Introduction
Lung cancer markedly impacts global health due to
its high incidence and mortality with ~2.4 million new cases and
1.8 million deaths reported annually worldwide (1). Among various subtypes of lung cancer,
small cell lung cancer (SCLC) is the most aggressive, characterized
by rapid progression and early metastasis. Notably, 67% of patients
with SCLC present with metastases at initial diagnosis, which
commonly affects the brain, liver, adrenal glands, bone and
contralateral lung (2).
Ocular metastases from lung cancer are rare, with
the choroid being the predominant intraocular site. Metastasis to
the eye predominantly involves the choroid (90%) and, less
frequently, the iris (8%) and ciliary body (2%), as well as other
intraocular structures (3).
Choroidal metastases typically manifest with visual disturbances,
including decreased visual acuity, blurred vision, photopsia,
floaters, metamorphopsia and diplopia, although asymptomatic
presentation may occur in certain cases (4).
This predilection for metastasis to the choroid is
attributed to its vascular anatomy, which is supplied by multiple
posterior ciliary arteries. The combination of sluggish blood flow,
high vascular density and absent lymphatic drainage facilitates
tumor cell deposition (5). Besides
hemodynamic factors, organ-specific metastasis involves
interactions between tumor cells and the host's microenvironment.
Therefore, to enhance understanding of this rare presentation and
optimize clinical pathways, this case report aims to describe the
diagnostic and therapeutic challenges encountered in a patient with
SCLC whose initial manifestation was blurred vision secondary to
choroidal metastasis and retinal detachment.
Case report
A 62-year-old man presented to the ophthalmology
clinic of The Second Hospital of Jilin University (Jilin, China) in
December 2017 with painless visual impairment in the right eye.
During the ophthalmological examination, the following findings
were observed: A transparent cornea, a round pupil measuring 3 mm
in diameter, a positive pupillary light reflex and a cloudy
lens.
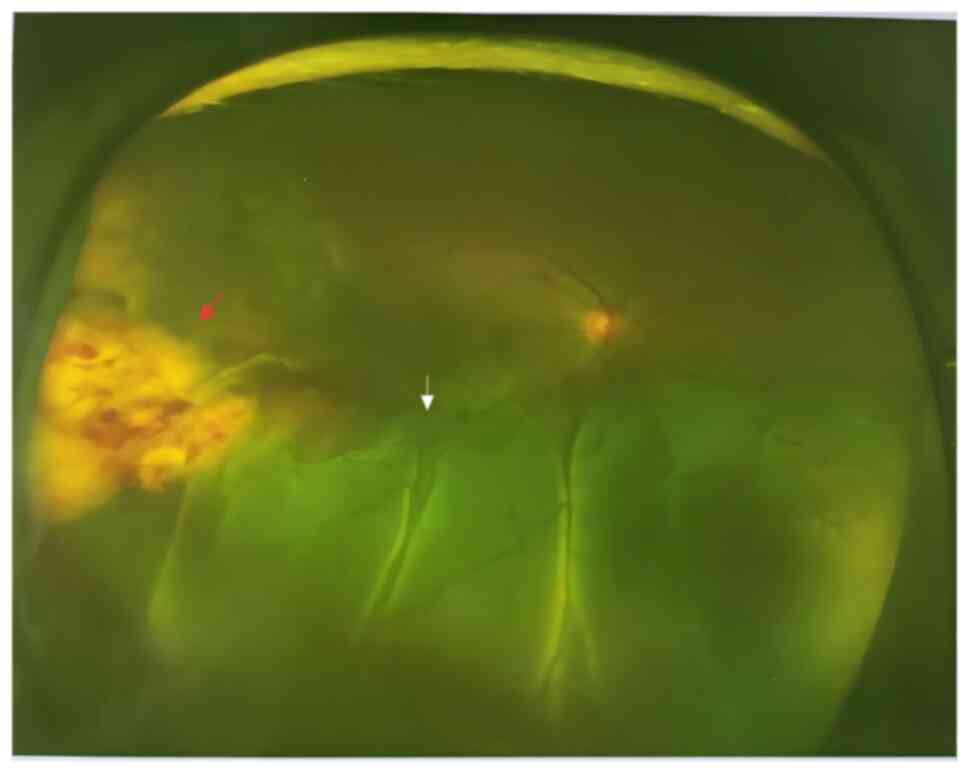
Digital ocular fundus imaging revealed a subretinal
lesion temporal to the optic disc and notable retinal detachment in
the lower region (Fig. 1).
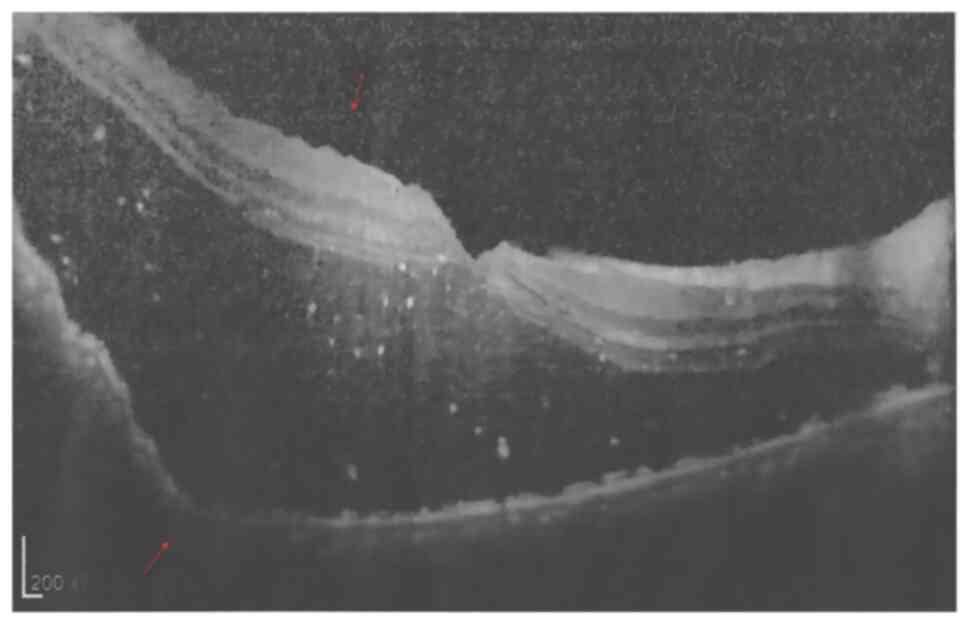
Ultrasound imaging demonstrated ciliary body leakage into the right
eye, with a low-to-medium solid mass echo on the fundus bulb wall.
