Introduction
Breast cancer remains a leading cause of
cancer-related mortality in women, with a high incidence of
metastasis. In total, 20–30% of patients with early stage breast
cancer develop metastatic disease, and metastatic breast cancer
accounts for the majority of breast cancer-related deaths. However,
metastases of the nasopharynx and nasal cavity are exceedingly
rare, representing <1% of all metastatic breast cancer cases
(1). Primary tumors most frequently
metastasizing to the nasopharynx originate from the lung, liver,
kidney, breast and colon. Among these, lung cancer has the highest
incidence rate of nasopharyngeal metastasis, with it being reported
in 30–40% of cases. Liver cancer follows next, with an incidence of
10–15%, while kidney cancer has an incidence rate of 5–10% of
cases. Colorectal cancer has a relatively low incidence rate,
ranging from 2–5%. Breast cancer is the least frequent, with an
incidence rate of <1% of all nasopharyngeal metastases (2–6). The
current study presents a case of breast cancer metastasizing to the
nasopharynx, alongside a literature review, to explore diagnostic
and therapeutic approaches, and provide valuable clinical
insights.
Case report
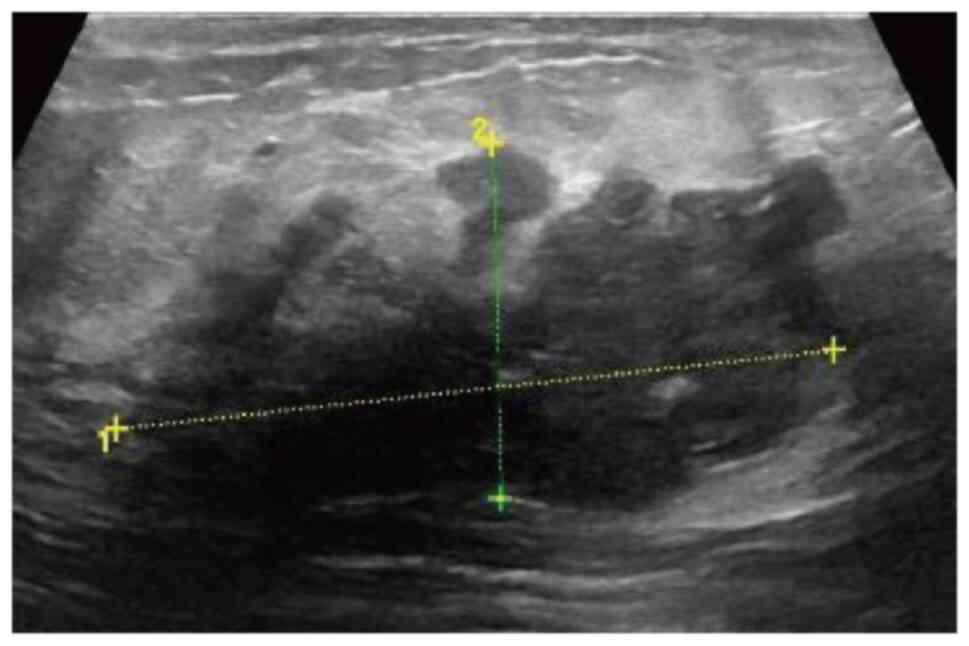
