|
1
|
Asrani SK, Devarbhavi H, Eaton J and
Kamath PS: Burden of liver diseases in the world. J Hepatol.
70:151–171. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Devarbhavi H, Asrani SK, Arab JP, Nartey
YA, Pose E and Kamath PS: Global burden of liver disease: 2023
Update. J Hepatol. 79:516–537. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Boldo E, Santafe A, Mayol A, Lozoya R,
Coret A, Escribano D, Fortea-Sanchis C, Muñoz A, Pastor JC, Perez
de Lucia G and Bosch N: Rare site hepatocellular carcinoma
metastasis. J Hepatocell Carcinoma. 7:39–44. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Singal AG, Kudo M and Bruix J:
Breakthroughs in hepatocellular carcinoma therapies. Clin
Gastroenterol Hepatol. 21:2135–2149. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gao R, Kalathur RKR, Coto-Llerena M, Ercan
C, Buechel D, Shuang S, Piscuoglio S, Dill MT, Camargo FD,
Christofori G and Tang F: YAP/TAZ and ATF4 drive resistance to
sorafenib in hepatocellular carcinoma by preventing ferroptosis.
EMBO Mol Med. 13:e143512021. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bodzin AS and Busuttil RW: Hepatocellular
carcinoma: Advances in diagnosis, management, and long term
outcome. World J Hepatol. 7:1157–1167. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhang Y, Shi ZL, Yang X and Yin ZF:
Targeting of circulating hepatocellular carcinoma cells to prevent
postoperative recurrence and metastasis. World J Gastroenterol.
20:142–147. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhu JZ, Zhou QY, Wang YM, Dai YN, Zhu J,
Yu CH and Li YM: Prevalence of fatty liver disease and the economy
in China: A systematic review. World J Gastroenterol. 21:5695–5706.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wu Y, Zheng Q, Zou B, Yeo YH, Li X, Li J,
Xie X, Feng Y, Stave CD, Zhu Q, et al: The epidemiology of NAFLD in
Mainland China with analysis by adjusted gross regional domestic
product: A meta-analysis. Hepatol Int. 14:259–269. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Younossi ZM, Golabi P, Paik JM, Henry A,
Van Dongen C and Henry L: The global epidemiology of nonalcoholic
fatty liver disease (NAFLD) and nonalcoholic steatohepatitis
(NASH): A systematic review. Hepatology. 77:1335–1347. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Greten TF, Villanueva A, Korangy F, Ruf B,
Yarchoan M, Ma L, Ruppin E and Wang XW: Biomarkers for
immunotherapy of hepatocellular carcinoma. Nat Rev Clin Oncol.
20:780–798. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhang Y, Wei C, Guo CC, Bi RX, Xie J, Guan
DH, Yang CH and Jiang YH: Prognostic value of microRNAs in
hepatocellular carcinoma: A meta-analysis. Oncotarget.
8:107237–107257. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
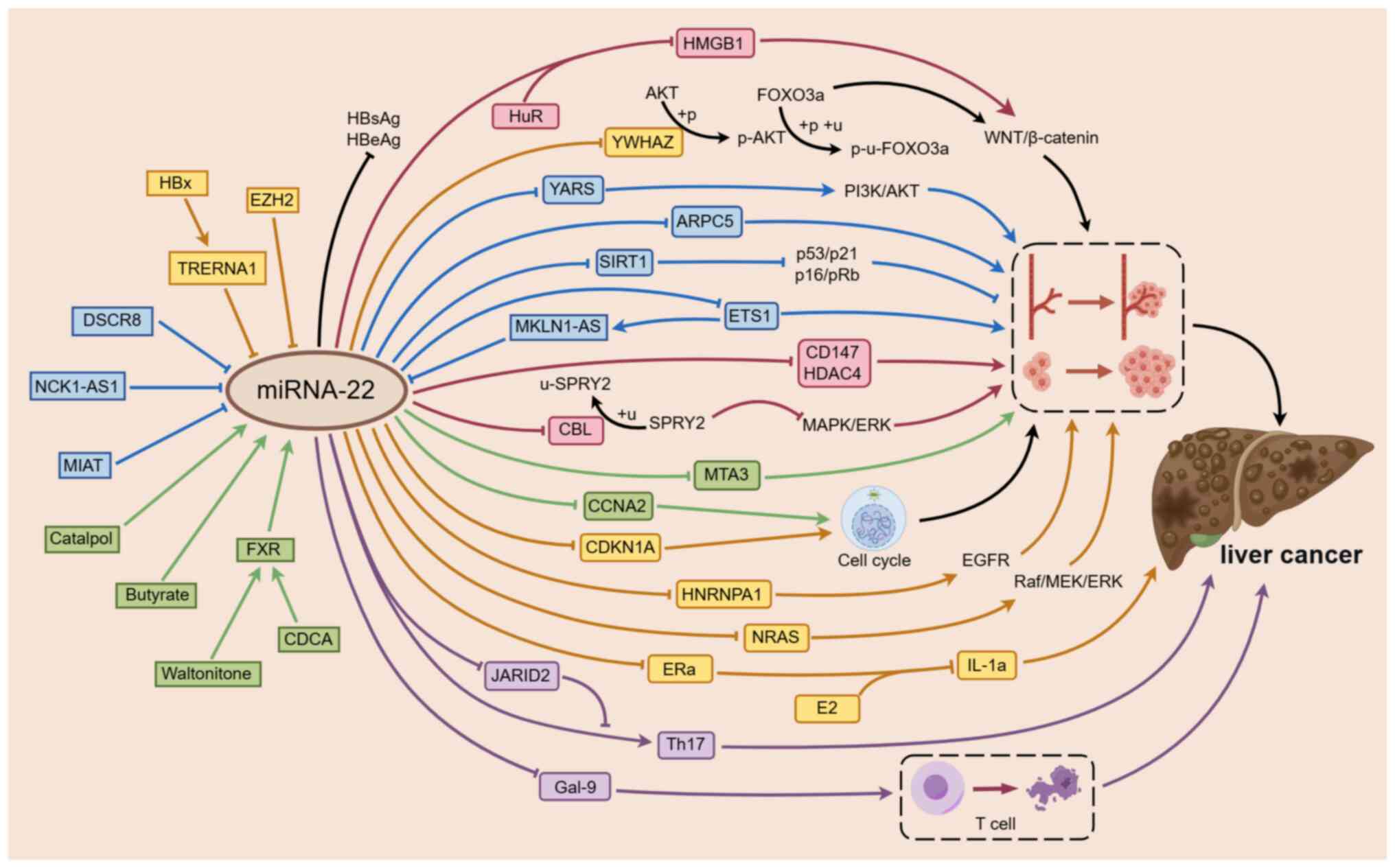
Hu Y, Setayesh T, Vaziri F, Wu X, Hwang
ST, Chen X and Yvonne Wan YJ: miR-22 gene therapy treats HCC by
promoting anti-tumor immunity and enhancing metabolism. Mol Ther.
