Introduction
Malignant mesothelioma of the tunica vaginalis
testis is a rare tumor that accounts for <1% of all mesothelioma
cases (1,2). It can occur at any age; however, the
majority of patients are between 55 and 75 years of age, with
occasional cases in adolescents (3). Since its first recording in 1957,
<300 cases have been reported worldwide (4,5). The
most common clinical manifestation of this disease is scrotal
enlargement with an unexplained hydrocele; a small number of
patients present with internal scrotal masses and pain in the
inguinal area (6). Early
preoperative diagnosis is challenging (7,8). This
disease is associated with difficulty in diagnosis, high
malignancy, easy recurrence, poor prognosis and unclear
epidemiological and risk factors (2,9,10), The
present study reports a case of malignant mesothelioma of
testicular sheath.
Case report
A 52-year-old man was referred to the Department of
Urology of Xiaoshan Hospital, Affiliated with Wenzhou Medical
University (Xiaoshan, China) in December 2022, complaining of
swelling and pain in the right testis for 2 months. The patient had
a previous history of hypertension, and blood pressure was well
controlled. Moreover, the patient had no known exposure to
asbestos. In December 2022, the pre-admission computed tomography
(CT) scan of the patient showed significant hydrocele of the right
testicular tunica vaginalis, suggesting epididymitis (Fig. 1). After admission, B-ultrasound
revealed a cyst in the right epididymis head and significant
hydrocele in the right testicle. Meanwhile, tumor indicators did
not show any abnormalities. After excluding contraindications, the
right testicular sheath reversal and right testicular sheath lesion
resection were performed under general anesthesia, and the
procedure went smoothly.
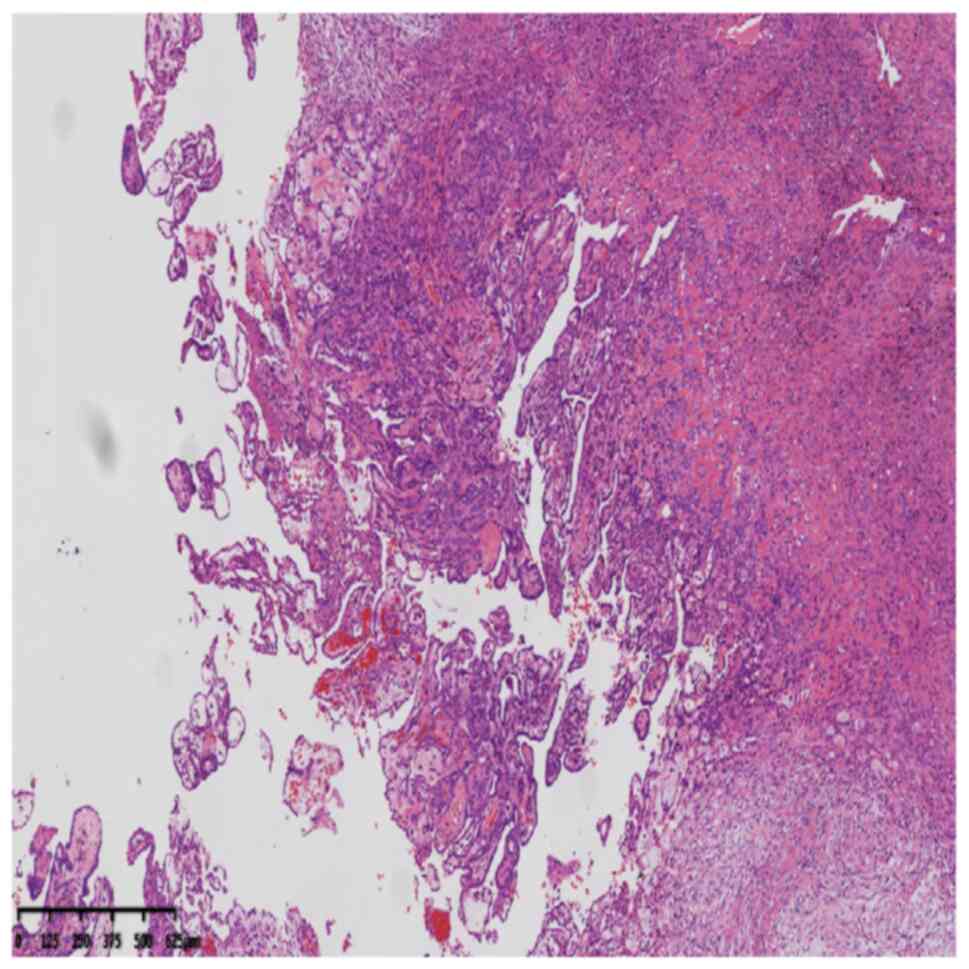
Postoperative pathological microscopic observations
revealed two forms, epithelial and sarcomatoid, and reciprocal
migration between the two was observed. The epithelial components
were characterized by small tubular, papillary and solid
arrangements. The tumor cells were cubic, flattened or low-columnar
in shape, with eosinophilic cytoplasm and round nuclei with visible
nucleoli. Sarcomas were comprised of spindle-shaped cell clusters
arranged in bundles or mats with spindle-shaped nuclei and visible
nucleoli (Fig. 2).
