Introduction
Angiosarcoma (AS) is a rare soft tissue sarcoma,
accounting for 2–5% of all soft tissue sarcomas (1). Since the tumor originates from
vascular endothelial cells, it can occur at any anatomical site,
although it frequently occurs in the skin of the head and neck in
elderly men.
The etiology of primary AS is unknown, but secondary
AS is associated with radiation exposure, and chronic lymphoedema
(Stewart-Treves syndrome), exogenous toxins, and familial syndromes
such as neurofibromatosis are hypothesized to be risk factors as
well (1,2).
Primary uterine AS is an extremely rare type of
tumor, and only 30 cases have been reported in the English
literature to date (3). The 5-year
survival rate is <35%, which is equivalent to that of other
sites of AS (2,4). In addition, the median overall
survival time for patients with metastatic AS is <11 months
(5). Standard systemic chemotherapy
for patients with unresectable disease has not yet been
established.
Here, the patient presented with intra-abdominal
recurrence very early on after complete surgical removal for
uterine AS, but achieved remission with paclitaxel and carboplatin
combination therapy. Further research, including more case reports,
is required to improve our understanding of this rare histological
type. In the present report, the case of a 57-year-old woman is
documented in detail and a literature review on AS is provided.
Case report
The patient was a 57-year-old woman, gravida 1, para
1, with no complications. She had a history of an open abdominal