31:1829–1845. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Song W, Zheng C, Liu M, Xu Y, Qian Y,
Zhang Z, Su H, Li X, Wu H, Gong P, et al: TRERNA1 upregulation
mediated by HBx promotes sorafenib resistance and cell
proliferation in HCC via targeting NRAS by sponging miR-22-3p. Mol
Ther. 29:2601–2616. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Menon A, Abd-Aziz N, Khalid K, Poh CL and
Naidu R: miRNA: A promising therapeutic target in cancer. Int J Mol
Sci. 23:115022022. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Shukla GC, Singh J and Barik S: MicroRNAs:
Processing, maturation, target recognition and regulatory
functions. Mol Cell Pharmacol. 3:83–92. 2011.PubMed/NCBI
|
|
17
|
Cui S, Chen Y, Guo Y, Wang X and Chen D:
Hsa-miR-22-3p inhibits liver cancer cell EMT and cell
migration/invasion by indirectly regulating SPRY2. PLoS One.
18:e02815362023. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Fan T, Wang CQ, Li XT, Yang H, Zhou J and
Song YJ: MiR-22-3p suppresses cell migration and invasion by
targeting PLAGL2 in breast cancer. J Coll Physicians Surg Pak.
31:937–940. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wang X, Wang X, Jiang T, Zhang Z, Xie N
and Yang G: MiR-22-3p suppresses NSCLC cell migration and EMT via
targeting RAC1 expression. Funct Integr Genomics. 23:2812023.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Qiao H, Wang N, Guan QL, Xie P and Li XK:
miR-22-3p suppresses cell proliferation and migration of gastric
cancer by targeting ENO1. Altern Ther Health Med. 29:278–283.
2023.PubMed/NCBI
|
|
21
|
Liu Y, Chen X, Cheng R, Yang F, Yu M, Wang
C, Cui S, Hong Y, Liang H, Liu M, et al: The Jun/miR-22/HuR
regulatory axis contributes to tumourigenesis in colorectal cancer.
Mol Cancer. 17:112018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zeng Z, Dong J, Li Y, Dong Z, Liu Z, Huang
J, Wang Y, Zhen Y and Lu Y: The expression level and diagnostic
value of microRNA-22 in HCC patients. Artif Cells Nanomed
Biotechnol. 48:683–686. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Panella R, Petri A, Desai BN, Fagoonee S,
Cotton CA, Nguyen PK, Lundin EM, Wagshal A, Wang DZ, Näär AM, et
al: MicroRNA-22 is a key regulator of lipid and metabolic
homeostasis. Int J Mol Sci. 24:128702023. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
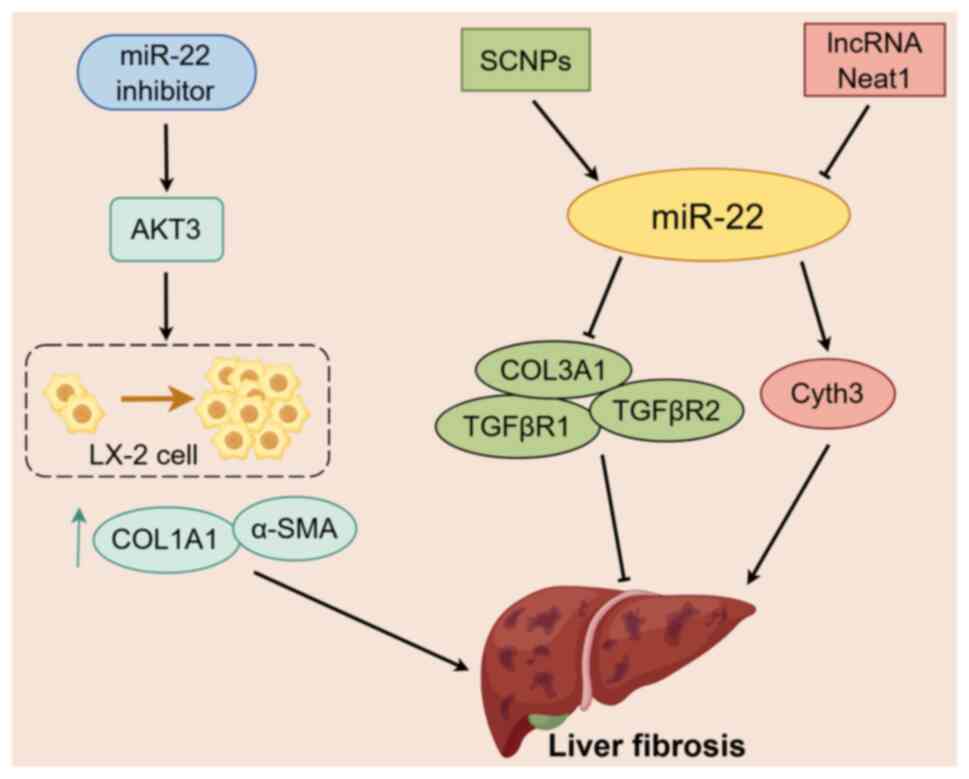
Wang Y, Zhang R, Li J, Han X, Lu H, Su J,
Liu Y, Tian X, Wang M, Xiong Y, et al: MiR-22-3p and miR-29a-3p
synergistically inhibit hepatic stellate cell activation by
targeting AKT3. Exp Biol Med (Maywood). 247:1712–1731. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Azar S, Udi S, Drori A, Hadar R,
Nemirovski A, Vemuri KV, Miller M, Sherill-Rofe D, Arad Y,
Gur-Wahnon D, et al: Reversal of diet-induced hepatic steatosis by
peripheral CB1 receptor blockade in mice is
p53/miRNA-22/SIRT1/PPARα dependent. Mol Metab. 42:1010872020.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Chen J, Wu FX, Luo HL, Liu JJ, Luo T, Bai
T, Li LQ and Fan XH: Berberine upregulates miR-22-3p to suppress
hepatocellular carcinoma cell proliferation by targeting Sp1. Am J
Transl Res. 8:4932–4941. 2016.PubMed/NCBI
|
|
27
|
Huang W, Huang F, Zhang R and Luo H:
LncRNA Neat1 expedites the progression of liver fibrosis in mice
through targeting miR-148a-3p and miR-22-3p to upregulate Cyth3.
