Introduction
Colorectal cancer (CRC) is one of the most common
cancer types in Japan. The Japanese national database reports
150,000 new cases and 50,000 deaths annually. The overall 5-year
survival rate of the disease is 71.4%, but the survival rate of
patients with distant metastases (stage IV) is 16.8% (1,2).
Worldwide, CRC is the third most common cancer and the second
leading cause of cancer-related deaths, with 1.8 million new cases
and 800,000 associated deaths annually. The overall 5-year survival
rate is 64%, but the survival rate is 17% for patients with distant
metastases (3,4). The treatment strategies for distant
metastases or postoperative recurrence after resection of primary
CRC are controversial.
At the International University of Health and
Welfare (IUHW), Shioya Hospital (Yaita, Japan), a total of 172
patients underwent resection of CRC between January 2012 and
December 2017. Among them, 10 patients had double primary CRCs and
one patient had triple primary CRCs resulting in a total of 184
CRCs consisting of 11, 34, 58, 58, 22 and 1 CRC at stages 0, I, II,
III, IV and unknown, respectively. A total of 22/172 patients were
at clinical or pathological stage IV at the time of surgery and
38/150 patients with maximal stages I–III (25.3%; 1, 10 and 27
patients at stages I, II and III, respectively) at the time of
surgery experienced postoperative recurrence. In the present study,
two cases of patients with stage IV CRC at the time of resection of
the primary tumor, and two cases of patients with stage II/III
colon cancer and liver metastasis after resection of the primary
tumors were reported. These four patients underwent resection of
the primary tumor followed by multimodal therapies, and achieved
disease-free survival (DFS) for >5 years, indicating that
patients were considered cured. Until now, there have been no case
series of potentially cured patients with CRC and distant
metastasis from a single institution. Single center study has a
merit of less variations in treatment strategies, surgical quality
and pathological diagnosis and can be a pilot study for future
multicenter studies to establish therapeutic strategies for curing
patients with recurrent CRC and distant metastasis. The current
study was approved by the Ethics Committee of the IUHW
(Nasushiobara, Japan; approval no. 22-B-43), and written informed
consent was obtained from the patients who could fully understand
the content of the present study.
Case report
Case 1
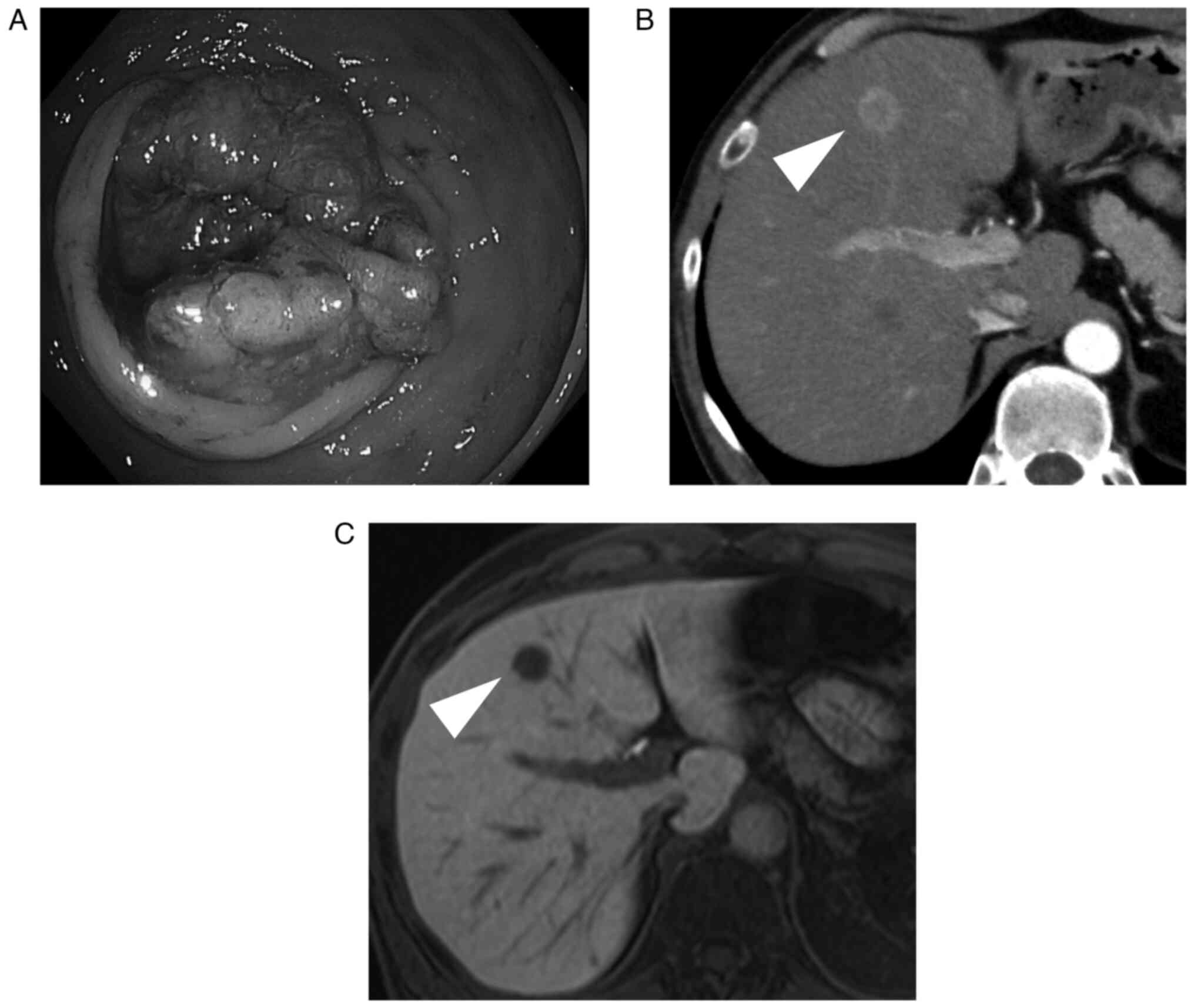
A 53-year-old male patient presented to IUHW, Shioya
Hospital (Yaita, Japan) with a diagnosis of rectal cancer in
November 2017. Contrast-enhanced computed tomography (CECT)
revealed two liver metastases [10 mm in size in segment (S)3 and 7
mm in size in S4], and the patient was diagnosed with stage IV
rectal cancer (Fig. 1A and B).
