Introduction
Osteosarcoma is recognized as the most prevalent
type of malignant bone tumor, with a notably higher incidence in
adolescents aged 15–19 years, presenting with a male-to-female
ratio of 1.4:1 (1). In young
patients aged 15–19 years, osteosarcoma predominantly arises in the
extremities, particularly around the knee, and the lungs serve as
the most common site for metastasis, followed by distant bones
(2). The diagnosis of osteosarcoma
mainly relies on pathological examination and treatment protocols
are tailored according to the stage of the tumor. In recent years,
neoadjuvant chemotherapy, combined with limb-salvage surgery, has
emerged as the primary treatment approach for early-stage
osteosarcoma (3). However, the
deep-seated location of the tumor and the intricacies of
surrounding anatomical structures often render complete surgical
removal challenging, which may result in both physical and
psychological trauma to the patient (4). Additionally, systemic chemotherapy can
lead to complications, such as renal, cardiac and auditory
dysfunction (5). Despite notable
advancements in surgical techniques and chemotherapy agents in
recent decades, the overall prognosis for osteosarcoma remains less
than ideal. Consequently, there exists some debate regarding the
most appropriate treatment strategy.
The rapid advancement of local treatment
technologies has highlighted the benefits of transarterial
chemoembolization (TACE) and iodine-125 seed implantation in
enhancing local tumor control rates and minimizing treatment
toxicity (6,7). These approaches have demonstrated
considerable clinical value, particularly in the management of
hypervascular tumors. TACE embolization involves administering
chemotherapy drugs directly through the tumor-feeding artery in
combination with vascular embolization techniques. This method
achieves multiple therapeutic effects, such as increasing local
drug concentrations, reducing systemic toxicity and obstructing the
blood supply of the tumor (6).
Iodine-125 seed implantation is a type of brachytherapy that
entails implanting radioactive seeds into the tumor under imaging
guidance. These iodine-125 seeds continuously emit low-dose γ rays,
inducing DNA breakage and damage within the tumor by generating
free radicals (7). This mechanism
allows for the radiation dose to be concentrated precisely on the
tumor. Given that the effective radius of the iodine-125 seed is
only 1.7 cm, it can effectively target the tumor while minimizing
damage to surrounding healthy tissues (8).
To the best of our knowledge, there have been no
documented cases of osteosarcoma treated with a combination of TACE
and iodine-125 seed therapy. The present study describes a detailed
case of a patient with osteosarcoma who received this combined
treatment. In addition, the clinical application and advantages of
this method in improving local tumor control rates and reducing
side effects are discussed in the current study. The successful
outcome of the present case offers valuable insights and serves as
a reference for future clinical research.
Case report
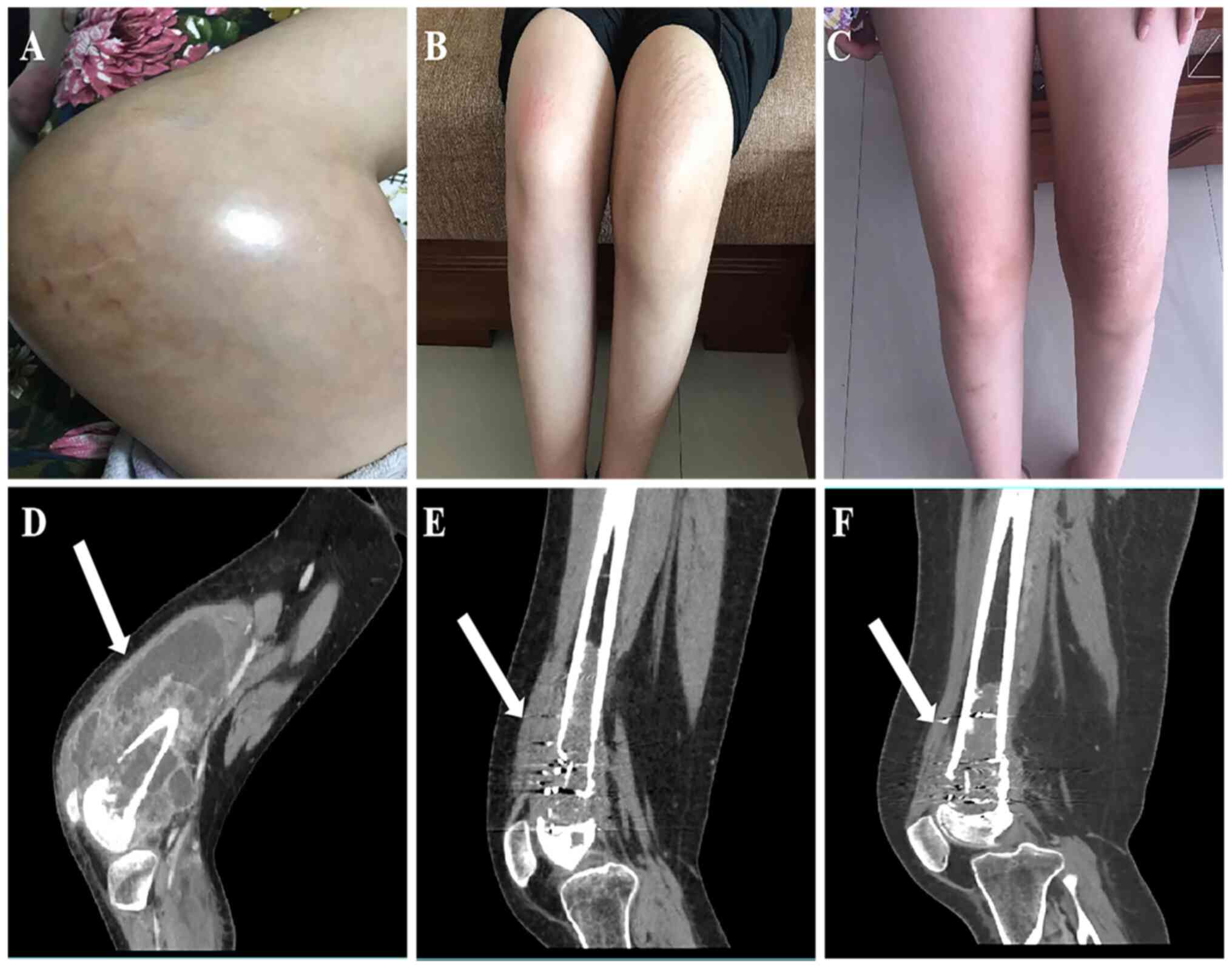
In September 2018, a 13-year-old female patient
presented to Banan District Third People's Hospital (Chongqing,
China) with a 3-month history of swelling in the left knee joint
(Fig. 1A and D). The swelling
progressively worsened, accompanied by severe pain rated 8 on the
Numeric Rating Scale (NRS) (9),
which gradually impacted their gait. An MRI conducted at the local
hospital revealed osteolysis of the lower left femur with
surrounding soft tissue masses, the largest measuring 12.6 cm,
suggesting a malignant tumor. Following the initial assessment, a
CT-guided puncture biopsy was carried out on the left femoral mass,
and the pathological results established the diagnosis of a
high-grade osteosarcoma. The local hospital recommended amputation;
however, the patient declined the procedure. In search of further
treatment options, the patient presented to Banan Hospital of
Chongqing Medical University (Chongqing, China) in October 2018.