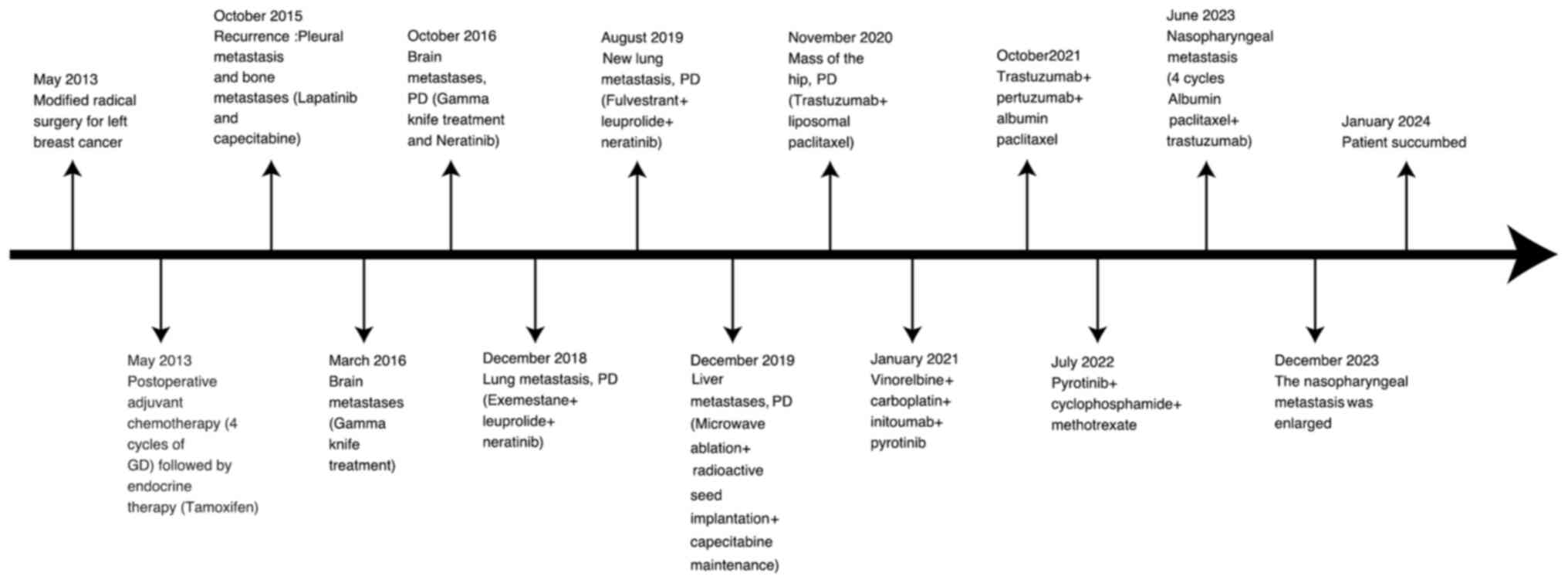
In February 2013, a 53-year-old female patient
detected a progressively enlarging right breast mass (4.0×5.0 cm)
accompanied by distending pain, pruritus, skin ulceration and
reddish nipple discharge. In May 2013, the patient was admitted to
Affiliated Hospital of Shandong Second Medical University (Weifang,
China). A breast ultrasound suggested malignancy, leading to an
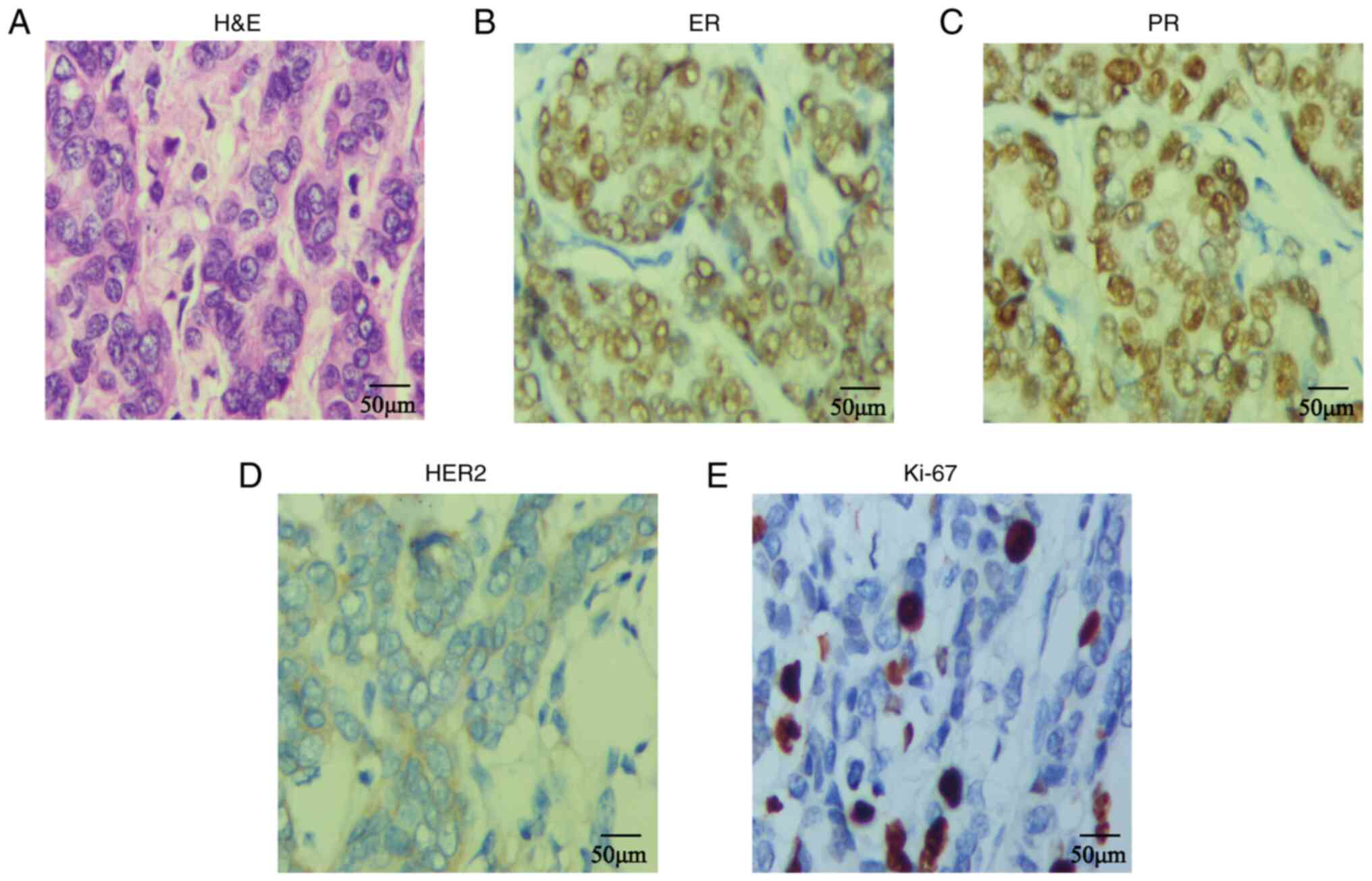
immediate modified radical mastectomy (Fig. 1). Postoperative histopathology
confirmed invasive ductal carcinoma with axillary lymph node
metastasis (4/15 lymph nodes affected). Immunohistochemistry (IHC)
results were positive for estrogen receptor (ER), progesterone
receptor (PR) and human epidermal growth factor receptor 2 (HER2),
with a Ki-67 proliferation index at 30% (Fig. 2). All IHC staining procedures
(Data S1) followed standardized
protocols at the Department of Pathology, Weifang People's Hospital
(Weifang, China). The Tumor-Node-Metastasis stage was classified as
T2N2M0 (stage IIIA) according to the 8th edition of the American
Joint Committee on Cancer Staging Manual (7). The patient underwent four cycles of
gemcitabine plus docetaxel chemotherapy, followed by tamoxifen
therapy.