Preoperative examination revealed a mild decline in respiratory
function (Table I) (5–7). A low
anterior resection was performed initially due to bleeding from the
main tumor. Pathological examination revealed a moderately
differentiated adenocarcinoma of stage pT3N2bM1, pStage IV,
according to the American Joint Committee on Cancer TNM staging
system (8). After 2 months of
observation, imaging showed no increase in the number of liver
metastases (Fig. 1C), and a partial
hepatectomy was performed. Postoperatively, the patient was
scheduled for 6 months (10–12 courses) of treatment with folinic
acid (200 mg/m2), fluorouracil [400 mg/m2
(bolus)], fluorouracil [2,400 mg/m2 (46-h continuous
intravenous infusion)] and oxaliplatin [85 mg/m2;
(FOLFOX)], but the treatment was discontinued due to
myelosuppression after the completion of three courses of
treatment. The treatment plan was altered to capecitabine
monotherapy (3,600 mg/day) for four courses, and chemotherapy was
administered for 6 months after hepatectomy. The patient has been
alive for 1,826 days since hepatectomy without recurrence. Patient
follow-up was performed every 1–2 months at the outpatient
clinic.
 | Table I.Patient characteristics at the time of
resection of the primary tumor. |
Table I.
Patient characteristics at the time of
resection of the primary tumor.
| Patient
characteristics | Case 1 | Case 2 | Case 3 | Case 4 | Reference range |
|---|
| Age, years | 53 | 58 | 75 | 73 | NA |
| Sex | M | F | M | M | NA |
| ASA physical status
classification system | 1 | 2 | 2 | 2 | NA |
| Charlson-Deyo
comorbidity index (6) | 2 | 2 | 3 | 3 | NA |
| BMI,
kg/m2 | 21.9 | 22.2 | 23.5 | 24.2 | 18.5≤; <25 |
| EF, % | NA | NA | 81.9 | NA | ≥55 |
| FEV1, liters | 2.71 | 2.29 | 1.99 | 3.07 | NA |
| FEV1, % | 66.7 | 87.1 | 79.3 | 80 | ≥70 |
| T. Bil, mg/dl | 0.7 | 0.4 | 1.2 | 0.7 | 0.4-1.5 |
| Alb, g/dl | 4.0 | 3.8 | 4.5 | 3.7 | 4.1-5.1 |
| ICGR15, % | NA | NA | 14 | NA | ≤10 |
| Cr, mg/dl | 0.84 | 0.48 | 0.94 | 0.71 | 0.65-1.07 |
| eGFR, ml/min/1.73
m2 | 75.1 | 99.8 | 60.1 | 82.4 | ≥60 |
| HbA1c, % | 5.5 | 5.9 | 6.8 | 6.4 | 4.9-6.0 |
| Onodera's
