Introduction
Ependymoma is a neuroepithelial tumor that can
originate from ependymal cells in the brain, the central canal of
the spinal cord or the cortex. The incidence rate of ependymoma is
low, accounting for 1.6–1.8% of all primary central nervous system
tumors; it is more common in children, accounting for 5.2%, while
it is ~4% in adults. The incidence rate in males is slightly higher
than that in females (1.3:1) (1).
The location of the tumor largely depends on the patient's age,
with ~90% of pediatric ependymomas occurring in the intracranial
region and 65% of adult tumors occurring in the spinal cord
(2). Carcinomas commonly
metastasize to the lymph nodes, lungs, bones, liver and brain.
However, metastases to the gallbladder are rare and have only been
reported minimally in the literature (3–5). In
addition, primary tumors, such as hepatocellular carcinoma
(6) and pancreatic cancer (7), may invade the gallbladder. However,
ependymoma that metastasizes to the gallbladder has not been
reported previously. In the present study, the case of a patient
with metastatic ependymoma to the gallbladder who underwent
cholecystectomy under general anesthesia with nerve block
anesthesia was described. Furthermore, a review of the literature
on this condition was provided in the present report.
Case report
A 42-year-old female patient presented at Cangzhou
People's Hospital (Cangzhou, China) in May 2022 due to the
discovery of a gallbladder mass in an ultrasound examination 11
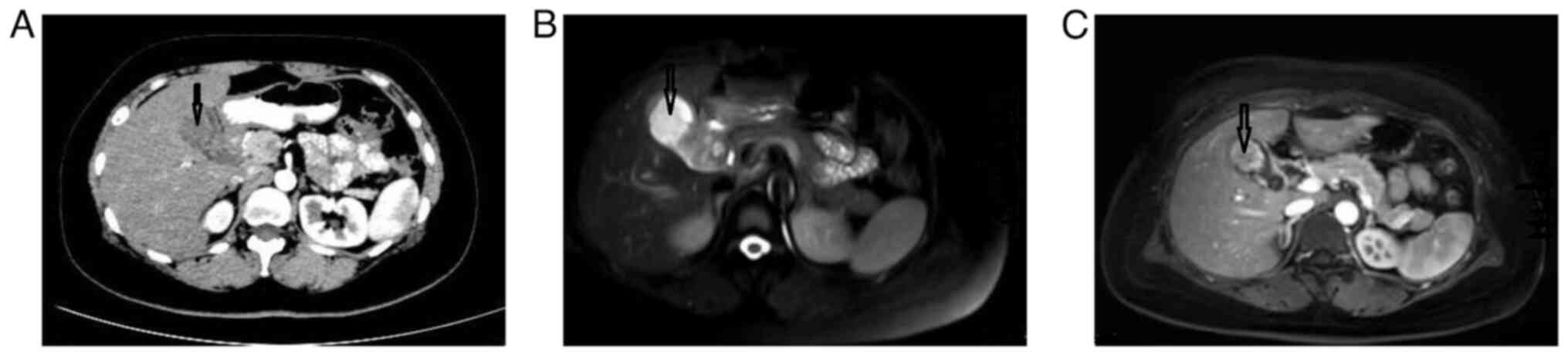
days prior. The patient underwent an enhanced spiral CT scan of the
lower abdomen, which revealed irregular thickening of the
gallbladder wall protruding into the cavity (May 2022). The
enhancement progressively increased after administration of
contrast agent, and there was an unclear boundary between the
lesion and the liver (Fig. 1A).
Based on these findings, the possibility of gallbladder cancer was
considered. An abdominal MRI (May 2022) showed that the upper part
of the gallbladder body was occupied, with significant enhancement
on the enhanced scan. In addition, the cystic duct was dilated,
indicating the presence of possible gallbladder malignant tumor
lesions (Fig. 1B and C).
The patient had previously undergone a craniotomy at
The Third Medical Center of the Chinese People's Liberation Army
General Hospital (Beijing, China) for a right frontal lobe mass in
2017. The postoperative pathological report confirmed it as an
anaplastic ependymoma [World Health Organization (WHO) grade III]
(8) in the right frontal lobe.