This mass echo had an uneven internal echo and a clear boundary,
with a membranous bulge noted on its surface. Color Doppler flow
imaging exhibited abundant blood flow within the membranous mass,
indicating intraocular tumor or metastasis (Fig. 2). Optical coherence tomography
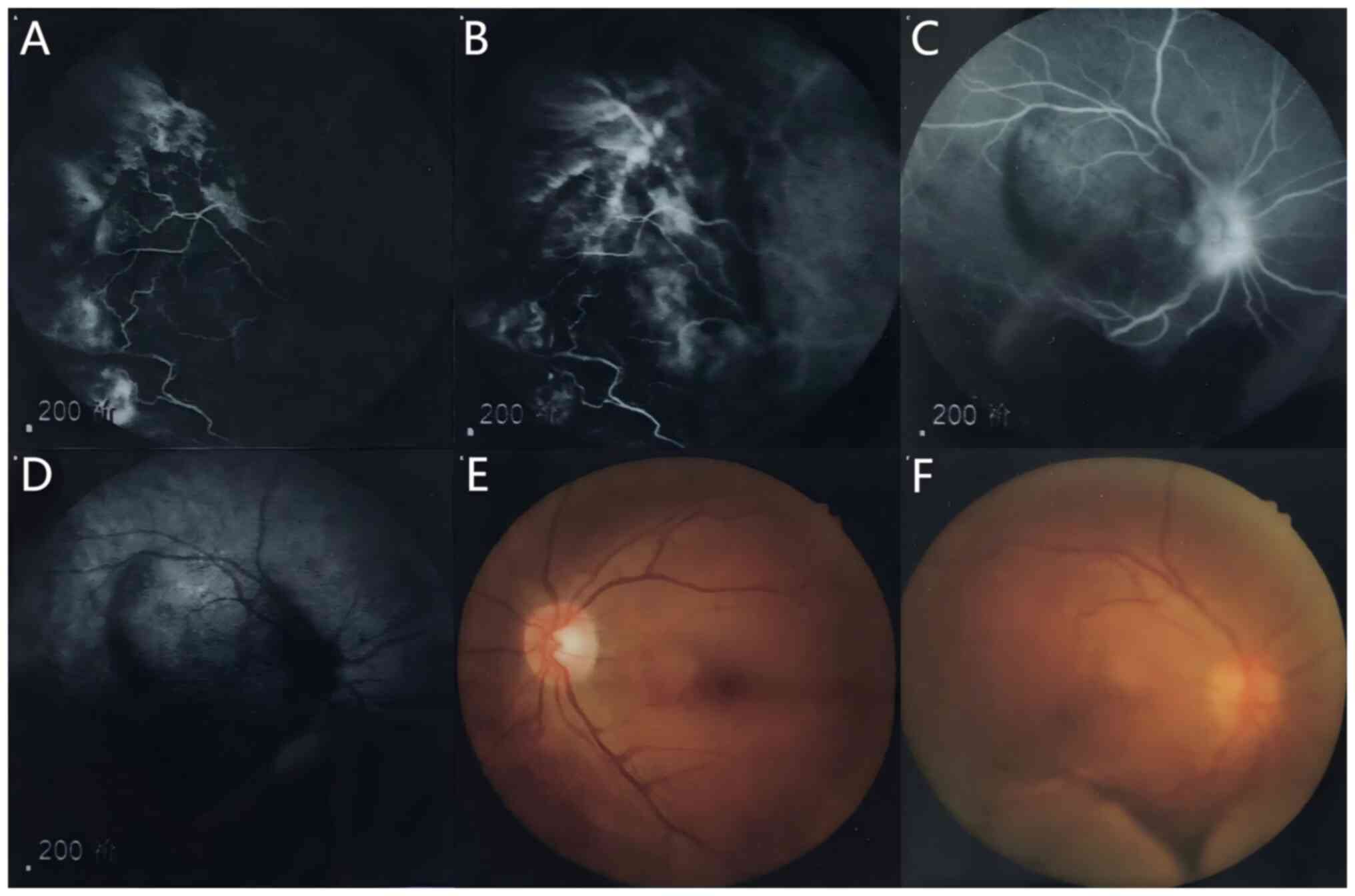
revealed a prominent macular protrusion (Fig. 3). Angiography demonstrated a
prominent and compact mass in the right eye with an elevated
momentum underneath and fluorescein and indocyanine green
angiography indicated blood vessel leakage and scattered areas of
intense fluorescence (Fig. 4). The
definitive diagnosis of choroidal metastases remains challenging
compared to choroidal melanoma or hemangioma due to overlapping
clinical features, similar imaging characteristics and the low
incidence of this condition (6–8).
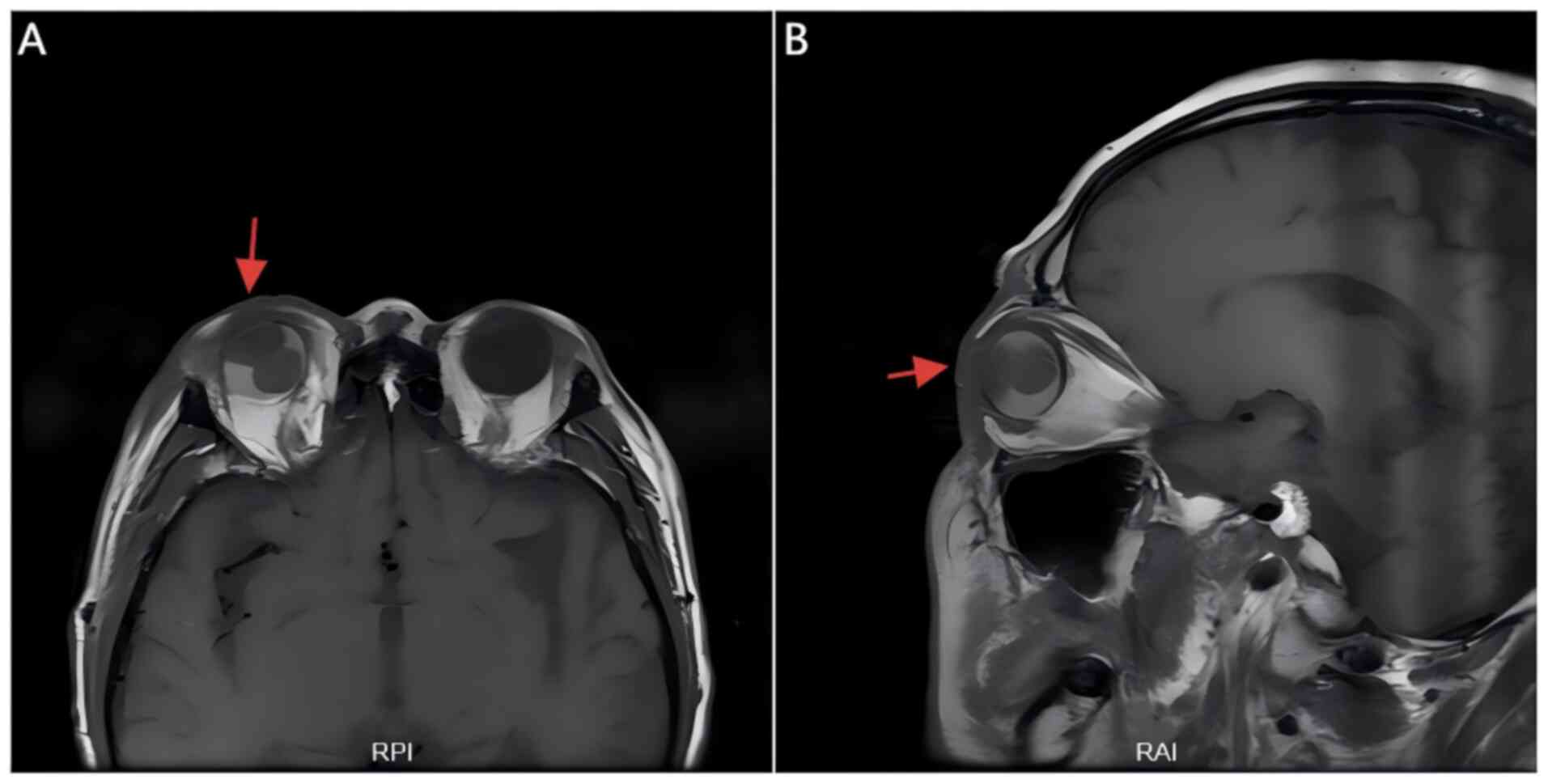
Therefore, dynamic MRI scans were performed with both plain and
contrast-enhanced imaging of both eyes, which demonstrated a tumor
in the right eyeball characterized by choroidal metastasis with
concurrent retinal detachment (Fig.
