Introduction
The treatments for hepatocellular carcinoma (HCC)
are diverse and multidisciplinary. While multi-modal therapies are
available for HCC, therapy is determined on the basis of tumor- and
patient-related factors, including liver function (1,2).
Recently, owing to advances in radiotherapy (RT), there have been
numerous reports of the efficacy of particle beam treatment, such
as carbon-ion RT (C-ion RT) and proton beam RT for HCC (3–7).
However, to the best of our knowledge, there are no prospective
studies regarding the treatment outcomes of particle beam therapy
for solitary and small HCCs for which resection or radiofrequency
ablation (RFA) is recommended. Additionally, C-ion RT and proton
beam RT are performed mainly for recurrent cases and for patients
with poor liver function who cannot tolerate surgery. To the best
of our knowledge, there are no reports of surgical resection for
local recurrence after these RTs. Therefore, the long-term outcomes
and clinical and pathological features of locoregional recurrence
after initial treatment by particle beam therapy are still
unclear.
The present study reports the case of a patient who
underwent a curative laparoscopic liver resection for a local
recurrence of HCC after C-ion RT. The study presents the
intraoperative features and histopathological findings of this
locoregional recurrent tumor and the surrounding liver parenchyma
after initial C-ion RT.
Case report
A 73-year-old man was referred to Department of
Surgery in Saga University Hospital (Saga, Japan) in September 2022
for recurrence of HCC in segment 7 (S7) after C-ion RT, which was
performed 16 months earlier in May 2021 as an initial treatment.
Approximately 15 years earlier, the patient was diagnosed as
hepatitis C virus-positive, and antiviral therapy with pegylated
interferon-α2b and oral ribavirin (pegylated interferon-α2b, 80
µg/week, oral ribavirin: 600 mg/day) for 24 weeks was administered
5 years after the diagnosis. A sustained virological response was
achieved with this treatment, and the patient underwent regular
examinations including physical examination, blood test and
abdominal ultrasonography, at the Department of Hepatology in Saga
University Hospital, thereafter. A total of 8 years after first
achieving a sustained virological response, the initial HCC was
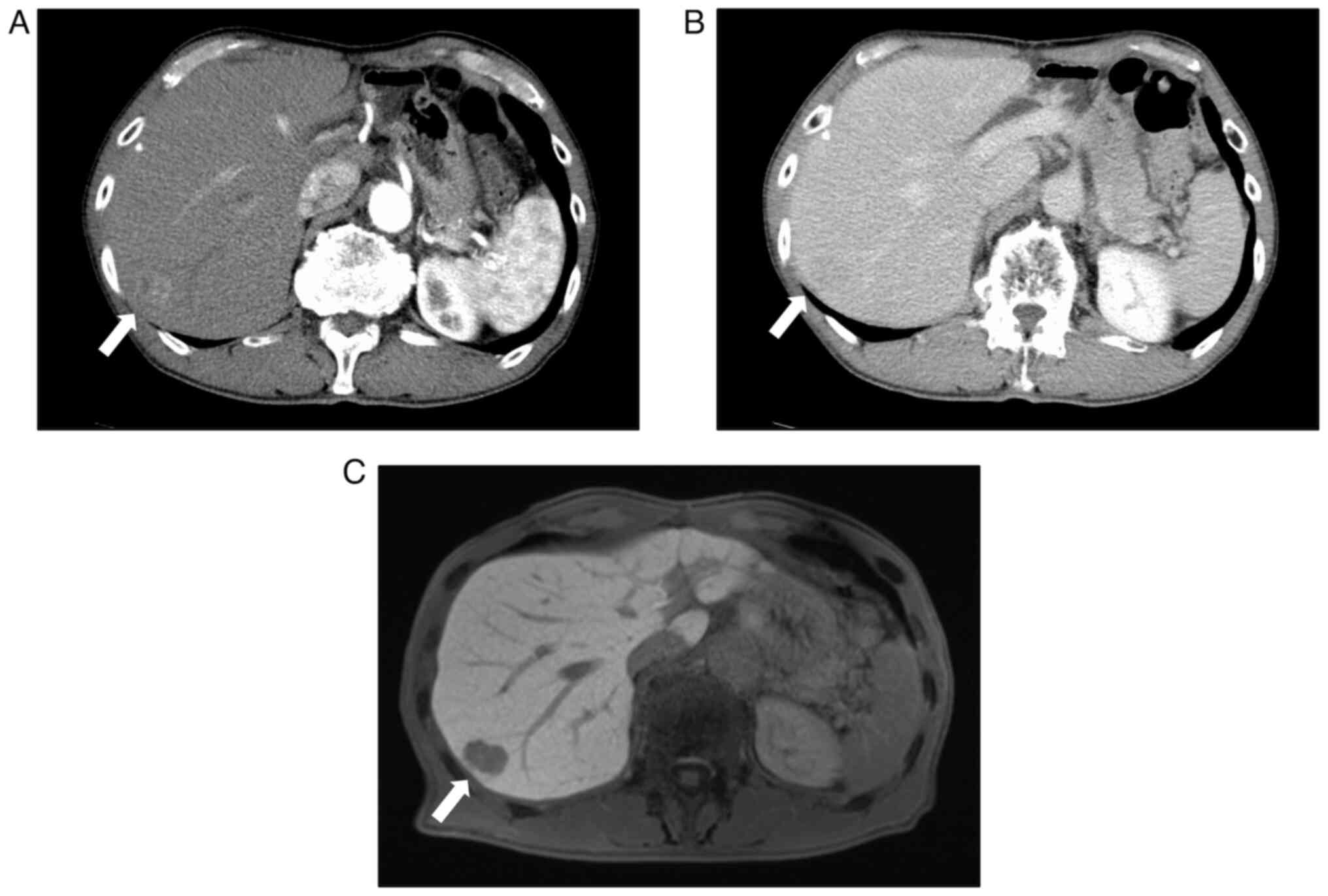
detected by imaging examinations in March 2021. Contrast-enhanced
computed tomography (CT) showed an 18-mm lesion on the surface of
liver S7 that was heterogeneously enhanced in the arterial phase
and washed out in the delayed phase (Fig. 1A and B).
Gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic
acid-enhanced magnetic resonance imaging (EOB-MRI) showed no EOB
uptake in the tumor (Fig. 1C). At
that point, the HCC was diagnosed as T1aN0M0, stage IA, in
accordance with the Union for International Cancer Control 8th
edition (8), indicating that the
tumor was amenable to radical surgical resection. The patient's
general condition was stable, liver function was well preserved,
the Child-Pugh grade (9) was A, the
albumin-bilirubin grade (10) was 1
and there were no severe comorbidities; however, the patient opted
for C-ion RT as the initial treatment for the HCC. After completing
the schedule of C-ion RT (a dose of 60 Gy in 4 fractions within a
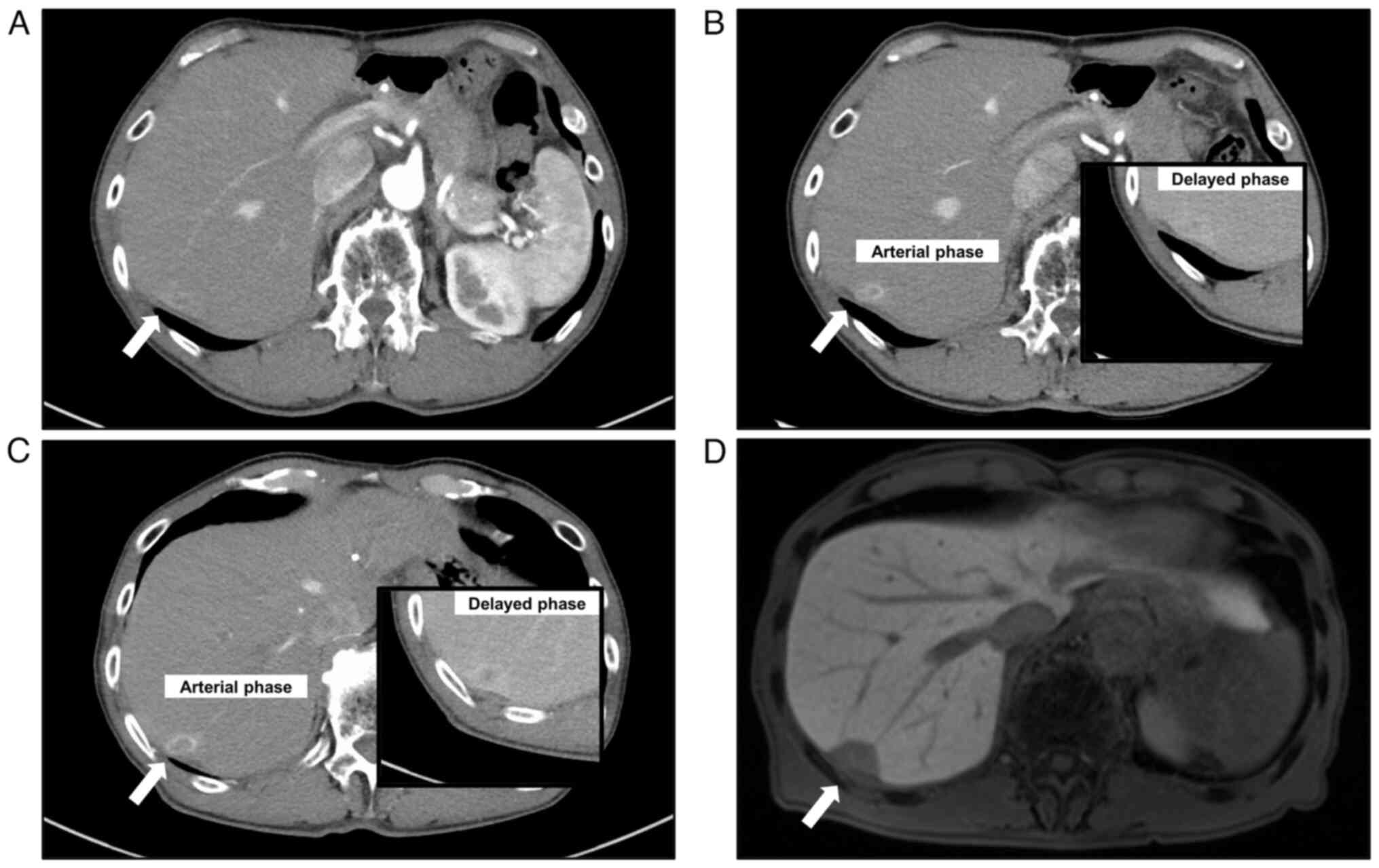
9-day time period), the patient received follow-up CT every 4
months, which confirmed post-treatment changes in the tumor
location (Fig. 2A). The tumor
lesion shrank to a nodule of ~10-mm with a surrounding low-density
area, and a delayed enhancement effect was observed, consistent
with changes after C-ion RT. Blood test results showed that levels
of both α-fetoprotein and protein induced by vitamin K absence
(PIVKAII), which are tumor markers for HCC, were within the normal
ranges (α-fetoprotein: 2.0 ng/ml [normal range: 0–10 ng/ml],
PIVKAII: 19 mAU/ml [normal range: 0–40 mAU/ml]), and the
hepatobiliary enzyme levels were not elevated (AST: 25 IU/l [normal
range: 13–30 IU/l], ALT: 9 IU/l [normal range: 10–42 IU/l), ALP: 78
IU/l [normal range: 38–113 IU/l], γ-GTP: 22 IU/l [normal range:
13–64 IU/l]). However, recurrence was suspected, as CT performed 16
months after C-ion RT revealed an area with a distorted shape that
was ring-enhanced in the arterial phase and washed out in the
delayed phase within the previously irradiated area of S7 (Fig. 2B). Short-term follow-up CT, which
was conducted 1 month after the most recent CT and 18 months after
C-ion RT, revealed that the area suspected as recurrence had
clearly enlarged, and the ring enhancement was stronger compared
with that in the previous CT images (Fig. 2C). As another modality, EOB-MRI
revealed a mass lesion on the surface of liver S7 that was
hyperintense on T2-weighted/fat-suppressed imaging and
diffusion-weighted imaging. Moreover, the lesion showed ring