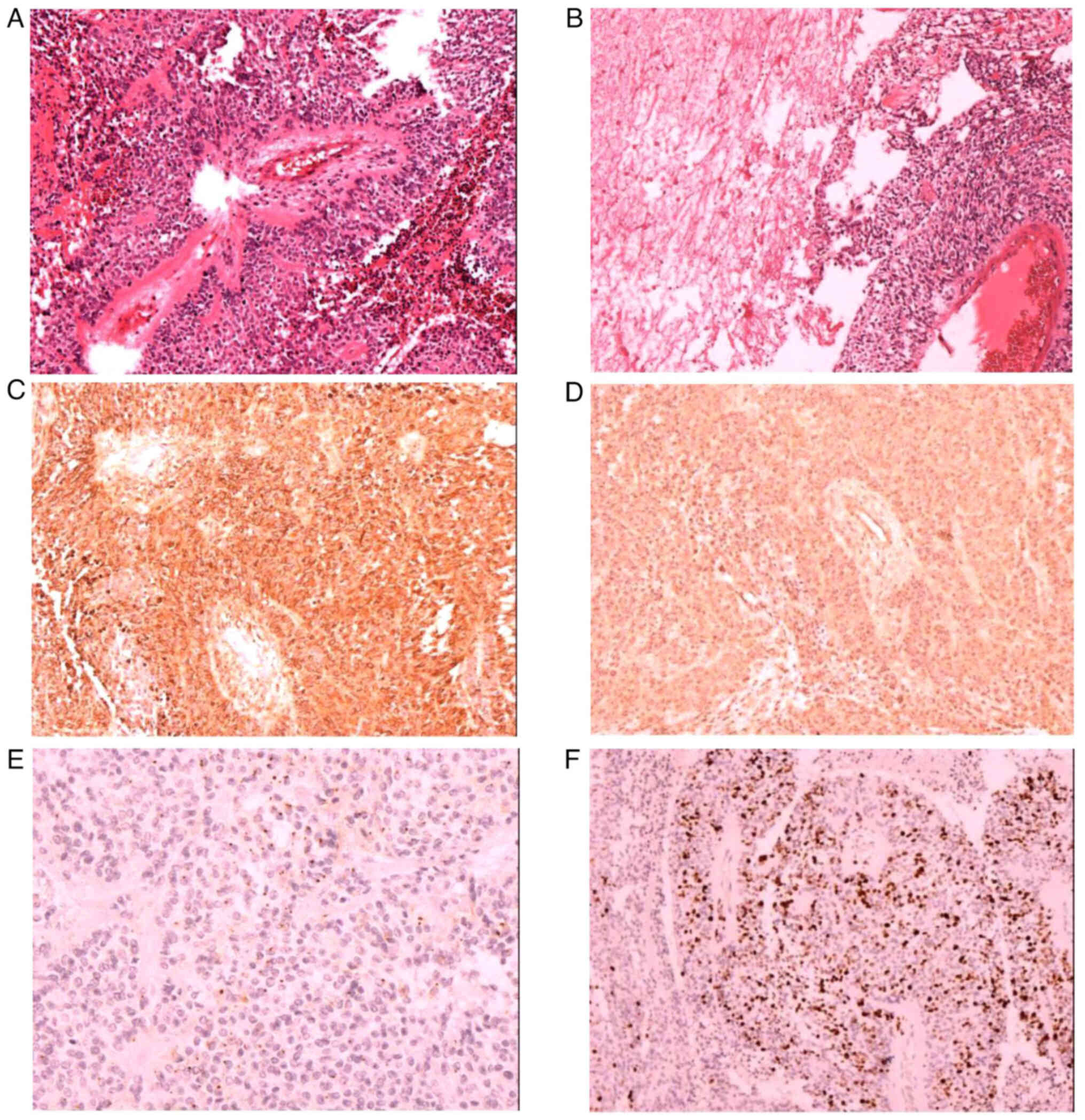
Under a microscope, tumor cells can be observed to be circular or
elliptical in shape, with a false rosette like structure around the
blood vessels (Fig. 2A). In
addition, necrosis can be observed in the tumor tissue (Fig. 2B). Immunohistochemistry [performed
using the Ventura BenchMark ULTRA (Roche Diagnostics) staining
procedure; all reagents were from Roche Diagnostics] indicated that
the mass was glial fibrillary acidic protein GFAP+ (cat. no.