myomectomy at age 31. There were no significant findings in her
family history.
She presented to the outpatient department of
Ishikiriseiki Hospital (Higashiosaka, Osaka, Japan) in August 2022
with complaints of abdominal distention, loss of appetite, and
dyspnea. Transvaginal ultrasound (Xario 100G; Canon Inc.) revealed
a large uterine tumor. No abnormal vaginal bleeding was observed on
internal examination. A blood test showed hemoglobin (Hb) 4.5 g/dl
(normal range: 12.0–15.2 g/dl), serum lactate dehydrogenase (LDH)
409 IU/l (normal range: 106–211 IU/l), and D-dimer 9.4 µg/ml
(normal range: <1.0 µg/ml), and carbohydrate antigen (CA) 125
66.6 U/ml (normal value: <35.0 U/ml). CA125 was measured using
CA125 II Abbott Alinity G06330R04 (Abbott Molecular Inc.). Magnetic
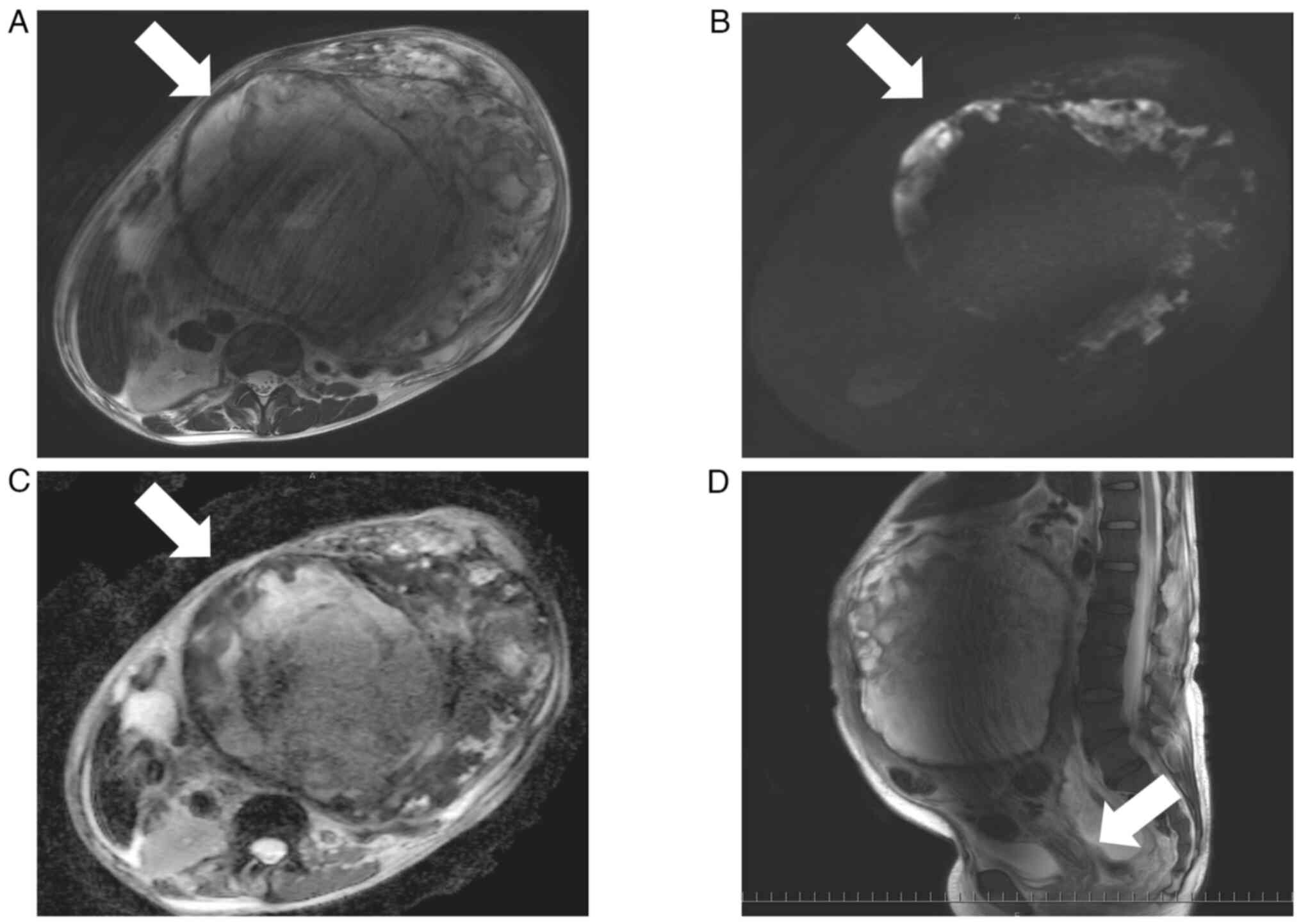
resonance imaging (MRI) (Ingenia 3T; Philips) showed a
heterogeneous 27×20 cm mass in the uterus with high and low signal
areas in the T2-weighted imaging. The solid part of the tumor
showed a high signal in the diffusion-weighted imaging and a low
signal in the apparent diffusion coefficient map (b value=0
sec/mm2), suggesting the presence of a malignant tumor
(Fig. 1A-C). There were no abnormal
findings in the cervix, suggesting that there was no cervical
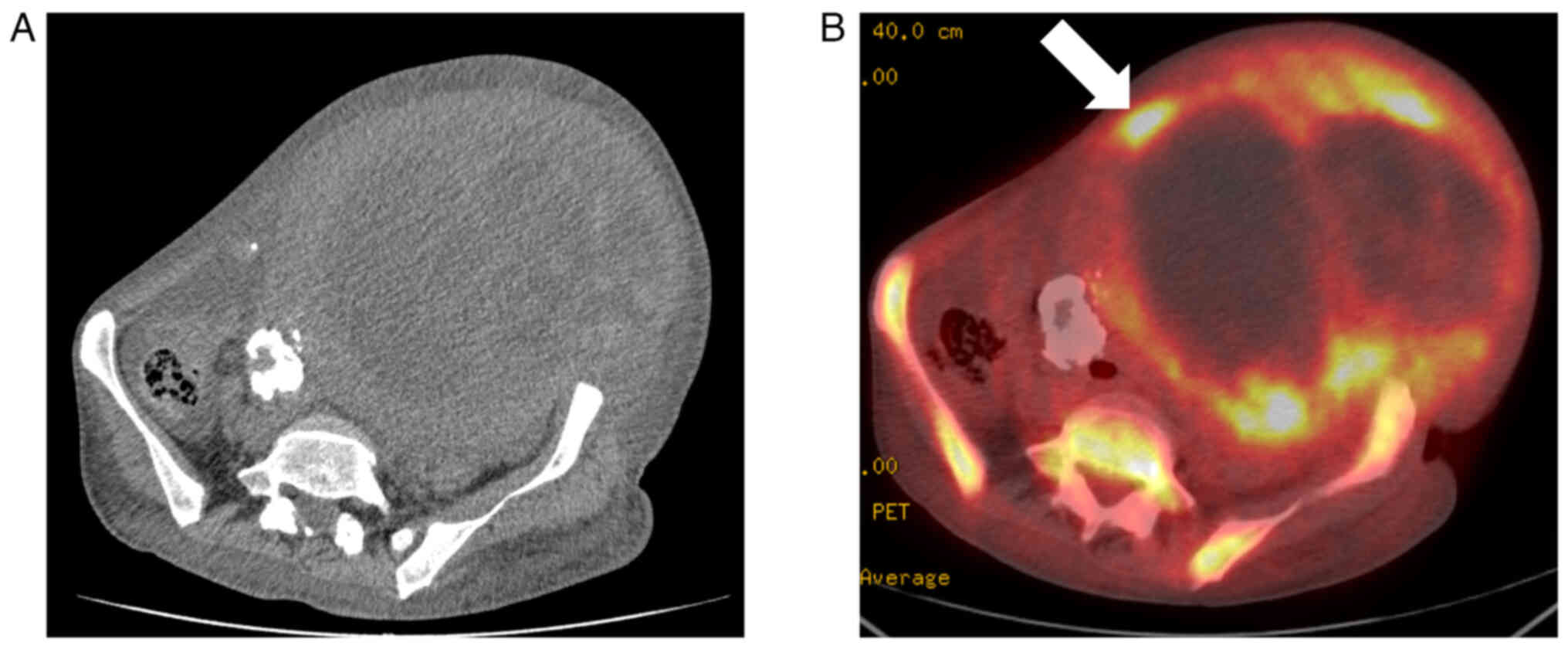
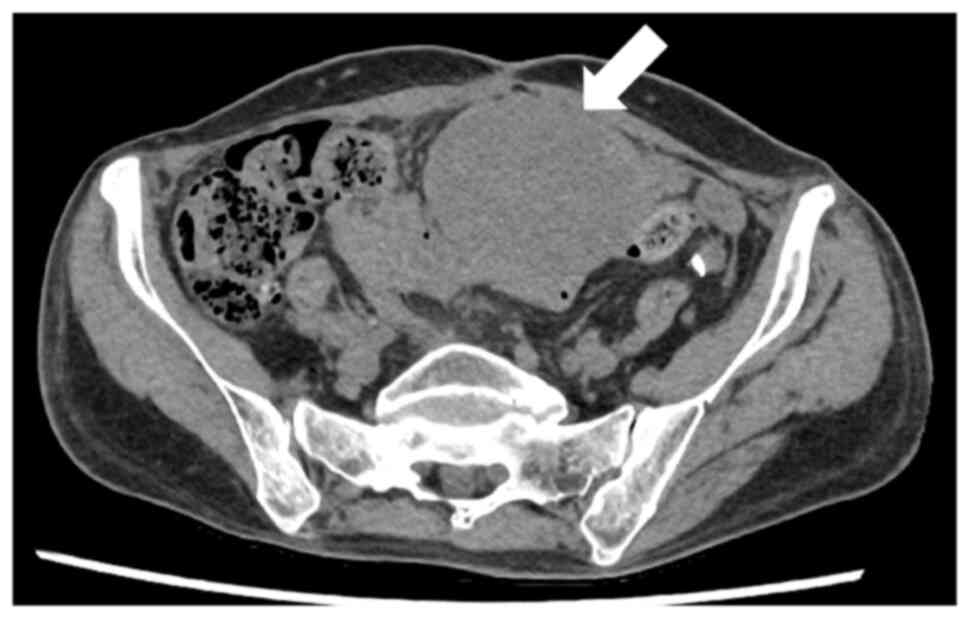
invasion or malignant tumor originating from the cervix (Fig. 1D). Computed tomography (CT)
(Aquilion PRIME; Canon Inc.) (Fig.
2A) showed a heterogeneous, septate, mixed density mass with