prognostic nutrition index (7) | NA | 39.5 | 46.2 | 38.1 | NA |
| Tumor location | Rectum | Transverse
colon | Descending
colon | Sigmoid colon | NA |
| Surgery | Laparotomy | Laparotomy | Laparotomy | Laparotomy | NA |
| pT | 3 | 3 | 3 | 3 | NA |
| pN | 2b | 1 | 1 | 0 | NA |
| cM | 1 | 1 | 0 | 0 | NA |
| pStage | IV | IV | IIIB | IIA | NA |
| Histology | Moderate | Mucinous | Moderate | Moderate | NA |
| Clavien-Dindo
classification of surgical complications (8) | Surgical site
infection (Grade I) | None | None | None | NA |
Case 2
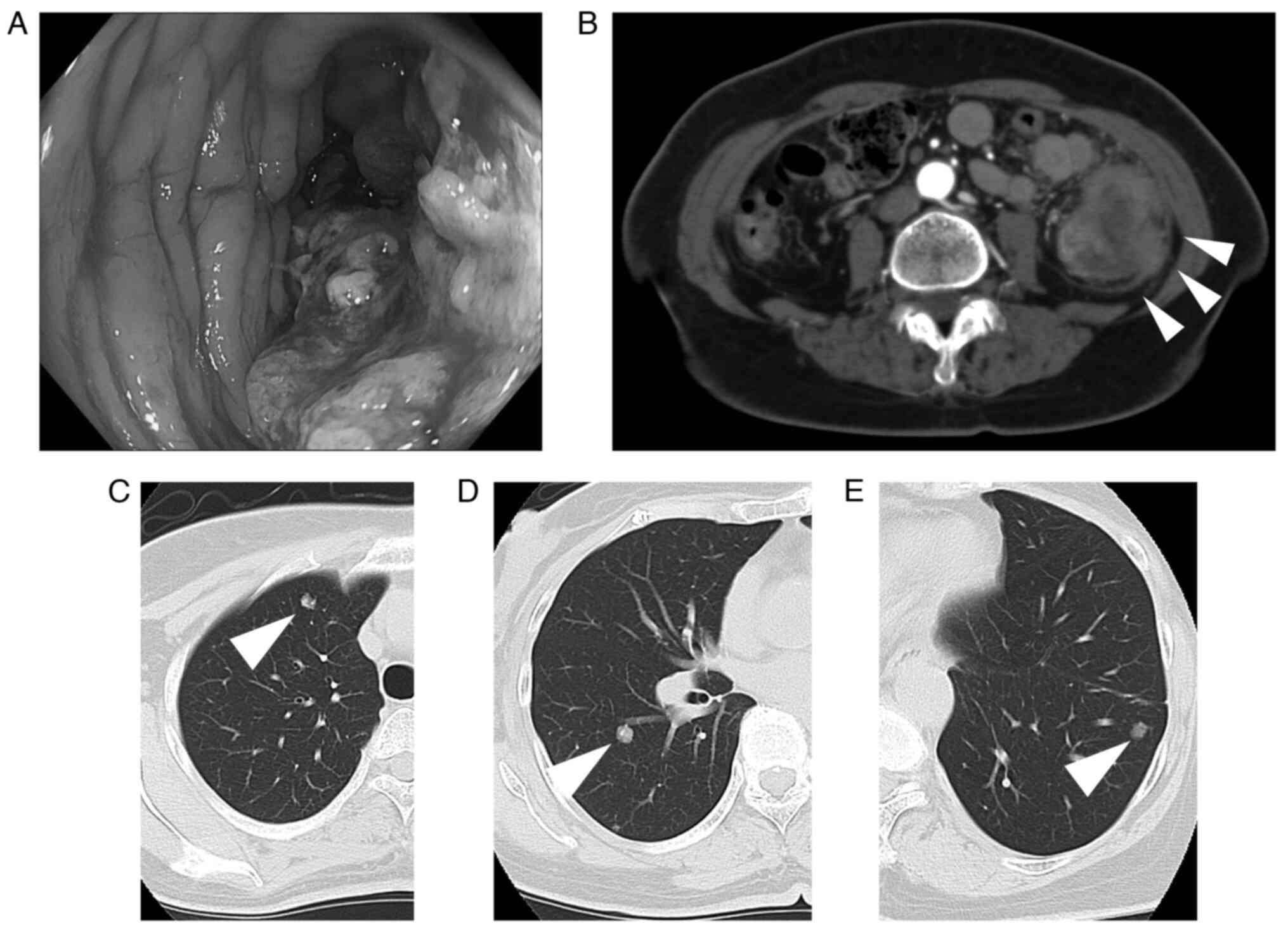
A 58-year-old female patient was referred to IUHW,
Shioya Hospital (Yaita, Japan) with a diagnosis of descending colon
cancer (Fig. 2A and B) in January
2016. CECT showed four metastases measuring 8×6, 9×9, 2×2 and 1×1
mm in the right lung (Fig. 2C and
D). The patient was diagnosed with stage IV colon cancer.
First, a partial descending colon resection was performed.
Pathological examination revealed that the tumor was a pT3N1M1,
pStage IV mucinous adenocarcinoma. Since CECT showed no new
metastatic lesions after a 5-month surveillance following initial
surgery, partial right upper and lower lobectomies were performed.
However, a new metastatic lesion, 8×6 mm in size, appeared in the
left lung 2 months later (Fig. 2E).
After a 6-month observation period, a partial left lower lobectomy
was performed. After surgery, the patient received chemotherapy
with 130 mg/m2 oxaliplatin on day 1 and 1,000
mg/m2 capecitabine, twice daily, for 2 weeks (CapeOX)
for 4 months (7 courses), but further treatment was discontinued
owing to neuralgia. The patient has been disease-free for 2,212
days since the last surgery. Patient follow-up was performed every
1–2 months at the outpatient clinic.
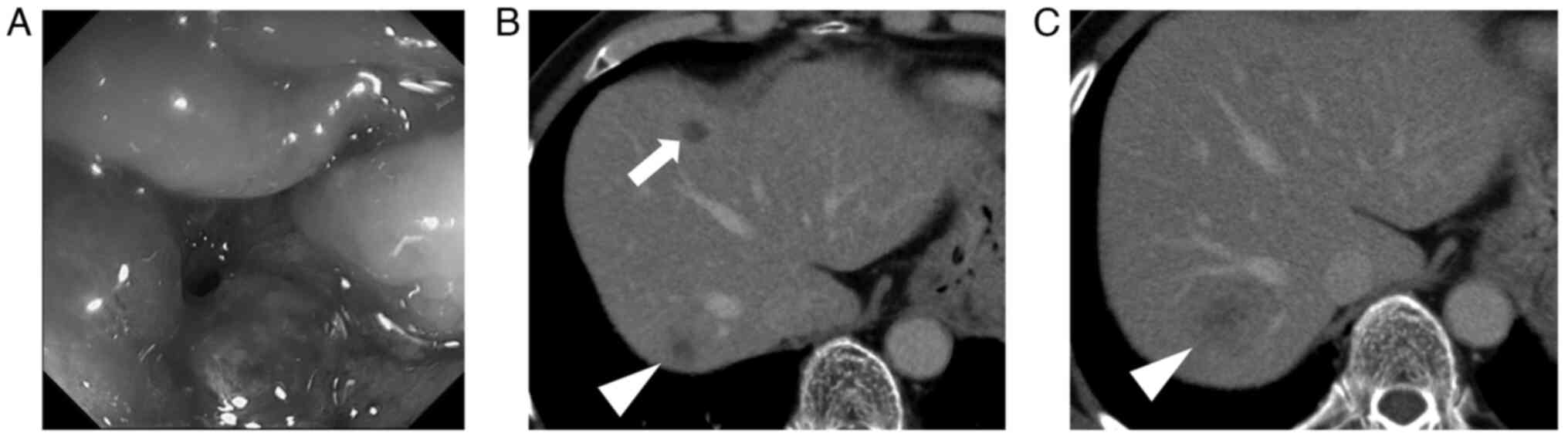
Case 3
A 75-year-old male patient was referred to IUHW,
Shioya Hospital (Yaita, Japan) with a diagnosis of transverse colon
cancer (Fig. 3A). The patient also
had diabetes mellitus with 6.8% haemoglobin A1c (HbA1c; Table I). CECT showed no obvious distant
metastasis, and a transverse colon resection was performed.