GM-0031; 1:100 dilution; Fig. 2C),
partially S-100+ (cat. no. SM-0011; 1:100 dilution), Vimentin+
(cat. no. VM-0031; 1:100 dilution; Fig.
2D), EMA+ (cat. no. EM0-0041; 1:100 dilution; Fig. 2E), Olig2− (cat. no.
ORM-0015; 1:100 dilution), Ki67 (10–20%; cat. no. KM-0021; 1:100
dilution; Fig. 2F), neuron-specific
enolase+ (cat. no. NM-0019; 1:100 dilution) and D2-40−
(cat. no. DM-0011; 1:100 dilution). Postoperative radiotherapy was
administered.
In June 2022, the patient underwent cholecystectomy
under general anesthesia with nerve block at Cangzhou People's
Hospital (Cangzhou, China). Intraoperative exploration revealed
adhesions between the omentum and gallbladder, with no thickening
of the common bile duct and no palpable calculi. A medium-sized
mass measuring ~5×3×3 cm was palpable at the bottom of the
gallbladder, but it did not invade the surrounding tissues. Visual
inspection indicated that the gallbladder had a size of 7×4×3 cm
and had been previously incised. A mass, measuring 5×4×3 cm, was
observed in the cyst at the bottom of the gallbladder, with a soft
and tough cut surface and focal necrosis.
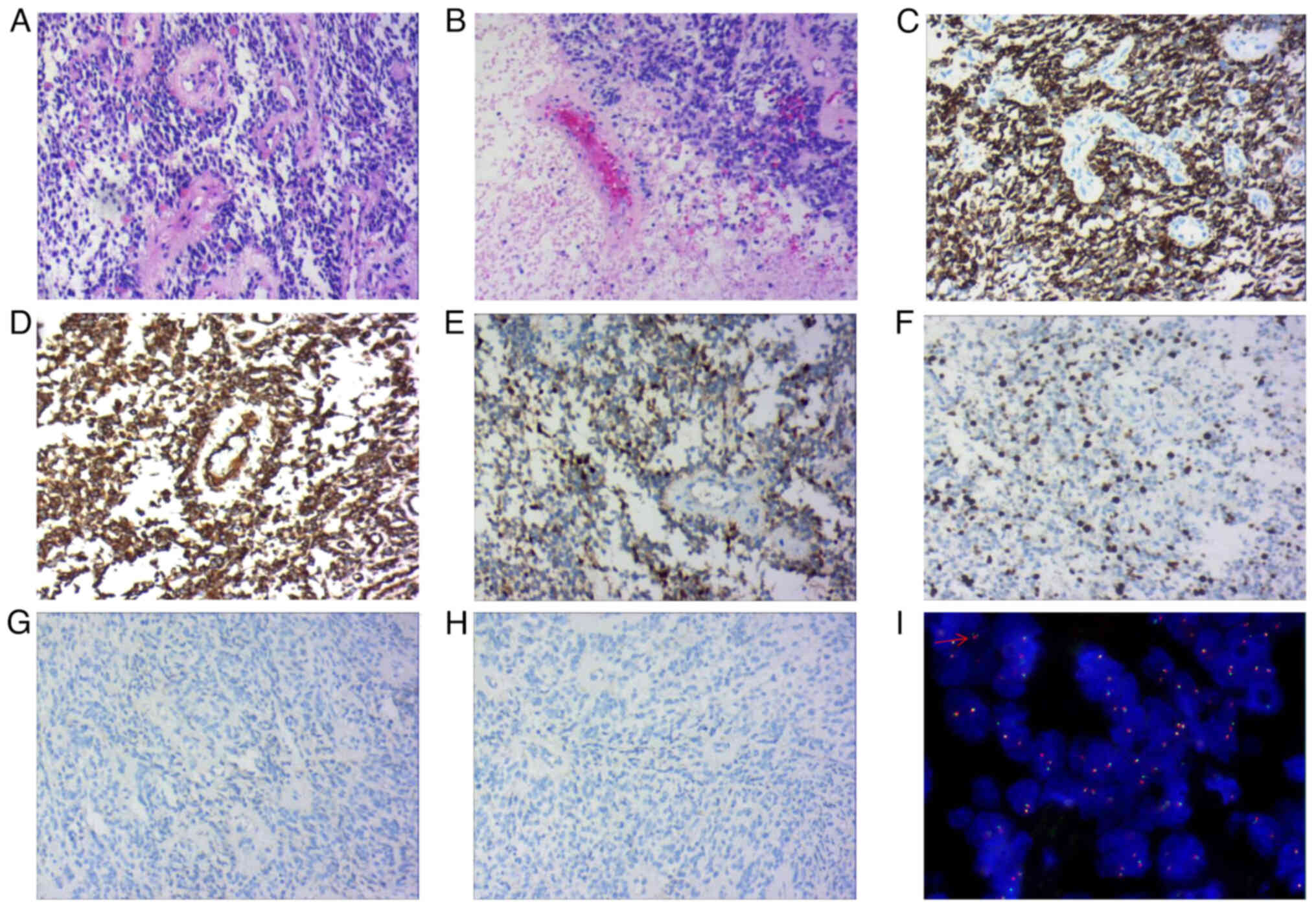
Histological examination (samples were prepared
using the Ventura BenchMark ULTRA staining procedure; all reagents
were from Roche Diagnostics) revealed the presence of round or oval
monomorphic cells of uniform size within the tumor tissue. Numerous
tumor cells formed a pseudo rosette-like structure around blood
vessels. Immunohistochemistry (May 2022) results showed that the
mass was GFAP+ (cat. no. GM-0031; 1:100 dilution),
Vimentin+ (cat. no. VM-0031; 1:100 dilution), Ki67
(index ~10%; cat. no. KM-0021; 1:100 dilution), partially