Cell Cycle. 20:490–507. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Li H, Zhang P and Li F, Yuan G, Wang X,
Zhang A and Li F: Plasma miR-22-5p, miR-132-5p, and miR-150-3p are
associated with acute myocardial infarction. Biomed Res Int.
2019:50126482019.PubMed/NCBI
|
|
29
|
Wang Y, Chang W, Zhang Y, Zhang L, Ding H,
Qi H, Xue S, Yu H, Hu L, Liu D, et al: Circulating miR-22-5p and
miR-122-5p are promising novel biomarkers for diagnosis of acute
myocardial infarction. J Cell Physiol. 234:4778–4786. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Peng WX, Koirala P and Mo YY:
LncRNA-mediated regulation of cell signaling in cancer. Oncogene.
36:5661–5667. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Xu J, Shao T, Song M, Xie Y, Zhou J, Yin
J, Ding N, Zou H, Li Y and Zhang J: MIR22HG acts as a tumor
suppressor via TGFbeta/SMAD signaling and facilitates immunotherapy
in colorectal cancer. Mol Cancer. 19:512020. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Zhang W, Shi C, Xu Q, Chen X, Zhu H and
Zheng B: Long non-coding RNA MIR22HG suppresses cell proliferation
and promotes apoptosis in prostate cancer cells by sponging
microRNA-9-3p. Bioengineered. 13:13108–13117. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Deng X, Ye D, Hua K, Song H, Luo Q,
Munankarmy A, Liu D, Zhou B, Zheng W, Zhou X, et al: MIR22HG
inhibits breast cancer progression by stabilizing LATS2 tumor
suppressor. Cell Death Dis. 12:8102021. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Zhang L, Li C and Su X: Emerging impact of
the long noncoding RNA MIR22HG on proliferation and apoptosis in
multiple human cancers. J Exp Clin Cancer Res. 39:2712020.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Zhang J, Yang Y, Yang T, Liu Y, Li A, Fu
S, Wu M, Pan Z and Zhou W: microRNA-22, downregulated in
hepatocellular carcinoma and correlated with prognosis, suppresses
cell proliferation and tumourigenicity. Br J Cancer. 103:1215–1220.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Yang F, Hu Y, Liu HX and Wan YJY:
MiR-22-silenced cyclin A expression in colon and liver cancer cells
is regulated by bile acid receptor. J Biol Chem. 290:6507–6515.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Huang JN, Zhang HM, Cai JD, Wang WL and
Wang P: Long noncoding RNA DSCR8 promotes the proliferation of
liver cancer cells and inhibits apoptosis via the miR-22-3p/ARPC5
axis. J Cancer. 14:35–49. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Chen M, Hu W, Xiong CL, Qu Z, Yin CQ, Wang
YH, Luo CL, Guan Q, Yuan CH and Wang FB: miR-22 targets YWHAZ to
inhibit metastasis of hepatocellular carcinoma and its
down-regulation predicts a poor survival. Oncotarget.
7:80751–80764. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Gjorgjieva M, Ay AS, Correia de Sousa M,
Delangre E, Dolicka D, Sobolewski C, Maeder C, Fournier M, Sempoux
C and Foti M: MiR-22 deficiency fosters hepatocellular carcinoma
development in fatty liver. Cells. 11:28602022. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Zhang L, Yang P, Wang J, Liu Q, Wang T,
Wang Y and Lin F: MiR-22 regulated T cell differentiation and
hepatocellular carcinoma growth by directly targeting Jarid2. Am J
Cancer Res. 11:2159–2173. 2021.PubMed/NCBI
|
|
41
|
Zhao L, Wang Y and Liu Q: Catalpol
inhibits cell proliferation, invasion and migration through
regulating miR-22-3p/MTA3 signalling in hepatocellular carcinoma.