Pathological examination revealed that the tumor was a pT3N1M0,
pStage IIIB, moderately differentiated adenocarcinoma. After
surgery, the patient underwent chemotherapy with capecitabine
(3,600 mg/day) for 6 months (8 courses). At 1 year and 8 months
after surgery, three liver metastases measuring 27×21 and 10×6 mm
in the right lobe and 17×11 mm in S4 (Fig. 3B and C) were found. Laboratory
testing revealed that indocyanine green retention rate (ICG-R15) at
15 min was 14% (Table I), and the
patient underwent a partial right-posterior segmentectomy and S4
local resection after two courses (1 month) of FOLFOX plus
bevacizumab [folinic acid, 200 mg/m2; fluorouracil, 400
mg/m2 (bolus), fluorouracil, 2,400 mg/m2
(46-h continuous intravenous infusion), oxaliplatin, 85
mg/m2 and bevacizumab, 5 mg/kg]. The patient has been
disease-free for 2,035 days since the hepatectomy. Patient
follow-up was performed every 1–2 months at the outpatient
clinic.
Case 4
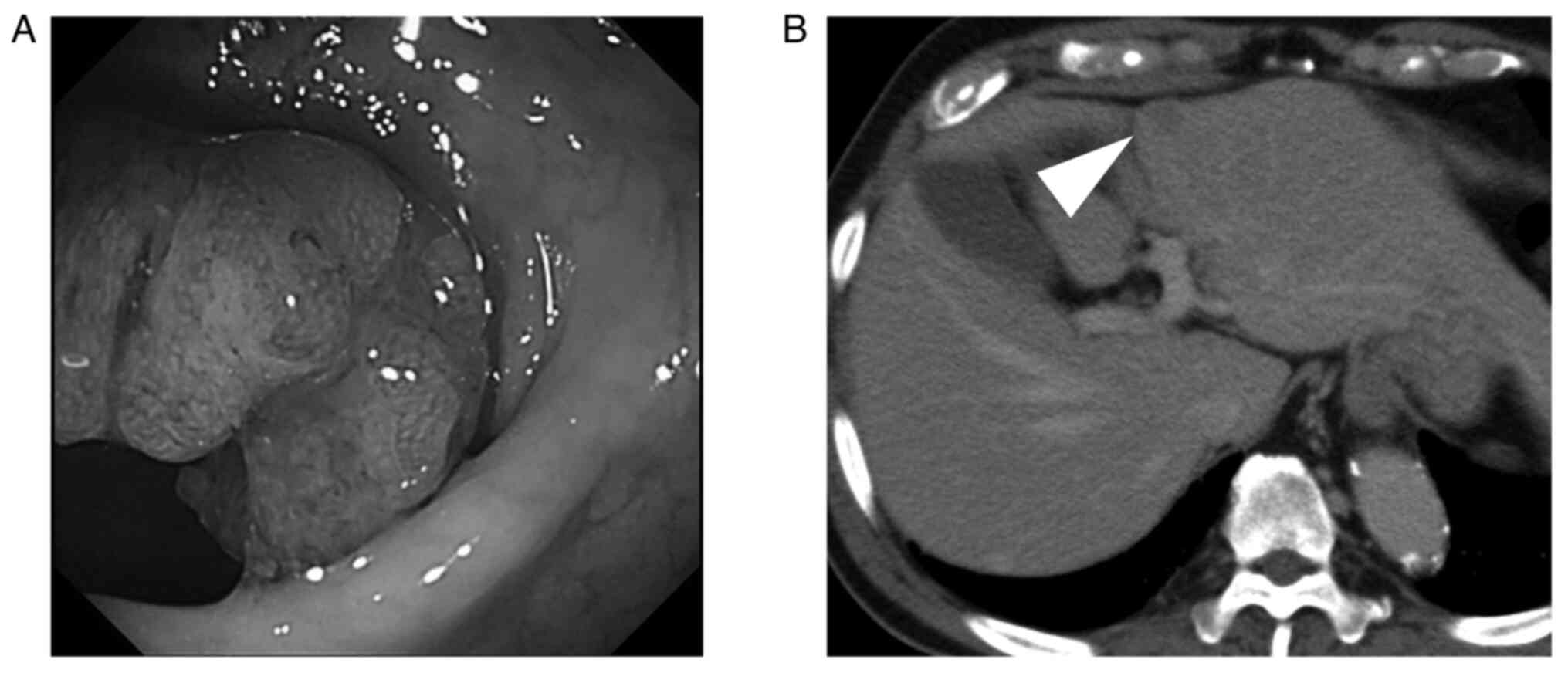
A 73-year-old male patient was referred to IUHW,
Shioya Hospital (Yaita, Japan) with a diagnosis of sigmoid colon
cancer without distant metastasis. The patient also had diabetes
mellitus with 6.4% HbA1c (Table I).
