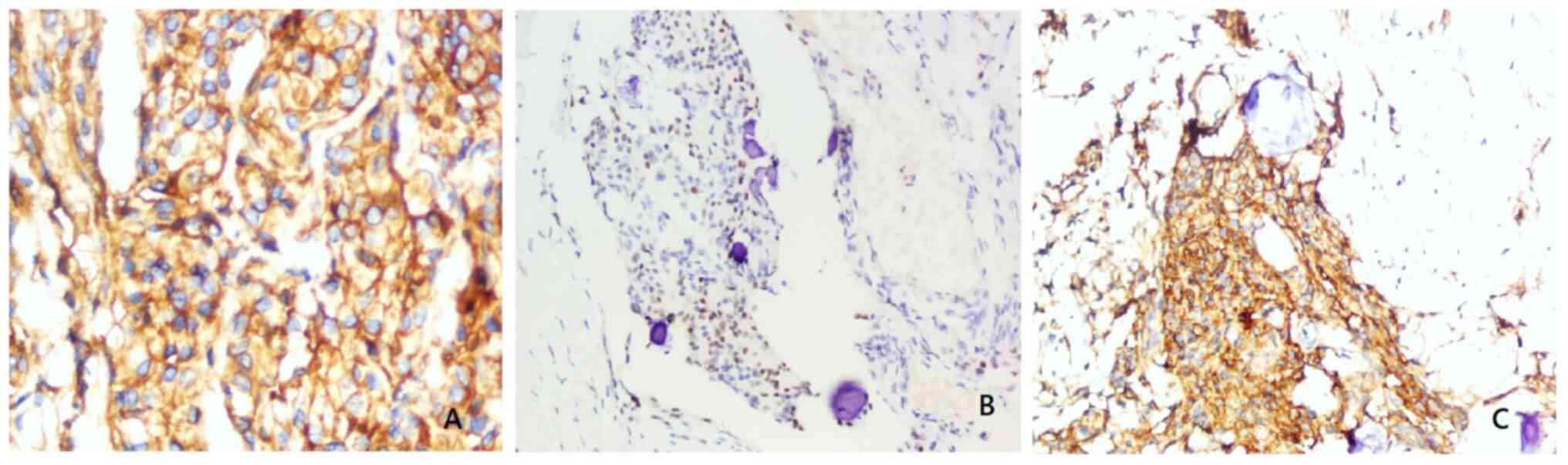
and no neoplastic necrosis or spinal cord invasion (Fig. 4). Immunohistochemical results
(Fig. 5) were as follows: Broad
spectrum cytokeratin (focal weak data not shown), epithelial
membrane antigen (Fig. 5C), glial
fibrillary acidic protein (data not shown), progesterone receptor
(Fig. 5B), vimentin (data not
shown), H3K27me3 (data not shown), STAT6 (data not shown),
somatostatin receptor type 2 (Fig.
5A), S-100 (data not shown) and Ki-67 (~2%, data not shown).
Immunohistochemistry was performed according to a previously
described protocol (7). A total of
12 days after admission, cervical spine CT showed satisfactory
tumor resection (Fig. 6). The
patient was treated with mannitol (125 ml/time, tid),
methylprednisolone (500 mg/time, qd) and methylcobalamin (0.5
mg/time, tid) after surgery. Eventually, the condition of the
patient improved and they were discharged.