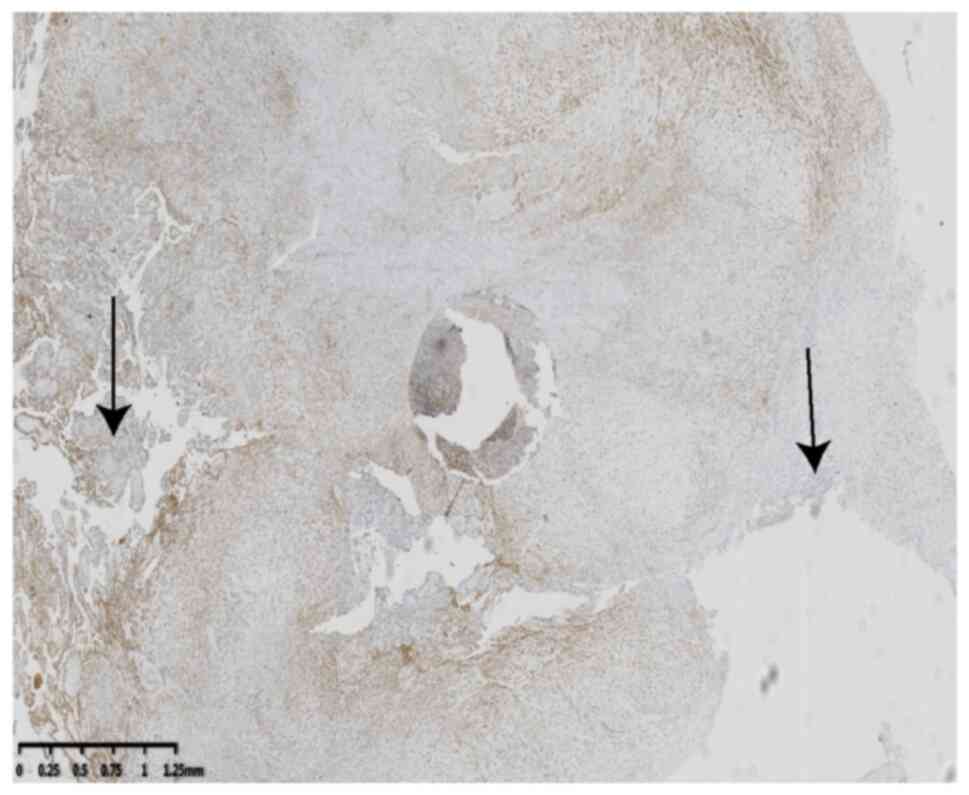
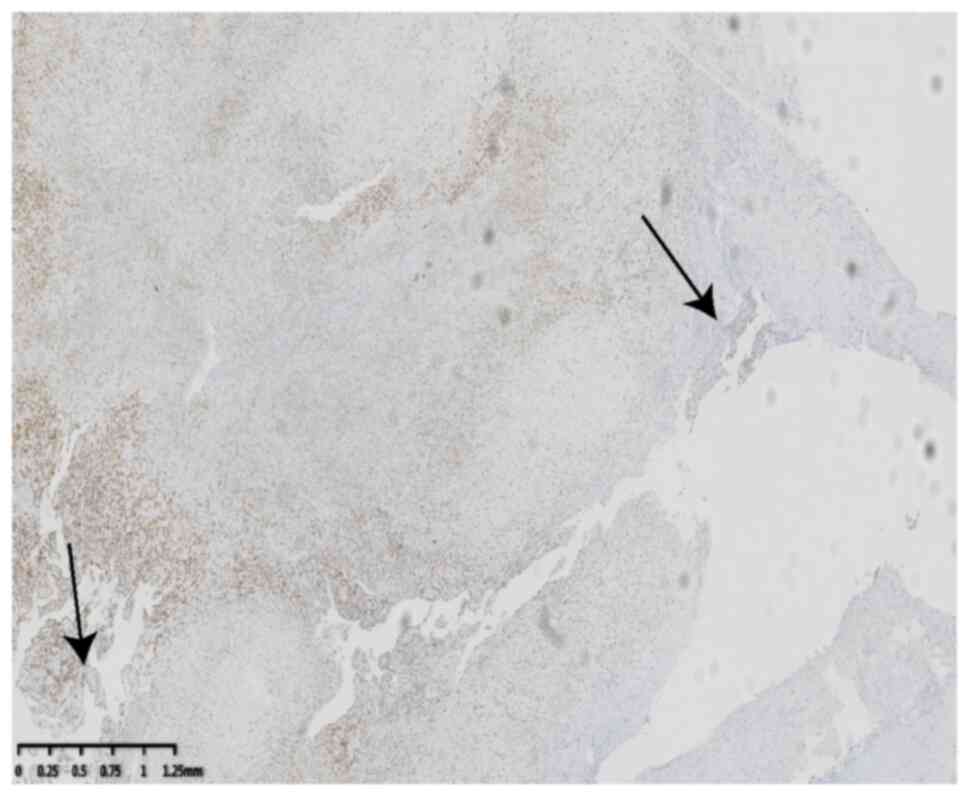
Immunohistochemical and specific staining results were as follows:
Calretinin(+) (Fig. 3),
carcinoembryonic antigen(−), cytokeratin (CK)5/6(+) (Fig. 4), D2-40(+), Wilms' tumor 1 (WT-1)(+)
(Fig. 5), human bone marrow
endothelial cell marker-1(+), Gata-3(+), vimentin(+),desmin+),
Ki-67(10%+), CD15(−), CD34(−) and smooth muscle actin(+). The
antibody list and detailed information sources are as follows.
ZM-0036 is a mouse anti-human Calretinin monoclonal antibody
(isoform, IgG1; clone number, OTI1D5) purchased from Beijing
Zhongshan Jinqiao Biotechnology Co., Ltd. WT-1 antibody (cat. no.
MAB-0678; clone no. MX012) and CK5/6 antibody (cat. no. MAB-0744;
clone no. MX040) were purchased from Fuzhou Maixin Biotechnology
Development Co., Ltd. The pathological diagnosis was a biphasic
mesothelioma. The patient recovered well postoperatively and was
discharged 7 day after admission.
Due to the high recurrence rate of bidirectional
mesothelioma, the patient was readmitted for right orchiectomy in
March 2023. The following postoperative pathology was observed:
Testicular (right) and partial scrotal resection specimens below
the skin, testis and epididymis were observed; fibrous tissue
hyperplasia; lymphocyte infiltration; and a large number of foreign
body giant cell aggregates and line knot reactions. No definite
tumor residue was found, consistent with the changes observed after
tumor resection, and the spermatic margin was negative. The patient
recovered well after surgery and was closely followed up.
Discussion
Malignant mesothelioma occurs most frequently in the
pleura or peritoneal cavity; testicular sheath malignant
mesothelioma is rare, accounting for <5% of all cases (11). Since Barbera and Rubino first
reported malignant mesothelioma of the testicular sphincter in 1957
(12), to the best of our
knowledge, the total number of cases reported in national and
international literature has not exceeded 100 to date (2). The annual incidence of malignant
mesothelioma in the United States is ~11 cases per million
individuals (3). Plas et al
(13) analyzed the ages of 74
patients with malignant mesothelioma of the tunica vaginalis and
found that the age distribution was between 7 and 87 years, mostly
occurring in middle-aged and older adult individuals. Nearly half
of the patients were aged 55–75 years old, 75% were >45 years
and only 10% were <25 years old.