Laboratory tests revealed elevated levels of alkaline phosphatase
(ALP) at 1,752 U/l (reference range: 30–130 U/l) and lactate
dehydrogenase (LDH) at 735 U/l (reference range: 120–250 U/l),
while all other tests (e.g., bilirubin, ALT, AST and reticulocyte
counts) returned normal results. Based on the American Joint
Committee on Cancer staging system for malignant tumors (10,11)
and the Enneking grading system (12), the patient was classified as having
stage IIB osteosarcoma. After a multidisciplinary team discussion,
it was recommended that the patient undergo neoadjuvant
chemotherapy followed by limb-sparing surgery, in accordance with
current treatment guidelines, especially considering the invasion
of the tumor into surrounding blood vessels. However, the patient
refused surgical intervention due to psychological and other
personal reasons. Consequently, an alternative treatment plan was
formulated, consisting of TACE and iodine-125 seed implantation,
complemented by systemic intravenous chemotherapy; the treatment
process is shown in Fig. S1. The
team clearly communicated to the patient and their guardians the
structural instability of the femur and the possibility of
spontaneous fracture occurring under minimal stress. The discussion
highlighted that pathological fractures could result in notable
pain, functional impairment and complications in future treatment.
To mitigate these risks, the patient was advised to completely
avoid weight-bearing on the affected limb, and to use crutches for
mobility to minimize mechanical stress on the femur. The patient
and their family acknowledged the associated risks and agreed to
adhere strictly to the recommended precautions.
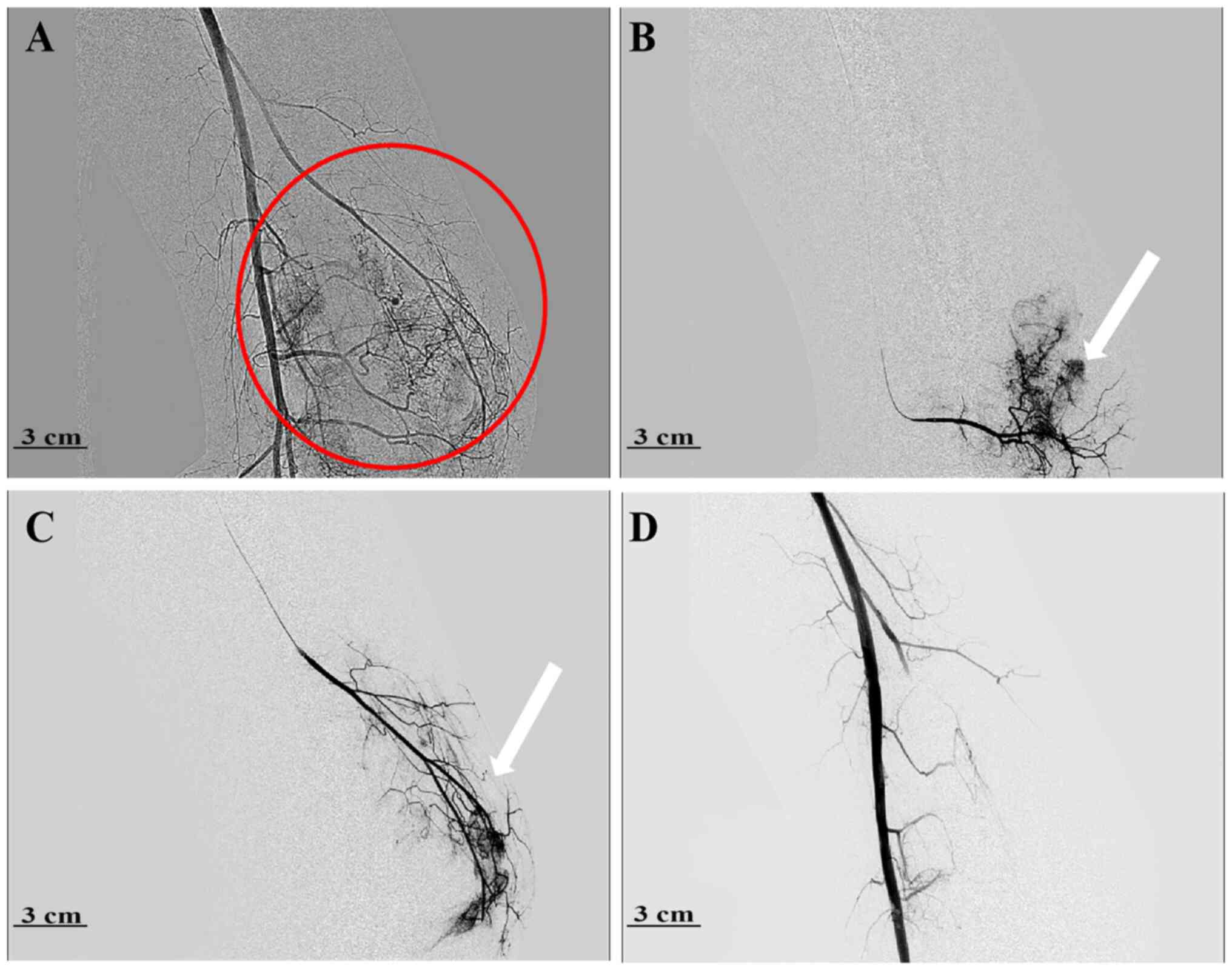
In October 2018, on day 6 following admission, the
patient underwent left femoral TACE, guided by a digital
subtraction angiography (DSA) machine (Allura Xper FD20; Philips