In October 2015, the patient developed pleural and
bone metastases. IHC (Data S1)
revealed HER2 overexpression. Declining intravenous anti-HER2
therapy, the patient opted for oral lapatinib with capecitabine
after providing informed consent. The patient experienced
sequential metastases to the brain, liver and soft tissue of the
hip. Brain metastases were treated with GammaKnife radiosurgery,
while liver metastases underwent local tumor-reducing therapy
combining microwave ablation with radioactive seed implantation.
The treatment regimen was promptly adjusted in response to disease
progression. Despite treatment, metastatic progression continued.
Regular follow-ups allowed timely treatment adjustments.
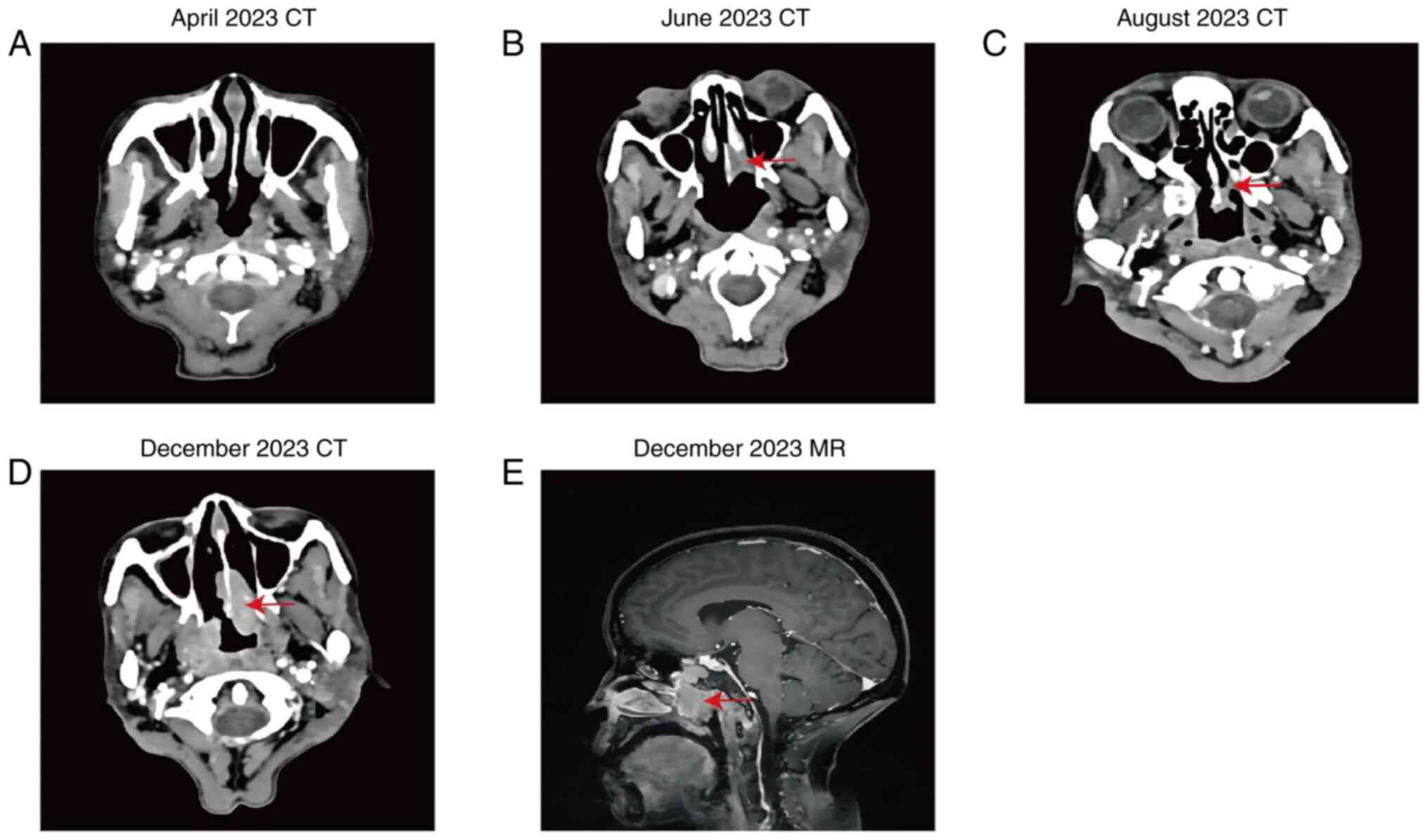
In April 2023, a CT scan of the patient showed no
evidence of a nasopharyngeal mass (Fig.