A laparoscopic sigmoidectomy was performed. Pathological
examination revealed a pT3N0M0, pStage IIA, moderately
differentiated adenocarcinoma (Fig.
4A). At 8 months postoperatively, imaging revealed two liver
metastases measuring 17×14 and 2×1 mm in S3 and S5, respectively
(Fig. 4B). The two lesions were
identified by intraoperative ultrasonography and a local resection
was performed to remove them. After surgery, the patient was
treated with FOLFOX [folinic acid 200 mg/m2,
fluorouracil 400 mg/m2 (bolus), fluorouracil 2,400
mg/m2 (46-h continuous intravenous infusion) and
oxaliplatin 85 mg/m2] for 6 months (10 courses). The
patient has been disease-free for 2,402 days since hepatic
resection. Patient follow-up was performed every 1–2 months at the
outpatient clinic.
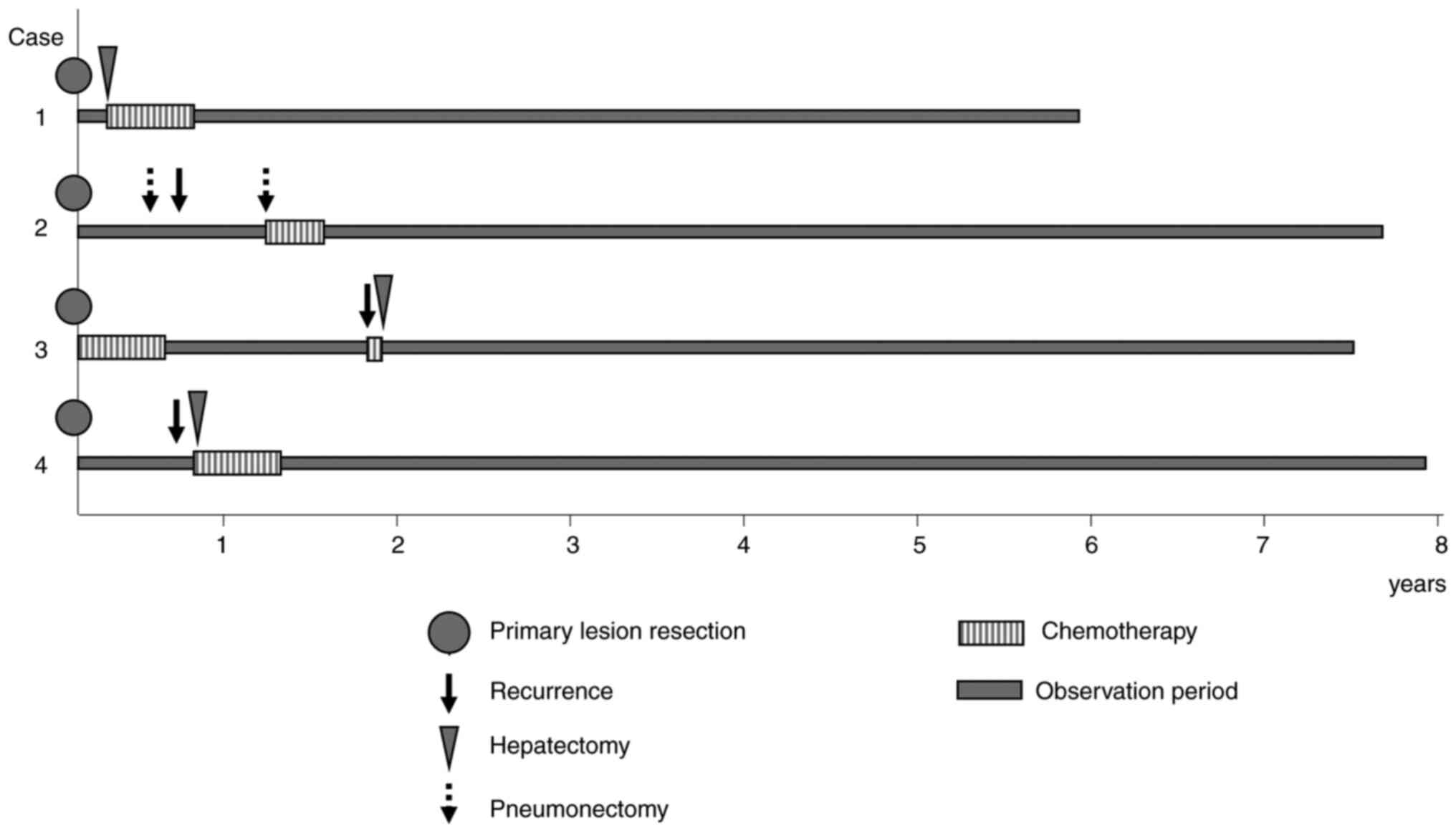
All cases
The clinicopathological characteristics of the
patients at the time of surgery of the primary lesions and the
information on the metastatic lesions are summarized in Tables I and II, respectively, and their clinical
courses are shown in Fig. 5.
 | Table II.Metastasis of colorectal cancer. |
Table II.