calcified areas on the left medial side in transverse section.
Using 18-fluorodeoxyglucose-positron emission tomography CT [(18F)
FDG-PET/CT; Discovery ST; GE Yokogawa Medical Systems Inc.] showed
no lymph node swelling and no evidence of metastatic lesions.
Hypermetabolism was observed at the margins of the uterine tumor,
where MRI images suggested the presence of a malignant tumor
(Fig. 2B). An ultrasound
examination of the lower limbs did not reveal deep vein thrombosis.
Cytological examinations of the cervix and endometrium were all
negative.
Despite a total of 20 units of red blood cell (RBC)
transfusion (140 ml/unit), the Hb levels remained low, and the
patient developed heart and respiratory failure, requiring
intensive care, including ventilator management. The patient
underwent surgery with strict anesthetic management to improve
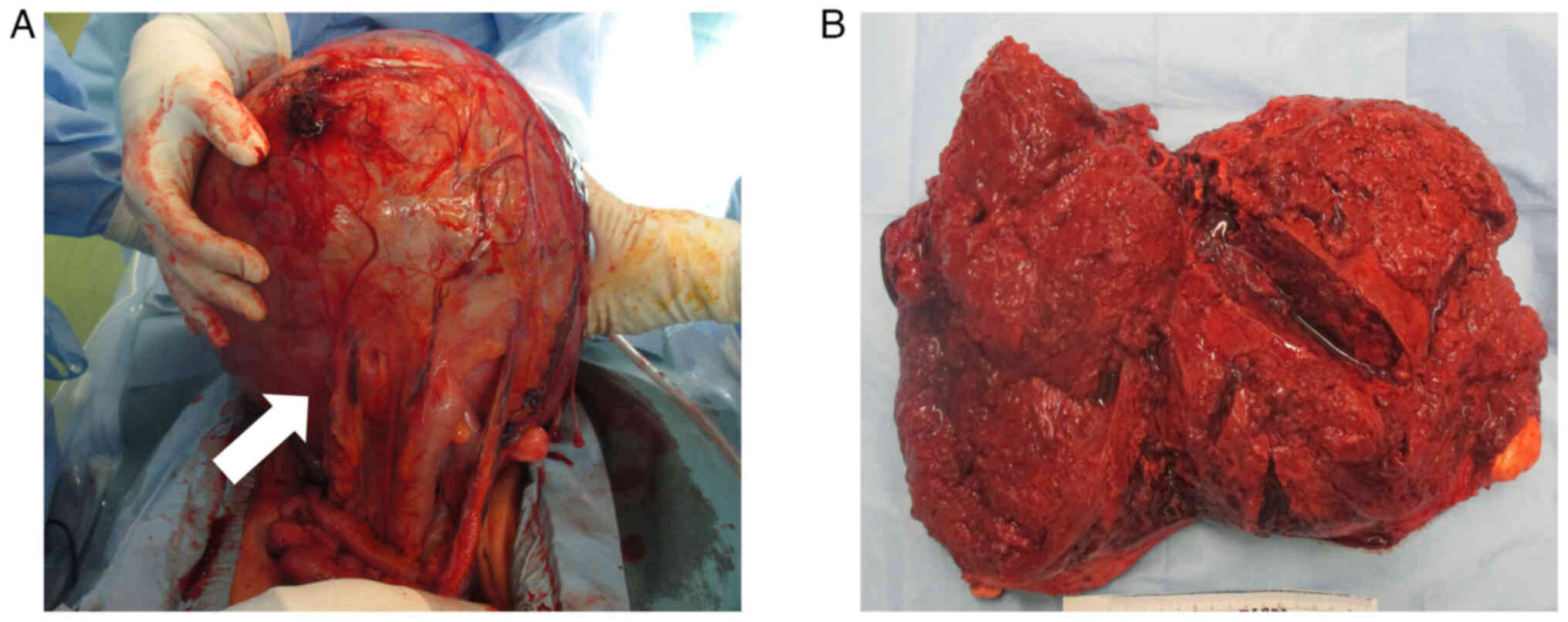
their condition. Intraoperative findings showed massive hemorrhagic
ascites and a smooth, enlarged uterus with numerous dilated blood
vessels (Fig. 3A). There were no
disseminated lesions in the abdominal cavity, and there were firm
adhesions between the uterus and the sigmoid colon. Intraoperative
frozen section analysis suggested leiomyosarcoma. Finally, total
abdominal hysterectomy, bilateral salpingo-oophorectomy, partial
sigmoid colectomy: Functional end-to-end anastomosis were
performed. The total blood loss and weight of the excised specimen
were 3,140 ml and 7,100 g, respectively. A total of 8 units of RBC
transfusion was required during the operation. The macroscopic