S-100+ (cat. no. SM-0011; 1:100 dilution),
EMA− (cat. no. EM0-0041; 1:100 dilution),
CD56+ (cat. no. CRM-0351; 1:100 dilution),
neuron-specific enolase+ (cat. no. NM-0019; 1:100
dilution; all from Shanghai Jiehao Biotechnology Co., Ltd.),
β-catenin+ (Qiagen; cat. no. BM-0267; 1:100 dilution)
and cytokeratin− (CK; cat. no. CM-0641; 1:100 dilution;
Shanghai Jiehao Biotechnology Co., Ltd.) (Fig. 3A-H). Molecular detection using the
C11orf95 zinc finger translocation associated (ZFTA)-RELA
proto-oncogene fusion probe indicated positive fluorescence in
situ hybridization expression (Fig.
3I; Appendix S1). At the same
time, tumor markers related to differential diagnosis (lymphatic
tissue tumors, vascular-derived tumors, biliary epithelial tumors,
myoepithelial derived tumors and neuroendocrine tumors), including
leukocyte common antigen− (cat. no. LM-0032; 1:100
dilution), CD31− (cat. no. CM-0251; 1:100 dilution),
CD34− (cat. no. CM-0271; 1:100 dilution),
CK19− (cat. no. CM-0621; 1:100 dilution),
SMA− (cat. no. AM-0051; 1:100 dilution),
calponin− (cat. no. CM-0081; 1:100 dilution) and
CD99− (cat. no. CM-0211; 1:100 dilution; all from
Shanghai Jiehao Biotechnology Co., Ltd.) (May 2022), were
investigated. Through these immunohistochemistry methods, diseases
such as primary gallbladder adenocarcinoma, angiosarcoma and
lymphoma were excluded.
The pathological diagnosis indicated metastatic
anaplastic ependymoma of the gallbladder (WHO grade III). The
patient was followed up for 10 months after surgery and received
targeted treatment at another hospital (Tianjin Medical University
Cancer Institute Hospital; Tianjin, China). At present, the tumor
has metastasized to the lungs and bones.