Metastasis of colorectal cancer.
| A, At resection of
primary tumor |
|---|
|
|---|
| Parameter | Case 1 | Case 2 | Case 3 | Case 4 |
|---|
| Organ of
metastasis | Liver | Right lung | None | None |
| Number of
metastasis | 2 | 4 | None | None |
| Site of metastasis,
mm (site) | 10×7 (S3), 7×5
(S4) | 8×6 (Upper lobe),
9×9 (Lower lobe), 2×2 (Lower lobe), 1×1 (Lower lobe) | NA | NA |
| Metastasectomy | S3 and S4 local
resection | Partial right upper
lobectomy, right lower lobectomy | NA | NA |
| Clavien-Dindo
classification of surgical complications | None | None | None | None |
|
| B, After
resection of primary tumor |
|
|
Parameter | Case 1 | Case 2 | Case 3 | Case 4 |
|
| Organ of
metastasis | None | Left lung | Liver | Liver |
| Number of
metastasis | None | 1 | 3 | 2 |
| Site of metastasis,
mm (site) | NA | 8×6 (Lower
lobe) | 27×21 (Right lobe),
10×6 (Right lobe), 17×11 (S4) | 17×14 (S3) 2×1
(S5) |
| Metastasectomy | NA | Partial left lower
lobectomy | Right-posterior
segmentectomy, S4 local resection | S3 local resection,
right-anterior local resection |
| Clavien-Dindo
classification of surgical complications | None | None | None | None |
Discussion
Resection of distant metastases is as important as
resection of the primary tumor to improve the prognosis of CRC
(1,9,10). The
2019 Japanese Society for Cancer of the Colon and Rectum (JSCCR)
guidelines for the treatment of CRC recommend resection of the
metastases if both primary and metastatic lesions are considered
resectable (1). It is also
recommended that surgical excision be considered for recurrence if
lesions are resectable (1).
However, no specific criteria have been defined for lesion
resectability thus far.
Treatment strategies for hepatectomy vary among
experienced surgeons (11). At
IUHW, Shioya Hospital, hepatectomy for metastatic lesions is
performed when cure or at least extension of prognosis is expected
upon combination with chemotherapy. As a premise, patients should
understand the significance of treatment and be willing to undergo
this treatment. In addition, the following standards of general
condition are to be met: i) Evaluation of condition by
cardiologists using electrocardiogram and echocardiography as
operable; ii) no requirement for daily oxygen inhalation; iii) no
ascites and total bilirubin <2 mg/dl; and iv) creatinine <2.0
mg/dl, preferably <1.5 mg/dl. Resection area is determined
according to ICG-R15. Poor Onodera's prognostic nutrition index
(OPNI) (6) or low albumin does not
preclude lower gastrointestinal surgery. Previous studies showed
that cardiovascular evaluation and respiratory function, such as
spirometry to measure forced expiratory volume 1 and the diffusing
capacity of carbon monoxide, are deemed to be important for
pneumonectomy, but these tests do not define the limitations of
resection (12). For the cure of
liver metastases, it was decided that resectability would primarily
be based on the involvement of the portal vein and the muscular
arteries (11). It is noteworthy
that the intuition of experienced surgeons that a patient can
tolerate treatment is important; however, it is not quantitative.
In the present case report, all patients demonstrated normal
cardiovascular, respiratory and liver function (Table I). Cases 2 and 4 demonstrated mildly
low albumin levels and OPNI.
In cases 1 and 2, liver and lung metastases were
detected by CECT before surgery. There are various studies on the
possibility of performing liver resection simultaneously or in
stages, but no conclusion was reached (13–15).
Since it has been reported that 60% of liver metastases recur
within 2 years of metastasectomy (16), in the treatment strategy of the
present study, two-stage surgery was carried out with a follow-up
period of 1–3 months in between. By contrast, there is no standard
for the surgical management of pulmonary metastasis in patients
with CRC (17). There is also no
consensus on chemotherapy and length of surveillance before
pneumonectomy. Furthermore, the effect of lung metastasectomy on
outcomes is controversial in metastatic CRC (18). Given that there are cases of cured
patients such as case 2 in the present report, pneumonectomy should
be considered if technically and physically feasible. If lung
metastases reappear after pneumonectomy, an additional
pneumonectomy may also lead to a favourable prognosis (19).
Regarding treatment first of either primary or
metastatic cancer, the primary lesion was either treated alone or
simultaneously with the metastatic lesion (20). On the other hand, a study reported
that treating liver metastasis first leads to a good prognosis
(20). In any case, repeated
resection of metastases is considered to result in a good prognosis
(21,22).
Chemotherapy after resection of the liver metastases
has been reported to improve progression-free survival or DFS but
has limited effects on overall survival times (23–25).
However, a potential cure was achieved by doublet backbone
chemotherapy (FOLFOX) combined with a hepatic resection in cases 3
and 4. Further evidence is required for perioperative chemotherapy
of a hepatic resection. Recently, chemotherapeutic regimen for
metastatic CRC has been selected based on specific molecular
subtypes. Doublet (FOLFOX, CapeOX, S-1/oxaliplatin,
5-FU/leucovorin/irinotecan, S-1/irinotecan) and triplet
(5-fluorouracil, oxaliplatin, irinotecan) backbone chemotherapy,
immune therapy (pembrolizumab), anti-epidermal growth factor
receptor antibodies (cetuximab and panitumumab) and anti-vascular
endothelial growth factor antibodies (bevacizumab) were offered
based on the presence of KRAS and BRAF gene mutations and
microsatellite instability (26).