3A). In June 2023, the patient presented with nasal congestion
and rhinorrhea. A computed tomography (CT) scan detected a
nasopharyngeal soft-tissue mass (Fig.
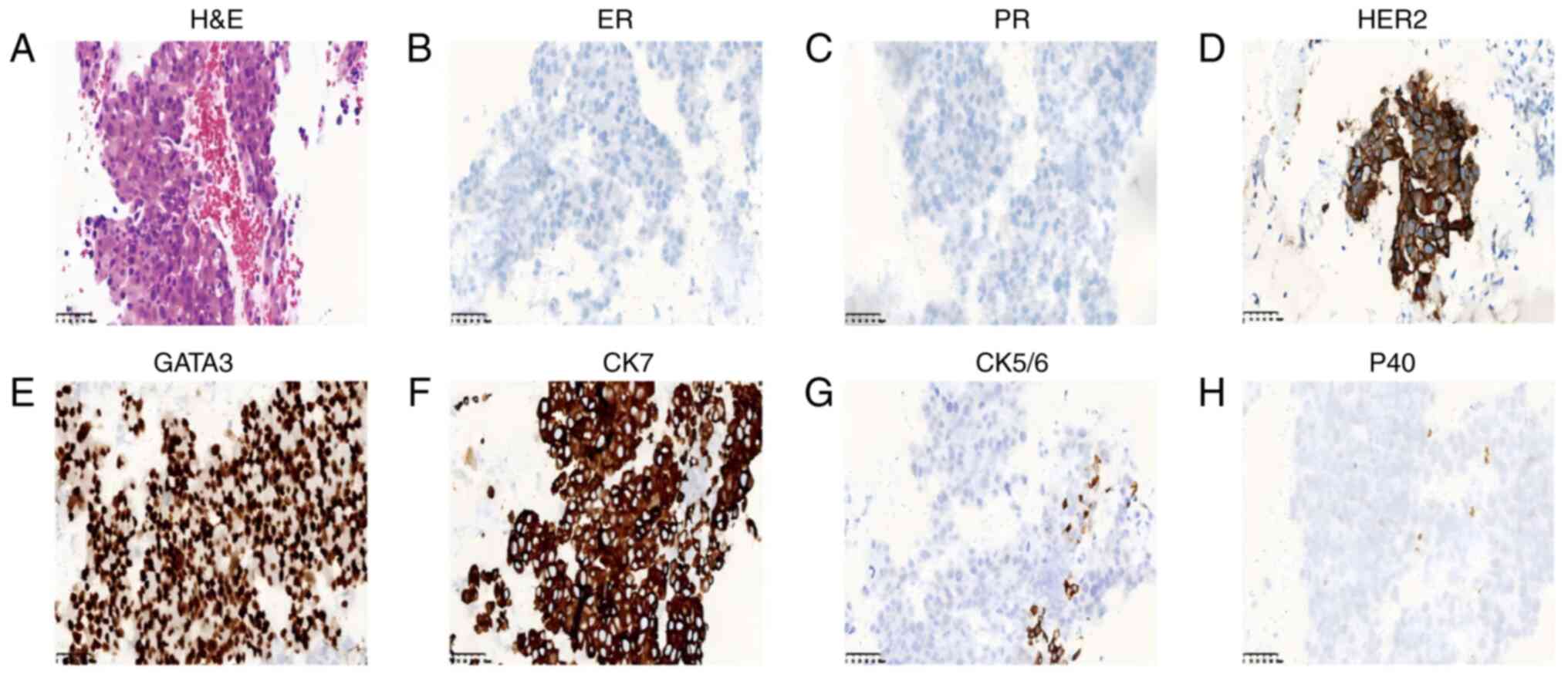
3B). Biopsy findings revealed fragmented mucosal tissue with
scattered atypical cells (Fig. 4A).
The IHC results were as follows: ER(−), PR(−), HER2(3+),
guanine-adenine-thymine-adenine-binding protein 3 [GATA3(+)],
cytokeratin 7 [CK7(+)], CK5/6(focal +) and p40 (sparse +) (Fig. 4; Table
SI; Data S1). Considering the
medical history, histopathology and IHC profile, the diagnosis
confirmed metastatic breast cancer. Later that same month,
treatment was initiated promptly, with four cycles of albumin-bound
paclitaxel and trastuzumab, resulting in a partial tumor response
in August 2023 (Fig. 1C). However,
drug resistance developed, leading to rapid disease progression by
December 2023 (Fig. 1D and E). By
January 2024, after 7 months, the patient was transferred to a
local hospital, where treatment modifications failed to lead to an
improved condition. Despite optimal hospice care, the patient
ultimately passed away at the local hospital. The patient timeline
is presented in Fig. 5. Detailed
treatment protocols are presented in Table I.
 | Table I.A more detailed treatment plan. |
Table I.