Medical Systems, Inc.). The right femoral artery was punctured
under local anesthesia, and a 5 F femoral artery sheath (Terumo
Corporation) was introduced. Subsequently, a 5 F vertebral catheter
(Terumo Corporation) was utilized for super-selective
catheterization of the left superficial femoral artery.
Angiographic imaging revealed multiple branch vessels from the left
superficial femoral artery supplying the tumor. The vertebral
catheter was positioned within the left superficial femoral artery,
allowing for the administration of the first-line chemotherapy
regimen for osteosarcoma: Methotrexate, doxorubicin and cisplatin
(MAP), via continuous arterial infusion. This regimen included
cisplatin at 120 mg/m2 (administered continuously for 24
h on the day 1), doxorubicin at 37.5 mg/m2 (maintained
for 24 h on day 2) and methotrexate at 12 g/kg (administered over
24 h on day 3). During the chemotherapy infusion, the patient
received daily subcutaneous injections of low-molecular-weight
heparin sodium at 3,000 U for anticoagulation. After completing the
arterial infusion chemotherapy, a 2.7 F microcatheter (Hunan APT
Medical Inc.) was used for super-selective catheterization of the
tumor-supplying arteries under DSA guidance. Embolization was
carried out using 300–500 µm embolization microspheres (Jiangsu
Hengrui Pharmaceuticals Co., Ltd.) until the tumor-supplying
arteries were no longer visible and the vessels appeared tapered
(Fig. 2). In December 2018, a
repeat of the aforementioned procedure was performed for the second
TACE treatment.
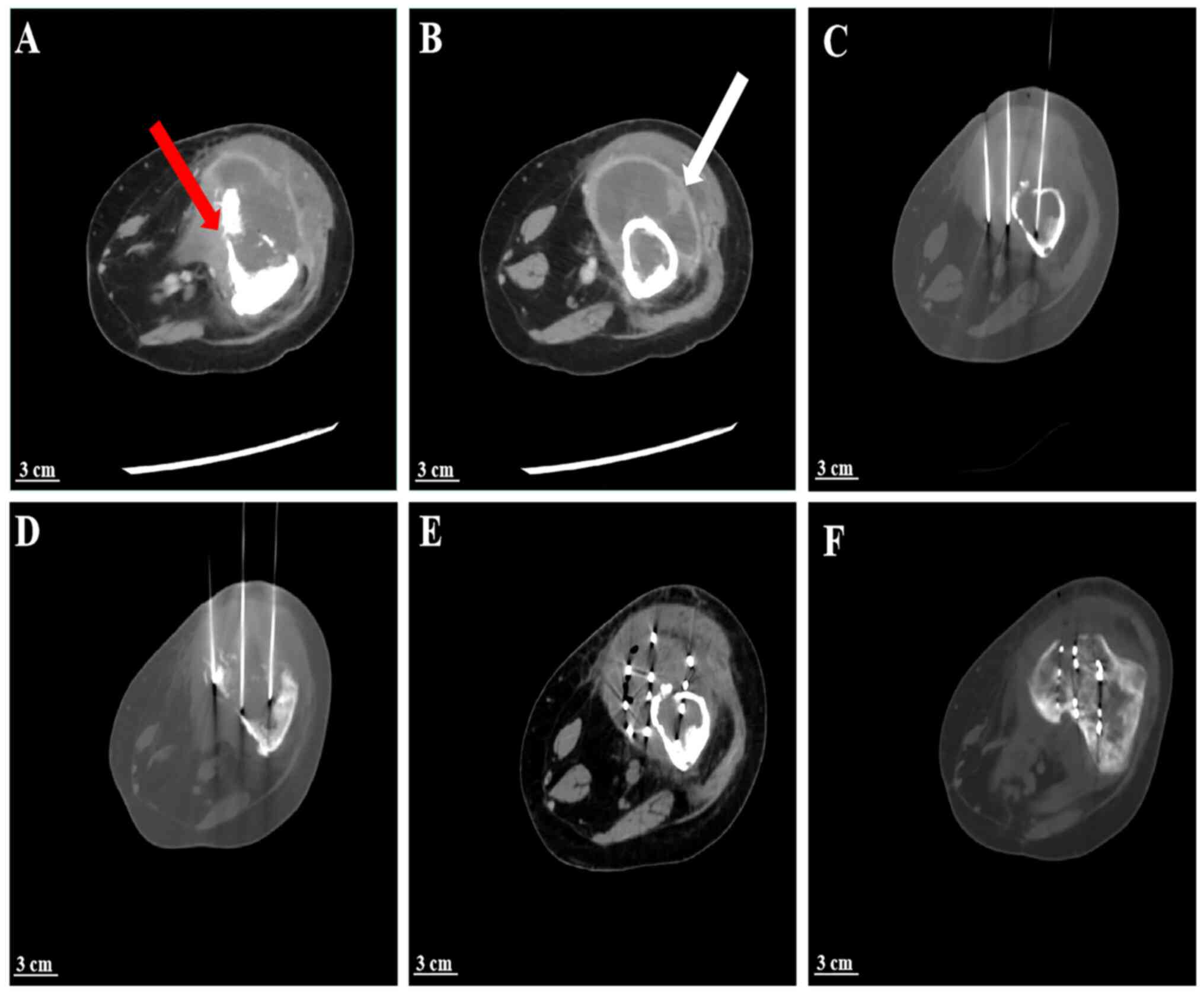
After two TACE treatments, at the time of follow-up
in January 2019, the left knee swelling was considerably
diminished, and the pain score was decreased to 4, as measured
using the NRS. Enhanced CT follow-up (Fig. 3A and B) revealed a notable reduction
in tumor blood supply and a decrease in the maximum tumor diameter.