These tailored therapies are expected to improve the cure rate of
CRC in the near future.
Finally, according to the 2019 JSCCR guidelines for
the treatment of CRC, radiation therapy is considered to have a
limited therapeutic effect on colon cancer, excluding rectal
cancer, and its main purpose is for palliative care and symptom
relief (1). Treatment of lung
metastases involves pneumonectomy and systemic chemotherapy but not
radiotherapy; pneumonectomy is considered first if the metastatic
lung tumor is resectable (1). None
of the cured patients with advanced CRC at IUHW, Shioya Hospital
had undergone radiation therapy. At present, pneumonectomy is
recommended for patients aiming for a complete cure. A case report
on the therapeutic effect of radiation therapy for CRC was
previously published (27).
Radiotherapy, particularly stereotactic body radiation therapy
(SBRT), is rapidly progressing as a non-invasive treatment
modality. SBRT actually has the potential to be equally effective
with less toxicity compared with surgery, particularly in elderly
patients and those patients with comorbidities such as respiratory
or heart failure. However, the recurrence rate may be higher in the
SBRT cohort than in the surgery cohort, although a death rate may
be similar in the two cohorts (28). The efficacy of radiation therapy may
be demonstrated in future studies with larger sample sizes.
The present study has a limitation. In Japan,
investigations of KRAS and BRAF gene mutations, and microsatellite
instability have been available since April 2010, August 2018 and
December 2020, respectively, using public insurance. Therefore, the
patients of the present report could not undergo genetic testing.
More cases might have been cured if the optimal therapy had been
selected base on the genotype.
In summary, in the present report, the cases of four
patients with CRC and distant metastasis who underwent multimodal
treatment and were potentially cured were reported. Further case
reports could improve the treatment strategies aimed at curing CRC
with metastasis or recurrence.
Acknowledgements
The authors would like to thank Mr. Mitsuhiko Ono,
Ms. Setsuko Hiraide and Ms. Rei Kotaki at the Department of
Pathology, Shioya Hospital, International University of Health and
Welfare (Yaita, Japan), for clerical assistance.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
YK and YI conceptualized the study and wrote the
manuscript. MI designed the treatment strategy. YK, AH and MI
treated the patients and collected the clinical data. YI performed
the pathological diagnosis. YK and YI confirm the authenticity of
all the raw data. All authors have read and approved the final
version of the manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the International University of Health and Welfare
(Nasushiobara, Japan; approval no. 22-B-43).
Patient consent for publication
Written informed consent was obtained from the
patients for their information to be published in this study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hashiguchi Y, Muro K, Saito Y, Ito Y,
Ajioka Y, Hamaguchi T, Hasegawa K, Hotta K, Ishida H, Ishiguro M,
et al: Japanese society for cancer of the colon and rectum.
Japanese society for cancer of the colon and rectum (JSCCR)
guidelines 2019 for the treatment of colorectal cancer. Int J Clin
Oncol. 25:1–42. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
National Cancer Center Japan, . GanJoho
Service. (In Japanese). https://ganjoho.jp/public/cancer/colon/index.htmlJuly
7–2022
|
|
3
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin. 68:394–424. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
American Cancer Society. Survival Rates
for Colorectal Cancer. https://www.cancer.org/cancer/colon-rectal-cancer/detection-diagnosis-staging/survival-rates.htmlAugust
20–2022
|
|
5
|
Deyo RA, Cherkin DC and Ciol MA: Adapting
a clinical comorbidity index for use with ICD-9-CM administrative
databases. J Clin Epidemiol. 45:613–619. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Onodera T, Goseki N and Kosaki G:
Prognostic nutritional index in gastrointestinal surgery of
malnourished cancer patients. Nihon Geka Gakkai Zasshi.
85:1001–1005. 1984.(In Japanese). PubMed/NCBI
|
|
7
|
Dindo D, Demartines N and Clavien PA:
Classification of surgical complications: A new proposal with
evaluation in a cohort of 6336 patients and results of a survey.
Ann Surg. 240:205–213. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
American Joint Committee on Cancer (AJCC),
. AJCC Cancer Staging Manual Seventh Edition. https://www.facs.org/media/j30havyf/ajcc_7thed_cancer_staging_manual.pdfJuly
1–2023
|
|
9
|
Mise Y, Imamura H, Hashimoto T, Seyama Y,
Aoki T, Hasegawa K, Beck Y, Sugawara Y, Makuuchi M, Nakajima J and
Kokudo N: Cohort study of the survival benefit of resection for
recurrent hepatic and/or pulmonary metastases after primary
hepatectomy for colorectal metastases. Ann Surg. 251:902–909. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Matsumoto T, Hasegawa S, Hida K, Kawada K,
Sakai Y and Sugihara K: Role of repeat resection in patients with
metastatic colorectal cancer: A multicenter retrospective study.
Dis Colon Rectum. 62:561–567. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ignatavicius P, Oberkofler CE, Chapman WC,
DeMatteo RP, Clary BM, D'Angelica MI, Tanabe KK, Hong JC, Aloia TA,
Pawlik TM, et al: Choices of therapeutic strategies for colorectal
liver metastases among expert liver surgeons: A throw of the dice?