Exp Mol Pathol. 109:51–60. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Wu Y, Zhou Y, Huan L, Xu L, Shen M, Huang
S and Liang L: LncRNA MIR22HG inhibits growth, migration and
invasion through regulating the miR-10a-5p/NCOR2 axis in
hepatocellular carcinoma cells. Cancer Sci. 110:973–984. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Zhang DY, Zou XJ, Cao CH, Zhang T, Lei L,
Qi XL, Liu L and Wu DH: Identification and functional
characterization of long non-coding RNA MIR22HG as a tumor
suppressor for hepatocellular carcinoma. Theranostics. 8:3751–3765.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Luo LJ, Zhang LP, Duan CY, Wang B, He NN,
Abulimiti P and Lin Y: The inhibition role of miR-22 in
hepatocellular carcinoma cell migration and invasion via targeting
CD147. Cancer Cell Int. 17:172017. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Yim DGR, Ghosh S, Guy GR and Virshup DM:
Casein kinase 1 regulates sprouty2 in FGF-ERK signaling. Oncogene.
34:474–484. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Quinn JJ and Chang HY: Unique features of
long non-coding RNA biogenesis and function. Nat Rev Genet.
17:47–62. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Zhao L, Hu K, Cao J, Wang P, Li J, Zeng K,
He X, Tu PF, Tong T and Han L: lncRNA miat functions as a ceRNA to
upregulate sirt1 by sponging miR-22-3p in HCC cellular senescence.
Aging (Albany NY). 11:7098–7122. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Guo C, Zhou S, Yi W, Yang P, Li O, Liu J
and Peng C: Long non-coding RNA muskelin 1 antisense RNA (MKLN1-AS)
is a potential diagnostic and prognostic biomarker and therapeutic
target for hepatocellular carcinoma. Exp Mol Pathol.
120:1046382021. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Pan G, Zhang J, You F, Cui T, Luo P, Wang
S, Li X and Yuan Q: ETS proto-oncogene 1-activated muskelin 1
antisense RNA drives the malignant progression of hepatocellular
carcinoma by targeting miR-22-3p to upregulate ETS proto-oncogene
1. Bioengineered. 13:1346–1358. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Guan B, Ma J, Yang Z, Yu F and Yao J:
LncRNA NCK1-AS1 exerts oncogenic property in gastric cancer by
targeting the miR-22-3p/BCL9 axis to activate the Wnt/β-catenin
signaling. Environ Toxicol. 36:1640–1653. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Wang B, Wang K, Jin T, Xu Q, He Y, Cui B
and Wang Y: NCK1-AS1 enhances glioma cell proliferation,
radioresistance and chemoresistance via miR-22-3p/IGF1R ceRNA
pathway. Biomed Pharmacother. 129:1103952020. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Zhou W, Wang J, Zhang J, Wang Y, Jiang L,
Guo T, Luo B, Xu Q and Huang Y: LncRNA NCK1-AS1 aggravates
hepatocellular carcinoma by the miR-22-3p/YARS axis to activate
PI3K/AKT signaling. J Gastrointestin Liver Dis. 31:48–59. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Zhang C, Lin X, Zhao Q, Wang Y, Jiang F,
Ji C, Li Y, Gao J, Li J and Shen L: YARS as an oncogenic protein
that promotes gastric cancer progression through activating
PI3K-Akt signaling. J Cancer Res Clin Oncol. 146:329–342. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Pant K, Yadav AK, Gupta P, Islam R, Saraya
A and Venugopal SK: Butyrate induces ROS-mediated apoptosis by
modulating miR-22/SIRT-1 pathway in hepatic cancer cells. Redox
Biol. 12:340–349. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Yang F, Gong J, Wang G, Chen P, Yang L and
Wang Z: Waltonitone inhibits proliferation of hepatoma cells and
tumorigenesis via FXR-miR-22-CCNA2 signaling pathway. Oncotarget.
7:75165–75175. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Xia L, Oyang L, Lin J, Tan S, Han Y, Wu N,
Yi P, Tang L, Pan Q, Rao S, et al: The cancer metabolic
reprogramming and immune response. Mol Cancer. 20:282021.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Donne R and Lujambio A: The liver cancer
immune microenvironment: Therapeutic implications for
hepatocellular carcinoma. Hepatology. 77:1773–1796. 2023.PubMed/NCBI
|
|
58
|
Jhunjhunwala S, Hammer C and Delamarre L:
Antigen presentation in cancer: Insights into tumour immunogenicity
and immune evasion. Nat Rev Cancer. 21:298–312. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Kumar R, Theiss AL and Venuprasad K:
RORgammat protein modifications and IL-17-mediated inflammation.
Trends Immunol. 42:1037–1050. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Lequeux A, Noman MZ, Xiao M, Van Moer K,
Hasmim M, Benoit A, Bosseler M, Viry E, Arakelian T, Berchem G, et
al: Targeting HIF-1 alpha transcriptional activity drives cytotoxic
immune effector cells into melanoma and improves combination
immunotherapy. Oncogene. 40:4725–4735. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Togashi Y, Shitara K and Nishikawa H:
Regulatory T cells in cancer immunosuppression-implications for
anticancer therapy. Nat Rev Clin Oncol. 16:356–371. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Kang JH and Zappasodi R: Modulating Treg
stability to improve cancer immunotherapy. Trends Cancer.
9:911–927. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Golden-Mason L and Rosen HR: Galectin-9:
Diverse roles in hepatic immune homeostasis and inflammation.
Hepatology. 66:271–279. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Sauer N, Janicka N, Szlasa W, Skinderowicz
B, Kołodzińska K, Dwernicka W, Oślizło M, Kulbacka J, Novickij V
and Karłowicz-Bodalska K: TIM-3 as a promising target for cancer
immunotherapy in a wide range of tumors. Cancer Immunol Immunother.