enhancement in the early phase and wash out in the delayed phase on
dynamic study, and hypointensity, including the area around the
lesion, in the hepatobiliary phase, with EOB (Fig. 2D). At the 16-month visit when the
recurrence was first observed, both α-fetoprotein and PIVKAII
levels in the blood test were within the normal ranges and were not
elevated in comparison with previous data (α-fetoprotein, 1.6
ng/ml, PIVKAII: 17 mAU/ml). On the basis of the CT and MRI
findings, atypical recurrence of HCC after C-ion RT was diagnosed.
At this time, the attending hepatologist recommended a surgical
resection for the recurrent HCC, and the patient strongly desired
this approach. Regarding preoperative liver function, the
indocyanine green (ICG) retention rate at 15 min, whose normal
reference range is from 0 to 10%, was 16.2%. Additionally, the
Child-Pugh classification and albumin-bilirubin score were grade A
and grade 1, respectively, indicating that the patient could
tolerate surgery. Therefore, a laparoscopic partial liver resection
of S7 was performed in November 2022. The extent of the liver
resection was designed to include the area affected by the C-ion
RT. Regarding the potential of a biopsy before surgery, firstly the
hepatologist determined that a biopsy would be somewhat difficult
due to the location of the tumor. Furthermore, as the tumor was
small and its boundaries were unclear, the recurrence of HCC could
not be ruled out even if malignant cells were not detected by the
biopsy. Based on this, a decision was made to judge recurrence
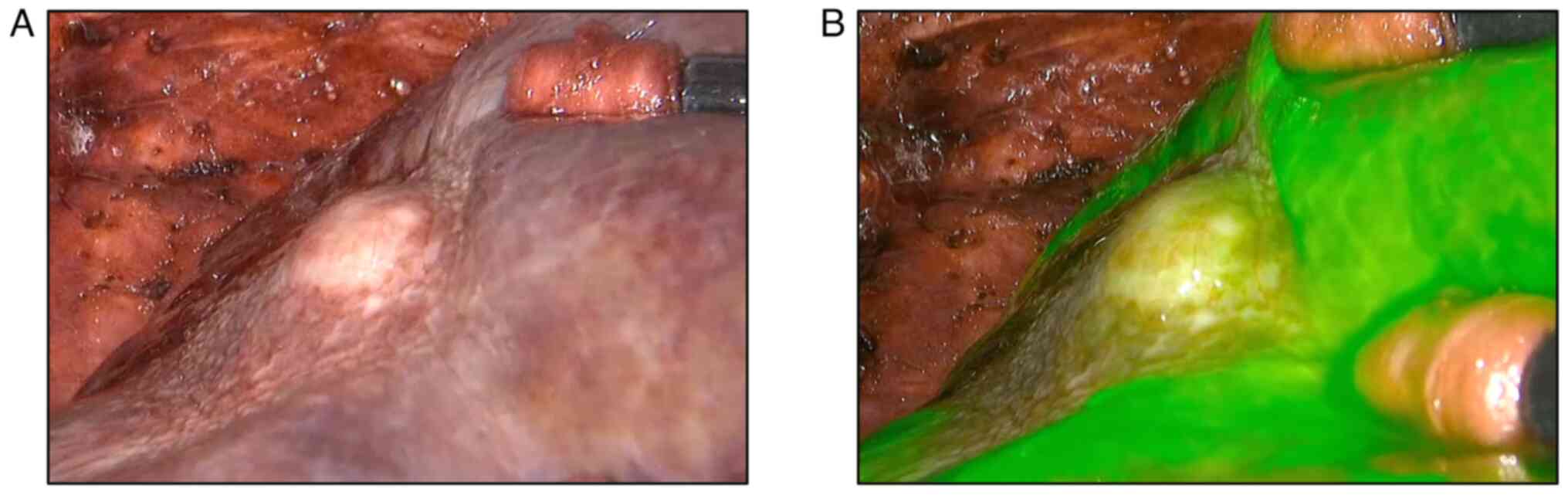
based on the imaging findings. Intraoperatively, the liver surface
above the tumor in S7 was depressed (delle), and atrophy and
fibrosis were observed around the lesion (Fig. 3A). Fluorescence imaging
(PINPOINT® Endoscopic Fluorescence Imaging System;
Stryker Corporation) revealed that ICG uptake was weaker in the
tumor and its surroundings than that in the normal parenchyma,
unlike that found in typical HCC (Fig.
3B). The designed liver resection was completed successfully
laparoscopically. Blood loss was 50 ml and the operating time was
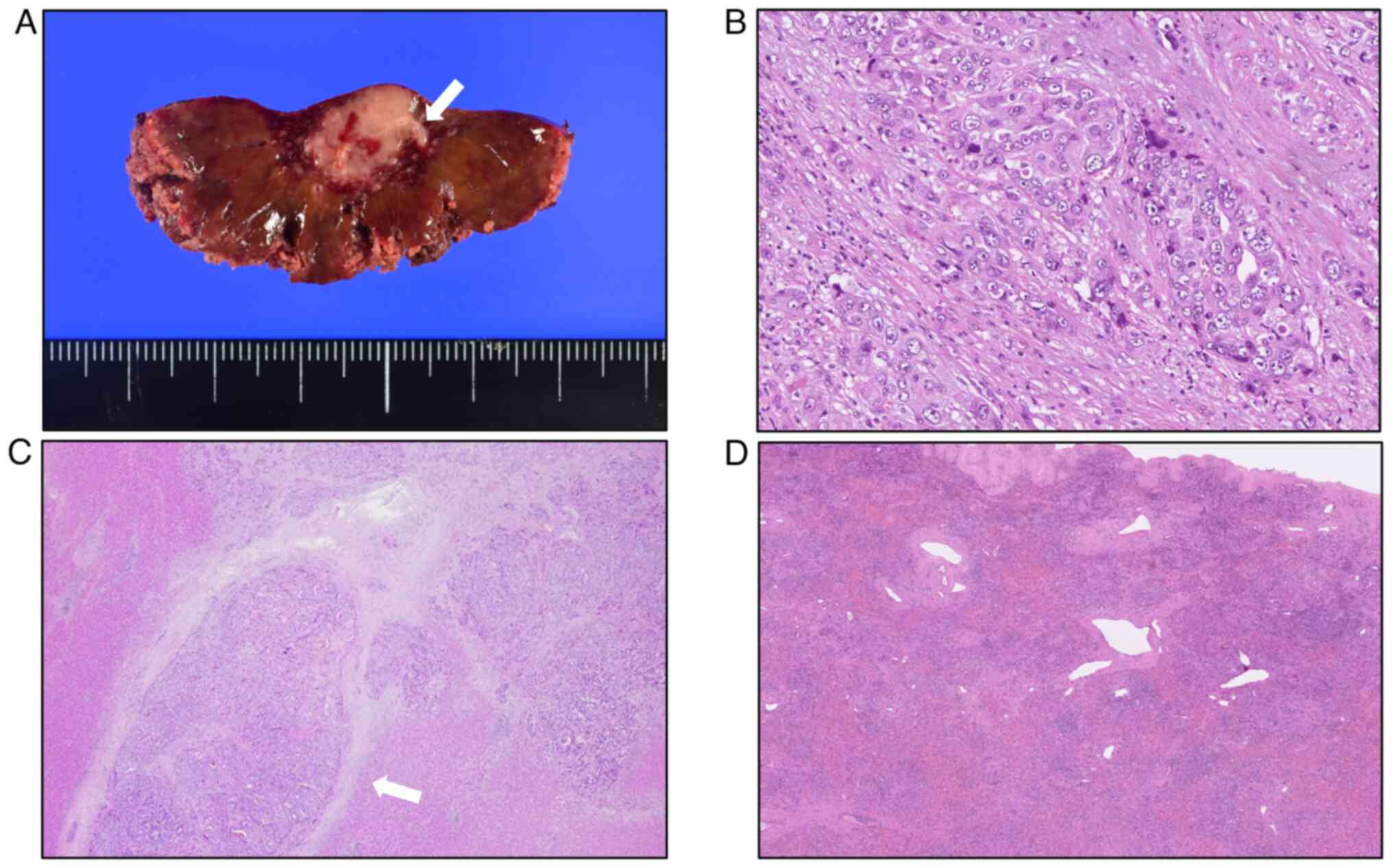
275 min. The cut surface of the resected specimen revealed a