In early August 2023, the patient was admitted to
the oncology department (Shengli Oilfield Hospital) for
radiotherapy due to postoperative atypical spinal meningioma of
cervical vertebra. The target volume included C2-C4 and the
radiation dose was 40 Gy. This patient underwent a total of 20
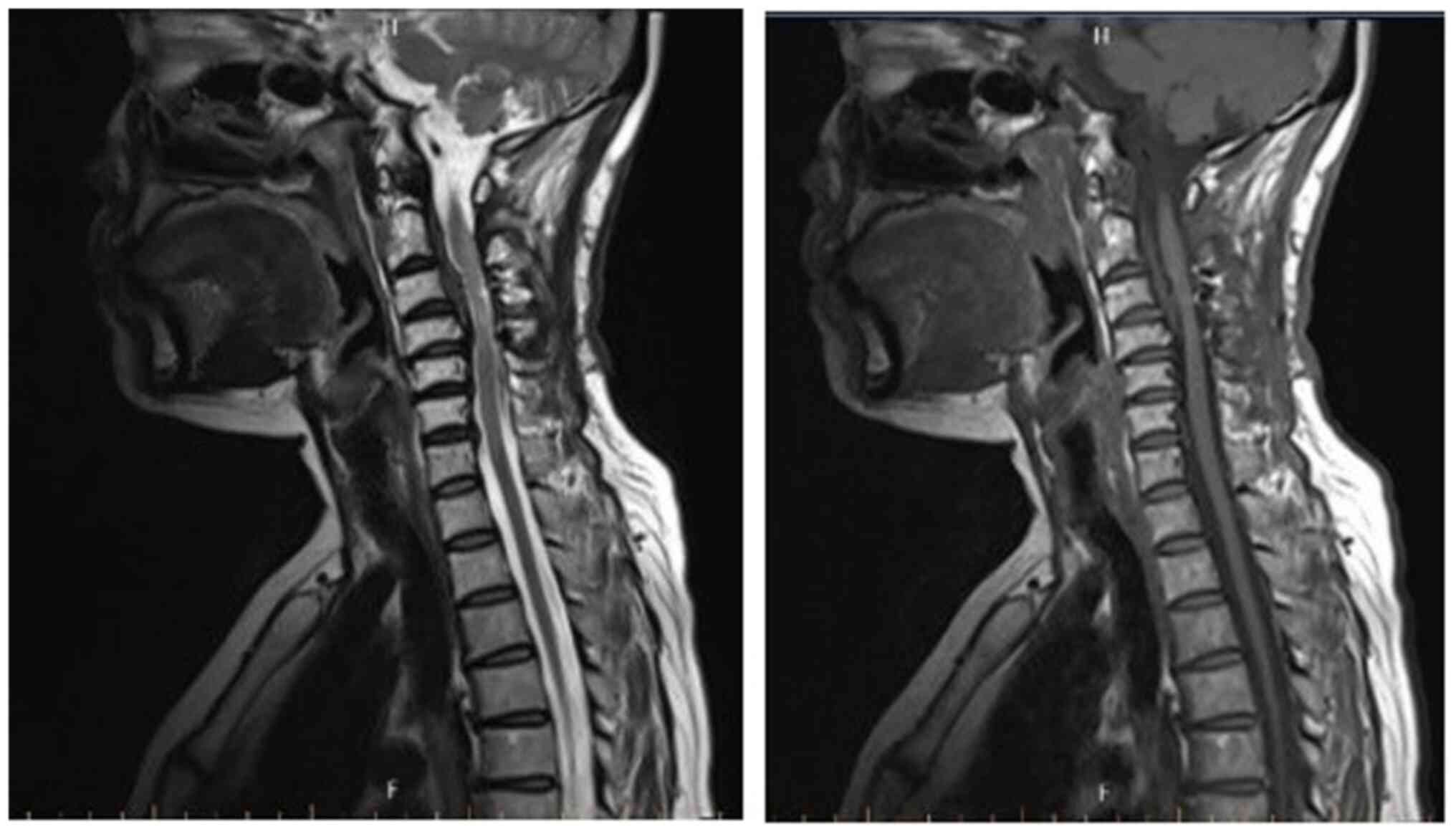
radiation treatments. A total of 4 days later, cervical spine
enhanced MRI showed that the lesion was markedly smaller than
before (Fig. 7). Repeated cervical
spine MRI in mid-October showed no marked tumor recurrence
(Fig. 8).
Discussion
Meningioma is the second most common benign tumor
after schwannoma in the extramedullary subdural space, which is
specifically common in women aged 40–70 years (8). In addition, meningioma is the most
common tumor in the thoracic spinal canal. The mean age of onset is
45 years, indicating that endocrine hormones have an effect on the
formation of meningioma (8). The
common early manifestations of the disease include: Numbness of the
extremities, fatigue, chest and back pain, and difficulty in
walking. Later, there may be hypertonia, active or hyperactive key
reflexes, paraplegia, and fecal and urinary dysfunction. In the
present case report, the patient was a 50-year-old woman who
developed a cervical spine meningioma. Previous studies have
reported that 85% of meningioma cases are intradural, 7% extend
epidurally and 8% are completely epidural (5,9). The
present case was intradural with cervical bone destruction. By
referring to the relevant literature, only one report of foraminal
invasion and bone erosion was found. The patient was a 39-year-old
woman who was found to have T3/4 and T5/6 meningiomas by MRI, with
symptoms including progressive numbness and weakness of both lower
limbs, and gait instability. The meningiomas were shown to be
invading the left and right foramina of T3/4, and the tumors were
found to have calcification and bone erosion during surgery
(5).
The exact pathogenesis of meningioma is unknown.