There are several risk factors for malignant
mesothelioma of the testis. Asbestos exposure is the main risk
factor for pleural and peritoneal mesotheliomas. However, the
association between asbestos and tunica vaginalis tumors remains
unclear (2,14). Spiess et al (15) reported that 4 of 5 patients with
mesothelioma had a history of asbestos exposure. A 10-fold increase
in the risk of malignant mesothelioma has been reported among the
immediate family members of patients with a history of asbestos
exposure (16). In addition,
conditions such as an old testicular injury, hiatal hernia and
long-term syringomyelia may also be predisposing factors for the
development of this disease (1,17,18).
The current patient had no clear history of asbestos exposure;
however, the patient had a long history of hydrocele.
The rarity of testicular mesothelioma poses a
challenge for its diagnosis, which is rarely achieved
preoperatively. More than 50% of malignant testicular mesothelioma
cases are characterized by testicular hydrocele, testicular mass,
epididymitis, hernia and semen cysts (4). Preoperative diagnosis is difficult
because of the lack of specific symptoms and diagnostic tests
(19). A detailed history, physical
examination, imaging, laboratory tests and pathological findings
are key to diagnosing malignant mesothelioma of the testis
(6,20). Plas et al (13) concluded that the diagnosis was
confirmed preoperatively in only 3 of 74 patients and that 97.3% of
patients were confirmed by pathological examination due to the
discovery of a bloody effusion, papillary mass on the tunica
vaginalis or fibrous thickening of the tunica vaginalis during
surgery.
The main diagnostic basis was the postoperative
pathological results. Malignant mesotheliomas are divided into
three histological types: Epithelioid, sarcomatoid and biphasic
(21). Paratesticular malignant
mesothelioma is usually the epithelioid histological subtype (~75%
of cases), whereas the rest are biphasic or sarcomatoid
histological subtypes (22,23). Since the morphology of epithelial
mesothelioma is consistent with that of adenocarcinoma on
hematoxylin-eosin staining, it should be differentiated from
adenocarcinoma and diagnosed by immunohistochemistry (2). The most reliable immune marker is
calretinin, which is highly sensitive and specific to mesothelioma.
It is positive in malignant mesothelioma and negative in
adenocarcinoma (2). In addition,
the immunohistochemical markers CK5/6 and WT-1 have guiding
significance in diagnosing mesothelioma (19,24).
In the present case, the histological characteristic of this
disease was bidirectional differentiation of tumor cells containing
both epithelial and interstitial components. Meanwhile,
immunohistochemical indicators such as calretinin, CK5/6 and WT-1
were positive. However, a lack of confirmation of calretinin, CK5/6
and WT-1 through mRNA expression experiments (such as RT-PCR) is a
limitation of the present study.
Owing to the small number of cases of malignant
testicular mesothelioma, no exact treatment guidelines have been
established. Radical resection is the first choice for treating
paratesticular malignant mesotheliomas (25). Inguinal lymph node dissection is
recommended in patients with suspected lymph node metastasis
(26). The use of radiotherapy and
chemotherapy for pleural mesothelioma has been suggested for
malignant testicular mesothelioma (27). Cisplatin and pemetrexed can be used
as chemotherapy drugs for testicular mesothelioma (28); Zhang et al (3) reported a case of testicular
mesothelioma treated with pemetrexed and cisplatin for six cycles
of chemotherapy with stable disease and no signs of recurrence or
metastasis. However, this remains controversial because there are
few reported cases of this disease and no clear outcomes (29). Malignant mesothelioma of the tunica
vaginalis of the testis, similar to other malignant mesotheliomas,
is highly invasive in all subtypes (2). Tumors can invade tissues surrounding
the scrotum, causing lymph node metastasis and distant organ
metastasis, such as to the lungs and liver. The most common site of
metastasis is the retroperitoneal lymph node (8). Therefore, close postoperative
follow-up is required. In the present case, the patient was
followed up once, and no abnormalities were observed. If progress
is found during follow-up, we will provide the necessary
radiotherapy or chemotherapy according to the location of
recurrence and metastasis.