Subsequently, a plan for iodine-125 seed implantation was developed
for the patient. Prior to the procedure, a treatment planning
system (Beijing Tianhang Kelin Technology Development Co., Ltd.)
was utilized to establish the initial implantation strategy. During
surgery, guidance was provided using a GE Revolution HD CT (GE
Healthcare), with a 5-mm slice thickness chosen for spiral
scanning. A total of 80 iodine-125 seeds, each with an activity of
0.8 mCi, were implanted to achieve a prescribed dose of 140 Gy
(Fig. 3C-F). A total of 3 days
post-iodine-125 seed implantation, the MAP regimen for systemic
intravenous chemotherapy was initiated. However, on day 1 of
chemotherapy, the patient experienced nausea and vomiting.
Antiemetic medications, such as ondansetron (8 mg administered
intravenously once daily) and metoclopramide hydrochloride (5 mg
administered orally three times/day), were administered as
adjunctive therapy, and adjustments were made to the chemotherapy
drug dosages. However, despite these interventions, the patient
could not endure the side effects of the chemotherapy drugs and was
therefore unable to persist with the treatment.
In February, June and September 2019, the patient
underwent additional iodine-125 seed implantations due to enhanced
CT follow-ups (Fig. 1B and E)
indicating areas of sparse particle distribution. A total of 30, 50
and 40 seeds were implanted during these procedures, respectively.
Throughout the subsequent treatments, the patient declined systemic
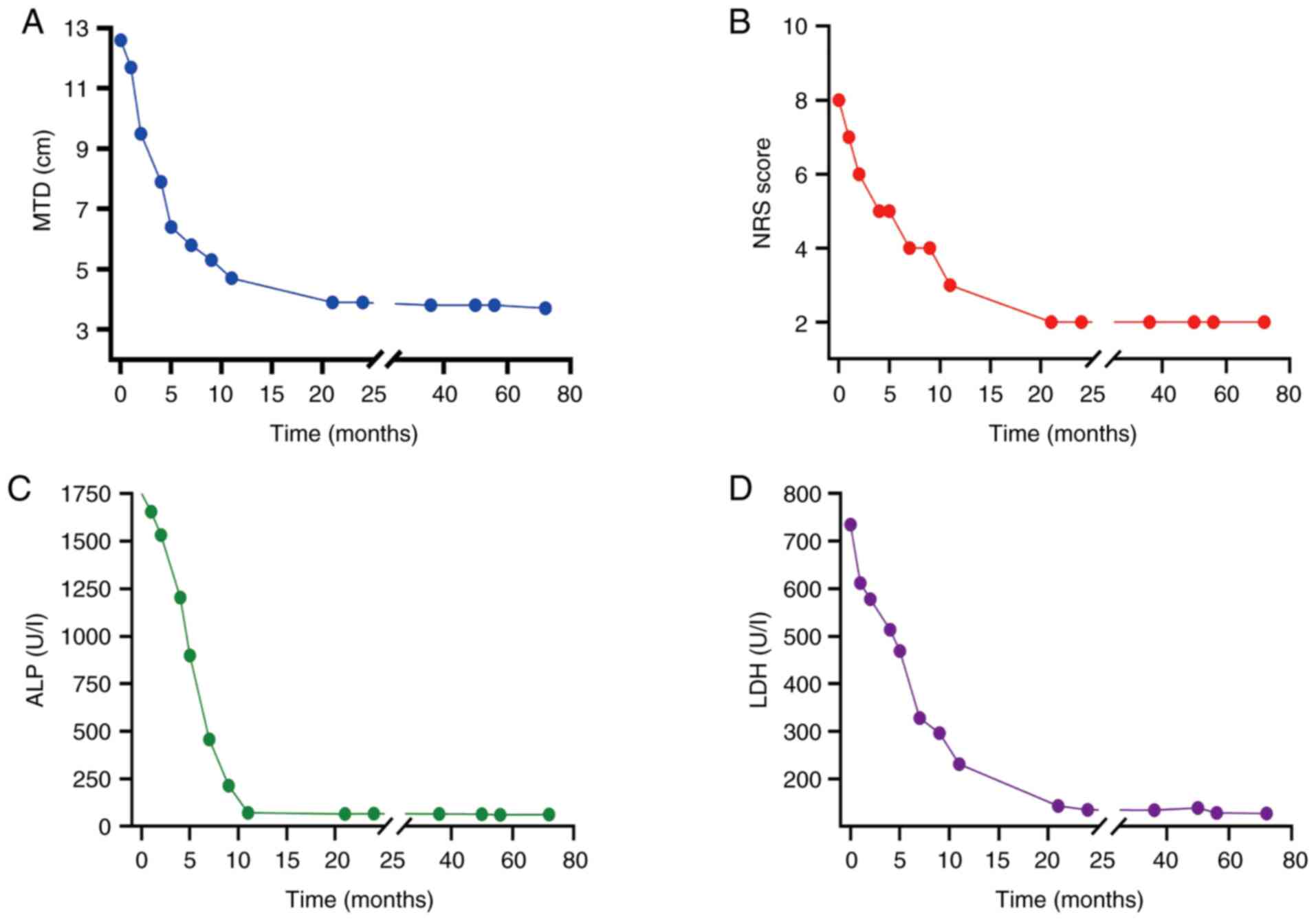
intravenous chemotherapy. After 11 months of treatment, follow-up
imaging, in accordance with the Response Evaluation Criteria in
Solid Tumors version 1.1 (13),
revealed a marked reduction in tumor volume. The patient was able
to walk using a single crutch, and there was a marked improvement
in quality of life (Fig. 1C and F).