Discussion
Ependymoma is a rare primary tumor of the central
nervous system that arises from ependymal cells and primarily
affects young adults and children (1). The most common site of occurrence is
the fourth ventricle, followed by the central canal of the spinal
cord (8). It rarely occurs outside
the cranial or spinal cord, with the sacrococcygeal region being
the most frequent extracranial location (9). Other sites of occurrence include the
ovaries, mediastinum, uterine ligaments, uterine rectal space and
omentum (9).
According to the 2016 WHO classification criteria,
subependymomas and mucopapillary ependymomas are classified as
grade I, ependymomas as grade II and anaplastic ependymomas as
grade III (8). The key diagnostic
features in terms of pathomorphology are perivascular pseudo
rosette-like structures, nodular growth patterns and ependymal
rosette-like structures or fissures. Mitotic figures are uncommon,
while atypia is occasionally observed. Sex nuclei degeneration is
frequently present and necrosis is relatively common (8).
In clinical practice, metastasis to the gallbladder
is infrequent. Specifically, malignant melanoma is the most common
primary tumor that metastasizes to the gallbladder, accounting for
15% of cases (10,11). Renal cell cancers, lung cancers,
cervical cancers and breast cancers can also lead to secondary
metastasis to the gallbladder, although they are less common
(12). Only a small number of cases
of metastasis to the gallbladder have been documented in the
literature (12,13). Metastasis to the gallbladder
typically presents with symptoms resembling acute/chronic
cholecystitis or complaints such as abdominal pain (14–16).
There have been no reports of ependymoma metastasis
to the gallbladder. Unlike previously reported cases (12), the present case was identified
through physical examination. Due to the rarity of metastatic
ependymoma in the gallbladder and the absence of specific clinical
and imaging findings, diagnosis without a clear medical history has
been challenging (12). Therefore,
molecular biology and immunohistochemical evaluation are often
necessary. Risk factors for dissemination and metastasis of
ependymoma include younger age, incomplete tumor resection,
high-grade or mucopapillary ependymoma and a higher tumor
proliferation index, among others (17).
Patients with gallbladder metastasis may experience
abdominal pain, cholangitis, bile peritonitis or cholestasis.
Histopathological examination facilitates the establishment of a
diagnosis, as abdominal imaging has limited diagnostic value. Due
to the poor condition of the patient after gallbladder metastasis,
palliative treatment was adopted with a focus on alleviating the
patient's symptoms. One report indicated that gallbladder
metastasis accounted for 4.8% of all gallbladder malignancies
(18). The prognosis for patients
with gallbladder metastasis who undergo radical resection is
favorable. However, patients primarily presenting with acute
cholecystitis as a result of gallbladder metastasis have a poorer
prognosis (19). Clinicians should
remain aware of gallbladder metastasis in patients with malignant
tumors exhibiting biliary symptoms. The present study had certain
limitations, mainly as the technology used could not provide
detailed molecular typing of ependymoma, such as Yes-associated
protein 1 fusion-positive and ZFTA fusion, which are closely
associated with biological behavior and clinical prognosis
(20).
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during this study
are available from the corresponding author on reasonable
request.
Authors' contributions
XYH and ZGZ were involved in the conception and
design of the study; QMS and SS performed imaging analyses; HZL and
SLH completed the FISH detection; XYH and ZGZ confirm the
authenticity of all the raw data. All authors have read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient provided written informed consent for
the publication of any data and/or accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
McGuire CS, Sainani KL and Fisher PG:
Incidence patterns for ependymoma: A surveillance, epidemiology,
and end results study. J Neurosurg. 110:725–729. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wani K, Armstrong TS, Vera-Bolanos E,
Raghunathan A, Ellison D, Gilbertson R, Vaillant B, Goldman S,
Packer RJ, Fouladi M, et al: A prognostic gene expression signature
in infratentorial ependymoma. Acta Neuropathol. 123:727–738. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Missori G, Serra F, Prestigiacomo G,
Ricciardolo AA, Brugioni L and Gelmini R: Case report: Metastatic
breast cancer to the gallbladder. F1000Res. 9:3432020. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chung PH, Srinivasan R, Linehan WM, Pinto
PA and Bratslavsky G: Renal cell carcinoma with metastases to the
gallbladder: Four cases from the national cancer institute (NCI)
and review of the literature. Urol Oncol. 30:476–481. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zagouri F, Sergentanis TN, Koulocheri D,
Nonni A, Bousiotou A, Domeyer P, Michalopoulos NV, Dardamanis D,
Konstadoulakis MM and Zografos GC: Bilateral synchronous breast
carcinomas followed by a metastasis to the gallbladder: Acase
report. World J Surg Oncol. 5:1012007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ma Y, Li GY and Chen G: A case of
long-term gallbladder metastasis after primary liver cancer
surgery. Chinese J Surg. 59:22021.