72:3405–3425. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Zhao L, Cheng S, Fan L, Zhang B and Xu S:
TIM-3: An update on immunotherapy. Int Immunopharmacol.
99:1079332021. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Yang Q, Jiang W, Zhuang C, Geng Z, Hou C,
Huang D, Hu L and Wang X: microRNA-22 downregulation of galectin-9
influences lymphocyte apoptosis and tumor cell proliferation in
liver cancer. Oncol Rep. 34:1771–1778. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Shao X, Zhu J, Shi Y, Fang H, Chen J,
Zhang Y, Wang J, Jian H, Lan S, Jiang F, et al: Upregulated UBE4B
expression correlates with poor prognosis and tumor immune
infiltration in hepatocellular carcinoma. Aging (Albany NY).
14:9632–9646. 2022.PubMed/NCBI
|
|
68
|
McGlynn KA, Petrick JL and El-Serag HB:
Epidemiology of hepatocellular carcinoma. Hepatology. 73 (Suppl
1):S4–S13. 2021. View Article : Google Scholar
|
|
69
|
Qiao DD, Yang J, Lei XF, Mi GL, Li SL, Li
K, Xu CQ and Yang HL: Expression of microRNA-122 and microRNA-22 in
HBV-related liver cancer and the correlation with clinical
features. Eur Rev Med Pharmacol Sci. 21:742–747. 2017.PubMed/NCBI
|
|
70
|
Ke RS, Zhang K, Lv LZ, Dong YP, Pan F,
Yang F, Cai QC and Jiang Y: Prognostic value and oncogene function
of heterogeneous nuclear ribonucleoprotein A1 overexpression in
HBV-related hepatocellular carcinoma. Int J Biol Macromol.
129:140–151. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Shi C and Xu X: MicroRNA-22 is
down-regulated in hepatitis B virus-related hepatocellular
carcinoma. Biomed Pharmacother. 67:375–380. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Qian C and Liu Q: FOXO3a inhibits
nephroblastoma cell proliferation, migration and invasion, and
induces apoptosis through downregulating the Wnt/β-catenin
signaling pathway. Mol Med Rep. 24:7962021. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Tian Y, Qi P and Hu X: Downregulated
FOXO3a associates with poor prognosis and promotes cell invasion
and migration via WNT/β-catenin signaling in cervical carcinoma.
Front Oncol. 10:9032020. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Naugler WE, Sakurai T, Kim S, Maeda S, Kim
K, Elsharkawy AM and Karin M: Gender disparity in liver cancer due
to sex differences in MyD88-dependent IL-6 production. Science.
317:121–124. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Sakurai T, He G, Matsuzawa A, Yu GY, Maeda
S, Hardiman G and Karin M: Hepatocyte necrosis induced by oxidative
stress and IL-1 alpha release mediate carcinogen-induced
compensatory proliferation and liver tumorigenesis. Cancer Cell.
14:156–165. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Jiang R, Deng L, Zhao L, Li X, Zhang F,
Xia Y, Gao Y, Wang X and Sun B: miR-22 promotes HBV-related
hepatocellular carcinoma development in males. Clin Cancer Res.
17:5593–5603. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Pandey DP and Picard D: miR-22 inhibits
estrogen signaling by directly targeting the estrogen receptor
alpha mRNA. Mol Cell Biol. 29:3783–3790. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Chen S, Pu J, Bai J, Yin Y, Wu K, Wang J,
Shuai X, Gao J, Tao K, Wang G and Li H: EZH2 promotes
hepatocellular carcinoma progression through modulating
miR-22/galectin-9 axis. J Exp Clin Cancer Res. 37:32018. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Guo L, Hu C, Yao M and Han G: Mechanism of
sorafenib resistance associated with ferroptosis in HCC. Front
Pharmacol. 14:12074962023. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Cheng Y, Takeuchi H, Sonobe Y, Jin S, Wang
Y, Horiuchi H, Parajuli B, Kawanokuchi J, Mizuno T and Suzumura A:
Sirtuin 1 attenuates oxidative stress via upregulation of
superoxide dismutase 2 and catalase in astrocytes. J Neuroimmunol.
269:38–43. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Portmann S, Fahrner R, Lechleiter A, Keogh
A, Overney S, Laemmle A, Mikami K, Montani M, Tschan MP, Candinas D
and Stroka D: Antitumor effect of SIRT1 inhibition in human HCC
tumor models in vitro and in vivo. Mol Cancer Ther. 12:499–508.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Jin Q, Hu H, Yan S, Jin L, Pan Y, Li X,
Peng Y and Cao P: lncRNA MIR22HG-derived miR-22-5p enhances the
radiosensitivity of hepatocellular carcinoma by increasing histone
acetylation through the inhibition of HDAC2 activity. Front Oncol.
11:5725852021. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Yang J, Yan B, Yang L, Li H, Fan Y, Zhu F,
Zheng J and Ma X: Macrocytic anemia is associated with the severity
of liver impairment in patients with hepatitis B virus-related
decompensated cirrhosis: A retrospective cross-sectional study. BMC
Gastroenterol. 18:1612018. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Adigun OO, Yarrarapu SNS, Zubair M and
Khetarpal S: Alpha-fetoprotein analysis. In: StatPearls [Internet].
Treasure Island (FL): StatPearls Publishing; 2024
|
|
85
|
Li CQ, Huang H, Ruan SM, Hu HT, Xian MF,
Xie XY, Lu MD, Kuang M, Wang Y and Chen LD: An assessment of liver
lesions using a combination of CEUS LI-RADS and AFP. Abdom Radiol
(NY). 47:1311–1320. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Tzartzeva K and Singal AG: Testing for AFP
in combination with ultrasound improves early liver cancer
detection. Expert Rev Gastroenterol Hepatol. 12:947–949. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Zekri ARN, Youssef ASED, El-Desouky ED,
Ahmed OS, Lotfy MM, Nassar AAM and Bahnassey AA: Serum microRNA
panels as potential biomarkers for early detection of
hepatocellular carcinoma on top of HCV infection. Tumour Biol.