5).
Following an initial diagnosis of choroidal
metastasis, a systematic search for the primary tumor was
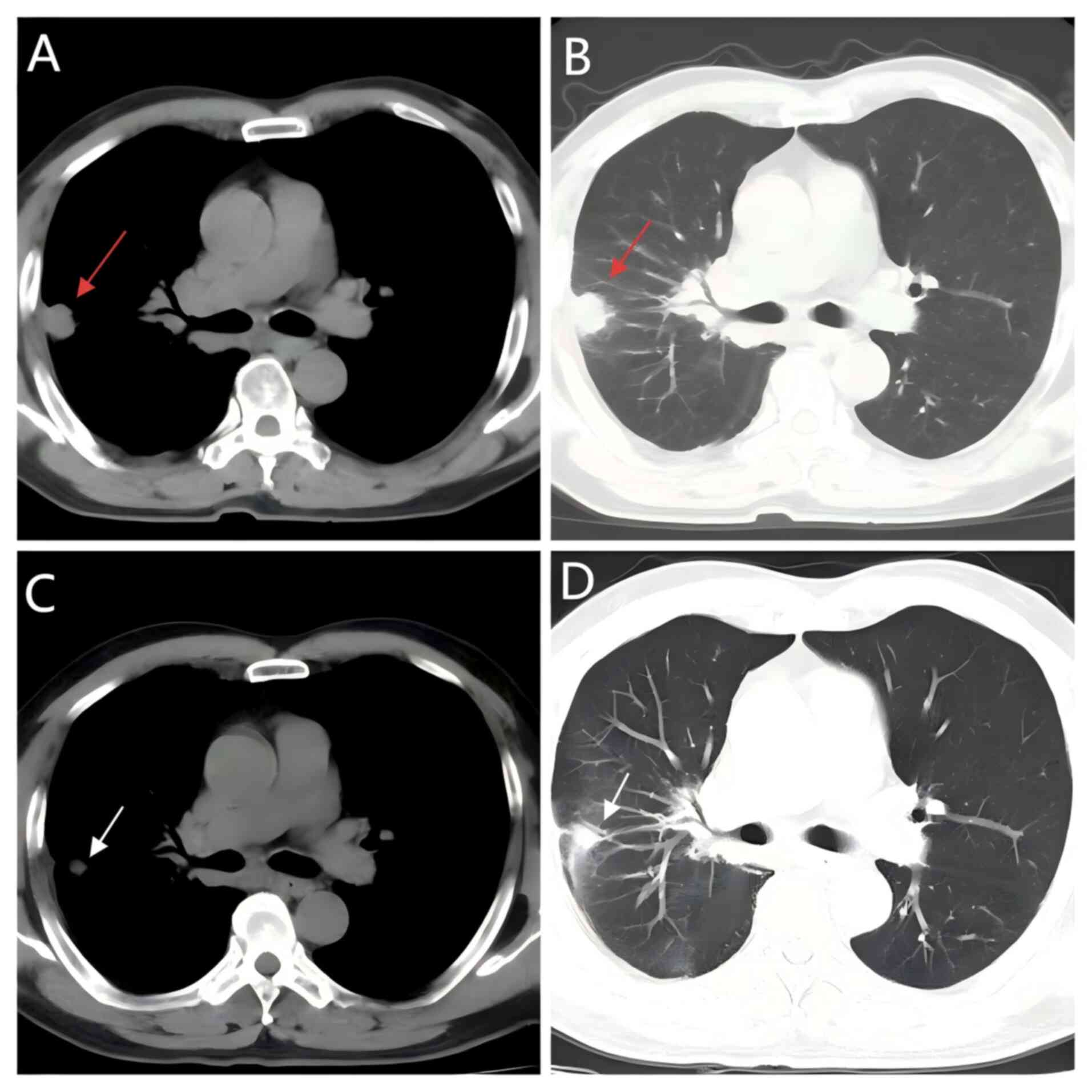
conducted. Chest CT imaging revealed a heterogeneously enhancing
mass (46×35 mm) in the right lower lung lobe, accompanied by
suspected malignant pleural effusion and probable metastatic
involvement of right hilar/mediastinal lymph nodes (Fig. 6). Histopathological examination of
transbronchial biopsy specimens that had been formalin-fixed and
paraffin-embedded (FFPE) (following standardized dewaxing,
rehydration, routine hematoxylin and eosin staining, dehydration
and mounting of paraffin sections) was performed using a light
microscope (BX51; Olympus Corp.), and revealed sheets of atypical
cells with hyperchromatic nuclei and scant cytoplasm,
characteristic of poorly differentiated carcinoma. Cellular
morphology indicated nuclear molding and crush artifacts, which
strongly suggested small cell carcinoma (Fig. 7). Immunohistochemical staining was
performed on FFPE tissue samples. Tissue sections (3 µm thick)
mounted on adhesive glass slides were dewaxed in xylene (3×10 min)
and rehydrated through graded ethanols (100%, 2×5 min; 95, 85 and
75%, each for 2 min). Permeabilization was not specifically
applied. Endogenous peroxidase activity was blocked using
peroxidase blocking reagent (ready-to-use; Fuzhou Maixin
Biotechnology Development Co., Ltd.) for 30 min at room
temperature, followed by non-specific blocking with blocking
reagent (ready-to-use; Dako; Agilent Technologies, Inc.) for 30 min
at room temperature. The following primary antibodies were applied:
Anti-Cytokeratin AE1/AE3 [CK(AE1/AE3); monoclonal antibody; cat.
no. A500-019A; Thermo Fisher Scientific, Inc.]; anti-chromogranin A
(CgA; polyclonal antibody; cat. no. ab15160; Abcam);
anti-synaptophysin (Syn) (monoclonal antibody; cat. no. ab32127;
Abcam); anti-cluster of differentiation 56 (CD56/NCAM; monoclonal
antibody; cat. no. 313602; BioLegend); anti-Ki-67 (monoclonal
antibody; cat. no. M7240; Dako; Agilent Technologies); anti-thyroid
transcription factor-1 (TTF-1) (monoclonal antibody; cat. no.
MS-063-P; Cell Marque); anti-leukocyte common antigen (CD45)
(monoclonal antibody; cat. no. 555482; BD Biosciences); anti-napsin
A (monoclonal antibody; cat. no. CM007A; Biocare Medical); anti-p40
(ΔNp63; monoclonal antibody; cat. no. CM163A; Biocare Medical); and
anti-CK5/6 (monoclonal antibody; cat. no. M7237; Dako; Agilent
Technologies). Secondary detection used biotin-labeled goat
anti-mouse/rabbit IgG polymer (UltraSensitive SP kit; ready-to-use;
Fuzhou Maixin Biotechnology Development Co., Ltd.) for 30 min at
room temperature, followed by streptavidin-HRP (UltraSensitive SP
kit; ready-to-use; Fuzhou Maixin Biotechnology Development Co.,
Ltd.) for 30 min at room temperature. Stained slides were examined
using a light microscope (BX51; Olympus Corp.) at ×100
magnification. The staining revealed the following: CK(AE1/AE3)
(+), CgA (+), Syn (+), CD56) (+), Ki-67 (90%), TTF-1 (+), CD45 (−),
Napsin A (−), p40 (−) and CK5/6 (−). These findings confirmed the
diagnosis of SCLC. Subsequent CT and whole-body bone scan
corroborated the final diagnoses of serous retinal detachment,
malignant pleural effusion, choroidal metastases and SCLC of the
right lung.