The pain score had decreased to 2, as measured using the NRS, and
both ALP and LDH levels progressively returned to normal ranges
(Fig. 4), the rest of the
laboratory tests were normal. The patient continued to have
follow-up examinations every 6 months. In year 2 following surgery,
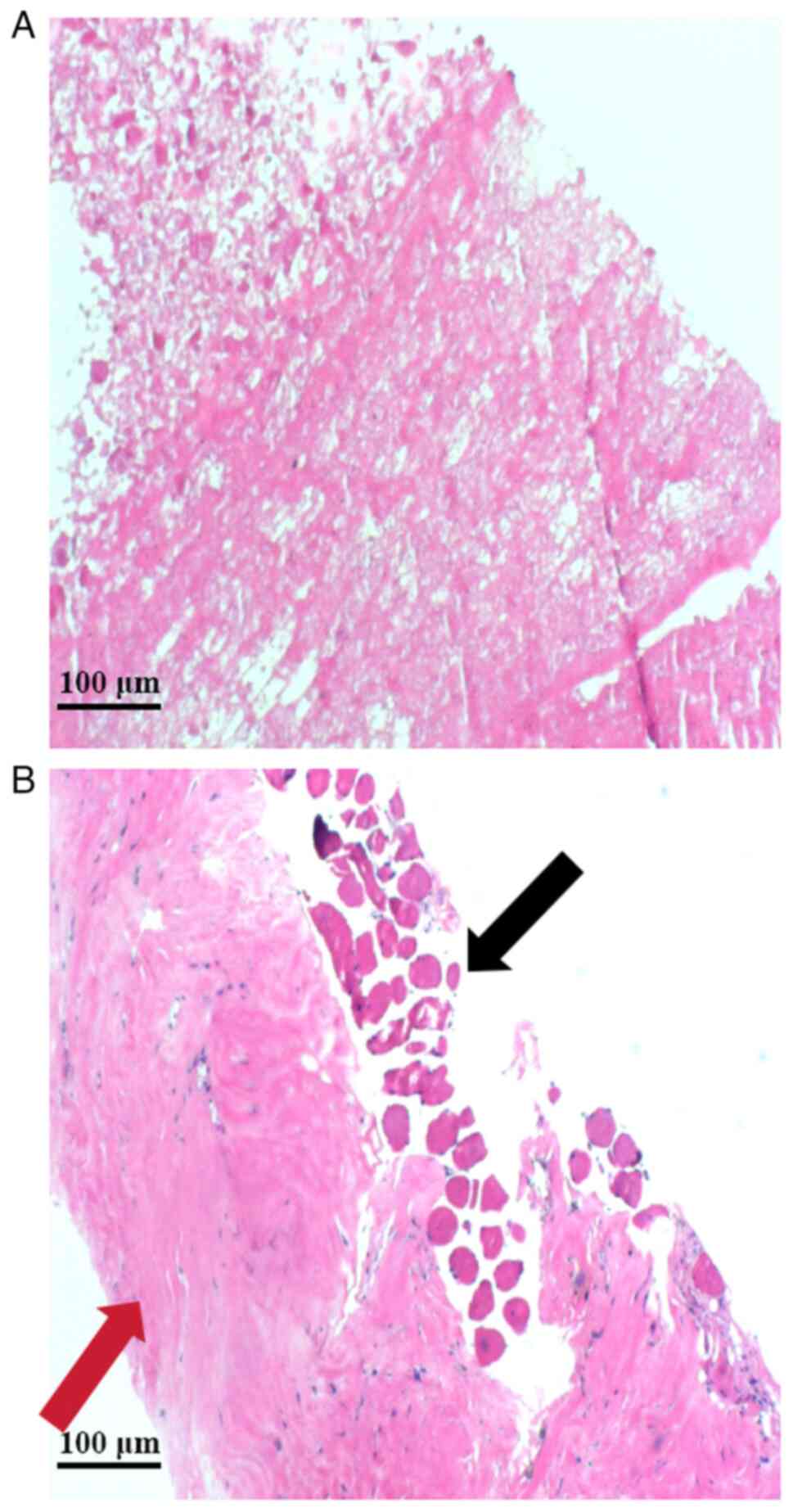
a repeat biopsy was conducted. Tissue samples were preserved in
neutral formalin (4% formaldehyde solution) for 24 h at 20–25°C.