whitish solid tumor with irregular borders measuring 15.3×13.4 mm
in diameter (Fig. 4A). The resected
specimens were fixed with 10% neutral buffered formalin for 24 h at
room temperature. Formalin-fixed paraffin-embedded tissue was
sectioned at a thickness of 4 µm and stained with hematoxylin and
eosin (H&E). The H&E-stained slides were scanned and
converted to digital slides by NanoZoomer S360 (Hamamatsu Photonics
K.K.). Presented figures were obtained by digital slides.
Histologically, proliferation of moderately differentiated HCC
showing marked nuclear atypia was observed (Fig. 4B). The tumor showed an invasive
growth pattern without a fibrous capsule between the tumor and the
surrounding liver parenchyma, and numerous portal vein invasions
were observed (Fig. 4C). The liver
parenchyma around the tumor was collapsed owing to the loss of
hepatocytes, and abundant infiltration of inflammatory cells in
both the portal tract and hepatic lobules, with reactive
cholangiolar proliferation, was observed (Fig. 4D). These liver parenchymal findings
were considered the effects of C-ion RT. The surgical margins were
negative and an R0 resection was confirmed. Based on the
pathological findings, the final stage of the tumor was T1aN0M0,
stage IA, in accordance with the Union for International Cancer
Control 8th edition.
Postoperatively, the patient experienced no
complications and was discharged on day 9. The patient visited the
outpatient clinic every 3 months thereafter. An enhanced CT was
performed each visit to check for recurrence, and tumor markers,
such as α-fetoprotein and PIVKAII, were measured. There was no
recurrence up to 13 months after surgery. Patient will continue to
be followed up every 3 months to check for recurrence.
Discussion
The present study reports a case of curative
laparoscopic liver resection for local recurrence of HCC after
C-ion RT as the initial treatment. To the best of our knowledge,
this is the first report of such a specific therapeutic
process.
C-ion RT is a promising modality in RT that allows
higher dose localization and relative biological efficacy compared
with X-ray RT (11,12). Additionally, as C-ion RT has a
‘Bragg peak’, meaning an energy distribution in penetration depth,
it is characterized by minimal damage to the normal cells