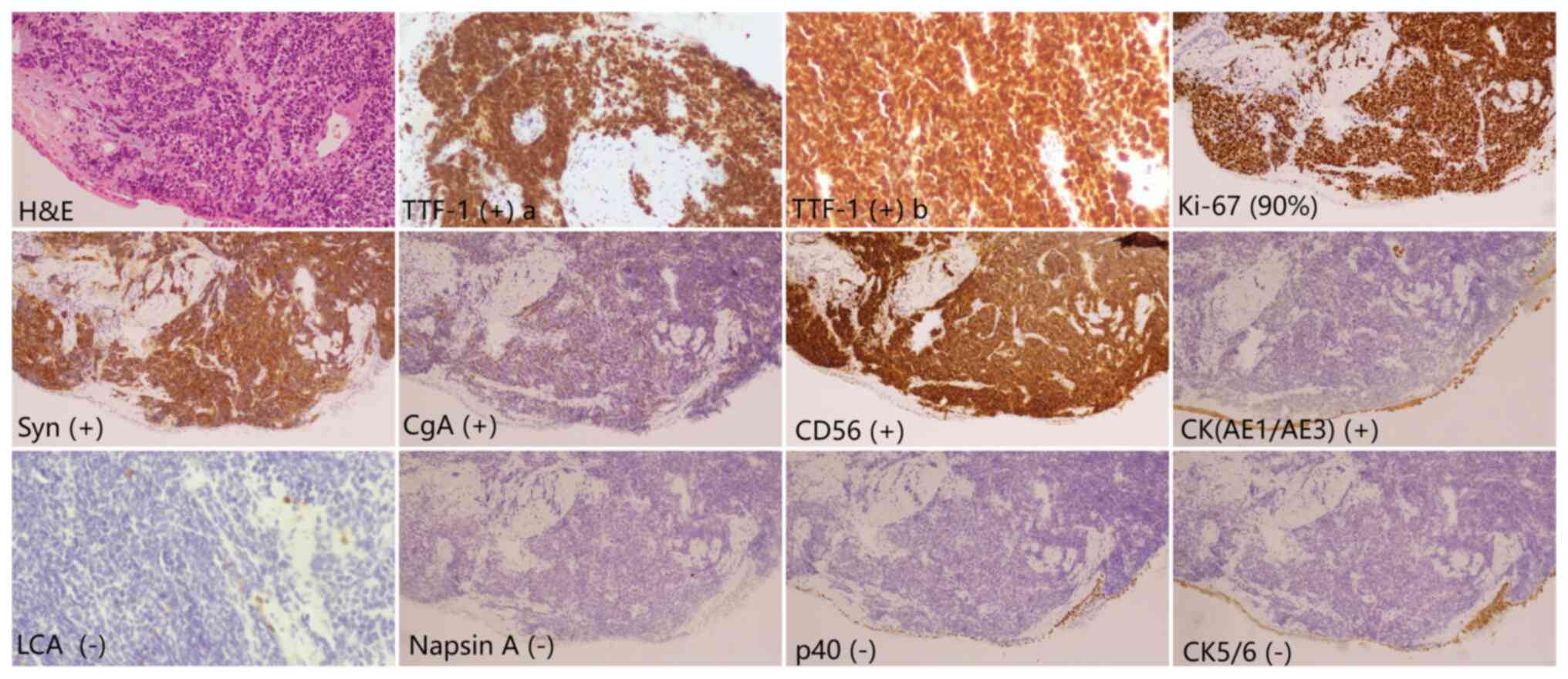
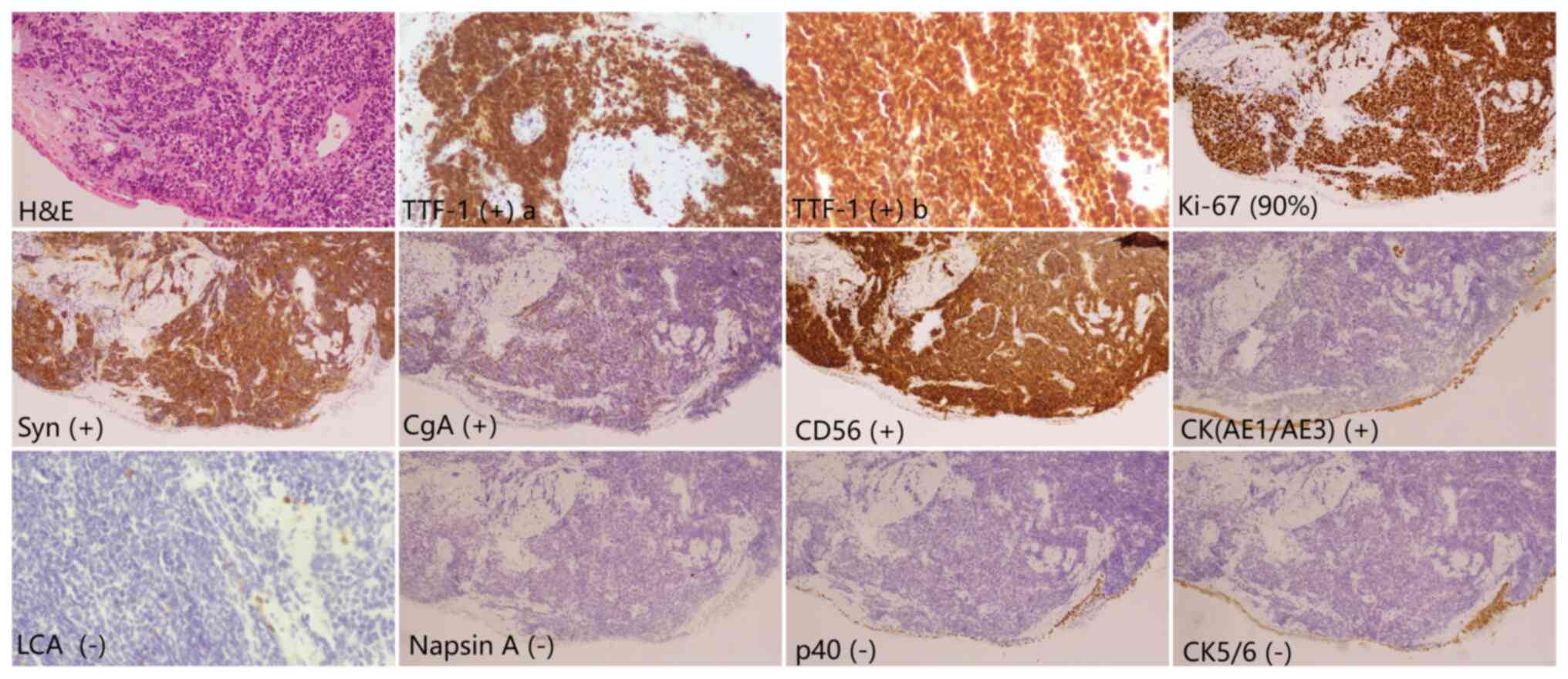 | Figure 7.Histopathological and
immunohistochemical analysis of the pulmonary lesion obtained via
transbronchial biopsy. Cellular morphology shows nuclear molding
and crush artifacts, consistent with small cell carcinoma.