Ann Surg. 272:715–722. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sawabata N, Nagayasu T, Kadota Y, Goto T,
Horio H, Mori T, Yamashita S and Iwasaki A: Risk assessment of lung
resection for lung cancer according to pulmonary function:
Republication of systematic review and proposals by guideline
committee of the Japanese association for chest surgery 2014. Gen
Thorac Cardiovasc Surg. 63:14–21. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li ZQ, Liu K, Duan JC, Li Z, Su CQ and
Yang JH: Meta-analysis of simultaneous versus staged resection for
synchronous colorectal liver metastases. Hepatol Res. 43:72–83.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bogach J, Wang J, Griffiths C, Parpia S,
Saskin R, Hallet J, Ruo L, Simunovic M and Serrano PE: Simultaneous
versus staged resection for synchronous colorectal liver
metastases: A population-based cohort study. Int J Surg. 74:68–75.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tsilimigras DI, Sahara K, Hyer JM, Diaz A,
Moris D, Bagante F, Guglielmi A, Ruzzenente A, Alexandrescu S,
Poultsides G, et al: Trends and outcomes of simultaneous versus
staged resection of synchronous colorectal cancer and colorectal
liver metastases. Surgery. 170:160–166. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
de Jong MC, Pulitano C, Ribero D, Strub J,
Mentha G, Schulick RD, Choti MA, Aldrighetti L, Capussotti L and
Pawlik TM: Rates and patterns of recurrence following curative
intent surgery for colorectal liver metastasis: An international
multi-institutional analysis of 1669 patients. Ann Surg.
250:440–448. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zellweger M, Abdelnour-Berchtold E,
Krueger T, Ris HB, Perentes JY and Gonzalez M: Surgical treatment
of pulmonary metastasis in colorectal cancer patients: Current
practice and results. Crit Rev Oncol Hematol. 127:105–116. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lee KY, Lau J, Siew BE, Chua YK, Lim YX,
Lim XY, Chong CS and Tan KK: Does pulmonary metastasectomy of
colorectal metastases translate to better survival? A systematic
review. Ann Acad Med Singap. 50:773–781. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Matsuguma H, Mun M, Sano A, Yoshino I,
Hashimoto H, Shintani Y, Iida T, Shiono S, Chida M, Kuroda H, et
al: Time to incurable recurrence for patients treated with
pulmonary metastasectomy for colorectal cancer. Ann Surg Oncol.
29:6909–6917. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kurbatov V, Resio BJ, Cama CA, Heller DR,
Cha C, Zhang Y, Lu J and Khan SA: Liver-first approach to stage IV
colon cancer with synchronous isolated liver metastases. J
Gastrointest Oncol. 11:76–83. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bellier J, De Wolf J, Hebbar M, Amrani ME,
Desauw C, Leteurtre E, Pruvot FR, Porte H and Truant S: Repeated
resections of hepatic and pulmonary metastases from colorectal
cancer provide long-term survival. World J Surg. 42:1171–1179.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Rajakannu M, Magdeleinat P, Vibert E,
Ciacio O, Pittau G, Innominato P, SaCunha A, Cherqui D, Morère JF,
Castaing D and Adam R: Is cure possible after sequential resection
of hepatic and pulmonary metastases from colorectal cancer? Clin
Colorectal Cancer. 17:41–49. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Nordlinger B, Sorbye H, Glimelius B,
Poston GJ, Schlag PM, Rougier P, Bechstein WO, Primrose JN, Walpole
ET, Finch-Jones M, et al: Perioperative chemotherapy with FOLFOX4
and surgery versus surgery alone for resectable liver metastases
from colorectal cancer (EORTC Intergroup trial 40983): A randomised
controlled trial. Lancet. 371:1007–1016. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Nordlinger B, Sorbye H, Glimelius B,
Poston GJ, Schlag PM, Rougier P, Bechstein WO, Primrose JN, Walpole
ET, Finch-Jones M, et al: Perioperative FOLFOX4 chemotherapy and
surgery versus surgery alone for resectable liver metastases from
colorectal cancer (EORTC 40983): Long-term results of a randomised,
controlled, phase 3 trial. Lancet Oncol. 14:1208–1215. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kanemitsu Y, Shimizu Y, Mizusawa J, Inaba
Y, Hamaguchi T, Shida D, Ohue M, Komori K, Shiomi A, Shiozawa M, et
al: Hepatectomy followed by mFOLFOX6 versus hepatectomy alone for
liver-only metastatic colorectal cancer (JCOG0603): A phase II or
III randomized controlled trial. J Clin Oncol. 39:3789–3799. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Morris VK, Kennedy EB, Baxter NN, Benson
AB III, Cercek A, Cho M, Ciombor KK, Cremolini C, Davis A, Deming
DA, et al: Treatment of metastatic colorectal cancer: ASCO
guideline. J Clin Oncol. 41:678–700. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sekiya S, Imamura K, Takeuchi S, Teramura
K, Watanabe Y, Tamoto E, Takada M, Kinoshita Y, Anbo Y, Nakamura F,
et al: Pathological complete response of locally advanced colon
cancer after preoperative radiotherapy: A case report and narrative
review of the literature. Surg Case Rep. 4:582018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chiappetta M, Salvatore L, Congedo MT,
Bensi M, De Luca V, Ciavarella LV, Camarda F, Evangelista J,
Valentini V, Tortora G, et al: Management of single pulmonary
metastases from colorectal cancer: State of the art. World J
Gastrointest Oncol. 14:820–832. 2022. View Article : Google Scholar : PubMed/NCBI
|