appearance of the resected uterine tumor was a spongy hemorrhagic
tumor with necrotic tissue (Fig.
3B). Cytological examination of the hemorrhagic ascites was
negative.
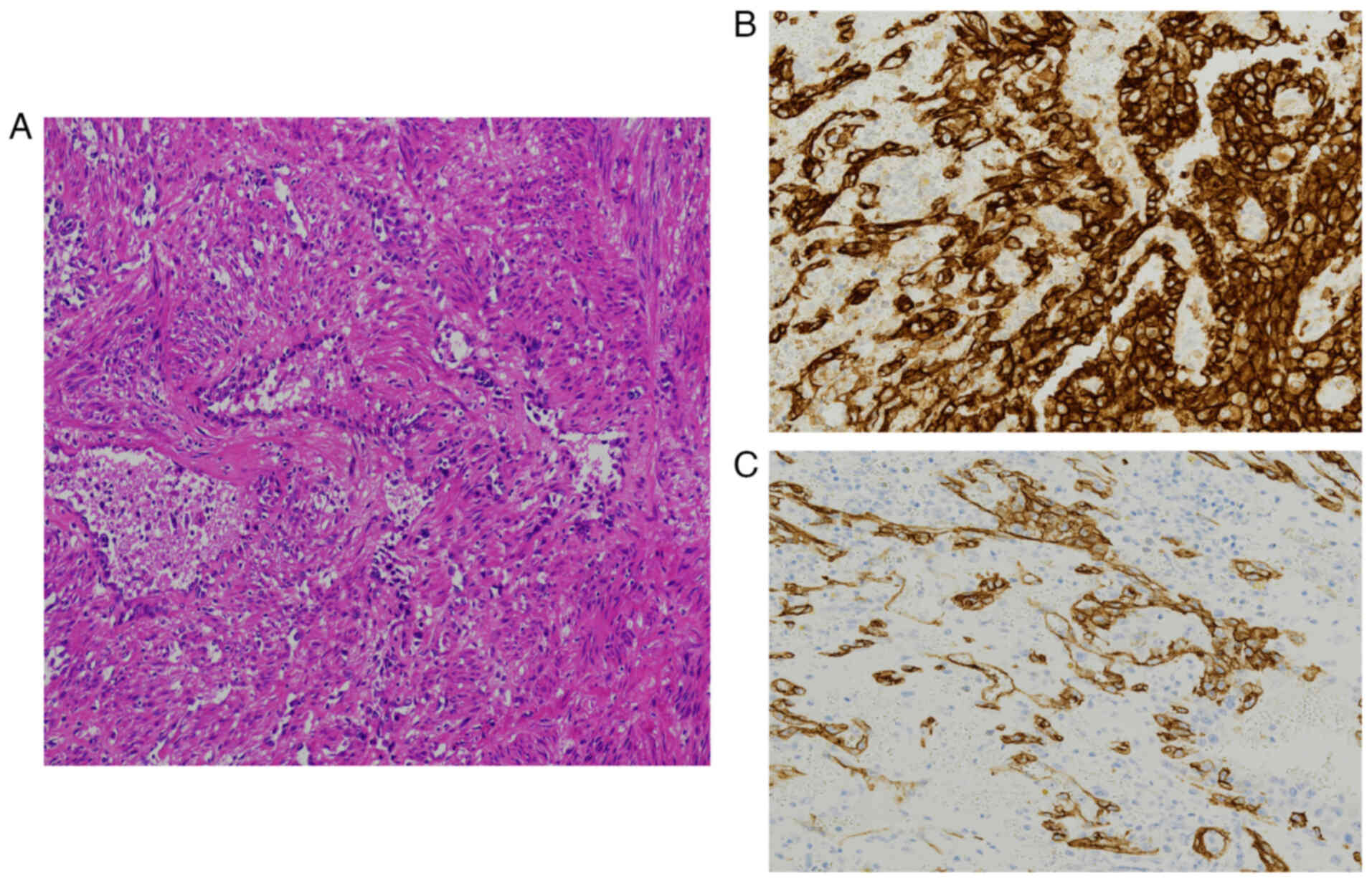
Pathological examination revealed that the atypical
cells with enlarged nuclei and distinct nucleoli formed a reticular
structure like a vascular cavity and proliferated (Fig. 4A). Immunohistochemical staining of
paraffin-embedded tissue showed strong positivity for CD31
(Fig. 4B) and partial positivity
for CD34 (Fig. 4C). Based on the
above, the patient was diagnosed with primary epithelioid
angiosarcoma. Hematoxylin and eosin staining was performed using
Carrazi's hematoxylin (Muto Pure Chemicals Co., Ltd) and Pure Eosin
Solution (Muto Pure Chemicals Co., Ltd) on an automated staining
device (Tissue-Tek® Prisma™ Plus; Sakura Finetek Japan
Co., Ltd). For immunohistochemical staining, CD31 antibody (cat.
no. IR61061-2; Ready-to-Use) and CD34 antibody (cat. no. IR63261-2;
Ready-to-Use) were used as primary antibodies, and EnVision
FLEX/HRP (cat. no. K800021-2J; Ready-to-Use) was used as the
secondary antibody (all from Agilent Technologies Japan, Ltd), all
tests were performed in the department of pathology according to
the standard protocol, following the manufacturer's instructions.
The tumor was confined to the uterus, and it was diagnosed as
primary uterine angiosarcoma (T1NXM0; 8th edition of the American
Joint Committee on Cancer).
Adjuvant chemotherapy was not performed at the
patient's request. Even though a complete surgical resection was