Immunohistochemistry reveals positivity for CK(AE1/AE3), CgA, Syn,
CD56, Ki-67 (90%) and TTF-1, and negativity for LCA/CD45, Napsin A,
p40 and CK5/6 (magnification, ×100). CK, cytokeratin; CgA,
chromogranin A; Syn, synaptophysin; CD, cluster of differentiation;
TTF-1, thyroid transcription factor-1; LCA, leukocyte common
antigen. |
The patient was administered the etoposide and
nedaplatin regimen (EP regimen) (etoposide 100 mg/m2 +
nedaplatin 80 mg/m2, once every 3 weeks). The
chemotherapy dosage and treatment intervals were adjusted based on
the tumor burden and physical condition of the patient. After four
cycles of EP chemotherapy, follow-up lung CT in May 2018
demonstrated a notable therapeutic response: The primary tumor
(pre-treatment size, 46×35 mm) in the right lower lobe showed
regression to a 15×15 mm nodular shadow, with concomitant reduction
in mediastinal lymphadenopathy (Fig.
6). This radiographic improvement was consistent with partial
remission according to the Response Evaluation Criteria In Solid
Tumors (9). Notably, serous retinal
detachment and choroidal metastases remained stable on concurrent
ophthalmologic evaluation.
The patient underwent six cycles of chemotherapy
with the EP regimen, achieving a partial response, which
demonstrated the efficacy of the treatment. However, after 5 cycles
of chemotherapy, the ocular symptoms of the patient were
exacerbated. Shortly thereafter, the patient experienced complete
vision loss in the right eye, along with redness, swelling and
increased blood flow in the surrounding area. The retina exhibited
a large blue-gray swelling with no light reflection. The patient
then underwent localized radiation therapy to relieve ocular
discomfort.
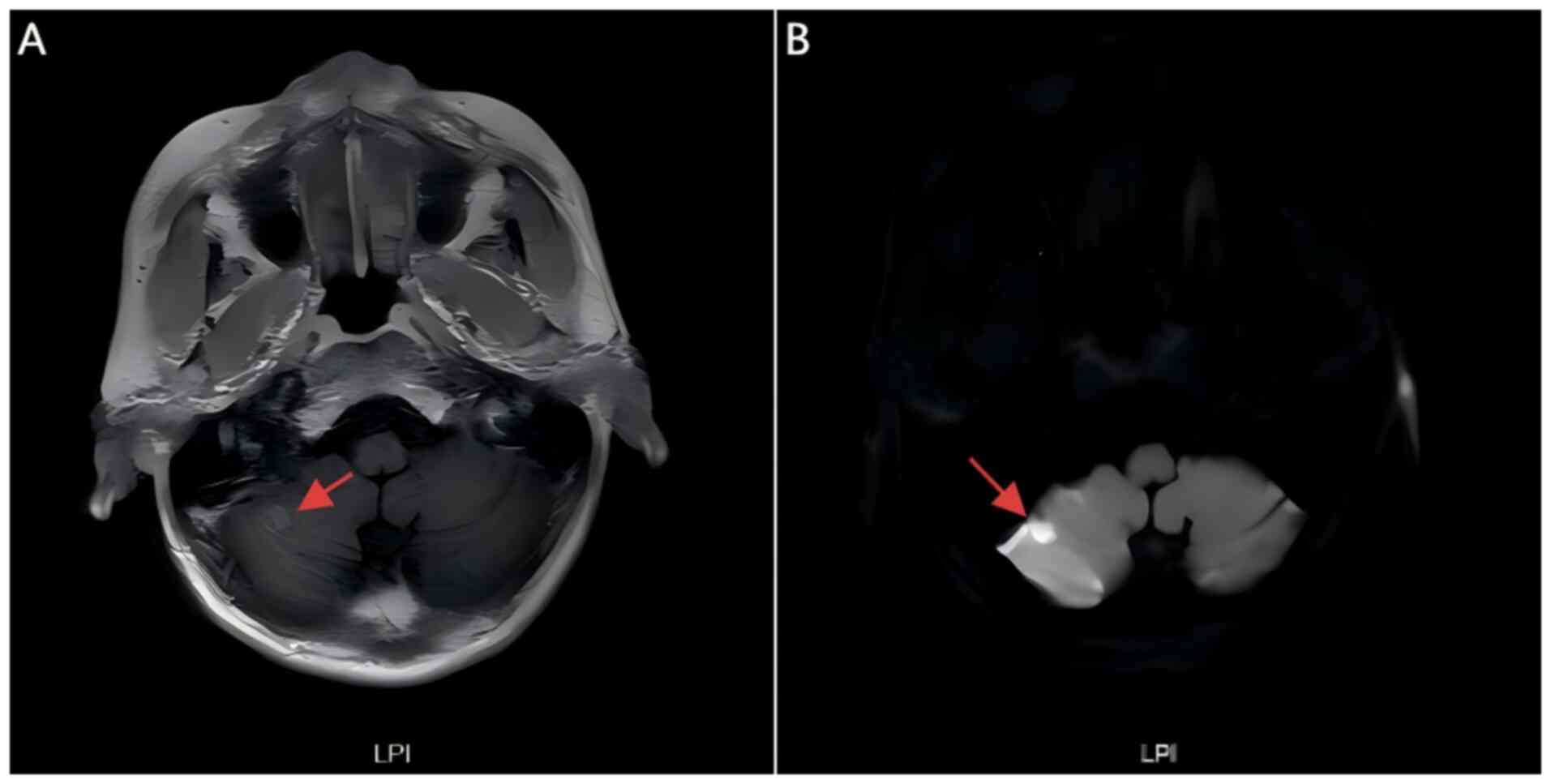
In September 2018, within 3 months following the
completion of chemotherapy, the patient presented again to the
Second Hospital of Jilin University (Jilin, China) with a headache
on the right side. The patient exhibited electrolyte abnormalities
and elevated tumor markers (neuron-specific enolase elevation,
CA125 elevation, hyponatremia, hypokalemia). A chest CT revealed an
enlarged area of dense opacities in the right lung and an MRI of
the head indicated an abnormal signal in the right cerebellar
hemisphere (Fig. 8), which
suggested metastasis and local recurrence of the extensive stage
SCLC in the patient.
Given that patients with this condition typically
receive an EP regimen with a response duration of <3 months,
primary resistance to the initial regimen was suspected (10). In SCLC treatment, lobaplatin, as a
third-generation platinum agent, exhibits lower cross-resistance
compared with first- and second-generation platinum drugs (11). The patient currently has an Eastern
Cooperative Oncology Group (ECOG) performance status (12) of 0 and a numerical rating scale pain
score (13) of 3. In addition to
controlling disease progression to extend survival, contemporary
treatment strategies prioritize pain management and enhancement of
quality of life. Therefore, the lobaplatin-liposomal paclitaxel
combination was chosen for palliative treatment (liposomal
paclitaxel 135 mg/m2 + lobaplatin 50 mg, once every 3
weeks). After completing the lobaplatin-liposomal paclitaxel
combination treatment regimen, the patient discontinued further
therapy and succumbed to his illness in December 2018.