The samples underwent graded alcohol dehydration (70, 80, 90, 95
and 100%), were embedded with paraffin and sliced into 3–4 µm
sections. For hematoxylin staining, the sections were submerged in
Harris Hematoxylin Stain for 5–10 min, followed by eosin staining
(0.5–1% alcohol solution) for 1–3 min at room temperature
(20–25°C). Finally, the samples were sealed with neutral gum and
examined under a light microscope. The tissue was predominantly
characterized by collagen degeneration and sclerosis, a small
amount of muscle tissue was noticed at the periphery, and
importantly, no residual tumor cells were detected, indicating that
the patient had achieved a pathological complete response (Fig. 5). In addition, the patient regained
independent ambulation, with their knee range of motion improving
from 30–90° pre-treatment to 0–110° post-treatment. As of the last
follow-up in December 2024, the patient has remained stable for
>6 years and no secondary tumors were observed.
Discussion
Osteosarcoma is a highly malignant primary bone
tumor that primarily affects adolescents. It is characterized by
rapid progression, notable local invasiveness and a high likelihood
of distant metastasis (1).
Currently, the typical treatment approach involves a combination of
surgery, radiotherapy and chemotherapy. However, surgical resection
often necessitates extensive tissue removal, which can result in
asymmetrical limb growth, considerable functional loss and a
profound psychological impact on the patient (4). Additionally, multi-cycle systemic
chemotherapy is frequently accompanied by severe side effects,
which can greatly affect the quality of life of the patient.
Although radiotherapy can help control local tumor growth, its
effectiveness is limited and it may also cause damage to
surrounding healthy tissues (14).
Consequently, current research efforts have focused on maximizing
the preservation of limb function while minimizing
treatment-related toxicities, all while ensuring therapeutic
efficacy.
In recent years, the combination of neoadjuvant
chemotherapy with limb-saving surgery has enhanced disease-free
survival rates for patients with osteosarcoma. A study conducted by
Smeland et al (15) reported
3- and 5-year event-free survival rates of 59 and 54%,
respectively, with this combined therapeutic approach. Limb-saving
surgery marks a substantial advancement in the treatment of
osteosarcoma, offering a balance between effective cancer
management and the preservation of limb function, thus markedly
improving the quality of life for young patients. However, this
approach also presents challenges related to growth and long-term
health. Research using a mouse model of osteosarcoma (16) has indicated that the surgical
removal of the primary tumor could accelerate the growth of lung
metastases, suggesting that surgery may alter the immune
microenvironment, thereby promoting tumor metastasis. Additionally,
it has been demonstrated that children who undergo limb-saving
surgery are at risk of developing chronic health conditions later
in life, such as cardiovascular diseases and secondary
malignancies. These risks are likely attributed to the toxic
effects of chemotherapy drugs, and multi-cycle chemotherapy can
exacerbate these health concerns for patients (17). Gaspar et al (18) reported that in the treatment of
refractory or recurrent osteosarcoma with lenvatinib combined with
etoposide and ifosfamide, 27 out of 35 patients (77%) experienced
neutropenia, 25 patients (71%) suffered from thrombocytopenia, 19
patients (54%) had anemia and 19 patients (54%) saw a decrease in
white blood cell count. These findings indicate the toxic side
effects associated with chemotherapy agents.
TACE has shown marked efficacy in treating various
malignancies, including liver and lung cancer (19,20).
Peng et al (6) compared
preoperative TACE with intravenous chemotherapy in patients with
colorectal cancer. The results indicated that adverse events, such
as myelosuppression, gastrointestinal reactions, abnormal liver
function and neurotoxicity, were considerably lower in the
intra-arterial group compared with those in the intravenous group,
which also demonstrated a higher disease control rate.
Additionally, iodine-125 seeds have been reported to exert
promising therapeutic effects in treating malignancies such as
prostate cancer and lung cancer (21,22).
Sui et al (23) explored the
combination of iodine-125 seeds and PD-1 therapy for lung cancer,
and revealed that all three patients experienced complete or
partial remission. Furthermore, Chen et al (24) assessed the efficacy of combining
iodine-125 seeds with TACE for advanced lung cancer treatment,
reporting an objective response rate of 71.42% and a disease
control rate of 92.86% at the 6-month time point. Notably, no
serious complications were reported during follow-up. The duration
of local control ranged from 5 to 12 months, with a median
progression-free survival time of 8 months (95% confidence
interval: 7.3–8.8 months).
In a case study conducted by Katagiri et al
(25), a patient diagnosed with
pelvic osteosarcoma underwent TACE in conjunction with
radiotherapy. Following multiple rounds of intra-arterial
chemotherapy and radiation therapy, the patient faced two
recurrences at 8 and 14 years after surgery during a 21-year
follow-up period. Nevertheless, the patient ultimately achieved
complete remission after undergoing aggressive treatment. In the
current study, the treatment regimen notably decreased the
frequency of chemotherapy compared to the standard regimen. This
reduction may be attributed to embolization of the blood supply to
the tumor, which obstructs its blood flow, leading to swift tumor
necrosis and a decreased need for chemotherapy agents. This method
not only diminishes the risk of cardiovascular issues and secondary
malignancies, but also enhances the overall quality of life for
patients. Arterial embolization may alter the immune
microenvironment of the tumor, thereby enhancing the immune
response to the tumor. In an animal study (26), hepatic artery embolization was shown
to enhance intratumoral and peritumoral PD-L1 expression in a rat
model of hepatocellular carcinoma (HCC). In addition, Chao et
al (27) revealed that TACE is
associated with the modulation of serum angiogenic, inflammatory
and cell growth cytokines in patients with HCC. Additionally, the
present case report used iodine-125 seed implantation, which offers
improved local control of the tumor while maximizing the protection
of adjacent healthy tissues. Ferrari et al (14) previously explored the effects of
high-dose ifosfamide in the first-line treatment of patients ≤40
years of age with nonmetastatic osteosarcoma of the extremity. The
results showed that the program, while feasible, produces major
renal and hematologic toxicity.