A more detailed treatment plan.
| Month and year | Treatment |
|---|
| May 2013 | Modified radical
surgery for left breast cancer |
| May 2013 | Postoperative
adjuvant chemotherapy (4 cycles of GD, no details) followed by
endocrine therapy (10 mg tamoxifen bid po) |
| October 2015 | Recurrence: Pleural
metastasis and bone metastases (1.25 mg lapatinib qd po/25 days and
1.5 g capecitabine bid po days 1–14/21 days) |
| March 2016 | Brain metastases
(Gamma knife treatment) |
| October 2016 | Brain metastases, PD
(Gamma knife treatment and 240 mg neratinib qd po) |
| December 2018 | Lung metastases, PD
(25 mg exemestane qd po + 3.75 mg leuprolide by subcutaneous
injection/q4w + 240 mg neratinib qd po) |
| August 2019 | New lung metastases,
PD (500 mg fulvestrant im/q4w + 3.75 mg leuprolide by subcutaneous
injection/q4w + 240 mg neratinib qd po) |
| December 2019 | Liver metastases, PD
(microwave ablation + radioactive seed implantation + capecitabine
maintenance at 1.5 g bid po days 1–14/21 days) |
| November 2020 | Mass of the hip, PD
(trastuzumab: First time, 8 mg/kg, and after at 6 mg/kg iv drip +
240 mg liposomal paclitaxel day 1 iv drip) |
| January 2021 | Vinorelbine: 30 mg
day 1 and 40 mg day 8 iv drip + 1.5 g carboplatin bid days 1–14/21
days + 8 mg/kg initoumab iv drip + 400 mg pyrotinib qd po |
| October 2021 | 273 mg trastuzumab
day 1 iv drip + 420 mg pertuzumab day 1 iv drip + 370 mg albumin
paclitaxel day 1 iv drip |
| July 2022 | 400 mg pyrotinib qd
po + 20 mg/kg cyclophosphamide q3-4w iv drip + 10 mg methotrexate
q1w po |
| June 2023 | Nasopharyngeal
metastasis (4 cycles 100 mg albumin paclitaxel days 1, 8 and 15
q21d iv drip + 8 mg/kg trastuzumab day 1 iv drip) |
| December 2023 | The nasopharyngeal
metastasis was enlarged |
| January 2024 | Patient
succumbed |
Discussion
Metastasis of breast cancer to the nasopharynx is
exceptionally rare, with only a few documented cases (8–11)
(Table II). Unlike more common
metastatic sites such as the bones, lungs, liver and brain,
nasopharyngeal involvement poses unique diagnostic and therapeutic
challenges. The clinical presentation varies widely and depends on
multiple factors, including the primary tumor stage, tumor
aggressiveness, pathological type, immunohistochemical profile and
extent of invasion. The first reported case of breast cancer
metastasizing to the nasopharynx was described by Saab et al
(1) and initially presented with
cervical lymphadenopathy. The present patient experienced nasal
congestion and rhinorrhea, likely due to tumor-induced growth
obstruction of the nasal cavity. Moreover, metastasis to this site
can remain asymptomatic for an extended period, as observed in a
case reported by Başpinar et al (12) in 2006. Other typical clinical
manifestations include hoarseness, dyspnea, facial cellulitis,
headache, periorbital mass, diplopia, ptosis, facial palsy,
abducent nerve palsy, exophthalmos, vision impairment, headache and
anosmia. The interval between breast cancer diagnosis and the onset
of nasopharyngeal metastases can vary widely, ranging from 10
months to 10 years (Table II).
 | Table II.Cases of nasopharyngeal metastasis
from breast cancer reported in the literature. |
Table II.
Cases of nasopharyngeal metastasis
from breast cancer reported in the literature.