Some scholars hypothesize that tumors arise from arachnoid cells
extending along peripheral nerves, and these ectopic or isolated
arachnoid tissues initially accumulate in arachnoid villi,
especially around the peripheral nerve root sleeves, where the
spinal leptomeninges directly drain into the dura mater (10). Some scholars believe that the dura
mater around nerve roots may contain residual superficial embryonic
arachnoid villi, which may explain epidural and some periradicular
meningiomas; others believe that arachnoid islands may migrate into
the epidural space, such as orbital meningiomas without associated
optic nerve sheaths (11–13). The present case of meningioma
breakthrough into the intervertebral foramen can be explained by
the fact that the tumor may arise from arachnoid cells around the
spinal nerve roots (10,11), but such patients are extremely rare
in clinical practice.
Differential diagnosis of meningioma includes
schwannoma, metastases of cancer, such as breast cancer and lung
cancer, in the spinal canal, lymphoma and tuberculoma (14). MRI is the first imaging choice for
this disease, and can show the location, size and shape of
intraspinal tumors, whether there is bleeding or cystic
degeneration in the tumor, and the relationship with neural tissue.
Meningioma exhibits low signal intensity on T1-weighted images and
high signal intensity on T2-weighted images, and exhibits moderate
homogeneous enhancement after gadopentetic acid injection (3). Intraoperative findings and
pathological examination are the main basis for definitive
diagnosis.
The main treatment of atypical meningioma is
surgical resection, and whether the tumor recurs and the survival
time of patients is closely related to the degree of the first
surgical resection of the tumor (15,16).
In the present case report, the patient was a middle-aged woman;
total resection should be completed as much as possible if the
diagnosis is not completely confirmed; however, in the present
case, the tumor invaded the intervertebral foramen and was
accompanied by bone destruction, thus making total resection
difficult. In the present case, the tumor was surgically removed
under general anesthesia using a microscope. Extramedullary
intradural tumors are most commonly located in the anterolateral
aspect of the spinal canal (17),
and the spinal cord often protrudes backwards due to compression
from the meningioma. After opening the dura mater, the relationship
between the tumor and the spinal cord and nerve roots should be
carefully explored. In the present case, after separating the
spinal cord and tumor, the spinal cord was protected with a piece
of cotton, the base of the tumor was fully exposed,
electrocoagulation was performed to stop bleeding, and the tumor
was removed together with the attached dura mater. Notably, in the
case of large tumors, it can be removed in pieces. During tumor
resection, the nerve surrounded by the tumor should be carefully
separated, and when the nerve root adheres tightly to the tumor or
penetrates out of the tumor, the tumor capsule should be incised,
the tumor should be removed piecemeal in the capsule and the nerve
should be separated as much as possible. In addition, the nerve
root should be protected as much as possible, and the tumor should
be removed as completely as possible during surgery. When the
boundary between the tumor and the spinal cord is unclear, surgeons
should be careful and avoid removing the tumor that adheres to the
spinal cord to avoid causing spinal cord injury. For patients with
subtotal resection, postoperative radiotherapy can achieve a
certain period of remission. The irradiation dose is generally
40–50 Gy for 4–5 weeks; however, radiotherapy can cause radiation
myelitis. In the present case, adjuvant radiotherapy was performed
after surgery because some tumor cells remained in the
intervertebral foramen and the patient did not develop radiation
myelitis during the treatment.
The long-term prognosis of atypical meningioma is
still unclear. Early MRI signals are often affected by surgery. In
order to accurately show the extent of tumor resection, MRI should
be performed 3 months after surgery in patients with meningioma.
MRI is also recommended to be performed every 1–2 years for 10
years after surgery. The global recurrence rate of meningioma is
6–15% and recurrence may depend on whether the tumor is completely
resected (18). Globally, if the
tumor is completely resected, the 5-, 10- and 15-year
recurrence-free survival rates are 93, 80, and 68%, respectively
(19); in cases of subtotal
resection, the 5-, 10- and 15-year recurrence-free survival rates
are 63, 45 and 9%, respectively (20). Other factors associated with poor
prognosis are epidural invasion, age <50 years, multiple
lesions, calcification, ossification and anterior location of the
lesion (8,14,20).
In the present case report, the patient was reexamined 3 months
after surgery, and no tumor recurrence was observed.
In conclusion, atypical meningioma exhibits
nonspecific symptoms before surgery, and the diagnosis mainly
depends on intraoperative macroscopic findings and pathological
examination. Surgical resection is the main treatment for atypical
meningioma and radiotherapy is the main adjuvant therapy after
surgery. Notably, total tumor resection can markedly reduce the
recurrence rate of postoperative tumors and prolong the survival
time of patients.