achieved, a CT scan performed 1 month after surgery revealed the
presence of three new solid tumors (maximum diameter of 7 cm) in
the abdominal cavity (Fig. 5). The
patient was diagnosed with intra-abdominal recurrence of uterine AS
and received 21 cycles of intravenous paclitaxel (175
mg/m2) and carboplatin (area under the curve=6
mg/ml/min) once every 3–4 weeks. Tumor response was evaluated every
3 cycles. Tumors gradually decreased in size, therefore, the
patient requested long-term chemotherapy. In addition, CA125 and
LDH levels normalized after 3 cycles of chemotherapy and have
remained normal. D-dimer levels gradually decreased from the start
of chemotherapy and normalized 10 months after the last cycle,
where they remained normal. No serious adverse events were observed
during chemotherapy, but according to the Common Terminology
Criteria for Adverse Events version 5.0, grade 1 neutropenia and
peripheral neuropathy were observed. At the time of writing this
report, she was still alive with no disease 31 months after the
primary surgery.
Discussion
AS is a very rare disease, with the skin being the
most common primary site of origin. A small number of cases have
also been reported in gynecological organs such as the uterus,
ovaries, vagina, and vulva (1,2,4). AS is
classified into primary and secondary forms. In this case, no risk
factors for secondary AS were identified. Therefore, it was
diagnosed as primary uterine AS (1,2). To
the best of our knowledge, as summarized previously (3), only 30 cases have been reported to
date.