| First author,
publication year | Age, years | Sex | Time
intervala | Presentation | Other metastases | Treatment | Outcome | Survival time after
discovery of nasopharyngeal | (Refs.) |
|---|
| Saab et al,
1987 | 58 | F | 8 years | Enlarged cervical
lymph node | Lungs, sella turcica
and skull base | Radiotherapy and
hormonal therapy | Died | 15 months | (1) |
| Wanamaker et
al, 1993 | i) 77; ii) 44 | i) F; ii) F | i) 16 months; ii) 10
months | i) Hoarseness,
progressive shortness of breath and dyspnea on exertion; ii) facial
cellulitis | i) Bone; ii)
contralateral breasts and lungs | i) Chemotherapy; ii)
chemotherapy | i) Died; ii)
died | i) 14 months; ii) 5
months | (8) |
| Marchioni et
al, 2004 | 78 | F | 6 years | Non-specific
headache, a right periorbital mass, diplopia and ptosis | Lungs | Radiotherapy | Died | 4 months | (15) |
| Başpinar et
al, 2006 | 56 | F | 2 years | A 0.5-cm mass in the
nasopharynx but asymptomatic | Lungs, liver, spleen
and left adrenal gland | Palliative
chemotherapy | Died | 1 months | (12) |
| Liao et al,
2010 | 50 | F | 4 years | Nose bleeding and
nasal congestion | - | Surgery | Alive | Disease-free for 37
months postoperatively | (25) |
| Davey and Baer,
2012 | 75 | F | 2 years | Left facial weakness,
diplopia, nasal obstruction and left abducens nerve palsy | Sphenoid and ethmoid
sinuses | Radiotherapy | Died | - | (9) |
| Tewari et
al, 2013 | 62 | F | 3 years | Blurred vision in
the right eye, proptosis, diplopia and abducent nerve palsy | Meninx, orbit and
bone | Chemotherapy,
bisphosphonate and radiotherapy | - | - | (27) |
| Agrawal et
al, 2015 | 65 | M | 18 months | Severe headache,
postnasal drip, sinus fullness and dry chronic cough | Lungs, bone and
liver | Palliative
chemotherapy and hormonal therapy | Died | 1 year | (10) |
| Alaoui Slimani
et al, 2016 | 65 | F | 3 years | Severe headache and
bilateral blindness | Bone and lungs | Palliative
chemotherapy | Died | - | (11) |
| Copson et
al, 2018 | 52 | F | 5 years | Nasal obstruction,
anosmia, rhinorrhea and right facial paresthesia | Skull base,
anterior cranial fossa, liver and lungs | Immunotherapy and
palliative chemotherapy | - | - | (16) |
| Sellami et
al, 2025 | 52 | F | 2 years | Headache,
unilateral hearing loss, otalgia | Bone | Palliative
chemotherapy | Alive | - | (26) |
| Present case,
2025 | 53 | F | 10 years | Nasal obstruction
and rhinorrhea | Bone, brain, liver
and hip | Targeted therapy,
chemotherapy and hormonal therapy | Died | 7 months |
|
Due to the rarity of nasopharyngeal metastatic
tumors and their frequent submucosal location, CT and magnetic
resonance imaging fail to provide distinct diagnostic features.
Positron emission tomography-CT remains the most effective imaging
modality for evaluating systemic metastases, detecting disease
recurrence, assessing tumor burden and identifying distant lesions
(13). However, its high cost and
the potential for false-positive results due to inflammatory
conditions complicate the diagnosis. The clinical manifestations of
metastatic nasopharyngeal tumors closely resemble those of
non-specific nasal inflammation and upper respiratory tract
infections, frequently presenting with facial pain, epistaxis,
nasal congestion and rhinorrhea. When differentiation proves
challenging, an empirical anti-infective treatment may be
attempted. If symptoms persist, primary or secondary nasopharyngeal
tumors must be strongly suspected. Given their high expression in
breast tissue, IHC markers such as gross cystic disease fluid
protein 15 and GATA3 are crucial in distinguishing breast cancer
metastases (14). There is limited
evidence suggesting that increased CK expression in metastatic
lesions may indicate a predilection for nasopharyngeal
colonization, as CK serves as a key immunomarker for nasopharyngeal
squamous cell carcinoma. The patients in the studies by Marchioni
et al (15) and Copson et
al (16), and the present
patient, all exhibited increased CK/CK7 expression, further
supporting the potential role of CK/CK7 in the metastatic process.
However, this phenomenon's mechanisms require further investigation
(Table III). A thorough
histopathological assessment, IHC analysis and a high index of
suspicion are essential for accurately diagnosing nasopharyngeal
metastases. The IHC profiles may differ from those of the primary
tumor, exhibiting partial or complete heterogeneity. In a case
reported by Copson et al (16), the only IHC difference between the
primary breast cancer tumor and its nasopharyngeal metastasis was
the HER2 expression, with HER2 positivity observed in the
nasopharyngeal metastasis but lacking in the primary tumor, while
the expression of estrogen and progesterone receptors remained
consistent in both tissues. Significant discrepancies in hormone
receptor and HER2 status have been observed between primary breast
cancer and secondary nasopharyngeal lesions. While it was
previously believed that HER2 status remained consistent between
primary and metastatic tumors, recent findings challenge this
assumption (17). However, up to
25% of patients exhibit discrepancies in IHC results (17,18),
with inconsistencies in ER and PR expression being more prevalent
than those in HER2 (19). In the
present patient, prolonged secretion of ER and PR may have
contributed to the suppression of hormone receptor expression. The
heterogeneity of HER2 refers to variations in expression or
amplification across different tumor sites, time points or within
the same patient. This phenomenon has been extensively documented
in previous studies and has been observed in up to 34% of breast
cancer cases (20–23). Undetected HER2-amplified subclones
were hypothesized to exist in the original pathological samples.
This may be due to the fact that in genetic or tumor heterogeneity,
chemotherapy selectively targets most HER2-related primary tumor
cells, potentially enriching HER2-overexpressing clones. Moreover,
long-term antitumor therapy may induce alterations in the tumor
microenvironment, further contributing to these changes (24).
 | Table III.Immunohistochemical profile of the
primary breast lesion and its nasopharyngeal metastasis in the
present case and previous literature. |
Table III.