In summary, the present study reported a case of
testicular mesothelioma. The rarity of testicular mesothelioma
poses a challenge to its etiology and diagnosis, which is rarely
achieved preoperatively. Malignant mesothelioma of the testicular
tunica vaginalis has a poor prognosis and is not sensitive to
radiotherapy or chemotherapy, requiring close postoperative
follow-up. Furthermore, the analysis of clinical signs and
immunohistochemistry deepens our understanding of malignant
mesothelioma of the testicular tunica vaginalis and provides a
diagnostic reference for clinicians who encounter these conditions
in the future.
Acknowledgements
Not applicable.
Funding
This study was financially supported by the Science and
Technology Project of the Xiaoshan District (grant no.
2021306).
Availability of data and materials
The datasets used and/or analyzed during the paper
are available from the corresponding author on reasonable
request.
Authors' contributions
YJ and JC performed case data collection, drafting
of the manuscript and conception of the study. YC, XK and XX
analyzed, interpretated and discussed the data. YJ and JC confirm
the authenticity of all the raw data. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
An ethical statement was obtained from Xiaoshan
Hospital of Wenzhou Medical University, which agreed to publish the
case.
Patient consent for publication
The patient has given consent for the case to be
published publicly.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Iczkowski KA: Malignant mesothelioma of
tunica vaginalis testis: Update for 2022. Adv Anat Pathol.
30:259–261. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Drevinskaite M, Patasius A, Kevlicius L,
Mickys U and Smailyte G: Malignant mesothelioma of the tunica
vaginalis testis: A rare case and review of literature. BMC Cancer.
20:1622020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhang N, Fu N, Peng S and Luo X: Malignant
mesothelioma of the tunica vaginalis testis: A case report and
literature review. Mol Clin Oncol. 7:1053–1056. 2017.PubMed/NCBI
|
|
4
|
von Amsberg G, Sehovic M, Hartmann M and
Bokemeyer C: Diagnosis and treatment of rare testicular tumors
using the example of malignant mesothelioma of the tunica vaginalis
testis and Sertoli cell tumors. Urologe A. 60:872–879. 2021.(In
German). View Article : Google Scholar : PubMed/NCBI
|
|
5
|
de Sá, Barrêto Callou Peixoto M, Bernardo
Soares MK, Libânio BB, Albuquerque KS and Bacchi CE: Malignant
mesothelioma of the tunica vaginalis testis: A rare cause of
hydrocele. Urol Case Rep. 43:1020482022. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Park YJ, Kong HJ, Jang HC, Shin HS, Oh HK
and Park JS: Malignant mesothelioma of the spermatic cord. Korean J
Urol. 52:225–229. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Oshima J, Inoue H, Fukuda S, Nishimura K
and Hara T: Malignant mesothelioma of the tunica vaginalis testis:
A case report. Hinyokika Kiyo. 65:215–218. 2019.(In Japanese).
PubMed/NCBI
|
|
8
|
Baqui AA, Boire NA, Baqui TT and Etwaru
DJ: Malignant mesothelioma of the tunica vaginalis Testis-A
Malignancy associated with asbestos exposure and trauma: A case
report and literature review. J Investig Med High Impact Case Rep.
7:23247096198273352019.PubMed/NCBI
|
|
9
|
Mezei G, Chang ET, Mowat FS and Moolgavkar
SH: Comments on a recent case-control study of malignant
mesothelioma of the pericardium and the tunica vaginalis testis.
Scand J Work Environ Health. 47:85–86. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Arda E, Arıkan MG, Cetin G, Kuyumcuoğlu U
and Usta U: Malignant mesothelioma of tunica vaginalis testis:
Macroscopic and microscopic features of a very rare malignancy.