surrounding the treatment target (13). Previous studies have reported that
C-ion RT is associated with better sparing of the surrounding
normal liver compared with stereotactic body RT (14,15).
Considering these physical and biological advantages, C-ion RT is
well tolerated in patients with HCC who are older, fragile, and/or
who have severe comorbidities or poor liver function (16,17).
Thus, C-ion RT may be a treatment option even for small and
solitary HCC, for which surgical resection or RFA is recommended,
if the patient cannot tolerate these treatments. Therefore,
surgical resection is extremely rare for local recurrence after
C-ion RT. From this point of view, the current case is valuable to
clarify the long-term outcomes or intraoperative findings and
pathological features of locoregional recurrence after initial
C-ion RT.
In the present case, CT at recurrence showed a clear
increase in tumor size over a short period of time, while
depression of the liver surface above the tumor, and communication
between the tumor and the portal vein were observed, suggesting HCC
with high malignant potential. Huang et al (18) reported the surgical findings of two
patients who underwent living donor liver transplantation for HCC
recurrence after C-ion RT. Severe atrophy of the liver parenchyma
was found in the irradiated area, and the tissues adjacent to the
irradiated area were strongly adhered, which resulted in difficulty
with adhesiolysis during surgery. These changes following C-ion RT
increase surgical difficulty, and adhesiolysis to address strong
adhesions poses the risk of cancer dissemination. In the present
case, severe atrophy and fibrosis were observed in the irradiated
area during surgery. However, no adhesions were observed between
the irradiated area and the diaphragm, and laparoscopic resection
was completed without intraoperative complications. Additionally,
in this case, the liver surface above the tumor had a delle. These
changes were considered to be effects of C-ion RT and also may have
indicated HCC with high malignant potential. Regarding the ICG
uptake, it was hypothesized that accumulation did not occur, as the
liver parenchyma around the tumor was markedly collapsed by the
loss of hepatocytes.