Immunohistochemical profile of the
primary breast lesion and its nasopharyngeal metastasis in the
present case and previous literature.
| First author,
publication year | Primary tumor | Metastasis | (Refs.) |
|---|
| Saab et al,
1987 | - | - | (1) |
| Wanamaker et
al, 1993 | - | - | (8) |
| Marchioni et
al, 2004 | ER(+), PR(+),
HER2(−) | ER(+), PR(+),
HER2(−), CK(3+), GCDFP-15(1+/2+), p53(3+) | (15) |
| Başpinar et
al, 2006 | - | - | (12) |
| Liao et al,
2010 | ER(−), PR(−),
HER2(2+) | ER(2+), PR(−),
HER2(2+) | (25) |
| Davey and
Baer, 2012 | ER(+), PR(+),
HER2(−) | ER(+), PR(+),
HER2(−) | (9) |
| Tewari et
al, 2013 | ER(+), PR(+),
HER2(−) | - | (27) |
| Agrawal et
al, 2015 | ER(+), PR(+),
HER2(−) | ER(+), PR(+),
HER2(−) | (10) |
| Alaoui Slimani
et al, 2016 | - | - | (11) |
| Copson et
al, 2018 | ER(−), PR(−),
HER2(−) | CK 7(+), ER(−),
PR(−), HER2(3+) | (16) |
| Sellami et
al, 2025 | ER(+), PR(+),
HER2(−) | ER(+), PR(+),
HER2(−), p63(−), GATA3(+) | (26) |
| Present case,
2025 | ER(+), PR(+),
HER2(+) | ER(−), PR(−),
HER2(3+), GATA3(3+), CK7(3+), CK5/6(+), p40(+) |
|
Treatment strategies vary across studies due to the
rarity of nasopharyngeal metastases from breast cancer. Therapeutic
selection depends on multiple factors, including the tumor's
hormonal and HER2 status, the local invasion extent and other
metastatic sites. The present study describes the patient treatment
in detail, hoping to enlighten the general medical staff in the
treatment of such patients (Table
I). To date, to the best of our knowledge, only one case was
reported with isolated breast cancer metastasis to the nasopharynx,
involved a 54-year-old woman who underwent surgical resection
(25). The patient remained
disease-free for 37 months postoperatively, suggesting that
surgical intervention may be a viable option for solitary
nasopharyngeal metastases. However, most patients present with
multiple metastases, limiting surgical feasibility. The present
patient received four cycles of albumin-bound paclitaxel combined
with trastuzumab, initially achieving a partial response. However,
the nasopharyngeal tumor eventually developed drug resistance and
progressed rapidly. As observed in previous cases, despite
multimodal treatment, including chemotherapy, targeted therapy and
radiotherapy, the prognosis remained poor. Given the limited number
of reported cases, standardized treatment guidelines have yet to be
established. The management is currently individualized,
integrating targeted therapy, radiotherapy, chemotherapy,
immunotherapy and endocrine therapy, with multidisciplinary
collaboration being essential for treatment planning (26). Early detection and intervention are
critical for improving the patient prognosis (27).
In summary, the present case highlights the need to
consider nasopharyngeal metastasis in patients with a history of
breast cancer presenting with nasal or auditory symptoms. Prompt
diagnosis and targeted therapy are essential for enhancing quality
of life and prolonging survival. Further research is required to
establish optimal management strategies for this rare metastatic
presentation.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
YB conceptualized and designed the study, and
drafted the manuscript. GY provided methodological guidance and
revised the manuscript. CS obtained the medical imaging data. YN
and XS conducted the analysis of the patient's clinical data. FH
and GY were involved in the development of the patient's subsequent
treatment strategy and participated in the medical decision-making
process. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient to publish this case report and any accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Saab GA, Abdul-Karim FW and Samara M:
Breast carcinoma metastatic to the nasopharynx. J Laryngol Otol.
101:723–725. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rakha EA and Chan S: Metastatic
triple-negative breast cancer. Clin Oncol (R Coll Radiol).
23:587–600. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ridlon HC and McAdams GB: Breast carcinoma
metastatic to kidney. J Urol. 98:328–330. 1967. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Iqneibi S, Nazzal J, Amoudi R, Owda B,
Al-Ibraheem A, Yaser S and Al-Hussaini M: Metastatic pulmonary
adenocarcinoma to the nasopharynx at first clinical presentation: A
case report and review of literature. SAGE Open Med Case Rep.
8:2050313X209398262020. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Agrawal S and Jayant K: Breast cancer with
metastasis to the nasopharynx and paranasal sinuses. Breast J.
22:476–477. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Liu YH, Lin BB and Lv SX: Nasopharyngeal
metastasis from colorectal cancer: A case report. Ann Palliat Med.