The majority of patients with uterine AS are
postmenopausal, with a median age of 61 years (age range: 17–81
years). The most common symptom is postmenopausal vaginal bleeding,
and patients may present with weight loss and anemia (3). Our patient was postmenopausal but,
notably, did not present with vaginal bleeding; instead, she
exhibited an enlarged uterus and ascites. A distinctive clinical
feature in this case was the patient's poor response to massive
blood transfusions, coupled with the observation of extensive
hemorrhagic ascites intraoperatively. The anemia improved rapidly
following hysterectomy. We hypothesize that the persistent anemia,
despite no visible vaginal bleeding, likely resulted from internal
hemorrhage due to the tumor's friable and abnormally proliferative
vasculature. This internal bleeding may have contributed to both
intratumoral hemorrhage and the accumulation of hemorrhagic
ascites, which were confirmed during surgery.
Radiologically, the most distinctive characteristic
of uterine AS is the heterogeneous tumor with a mixture of
different signal intensities, described ‘cauliflower-like’ on
T2-weighted imaging (6). Although
the MRI in our case was affected by motion artifacts due to the
patient's inability to remain still, the characteristic findings
were evident, supporting the diagnosis. Radiomics analysis, which
has been increasingly utilized to enhance diagnostic accuracy in
uterine malignancies (7), has not
yet been specifically applied to uterine angiosarcoma due to its
rarity. Future development of radiomics-based approaches could
potentially contribute to the non-invasive assessment of such rare
tumors.
Macroscopically, consistent with previous case
reports, the tumor presented as a spongy, hemorrhagic mass with
necrotic tissue (6,8). Histopathologically, anastomotic
vascular lumens lined by highly atypical endothelial cells were
observed, accompanied by extensive hemorrhage and necrosis-features
characteristic of AS. Tumor cells in AS exhibit varying degrees of
nuclear atypia and may present with epithelial or spindle cell
morphology, sometimes making differentiation from benign vascular
proliferations challenging. Conversely, highly atypical cells may
form solid sheets with minimal vascular formation, necessitating
differentiation from carcinosarcoma, leiomyosarcoma, adenosarcoma,
metastatic carcinoma, and malignant melanoma. Immunohistochemical
staining is therefore crucial for definitive diagnosis of AS. These
tumors typically express endothelial cell markers such as CD31,
CD34, and von Willebrand factor (2). In our case, positive staining for CD31
and CD34 enabled an accurate diagnosis at an early stage.
To date, evidence-based treatment regimens for AS
remain limited, with most published reports consisting of
retrospective case series. Uterine AS typically progresses rapidly
and carries poor prognosis, with a 5-year survival rate of <35%
(4). Furthermore, the median
overall survival for patients with metastatic AS is <11 months
(5). Despite these discouraging
statistics, our patient achieved complete remission following
recurrence of uterine AS through systemic chemotherapy. The patient
is still alive with no evidence of disease 31 months after the
initial treatment.
Radical surgery remains the first-line treatment for
resectable AS. For most cases of uterine AS over the past 50 years,
surgical treatment (simple hysterectomy and bilateral
salpingo-oophorectomy) has been the primary treatment approach
(3). Generally, lymphadenectomy is
not recommended for visceral AS unless there is clear involvement
of regional lymph nodes (9).
Neoadjuvant/adjuvant chemotherapy for localized resectable AS is
not a standard treatment. Despite the limited number of cases,
adjuvant chemotherapy for stage III or IV ovarian AS has been
reported to potentially improve overall survival (4). A European retrospective study of
primary AS involving 33 sarcoma centers demonstrated that adjuvant
chemotherapy may improve outcomes in patients with large tumors
(>5 cm) and/or high predicted 10-year mortality risk (>60%),
although the optimal regimen remains undetermined (10). In our case, surgery was performed as
the primary treatment, achieving complete resection with negative
margins (R0). Intraoperative frozen section analysis suggested
leiomyosarcoma, a subtype for which lymph node assessment is
generally not indicated. Therefore, nodal sampling was not
performed. The diagnosis of primary AS confined to the uterus
(T1NXM0) was clinically appropriate, though it should be noted that
standardized prognostic staging of visceral AS has not yet been
established. Previous reports have indicated that tumors >5 cm
portend a poor prognosis in uterine AS (3). While adjuvant therapy was recommended,
our patient declined this treatment option. Despite an initially
favorable postoperative course, early imaging was performed due to
the high risk of recurrence and metastasis. This revealed three
distinct solid tumors in the abdominal cavity. We postulate that
microscopic hematogenous metastases were likely present at the time
of surgery despite complete macroscopic resection, leading to early
recurrence. This reflects the aggressive biological behavior of
uterine AS.