Histopathologically, studies have shown that tumors
measuring ≤2 cm have poor growth of the tumor vasculature, and ~10%
of cases will have microvascular invasion of portal branches by the
tumor (19–22). By contrast, numerous studies have
shown that portal vein invasion is one of the strongest prognostic
factors for HCC (23). In the
present case, numerous portal vein invasions were observed despite
the small size of the tumor (15 mm). Several studies have also
shown that irradiation augments the invasiveness of some types of
cancer cells, such as non-small cell lung cancer cells (24–26).
Therefore, although pathological information before C-ion RT was
not available in the present case, we hypothesized that the
recurrent tumor after C-ion RT gained malignant potential; the
tumor showed marked invasive growth with portal vein invasion. In a
study where metastatic liver cancer from colon cancer for which
C-ion beam therapy was selected even though the tumor was
resectable, both local recurrence and massive tumor thrombi in the
portal vein and hepatic vein were reported after C-ion beam therapy
(27).
Regarding the basic concept of treatment for HCC,
radical treatment is indicated for patients with HCC and good liver
function, and the absence of high vascular invasion or distant
metastasis (1,2,28). To
achieve a safe and maximum therapeutic effect in HCC, it is
necessary to select the optimal treatment on the basis of the stage
of cancer progression and the patient's condition. In fact, liver
resection is strongly recommended for HCC measuring ≤3 cm with no
vascular invasion, according to the Japan Society of Hepatology HCC
Guidelines 2021 (1). Similarly, in
the Barcelona Clinic Liver Cancer staging and treatment strategy
(2022 version), liver resection is recommended for single HCC
without vascular invasion or extrahepatic spread in patients with
preserved liver function and no increased portal pressure or
bilirubin levels (2). The present
case involved an initial single HCC measuring 18 mm in size;
therefore, the best indication was a surgical approach. However,
the patient selected C-ion RT as the initial treatment for the HCC.
This decision was based on the fact that he had special health
insurance, which paid for the advanced medical treatment; the
national health insurance program in Japan does not cover C-ion RT.
It is an important fact that the treatment choice resulted in
recurrence with numerous portal vein invasions. Physicians involved
in the treatment of HCC should note that such cases exist.
Therefore, the present report is valuable in the sense that it
warns against the easy selection of C-ion RT for patients with HCC
for whom resection is considered optimal surgically and
functionally.
It also must be noted that there is insufficient
evidence confirming a therapeutic outcome of C-ion RT for early
stage HCC, such as Barcelona Clinic Liver Stage 0 and A, and no
studies have compared the outcomes of surgical resection and C-ion
RT for these stages of HCC. Based on current evidence for the
treatment of HCC, the standard treatment for early stage HCC is
liver resection or RFA if the patient's general condition and liver
function are preserved. In the current information-oriented
society, there is a possibility that the number of patients who
desire less invasive treatment and have excessive expectations for
C-ion RT will increase. The possibility of unusual recurrence after
C-ion RT, such as that reported in the present case, should be
considered, and sufficient informed consent should be obtained from
patients when selecting the treatment for HCC. By contrast, C-ion
RT can be a very effective treatment option, with appropriate
indications. However, currently, there is no international
guideline for the indications for C-ion RT in HCC. Additional
understanding must be gained regarding the hepatic biological and
histopathological features after C-ion RT to optimize the treatment
of HCC.
Finally, we speculate why HCC relapsed after initial
C-ion RT in this case in association with clinical and pathological
features. CT examination at the time of recurrence revealed a new
distorted area at the central region of the irradiated S7. In other
words, this clinical feature suggested that the recurrent tumor
occurred inside of the irradiated area instead of on its margins.
Regarding pathological features, histological examination of the
resected specimen showed tumor cells adjacent to scar tissue that
was considered to occur by irradiation of C-ion RT. Considering
these clinical and pathological features, although the tumor was
within the irradiated field of C-ion RT, the delivered radiation
dose may have been insufficient to completely destroy the tumor
cells. Chen et al (29)
reported that the center of the irradiated area tends to be
hypoxic, which may reduce the effectiveness of irradiation in this
region.
In conclusion, the present study described surgery
for an unusual recurrence of HCC after C-ion RT, which was
successfully treated with a laparoscopic liver resection.
Locoregional recurrence of HCC after C-ion RT could result in
highly malignant cancer with extensive portal vein invasion. In
addition to hepatocyte atrophy and fibrosis, C-ion RT may cause
severe intra-abdominal adhesions, and it is necessary to be aware
of these changes when performing surgical resection for recurrence
after C-ion RT. The present case may raise concerns about the true
efficacy of C-ion RT and indicates the importance of appropriate
treatment selection on the basis of individual patient- and
tumor-related characteristics.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author upon reasonable
request.