10:4911–4816. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Amin MB, Edge SB and Greene FL: AJCC
cancer staging manual. Breast Cancer. 8th edition. Springer; New
York, NY: pp. 589–636. 2017
|
|
8
|
Wanamaker JR, Kraus DH, Eliachar I and
Lavertu P: Manifestations of metastatic breast carcinoma to the
head and neck. Head Neck. 15:257–262. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Davey S and Baer S: A rare case of breast
cancer metastasising to the nasopharynx and paranasal sinuses. Int
J Surg Case Rep. 3:460–462. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Agrawal S, Jayant K, Agarwal RK, Dayama KG
and Arora S: An unusual case of metastatic male breast cancer to
the nasopharynx-review of literature. Ann Palliat Med. 4:233–238.
2015.PubMed/NCBI
|
|
11
|
Alaoui Slimani K, Debbagh A, Sbitti Y,
Errihani H and Ichou M: Male breast cancer in Morocco: Epidemiology
and prognostic factors. A report of 140 cases. Gynecol Obstet
Fertil. 44:636–640. 2016.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Başpinar Ş, Kapucuoğlu N, Karahan N, Yasan
H, Coşkun S and Çandir Ö: Breast carcinoma metastatic to
nasopharynx. Turk J Pathol. 22:196–199. 2006.
|
|
13
|
Shen G, Zhang W, Jia Z, Li J, Wang Q and
Deng H: Meta-analysis of diagnostic value of 18F-FDG PET or PET/CT
for detecting lymph node and distant metastases in patients with
nasopharyngeal carcinoma. Br J Radiol. 87:201402962014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Cimino-Mathews A, Subhawong AP, Illei PB,
Sharma R, Halushka MK, Vang R, Fetting JH, Park BH and Argani P:
GATA3 expression in breast carcinoma: utility in triple-negative,
sarcomatoid, and metastatic carcinomas. Hum Pathol. 44:1341–1349.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Marchioni D, Monzani D, Rossi G, Rivasi F
and Presutti L: Breast carcinoma metastases in paranasal sinuses, a
rare occurrence mimicking a primary nasal malignancy. Case report.
Acta Otorhinolaryngol Ital. 24:87–91. 2004.PubMed/NCBI
|
|
16
|
Copson B, Pratap U, McLean C and Hayes T:
Nasopharyngeal metastasis of breast carcinoma with HER 2
discordance: A case report. ANZ J Surg. 88:508–509. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Regitnig P, Schippinger W, Lindbauer M,
Samonigg H and Lax SF: Change of HER-2/neu status in a subset of
distant metastases from breast carcinomas. J Pathol. 203:918–926.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Aurilio G, Disalvatore D, Pruneri G,
Bagnardi V, Viale G, Curigliano G, Adamoli L, Munzone E,
Sciandivasci A, De Vita F, et al: A meta-analysis of oestrogen
receptor, progesterone receptor and human epidermal growth factor
receptor 2 discordance between primary breast cancer and
metastases. Eur J Cancer. 50:277–289. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Amir E, Miller N, Geddie W, Freedman O,
Kassam F, Simmons C, Oldfield M, Dranitsaris G, Tomlinson G,
Laupacis A, et al: Prospective study evaluating the impact of
tissue confirmation of metastatic disease in patients with breast
cancer. J Clin Oncol. 30:587–592. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Allison KH, Dintzis SM and Schmidt RA:
Frequency of HER2 heterogeneity by fluorescence in situ
hybridization according to CAP expert panel recommendations: Time
for a new look at how to report heterogeneity. Am J Clin Pathol.
136:864–871. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ohlschlegel C, Zahel K, Kradolfer D, Hell
M and Jochum W: HER2 genetic heterogeneity in breast carcinoma. J
Clin Pathol. 64:1112–1116. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Seol H, Lee HJ, Choi Y, Lee HE, Kim YJ,
Kim JH, Kang E, Kim SW and Park SY: Intratumoral heterogeneity of
HER2 gene amplification in breast cancer: Its clinicopathological
significance. Mod Pathol. 25:938–948. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lee HJ, Seo AN, Kim EJ, Jang MH, Suh KJ,
Ryu HS, Kim YJ, Kim JH, Im SA, Gong G, et al: HER2 heterogeneity
affects trastuzumab responses and survival in patients with
HER2-positive metastatic breast cancer. Am J Clin Pathol.
142:755–766. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Vitale I, Shema E, Loi S and Galluzzi L:
Intratumoral heterogeneity in cancer progression and response to
immunotherapy. Nat Med. 27:212–224. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Liao HS, Hsueh C, Chen SC, Chen IH, Liao
CT and Huang SF: Solitary nasal cavity metastasis of breast cancer.
Breast J. 16:321–322. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sellami M, Kallel S, Ben Ayed M, Mellouli
M, Boudawara TS, Mnejja M, Hammami B, Achour I and Charfeddine I:
Nasopharyngeal metastasis from breast carcinoma: A case report and
a review of the literature. Ear Nose Throat J. 104 (Suppl
1):80S–84S. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Tewari A, Subramanyam P, Palaniswamy SS
and Satheesh TS: Nasopharynx-A rare site of metastases from
carcinoma breast. Egypt J Ear Nose Throat Allied Sci. 14:143–146.
2013. View Article : Google Scholar
|