37:12273–12286. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Xia L, Wang S, Zhang H, Yang Y, Wei J, Shi
Y, Zou C, Liu J, Luo M, Huang A and Wang D: The HBx and HBc of
hepatitis B virus can influence Id1 and Id3 by reducing their
transcription and stability. Virus Res. 284:1979732020. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Li J, Zhang X, Chen L, Zhang Z, Zhang J,
Wang W, Wu M, Shi B, Zhang X, Kozlowski M, et al: Circulating
miR-210 and miR-22 combined with ALT predict the virological
response to interferon-alpha therapy of CHB patients. Sci Rep.
7:156582017. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Hu Q, Wang Q, Zhang Y, Tao S, Zhang X, Liu
X, Li X, Jiang X, Huang C, Xu W, et al: Baseline serum
exosome-derived miRNAs predict HBeAg seroconversion in chronic
hepatitis B patients treated with peginterferon. J Med Virol.
93:4939–4948. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Badmus OO, Hillhouse SA, Anderson CD,
Hinds TD and Stec DE: Molecular mechanisms of metabolic associated
fatty liver disease (MAFLD): Functional analysis of lipid
metabolism pathways. Clin Sci (Lond). 136:1347–1366. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Zhang P, Wang W, Mao M, Gao R, Shi W, Li
D, Calderone R, Sui B, Tian X and Meng X: Similarities and
differences: A comparative review of the molecular mechanisms and
effectors of NAFLD and AFLD. Front Physiol. 12:7102852021.
View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Chen D, Yan Y, Wang X, Li S, Liu Y, Yu D,
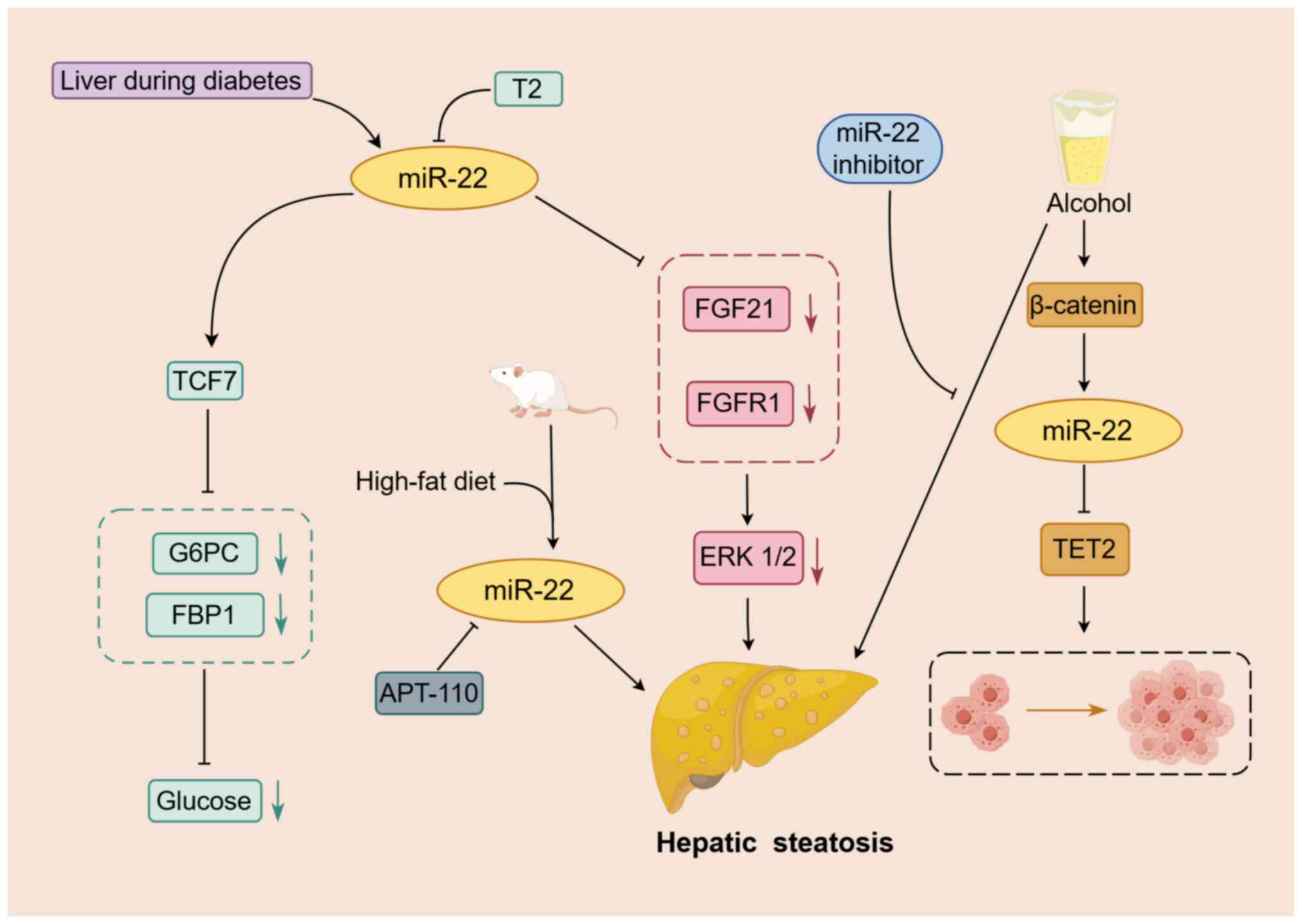
He Y, Deng R, Liu Y, Xu M, et al: Chronic alcohol exposure promotes
HCC stemness and metastasis through β-catenin/miR-22-3p/TET2 axis.