Authors' contributions
TT was responsible for the conception of the study
and drafting the case report. TT, TI and KI performed the surgery
and perioperative management of the patient and edited the
manuscript. TT, KI, KK and TI performed the acquisition and
analysis of data. HN advised on patient treatment. TT, TI and HN
reviewed the manuscript. TT, TI and HN confirm the authenticity of
all the raw data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient provided written informed consent for
the publication of the data.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
HCC
|
hepatocellular carcinoma
|
|
RT
|
radiotherapy
|
|
C-ion
|
carbon-ion
|
|
RFA
|
radiofrequency ablation
|
|
S7
|
segment 7
|
|
CT
|
computed tomography
|
|
EOB-MRI
|
gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic
acid-enhanced magnetic resonance imaging
|
|
PIVKAII
|
protein induced by vitamin K
absence
|
|
ICG
|
indocyanine green
|
References
|
1
|
Hasegawa K, Takemura N, Yamashita T,
Watadani T, Kaibori M, Kubo S, Shimada M, Nagano H, Hatano E,
Aikata H, et al: Clinical practice guidelines for hepatocellular
carcinoma: The Japan society of hepatology 2021 version (5th
JSH-HCC guidelines). Hepatol Res. 53:383–390. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Reig M, Forner A, Rimola J, Ferrer-Fàbrega
J, Burrel M, Garcia-Criado Á, Kelley RK, Galle PR, Mazzaferro V,
Salem R, et al: BCLC strategy for prognosis prediction and
treatment recommendation: The 2022 update. J Hepatol. 76:681–693.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bush DA, Smith JC, Slater JD, Volk ML,
Reeves ME, Cheng J, Grove R and de Vera ME: Randomized clinical
trial comparing proton beam radiation therapy with transarterial
chemoembolization for hepatocellular carcinoma: Results of an
interim analysis. Int J Radiat Oncol Biol Phys. 95:477–482. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kim TH, Koh YH, Kim BH, Kim MJ, Lee JH,
Park B and Park JW: Proton beam radiotherapy vs. radiofrequency
ablation for recurrent hepatocellular carcinoma: A randomized phase
III trial. J Hepatol. 74:603–612. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hara K, Takeda A, Tsurugai Y, Saigusa Y,
Sanuki N, Eriguchi T, Maeda S, Tanaka K and Numata K: Radiotherapy
for hepatocellular carcinoma results in comparable survival to
radiofrequency ablation: A propensity score analysis. Hepatology.
69:2533–2545. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kim N, Cheng J, Jung I, Liang J, Shih YL,
Huang WY, Kimura T, Lee VHF, Zeng ZC, Zhenggan R, et al:
Stereotactic body radiation therapy vs. radiofrequency ablation in
Asian patients with hepatocellular carcinoma. J Hepatol.
73:121–129. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shiba S, Shibuya K, Katoh H, Kaminuma T,
Miyazaki M, Kakizaki S, Shirabe K, Ohno T and Nakano T: A
comparison of carbon ion radiotherapy and transarterial
chemoembolization treatment outcomes for single hepatocellular
carcinoma: A propensity score matching study. Radiat Oncol.
14:1372019. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Brierley J, Gospodarowicz MK and Wittekind
Ch: TNM Classification of Malignant Tumours. 8th edition. John
Wiley & Sons, Inc.; Hoboken, NJ: pp. 106–112. 2017
|
|
9
|
Pugh RN, Murray-Lyon IM, Dawson JL,
Pietroni MC and Williams R: Transection of the oesophagus for
bleeding oesophageal varices. Br J Surg. 60:646–649. 1973.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Johnson PJ, Berhane S, Kagebayashi C,
Satomura S, Teng M, Reeves HL, O'Beirne J, Fox R, Skowronska A,
Palmer D, et al: Assessment of liver function in patients with
hepatocellular carcinoma: A new evidence-based approach-the ALBI
grade. J Clin Oncol. 33:550–558. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shibuya K, Ohno T, Katoh H, Okamoto M,
Shiba S, Koyama Y, Kakizaki S, Shirabe K and Nakano T: A
feasibility study of high dose hypofractionated carbon ion
radiation therapy using four fractions for localized hepatocellular
carcinoma measuring 3 cm or larger. Radiother Oncol. 132:230–235.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kasuya G, Kato H, Yasuda S, Tsuji H,
Yamada S, Haruyama Y, Kobashi G, Ebner DK, Okada NN, Makishima H,
et al: Progressive hypofractionated carbon-ion radiotherapy for
hepatocellular carcinoma: Combined analyses of 2 prospective
trials. Cancer. 123:3955–3965. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kato H, Tsujii H, Miyamoto T, Mizoe JE,
Kamada T, Tsuji H, Yamada S, Kandatsu S, Yoshikawa K, Obata T, et
al: Results of the first prospective study of carbon ion