Discussion
Choroidal metastases are the most common site of
intraocular metastases, which accounted for 80–90% of cases in
previous studies (14–16). Of these, breast cancer is the most
common cause, accounting for 37–47% of all reported cases.
Furthermore, lung cancer is another important cause, being the
origin of 21–44% of all reported cases of choroidal metastases
(16–18). Due to its increased aggressiveness
and potential for hematogenous dispersion, lung carcinoma has a
higher propensity for ocular metastasis compared with other solid
tumors (19–21).
Adenocarcinoma is the most common histological type
of lung cancer in patients with choroidal metastasis of lung
cancer, followed by squamous cell carcinoma and SCLC (22,23).
Among the subtypes of lung carcinoma, SCLC has a markedly higher
incidence of choroidal metastasis compared with non-SCLC (NSCLC),
likely due to its higher malignant potential and early hematogenous
dissemination (24–26). SCLC choroidal metastasis is often
bilateral and multifocal, characterized by rapid growth and
sensitivity to chemotherapy; however, it has a higher likelihood of
drug resistance and shorter survival (median, 3–6 months) (20,26).
Unilateral involvement is uncommon in ocular metastases from lung
cancer, accounting for only 12% of cases (20,25,27).
Although precise incidence data for SCLC choroidal metastasis are
limited, its clinical significance as a rare initial symptom is
substantial and warrants high vigilance.
The mechanism underlying vision loss due to
choroidal metastasis is multifaceted and involves various factors,
such as direct compression of tumors, retinal detachment, vascular
changes and inflammatory responses (28).
Choroidal metastases are frequently underdiagnosed
due to their asymptomatic presentation or nonspecific ocular
symptoms (e.g., visual field defects, photopsia), which lead to
potential underestimation of their true incidence (29,30).
After an actual diagnosis of lung cancer, some cases have been
identified using systematic screening techniques (such as
fundoscopy, ultrasonography or optical coherence tomography). In
patients with SCLC, notable systemic metastases or concurrent brain
metastases often overwhelm ocular evaluations, which delays
diagnosis (31,32). However, when patients with
undiagnosed cancer present with visual impairment, the integration
of imaging techniques (e.g., MRI/CT) with histopathological
confirmation via fine-needle aspiration biopsy achieves diagnostic
accuracy exceeding 90% (33).
Several recent reviews and systematic studies recommend baseline
ophthalmic evaluations for patients with SCLC to enhance early
detection rates and optimize prognostic outcomes (34,35).
Choroidal metastasis from SCLC is characterized by
acute visual impairment, with a markedly faster symptom progression
compared with other metastatic intraocular tumors, such as breast
or renal carcinoma. The typical signs of choroidal metastasis
include flat, yellowish-white lesions in the posterior pole of the
fundus, which often grow infiltratively and are frequently
associated with serous retinal detachment, important clinical clues
for identification (36). Compared
with other primary tumors, such as breast cancer, SCLC-related
choroidal metastases are more likely to present as multifocal and
have a notably higher rate of bilateral involvement compared with
NSCLC, which indicates a more aggressive biological behavior
(37).
Given these clinical manifestations, multimodal
imaging techniques are key to a definitive diagnosis. It is
essential to integrate radiological, metabolic and molecular
biological evidence to clarify the nature of the lesion and trace
the primary site. Ultrasound biomicroscopy can precisely measure
lesion thickness and has a significantly higher detection rate for
micro-metastases compared with conventional B-mode ultrasound
(38). Optical coherence tomography
angiography technology can be used to analyze the microvascular
patterns of choroidal metastases and identify specific
microvascular structural features of choroidal metastases, which
provides important evidence for their diagnosis (39). In high-risk patients, whole-body
positron emission tomography (PET)-CT and single-photon emission CT
bone scans can be useful diagnostic tools for the identification of
metastases.
The systemic treatment of SCLC with choroidal
metastasis should consider primary tumor control and metastasis
suppression. According to the 2025 National Comprehensive Cancer
Network guidelines (40), the
combination of etoposide and platinum (EP regimen) as first-line
therapy achieved an objective response rate of 68–75%, with a
median progression-free survival of 5.2 months, and it remains the
standard regimen for extensive-stage SCLC.
Recent years have witnessed breakthroughs in
systemic therapeutic strategies for SCLC. Novel evidence from
multiple phase III clinical trials and meta-analyses (41–45)
has established programmed cell death protein 1/programmed cell
death-ligand 1 inhibitors combined with platinum-etoposide regimens
as the first-line standard of care for extensive-stage SCLC in both
National Comprehensive Cancer Network and Chinese Society of
Clinical Oncology guidelines, with their survival benefits,
particularly the notable improvement in median overall survival
(OS), which achieved broad clinical validation.
Emerging evidence further highlights the therapeutic
importance of integrating multi-targeted antiangiogenic agents with
immunochemotherapy for SCLC (46–48). A
recent randomized phase 3 trial demonstrated that this
combinatorial approach achieved a median OS of 19.3 months compared
with 11.9 months in the control group, which corresponded to a 38%
reduction in mortality risk (hazard ratio=0.61; P=0.0002) (49).
Radiotherapy constitutes a cornerstone of SCLC
management, which serves as a key component in both primary tumor
control and metastatic disease targeting. Conventional external
beam radiotherapy is currently the standard radiation technique for
the treatment of choroidal metastases, which provides tumor control
(response or stability) in ~90% of all cases (50). Stereotactic radiosurgery has been
demonstrated to effectively reduce tumor volume and attenuate signs
of fibrosis during follow-up (51).
Intravitreal injection of bevacizumab can alleviate macular edema
and improve visual acuity (52).
The clinical efficacy of ophthalmic treatments appears promising,
particularly for patients with a short life expectancy. Minimally
invasive procedures can enhance quality of life and minimize ocular
toxicity.
The advent of precision medicine is ushering in
novel dimensions for individualized SCLC management through the
strategic convergence of molecular subtyping-guided multi-target
interventions and immune microenvironment modulation. Future
translational research must prioritize the optimization of
therapeutic efficacy via multidisciplinary collaboration
underpinned by multi-omics biomarker profiling, which thereby
addresses the long-standing challenges posed by SCLC.
Of note, the present study had certain limitations.
PET-CT was not performed during initial staging or
post-chemotherapy evaluation due to financial constraints of the
patient. Although conventional imaging modalities (including chest
CT, head CT, abdominal CT, whole-body bone scintigraphy and brain
MRI) provided sufficient evidence for the diagnosis of
extensive-stage SCLC, the absence of PET-CT may limit the precise
assessment of metabolic activity in metastatic lesions.
In conclusion, the importance of a multidisciplinary
team co-led by ophthalmologists and oncologists, as well as the
integration of radiology, pathology and radiotherapy knowledge for
diagnosis and treatment, is highlighted in the present case.
Additionally, throughout the treatment and follow-up phases of
patients with malignant tumors, relevant vision tests and fundus
monitoring methods should be included in the follow-up plans to
identify ocular metastases as early as possible. Finally, patients
need not only palliative care but also economical and psychological
support, which can optimize treatment continuity and lower the risk
of treatment cessation. This case underscores the need for
comprehensive diagnostic and management strategies to improve early
detection, treatment continuity and quality of life in patients at
risk for ocular metastases.