Aging (Albany NY). 13:14433–14455. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Yang Z, Qin W, Huo J, Zhuo Q, Wang J and
Wang L: MiR-22 modulates the expression of lipogenesis-related
genes and promotes hepatic steatosis in vitro. FEBS Open Bio.
11:322–332. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Hu Y, Liu HX, Jena PK, Sheng L, Ali MR and
Wan YY: miR-22 inhibition reduces hepatic steatosis via FGF21 and
FGFR1 induction. JHEP Rep. 2:1000932020. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Pouwels S, Sakran N, Graham Y, Leal A,
Pintar T, Yang W, Kassir R, Singhal R, Mahawar K and Ramnarain D:
Non-alcoholic fatty liver disease (NAFLD): A review of
pathophysiology, clinical management and effects of weight loss.
BMC Endocr Disord. 22:632022. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Liu Q, Li J, Zhang W, Xiao C, Zhang S,
Nian C, Li J, Su D, Chen L, Zhao Q, et al: Glycogen accumulation
and phase separation drives liver tumor initiation. Cell.
184:5559–5576.e19. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Agosti P, Sabbà C and Mazzocca A: Emerging
metabolic risk factors in hepatocellular carcinoma and their
influence on the liver microenvironment. Biochim Biophys Acta Mol
Basis Dis. 1864:607–617. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Hyun J, Han J, Lee C, Yoon M and Jung Y:
Pathophysiological aspects of alcohol metabolism in the liver. Int
J Mol Sci. 22:57172021. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Jeon S and Carr R: Alcohol effects on
hepatic lipid metabolism. J Lipid Res. 61:470–479. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Lu W, Li X and Luo Y: FGF21 in obesity and
cancer: New insights. Cancer Lett. 499:5–13. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Rodríguez-Agudo R, González-Recio I,
Serrano-Maciá M, Bravo M, Petrov P, Blaya D, Herranz JM,
Mercado-Gómez M, Rejano-Gordillo CM, Lachiondo-Ortega S, et al:
Anti-miR-873-5p improves alcohol-related liver disease by enhancing
hepatic deacetylation via SIRT1. JHEP Rep. 6:1009182023. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Iwagami Y, Zou J, Zhang H, Cao K, Ji C,
Kim M and Huang CK: Alcohol-mediated miR-34a modulates hepatocyte
growth and apoptosis. J Cell Mol Med. 22:3987–3995. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Rinella ME, Neuschwander-Tetri BA,
Siddiqui MS, Abdelmalek MF, Caldwell S, Barb D, Kleiner DE and
Loomba R: AASLD practice guidance on the clinical assessment and
management of nonalcoholic fatty liver disease. Hepatology.
77:1797–1835. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
No authors listed. The diagnosis and
management of nonalcoholic fatty liver disease: Practice guidance
from the American association for the study of liver diseases. Clin
Liver Dis (Hoboken). 11:812018. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Castano C, Novials A and Párrizas M:
Exosomes from short-term high-fat or high-sucrose fed mice induce
hepatic steatosis through different pathways. Cells. 12:1692022.
View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Thibonnier M and Esau C: Metabolic
benefits of MicroRNA-22 inhibition. Nucleic Acid Ther. 30:104–116.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Thibonnier M, Esau C, Ghosh S, Wargent E
and Stocker C: Metabolic and energetic benefits of microRNA-22
inhibition. BMJ Open Diabetes Res Care. 8:e0014782020. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Gjorgjieva M, Sobolewski C, Ay AS, Abegg
D, Correia de Sousa M, Portius D, Berthou F, Fournier M, Maeder C,
Rantakari P, et al: Genetic ablation of MiR-22 fosters diet-induced
obesity and NAFLD development. J Pers Med. 10:1702020. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Younossi ZM, Golabi P, de Avila L, Paik
JM, Srishord M, Fukui N, Qiu Y, Burns L, Afendy A and Nader F: The
global epidemiology of NAFLD and NASH in patients with type 2
diabetes: A systematic review and meta-analysis. J Hepatol.
71:793–801. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Agbu P and Carthew RW: MicroRNA-mediated
regulation of glucose and lipid metabolism. Nat Rev Mol Cell Biol.
22:425–438. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Kaur K, Vig S, Srivastava R, Mishra A,
Singh VP, Srivastava AK and Datta M: Elevated hepatic miR-22-3p
expression impairs gluconeogenesis by silencing the Wnt-responsive
transcription factor Tcf7. Diabetes. 64:3659–3669. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Petito G, Cioffi F, Silvestri E, De
Matteis R, Lattanzi D, de Lange P, Lombardi A, Moreno M, Goglia F,
Lanni A and Senese R: 3,5-Diiodo-L-thyronine (T2) administration
affects visceral adipose tissue inflammatory state in rats
receiving long-lasting high-fat diet. Front Endocrinol (Lausanne).