Cureus. 9:e18602017.PubMed/NCBI
|
|
11
|
Yang LH, Yu JH, Xu HT, Lin XY, Liu Y, Miao
Y, Wang L, Fan CF, Jiang GY, Ding SL, et al: Mesothelioma of the
tunica vaginalis testis with prominent adenomatoid features: A case
report. Int J Clin Exp Pathol. 7:7082–7087. 2014.PubMed/NCBI
|
|
12
|
Barbera V and Rubino M: Papillary
mesothelioma of the tunica vaginalis. Cancer. 10:183–189. 1957.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Plas E, Riedl CR and Pflüger H: Malignant
mesothelioma of the tunica vaginalis testis: Review of the
literature and assessment of prognostic parameters. Cancer.
83:2437–2446. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Trenti E, Palermo SM, D'Elia C, Elia C,
Comploj E and Pycha A, Carella R and Pycha A: Malignant
mesothelioma of tunica vaginalis testis: Report of a very rare case
with review of the literature. Arch Ital Urol Androl. 90:212–214.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Spiess PE, Tuziak T, Kassouf W, Grossman
HB and Czerniak B: Malignant mesothelioma of the tunica vaginalis.
Urology. 66:397–401. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Karabacakoğlu B, Kısa E, Özbilen MH,
Karademir B, Yardım S, Çelik O, Süelözgen T and İlbey YÖ: Malignant
mesothelioma of tunica vaginalis: Two extremely rare case reports.
Urologia. 90:422–425. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chys B, De Graeve N and Merckx L: Well
differentiated papillary mesothelioma of the tunica vaginalis: Case
report. Acta Chir Belg. 123:555–558. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mezei G, Chang ET, Mowat FS and Moolgavkar
SH: Epidemiology of mesothelioma of the pericardium and tunica
vaginalis testis. Ann Epidemiol. 27:348–359.e11. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kazaz IO, Teoman AS and Mungan S:
Mesothelioma of the tunica vaginalis testis: A case report. Indian
J Pathol Microbiol. 63:475–477. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ahmed Z, Singh S, Mangal A and Mittal A:
Primary malignant mesothelioma of the spermatic cord. BMJ Case Rep.
2016:bcr20162146022016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hai B, Yang Y, Xiao Y, Li B and Chen C:
Diagnosis and prognosis of malignant mesothelioma of the tunica
vaginalis testis. Can Urol Assoc J. 6:E238–E241. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chekol SS and Sun CC: Malignant
mesothelioma of the tunica vaginalis testis: Diagnostic studies and
differential diagnosis. Arch Pathol Lab Med. 136:113–117. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Nazemi A, Nassiri N, Pearce S and
Daneshmand S: Testicular mesothelioma: An analysis of epidemiology,
patient outcomes, and prognostic factors. Urology. 126:140–144.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Guney N, Basaran M, Karayigit E,
Müslümanoglu A, Guney S, Kilicaslan I and Gulbarut S: Malignant
mesothelioma of the tunica vaginalis testis: A case report and
review of the literature. Med Oncol. 24:449–452. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Candura SM, Canto A, Amatu A, Gerardini M,
Stella G, Mensi M and Poggi G: Malignant mesothelioma of the tunica
vaginalis testis in a petrochemical worker exposed to asbestos.
Anticancer Res. 28:1365–1368. 2008.PubMed/NCBI
|
|
26
|
Arslan A, Ozcakir-Tomruk C, Deniz E and
Akin O: A case report of metastasis of malignant mesothelioma to
the retromolar trigone. World J Surg Oncol. 14:1882016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Recabal P, Rosenzweig B, Bazzi WM, Carver
BS and Sheinfeld J: Malignant mesothelioma of the tunica vaginalis
testis: Outcomes following surgical management beyond radical
orchiectomy. Urology. 107:166–170. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ceresoli GL, Zucali PA, Mencoboni M, Botta
M, Grossi F, Cortinovis D, Zilembo N, Ripa C, Tiseo M, Favaretto
AG, et al: Phase II study of pemetrexed and carboplatin plus
bevacizumab as first-line therapy in malignant pleural
mesothelioma. Br J Cancer. 109:552–558. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Borrelli EP and McGladrigan CG: A review
of pharmacologic management in the treatment of mesothelioma. Curr
Treat Options Oncol. 22:142021. View Article : Google Scholar : PubMed/NCBI
|