Acknowledgements
The authors would like to thank Dr Bin Xu and Dr
Quan Zhi (Department of Pathology, Shengli Oilfield Central
Hospital) for providing pathological information.
Funding
The present study was personally supported by Likun Mu.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LM and MW conceived and designed the study. ZS, LC
and GC provided study materials and treated the patient. LM and MW
wrote the manuscript. LM and MW confirm the authenticity of all the
raw data. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient signed an informed consent form.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Koeller KK, Rosenblum RS and Morrison AL:
Neoplasms of the spinal cord and filum terminale:
Radiologic-pathologic correlation. Radiographics. 20:172l–1749.
2000. View Article : Google Scholar
|
|
2
|
Buetow MP, Buetow PC and Smimiotopoulos
JG: At typical and misleading features in meningiomas.
Radiographics. 11:1087–1106. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Salpietro FM, Alafaci C, Lucerna S,
Iacopino DG and Tomasello F: Do spinal meningiomas penetrate the
pial layer? Correlation between magnetic resonance imaging and
microsurgical findings and intracranial tumor interfaces.
Neurosurgery. 41:254–257; discussion 257–258. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Dehcordi SR, Ricci A, Chiominto A, De
Paulis D, Di Vitantonio H and Galzio RJ: Dorsal extradural
meningioma: Case report and literature review. Surg Neurol Int.
7:762016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Takeuchi H, Kubota T, Sato K and Hirose S:
Cervical extradural-meningioma with rapidly progressive myelopathy.
J Clin Neurosci. 13:397–400. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Louis DN, Perry A, Reifenberger G, von
Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD,
Kleihues P and Ellison DW: The 2016 world health organization
classification of tumors of the central nervous system: A summary.
Acta Neuropathologica. 131:803–820. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cimino PJ: Malignant progression to
anaplastic meningioma: Neuropathology, molecular pathology, and
experimental models. Exp Mol Pathol. 99:354–359. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Levy WJ Jr, Bay J and Dohn D: Spinal cord
meningioma. J Neurosurg. 57:804–812. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Solero CL, Fornari M, Giombini S, Lasio G,
Oliveri G, Cimino C and Pluchino F: Spinal meningiomas: Review of
174 operated cases. Neurosurgery. 25:153–160. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zevgaridis D and Thomé C: Purely epidural
spinal meningioma mimicking metastatic tumor: Case report and
review of the literature. Spine (Phila Pa 1976). 27:E403–E405.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Frank BL, Harrop JS, Hanna A and Ratliff
J: Cervical extradural meningioma: Case report and literature
review. J Spinal Cord Med. 31:302–305. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Savardekar A, Chatterjee D, Chatterjee D,
Dhandapani S, Mohindra S and Salunke P: Totally extradural spinal
en plaque meningiomas-diagnostic dilemmas and treatment strategies.
Surg Neurol Int. 5 (Suppl 7):S291–S294. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Singh R, Coerkamp G and Luyendijk W:
Spinal epidural meningiomas. Acta Neurochir (Wien). 18:237–245.
1968. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chotai SP, Mrak RE, Mutgi SA and Medhkour
A: Ossification in an extra-intradural spinal meningioma-pathologic
and surgical vistas. Spine J. 13:e21–e26. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Subaciute J: Extramedullar spinal cord
tumours. Clin Neurol Neurosurg. 99:175–176. 1997. View Article : Google Scholar
|
|
16
|
Klekamp J and Samii M: Surgical results
for spinal meningiomas. Surg Neurol. 52:552–562. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kocheregkin BA, Katchkov LA and Makarenko
MF: Microsurgical aspects of extramedullary intradural tumors of
spinal cord. Clin Neurol Neurosurg. 99:204–205. 1997. View Article : Google Scholar
|
|
18
|
Black PM: Meningiomas. Neurosurgery.
32:643–657. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mirimanoff RO, Dosoretz DE, Linggood RM,
Ojemann RG and Martuza RL: Meningioma: analysis of recurrence and
progression following neurosurgical resection. J Neurosurg.
62:18–24. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Nakamura M, Tsuji O, Fujiyoshi K, Hosogane
N, Watanabe K, Tsuji T, Ishii K, Toyama Y, Chiba K and Matsumoto M:
Long-term surgical outcomes of spinal meningiomas-Spine. (Phila Pa
1976). 37:E617–E623. 2012. View Article : Google Scholar
|