Chemotherapy is generally considered the first-line
treatment for metastatic and locally advanced AS (2). In our case, given the presence of
atypical tumors in the vascular cavity of the primary uterine AS
and the development multiple abdominal tumors hypothesized to be
hematogenous metastases, chemotherapy was selected rather than
radiotherapy. Anthracycline (5,11,12),
paclitaxel (13,14), or gemcitabine (15) based regimens are currently
considered first-line treatments, although there is no consensus
regarding the optimal chemotherapy regimen for these patients. At
the time of treatment decision, evidence-based chemotherapy options
were limited; however, paclitaxel-based chemotherapy had shown
efficacy in a small number of AS cases. Notably, the ANGIOTAX study
investigating cutaneous angiosarcoma demonstrated complete
responses with paclitaxel-containing chemotherapy (14). Three previous cases of uterine AS
treated with paclitaxel and carboplatin have been reported in the
literature (3,6,16). In
all these cases, surgery was performed as the primary treatment,
with paclitaxel and carboplatin combination therapy administered as
adjuvant chemotherapy. Overall survival in these cases ranged from
2–14 months: one patient died from lung metastasis, while the other
two patients remained alive with no evidence of disease. Based on
these observations, paclitaxel and carboplatin combination therapy
appears potentially effective for uterine AS when chemotherapy is
indicated. However, this conclusion is limited by the absence of
robust retrospective or prospective studies and the small number of
documented cases.
In our patient, elevated levels of CA125, LDH, and
D-dimer were observed after surgery and at the time of recurrence.
These values gradually decreased during chemotherapy and eventually
normalized. While previous reports have suggested associations
between CA125, LDH, and AS, the literature lacks data regarding
their changes following treatment. Konishi et al (6) and Strickland et al (17) reported elevated pre-treatment CA125
levels in cases of uterine AS. Wang et al (18) identified pretreatment LDH levels as
an independent prognostic factor for AS through multivariate
analysis. These markers, being readily measurable in general
clinical practice, may potentially serve as valuable biomarkers for
monitoring treatment response and disease status in uterine AS.
In general, the response to chemotherapy for
metastatic and locally advanced AS is not sustained. As in this
case, the options after remission with taxane-based chemotherapy
are limited. Immune checkpoint inhibitors (ICI) have revolutionized
treatment in multiple cancer types, but development has been slow
due to the heterogeneity of sarcoma types. Recent trials have
evaluated various ICI strategies in AS, including ICI monotherapy,
combinations with tyrosine kinase inhibitors (TKI), and
chemotherapy combinations, with results varying by subtype. The
combination of ipilimumab and nivolumab (SWOG S1609, objective
response rate, 25%) suggests potential value, but this was limited
to cutaneous AS (19). Combination
therapies such as cabozantinib and nivolumab (Alliance A091902,
objective response rate, 59%) have shown similar responses in
cutaneous and non-cutaneous angiosarcoma, suggesting that TKIs may
improve responses in tumors that have been resistant to ICIs to
date (20). These findings may
serve as a reference treatment strategy for future relapses in our
patient.
In conclusion, we report a rare case of recurrent
uterine AS that achieved complete remission with long-term systemic
chemotherapy using paclitaxel and carboplatin. Early detection of
recurrence through vigilant follow-up was critical, given the
aggressive nature of angiosarcoma. While this case showed a
favorable response to chemotherapy, the findings should be
interpreted cautiously and may not be generalizable, considering
the limitations inherent to a single case report. Despite the lack
of standardized treatment protocols for recurrent or advanced
uterine AS, our report suggests that paclitaxel and carboplatin
combination therapy may represent a viable therapeutic option.
Further accumulation of cases and studies is warranted to enhance
our understanding and optimize management for this rare and
aggressive malignancy.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
YI, YH and KT conceived and designed the study. YI,
YH, AY, MK, KY and KT acquired, analyzed and interpreted the data.