|
|
7
|
Yu S, Wang TK, Chen BY, et al: Diagnosis
and treatment of 2 cases of metastatic tumors of the gallbladder
and literature review. J Hepatopancreatobiliary Surg. 30:32018.
|
|
8
|
Louis DN, Perry A, Reifenberger G, von
Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD,
Kleihues P and Ellison DW: The 2016 world health organization
classification of tumors of the central nervous system: A summary.
Acta Neuropathol. 131:803–820. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chen YR, Lin JM, Li J, et al: Uterine
broad ligament ependymoma: A case report and literature review.
Progress Obstet Gynecol. 26:22017.
|
|
10
|
Lee YT: Breast carcinoma: Pattern of
metastasis at autopsy. J Surg Oncol. 23:175–180. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Langley RG, Bailey EM and Sober AJ: Acute
cholecystitis from metastatic melanoma to the gall-bladder in a
patient with a low-risk melanoma. Br J Dermatol. 136:279–282. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Shah RJ, Koehler A and Long JD: Bile
peritonitis secondary to breast cancer metastatic to the
gallbladder. Am J Gastroenterol. 95:1379–1381. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Abdelilah B, Mohamed O, Yamoul R, Elkhiyat
I, Al Bouzidi A, Alkandry S and Abdelkader E: Acute cholecystitis
as a rare presentation of metastatic breast carcinoma of the
gallbladder: A case report and review of the literature. Pan Afr
Med J. 17:2162014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Calafat P, de Diller AB and Sanchez C:
Metástasis de carcinoma de mama en ileon-colon y vesicula biliar
simulando enfermedades inflamatorias (Breast carcinoma metastasis
in ileum-colon and gallbladder simulating inflammatory diseases).
Rev Fac Cien Med Univ Nac Cordoba. 56:123–127. 1999.(In Spanish).
PubMed/NCBI
|
|
15
|
Borst MJ and Ingold JA: Metastatic
patterns of invasive lobular versus invasive ductal carcinoma of
the breast. Surg. 114:637–641. 1993.PubMed/NCBI
|
|
16
|
Murguia E, Quiroga D, Canteros G,
Sanmartino C, Barreiro M and Herrera J: Gallbladder metastases from
ductal papillary carcinoma of the breast. J Hepatobiliary Pancreat
Surg. 13:591–593. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Markelov A, Taheri H, Vunnamadala K and
Ibrahim G: Biliary dyskinesia as a rare presentation of metastatic
breast carcinoma of the gallbladder: A case report. Case Rep
Pathol. 2011:8065702011.PubMed/NCBI
|
|
18
|
Yoon WJ, Yoon YB, Kim YJ, Ryu JK and Kim
YT: Metastasis to the gallbladder: A single-center experience of 20
cases in South Korea. World J Gastroenterol. 15:4806–4809. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Doval DC, Bhatia K, Pavithran K, Sharma
JB, Vaid AK and Hazarika D: Breast carcinoma with metastasis to the
gallbladder: An unusual case report with a short review of
literature. Hepatobiliary Pancreat Dis Int. 5:305–307.
2006.PubMed/NCBI
|
|
20
|
Bale TA and Rosenblum MK: The 2021 WHO
classification of tumors of the central nervous system: An update
on pediatric low-grade gliomas and glioneuronal tumors. Brain
Pathol. 32:e130602022. View Article : Google Scholar : PubMed/NCBI
|