Acknowledgements
Not applicable.
Funding
The present case report was supported by Jilin University (grant
nos. 24AI098Z, 24AI099Z and 24AI100Z).
Availability of data and materials
The data generated in the present case report are
included in the figures of this article.
Authors' contributions
KW conceptualized the present case report, wrote the
original draft and reviewed and edited the manuscript. FL
systematically collected and verified clinical records, imaging,
pathology, and follow-up data and devised the methodology. CN
performed the formal analysis. CH acquired funding, provided
project administration, resources and supervised the present case
report. YZ prepared the study documents, wrote the original draft,
conducted literature review, contributed to differential diagnosis
and drafted clinical implications. CH directed diagnostic strategy,
validated clinico-pathological correlations, interpreted oncology
data, critically revised manuscript. KW and CH validated the data
and visualized the data in the present case report. KW and CH
confirm the authenticity of all the raw data. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The present case report adheres to ethical
guidelines outlined in the Declaration of Helsinki. Ethical
approval for the present case report was provided by the Ethics
Committee of the Second Hospital of Jilin University (approval no.
2024-348) on August 26, 2024.
Patient consent for publication
Informed consent was obtained from the patient and
his family members for the publication of anonymized clinical
details, images and data in May 2018.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
SCLC
|
small cell lung cancer
|
|
OS
|
overall survival
|
|
RAI
|
right-anterior-inferior
|
|
RPI
|
right-posterior-inferior
|
|
CK
|
cytokeratin
|
|
CgA
|
chromogranin A
|
|
Syn
|
synaptophysin
|
|
CD
|
cluster of differentiation
|
|
TTF-1
|
thyroid transcription factor-1
|
|
LCA
|
leukocyte common antigen
|
|
DWI
|
diffusion-weighted imaging
|
|
MRI
|
magnetic resonance imaging
|
References
|
1
|
Bray F, Laversanne M, Sung H, Ferlay J,
Siegel RL, Soerjomataram I and Jemal A: Global cancer statistics
2022: GLOBOCAN estimates of incidence and mortality worldwide for
36 cancers in 185 countries. CA Cancer J Clin. 74:229–263.
2024.PubMed/NCBI
|
|
2
|
Rudin CM, Brambilla E, Faivre-Finn C and
Sage J: Small-cell lung cancer. Nat Rev Dis Primers. 7:32021.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shields CL, Kalafatis NE, Gad M, Sen M,
Laiton A, Silva AMV, Agrawal K, Lally SE and Shields JA: Metastatic
tumours to the eye. Review of metastasis to the iris, ciliary body,
choroid, retina, optic disc, vitreous, and/or lens capsule. Eye
(Lond). 37:809–814. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Shields CL, Welch RJ, Malik K,
Acaba-Berrocal LA, Selzer EB, Newman JH, Mayro EL, Constantinescu
AB, Spencer MA, McGarrey MP, et al: Uveal metastasis: Clinical
features and survival outcome of 2214 tumors in 1111 patients based
on primary tumor origin. Middle East Afr J Ophthalmol. 25:81–90.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kur J, Newman EA and Chan-Ling T: Cellular
and physiological mechanisms underlying blood flow regulation in
the retina and choroid in health and disease. Prog Retin Eye Res.
31:377–406. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Jager MJ, Shields CL, Cebulla CM,
Abdel-Rahman MH, Grossniklaus HE, Stern MH, Carvajal RD, Belfort
RN, Jia R, Shields JA and Damato BE: Uveal melanoma. Nat Rev Dis
Primers. 6:242020. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Jouhi S, Al-Jamal RT, Täll M, Eskelin S
and Kivelä TT: Presumed incipient choroidal melanoma: Proposed
diagnostic criteria and management. Br J Ophthalmol. 107:412–417.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mahajan A, Crum A, Johnson MH and Materin
MA: Ocular neoplastic disease. Semin Ultrasound CT MR. 32:28–37.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Eisenhauer EA, Therasse P, Bogaerts J,
Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S,
Mooney M, et al: New response evaluation criteria in solid tumours:
Revised RECIST guideline (version 1.1). Eur J Cancer. 45:228–247.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zugazagoitia J and Paz-Ares L:
Extensive-stage small-cell lung cancer: First-line and second-line
treatment options. J Clin Oncol. 40:671–680. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
McKeage MJ: Lobaplatin: A new antitumour
platinum drug. Expert Opin Investig Drugs. 10:119–128. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Oken MM, Creech RH, Tormey DC, Horton J,
Davis TE, McFadden ET and Carbone PP: Toxicity and response
criteria of the eastern cooperative oncology group. Am J Clin
Oncol. 5:649–655. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Farrar JT, Young JP Jr, LaMoreaux L, Werth
JL and Poole MR: Clinical importance of changes in chronic pain
intensity measured on an 11-point numerical pain rating scale.
Pain. 94:149–158. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shah SU, Mashayekhi A, Shields CL, Walia
HS, Hubbard GB III, Zhang J and Shields JA: Uveal metastasis from
lung cancer: Clinical features, treatment, and outcome in 194
patients. Ophthalmology. 121:352–357. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gerba-Górecka K, Romanowska-Dixon B,
Karska-Basta I, Cieplińska-Kechner E and Nowak MS: Clinical
characteristics and management of ocular metastases. Cancers
(Basel). 17:10412025. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Li H, Luo J, Feng Z, Maberley D, Li Y, Wei
W and Liu Y: Uveal metastasis: Clinical characteristics, treatment,
and prognostic factors in a cohort of 161 patients in China. Can J
Ophthalmol. Jan 13–2025.(Epub ahead of print). doi:
10.1016/j.jcjo.2024.12.002. View Article : Google Scholar
|
|
17
|
Arepalli S, Kaliki S and Shields CL:
Choroidal metastasis: Origin, features, and therapy. Indian J
Ophthalmol. 63:122–127. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Jardel P, Sauerwein W, Olivier T,
Bensoussan E, Maschi C, Lanza F, Mosci C, Gastaud L, Angellier G,
Marcy PY, et al: Management of choroidal metastases. Cancer Treat
Rev. 40:1119–1128. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Massagué J and Ganesh K:
Metastasis-initiating cells and ecosystems. Cancer Discov.
11:971–994. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Nguyen DX and Massagué J: Genetic
determinants of cancer metastasis. Nat Rev Genet. 8:341–352. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Fernandes BF, Fernandes LH and Burnier MN
Jr: Choroidal mass as the presenting sign of small cell lung
carcinoma. Can J Ophthalmol. 41:605–608. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Aichouni N, Ziani H, Kamaoui I, Nasri S
and Skiker I: Choroidal metastasis revealing a lung adenocarcinoma:
A case report. Cureus. 13:e189682021.PubMed/NCBI
|
|
23
|
Singh N, Kulkarni P and Aggarwal AN:
Clinical manifestation and outcome of lung cancer patients with
ocular metastasis: 16 Case reports and system of the literature.
Medicine (Baltimore). 91:179–194. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Qu Z, Liu J, Zhu L and Zhou Q: A
comprehensive understanding of choroidal metastasis from lung
cancer. Onco Targets Ther. 14:4451–4465. 2012. View Article : Google Scholar
|
|
25
|
Liu Y, Feng X, Xu Y, Yu S and Wang M:
Clinical manifestation and outcome of lung cancer patients with
ocular metastasis: 16 Case reports and systematic review. Thorac
Cancer. 15:2147–2155. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
John VJ, Jacobson MS and Grossniklaus HE:
Bilateral choroidal metastasis as the presenting sign of small cell
lung carcinoma. J Thorac Oncol. 5:12892010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Anwar J, Amin T, Sarfraz Z, Khalid M, Khan
MS and Abdelhakeem A: Unilateral choroidal metastases as an unusual
presentation of small cell lung cancer. Proc (Bayl Univ Med Cent).