In the present case report, a 13-year-old female
patient was diagnosed with high-grade osteosarcoma through a
pathological biopsy. A treatment plan that combined TACE with
iodine-125 seed implantation was subsequently implemented.
Postoperative follow-up results revealed notable pain relief, a
gradual recovery of limb function and complete tumor remission as
observed in imaging studies. Over a follow-up period of >6
years, the patient exhibited effective local tumor control, no
distant metastasis, no notable complications and an improvement in
quality of life. While the use of arterial chemoembolization has
been reported, its combination with iodine-125 seeds for
osteosarcoma is novel. The patient had a large tumor volume and
rich blood supply at the time of initial treatment, and there was a
high risk of bleeding with direct iodine-125 seed implantation.
Therefore, arterial embolization was performed followed by seed
implantation, and an operation sequence was chosen that not only
reduced the risk of bleeding, but also reduced the dosage of
iodine-125 seeds and radiation damage. These findings indicated
that the combination of iodine-125 seeds and TACE may demonstrate
considerable clinical efficacy in treating osteosarcoma, with fewer
adverse effects compared with traditional radiotherapy and
chemotherapy. This approach has potential as an essential adjunct
therapy for osteosarcoma, yielding improved treatment outcomes and
quality of life for patients.
In conclusion, the combination of TACE and
iodine-125 seed implantation represents an innovative treatment
modality that provides a potential supplementary option for
managing osteosarcoma, especially for patients with osteosarcoma
with abundant blood supply and no distant metastasis, and those
whose tumor is unable to be completely resected or refuse to
undergo surgery. The successful treatment of this case strongly
supports the clinical application of this method. Although the
results are promising, the present study has several limitations.
Since the previous biopsy was conducted at another hospital,
pre-treatment pathology images cannot be provided. To determine the
efficacy and safety of the present treatment plan, further
validation through larger clinical studies is necessary to assess
its applicability and long-term outcomes for patients with
osteosarcoma. Additionally, exploration of optimal dosing and
treatment regimens is essential to enhance therapeutic effects
while minimizing side effects.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
LR and FL contributed to study conceptualization and
manuscript writing. LJ and YL conducted the study design and
analyzed the data. LY analyzed the re-biopsy pathology slides. LR,
LY and YL confirm the authenticity of all the raw data. All authors
read and approved the final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The mother of the patient provided written informed
consent for the publication of this research.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
ALP
|
alkaline phosphatase
|
|
DSA
|
digital subtraction angiography
|
|
LDH
|
lactate dehydrogenase
|
|
MAP
|
methotrexate, doxorubicin and
cisplatin
|
|
NRS
|
Numeric Rating Scale
|
|
TACE
|
transarterial chemoembolization
|
References
|
1
|
Gatta G, Capocaccia R, Botta L, Mallone S,
De Angelis R, Ardanaz E, Comber H, Dimitrova N, Leinonen MK,
Siesling S, et al: Burden and centralised treatment in Europe of
rare tumours: Results of RARECAREnet-a population-based study.
Lancet Oncol. 18:1022–1039. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
De Pinieux G, Karanian M, Le Loarer F, Le
Guellec S, Chabaud S, Terrier P, Bouvier C, Batistella M, Neuville
A, Robin YM, et al: Nationwide incidence of sarcomas and connective
tissue tumors of intermediate malignancy over four years using an
expert pathology review network. PLoS One. 16:e02469582021.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Strauss SJ, Frezza AM, Abecassis N, Bajpai
J, Bauer S, Biagini R, Bielack S, Blay JY, Bolle S, Bonvalot S, et
al: Bone sarcomas: Esmoeuracan-genturis-ernpaedcan clinical
practice guideline for diagnosis, treatment and follow-up. Ann
Oncol. 32:1520–1536. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Storey L, Fern LA, Martins A, Wells M,
Bennister L, Gerrand C, Onasanya M, Whelan JS, Windsor R, Woodford
J and Taylor RM: A critical review of the impact of sarcoma on
psychosocial wellbeing. Sarcoma. 2019:97308672019. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Li F, Zhang DB, Ma Y, Song Y and Duan XL:
Effects of combined sintilimab and chemotherapy on progression-free
survival and overall survival in osteosarcoma patients with
metastasis. Pak J Med Sci. 40:648–651. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Peng SH, Mbarak HS, Li YH, Ma C, Shang QL,
Chen Z, Bian DJ and Xiao EH: Neoadjuvant intra-arterial versus
intravenous chemotherapy in colorectal cancer. Medicine.