YI, YH and KT drafted and revised the manuscript. YK reviewed the
pathological specimens. All authors have read and approved the
final manuscript. YH and KT confirm the authenticity of all the raw
data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the case details and associated
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wagner MJ, Ravi V, Schaub SK, Kim EY,
Sharib J, Mogal H, Park M, Tsai M, Duarte-Bateman D, Tufaro A, et
al: Incidence and presenting characteristics of angiosarcoma in the
US, 2001–2020. JAMA Netw Open. 7:e2462352024. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Young RJ, Brown NJ, Reed MW, Hughes D and
Woll PJ: Angiosarcoma. Lancet Oncol. 11:983–991. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Deb PQ, Weiss RE and Heller DS:
Angiosarcoma of the uterus: A systematic review. Int J Gynecol
Pathol. 41:496–502. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kruse AJ, Sep S, Slangen BF, Vandevijver
NM, Van Gorp T, Kruitwagen RF and de Vijver KK: Angiosarcomas of
primary gynecologic origin: A clinicopathologic review and
quantitative analysis of survival. Int J Gynecol Cancer. 24:4–12.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Penel N, Italiano A, Ray-Coquard I,
Chaigneau L, Delcambre C, Robin YM, Bui B, Bertucci F, Isambert N,
Cupissol D, et al: Metastatic angiosarcomas: Doxorubicin-based
regimens, weekly paclitaxel and metastasectomy significantly
improve the outcome. Ann Oncol. 23:517–523. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Konishi Y, Sato H, Fujimoto T, Tanaka H,
Takahashi O and Tanaka T: A case of primary uterine angiosarcoma:
Magnetic resonance imaging and computed tomography findings. Int J
Gynecol Cancer. 17:280–284. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Di Donato V, Kontopantelis E, Cuccu I,
Sgamba L, Golia D'Augè T, Pernazza A, Rocca CD, Manganaro L,
Catalano C, Perniola G, et al: Magnetic resonance imaging-radiomics
in endometrial cancer: A systematic review and meta-analysis. Int J
Gynecol Cancer. 33:1070–1076. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Schammel DP and Tavassoli FA: Uterine
angiosarcomas: A morphologic and immunohistochemical study of four
cases. Am J Surg Pathol. 22:246–250. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gronchi A, Miah AB, Dei Tos AP, Abecassis
N, Bajpai J, Bauer S, Biagini R, Bielack S, Blay JY, Bolle S, et
al: Soft tissue and visceral sarcomas: ESMO-EURACAN-GENTURIS
clinical practice guidelines for diagnosis, treatment and
follow-up. Ann Oncol. 32:1348–1365. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Conforti F, Gronchi A, Penel N, Jones RL,
Broto JM, Sala I, Bagnardi V, Napolitano A, Pala L, Pennacchioli E,
et al: Chemotherapy in patients with localized angiosarcoma of any
site: A retrospective European study. Eur J Cancer. 171:183–192.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Italiano A, Cioffi A, Penel N, Levra MG,
Delcambre C, Kalbacher E, Chevreau C, Bertucci F, Isambert N, Blay
JY, et al: Comparison of doxorubicin and weekly paclitaxel efficacy
in metastatic angiosarcomas. Cancer. 118:3330–3336. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Young RJ, Natukunda A, Litière S, Woll PJ,
Wardelmann E and van der Graaf WT: First-line anthracycline-based
chemotherapy for angiosarcoma and other soft tissue sarcoma
subtypes: Pooled analysis of eleven EORTC soft tissue and bone
sarcoma group trials. Eur J Cancer. 50:3178–3186. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Schlemmer M, Reichardt P, Verweij J,
Hartmann JT, Judson I, Thyss A, Hogendoorn PC, Marreaud S, Van
Glabbeke M and Blay JY: Paclitaxel in patients with advanced
angiosarcomas of soft tissue: A retrospective study of the EORTC
soft tissue and bone sarcoma group. Eur J Cancer. 44:2433–2436.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Penel N, Bui BN, Bay JO, Cupissol D,
Ray-Coquard I, Piperno-Neumann S, Kerbrat P, Fournier C, Taieb S,
Jimenez M, et al: Phase II trial of weekly paclitaxel for
unresectable angiosarcoma: The ANGIOTAX study. J Clin Oncol.
26:5269–5274. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Stacchiotti S, Palassini E, Sanfilippo R,
Vincenzi B, Arena MG, Bochicchio AM, De Rosa P, Nuzzo A, Turano S,
Morosi C, et al: Gemcitabine in advanced angiosarcoma: A
retrospective case series analysis from the Italian rare cancer
network. Ann Oncol. 23:501–508. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Roma AA, Allende D, Fadare O, Forscher C
and Rutgers JK: On uterine angiosarcomas: 2 additional cases. Int J
Gynecol Pathol. 36:369–371. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Strickland SV, Kilgore MR, Simons EJ and
Rendi MH: Epithelioid angiosarcoma arising in a uterine leiomyoma
with associated elevated CA-125: A case report. Gynecol Oncol Rep.
21:1–4. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wang M, Wu S, Tong A, Cui X and Ma X: The
prognostic value of pretreatment inflammatory biomarkers in primary
angiosarcoma. Cancer Manag Res. 11:7981–7989. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wagner MJ, Othus M, Patel SP, Ryan C,
Sangal A, Powers B, Budd GT, Victor AI, Hsueh CT, Chugh R, et al:
Multicenter phase II trial (SWOG S1609, cohort 51) of ipilimumab
and nivolumab in metastatic or unresectable angiosarcoma: A
substudy of dual anti-CTLA-4 and anti-PD-1 blockade in rare tumors
(DART). J Immunother Cancer. 9:e0029902021. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Grilley-Olson JE, Allred JB, Schuetze S,
Davis EJ, Wagner MJ, Poklepovic AS, Waechter B and Schwartz GK: A
multicenter phase II study of cabozantinib plus nivolumab for
patients with advanced angiosarcoma previously treated with a
taxane (Alliance A091902). J Clin Oncol. 41:115032023. View Article : Google Scholar
|