37:870–873. 2024.PubMed/NCBI
|
|
28
|
Dabouz R, Abram P, Rivera JC and Chemtob
S: Mast cells promote choroidal neovascularization in a model of
age-related macular degeneration. J Neuroinflammation. 21:2472024.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Janetos TM, Volpe NJ and Simon SS:
Neuro-ophthalmic manifestations of cancer: A narrative review. Chin
Clin Oncol. 11:252022. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Lin P and Mruthyunjaya P: Retinal
manifestations of oncologic and hematologic conditions. Int
Ophthalmol Clin. 52:67–91. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Baldwin KJ, Zivković SA and Lieberman FS:
Neurologic emergencies in patients who have cancer: Diagnosis and
management. Neurol Clin. 30:101–128. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Yue Y, Ren Y, Lu C, Jiang N, Wang S, Fu J,
Kong M and Zhang G: The research progress on meningeal metastasis
in solid tumors. Discov Oncol. 16:2542025. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Bouhlel L, Hofman V, Maschi C, Ilié M,
Allégra M, Marquette CH, Audigier-Valette C, Thariat J and Hofman
P: The liquid biopsy: A tool for a combined diagnostic and
theranostic approach for care of a patient with late-stage lung
carcinoma presenting with bilateral ocular metastases. Expert Rev
Anticancer Ther. 17:1087–1092. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Konstantinidis L and Damato B: Intraocular
metastases-a review. Asia Pac J Ophthalmol (Phila). 6:208–214.
2017.PubMed/NCBI
|
|
35
|
Maller B, Salvatori S and Tanvetyanon T:
Outcomes of intraocular metastasis from lung cancer in the era of
targeted therapy: A systematic review and pooled analysis. Clin
Lung Cancer. 23:e519–e525. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Bolletta E, De Simone L, Pellegrini M,
Preziosa C, Mastrofilippo V, Adani C, Gentile P, Gozzi F and Cimino
L: Optical coherence tomography in inflammatory and neoplastic
lesions deforming the choroidal profile. Diagnostics (Basel).
13:19912023. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Qu Z, Liu J, Zhu L and Zhou Q: Clinical
features and treatment modalities of rare choroid metastasis from
lung malignancy. Chin Med J (Engl). 135:1628–1630. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Bianciotto C, Shields CL, Guzman JM,
Romanelli-Gobbi M, Mazzuca D Jr, Green WR and Shields JA:
Assessment of anterior segment tumors with ultrasound biomicroscopy
versus anterior segment optical coherence tomography in 200 cases.
Ophthalmology. 118:1297–1302. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Solnik M, Paduszyńska N, Czarnecka AM,
Synoradzki KJ, Yousef YA, Chorągiewicz T, Rejdak R, Toro MD,
Zweifel S, Dyndor K and Fiedorowicz M: Imaging of uveal
melanoma-current standard and methods in development. Cancers
(Basel). 14:31472022. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
National Comprehensive Cancer Network, .
NCCN Clinical Practice Guidelines in Oncology (NCCN
Guidelines®). Small Cell Lung Cancer. Version 1.2025.
2025.
|
|
41
|
Horn L, Mansfield AS, Szczesna A, Havel L,
Krzakowski M, Hochmair MJ and Huemer F: IMpower133: Updated overall
survival (OS) analysis of first-line atezolizumab plus carboplatin
and etoposide in extensive-stage SCLC. Ann Oncol. 30 (Suppl
5):v7132019.
|
|
42
|
Liu SV, Reck M, Mansfield AS, Mok T,
Scherpereel A, Reinmuth N, Garassino MC, De Castro Carpeno J,
Califano R, Nishio M, et al: Updated overall survival and PD-L1
subgroup analysis of patients with extensive-stage small-cell lung
cancer treated with atezolizumab, carboplatin, and etoposide
(IMpower133). J Clin Oncol. 39:619–630. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Li H, Han H, Li C, Wu R, Wang Z, Wang Y,
Zhan P, Lv T, Zhang F, Song Y and Liu H: Efficacy and safety of
first-line PD-1/PD-L1 inhibitor combinations for extensive-stage
small-cell lung cancer: A Bayesian network meta-analysis. Ther Adv
Med Oncol. Oct 24–2023.(Epub ahead of print). View Article : Google Scholar
|
|
44
|
Paz-Ares L, Dvorkin M, Chen Y, Reinmuth N,
Hotta K, Trukhin D, Statsenko G, Hochmair MJ, Özgüroğlu M, Ji JH,
et al: Durvalumab plus platinum-etoposide versus platinum-etoposide
in first-line treatment of extensive-stage small-cell lung cancer
(CASPIAN): A randomised, controlled, open-label, phase 3 trial.
Lancet. 394:1929–1939. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Xie Z, Liu J, Wu M, Wang X, Lu Y, Han C,
Cong L, Li J and Meng X: Real-world efficacy and safety of thoracic
radiotherapy after first-line chemo-immunotherapy in
extensive-stage small-cell lung cancer. J Clin Med. 12:38282023.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Hetta HF, Aljohani HM, Sirag N, Elfadil H,
Salama A, Al-Twalhy R, Alanazi D, Al-Johani MD, Albalawi JH,
Al-Otaibi RM, et al: Synergizing success: The role of anlotinib
combinations in advanced non-small cell lung cancer treatment.
Pharmaceuticals (Basel). 18:5852025. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Sun J, Ren S, Zhao Q, He J, Wang Y and Ren
M: Endostatin-based anti-angiogenic therapy and immune modulation:
Mechanisms and synergistic potential in cancer treatment. Front
Immunol. 16:16238592025. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Liu M, Qiu G, Guan W, Xie X, Lin X, Xie Z,
Zhang J, Qin Y, Du H, Chen X, et al: Induction chemotherapy
followed by camrelizumab plus apatinib and chemotherapy as
first-line treatment for extensive-stage small-cell lung cancer: A
multicenter, single-arm trial. Signal Transduct Target Ther.
10:652025. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Cheng Y, Chen J, Zhang W, Xie C, Hu Q,
Zhou N, Huang C, Wei S, Sun H, Li X, et al: Benmelstobart,
anlotinib and chemotherapy in extensive-stage small-cell lung
cancer: A randomized phase 3 trial. Nat Med. 30:2967–2976. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Thariat J, Boudin L, Loria O, Nguyen AM,
Kodjikian L and Mathis T: How to manage a patient with ocular
metastases? Biomedicines. 10:30442022. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Schmelter V, Heidorn S, Fuerweger C,
Muacevic A, Priglinger SG, Foerster P and Liegl R: Robotic assisted
CyberKnife radiosurgery for the treatment of choroidal metastasis.
Eye (Lond). 35:3376–3383. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Lin IH, Kuo BI and Liu FY: Adjuvant
intravitreal bevacizumab injection for choroidal and orbital
metastases of refractory invasive ductal carcinoma of the breast.
Medicina (Kaunas). 57:4042021. View Article : Google Scholar : PubMed/NCBI
|