radiotherapy for hepatocellular carcinoma with liver cirrhosis. Int
J Radiat Oncol Biol Phys. 59:1468–1476. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Abe T, Saitoh J, Kobayashi D, Shibuya K,
Koyama Y, Shimada H, Shirai K, Ohno T and Nakano T: Dosimetric
comparison of carbon ion radiotherapy and stereotactic body
radiotherapy with photon beams for the treatment of hepatocellular
carcinoma. Radiat Oncol. 10:1872015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Shiba S, Shibuya K, Kawashima M, Okano N,
Kaminuma T, Okamoto M, Kubota Y, Nakano T and Ohno T: Comparison of
dose distributions when using carbon ion radiotherapy versus
intensity modulated radiotherapy for hepatocellular carcinoma with
macroscopic vascular invasion: A retrospective analysis. Anticancer
Res. 40:459–464. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Shiba S, Abe T, Shibuya K, Katoh H, Koyama
Y, Shimada H, Kakizaki S, Shirabe K, Kuwano H, Ohno T and Nakano T:
Carbon ion radiotherapy for 80 years or older patients with
hepatocellular carcinoma. BMC Cancer. 17:7212017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shiba S, Shibuya K, Katoh H, Koyama Y,
Okamoto M, Abe T, Ohno T and Nakano T: No deterioration in clinical
outcomes of carbon ion radiotherapy for sarcopenia patients with
hepatocellular carcinoma. Anticancer Res. 38:3579–3586. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Huang Y, Hidaka M, Takatsuki M, Soyama A,
Adachi T, Ono S, Kugiyama T, Hara T, Okada S, Yoshimoto T, et al:
Surgical findings and technical knacks to performing living donor
liver transplantation for hepatocellular carcinoma recurrence after
carbon ion radiotherapy. J Surg Case Rep. 2018:rjy2282018.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kojiro M and Nakashima O: Histopathologic
evaluation of hepatocellular carcinoma with special reference to
small early stage tumors. Semin Liver Dis. 19:287–296. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Maeda T, Takenaka K, Taguchi K, Kajiyama
K, Shirabe K, Shimada M, Tsuneyoshi M and Sugimachi K:
Clinicopathological characteristics of surgically resected minute
hepatocellular carcinomas. Hepatogastroenterology. 47:498–503.
2000.PubMed/NCBI
|
|
21
|
Nakashima Y, Nakashima O, Tanaka M, Okuda
K, Nakashima M and Kojiro M: Portal vein invasion and intrahepatic
micrometastasis in small hepatocellular carcinoma by gross type.
Hepatol Res. 26:142–147. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Okusaka T, Okada S, Ueno H, Ikeda M,
Shimada K, Yamamoto J, Kosuge T, Yamasaki S, Fukushima N and
Sakamoto M: Satellite lesions in patients with small hepatocellular
carcinoma with reference to clinicopathologic features. Cancer.
95:1931–1937. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kokudo T, Hasegawa K, Matsuyama Y,
Takayama T, Izumi N, Kadoya M, Kudo M, Ku Y, Sakamoto M, Nakashima
O, et al: Survival benefit of liver resection for hepatocellular
carcinoma associated with portal vein invasion. J Hepatol.
65:938–943. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ishihara S, Haga H, Yasuda M, Mizutani T,
Kawabata K, Shirato H and Nishioka T: Integrin beta1-dependent
invasive migration of irradiation-tolerant human lung
adenocarcinoma cells in 3D collagen matrix. Biochem Biophys Res
Commun. 396:651–655. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Tsutsumi K, Tsuda M, Yazawa N, Nakamura H,
Ishihara S, Haga H, Yasuda M, Yamazaki R, Shirato H, Kawaguchi H,
et al: Increased motility and invasiveness of tumor cells that
survived 10 Gy irradiation. Cell Struct Funct. 34:89–96. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Nishioka T, Yasuda M, Tsutsumi K, Haga H
and Shirato H: Matrixmetalloproteinases: Up-regulated in subclones
that survived 10-Gy irradiation. Radiat Med. 25:430–431. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Hokuto D, Nomi T and Yamato I: Colorectal
liver metastasis resected in a salvage operation for local
recurrence after proton beam radiotherapy. Jpn J Gastroenterol
Surg. 48:684–690. 2015. View Article : Google Scholar
|
|
28
|
Bruix J and Sherman M: American
Association for the Study of Liver Diseases: Management of
hepatocellular carcinoma: An update. Hepatology. 53:1020–1022.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chen F, Matsuo Y, Yoshizawa A, Sato T,
Sakai H, Bando T, Okubo K, Shibuya K and Date H: Salvage lung
resection for non-small cell lung cancer after stereotactic body
radiotherapy in initially operable patients. J Thorac Oncol.
5:1999–2002. 2010. View Article : Google Scholar : PubMed/NCBI
|