12:7031702021. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Silvestri E, Cioffi F, De Matteis R,
Senese R, de Lange P, Coppola M, Salzano AM, Scaloni A, Ceccarelli
M, Goglia F, et al: 3,5-Diiodo-L-thyronine affects structural and
metabolic features of skeletal muscle mitochondria in high-fat-diet
fed rats producing a co-adaptation to the glycolytic fiber
phenotype. Front Physiol. 9:1942018. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Senese R, Cioffi F, Petito G, de Lange P,
Russo A, Goglia F, Lanni A and Potenza N: miR-22-3p is involved in
gluconeogenic pathway modulated by 3,5-diiodo-L-thyronine (T2). Sci
Rep. 9:166452019. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Zhao T, Wang J, He A, Wang S, Chen Y, Lu
J, Lv J, Li S, Wang J, Qian M, et al: Mebhydrolin ameliorates
glucose homeostasis in type 2 diabetic mice by functioning as a
selective FXR antagonist. Metabolism. 119:1547712021. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Cohen-Naftaly M and Friedman SL: Current
status of novel antifibrotic therapies in patients with chronic
liver disease. Therap Adv Gastroenterol. 4:391–417. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Elpek GÖ: Cellular and molecular
mechanisms in the pathogenesis of liver fibrosis: An update. World
J Gastroenterol. 20:7260–7276. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Higashi T, Friedman SL and Hoshida Y:
Hepatic stellate cells as key target in liver fibrosis. Adv Drug
Deliv Rev. 121:27–42. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Ezhilarasan D: MicroRNA interplay between
hepatic stellate cell quiescence and activation. Eur J Pharmacol.
885:1735072020. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Riaz F, Chen Q, Lu K, Osoro EK, Wu L, Feng
L, Zhao R, Yang L, Zhou Y, He Y, et al: Inhibition of miR-188-5p
alleviates hepatic fibrosis by significantly reducing the
activation and proliferation of HSCs through PTEN/PI3K/AKT pathway.
J Cell Mol Med. 25:4073–4087. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Chen X, Zhu S, Chen SY, Wang JN, Sun LJ,
Tao SM, Li XF, Li HD, Sun YY, Xu CH, et al: miR-301a-3p promotes
hepatic stellate cells activation and liver fibrogenesis via
regulating PTEN/PDGFR-β. Int Immunopharmacol. 110:1090342022.
View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Ju A, Shen Y and Yue A: Circ_0011232
contributes to hepatocellular carcinoma progression through
miR-503-5p/AKT3 axis. Hepatol Res. 52:532–545. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Zheng Y, Cai B, Li X, Li D and Yin G:
MiR-125b-5p and miR-181b-5p inhibit keratinocyte proliferation in
skin by targeting Akt3. Eur J Pharmacol. 862:1726592019. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Zhang Y, Wang F, Chen G, He R and Yang L:
LncRNA MALAT1 promotes osteoarthritis by modulating miR-150-5p/AKT3
axis. Cell Biosci. 9:542019. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Abdullah AS, Sayed IETE, El-Torgoman AMA,
Kalam A, Wageh S and Kamel MA: Green synthesis of
silymarin-chitosan nanoparticles as a new nano formulation with
enhanced anti-fibrotic effects against liver fibrosis. Int J Mol
Sci. 23:54202022. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Abdullah AS, El Sayed IET, El-Torgoman
AMA, Alghamdi NA, Ullah S, Wageh S and Kamel MA: Preparation and
characterization of silymarin-conjugated gold nanoparticles with
enhanced anti-fibrotic therapeutic effects against hepatic fibrosis
in rats: Role of MicroRNAs as molecular targets. Biomedicines.
9:17672021. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Tsuchida T, Lee YA, Fujiwara N, Ybanez M,
Allen B, Martins S, Fiel MI, Goossens N, Chou HI, Hoshida Y and
Friedman SL: A simple diet- and chemical-induced murine NASH model
with rapid progression of steatohepatitis, fibrosis and liver
cancer. J Hepatol. 69:385–395. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Ji D, Li B, Shao Q, Li F, Li Z and Chen G:
MiR-22 suppresses BMP7 in the development of cirrhosis. Cell
Physiol Biochem. 36:1026–1036. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Onakpoya IJ, Heneghan CJ and Aronson JK:
Post-marketing withdrawal of 462 medicinal products because of
adverse drug reactions: A systematic review of the world
literature. BMC Med. 14:102016. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Li X, Tang J and Mao Y: Incidence and risk
factors of drug-induced liver injury. Liver Int. 42:1999–2014.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Kleiner DE: Drug-induced liver injury: The
hepatic pathologist's approach. Gastroenterol Clin North Am.
46:273–296. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Kleiner DE, Chalasani NP, Lee WM, Fontana
RJ, Bonkovsky HL, Watkins PB, Hayashi PH, Davern TJ, Navarro V,
Reddy R, et al: Hepatic histological findings in suspected
drug-induced liver injury: Systematic evaluation and clinical
associations. Hepatology. 59:661–670. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Yang Z, Wu W, Ou P, Wu M, Zeng F, Zhou B
and Wu S: MiR-122-5p knockdown protects against APAP-mediated liver
injury through up-regulating NDRG3. Mol Cell Biochem.
476:1257–1267. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Vliegenthart ADB, Berends C, Potter CMJ,
Kersaudy-Kerhoas M and Dear JW: MicroRNA-122 can be measured in
capillary blood which facilitates point-of-care testing for
drug-induced liver injury. Br J Clin Pharmacol. 83:2027–2033. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Liu Y, Chen H, Hao J, Li Z, Hou T and Hao
H: Characterization and functional prediction of the microRNAs
differentially expressed in a mouse model of concanavalin A-induced
autoimmune hepatitis. Int J Med Sci. 17:2312–2327. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
López-Riera M, Conde I, Tolosa L, Zaragoza
A, Castell JV, Gómez-Lechón MJ and Jover R: New microRNA biomarkers
for drug-induced steatosis and their potential to predict the
contribution of drugs to non-alcoholic fatty liver disease. Front
Pharmacol. 8:32017. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Amacher DE and Chalasani N: Drug-induced
hepatic steatosis. Semin Liver Dis. 34:205–214. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Allard J, Le Guillou D, Begriche K and
Fromenty B: Drug-induced liver injury in obesity and nonalcoholic
fatty liver disease. Adv Pharmacol. 85:75–107. 2019. View Article : Google Scholar : PubMed/NCBI
|