100:e283122021. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kou F, Gao S, Liu S, Wang X, Chen H, Zhu
X, Guo J, Zhang X, Feng A and Liu B: Preliminary clinical efficacy
of iodine-125 seed implantation for the treatment of advanced
malignant lung tumors. J Cancer Res Ther. 15:1567–1573. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen Y, Jiang Y, Ji Z, Jiang P, Xu F,
Zhang Y, Zhang P, Guo F, Li X, Sun H, et al: Dosimetry, efficacy,
and safety of three-dimensional printing noncoplanar
template-assisted and CT-guided 125I seed implantation for
recurrent retroperitoneal lymphatic metastasis after external beam
radiotherapy. Brachytherapy. 19:380–388. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
He S, Renne A, Argandykov D, Convissar D
and Lee J: Comparison of an emoji-based visual analog scale with a
numeric rating scale for pain assessment. JAMA. 328:208–209. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cates JMM: Comparison of the AJCC, MSTS,
and Modified Spanier Systems for Clinical and Pathologic Staging of
Osteosarcoma. Am J Surg Pathol. 41:405–413. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Brierley JD and Wittekind C: TNM
Classification of Malignant Tumours. 8 edition. John Wiley &
Sons; Oxford: 2016
|
|
12
|
Jin Q, Xie X, Yao H, Wen L, Li H, Lv D,
Zeng Z, Wang Y, Zou C, Yin J, Huang G, Wang B, et al: Clinical
significance of the radiological relationship between the tumor and
the main blood vessels in Enneking IIB osteosarcoma of the
extremities. J Cancer. 11:3235–3245. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Eisenhauer EA, Therasse P, Bogaerts J,
Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S,
Mooney M, et al: New response evaluation criteria in solid tumours:
Revised RECIST guideline (version 1.1). Eur J Cancer. 45:228–247.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ferrari S, Smeland S, Mercuri M, Bertoni
F, Longhi A, Ruggieri P, AlvegardAlvegard TA, Picci P, Capanna R,
Bernini G, et al: Neoadjuvant chemotherapy with high-dose
Ifosfamide, high-dose methotrexate, cisplatin, and doxorubicin for
patients with localized osteosarcoma of the extremity: A joint
study by the Italian and Scandinavian Sarcoma Groups. J Clin Oncol.
23:8845–8852. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Smeland S, Bielack SS, Whelan J, Bernstein
M, Hogendoorn P, Krailo MD, Gorlick R, Janeway KA, Ingleby FC,
Anninga J, et al: Survival and prognosis with osteosarcoma:
Outcomes in more than 2000 patients in the EURAMOS-1 (European and
American Osteosarcoma Study) cohort. Eur J Cancer. 109:36–50. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kallis M, Maloney C, Edelman M, Soffer S,
Symons M and Steinberg B: Abstract PR13: Surgical excision of the
primary tumor in osteosarcoma model results in enhanced metastatic
growth by modulating the lung immune microenvironment. Cancer Res.
80 (Suppl 1):PR13. 2020. View Article : Google Scholar
|
|
17
|
Niculescu ȘA, Grecu AF, Gheonea C and
Grecu DC: Limb salvage surgery in pediatric patients with
osteosarcoma. Curr Health Sci J. 50:360–367. 2024.PubMed/NCBI
|
|
18
|
Gaspar N, Venkatramani R, Hecker-Nolting
S, Melcon SG, Locatelli F, Bautista F, Longhi A, Lervat C,
Entz-Werle N, Casanova M, et al: Lenvatinib with etoposide plus
ifosfamide in patients with refractory or relapsed osteosarcoma
(ITCC-050): A multicentre, open-label, multicohort, phase 1/2
study. Lancet Oncol. 22:1312–1321. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Liao L, Li X, Wei G, Lu Y, Wei S, Lin K
and Zhang F: Efficacy of transcatheter arterial chemoembolization
combined with radiotherapy for locally advanced hepatocellular
carcinoma. Am J Transl Res. 16:6935–6945. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhao YW, Liu S, Qin H, Sun JB, Su M, Yu
GJ, Zhou J, Gao F, Wang RY, Zhao T and Zhao GS: Efficacy and safety
of CalliSpheres drug-eluting beads for bronchial arterial
chemoembolization for refractory non-small-cell lung cancer and its
impact on quality of life: A multicenter prospective study. Front
Oncol. 13:11109172023. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Di X, Zhang H, Liu X, Zhao J, Gao Z, Yu H,
Su X, Liang Y and Wang J: A new technique for trans-perirectal
iodine-125 seed implantation in prostatic cancer guided by CT and
3D printed template: Two case reports. Front Oncol. 12:10319702022.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Tang M, Lin X, Zhu L, Liu J, Ye X, Miu R
and Hu J: The efficacy and safety of percutaneous CT-guided
iodine-125 brachytherapy combined with standard chemotherapy and
brachytherapy alone for lung malignant nodule: A retrospective
comparative cohort study. J Thorac Dis. 16:573–580. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sui A, Song H, Yu H, Zhang H, Hu Q, Lei Y,
Zhang L and Wang J: Clinical application of iodine-125 seed
brachytherapy combined with anti-PD-1 antibodies in the treatment
of lung cancer. Clin Ther. 42:1612–1616. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Chen C, Wang W, Yu Z, Tian S, Li Y and
Wang Y: Combination of computed tomography-guided iodine-125
brachytherapy and bronchial arterial chemoembolization for locally
advanced stage III non-small cell lung cancer after failure of
concurrent chemoradiotherapy. Lung Cancer. 146:290–296. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Katagiri H, Sugiyama H, Takahashi M,
Murata H, Wasa J, Hosaka S and Miyagi M: Osteosarcoma of the pelvis
treated successfully with repetitive intra-arterial chemotherapy
and radiation therapy: A report of a case with a 21-year follow-up.
J Orthop Sci. 20:568–573. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Takaki H, Hirata Y, Ueshima E, Kodama H,
Matsumoto S, Wada R, Suzuki H, Nakasho K and Yamakado K: Hepatic
artery embolization enhances expression of programmed cell death 1
ligand 1 in an orthotopic rat hepatocellular carcinoma model: in
vivo and in vitro experimentation. J Vasc Interv Radiol.
31:1475–1482.e2. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chao Y, Wu CY, Kuo CY, Wang JP, Luo JC,
Kao CH, Lee RC, Lee WP and Li CP: Cytokines are associated with
postembolization fever and survival in hepatocellular carcinoma
patients receiving transcatheter arterial chemoembolization.
Hepatol Int. 7:883–892. 2013. View Article : Google Scholar : PubMed/NCBI
|